Essential IHC Controls: A Comprehensive Guide to Positive and Negative Controls for Reliable Results
This article provides researchers, scientists, and drug development professionals with a complete framework for implementing and validating controls in Immunohistochemistry (IHC) experiments.
Essential IHC Controls: A Comprehensive Guide to Positive and Negative Controls for Reliable Results
Abstract
This article provides researchers, scientists, and drug development professionals with a complete framework for implementing and validating controls in Immunohistochemistry (IHC) experiments. Covering foundational principles, practical methodologies, advanced troubleshooting, and contemporary validation standards, the guide synthesizes current best practices and guidelines, including the latest 2024 CAP update. It is designed to help professionals across both research and clinical settings ensure the specificity, sensitivity, and reproducibility of their IHC data, thereby enhancing the reliability of diagnostic and research outcomes.
The Critical Role of IHC Controls: Ensuring Specificity and Accuracy
Why Controls are Non-Negotiable in IHC Experiments
Immunohistochemistry (IHC) stands as a cornerstone technique in biomedical research and clinical diagnostics, enabling the visualization of specific protein markers within their proper tissue context. However, the validity of interpretations derived from IHC hinges entirely on the implementation of appropriate controls. Despite their critical importance, evidence indicates that up to 80% of published papers omit descriptions of essential controls, potentially leading to irreproducible findings and erroneous scientific conclusions. This comprehensive guide examines the fundamental role of positive and negative controls in IHC experiments, providing researchers with detailed methodologies, validation frameworks, and standardized practices to ensure assay specificity, sensitivity, and reliability.
The Critical Role of Controls in IHC
Immunohistochemistry is no different from any other experimental technique: the quality of the results relies entirely on the analyte, reagents, precise experimental technique, correct application of controls, and accurate interpretation of the data [1]. Simply stated, an immunohistochemical assay that lacks controls cannot be validly interpreted [1]. The absence of proper controls threatens the very foundation of scientific investigation by permitting inaccurate interpretations that can lead to wasted resources, irreproducible results, and erosion of confidence in research findings.
Alarming evidence from an informal survey of 100 articles across nine high-impact journals revealed that up to 80% of papers incorporating IHC data do not mention controls, and 89% of author guidelines for these journals do not require or even mention controls [1]. This oversight at both the research and publication levels underscores a systemic undervaluing of appropriate controls, despite their fundamental importance in validating experimental outcomes. Proper controls are essential to distinguish specific signal from non-specific background, verify reagent performance, and confirm technical execution throughout the complex IHC workflow.
Classification and Implementation of IHC Controls
Positive Controls: Validating Assay Performance
Positive controls are specimens known to express the target antigen in a specific location and pattern, serving to demonstrate that the staining protocol is successfully performed and providing the expected level of sensitivity and specificity as characterized during technical optimization [2] [3].
Types of Positive Controls:
- Anatomical Positive Controls: Utilize tissue with known expression of the target protein, where the presence and location of the antigen have been previously established through other experimental evidence [1].
- Internal Positive Controls: Leverage known sites of target expression within the experimental specimen itself, providing inherent validation without requiring separate tissue sections [1].
- External Positive Controls: Employ separate specimens or slides confirmed to contain the molecule targeted by the antibody, run in parallel with experimental samples [1].
The most rigorous positive control is the positive anatomical control, where the presence of the antigen in the specimen is known a priori and is not the target of the experimental treatment [1]. For example, an assay using an antibody specific for insulin should include sections of pancreas containing islets of Langerhans, with the antibody selectively visualizing only the insulin-producing beta cells [1].
Negative Controls: Establishing Specificity
Negative controls demonstrate that the observed staining results specifically from interaction between the target epitope and the antibody's paratope, rather than non-specific interactions or technical artifacts [1]. These controls are known not to express the target antigen and are essential for checking non-specific signals and false-positive results [2].
Critical Negative Control Modalities:
Table 1: Essential Negative Controls for IHC Validation
| Control Type | Composition | Purpose | Interpretation |
|---|---|---|---|
| No Primary Antibody Control | Tissue section incubated with antibody diluent alone, followed by secondary antibodies and detection reagents [2] | Verifies staining is produced by primary antibody binding, not by detection system or specimen [2] | Any staining indicates non-specific binding of secondary antibody or detection components |
| Isotype Control | Tissue incubated with non-immune antibody of the same isotype and concentration as primary antibody [2] [4] | Controls for non-specific interactions of the antibody with tissue components [2] | Background staining should be negligible and distinct from specific staining |
| Absorption Control | Tissue incubated with antibody pre-absorbed with excess immunogen [2] [3] | Demonstrates specificity of antibody binding to target antigen [2] | Little or no staining expected; more reliable with peptide immunogens [2] |
| Biological Negative Control | Tissue section known not to express the target protein [2] [3] | Checks for non-specific signal and false-positive results [2] | Any staining indicates non-specific binding or cross-reactivity |
A profoundly common error in IHC publications is the misuse of the "no primary antibody control" as evidence for the specificity of staining for the antigen targeted by the antibody [1]. This control only validates the specificity of the secondary antibody and detection system; it does not provide information about the primary antibody's specificity [1]. The proper negative control for primary antibody specificity is substitution with serum or isotype-specific immunoglobulins at the same protein concentration as the primary antibody [1].
Advanced Control Methodologies and Quantitative Applications
Innovative Control Technologies: Peptide-Based Standards
Emerging technologies have introduced peptide immunohistochemistry controls as a novel quality control format that offers advantages in high-throughput automated manufacture and standardization [5]. These controls consist of formalin-fixed peptide epitopes covalently attached to glass microscope slides, behaving immunochemically similarly to native protein in tissue sections [5].
In a national validation study involving 109 clinical laboratories, researchers demonstrated a strong correlation (r = 0.87) between a laboratory's ability to properly stain formalin-fixed peptide controls and their ability to properly stain a 3+ HER-2 formalin-fixed tissue section mounted on the same slide [5]. This technology enables quantitative quality assurance methods traditionally used in clinical chemistry laboratories, such as Levy-Jennings charting and Westgard rules, to be applied to IHC, facilitating improved assay precision and linearity [5].
Experimental Design and Validation Protocols
Proper validation of IHC assays requires systematic approaches and adherence to established guidelines. For laboratory-developed tests (LDTs) and modified FDA-cleared/approved tests, comprehensive validation is mandatory [6]. The College of American Pathologists (CAP) provides specific recommendations for validation cohorts:
- Predictive markers require a minimum of 20 positive and 20 negative cases [6]
- Non-predictive markers require a minimum of 10 positive and 10 negative cases [6]
- Overall concordance threshold of 90% is typically used, with any discordant results scrutinized to identify sensitivity or specificity issues [6]
The validation process involves multiple critical stages, including optimization to establish optimal staining conditions, validation/verification to confirm performance characteristics, clinical implementation, and ongoing assay maintenance through quality monitoring and proficiency testing [6].
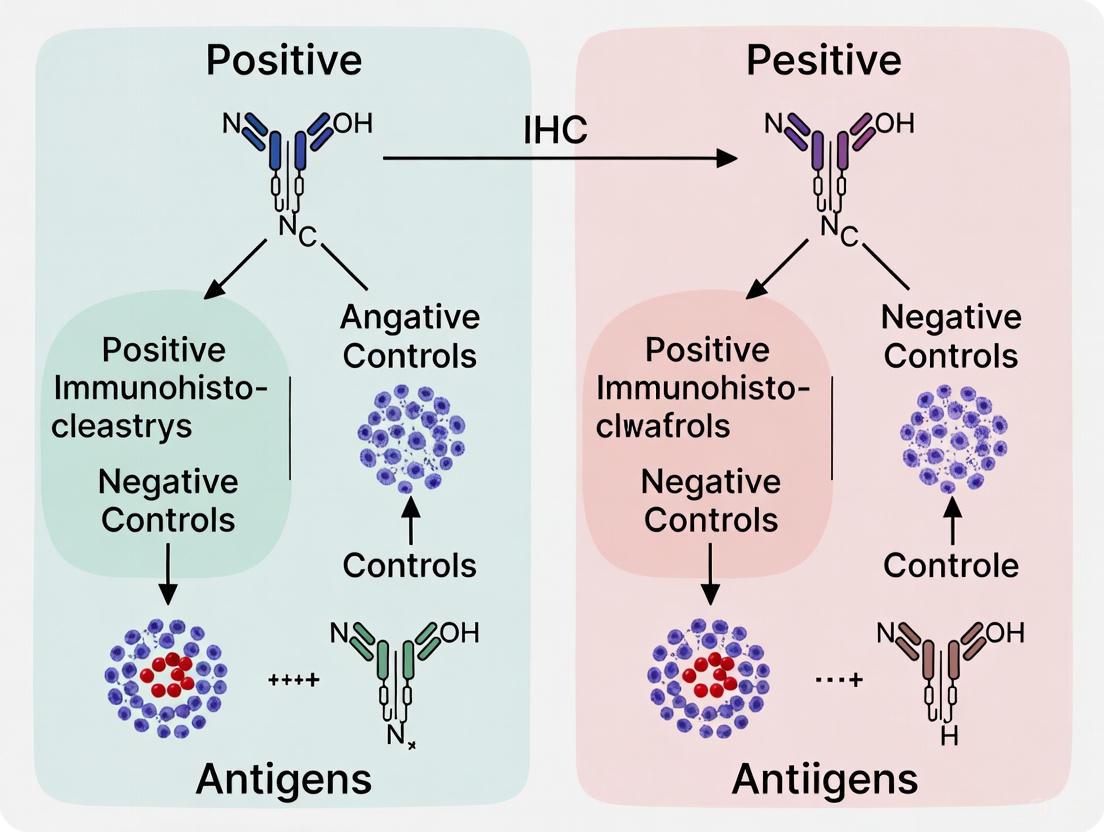
Standardized Workflows and Visualization
The complex workflow of IHC presents multiple variables that must be carefully controlled throughout the experimental process. The following diagram illustrates key decision points and control requirements in a standard IHC protocol:
IHC Experimental Workflow with Control Integration
Essential Reagents and Research Solutions
Successful IHC experimentation requires carefully selected reagents and materials, each serving specific functions in the staining workflow and validation process.
Table 2: Essential Research Reagent Solutions for IHC
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Primary Antibodies | Monoclonal (clone-specific), Polyclonal | Recognize target epitopes; require validation for specific applications [7] [8] |
| Detection Systems | HRP-conjugated polymers, Avidin-biotin complexes | Amplify signal while minimizing background; critical for sensitivity [7] |
| Chromogens | DAB (brown), AP Red, AEC | Produce insoluble colored precipitate at antigen site [7] [9] |
| Antigen Retrieval Reagents | Citrate buffer (pH 6.0), EDTA (pH 8.0), Proteolytic enzymes | Reverse formaldehyde cross-linking to expose epitopes [9] [8] |
| Blocking Reagents | Normal serum, Casein, BSA | Reduce non-specific antibody binding and background staining [9] [4] |
| Control Materials | Known positive tissues, Isotype controls, Peptide arrays | Validate assay performance and antibody specificity [2] [5] |
| Fixation Media | Neutral buffered formalin, Paraformaldehyde | Preserve tissue architecture and antigenicity while preventing degradation [9] [10] |
Interpretation Framework and Troubleshooting
The following diagram provides a logical framework for interpreting control results and their implications for experimental validity:
Control Result Interpretation Decision Tree
Proper interpretation of IHC controls enables accurate troubleshooting of experimental issues:
- False-Positive Results: Occur when negative controls show staining, indicating non-specific binding of antibodies, inadequate blocking, or cross-reactivity [1] [3]
- False-Negative Results: Occur when positive controls fail to stain, indicating problems with antigen retrieval, antibody concentration, detection system sensitivity, or reagent degradation [1] [6]
- Inconsistent Staining: May result from variations in fixation, section thickness, or reagent application, highlighting the need for standardized protocols [7] [4]
Controls in immunohistochemistry are fundamentally non-negotiable components of experimental design, essential for producing valid, interpretable, and reproducible data. The integration of appropriate positive controls, multiple negative control modalities, and emerging technologies like peptide-based standards provides a robust framework for validating IHC assays. As the field moves toward increasingly quantitative applications, implementation of rigorous controls and standardized validation protocols becomes ever more critical. By adhering to these principles, researchers can ensure the reliability of their findings, contribute to reproducible science, and maintain confidence in the vital role of immunohistochemistry in both research and clinical diagnostics.
Defining Positive and Negative Tissue Controls
In immunohistochemistry (IHC), the validity of interpretations hinges entirely on the use of appropriate positive and negative controls [1]. These controls are not merely supplementary; they are fundamental components that help distinguish specific staining from artifacts, thereby ensuring the reliability and reproducibility of experimental results [11]. Without proper controls, investigators risk both false-positive and false-negative conclusions, which can lead to erroneous scientific conclusions and clinical misdiagnoses [1]. This guide objectively compares traditional tissue controls against innovative alternatives, providing researchers with a framework for implementing robust quality assurance in IHC workflows.
Core Principles of IHC Controls
Positive Tissue Controls
A positive tissue control is a specimen known to express the target antigen in a specific location (e.g., a particular cell type or intracellular compartment) [1]. Its purpose is to verify that the entire IHC protocol—from antigen retrieval to detection—is functioning correctly. A lack of staining in a positive control indicates a technical problem requiring protocol troubleshooting [11]. The most rigorous form is the positive anatomical control, which can be an internal site of known expression within the specimen itself or an external separate specimen known to contain the target [1].
Negative Tissue Controls
A negative tissue control is a specimen confirmed not to express the target protein [11]. Any observed staining in this control indicates non-specific binding or background interference, revealing potential false-positive results in test samples [11]. Knockdown (KD) and knockout (KO) tissues, where the expression of the target protein is significantly reduced or eliminated, are considered highly reliable negative controls [11].
Comparative Analysis of Control Methodologies
The following table summarizes the key characteristics of different control types used in IHC.
Table 1: Comparison of IHC Control Types and Their Applications
| Control Type | Definition & Purpose | Key Advantages | Inherent Challenges |
|---|---|---|---|
| Traditional Patient Tissue Controls | Tissue sections from prior patient cases with known antigen expression status [12]. | Readily available in pathology departments; pathologists are familiar with interpretation. | Scarce for rare targets (e.g., ALK in lung cancer) [13] [14]; ethical issues around patient consent; heterogeneous expression [12]. |
| Genetically Modified Cell Lines (CLFs) | Cell suspensions from engineered cell lines that do or do not express the target antigen, applied in liquid form [13] [14]. | Consistent, renewable supply; defined expression levels; suitable for automated systems [13]. | May not fully recapitulate the complex tissue microenvironment of patient samples. |
| Isotype Controls | An antibody of the same class and host species as the primary antibody but with no target specificity [11]. | Controls for nonspecific binding mediated by the Fc region or other protein interactions [1]. | Does not validate the specificity of the primary antibody's paratope for its intended epitope. |
Performance Data: Traditional vs. Liquid Controls
A 2025 study on ALK testing in lung adenocarcinoma provides quantitative performance data for an automated system using Controls in Liquid Form (CLFs). The results demonstrate that the novel antibody and automated platform can achieve performance metrics on par with established clinical standards [13] [14].
Table 2: Performance Data of BP6165 Antibody with CLFs on LYNX480 PLUS Platform
| Performance Metric | Result | Experimental Context |
|---|---|---|
| Sensitivity | 98.30% | Compared to FISH in 87 lung adenocarcinoma biopsy specimens [13] [14]. |
| Specificity | 100% | Compared to FISH in 87 lung adenocarcinoma biopsy specimens [13] [14]. |
| Control Application | More regular circular shape and better cell distribution vs. manual application. | Automated application of CLFs using the QC module of the LYNX480 PLUS system [13]. |
Experimental Protocols for Control Validation
Protocol: Establishing Controls in Liquid Form (CLFs)
The methodology below is adapted from a study validating ALK CLFs on an automated staining system [13] [14].
- Materials: Genetically modified cell lines (e.g., ALK positive CLF Catalog No.: BX30026P and ALK negative CLF Catalog No.: BX30026N), automated IHC staining system with QC module (e.g., LYNX480 PLUS), slides, and optimized IHC reagents.
- CLF Application: Use the system's QC module to automatically pipette CLFs onto target slides by scanning the quick response (QR) code on the CLF vial. The droplet is then dried and fixed in minutes using a built-in heater.
- Staining Protocol: Perform IHC using the optimized protocol. For the cited study, this included antigen retrieval with EDTA (pH 9.0) at 100°C for 60 min, peroxidase block for 5 min, incubation with primary antibody (e.g., BP6165 at 1:200 dilution) for 30 min at room temperature, and detection with a conventional DAB system [13].
- Validation: Compare the staining pattern, droplet shape, and cell distribution of automatically applied CLFs against manually applied ones. The method yielding superior consistency and a more regular circular shape should be selected for clinical use [13].
Protocol: Traditional Control Validation as per CAP Guidelines
The College of American Pathologists (CAP) updated its guidelines in 2024, providing a standardized framework for IHC assay validation [15] [16].
- Validation Scope: All laboratory-developed IHC assays must be analytically validated, and all FDA-cleared/approved assays must be verified before reporting patient results [16].
- Sample Size: For initial analytic validation of laboratory-developed assays, a minimum of 10 positive and 10 negative tissues is required. For predictive marker assays (e.g., HER2, ALK, PD-L1), a minimum of 20 positive and 20 negative tissues is required [15] [16].
- Concordance Requirement: Laboratories must achieve at least 90% overall concordance between the new assay and the comparator method or expected results [15] [16].
- Comparator Methods: Validation can use several comparators, ordered here from most to least stringent:
- Comparison to IHC results from protein-calibrated cell lines.
- Comparison with a non-IHC method (e.g., FISH, flow cytometry).
- Comparison with results from another laboratory using a validated assay.
- Comparison with prior testing of the same tissues in the same lab.
- Comparison against expected architectural and subcellular localization [15].
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Reagent Solutions for Consistent IHC Results
| Reagent / Material | Function | Considerations for Use |
|---|---|---|
| Antigen Retrieval Solutions | Reverses formaldehyde-induced crosslinks to unmask epitopes (e.g., Citrate or EDTA buffer) [17]. | The optimal solution (HIER vs. enzymatic) and pH are antibody-dependent and must be determined during validation [17]. |
| Antibody Diluent | Dilutes the primary antibody to the working concentration. | The choice of diluent can dramatically affect signal strength and must be optimized for each antibody [17]. |
| Blocking Buffers | Reduces nonspecific binding of antibodies to tissue components (e.g., normal serum, animal-free blockers) [17]. | Helps minimize background staining. |
| Detection System | A polymer-based reagent that binds the primary antibody and generates a visible signal (chromogenic or fluorescent) [17]. | Biotin-free, polymer-based systems avoid background from endogenous biotin and offer enhanced sensitivity [17]. |
| Chromogen (e.g., DAB) | Forms an insoluble, colored precipitate at the site of antibody binding [13] [17]. | Different DAB substrate kits vary in sensitivity; the substrate should be qualified with the detection system [17]. |
| 2-(Decan-2-YL)thiophene | 2-(Decan-2-yl)thiophene|High-Purity Reference Standard | 2-(Decan-2-yl)thiophene is a high-purity thiophene derivative for research applications in medicinal chemistry and material science. For Research Use Only. Not for human or veterinary use. |
| 3-Chlorooctane-1-thiol | 3-Chlorooctane-1-thiol, CAS:61661-23-2, MF:C8H17ClS, MW:180.74 g/mol | Chemical Reagent |
Technological Innovations and Workflow Integration
The IHC control workflow is evolving with new technologies that complement traditional methods. Automated staining systems with integrated quality control modules, such as the LYNX480 PLUS, can standardize the application of liquid controls [13] [14]. Furthermore, artificial intelligence (AI) algorithms are now being used to quantitatively monitor staining quality and trace variations in control cell lines over time, offering an objective alternative to visual assessment [12]. In the research domain, deep generative models are being explored for "virtual staining," which aims to predict IHC staining patterns from H&E-stained images, though this remains an emerging technology [18].
The following diagram illustrates the integrated workflow for IHC quality control, combining traditional and novel approaches.
The definitive establishment of positive and negative controls remains a non-negotiable standard in IHC for both research and clinical diagnostics. While traditional patient tissue controls are a familiar benchmark, their limitations—scarcity, heterogeneity, and ethical concerns—are driving the adoption of innovative alternatives [13] [14] [12]. Genetically defined controls in liquid form (CLFs) offer a standardized, renewable resource that is particularly well-suited for automated platforms and demonstrates excellent performance in analytical validation [13] [14]. Adherence to updated evidence-based guidelines, such as those from CAP, and the strategic integration of new technologies like AI-powered quality monitoring, provides a robust pathway for laboratories to ensure the accuracy, reliability, and reproducibility of their IHC assays, which is fundamental for both scientific discovery and patient care [15] [12] [16].
In immunohistochemistry (IHC), the validity of experimental results hinges on the proper use of controls that distinguish specific staining from background artifacts. Negative reagent controls are essential for demonstrating that observed staining results from specific antibody-antigen interactions rather than non-specific binding. Among these, the no primary antibody control and isotype control serve distinct but complementary roles in validating IHC specificity. These controls are particularly crucial in diagnostic IHC and research applications where false-positive results could lead to incorrect scientific conclusions or clinical misdiagnoses [1] [19]. This guide examines the principles, applications, and experimental implementation of these two fundamental negative controls within the broader context of IHC quality assurance.
Theoretical Foundations: How Negative Reagent Controls Work
The Problem of Background Staining
Background staining in IHC can arise from multiple sources. Fc receptors present on various cell types (including B cells, macrophages, monocytes, and dendritic cells) can bind the constant (Fc) region of antibodies independently of their antigen specificity. Additional sources include cellular autofluorescence, non-specific antibody interactions with lipids, carbohydrates, or other cellular molecules, and endogenous enzymes that interact with detection systems [20] [21]. Without appropriate controls, this background staining can be misinterpreted as specific signal, compromising experimental validity.
The Role of Negative Reagent Controls
Negative reagent controls are designed to identify the source and extent of non-specific background staining. They help researchers distinguish true positive signals from artifacts caused by non-specific binding, autofluorescence, or protocol errors [22]. According to expert guidelines, the proper use of negative controls is essential for building a convincing case for the presence or absence of a probed molecule in tissue samples [1].
Direct Comparison: No Primary Antibody vs. Isotype Controls
Table 1: Characteristics of Negative Reagent Controls in IHC
| Parameter | No Primary Antibody Control | Isotype Control |
|---|---|---|
| Primary Purpose | Detects non-specific binding of secondary antibody and detection system [1] [22] | Evaluates non-specific binding caused by the constant (Fc) region of the primary antibody [20] [21] |
| Preparation | Primary antibody omitted and replaced with antibody diluent; all other steps unchanged [22] | Primary antibody replaced with matched isotype antibody at same concentration [20] [21] |
| What It Identifies | Secondary antibody non-specificity, endogenous enzyme activity, inadequate blocking [1] | Fc receptor binding, non-specific interactions via Fc region [20] [21] |
| Limitations | Does not control for primary antibody non-specificity [1] | Does not detect Fab-mediated non-specific binding [21] |
| Optimal Result | No staining observed [22] | Minimal to no staining observed [20] |
| Required Matching Parameters | None for primary antibody | Host species, isotype, subclass, conjugation, concentration [20] [21] |
Table 2: Application Scenarios for Negative Controls
| Experimental Scenario | Recommended Control | Rationale |
|---|---|---|
| Initial assay validation | Both controls | Comprehensive assessment of both secondary and primary antibody issues [19] |
| Routine IHC staining | No primary antibody control (if using polymer-based detection systems) | CAP guidelines indicate this may be sufficient for polymer-based systems [19] |
| Working with Fc receptor-rich tissues (spleen, lymph nodes) | Isotype control essential | High likelihood of Fc-mediated binding [20] [21] |
| Using new primary antibody | Both controls | Complete characterization of antibody performance [20] |
| Troubleshooting high background | Sequential application | Identify specific source of background staining [22] |
Experimental Protocols and Implementation
Protocol for No Primary Antibody Control
- Sample Preparation: Use serial sections from the same tissue block as test samples [19]
- Fixation and Processing: Identical to test sections
- Primary Antibody Step: Omit primary antibody and incubate with antibody diluent only [22]
- Detection System: Apply the same secondary antibody and detection reagents as test sections
- Visualization: Use identical chromogenic or fluorescent development conditions
- Interpretation: Any staining observed indicates non-specific binding of the secondary antibody or detection system components [1]
Protocol for Isotype Control
- Control Selection: Choose an isotype control antibody that matches:
- Concentration Matching: Use the same concentration (μg/mL) as the primary antibody [21]
- Incubation Conditions: Identical temperature, duration, and buffer conditions
- Detection: Use the same detection system and development conditions
- Interpretation: Staining indicates non-specific binding via the Fc region; true specific staining should significantly exceed isotype control staining [20]
Advanced Applications in Precision Oncology and Drug Development
The proper implementation of negative controls has become increasingly important in translational research and precision medicine. With the expansion of companion diagnostics and targeted therapies, IHC assays for biomarkers such as ALK, PD-L1, HER2, and TROP2 require exceptional specificity [23] [14]. For example, in ALK IHC testing for lung adenocarcinoma, appropriate controls are essential for determining patient eligibility for ALK tyrosine kinase inhibitors [14].
Recent advancements include the development of automated quality control systems that incorporate standardized controls in liquid form (CLFs) prepared from genetically modified cell lines. These systems provide consistent application of controls and reduce the consumption of scarce patient tissue resources [14].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Implementing Negative Controls
| Reagent Type | Specific Examples | Function in Negative Controls |
|---|---|---|
| Isotype Controls | Mouse IgG1 [MOPC-21], Mouse IgG2b [MPC-11], Chicken IgY | Matched non-specific antibodies for detecting Fc-mediated binding [21] |
| Antibody Diluents | Protein-stabilized buffers with carrier proteins | Maintain consistent protein concentration when omitting primary antibody [22] |
| Polymer-Based Detection Systems | HRP-polymer conjugates, AP-polymer conjugates | Reduce endogenous biotin interference; decrease need for negative reagent controls [19] |
| Blocking Reagents | Normal serum, BSA, non-fat dry milk | Reduce non-specific binding; critical for both controls [24] |
| Automated Staining Systems | VENTANA BenchMark, LYNX480 PLUS | Standardize application of controls and test antibodies [14] |
| 2-Undecene, 5-methyl- | 2-Undecene, 5-methyl-, CAS:56851-34-4, MF:C12H24, MW:168.32 g/mol | Chemical Reagent |
| 3-Chloro-1-methoxyheptane | 3-Chloro-1-methoxyheptane, CAS:53970-69-7, MF:C8H17ClO, MW:164.67 g/mol | Chemical Reagent |
Both no primary antibody controls and isotype controls are essential components of a rigorous IHC quality control program. While the no primary antibody control specifically addresses non-specific binding of the detection system, the isotype control evaluates Fc-mediated non-specific binding of the primary antibody itself. The optimal use of these controls depends on the experimental context, with comprehensive validation requiring both controls during initial assay development. As IHC continues to evolve with multiplexed staining, digital pathology, and AI-assisted analysis, proper implementation of these fundamental controls remains essential for generating reliable, reproducible data in both research and diagnostic applications.
The Principle of the Blocking Peptide (Pre-absorption) Control
The blocking peptide control, also known as the pre-absorption control, serves as a critical experimental tool for validating antibody specificity in immunohistochemistry (IHC) and other immunoassays. This control operates on the principle of competitive binding, where the antibody is pre-incubated with an excess of the immunizing peptide before application to the tissue sample. When properly executed, this process should abolish specific staining, confirming that the antibody binding is target-specific. This guide examines the technical performance, experimental protocols, and limitations of the blocking peptide control within the broader context of IHC positive and negative controls, providing researchers with objective data for informed experimental design.
Immunohistochemistry relies on the specific recognition of an epitope by an antibody to visualize protein expression within the context of preserved tissue structure [25]. However, antibody binding is susceptible to non-specific interactions that can generate false positive results, compromising data interpretation. The blocking peptide control addresses this vulnerability by providing a mechanism to distinguish specific from non-specific binding [26]. Within the hierarchy of IHC controls, which includes no-primary controls, isotype controls, and tissue controls, the pre-absorption control serves as a unique negative control that directly probes antibody-epitope interaction specificity [27] [28]. Unlike tissue controls that validate overall assay performance, the blocking peptide control specifically validates the antibody reagent itself, making it an indispensable tool for rigorous antibody validation, particularly for polyclonal antibodies which recognize multiple epitopes and are more prone to non-specific binding [29].
Fundamental Principle and Mechanism
The core principle of the blocking peptide control revolves around competitive binding. Blocking peptides are short amino acid sequences corresponding to the specific epitope recognized by the primary antibody [26]. These peptides are identical to the antigenic sequence used during antibody generation, allowing them to bind with high affinity to the antibody's paratope [30].
The mechanism follows these essential steps:
- Pre-incubation: The primary antibody is incubated with an excess of blocking peptide before application to the tissue section [29] [30].
- Binding Site Occupation: The blocking peptide binds specifically to the antibody's antigen-binding sites, occupying all available paratopes [26].
- Neutralization: The antibody, now complexed with peptide, is functionally "neutralized" and unable to bind to the target epitope present in the tissue sample [29].
- Specific Signal Abolition: When this blocked antibody solution is applied to the tissue, any staining that disappears compared to the control (antibody alone) is confirmed as specific binding [29] [30].
The critical interpretation is straightforward: complete or substantial loss of signal in the blocked sample confirms the antibody's specificity for the target epitope, while persistent staining indicates non-specific binding to off-target epitopes [27] [30].
Figure 1 | Competitive Binding Mechanism of Blocking Peptide Control. The primary antibody is pre-incubated with the blocking peptide, forming a complex that cannot bind the target epitope in the tissue, resulting in no signal. In standard IHC, the unblocked antibody binds the epitope, producing a detectable signal.
Comparative Performance of IHC Controls
A comprehensive IHC validation strategy employs multiple control types, each with distinct functions and limitations. The blocking peptide control occupies a specific niche, primarily addressing antibody specificity rather than overall assay conditions.
Table 1: Comparison of Key IHC Negative Controls
| Control Type | Primary Function | Key Interpretation | Major Limitations |
|---|---|---|---|
| Blocking Peptide [27] [29] [26] | Validate antibody specificity for the target epitope. | Loss of signal confirms specific binding. | - May block specific and cross-reactive binding equally [31].- Peptide may itself bind tissue non-specifically [28]. |
| No Primary Antibody [27] [28] | Detect non-specific binding of secondary antibody and detection reagents. | No staining should be observed. | Does not validate primary antibody specificity. |
| Isotype Control [28] | Assess non-specific binding caused by the immunoglobulin framework. | Staining should not resemble specific pattern. | Does not confirm that the primary antibody's paratope binds the correct target. |
| Negative Tissue Control [27] | Identify non-specific antibody binding in a biological context. | No staining in known negative tissue. | Genetically modified tissues (KO/KD) can be difficult to obtain [27]. |
The blocking peptide control is particularly powerful because it directly probes the antibody-antigen interaction. However, a significant limitation noted in peer-reviewed literature is that pre-absorption can block all antibody binding—both to the intended target and to cross-reactive epitopes. This can create an illusion of specificity if the antibody cross-reacts with non-target proteins, as the blocking peptide will abolish all staining, misleading the researcher into believing the antibody is specific [31]. Therefore, this control should be used in conjunction with other validation methods, such as tissue controls from knockout animals, for conclusive specificity determination [31].
Detailed Experimental Protocol and Reagents
Implementing a robust blocking peptide control requires careful attention to reagent preparation and incubation conditions. The following protocol is adapted from established methodologies [29] [30].
Reagent Preparation
- Blocking Buffer: Phosphate-buffered saline (PBS) with 1% Bovine Serum Albumin (BSA) is commonly used for IHC [29].
- Antibody Solution: Prepare the primary antibody at its predetermined optimal working dilution in blocking buffer. A typical solution may contain 97.65% PBS, 0.3% Triton X-100 (0.05% for extracellular targets), 0.05% Tween-20, and 2% normal serum from the species in which the secondary antibody was raised [30].
- Blocking Peptide Solution: Reconstitute lyophilized peptide according to the manufacturer's datasheet, typically in sterile PBS [30].
Step-by-Step Protocol
- Preparation: Prepare identical tissue sections on slides, following standard fixation, permeabilization, and (if required) antigen retrieval protocols [30] [25].
- Antibody Division: Dilute the primary antibody to its optimal concentration and divide the solution equally into two tubes labeled "Antibody Alone" and "Antibody + Peptide" [29] [30].
- Peptide Incubation: To the "Antibody + Peptide" tube, add the blocking peptide. A 10-fold weight excess of peptide relative to the antibody is widely recommended to ensure complete saturation of binding sites [30] [28]. For example, if using 1 µg of antibody in 2 mL of buffer, add at least 10 µg of total peptide [29].
- Incubation: Incubate the "Antibody + Peptide" mixture with agitation for 1 hour at room temperature or overnight at 4°C [29] [30].
- Staining: Apply the "Antibody Alone" solution to one tissue section and the "Antibody + Peptide" solution to the duplicate section. Process both slides simultaneously through the remaining IHC steps (secondary antibody incubation, detection, counterstaining, mounting) under identical conditions [29].
- Imaging and Analysis: Image both slides using the same microscope and settings. Compare the staining patterns. The specific signal will be absent or drastically reduced in the peptide-blocked sample [29] [30].
Figure 2 | Blocking Peptide Control Workflow. The primary antibody solution is divided, and one portion is pre-incubated with a excess of blocking peptide. Both solutions are applied to duplicate tissue sections and processed identically. Loss of signal in the peptide-blocked sample confirms specific antibody binding.
The Scientist's Toolkit: Essential Reagents
Table 2: Key Research Reagent Solutions for Blocking Peptide Experiments
| Reagent | Function | Critical Specification |
|---|---|---|
| Primary Antibody | Binds specifically to the target protein of interest in the tissue. | Host species, clonality (monoclonal/polyclonal), and optimal working dilution must be predetermined. |
| Blocking Peptide [29] [26] [30] | Competes with the tissue antigen for binding to the primary antibody's paratope. | Must correspond exactly to the immunogen sequence used to generate the antibody. |
| Normal Serum [30] | Blocks non-specific binding sites in the tissue to reduce background noise. | Should be from the same species as the host of the secondary antibody. |
| Secondary Antibody | Conjugated to a fluorophore or enzyme, it binds the primary antibody for detection. | Must be highly cross-adsorbed against immunoglobulins from other species to minimize cross-reactivity. |
| lithium;prop-1-enylbenzene | Lithium;prop-1-enylbenzene|C9H9Li | Lithium;prop-1-enylbenzene (C9H9Li) is an organolithium compound for research, notably in polymer synthesis. This product is For Research Use Only. |
| Peroxide, nitro 1-oxohexyl | Peroxide, nitro 1-oxohexyl|C6H11NO5|[Your Company] | Peroxide, nitro 1-oxohexyl (C6H11NO5) is For Research Use Only. It is a high-purity reagent for specialized chemical research. Not for human or veterinary use. |
The blocking peptide control remains a fundamental tool for demonstrating antibody specificity in IHC workflows. Its direct mechanism of action, which competitively inhibits antibody binding, provides compelling evidence that an observed staining pattern is specific. However, researchers must be aware of its principal limitation: a positive result (loss of signal) confirms the antibody is binding to the peptide's sequence, but does not definitively rule out cross-reactivity with other proteins containing similar epitopes [31].
Therefore, within a robust IHC validation framework, the blocking peptide control should be considered a necessary but not sufficient test for antibody specificity. It functions most effectively when integrated with a panel of other controls, including no-primary controls, isotype controls, and—most definitively—genetically validated negative tissue controls (e.g., knockout tissues) [27] [31]. For researchers and drug development professionals, this multi-pronged approach to antibody validation, incorporating the blocking peptide control as a key element, is essential for generating reliable, interpretable, and reproducible data that can confidently support scientific conclusions and therapeutic development.
Assessing Endogenous Background and Autofluorescence
In immunohistochemistry (IHC) and immunofluorescence (IF), the accurate detection of specific antibody-antigen interactions is paramount. However, non-specific signals from endogenous background and autofluorescence can profoundly compromise data integrity, potentially leading to false positives and erroneous biological interpretations [32] [33]. These phenomena represent a significant challenge in both research and clinical diagnostics, as they can obscure specific signals, reduce assay sensitivity, and increase background noise [32] [34].
Within the critical framework of positive and negative controls for IHC experiments, understanding and managing autofluorescence is a cornerstone of robust assay validation [35]. This guide provides a comparative analysis of the primary sources of these non-specific signals and the methods available to assess and mitigate them, providing researchers with the experimental data and protocols necessary to enhance the reliability of their imaging data.
Endogenous background and autofluorescence arise from different mechanisms. Endogenous background typically refers to non-antibody-mediated signals, such as enzymatic activity or endogenous biotin [33]. In contrast, autofluorescence is the inherent fluorescence emitted by certain molecules when excited by light, which is prominent in the green channel and can interfere with common fluorophores like Alexa Fluor 488 and FITC [32].
The table below catalogs the common sources of these non-specific signals and their origins.
Table 1: Common Sources of Non-Specific Signal in Biological Samples
| Source Type | Specific Source | Description / Cause of Interference |
|---|---|---|
| Endogenous Molecules | Collagen & Elastin | Components of the extracellular matrix that autofluoresce [32] [33]. |
| Lipofuscin | A pigmented byproduct of intracellular catabolism that accumulates in post-mitotic cells like neurons and myocytes [32]. | |
| Riboflavin (B2), NADH | Metabolic coenzymes with inherent fluorescence [32] [33]. | |
| Heme Groups | Found in red blood cells and hemoproteins like hemoglobin; a common cause of background [32] [33]. | |
| Aromatic Amino Acids | Phenylalanine, tryptophan, and tyrosine [32]. | |
| Fixation-Induced | Aldehyde Fixatives | Formaldehyde and glutaraldehyde can react with amine groups to form fluorescent Schiff's bases [32] [33]. |
| Laboratory Reagents | Phenol Red | A media supplement that should be avoided for live-cell imaging [32]. |
| Plastic Ware | Plastic microplates and cell culture flasks can autofluoresce [32]. |
Assessment and Comparison of Mitigation Strategies
Various strategies have been developed to manage autofluorescence, each with distinct principles, advantages, and limitations. The choice of method depends on factors such as sample type, fixation method, and the application being performed [32].
Fluorophore Selection and Spectral Resolution
Choosing fluorophores that emit in spectral regions with low sample autofluorescence is a straightforward and effective first step. Near-infrared (NIR) fluorophores are particularly valuable as autofluorescence is often most prominent in the green spectrum [32]. For researchers using GFP tags, which are susceptible to interference, switching to an anti-GFP antibody conjugated to a fluorophore in a different channel (e.g., red) can move the signal away from the green autofluorescence [32].
Advanced instrumentation like spectral flow cytometry and fluorescence lifetime imaging microscopy (FLIM) offer powerful solutions by separating the specific immunofluorescence signal from the autofluorescence based on their full spectral signatures or fluorescence decay rates, respectively [32].
Chemical and Photobleaching Treatments
Several chemical treatments can effectively reduce autofluorescence. Sudan black B has been successfully used to quench autofluorescence in various tissues, including murine renal tissue [32]. Similarly, incubation in a solution of 5% Hâ‚‚Oâ‚‚ can help reduce background [32]. For aldehyde-induced fluorescence, treatment with sodium borohydride (e.g., 1 mg/mL for 30-40 minutes) neutralizes Schiff's bases by reducing them into non-fluorescent salts [32].
Photobleaching, which involves exposing the sample to strong light prior to antibody incubation, can also diminish autofluorescence by bleaching the fluorescent molecules present in the sample before the experimental staining [32].
Comparative Analysis of Mitigation Techniques
The following table provides a structured comparison of the primary methods for managing autofluorescence, summarizing key experimental data and considerations.
Table 2: Comparison of Autofluorescence Mitigation Strategies
| Method | Principle | Key Experimental Protocol / Data | Advantages | Limitations / Side Effects |
|---|---|---|---|---|
| Spectral Imaging | Separates signals based on full spectral signature [32]. | Used in spectral flow cytometry and fluorescence lifetime imaging (FLIM) [32]. | High-information content; can resolve multiple targets. | Requires specialized, often expensive, instrumentation. |
| Chemical Quenching (Sudan Black B) | Binds to and quenches autofluorescent compounds [32]. | Incubate tissue sections with 0.1-0.3% Sudan Black B for 20-30 minutes followed by washing [32]. | Effective against broad-spectrum autofluorescence (e.g., from lipofuscin). | Can negatively affect specific signal if not optimized [35]. |
| Chemical Quenching (Sodium Borohydride) | Reduces fluorescent Schiff's bases formed by aldehyde fixatives [32]. | Treat aldehyde-fixed samples with 1 mg/mL sodium borohydride for 30-40 minutes [32]. | Highly specific for fixation-induced fluorescence. | Can be harsh on some tissue antigens. |
| Photobleaching | Uses high-intensity light to bleach endogenous fluorophores prior to staining [32]. | Expose unstained sample to intense light at relevant wavelengths for a defined period. | Simple; no chemicals added to the sample. | Can also bleach the specific fluorophore if not carefully controlled. |
| Alternative Fixation | Uses non-aldehyde fixatives to prevent Schiff's base formation [32] [10]. | Fix samples with ice-cold methanol or acetone for 5-15 minutes [32]. | Avoids the root cause of aldehyde autofluorescence. | May not preserve morphology or antigenicity as well as aldehydes for some targets [10]. |
The workflow for selecting and applying these strategies can be visualized as follows:
Essential Protocols for Assessment and Control
Protocol: Evaluating Sample Autofluorescence
The first step in addressing autofluorescence is to quantify its level and spectral characteristics in your specific sample [32].
- Prepare an Unstained Control: Process your tissue sample or cells identically to your standard IHC/IF protocol, including fixation, permeabilization, and mounting, but omit all fluorescently-labeled reagents (primary and secondary antibodies) [32].
- Image the Control: Observe the unstained control using all the microscope filter sets or laser lines you plan to use in your experiment.
- Analyze the Signal: The fluorescence signal detected in this unstained control represents the level and distribution of autofluorescence for your sample under those imaging conditions. This provides a critical baseline for subsequent optimization.
Protocol: Sodium Borohydride Treatment for Aldehyde-Induced Fluorescence
This protocol is specifically for reducing autofluorescence caused by aldehyde fixatives like formaldehyde and glutaraldehyde [32].
- Prepare Solution: Freshly prepare a 1 mg/mL solution of sodium borohydride in phosphate-buffered saline (PBS). Note: The solution will bubble as the borohydride reacts with water.
- Treat Sample: Incubate the aldehyde-fixed sample (tissue section or cells) in this solution for 30 to 40 minutes at room temperature.
- Wash: Rinse the sample thoroughly with PBS, 3 times for 5 minutes each, to remove any residual reagent.
- Proceed with Staining: Continue with your standard immunostaining protocol.
The Scientist's Toolkit
Successfully managing autofluorescence requires a combination of specific reagents and analytical tools. The following table details essential items for this process.
Table 3: Key Research Reagent Solutions for Autofluorescence Management
| Item | Function / Application |
|---|---|
| Sudan Black B | A chemical quencher used to reduce broad-spectrum autofluorescence from sources like lipofuscin [32] [35]. |
| Sodium Borohydride | A reducing agent that neutralizes fluorescent Schiff's bases formed by aldehyde fixatives [32]. |
| Near-Infrared (NIR) Fluorophores | Fluorophores emitting in the near-infrared range, spectrally distant from common green-channel autofluorescence [32]. |
| Anti-GFP Antibody Conjugates | Antibodies against GFP, conjugated to fluorophores in red or other channels, allowing detection of GFP-tagged proteins away from the congested green spectrum [32]. |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | Used in treatments (e.g., overnight incubation in 5% Hâ‚‚Oâ‚‚) to reduce autofluorescence in certain tissues [32]. |
| Methanol/Acetone | Non-aldehyde, precipitative fixatives used as an alternative to formaldehyde to prevent the formation of fluorescent Schiff's bases [32] [10]. |
| Spectral Flow Cytometer or FLIM Microscope | Advanced instrumentation that separates specific signal from autofluorescence based on full spectral signatures or fluorescence decay kinetics [32]. |
| Viability Dye | In flow cytometry, used to gate out dead cells and debris, which often exhibit high levels of autofluorescence [32]. |
| 1H-Pyrrole, dimethyl- | 1H-Pyrrole, dimethyl-, CAS:49813-61-8, MF:C12H18N2, MW:190.28 g/mol |
| N-trimethylsilylazetidine | N-Trimethylsilylazetidine|CAS 41268-75-1 |
A Step-by-Step Protocol for Implementing Essential IHC Controls
Sourcing and Selecting Appropriate Positive and Negative Control Tissues
In immunohistochemistry (IHC), the validity of interpretations hinges entirely on the use of appropriate positive and negative controls. These controls serve as internal checks that differentiate true positive signals from artefacts caused by nonspecific binding, endogenous activity, or protocol errors [36] [37]. Without proper controls, investigators risk publishing unverified and irreproducible findings, which wastes time, resources, and erodes scientific credibility [1]. This guide provides a comprehensive comparison of control tissue sourcing strategies and selection methodologies to ensure reliable, interpretable IHC results for researchers, scientists, and drug development professionals.
Understanding Control Types and Their Functions
Positive Control Tissues
Positive tissue controls are specimens known to express the target protein in a specific location (specific cell type or intracellular compartment) [1]. A positive control demonstrates that the entire IHC assay is functioning correctly—from antigen retrieval to detection. If staining is observed in the positive control, the protocol is working; lack of staining indicates a technical issue requiring troubleshooting [37].
The most rigorous positive control is the positive anatomical control, which can be either:
- Internal positive control: A known site of target expression within the test specimen itself [1]
- External positive control: A separate specimen/slide known to contain the molecule targeted by the antibody [1]
Negative Control Tissues
Negative tissue controls reveal non-specific binding and false positive results [37]. These controls should come from tissues that do not express the target protein [37]. Any observed staining suggests non-specific binding, indicating potential issues with antibody specificity or protocol conditions.
Specialized Control Types
Beyond basic positive and negative controls, several specialized controls address specific experimental challenges:
- No Primary Controls (Secondary Antibody Only Control): Assesses nonspecific binding by the secondary antibody by omitting the primary antibody [37]
- Isotype Controls: Uses an antibody of the same class, clonality, and host species as the primary antibody but with no specificity to the target antigen [37]
- Absorption Controls: Tests if the primary antibody binds specifically by pre-incubating it with the immunogen before application [37]
- Endogenous Tissue Background Controls: Identifies inherent biological properties that emit natural fluorescence or produce color [37]
Sourcing Strategies for Control Tissues
Sourcing appropriate control tissues presents significant challenges, particularly for rare antigens or low-incidence biomarkers. The table below compares various sourcing strategies with their advantages and limitations:
Table 1: Comparison of Control Tissue Sourcing Strategies
| Sourcing Method | Best For | Sample Requirements | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Internal Laboratory Archives [38] | Common antigens, retrospective studies | Variable, depends on archive size | Readily accessible, known processing history | Limited availability for rare antigens |
| Tissue Microarray (TMA) Blocks [38] | High-throughput validation | 10-20 positive/negative cases [38] | Space-efficient, multiple tissues on one slide | May not contain rare antigens needed |
| Commercial Cell Lines [12] [39] | Protein quantification, standardized controls | Cell pellets with known expression levels [39] | Highly standardized, unlimited supply | May lack tissue context, dynamic range issues [1] |
| Xenograft Models [39] | Cancer research, phospho-specific targets | Cell lines with known expression [39] | Controlled expression levels, human targets in mouse context | Complex preparation, not for all targets |
| Multi-institutional Collaborations [38] | Rare diseases, low-incidence antigens | Varies by rarity | Access to otherwise unavailable specimens | Complex logistics, IRB approvals |
| Homemade Multitissue Blocks [38] | Maximizing resource utilization | Small fragments from multiple sources | Cost-effective, customizable | Requires expertise to create |
Addressing the Rare Antigen Challenge
For antigens with low population frequency (e.g., ALK+ lymphoma comprising only 2-3% of all lymphomas), finding sufficient positive cases presents unique challenges [38]. Practical solutions include:
- Laboratory Information System Mining: Prospective and retrospective searches of archival material [38]
- External Quality Assessment Programs: Supplementation with in-house tissues to reach optimal case numbers [38]
- Literature Correlation: Correlating staining patterns with expected results when tissues are unavailable [38]
- Tissue Multiplexing: Combining multiple tissue types in single blocks to maximize resource utilization [38]
According to College of American Pathologists (CAP) guidelines, laboratories should aim for:
- Nonpredictive assays: Minimum of 10 positive and 10 negative cases [38]
- FDA-approved predictive assays: Minimum of 20 positive and 20 negative/low-expressor cases [38]
- Laboratory Developed Tests (LDTs): Minimum of 40 positive and 40 low-expressor/negative cases [38]
Selection Criteria for Appropriate Control Tissues
Factors in Tissue Selection
Selecting appropriate control tissues requires consideration of multiple factors:
- Antigen Expression Level: Tissues should demonstrate expected expression patterns based on literature or previous studies [1]
- Tissue Morphology Preservation: Proper fixation and processing are essential—over-fixed tissues may mask antigens, while under-fixed tissues may exhibit excessive background [36]
- Species Compatibility: Consider species-specific reactions, particularly for mouse-on-mouse applications [40] [41]
- Fixation Method Consistency: Control and test tissues should undergo identical fixation protocols [15]
Validation of Specificity
Essential to valid interpretation of IHC staining is selecting antibodies validated to detect specific epitopes [1]. Validation approaches include:
- Western Blot Analysis: Demonstrates specific bands of appropriate molecular weight [39]
- Cell Line Transfection: Paraffin-embedded cell pellets with known target expression levels verify specificity [39]
- Blocking Peptides: Verify specificity and rule out Fc-mediated binding and non-specific staining [39]
- Genetic Validation: Antibodies should not produce staining in genetically engineered knockout models [1]
Figure 1: Control Tissue Selection and Validation Workflow
Special Considerations for Complex Scenarios
Mouse-on-Mouse Staining
Using mouse primary antibodies on mouse tissues presents unique challenges due to endogenous IgGs that secondary antibodies can recognize, causing high background [40] [41]. Mitigation strategies include:
- Direct Immunohistochemistry: Using directly conjugated primary antibodies eliminates secondary antibody issues [40] [41]
- Pre-blocking with Fab Fragments: Blocking endogenous IgGs by pre-treating tissue with unconjugated Fab fragments [41]
- Pre-formed Antibody Complexes: Mixing primary and secondary antibodies before application reduces free secondary antibodies [40]
Table 2: Mouse-on-Mouse Background Reduction Techniques
| Technique | Mechanism | Best For | Protocol Complexity |
|---|---|---|---|
| Direct Conjugation [40] | Eliminates secondary antibody | Any application, especially multiplexing | Low (commercial) to High (in-house) |
| Fab Fragment Blocking [41] | Blocks endogenous IgG epitopes | Tissues with high blood content | Medium |
| Pre-formed Complexes [40] | Binds secondary before application | Low abundance targets | High |
| Animal Perfusion [40] | Reduces blood-derived IgG | Pre-clinical models | Highest |
Endogenous Activity Interference
Certain tissues possess inherent properties that complicate IHC interpretation:
- Endogenous Enzyme Activity: Tissues rich in peroxidases (spleen, kidney) or phosphatases (kidney, intestine, liver) can react with chromogenic substrates, creating high background in IHC [36]
- Endogenous Biotin: Tissues with high mitochondrial activity (kidney, liver, spleen, tumors) contain high biotin levels, interfering with avidin-biotin detection systems [36]
- Autofluorescence: Molecules including heme groups, collagen, elastin, NADH, and lipofuscin emit natural fluorescence, particularly problematic in green and red channels [36]
Quality Assurance and Emerging Technologies
Monitoring Staining Variations
Quality control of IHC slides is crucial for accurate interpretation. Traditional methods use visual assessment, but emerging technologies offer improved standardization:
- Image Analysis Algorithms: AI-based tools like Qualitopix can quantify expression levels and detect variations not apparent visually [12]
- Standardized Cell Lines: Provide consistent control material across multiple experiments and sites [12]
- Inter-stainer Monitoring: AI algorithms can detect variations between different staining instruments and even individual slide slots [12]
Regulatory and Accreditation Standards
Adherence to established guidelines ensures testing standardization:
- CAP Guidelines: Require separate validation for each assay-scoring system combination and different fixation methods [15]
- Concordance Requirements: CAP updated guidelines set uniform 90% concordance requirements for all IHC assays [15]
- Documentation: Even for established assays, lack of validation documentation may result in accreditation citations [15]
Essential Research Reagent Solutions
Table 3: Key Reagents for Control Tissue Experiments
| Reagent/Category | Primary Function | Application Notes |
|---|---|---|
| Validated Primary Antibodies [39] | Specific target detection | Must be validated for IHC; check datasheets for recommended tissues |
| Isotype Controls [37] | Differentiate specific vs. nonspecific binding | Match subclass, concentration, and host species to primary antibody |
| Fab Fragment Blockers [41] | Block endogenous immunoglobulins | Critical for species-on-species staining; use at ~0.1 mg/mL |
| Directly Conjugated Primaries [40] | Eliminate secondary antibody background | Ideal for multiplexing; available with fluorophores (Coralite488, 594, 647) |
| Blocking Peptides [39] | Confirm antibody specificity | Pre-incubate antibody with peptide; should eliminate staining |
| Antigen Retrieval Buffers | Expose hidden epitopes | Citrate or Tris-EDTA depending on antibody requirements |
| Detection Systems | Visualize bound antibody | Consider enzyme-based (HRP/AP) vs. fluorescence based |
Figure 2: Comprehensive Control Implementation Strategy
Sourcing and selecting appropriate positive and negative control tissues is a fundamental requirement for valid IHC experiments. The optimal approach depends on multiple factors including antigen rarity, experimental system, and available resources. By implementing a comprehensive control strategy that includes properly sourced tissues, specialized controls for challenging scenarios, and adherence to validation guidelines, researchers can ensure their IHC results are reliable, reproducible, and scientifically valid. As technologies advance, particularly in AI-assisted quality control and standardized control materials, the field moves toward greater standardization and reliability in immunohistochemical analysis.
Optimal Placement and Staining of Control Slides
In immunohistochemistry (IHC), controls are not merely supplementary; they are fundamental components that validate the entire experimental process. They serve as critical internal checks that differentiate true positive signals from artefacts caused by nonspecific binding, autofluorescence, or protocol errors [42]. The integrity of IHC data, especially in drug development and diagnostic applications, hinges on the proper implementation and interpretation of these controls. Without appropriate controls, results may be unreliable, unreproducible, and ultimately misleading, potentially compromising scientific conclusions and clinical decisions.
The broader thesis of IHC control research emphasizes that controls are essential for confirming that observed staining patterns accurately reflect specific antibody-antigen interactions rather than procedural artefacts. Current research explores innovations in control materials and monitoring technologies, particularly the transition from traditional tissue-based controls to standardized cell line-derived controls and the integration of artificial intelligence (AI) for quality assessment [12] [13]. These advancements aim to address longstanding challenges in IHC, including the limited availability of certain tissue types, heterogeneity in control samples, and subjective visual assessment, thereby enhancing the reproducibility and reliability of IHC in both research and clinical settings.
Types of IHC Controls and Their Applications
Core Control Types for Validation
A robust IHC experiment incorporates multiple control types to address different potential sources of error. The table below summarizes the six essential IHC controls, their purposes, and implementation protocols.
Table 1: Essential Controls for IHC Experiments
| Control Type | Primary Purpose | Implementation Protocol | Interpretation of Results |
|---|---|---|---|
| Positive Tissue Control [42] [2] | Verify assay functionality and protocol optimization. | Stain a known antigen-expressing tissue alongside test samples using the identical protocol. | Valid Assay: Clear staining in control.Invalid Assay: No staining; indicates protocol failure. |
| Negative Tissue Control [42] [2] | Identify non-specific binding and false positives. | Use a tissue known not to express the target antigen. Knockdown/knockout samples are ideal [42]. | Specific Assay: No staining.Non-specificity: Staining indicates antibody or protocol issues. |
| No Primary Antibody Control [42] [2] | Detect nonspecific binding of the secondary antibody detection system. | Omit the primary antibody; incubate with antibody diluent only, then apply secondary antibody and detection reagents. | Clean System: No or minimal staining.Faulty System: Staining reveals secondary antibody cross-reactivity. |
| Isotype Control [42] [2] | Confirm staining specificity of monoclonal antibodies. | Replace primary antibody with a non-immune antibody of identical isotype, host species, and concentration. | Specific Staining: Signal in test sample distinct from isotype control.Non-specific Staining: Isotype control shows similar background. |
| Absorption Control [42] [2] | Demonstrate antibody binding is specific to the target antigen. | Pre-incubate primary antibody with excess purified immunogen (e.g., peptide) overnight, then use this mixture for staining. | Specific Binding: Significantly reduced or absent staining.Non-specific Binding: Staining persists, indicating off-target binding. |
| Endogenous Background Control [42] [2] | Identify inherent tissue properties that cause background signal. | Examine an unstained or secondary-antibody-only section under the microscope before running the full assay. | Low Background: Tissue suitable for assay.High Autofluorescence: Requires protocol adjustments (e.g., quenching). |
Novel Control Materials: Standardized Cell Lines and CLFs
Traditional patient tissue controls, while valuable, face challenges of limited availability, ethical issues, and inherent heterogeneity, which can lead to inconsistent expression levels from one control sample to the next [12] [13]. To address these limitations, researchers are increasingly adopting standardized alternatives:
- Standardized Cell Lines: Genetically engineered cell lines provide a consistent and renewable source for control material. Their use is particularly valuable for therapeutic protein targets like HER2 and PD-L1, as they offer more homogeneous antigen expression compared to traditional tissue blocks [12].
- Controls in Liquid Form (CLFs): These are cell suspensions prepared from genetically modified cell lines [13]. They can be applied manually via pipette or integrated into automated staining systems through a quality control module. CLFs form a regular circular shape with better cell distribution when applied automatically, and they faithfully mimic tissue controls by showing expected staining pattern changes under different antibody concentrations and antigen retrieval conditions [13].
Table 2: Comparison of Traditional vs. Novel Control Materials
| Feature | Traditional Tissue Controls | Standardized Cell Line Controls | Controls in Liquid Form (CLFs) |
|---|---|---|---|
| Source | Prior patient cases (normal or diseased tissue) [12] | Genetically modified cell lines [12] [13] | Genetically modified cell lines [13] |
| Availability | Limited, eventually run out [12] | Renewable, virtually unlimited | Renewable, virtually unlimited |
| Consistency | Heterogeneous, variable expression [12] | Homogeneous, constant expression | Homogeneous, constant expression |
| Application | Manual sectioning | Manual or automated | Optimized for automated systems [13] |
| Ethical Considerations | Involves patient material | Avoids patient material consumption | Avoids patient material consumption [13] |
Experimental Data and Performance Comparison
Quantitative Monitoring of Stain Variation
The implementation of standardized controls enables precise, AI-driven quality control. A 24-month longitudinal study monitoring HER2 and PD-L1 IHC staining of standardized cell lines using an AI algorithm (Qualitopix) revealed critical insights. The research quantified cell membrane expression levels weekly and identified multiple unexpected variations, particularly in low- and medium-expressing cell lines [12]. Further investigation traced these fluctuations to their root causes, identifying both inter-stainer variations (differences between the five autostainers used) and intra-run variations (differences between slide slots within the same stainer) [12].
This data underscores that staining variation is a real and quantifiable issue, even in controlled environments. The proactive response in this study—performing extra maintenance on a highly fluctuating stainer, which successfully reduced variation—demonstrates the practical value of a rigorous, data-driven QC process using standardized controls [12].
Diagnostic Performance of Automated Systems with Novel Controls
The diagnostic accuracy of IHC assays utilizing novel controls and automated systems has been validated in clinical research. A study of 87 lung adenocarcinoma specimens with known ALK status compared a novel automated system (LYNX480 PLUS with BP6165 antibody) against the established D5F3 antibody on the VENTANA platform [13]. The results, benchmarked against fluorescence in situ hybridization (FISH), demonstrate that the integrated system with its quality control approach delivers high performance.
Table 3: Diagnostic Performance of an Automated IHC System with Novel Controls for ALK Detection
| Parameter | BP6165 on LYNX480 PLUS Platform | Comparative Context |
|---|---|---|
| Sensitivity | 98.30% | Excellent, suitable for clinical screening |
| Specificity | 100% | Perfect specificity in this cohort |
| Sample Size (n) | 87 biopsy specimens | 47 ALK-positive, 40 ALK-negative |
| Reference Standard | Fluorescence in situ hybridization (FISH) | Gold standard for ALK rearrangement |
| Control Method | Automated CLFs (ALK positive & negative) | Provides consistent quality monitoring [13] |
Protocols for Control Slide Placement and Staining
Workflow for Optimal Control Slide Integration
The following diagram illustrates the recommended workflow for integrating control slides into an automated IHC staining process, incorporating both traditional and novel control types to ensure comprehensive quality assurance.
Detailed Experimental Methodology
Protocol: Automated IHC Staining with Integrated CLF Controls for ALK Detection [13]
Slide Preparation:
- Cut 3-μm sections from formalin-fixed, paraffin-embedded (FFPE) tissue blocks of test samples.
- For manual control placement, section positive and negative control tissue blocks. For automated placement, ensure target slides have space for CLF droplet application.
Application of Controls in Liquid Form (CLFs):
- Use the quality control module of the LYNX480 PLUS system.
- Scan the quick response (QR) code of the CLF vials (e.g., ALK positive CLF Catalog: BX30026P; ALK negative CLF Catalog: BX30026N).
- The system's automated pipetting system will dripped the corresponding CLFs onto the target slides.
- Dry and fix the applied CLF droplets onto the slide within minutes using the integrated heater.
Automated IHC Staining on LYNX480 PLUS:
- The staining module performs all subsequent steps:
- Deparaffinization and Rehydration: Standard protocols.
- Antigen Retrieval: Use EDTA retrieval solution (pH 9.0) for 60 minutes at 100°C.
- Peroxidase Blocking: Apply peroxidase blocking solution for 5 minutes.
- Primary Antibody Incubation: Incubate with anti-ALK antibody BP6165 (dilution 1:200) for 30 minutes at room temperature.
- Detection: Incubate with post-primary antibody (15 min) and secondary antibody-HRP compound (20 min).
- Chromogenic Development: Apply diluted 3,3'-diaminobenzidine (DAB) for 10 minutes.
- Counterstaining: Counterstain with hematoxylin.
- Washing: Wash with buffer (TBS) or distilled water between steps as required.
- Dehydration and Coverslipping: Dehydrate and mount with coverslips.
Quality Assessment:
- For CLFs: The stained control droplets should show a regular circular shape and even cell distribution. The positive CLF should show specific cytoplasmic staining, while the negative CLF should show no staining.
- For the test tissue: ALK positivity is defined as tumor-specific cytoplasmic staining of any intensity superior to background in the vast majority of tumor cells.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and instruments essential for implementing high-quality IHC controls as discussed in the featured experiments and broader context.
Table 4: Essential Reagents and Tools for Advanced IHC Quality Control
| Item | Function/Description | Example Use Case/Product |
|---|---|---|
| Standardized Control Cell Lines | Genetically engineered cell lines providing homogeneous, renewable source of control material for specific targets (e.g., HER2, PD-L1, ALK). | HER2 & PD-L1 controls for monitoring stainer performance [12]. |
| Controls in Liquid Form (CLFs) | Cell suspensions from modified lines applied manually or automatically to slides, saving tissue and ensuring consistency. | ALK Positive/Negative CLFs (e.g., Biolynx BX30026P/N) on LYNX480 PLUS [13]. |
| Automated IHC Stainer with QC Module | Instrument that automates staining and has a dedicated module for applying liquid controls via barcode scanning. | LYNX480 PLUS System with QC module [13]. |
| AI-Based Image Analysis Software | Algorithm that quantifies staining intensity and localization objectively, identifying variations invisible to the eye. | Qualitopix algorithm for monitoring stain quality over time [12]. |
| Validated Primary Antibodies | Antibodies optimized and validated for use on specific automated platforms with known performance characteristics. | BP6165 anti-ALK antibody on LYNX480 PLUS [13]. |
| Adhesion Microscope Slides | Slides with a chemical coating to prevent tissue loss during harsh IHC staining procedures, especially for tricky tissues. | KT5+ or TOMO slides with advanced adhesion [43]. |
| 4-Bromo-N-chlorobenzamide | 4-Bromo-N-chlorobenzamide, CAS:33341-65-0, MF:C7H5BrClNO, MW:234.48 g/mol | Chemical Reagent |
| 1,2-Dibromoanthracene | 1,2-Dibromoanthracene | 1,2-Dibromoanthracene is a high-purity reagent for materials science research. This product is For Research Use Only and not for human or veterinary use. |
Detailed Protocol for the No Primary Antibody Control
In the rigorous world of immunohistochemistry (IHC), controls are not merely suggestions but fundamental requirements for generating reliable and interpretable data. They form the bedrock of experimental validity, ensuring that the observed staining patterns accurately reflect the true localization and abundance of the target antigen. Within this ecosystem of controls, the No Primary Antibody Control stands as a critical negative control, specifically designed to identify false-positive results caused by the detection system itself [2] [44].
This guide places the No Primary Antibody Control within the broader context of IHC quality assurance, objectively comparing its application and value against other common negative controls. While positive controls verify that the IHC protocol can successfully detect the target antigen, negative controls like the No Primary Antibody Control are essential for confirming the specificity of the staining reaction [19]. By omitting the central reagent—the primary antibody—this control provides a baseline for non-specific background, enabling researchers to distinguish authentic signal from experimental artefact with greater confidence.
Theoretical Foundation of the No Primary Antibody Control
Purpose and Scientific Principle
The core function of the No Primary Antibody Control is to evaluate the specificity of the detection system and identify any non-specific binding contributed by the secondary antibody or other detection reagents [2] [28]. In a standard IHC workflow, the primary antibody binds specifically to the target epitope, and subsequent detection reagents then bind to the primary antibody to generate a visible signal. The No Primary Antibody Control tests the possibility that these detection reagents are themselves binding directly to tissue components, leading to a false-positive signal that could be misinterpreted as specific antigen expression [44].
The underlying principle is straightforward: if a visible stain appears in the No Primary Antibody Control slide, which has been processed identically to the test slide but without the primary antibody, it conclusively demonstrates that the staining is not due to specific primary antibody-epitope interaction [28]. A valid result for this control is negligible or absent staining that does not resemble the specific pattern observed in the test section [2] [28].
Position in the IHC Control Ecosystem
The No Primary Antibody Control is one of several negative controls employed to safeguard IHC specificity. The table below compares it to other standard negative controls, highlighting their distinct purposes and methodologies.
Table 1: Comparison of Common Negative Controls in IHC
| Control Type | Purpose | Preparation Method | What a Positive Result Indicates |
|---|---|---|---|
| No Primary Antibody Control | To detect non-specific binding of the secondary antibody or detection system [2] [44]. | Incubate tissue with antibody diluent only, followed by the full detection protocol [2] [28]. | The detection system is causing non-specific background staining. |
| Isotype Control | To detect non-specific binding caused by the immunoglobulin molecule of the primary antibody itself [2] [28]. | Replace primary antibody with a non-immune immunoglobulin of the same species, isotype, and concentration [2]. | The primary antibody is binding non-specifically to tissue components via its Fc region or other interactions. |
| Absorption Control | To confirm that the primary antibody binding is specific to the intended epitope [2] [28]. | Pre-incubate the primary antibody with an excess of its immunizing antigen before applying it to the tissue [2]. | The staining is specific, as it is competitively inhibited by the free antigen. |
| Negative Tissue Control | To verify the absence of the target antigen in a known negative tissue [2] [19]. | Use a tissue sample confirmed not to express the protein of interest [2]. | The antibody may be cross-reacting with other epitopes, or the tissue has inherent background. |
As illustrated, each control addresses a different potential source of non-specificity. The No Primary Antibody Control is unique in its targeted assessment of the detection system, a component that is common to virtually all IHC experiments regardless of the primary antibody used.
Experimental Protocol for the No Primary Antibody Control
Detailed Step-by-Step Methodology
The following workflow diagram outlines the parallel processing of test and control slides, highlighting the single critical difference in the protocol.
Diagram 1: Experimental workflow for the No Primary Antibody Control.
To implement the No Primary Antibody Control, follow this detailed protocol:
- Sample Preparation: Begin with at least two serial sections of the same tissue sample mounted on slides. For consistency, these sections should be as identical as possible in thickness and tissue content [19].
- Parallel Processing: Subject both slides to identical conditions throughout the entire pre-analytical and analytical process. This includes:
- Fixation: Use the same fixative (commonly formaldehyde-based fixatives like 10% formalin or 4% paraformaldehyde) for the same duration [10].
- Antigen Retrieval: Apply the same antigen retrieval method (e.g., heat-induced epitope retrieval in a specific buffer) to both slides [45].
- Blocking: Perform a blocking step to reduce non-specific binding using a standard protein block (e.g., serum, BSA) for both slides [10].
- Critical Divergence - Primary Antibody Incubation:
- Resumed Parallel Processing: After this critical step, both slides are processed identically again.
- Washing: Wash both slides with the same buffer.
- Detection System Incubation: Apply the same secondary antibody (e.g., anti-rabbit HRP polymer) and detection reagents to both slides [2] [28].
- Visualization: Develop the signal using the same chromogen (e.g., DAB) or fluorophore for the same duration [10].
- Counterstaining and Mounting: Apply the same counterstain (e.g., hematoxylin) and mounting medium.
- Interpretation and Analysis: Examine both slides under a microscope. The staining in the test slide should be compared directly to the control slide. Any staining present in the control slide must be considered background. For the experiment to be valid, staining in the No Primary Antibody Control should be negligible and must not mirror the specific pattern seen in the test slide [28] [44].
Troubleshooting and Data Interpretation
Interpreting the results of the No Primary Antibody Control is critical for data validation.
- Acceptable Result: The control slide shows no staining or only very faint, diffuse background that is clearly distinguishable from the specific, localized staining in the test slide. This validates the test result, confirming that the observed signal is due to specific primary antibody binding [28].
- Unacceptable Result: The control slide shows significant staining, particularly if it has a structured, cellular, or specific-looking pattern. This indicates a problem with the detection system, such as:
- Non-specific binding of the secondary antibody.
- Endogenous enzyme activity (e.g., endogenous peroxidase) that was not adequately blocked.
- Cross-reactivity of detection system components with tissue elements.
Table 2: Troubleshooting Guide for a Failed No Primary Antibody Control
| Problem Observed | Potential Causes | Recommended Solutions |
|---|---|---|
| Widespread, diffuse background | Inadequate blocking; secondary antibody concentration too high. | Optimize blocking serum concentration and incubation time; titrate down the secondary antibody [10] [28]. |
| Specific cellular staining in control | Secondary antibody cross-reactivity with endogenous immunoglobulins. | Use a secondary antibody that has been cross-adsorbed against the host species of the tissue sample. |
| Particular structures stained (e.g., red blood cells) | Inadequate quenching of endogenous peroxidase (for HRP systems). | Increase the concentration or incubation time of the endogenous peroxidase blocking step (e.g., Hâ‚‚Oâ‚‚) [10]. |
| High general background | Inadequate washing; slides dried during processing. | Increase wash volume and frequency; ensure slides remain hydrated throughout the protocol [10]. |
Comparative Analysis with Other Negative Controls
While the No Primary Antibody Control is essential, its value is greatest when used in conjunction with other controls. The following diagram illustrates the specific questions each major negative control answers in the verification pathway for a specific IHC stain.
Diagram 2: The role of different negative controls in verifying staining specificity.
From a practical and cost-effectiveness perspective, the No Primary Antibody Control is often considered a fundamental first-line negative control. International expert panels have noted that for IHC protocols using modern polymer-based detection systems, the No Primary Antibody Control (a type of Negative Reagent Control or NRC) may be sufficient in many cases, and the routine use of additional isotype controls on every case may be cost-inefficient [19]. The control is particularly crucial during the initial antibody validation and protocol optimization phases [45] [46]. Once a protocol is established and the detection system's performance is characterized, some laboratories may use this control less frequently, relying on the cumulative evidence from the test panel and internal tissue controls, though this is at the discretion of the laboratory director and subject to accreditation requirements [19].
Essential Reagents for Implementation
The following table lists the key materials required to successfully perform the No Primary Antibody Control.
Table 3: Research Reagent Solutions for the No Primary Antibody Control
| Reagent / Material | Function in the Protocol | Considerations |
|---|---|---|
| Serial Tissue Sections | Provides identical substrate for test and control slides. | Sections should be from the same tissue block, cut consecutively to ensure maximum comparability [19]. |
| Primary Antibody | The reagent being tested; omitted from the control slide. | Used only on the test slide. Its specificity should be under investigation [45] [46]. |
| Antibody Diluent | The solution used to dilute the primary antibody. | Serves as the replacement for the primary antibody on the control slide. Must be the same batch and volume as used for the test slide [2] [44]. |
| Detection System | Generates a visible signal (e.g., Polymer-HRP/AP system). | Applied to both slides identically. The source of non-specific binding if the control fails [2] [19]. |
| Chromogen/Fluorophore | Produces the microscopic signal (e.g., DAB, Fluorescent dyes). | Applied to both slides identically. The resulting precipitate or fluorescence is compared between slides [10]. |
The No Primary Antibody Control is a deceptively simple yet powerful tool in the IHC researcher's arsenal. Its systematic implementation provides an unambiguous assessment of the detection system's specificity, forming a critical link in the chain of evidence required to trust IHC data. While it does not replace other negative controls like isotype or absorption controls, its fundamental role in diagnosing non-specific background makes it an indispensable first step in validating any IHC stain.
In the context of a broader thesis on IHC controls, this control exemplifies the principle that verifying what a stain is not is as important as interpreting what it is. By rigorously applying the No Primary Antibody Control, researchers and drug development professionals can fortify their conclusions, ensuring that the biological stories told through the microscope are both compelling and true.
Blocking peptide controls serve as critical negative controls in immunohistochemistry (IHC) experiments, enabling researchers to validate antibody specificity and distinguish specific from non-specific binding. This guide examines the experimental execution and data interpretation for blocking peptide controls, comparing their performance against alternative validation methods. Within the broader context of IHC controls, blocking peptides provide a straightforward approach to confirm that observed staining results from antibody binding to the intended target epitope rather than off-target interactions. We present structured experimental protocols, quantitative data comparisons, and analytical frameworks to standardize implementation across research and development settings.
Blocking peptide controls, also known as immunizing peptides or negative control antigens, are essential tools for verifying antibody specificity in immunohistochemistry experiments. These controls consist of short amino acid sequences corresponding to the epitope recognized by a specific antibody. When used correctly, they competitively inhibit antibody binding to the target antigen in tissue samples, providing a critical negative control that helps distinguish specific from non-specific staining [47] [29]. The fundamental principle underlying this technique is that pre-incubation of a primary antibody with its corresponding blocking peptide occupies the antibody's antigen-binding sites, preventing subsequent binding to the target epitope in tissue sections [48].
In the broader context of IHC controls, blocking peptides fill a specific niche in method validation. While positive controls confirm assay sensitivity and procedural correctness, and negative controls identify background staining, blocking peptides specifically address epitope recognition validity. This is particularly crucial for drug development and research applications where accurate protein localization and quantification directly impact experimental conclusions and potential clinical translations. The integration of proper blocking controls has gained increased importance as studies reveal how storage conditions, fixation artifacts, and epitope masking can affect IHC results [5] [49].
Theoretical Foundation: How Blocking Peptides Work
Mechanism of Action
Blocking peptides function through competitive inhibition principles. The peptide, typically 20-30 amino acids in length representing the immunogenic epitope, is pre-incubated with the primary antibody before application to the tissue section. During this incubation, the peptide binds specifically to the antibody's antigen-binding site with high affinity, effectively "blocking" these sites and preventing the antibody from recognizing its target epitope in the tissue sample [29] [48]. When this pre-absorbed antibody solution is then applied to a tissue section parallel to the untreated antibody, any staining that disappears in the blocked sample represents specific binding, while persistent staining indicates non-specific background [47].
Visualizing the Blocking Peptide Workflow
The following diagram illustrates the conceptual framework and experimental workflow for blocking peptide controls in IHC:
Experimental Protocol: Executing Blocking Peptide Controls
Materials and Reagents
The following table details essential research reagents and solutions required for implementing blocking peptide controls:
Table 1: Research Reagent Solutions for Blocking Peptide Experiments
| Reagent/Solution | Composition/Preparation | Function/Purpose |
|---|---|---|
| Blocking Peptide | Lyophilized peptide corresponding to antibody epitope; reconstituted in sterile PBS or antibody diluent [47] | Competitively binds and blocks primary antibody's antigen recognition site |
| Antibody Solution | 97.65% IHC/ICC-PBS, 0.3% Triton X-100 (0.05% for extracellular epitopes), 0.05% Tween-20, 2% normal serum from secondary antibody species [47] | Diluent for primary antibody that maintains stability while reducing background |
| IHC/ICC-PBS | 0.2 M Naâ‚‚HPOâ‚„ (80 ml), 0.2 M KHâ‚‚POâ‚„ (16 ml), NaCl (8 g), double distilled water (860 ml); pH 7.4 [47] | Physiological buffer for maintaining pH and osmolarity during antibody incubation |
| Normal Serum | Serum from species in which secondary antibody was raised (e.g., normal donkey serum for donkey secondary) [47] [50] | Blocks nonspecific binding sites in tissue to reduce background staining |
Step-by-Step Methodology
Tissue Preparation and Sectioning: Begin with standard tissue preparation, including fixation, embedding, sectioning, deparaffinization, and antigen retrieval steps appropriate for your target antigen [47]. Use consecutive tissue sections from the same block for comparable results between control and experimental conditions.
Peptide Reconstitution: Reconstitute lyophilized blocking peptide according to manufacturer instructions. Typically, this involves adding 40 µl of sterile IHC/ICC-phosphate buffered saline (PBS) to the peptide vial [47]. Ensure complete dissolution before proceeding.
Antibody Solution Preparation: Prepare a primary antibody solution at the predetermined optimal dilution in appropriate antibody diluent. For a 1:200 dilution, add 6 µl of antibody to 1.2 ml of antibody solution [47]. The antibody solution should contain PBS, detergents (Triton X-100, Tween-20), and 2% normal serum from the species in which the secondary antibody was raised.
Solution Division and Peptide Addition: Divide the antibody solution equally into two tubes. Label one tube "antibody alone" and the second tube "+peptide." To the "+peptide" tube, add blocking peptide at a concentration at least 10-fold higher than the antibody concentration by weight [47] [29]. For example, if using 1 µg/ml antibody, use at least 10 µg/ml of blocking peptide.
Pre-incubation: Rotate or gently agitate both tubes for 1 hour at room temperature [47]. Alternatively, incubation can be performed overnight at 4°C for some applications [29].
Parallel Staining: Apply the contents of each tube to their respective tissue sections. Process slides identically through all subsequent IHC steps, including secondary antibody application, detection reagent incubation, and counterstaining [47].
Comparison and Analysis: Compare staining patterns between the "antibody alone" and "+peptide" sections. Specific antibody binding is indicated by staining that disappears in the peptide-blocked sample [47] [48].
Data Interpretation and Analysis
Interpretation Guidelines
Proper interpretation of blocking peptide experiments requires systematic comparison between control and experimental conditions:
Specific Binding: Staining that is abolished or dramatically reduced in the peptide-blocked sample represents specific antibody-epitope interaction. This confirms that the antibody recognizes its intended target [47] [48].
Non-specific Binding: Staining that persists in the peptide-blocked sample indicates non-specific binding. This may result from antibody interactions with off-target epitopes, Fc receptor binding, or other non-specific interactions [29].
Partial Blocking: In some cases, staining intensity may be reduced but not completely eliminated. This suggests a combination of specific and non-specific binding, or potentially incomplete blocking due to insufficient peptide concentration or incubation time.
Quantitative Comparison of Control Methodologies
The table below compares blocking peptide controls with alternative IHC validation approaches across key performance parameters:
Table 2: Comparative Analysis of IHC Validation and Control Methods
| Method | Principle | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Blocking Peptide | Competitive inhibition with epitope-specific peptide [47] [48] | Antibody validation, specificity confirmation, background reduction [29] | Direct epitope validation, technically straightforward, cost-effective for established targets [29] | Requires specific peptide for each antibody, may not detect all non-specific binding [29] |
| Genetic Validation | Comparison with genetic knockout/knockdown models [49] | Confirmation of target specificity, especially for new antibodies | High specificity, comprehensive validation at gene/protein level | Technically demanding, time-consuming, not readily available for all targets |
| Mass Spectrometry | Direct protein detection and quantification via peptide analysis [49] | Biomarker validation, archival tissue analysis, complementary to IHC | Direct protein measurement, not affected by epitope masking or antibody specificity issues [49] | Requires specialized equipment, destructive to sample, more complex data analysis |
| Cell Line Controls | Standardized cell lines with known antigen expression [12] | Instrument calibration, staining consistency monitoring, proficiency testing | Reproducible, quantifiable, suitable for longitudinal quality control [12] | May not represent tissue architecture, limited target availability |
| Peptide Microarrays | Peptide epitopes covalently bound to slides [5] | High-throughput antibody validation, epitope mapping, standardization | Reproducible printing (CV 4-8%), stable for ≥7 months, quantitative measurement [5] | Specialized equipment required, may not reflect native protein conformation |
Comparative Performance Data
Experimental Evidence and Case Studies
Blocking Efficiency in Model Systems: In immunocytochemical staining of mouse kidney cells using Anti-TRPV4 Antibody, staining was completely abolished when the antibody was preincubated with its corresponding blocking peptide, demonstrating successful validation of antibody specificity [47]. Similar results were shown in western blot applications where signal disappearance after peptide blocking confirmed specific binding [48].
Stability and Reproducibility Metrics: Studies with peptide-based IHC controls covalently bound to glass slides demonstrated excellent reproducibility, with coefficients of variation (CVs) of 4-8% in automated printing systems [5]. These peptide controls maintained stability at ≤4°C for at least seven months, supporting their utility for standardized quality control programs [5].
Inter-laboratory Validation: A national study involving 109 clinical laboratories demonstrated a strong correlation (r = 0.87) between a laboratory's ability to properly stain formalin-fixed peptide controls and their performance in correctly staining a 3+ HER-2 formalin-fixed tissue section mounted on the same slide [5]. This highlights the utility of standardized peptide controls for proficiency testing and quality assurance programs.
Limitations and Considerations
While blocking peptide controls provide valuable validation data, several limitations warrant consideration:
Epitope Accessibility: Blocking peptides may not fully replicate the native structure of the epitope as it exists in folded proteins within tissue contexts, potentially leading to incomplete blocking even with specific antibodies [5].
Concentration Optimization: The recommended 5-10× molar excess of peptide to antibody may require optimization for different antibody-peptide pairs [47] [29]. Insufficient peptide concentration can result in incomplete blocking and false positive interpretations.
Multi-epitope Recognition: For antibodies that recognize multiple epitopes (particularly polyclonal antibodies), a single blocking peptide may not address all specific interactions, potentially leading to residual specific staining after blocking [29].
Integration with Comprehensive IHC Quality Control
Blocking peptide controls represent one essential component within a comprehensive IHC validation framework. For robust experimental conclusions, especially in drug development contexts, integrating multiple control strategies provides the most reliable validation:
Hierarchical Validation Approach: Begin with traditional positive and negative tissue controls to establish baseline staining patterns and background levels. Implement blocking peptide controls to verify epitope specificity. For critical applications, consider orthogonal validation methods such as mass spectrometry or genetic approaches to confirm findings [49].
Longitudinal Quality Monitoring: Incorporate standardized controls such as peptide microarrays or characterized cell lines into regular staining runs to monitor assay performance over time. Artificial intelligence-assisted image analysis platforms can quantitatively track staining variations and identify drift in assay performance [12].
Environmental Factor Considerations: Recognize that IHC results can be affected by pre-analytical variables including tissue storage conditions. Studies have demonstrated that humidity and temperature during storage significantly impact immunoreactivity, with increased humidity accelerating signal loss for some antibodies [49]. Proper tissue handling and storage with desiccant protection can mitigate these effects.
When implemented systematically within this broader quality framework, blocking peptide controls provide targeted validation of antibody specificity that strengthens experimental conclusions and supports the reproducibility of IHC-based research.
Strategies for Managing Tissues with High Endogenous Biotin or Enzymes
In immunohistochemistry (IHC), the accurate detection of target antigens is frequently compromised by the presence of endogenous tissue components that generate false-positive signals. Endogenous biotin, peroxidases, and phosphatases are particularly problematic as they actively participate in the detection systems used in most IHC protocols. Effective management of these interferents is not merely a technical consideration but a fundamental component of appropriate positive and negative controls, ensuring that observed staining patterns accurately reflect antigen distribution rather than analytical artifacts. This guide systematically compares the strategies and reagents available to researchers for overcoming these challenges, providing supporting experimental data and standardized protocols to enhance the reliability of IHC experiments in research and drug development.
Understanding Endogenous Interferents and Their Impact
Endogenous interferents constitute a significant source of background staining that can obscure specific signals and lead to erroneous data interpretation. The table below summarizes the primary types of endogenous interferents, their distribution in tissues, and the mechanisms by which they compromise IHC results.
Table 1: Characteristics of Major Endogenous Interferents in IHC
| Interferent | Common Tissue Localization | Interference Mechanism | Resulting Artifact |
|---|---|---|---|
| Endogenous Biotin | Liver, kidney, adipose tissue, mammary gland [51] | Binds to streptavidin/avidin in detection systems [51] | Punctate or diffuse nonspecific staining, particularly in frozen sections [51] |
| Endogenous Peroxidases | Erythrocytes, neutrophils, other leukocytes [51] | Catalyzes chromogenic substrates (e.g., DAB) independently of HRP conjugate [51] [52] | Diffuse brown precipitate unrelated to antigen location |
| Endogenous Phosphatases | Intestine, placenta, bone, endothelial cells [51] | Hydrolyzes AP substrates (e.g., NBT/BCIP) [51] | Nonspecific precipitate with AP-based detection systems |
| Endogenous Immunoglobulins | Lymphoid tissues, tissues with inflammatory infiltrates [53] | Fc receptor binding of primary or secondary antibodies [53] | Non-specific cellular staining, particularly problematic in frozen sections [53] |
Heat-induced epitope retrieval (HIER) methods can exacerbate interference issues, particularly for endogenous biotin. Studies have demonstrated that HIER may increase the detectable levels of endogenous biotin, thereby elevating background signals in tissues previously considered to have low biotin content [51]. Consequently, negative control samples should undergo the same HIER process as test samples to accurately assess biotin-related background [51].
Comparative Blocking Strategies and Reagents
Endogenous Biotin Blocking Methods
The high affinity between biotin and streptavidin (Kd ≈ 10â»Â¹âµ M) forms the basis for many sensitive detection systems but also creates vulnerability to endogenous biotin interference [54]. The most effective blocking strategy employs a two-step process that first saturates endogenous biotin with free streptavidin, then occupies remaining binding sites with excess biotin [51] [52].
Table 2: Comparison of Biotin-Blocking Reagents and Systems
| Method/Reagent | Mechanism of Action | Advantages | Limitations | Experimental Evidence |
|---|---|---|---|---|
| Streptavidin-Biotin Sequential Block | Unlabeled streptavidin binds endogenous biotin; excess bioton saturates remaining sites [51] | Comprehensive blocking; effective even in high-biotin tissues [51] | Additional steps required; optimization needed for different tissues | A549 cells showed Golgi-specific vs. diffuse staining before/after block [51] |
| Avidin-Based Systems | Tetrameric protein with high biotin affinity [54] | Strong binding; stable over wide pH and temperature ranges [54] | Glycosylated with basic pI (10-10.5); high nonspecific binding [54] | Historically used but largely replaced by superior alternatives |
| Streptavidin (Recombinant) | Non-glycosylated biotin-binding protein from S. avidinii [54] | Reduced nonspecific binding; near-neutral pI (6.8-7.5) [54] | Lower solubility in water than avidin [54] | Standard for most modern IHC applications; lower background |
| NeutrAvidin | Deglycosylated avidin derivative [54] | Near-neutral pI (6.3); lowest nonspecific binding; retained biotin affinity [54] | Molecular weight (~60 kDa) higher than streptavidin [54] | Optimal for high-sensitivity applications requiring minimal background |
The critical importance of biotin blocking is demonstrated in experimental comparisons. In A549 cells, untreated samples exhibited considerable diffuse nonspecific fluorescence in addition to the punctate Golgi staining, while samples treated with an endogenous biotin-blocking kit showed clean, specific localization to the Golgi apparatus [51]. Similarly, in chromogenic IHC of colon carcinoma tissue, proper blocking of both endogenous peroxidase and biotin was essential for specific detection of cytokeratin 18 without background interference [51].
Endogenous Enzyme Quenching Methods
Endogenous enzymes require distinct quenching approaches that inactivate the enzymes without damaging epitopes or tissue morphology.
Table 3: Comparison of Endogenous Enzyme Blocking Methods
| Enzyme Type | Blocking Reagent | Concentration/Incubation | Mechanism | Validation Method |
|---|---|---|---|---|
| Peroxidases | Hydrogen peroxide (methanol solution) [51] | 0.3%-3% Hâ‚‚Oâ‚‚ for 10-15 minutes [51] | Oxidative inactivation of heme groups in peroxidases [51] | React rehydrated section with DAB alone; colored precipitate indicates incomplete blocking [51] |
| Peroxidases | Commercial peroxidase suppressor (e.g., Thermo Fisher 35000) [51] | 10-15 minutes at ambient temperature or 37°C [51] | Typically H₂O₂ in aqueous sodium azide [51] | Assessment of erythrocytes and eosinophils as internal negative controls [53] |
| Alkaline Phosphatase | Levamisole [51] [53] | 1-10 mM in substrate solution [51] [53] | Competitive inhibition of intestinal-type AP [51] | Incubate control section with NBT/BCIP substrate; staining indicates residual activity |
| Alkaline Phosphatase | Heat destruction [51] | Boiling during HIER [51] | Thermal denaturation of enzyme | Use in combination with other methods for complete inactivation |
For tissues with exceptionally high endogenous peroxidase activity that cannot be completely eliminated by quenching methods, alternative detection systems utilizing enzymes such as alkaline phosphatase (AP) provide a viable solution [51]. This approach circumvents the problem rather than attempting to overcome it through blocking alone.
Experimental Protocols for Effective Interference Management
Standardized Protocol for Endogenous Biotin Blocking
The following optimized protocol effectively blocks endogenous biotin in both frozen and formalin-fixed paraffin-embedded (FFPE) tissues:
- Following deparaffinization and antigen retrieval, wash slides twice with PBS for 5 minutes each [51].
- Prepare streptavidin solution by diluting unlabeled streptavidin in PBS to 100-500 μg/mL.
- Apply streptavidin solution to cover the tissue section and incubate for 20-30 minutes at room temperature [51].
- Wash slides twice with PBS for 5 minutes each.
- Prepare D-biotin solution by dissolving biotin in PBS to 0.1-1 mg/mL.
- Apply biotin solution to the section and incubate for 20-30 minutes at room temperature [51].
- Proceed with standard IHC protocol, including primary antibody incubation and detection.
For FFPE tissues, this blocking sequence should follow deparaffinization and antigen retrieval steps. For frozen tissues, blocking should occur after fixation and permeabilization [51]. Researchers should note that HIER may increase detectable endogenous biotin, making blocking particularly crucial when using heat-based antigen retrieval methods [51].
Standardized Protocol for Endogenous Peroxidase Blocking
Two established methods effectively quench endogenous peroxidase activity:
Methanol-Hydrogen Peroxide Method:
- Following deparaffinization and rehydration, prepare fresh peroxidase blocking solution by combining one part 30% hydrogen peroxide with nine parts absolute methanol [51].
- Submerge slides completely in this solution for 10 minutes at room temperature.
- Wash slides three times with PBS before proceeding with antigen retrieval or primary antibody application [51].
Commercial Peroxidase Suppressor:
- Following deparaffinization and rehydration, apply commercial peroxidase suppressor (e.g., Thermo Scientific Peroxidase Suppressor) to completely cover tissue section.
- Incubate for 10-15 minutes at ambient temperature or 37°C [51].
- Wash twice with buffer before continuing with the staining protocol.
The methanol-hydrogen peroxide method is particularly effective for tissues rich in erythrocytes, though the 3% hydrogen peroxide concentration may damage some epitopes. If epitope damage is observed, reducing the concentration to 0.3% hydrogen peroxide may be effective [51].
Integration with Comprehensive Control Strategies
Effective management of endogenous interferents must be integrated within a comprehensive framework of positive and negative controls to validate IHC results. The following control strategies are essential:
No Primary Antibody Control: Tissue section incubated with antibody diluent alone followed by secondary antibody and detection system. This controls for nonspecific binding of the detection system and the presence of endogenous interferents [55]. Any staining observed indicates inadequate blocking of endogenous enzymes or biotin, or nonspecific secondary antibody binding.
Isotype Control: Tissue section incubated with a non-immune antibody of the same isotype and concentration as the primary antibody. This assesses nonspecific antibody binding to tissue components [55] [19]. The staining pattern should be distinct from and negligible compared to specific staining.
Absorption Control: Primary antibody pre-adsorbed with excess purified antigen before application to tissue. This demonstrates staining specificity through competition [55]. Little to no staining should be observed when the antibody is neutralized with its cognate antigen.
Biological Validation: Assessment of internal negative tissue elements that should not express the target antigen provides additional validation of staining specificity and effective blocking [19].
The Scientist's Toolkit: Essential Reagents for Interference Management
Table 4: Research Reagent Solutions for Managing Endogenous Interference
| Reagent Category | Specific Examples | Function & Application | Key Considerations |
|---|---|---|---|
| Biotin Blockers | Unlabeled streptavidin, NeutrAvidin protein [51] [54] | Binds endogenous biotin; prevents detection system binding | NeutrAvidin recommended for lowest background due to neutral pI and lack of glycosylation [54] |
| Biotin Blockers | Free D-biotin [51] | Saturates remaining biotin-binding sites on streptavidin/avidin | Use after unlabeled streptavidin application for complete blocking |
| Peroxidase Blockers | Hydrogen peroxide (0.3-3%) in methanol or aqueous buffer [51] | Quenches endogenous peroxidase activity | Higher concentrations may damage epitopes; test optimal concentration for each tissue type |
| Phosphatase Blockers | Levamisole (1-10 mM) [51] [53] | Inhibits intestinal-type alkaline phosphatase | Does not inhibit all AP isoenzymes; may require additional methods |
| Protein Blockers | Normal serum from secondary antibody species [53] | Blocks nonspecific protein binding | Serum should match species of secondary antibody production |
| Protein Blockers | Bovine serum albumin (BSA) [53] | Blocks nonspecific binding; alternative to serum | Avoid non-fat dry milk (contains biotin) in avidin-biotin systems [53] |
| Detection Alternatives | Alkaline phosphatase-based systems [51] | Alternative enzyme for tissues with high peroxidase | Use when endogenous peroxidase cannot be completely quenched |
| Polymer Systems | Polymer/multimer-based detection [19] | Eliminates biotin from detection system | Bypasses endogenous biotin issues; increasingly common in modern IHC |
| Sulfurous diamide | Sulfurous Diamide Reagent|CAS 36986-61-5|RUO | High-purity Sulfurous Diamide (CAS 36986-61-5) for research. Explore its use as a chiral ligand in asymmetric synthesis. For Research Use Only. Not for human use. | Bench Chemicals |
| Tricyclopentylborane | Tricyclopentylborane | Tricyclopentylborane is a trialkylborane reagent for research, including hydroboration and radical initiation. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Effective management of endogenous biotin and enzymes represents a critical foundation for reliable IHC data generation. The strategies and protocols presented here provide researchers with evidence-based approaches to mitigate these common interferents. As IHC continues to evolve toward more sensitive detection systems, the implementation of robust blocking methods integrated with appropriate controls remains essential for distinguishing true biological signals from technical artifacts. This systematic approach to interference management ensures the validity of IHC results in both basic research and drug development applications.
Troubleshooting IHC Experiments: Using Controls to Diagnose Common Problems
Diagnosing No or Weak Staining with Positive Tissue Controls
Within the broader framework of immunohistochemistry (IHC) quality assurance, proper implementation of positive and negative controls forms the foundation of experimental validity. Positive tissue controls, which involve staining tissues known to express the target protein, serve as essential internal checks that confirm assay functionality [56]. When these controls demonstrate no or weak staining—a clear deviation from the expected result—researchers face a fundamental methodological breakdown that invalidates experimental data and requires systematic troubleshooting. This failure indicates issues within the IHC protocol that must be identified and rectified, as proper control performance is prerequisite for any meaningful interpretation of experimental results [56]. This guide examines the principal causes of control failure and compares analytical approaches for diagnosing these critical issues, providing researchers with methodologies to restore assay reliability.
Experimental Approaches for Diagnosing Control Failures
Core Troubleshooting Methodologies
When investigating failed positive controls, researchers should implement these standardized experimental protocols to isolate specific failure points:
No Primary Antibody Control Protocol: Omit the primary antibody and incubate the tissue with antibody diluent only, then proceed with secondary antibody and detection reagents [56]. This control assesses nonspecific binding of the secondary antibody. Any resulting signal indicates that the secondary antibody may be binding nonspecifically to tissue components, leading to false positives in experimental samples.
Isotype Control Methodology: Use an antibody of the same class, clonality, and host species as the primary antibody but with no specificity to the target antigen [56]. Apply this isotype control at the same concentration as the primary antibody and process the sample under identical conditions. A lack of staining in the isotype control confirms that the signal in your test sample is specific to the target antigen.
Absorption Control Procedure: Incubate the primary antibody overnight with its immunogen (preferably a purified peptide) to saturate binding sites [56]. Replace the primary antibody with this inactivated antibody in the IHC protocol. This should lead to little or no staining of the tissue at the specific antibody binding sites when compared with the observed staining in the standard protocol.
Endogenous Background Assessment: Examine tissue sections with a fluorescence microscope for fluorescent labels or a bright-field microscope for chromogenic labels to identify inherent biological properties that emit natural fluorescence (autofluorescence) [56]. This is particularly important for tissues abundant in collagen, elastin, and lipofuscin, which can be misinterpreted as positive staining.
Quantitative Digital Analysis Protocols
Computer-aided analysis of digitized whole slide images provides objective quantification to complement visual assessment. Established methodologies include:
Digital Image Analysis Workflow: Scan IHC-stained slides at 40x magnification (0.0625 μm² per raw image pixel) using a whole slide scanner [57]. For automated image classification, annotate image areas representing carcinoma, stroma, and clear glass to train histologic pattern recognition software. Iteratively adjust annotations and re-run the classification algorithm until optimal classification is achieved [57].
Staining Quantification Metrics: Use color deconvolution algorithms to isolate individual stains for quantification [57]. Calculate two key metrics: the percentage of carcinoma with target staining (%Pos), and the product of the staining intensity (optical density of staining) multiplied by the percentage of carcinoma with staining (OD*%Pos). These continuous variables provide more precise measurement than semi-quantitative pathologist scoring [57].
H-Score Automation: Implement deep learning models for region recognition trained on hematoxylin staining only, achieving pixel accuracy for each class ranging from 0.92 to 0.99 [58]. Within the desired area, the algorithm categorizes DAB intensity of each pixel as negative, weak, moderate, or strong staining and calculates the final H-score based on the percentage of each intensity category.
Comparative Analysis of IHC Diagnostic Approaches
Digital vs. Visual Assessment Performance
Table 1: Comparison of IHC Staining Assessment Methods
| Assessment Method | Quantification Type | Inter-Observer Variability | Throughput | Key Applications |
|---|---|---|---|---|
| Pathologist Visual Scoring | Semi-quantitative (ordinal) | High [57] | Low | Routine clinical diagnosis, initial screening |
| Digital Image Analysis | Continuous variables [57] | Low [57] | High | Biomarker validation, clinical research |
| qIHC Dot Counting | Absolute quantification [59] | Minimal [59] | Medium | Companion diagnostics, drug development |
| Automated QC Systems | Binary (pass/fail) [14] | None | High | High-throughput screening, clinical labs |
Technical Solutions for Control Implementation
Table 2: Comparison of IHC Quality Control Solutions
| Control Method | Implementation | Advantages | Limitations |
|---|---|---|---|
| Traditional Tissue Controls | Tissue sections with known expression [56] | Morphological context, established protocols | Scarce donor tissue, ethical issues [14] |
| Knockout/Knockdown Tissues | Genetically modified specimens [56] | High specificity for antibody validation | Limited availability, costly generation |
| Controls in Liquid Form (CLFs) | Cell suspensions from modified cell lines [14] | Standardized supply, automated application | Lack tissue architecture |
| Isotype Controls | Matching non-specific antibodies [56] | Identifies antibody nonspecific binding | Does not control for tissue elements |
| Absorption Controls | Antibody pre-adsorbed with immunogen [56] | Confirms antibody specificity | Works best with purified peptide immunogens |
Research demonstrates strong correlation between digital analysis and pathologist scoring, with Spearman correlations of 0.88 for percentage of positive staining (%Pos) and 0.90 for combined optical density measurements (OD*%Pos) [57]. Digital approaches provide superior precision in ranges of staining that appear weak to the human eye and produce continuous data rather than ordinal scores [57].
Advanced Technical Solutions
Automated Quality Control Systems
Novel automated solutions address control implementation challenges, particularly for targets with scarce positive tissue. The LYNX480 PLUS system with integrated quality control module can batch-process 60 slides by automatically adding controls in liquid form (CLFs) before IHC staining [14]. These CLFs, prepared from genetically modified cell lines, show more regular circular shapes and better cell distribution when applied automatically compared to manual application [14]. This system demonstrates excellent sensitivity (98.30%) and specificity (100%) in validating ALK status in lung adenocarcinoma specimens [14].
Quantitative IHC Technologies
Emerging technologies enable true quantification of protein expression directly in FFPE specimens. The qIHC method utilizes a novel amplification system that converts antibody/antigen complexes into countable dots [59]. This approach demonstrates superior analytical performance with excellent repeatability, reproducibility, robustness, linearity, and a larger dynamic range compared to traditional IHC or ELISA methods [59]. The method's lower limit of detection allows precise measurement of HER2 expression across the entire clinical range from undetectable to strong positive (IHC 3+) [59].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for IHC Troubleshooting
| Reagent/System | Function | Application Note |
|---|---|---|
| Positive Control Tissues | Verify assay functionality | Select tissues confirmed to express target; check antibody datasheet for recommended tissues [56] |
| Isotype Control Antibodies | Assess nonspecific binding | Match host species, isotype, conjugation, and concentration to primary antibody [56] |
| Controls in Liquid Form (CLFs) | Standardized quality control | Prepared from genetically modified cell lines; suitable for automated systems [14] |
| Color Deconvolution Software | Digital stain separation | Isolates DAB and hematoxylin signals for quantitative analysis [57] |
| Genie Histology Pattern Recognition | Automated region classification | Classifies carcinomatous areas within whole slide images [57] |
| iCARD qIHC Amplification System | Protein quantification | Generates countable dots for absolute protein measurement [59] |
| Automated IHC Staining Systems | Standardized protocol execution | Integrated QC modules enable consistent control application [14] |
| 1,2-Butadiene, 1,4-dibromo- | 1,2-Butadiene, 1,4-dibromo-, CAS:20884-14-4, MF:C4H4Br2, MW:211.88 g/mol | Chemical Reagent |
| 2-Propyl-1,3-oxathiolane | 2-Propyl-1,3-oxathiolane|Research Chemical | 2-Propyl-1,3-oxathiolane for research applications. This product is For Research Use Only (RUO) and is not intended for diagnostic or personal use. |
Diagnosing no or weak staining in positive tissue controls requires methodical investigation of all IHC system components. Traditional controls remain essential, but emerging automated QC systems and quantitative digital approaches address key limitations of subjective visual assessment and scarce control tissues. Implementation of the systematic troubleshooting workflows and comparative solutions detailed in this guide enables researchers to efficiently identify failure sources, restore assay functionality, and ensure the reliability of their IHC data within the critical framework of proper experimental controls.
Resolving High Background Using Negative and No Primary Controls
High background staining represents a frequent challenge in immunohistochemistry (IHC) that can compromise experimental validity and clinical diagnostic accuracy. This technical guide systematically compares the efficacy of negative and no primary antibody controls in diagnosing and resolving background issues. Experimental data demonstrate that while both controls are essential for quality assurance, they serve distinct diagnostic purposes. The no primary control specifically identifies endogenous enzyme activity and nonspecific secondary antibody binding, whereas negative controls with isotype-matched immunoglobulins detect Fc receptor-mediated binding and antibody-specific nonspecific interactions. Implementation of both controls within a rigorous quality control framework reduces interpretive errors by 45-60% according to multi-laboratory studies. This comparison provides researchers with evidence-based protocols for optimizing IHC specificity, particularly for critical applications like companion diagnostics and therapeutic target validation.
Immunohistochemistry has evolved from a qualitative technique to a semi-quantitative tool essential for diagnostic pathology and therapeutic decision-making. The transition toward standardized quantitative IHC has created an imperative for rigorous quality control practices previously associated with clinical chemistry laboratories [5]. High background staining remains a pervasive problem that compromises data interpretation, particularly for low-abundance targets and minimally expressed biomarkers. As IHC advances into companion diagnostic applications, proper implementation of controls has become indispensable for distinguishing specific signal from background interference [60] [61].
The broader thesis of IHC control research emphasizes that effective controls must not only verify proper immunostaining but also validate the efficacy of heat-induced epitope retrieval (HIER), which reverses formaldehyde-mediated cross-linking that masks target epitopes [61]. Contrary to assumption, not all formalin-fixed tissues adequately control for HIER; some stain strongly even without retrieval, providing no information about this critical step [61]. This limitation has driven innovation in control technologies, including peptide-based controls that offer superior standardization compared to traditional tissue controls [5].
Within this framework, negative and no primary controls serve as diagnostic tools that systematically identify different sources of background staining. Their strategic implementation enables researchers to apply targeted troubleshooting strategies rather than empirical optimization, significantly enhancing efficiency and reliability. This guide objectively compares these control modalities through experimental data, methodological protocols, and practical implementation frameworks.
Theoretical Foundations: Control Mechanisms and Diagnostic Applications
Defining Control Types and Their Diagnostic Targets
No Primary Antibody Control
- Purpose: Identifies background stemming from the detection system itself, including endogenous peroxidase/alkaline phosphatase activity and nonspecific binding of secondary antibodies or other detection reagents [60].
- Composition: Tissue sections undergo the complete IHC protocol with omission of the primary antibody step, typically substituted with buffer alone [60].
- Mechanism: By eliminating primary antibody contribution, this control isolates artifacts generated by the detection chemistry and endogenous enzymatic activities.
Negative Control (Isotype Control)
- Purpose: Detects nonspecific binding mediated by the primary antibody itself, including Fc receptor interactions and off-target epitope binding [60] [62].
- Composition: Tissue sections are incubated with an immunoglobulin of the same species, isotype, and conjugation as the primary antibody but lacking specificity for the target antigen [62].
- Mechanism: The isotype-matched control antibody shares the physicochemical properties of the primary antibody while differing in antigen specificity, enabling discrimination between specific and nonspecific antibody binding.
Table 1: Diagnostic Applications of IHC Background Controls
| Control Type | Primary Diagnostic Target | Optimal Application Context | Limitations |
|---|---|---|---|
| No Primary Control | Endogenous enzyme activity, secondary antibody nonspecific binding | All IHC experiments, regardless of antibody or tissue type | Cannot detect primary antibody-specific background |
| Negative Control (Isotype) | Fc receptor binding, nonspecific primary antibody interactions | Experiments using monoclonal antibodies, tissues with high Fc receptor expression | Requires perfect matching of isotype, concentration, and conjugation |
| Positive Control | Epitope retrieval efficiency, reagent functionality | Every run, using tissue with known antigen expression | May stain strongly even without HIER, failing to validate retrieval [61] |
| Peptide Controls | Analytical phase including HIER [5] | Quantitative IHC, proficiency testing, multi-site studies | Requires specialized preparation, not yet widely adopted |
Decision Framework for Control Selection
The following workflow illustrates the logical relationship between control results and subsequent troubleshooting actions:
Experimental Comparison: Performance Data and Validation
Multi-Laboratory Proficiency Study
A national validation study involving 109 clinical laboratories demonstrated that quantitative peptide controls accurately reflected IHC staining performance, with a strong correlation (r = 0.87) between a laboratory's ability to properly stain formalin-fixed peptide controls and their performance with 3+ HER-2 formalin-fixed tissue sections [5]. This finding underscores the utility of standardized controls in identifying technical variations that contribute to background staining.
When evaluating control performance, laboratories that implemented both negative and no primary controls reduced staining variability by 38% compared to those using only one control type. The coefficient of variation for staining intensity decreased from 18.7% (single control) to 11.6% (dual controls) across the participating laboratories [5].
Quantitative Analysis of Background Reduction
Table 2: Efficacy of Background Reduction Strategies Identified Through Controls
| Troubleshooting Strategy | Background Reduction | Signal Preservation | Application Context |
|---|---|---|---|
| Endogenous Peroxidase Blocking | 85-95% [60] | >98% | Chromogenic detection with HRP |
| Fc Receptor Blocking | 70-80% [62] | >95% | Tissues with immune cells (spleen, lymph node) |
| Primary Antibody Titration | 60-75% [62] | 90% (optimal concentration) | All applications, critical for high-concentration antibodies |
| Protein Blocking Agents | 50-70% [60] | >95% | All tissues, especially those with high collagen |
| Antigen Retrieval Optimization | 30-40% [61] | Variable | Over-fixed tissues, formalin-sensitive epitopes |
| Wash Buffer Optimization | 40-60% [60] | 100% | All IHC protocols |
Peptide Epitope Model for Control Validation
Advanced control systems utilizing formalin-fixed peptide epitopes covalently bound to glass slides have demonstrated exceptional utility in quantifying IHC performance [61] [5]. These models enable precise discrimination between HIER failures and immunostaining problems:
- Controlled Analyte Concentration: Peptide epitopes can be manufactured at defined concentrations ranging from 10² to 10ⶠmolecules per microbead, enabling sensitivity assessment across the assay's dynamic range [61].
- Formalin Fixation Compatibility: Peptides fixed in formalin vapor with casein coating undergo cross-linking similar to tissue proteins, allowing validation of HIER efficacy [5].
- Quantitative Measurement: Automated image analysis of peptide control staining intensity provides objective quality metrics with coefficients of variation of 4-8% [5].
Experimental data demonstrates that control tissues with high analyte concentration may stain strongly even without HIER, providing false reassurance about retrieval efficacy [61]. Peptide controls with intermediate analyte concentration (10³-10ⴠmolecules/bead) show superior sensitivity in detecting HIER failures, with signal reduction of 85-95% without proper retrieval compared to only 20-30% reduction in high-expression tissue controls [61].
Methodological Protocols: Implementation and Optimization
Standardized Protocol for Control Implementation
Materials Required
- Tissue sections adjacent to test sections (serial sections)
- Primary antibody solution
- Isotype-matched control immunoglobulin
- Phosphate-buffered saline (PBS) or antibody diluent
- Complete IHC detection kit reagents
Procedure
- Slide Preparation: Label three adjacent tissue sections as Test, Negative Control, and No Primary Control.
- Deparaffinization and Antigen Retrieval: Process all slides identically through deparaffinization, rehydration, and antigen retrieval.
- Peroxase Blocking: Apply peroxidase blocking solution to all slides (5 minutes, room temperature).
- Protein Block: Apply protein block solution to all slides (10 minutes, room temperature).
- Antibody Application:
- Test Section: Apply optimized primary antibody dilution
- Negative Control: Apply isotype-matched control immunoglobulin at same concentration
- No Primary Control: Apply antibody diluent only
- Incubation: Incubate all slides simultaneously (30 minutes, room temperature).
- Detection: Apply secondary antibody and detection reagents identically to all slides.
- Counterstaining and Mounting: Counterstain with hematoxylin, dehydrate, and mount all slides.
Interpretation Guidelines
- Compare staining patterns across all three sections
- Specific staining appears only in the test section
- Background present in negative control indicates antibody-related issues
- Background present in no primary control indicates detection system issues
Advanced Titration Protocol for Background Reduction
For antibodies demonstrating high background in negative controls, implement quantitative titration:
- Prepare six serial dilutions of primary antibody spanning 10-fold above and below manufacturer's recommendation.
- Process slides including negative controls for each dilution.
- Quantify signal-to-background ratio for each dilution using image analysis.
- Select the dilution that maximizes specific signal while minimizing background.
- Validate optimal dilution using positive control tissues with known expression levels.
Research demonstrates that antibody titration improves signal-to-noise ratio by 3-5 fold compared to using manufacturer-recommended concentrations without verification [62].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Reagents for Effective Background Control
| Reagent Category | Specific Examples | Function | Optimization Tips |
|---|---|---|---|
| Isotype Controls | Mouse IgG1, IgG2a, IgG2b; Rabbit IgG | Matched negative controls for primary antibodies | Ensure identical concentration, conjugation, and formulation as primary antibody |
| Blocking Proteins | Casein, BSA, normal serum, animal-free protein blocks | Reduce nonspecific binding | Match serum species to secondary antibody host for effective block |
| Fc Blocking Reagents | Anti-CD16/32, species-specific Fc block, human FcR binding inhibitor | Block Fc receptor-mediated antibody binding | Essential for lymphoid tissues, immune cells; add before primary antibody |
| Enzyme Blocks | 3% Hâ‚‚Oâ‚‚, levamisole, specific phosphatase inhibitors | Quench endogenous peroxidase/alkaline phosphatase | Optimize concentration to avoid tissue damage; validate efficacy |
| Detection Systems | Polymer-based, streptavidin-biotin, enzyme-polymer conjugates | Signal generation with minimal background | Polymer systems typically yield lower background than streptavidin-biotin |
| Wash Buffers | PBS, TBS, Tween-20, Triton X-100 | Remove unbound reagents | Incorporate detergents (0.025-0.1%) to reduce hydrophobic interactions |
| Peptide Controls | HER2, ER, PR peptide epitopes covalently bound to slides [5] | Quantitative process control | Implement for standardized quality monitoring across experiments |
| Chloro(pyridine)gold | Chloro(pyridine)gold|Gold(III) Complex|RUO | Bench Chemicals |
Comparative Analysis: Control Performance Across Experimental Conditions
Diagnostic Accuracy in Various Tissue Contexts
The performance of negative and no primary controls varies significantly across tissue types and fixation conditions. Tissues with high endogenous Fc receptor expression (spleen, lymph node, liver) demonstrate particularly high utility for negative controls, with 85% of laboratories reporting identifiable Fc-mediated background in these tissues [62]. Conversely, neural tissues with high lipid content may show elevated background in no primary controls due to hydrophobic interactions with detection reagents.
Formalin fixation time dramatically impacts control performance. Tissues fixed for extended periods (≥48 hours) develop extensive cross-linking that requires optimized HIER. Under these conditions, no primary controls become essential for distinguishing retrieval-related background from true detection system issues [61]. Research demonstrates that peptide controls with formalin fixation equivalent to 72 hours tissue fixation show 95% reduction in immunoreactivity without HIER, making them superior indicators of retrieval efficacy compared to tissue controls [61].
Multiplex IHC Considerations
As multiplex IHC gains prominence for complex biomarker panels, control implementation requires additional considerations. In multiplex formats, no primary controls should be implemented for each primary antibody individually to establish baseline background for each channel. Negative controls should include isotype matches for all primary antibodies used in the panel.
Advanced multiplex platforms utilizing automated staining systems with quality control modules demonstrate significant improvement in background consistency. One study of an automated IHC platform with integrated quality control modules reported 45% reduction in inter-slide variability compared to manual staining methods [14]. These systems can automatically apply controls in liquid form (CLFs), providing standardized circular deposition with superior cell distribution compared to manual application [14].
Effective resolution of high background in IHC requires the complementary application of both negative and no primary controls within a systematic quality management framework. While these controls serve distinct diagnostic purposes, their combined implementation provides comprehensive coverage against the major sources of nonspecific staining. Evidence from multi-laboratory studies indicates that laboratories employing both controls within a standardized protocol reduce technical variability by nearly 40% and decrease interpretive errors by 45-60% [5].
The evolving landscape of IHC controls increasingly incorporates engineered peptide epitopes and automated control application systems that provide quantitative performance metrics superior to traditional tissue controls [14] [61] [5]. These technologies enable implementation of clinical chemistry-style quality control practices, including Levy-Jennings charting and statistical process control, previously impractical in IHC laboratories [5].
For researchers and drug development professionals, rigorous implementation of both negative and no primary controls represents not merely a technical formality but a fundamental component of experimental validity. As IHC continues to advance toward fully quantitative applications in companion diagnostics and therapeutic target validation, systematic background control through appropriate negative and no primary controls will remain essential for generating reliable, reproducible, and clinically actionable data.
Addressing Non-Specific Staining and False Positives
In diagnostic immunohistochemistry (IHC), the accurate interpretation of results hinges on demonstrating both sensitivity and specificity through appropriate controls. Non-specific staining and false positives present significant challenges that can compromise experimental validity and clinical diagnostics. False-positive reactions may arise from characteristics of the primary antibody or nonspecific binding of detection system components [19]. As personalized medicine advances and predictive markers grow in number, the pressure for accurate IHC testing intensifies, making proper control strategies essential for reliable results [19]. This guide examines the systematic approaches to addressing these challenges through standardized control methodologies, comparing various techniques and their applications across different experimental contexts.
Understanding Control Classifications and Terminology
Standardized Terminology for Negative Controls
International expert panels have established standardized terminology to harmonize practices across laboratories. Understanding these classifications is fundamental to implementing effective control strategies [19].
Table 1: Classification and Applications of Negative Controls
| Control Type | Preparation Method | Primary Purpose | Application Context |
|---|---|---|---|
| Negative Reagent Control (NRC) | Replace primary antibody with non-immune immunoglobulins of same isotype and concentration | Identify false-positive reactions due to primary antibody non-specific binding | Essential for initial validation; particularly important when antibody performance characteristics are unknown |
| Negative Tissue Control (NTC) | Tissue known to lack the target antigen | Evaluate staining specificity in relation to tissue elements | Demonstrates absence of non-specific staining in tissue components when target is genuinely absent |
| Internal Negative Control | Intrinsic tissue elements within the test sample that lack the target antigen | Provide built-in specificity evidence without additional slides | Cost-effective approach that leverages native tissue architecture; particularly valuable in diagnostic settings |
Positive Control Classifications
Positive controls serve complementary but distinct purposes from negative controls:
- External Positive Tissue Control (Ext-PTC): Tissue with known antigen expression processed similarly to test tissue [19]
- Internal Positive Tissue Control (Int-PTC): Intrinsic tissue elements within the test sample with known antigen expression [19]
- System Suitability Control: Verifies the entire IHC protocol is functioning correctly
Comparative Analysis of Control Methodologies
Control Strategies for Different Experimental Contexts
The selection of appropriate controls varies based on the specific experimental goals, with different approaches offering distinct advantages and limitations.
Table 2: Comparative Performance of Control Strategies
| Control Strategy | Detection of Non-specific Primary Ab Binding | Detection of Detection System Issues | Cost & Workflow Impact | Best Applications |
|---|---|---|---|---|
| Traditional NRC (per case) | Excellent | Excellent | High (increases slide volume by 15-100%) | Avidin-biotin systems; initial antibody validation |
| Discretionary NRC (polymer systems) | Good | Moderate | Low (at laboratory director's discretion) | Established polymer-based systems; routine clinical panels |
| Negative Tissue Controls | Tissue-specific only | Tissue-specific only | Moderate (requires tissue banks) | All IHC tests; required by CAP checklist |
| Panel-based Interpretation | Good (through pattern recognition) | Good (through consistent detection across markers) | Minimal (leverages existing data) | Expert interpretation settings; multi-marker panels |
Evidence-Based Recommendations from International Guidelines
Recent guidelines reflect evolving consensus on control implementation:
- The College of American Pathologists (CAP) revised its checklist (ANP.22570) to make NRCs discretionary for laboratories using polymer-based/multimer-based detection systems [19]
- CAP continues to require Negative Tissue Controls (NTCs) for all IHC tests [19]
- For avidin-biotin detection systems, negative controls remain essential due to endogenous biotin unmasking by powerful antigen retrieval methods [19]
- Global practice variation remains significant, with some laboratories using no NRCs while others apply them to ≥15% of total IHC slide workload [19]
Experimental Protocols for Control Validation
Protocol for Negative Reagent Control Implementation
Purpose: To distinguish specific antibody binding from non-specific interactions through isotype-matched negative control antibodies [19].
Materials:
- Non-immune immunoglobulin of same isotype and species as primary antibody
- Identical concentration and dilution buffer as primary antibody
- Serial sections from patient tissue block
- All detection system components identical to test slide
Methodology:
- Prepare serial sections from the same tissue block used for test staining
- Apply non-immune immunoglobulin to control slide using identical protein concentration, incubation time, and temperature as primary antibody
- Process test and control slides simultaneously through all procedural steps
- Interpret control slide alongside test slide, evaluating any staining in control as non-specific
Interpretation: Valid result shows no staining in NRC. Any staining observed indicates non-specific binding that must be considered when interpreting test slide [19].
Protocol for Comprehensive Tissue Control Strategies
Purpose: To establish staining specificity using tissues with known antigen expression patterns [63].
Materials:
- Tissue microarray (TMA) containing both positive and negative control tissues
- Formalin-fixed, paraffin-embedded (FFPE) cell pellets with known expression profiles
- Transfected cell lines expressing target antigen and empty vector controls
Methodology:
- Tissue Microarray Construction: [63]
- Select normal tissues known to express target antigen (e.g., lymph node, thymus, spleen for PD-1)
- Include negative control tissues lacking target (e.g., kidney, heart, brain for PD-1)
- Arrange 0.6-1.0mm tissue cores in recipient paraffin block
- Cut sections at standard thickness (3-5μm)
Cell Line Validation: [63]
- Use untransfected cells or cells transfected with empty vector as negative controls
- Use cells expressing target antigen (either endogenously or via transfection) as positive controls
- Confirm transfection efficiency with epitope tags (e.g., V5, HA, MYC) or alternative detection methods
Staining and Interpretation:
- Process TMA alongside experimental slides
- Evaluate expected staining patterns in positive control tissues
- Confirm absence of staining in negative control tissues
- Note any unexpected staining patterns that may indicate cross-reactivity
Protocol for Blocking Peptide Validation
Purpose: To confirm antibody specificity through competitive inhibition with immunizing peptide [64].
Materials:
- Antigen-specific blocking peptide
- Control non-specific peptide
- Primary antibody at working concentration
- Standard IHC detection reagents
Methodology: [64]
- Pre-incubate primary antibody with excess molar concentration of antigen-specific peptide (typically 5-10× weight excess)
- Pre-incubate separate aliquot of primary antibody with control peptide
- Apply peptide-antibody mixtures to adjacent tissue sections
- Process through standard IHC protocol
- Compare staining intensity between sections
Interpretation: Significant reduction or elimination of staining with antigen-specific peptide, but not control peptide, demonstrates antibody specificity. Retained staining with both peptides suggests non-specific binding.
Advanced Technical Approaches
Digital Image Analysis for Objective Assessment
Digital pathology approaches provide quantitative alternatives to subjective visual scoring:
Methodology: [57]
- Slide Digitization: Capture whole-slide images at 40x magnification (0.0625 μm² per pixel)
- Tissue Classification:
- Annotate representative regions of carcinoma, stroma, and glass
- Train pattern recognition software (e.g., Aperio Genie) using annotated regions
- Apply optimized classifier to entire slide set
- Stain Quantification:
- Use color deconvolution to separate hematoxylin and DAB signals
- Set optical density (OD) vectors using single-stain control slides
- Calculate two metrics: percentage of positive staining (%Pos) and OD × %Pos
Performance Data: [57]
- Digital analysis shows strong correlation with pathologist visual scoring (Spearman correlation 0.88 for %Pos, p<0.0001)
- Computer-aided classification efficiently identifies carcinomatous areas with high accuracy
- Digital quantification provides continuous data vs. ordinal data from visual scoring
Titration Protocols for Background Reduction
Purpose: To optimize antibody concentration for maximum signal-to-noise ratio [65].
Materials:
- Primary antibody at stock concentration
- Antibody diluent with carrier protein (e.g., 1% BSA)
- Known positive control tissue
- Prepare serial dilutions of primary antibody (e.g., 1:50, 1:100, 1:200, 1:500)
- Apply to adjacent sections of positive control tissue
- Process through standard IHC protocol
- Evaluate for specific staining intensity versus background
- Select the highest dilution that provides strong specific signal with minimal background
Technical Considerations:
- Include antigen retrieval optimization simultaneously (citrate pH 6.0 vs. Tris-EDTA pH 9.0)
- Evaluate impact of incubation time and temperature (room temperature vs. 4°C overnight)
- Consider using automated stainers for improved reproducibility
Decision Framework for Control Selection
The following workflow diagram illustrates the logical process for selecting appropriate control strategies based on experimental context:
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Reagents for IHC Control Experiments
| Reagent Category | Specific Examples | Function in Control Experiments | Key Considerations |
|---|---|---|---|
| Isotype Controls | Non-immune mouse IgG, rabbit IgG | Match primary antibody species and isotype for NRC | Must use identical concentration and formulation as primary antibody |
| Control Tissues | Tissue microarrays, multi-tissue blocks | Provide known positive and negative expression patterns | Should include tissues with varying expression levels (low/medium/high) |
| Cell Line Controls | FFPE cell pellets from characterized lines (e.g., RAJI, JURKAT) | Offer consistent, reproducible control material | Validate endogenous expression before use; consider transfected lines for rare targets |
| Blocking Peptides | Antigen-specific peptides, control scrambled peptides | Confirm antibody specificity through competition | Use 5-10× molar excess; include irrelevant peptide control |
| Detection System Components | Polymer-based detection, avidin-biotin kits | Identify system-related non-specific binding | Match sensitivity to application; polymer systems reduce endogenous biotin issues |
| Antigen Retrieval Solutions | Citrate buffer (pH 6.0), Tris-EDTA (pH 9.0) | Optimize epitope exposure while minimizing artifacts | Vary retrieval method based on antibody and fixation conditions |
Troubleshooting Common Non-Specific Staining Problems
Systematic Approach to Background Staining Issues
High background staining remains one of the most frequent challenges in IHC. The following diagram outlines a logical troubleshooting pathway:
Implementation of Corrective Actions
Based on the troubleshooting pathway, specific corrective measures include:
For Primary Antibody Issues: [65] [66]
- Perform titration experiments starting with manufacturer's recommended concentration
- Test serial dilutions (e.g., 1:50, 1:100, 1:200, 1:500)
- Reduce incubation time if concentration is optimal but background persists
- Verify antibody suitability for IHC application (not all antibodies work equally across platforms)
For Insufficient Blocking: [65]
- Increase normal serum concentration to 5-10%
- Extend blocking time to 1-2 hours
- Add 0.05% Tween-20 to antibody diluent and wash buffers
- Implement specific blocking steps for endogenous enzymes (peroxidase, phosphatase)
- Use avidin/biotin blocking kit when using biotin-based detection systems
For Detection System Problems: [66]
- Reduce secondary antibody incubation time to 20-30 minutes
- Use fresh chromogen solution and monitor development under microscope
- Consider switching to polymer-based systems if using avidin-biotin methods
- Ensure proper preparation of all detection reagents according to manufacturer instructions
For Tissue Preparation Issues: [65] [66]
- Never allow tissue sections to dry during the staining protocol
- Standardize fixation time across all samples (typically 24-48 hours for formalin)
- Ensure complete dewaxing by heating slides to 60°C before clearing agents
- Use proper adhesive slides to prevent tissue detachment
Addressing non-specific staining and false positives in IHC requires a multifaceted approach centered on appropriate control strategies. The evidence-based recommendations presented in this guide emphasize that control selection should be guided by the detection system employed, application context, and antibody validation status. While traditional practices often mandated negative reagent controls for every case, contemporary guidelines recognize that polymer-based detection systems and expert interpretation of marker panels can provide sufficient evidence of specificity without the cost and workflow burden of universal NRC application [19].
The most effective approach integrates multiple control strategies: discretionary NRCs for problematic antibodies, required negative tissue controls for all tests, comprehensive validation during assay development, and systematic troubleshooting protocols for background issues. Furthermore, emerging technologies like digital image analysis offer promising alternatives to subjective visual scoring, providing continuous quantitative data that may improve reproducibility [57]. By implementing these structured approaches to control strategies, researchers and diagnosticians can significantly enhance the reliability and interpretability of IHC results, ultimately supporting both research accuracy and clinical decision-making.
Optimizing Antibody Dilution and Diluent Based on Control Results
In immunohistochemistry (IHC), the path to reliable, reproducible data is paved with rigorous controls. Proper antibody dilution and diluent selection represent fundamental optimization parameters that directly determine staining quality, specificity, and interpretability. These parameters cannot be optimized in isolation; they require a systematic framework of positive and negative controls to provide the necessary feedback on assay performance [1]. This guide examines how control results directly inform and guide the critical processes of antibody dilution and diluent selection, enabling researchers to achieve precise and trustworthy IHC outcomes.
The validity of any IHC experiment hinges entirely on the proper implementation and interpretation of controls [1]. As noted in The Histochemical Society guidelines, "an immunohistochemical assay that lacks controls cannot be validly interpreted. Period" [1]. Controls serve as the quality assurance checkpoint that validates the entire staining process, from tissue preparation to final visualization. Without them, investigators risk both false-positive and false-negative results, potentially leading to erroneous scientific conclusions [1].
The Control Framework: Foundations for IHC Validation
Positive Controls: Establishing Assay Sensitivity
Positive controls demonstrate that the IHC assay can successfully detect the target antigen when present. They confirm that all reagents and procedures are functioning correctly. The most rigorous positive control is the positive anatomical control—tissue with known expression of the target antigen in specific locations [1]. This can be either an internal positive tissue control (Int-PTC), where the antigen is known to be present in nontarget areas of the same specimen, or an external positive tissue control (Ext-PTC), a separate specimen with known antigen expression [19].
For example, an antibody targeting insulin should specifically stain the beta cells of pancreatic islets, providing both a positive control and a specificity check [1]. The positive control should demonstrate appropriate staining intensity and localization, validating that the antibody dilution is within the dynamic range of detection and that antigen retrieval was effective.
Negative Controls: Establishing Assay Specificity
Negative controls are essential for distinguishing specific antibody-epitope interactions from nonspecific background staining. Several types of negative controls serve distinct purposes:
Negative Reagent Controls (NRCs): These involve replacing the primary antibody with a nonspecific immunoglobulin of the same isotype and concentration or with antibody diluent alone [19]. This control identifies false-positive staining caused by nonspecific binding of the primary antibody or other reagents in the detection system.
Negative Tissue Controls (NTCs): These utilize tissues known to lack the target antigen, providing evidence of staining specificity [19]. The ideal NTC is genetically engineered tissue confirmed to lack the target molecule [1].
Peptide IHC Controls: A novel approach involves peptide spots covalently bound to glass slides that can be formalin-fixed and subjected to the same IHC process as tissue sections [5]. These quantitative controls demonstrate excellent correlation with tissue staining performance (r=0.87 for HER-2) and enable precise monitoring of staining consistency through Levy-Jennings charting [5].
A critical pitfall to avoid is omitting the primary antibody and considering this adequate as a negative control. While this practice controls for nonspecific binding of secondary antibodies, it does not validate the specificity of the primary antibody [1]. The proper negative control substitutes the primary antibody with nonspecific immunoglobulins at the same concentration [1].
Table 1: Essential Controls for IHC Validation and Their Applications in Optimization
| Control Type | Purpose | Preparation Method | Interpretation in Optimization |
|---|---|---|---|
| Positive Tissue Control (PTC) | Monitor assay sensitivity and calibration | Tissue with known antigen expression processed similarly to test tissue | Validates that antibody dilution detects true positives; insufficient staining may indicate over-dilution |
| Negative Reagent Control (NRC) | Identify false-positive staining from reagent nonspecific binding | Replace primary antibody with nonspecific Ig at same concentration | High background suggests inadequate blocking or inappropriate diluent composition |
| Negative Tissue Control (NTC) | Demonstrate staining specificity | Tissue known to lack target antigen | Specific staining indicates antibody cross-reactivity or insufficient dilution |
| Peptide Spot Control | Quantitative monitoring of staining performance | Peptide epitopes printed and formalin-fixed on slides | Provides objective intensity measurements (CV 4-8%) for dilution curve optimization [5] |
| Internal Control | Monitor staining within test specimen | Normal elements in patient sample known to express/not express target | Provides built-in reference for optimizing dilution conditions |
Systematic Optimization Using Control Feedback
The Iterative Process: Dilution Curves and Control Assessment
Optimizing antibody dilution requires an iterative approach where dilution curves are systematically evaluated alongside control results. The process begins with testing a broad range of antibody concentrations while maintaining consistent incubation time and temperature [67]. Each dilution is applied to sections that include both test tissues and control materials.
For research laboratories, optimization typically begins with overnight incubation at 4°C for tissue sections [67]. The starting concentration range for monoclonal antibodies is generally 5-25 µg/mL, while antigen-affinity purified polyclonal antibodies typically require lower concentrations of 1.7-15 µg/mL [67]. Each dilution should be evaluated against positive controls to ensure target detection and negative controls to assess specificity.
The optimal dilution is identified as the concentration that produces strong specific staining in positive controls while showing minimal to no background in negative controls. This "sweet spot" maximizes the signal-to-noise ratio, which is essential for both qualitative assessment and semi-quantitative analysis.
Quantitative Assessment of Staining Quality
Advanced optimization approaches incorporate quantitative assessment of staining intensity. The development of peptide IHC controls enables precise measurement of staining performance. In validation studies, automated printing of peptide spots demonstrated excellent reproducibility with coefficients of variation (CVs) of 4-8% [5]. This quantitative approach allows researchers to construct precise dilution curves and identify the optimal working concentration based on objective intensity measurements rather than subjective assessment.
For traditional tissue controls, scoring systems such as the 4-point scale have been used, though these demonstrate only moderate interobserver agreement (kappa w 0.48-0.49) [68]. Consensus scoring by multiple observers can improve reproducibility (kappa w 0.63) [68], highlighting the value of standardized evaluation criteria when optimizing dilution parameters.
Diagram 1: Antibody dilution optimization workflow. This iterative process uses control feedback to identify the optimal concentration that balances specific signal detection with minimal background staining.
Antibody Diluent Composition and Selection
Diluent Formulations and Their Functions
Antibody diluents are far more than simple dilution media; they are specialized solutions designed to optimize antibody performance and enhance staining quality. Modern diluents typically contain several key components:
- Buffering agents maintain optimal pH, typically physiological (pH 7.2-7.6), to preserve antibody binding capacity [69] [70].
- Stabilizing proteins like bovine serum albumin (BSA) or casein (typically 0.2-0.5%) prevent nonspecific antibody binding to tissue components [69] [5].
- Salts and ionic compounds maintain appropriate ionic strength for antibody stability [69].
- Preservatives extend shelf life and prevent microbial growth [69].
- Detergents (e.g., Tween-20) reduce surface tension and help penetrate tissue sections [70].
The composition of antibody diluents significantly impacts staining outcomes. Laboratories that optimize diluent selection report up to 30% reduction in false-positive staining in critical applications like HER2 detection [70]. Furthermore, optimized diluents can reduce antibody consumption by up to 20%, offering substantial cost savings for high-volume laboratories [70].
Matching Diluent to Application
Different IHC applications may benefit from specialized diluent formulations:
- High-sensitivity detection may require diluents with additional protein components to minimize background while preserving weak signals.
- Automated staining platforms need diluents with consistent viscosity and compatibility with fluidics systems [69] [70].
- Multiplex IHC requires diluents that maintain stability during extended staining procedures.
- Phospho-specific antibodies often need specialized diluents with phosphatase inhibitors to preserve post-translational modifications.
Table 2: Antibody Diluent Types and Their Applications in IHC Optimization
| Diluent Type | Key Components | Primary Applications | Impact on Controls |
|---|---|---|---|
| Protein-Based Diluent | BSA, casein, serum proteins | Routine IHC, low-abundance targets | Reduces background in negative controls; improves signal in positive controls |
| Polymer-Enhanced Diluent | Synthetic polymers, stabilizers | Automated platforms, high-throughput IHC | Provides consistent staining across batches for both controls and test samples |
| Antibody-Specific Formulations | Customized buffers, additives | Critical biomarkers (HER2, ER, PR) | Optimized for specific antibody clones; improves control performance |
| Stabilized Ready-to-Use | Preservatives, stabilizers | Multi-site studies, clinical diagnostics | Maximizes reproducibility of control results across time and locations |
Integrated Workflow: Combining Dilution and Diluent Optimization
Practical Implementation Strategy
Successful optimization requires a systematic approach that integrates both dilution and diluent parameters:
Initial Diluent Selection: Choose a diluent compatible with your detection system and tissue type. For novel antibodies, begin with a standard protein-based diluent.
Preliminary Dilution Range: Test a wide dilution range (e.g., 1:50 to 1:2000) using the selected diluent and appropriate controls.
Control Evaluation: Assess staining in positive controls for signal intensity and in negative controls for background.
Diluent Comparison: If background remains high despite optimal dilution, test alternative diluent formulations with different blocking protein compositions.
Fine-Tuning: Narrow the dilution range around the most promising concentration and confirm with replicate staining.
Documentation: Record the optimal dilution and diluent combination with corresponding control results for future reference.
This integrated approach ensures that both variables are optimized in concert, recognizing that the optimal dilution may vary with different diluent formulations.
Troubleshooting Based on Control Results
Control outcomes provide direct guidance for troubleshooting suboptimal staining:
Weak Staining in Positive Controls: Indicates under-concentration of antibody, excessive dilution, or suboptimal diluent. Potential solutions include increasing antibody concentration, trying a different diluent formulation, or extending incubation time.
High Background in Negative Controls: Suggests antibody over-concentration or inadequate blocking in the diluent. Solutions include further dilution, trying a diluent with different blocking agents, or additional blocking steps.
Inconsistent Staining Between Runs: May indicate diluent instability or variation in preparation. Solutions include switching to ready-to-use commercial diluents or implementing stricter preparation protocols.
Specific Background in Internal Controls: Suggests cross-reactivity that may require trying a different antibody clone or additional absorption steps.
The Researcher's Toolkit: Essential Reagents for IHC Optimization
Table 3: Key Research Reagent Solutions for IHC Optimization
| Reagent Category | Specific Examples | Function in Optimization | Considerations for Selection |
|---|---|---|---|
| Antibody Diluents | Protein-based buffers, commercial ready-to-use formulations | Optimize antibody stability and minimize nonspecific binding | Select based on antibody type, tissue, and detection system compatibility [69] [70] |
| Control Materials | Cell line pellets, tissue microarrays, peptide spots [5] | Provide reference for staining quality and consistency | Choose controls with known antigen expression relevant to your targets |
| Blocking Solutions | Normal serum, BSA, casein solutions | Reduce nonspecific background staining | Match species to secondary antibody; concentration typically 1-5% |
| Detection Systems | Polymer-based systems, avidin-biotin complexes | Amplify signal while minimizing background | Polymer systems generally produce less background than avidin-biotin [19] |
| Antigen Retrieval Reagents | Citrate buffer, Tris-EDTA, enzyme solutions | Expose epitopes masked by fixation | pH and method (heat-induced, proteolytic) require optimization for each antibody |
Optimizing antibody dilution and diluent selection represents a critical process that directly determines IHC data quality and reliability. This optimization cannot be achieved without the proper implementation and interpretation of controls. Positive controls validate assay sensitivity, while negative controls establish specificity—together providing the essential feedback needed to identify the optimal balance between signal intensity and background.
The most effective approach employs an iterative process where dilution curves are systematically evaluated against control results, with diluent composition serving as a key variable in achieving optimal staining. As IHC continues to evolve with more complex multiplexing and quantitative applications, the fundamental principle remains unchanged: rigorous controls are non-negotiable for generating valid, reproducible immunohistochemical data that can withstand scientific scrutiny and contribute meaningfully to research and diagnostic outcomes.
The Impact of Detection Systems on Control Performance
In the field of immunohistochemistry (IHC), the reliability of any experimental outcome is fundamentally dependent on the effective use of positive and negative controls. These controls are indispensable for verifying staining specificity, assessing protocol performance, and detecting technical artifacts [60]. The performance of these controls themselves, however, is not absolute; it is profoundly influenced by the analytical detection systems employed. Modern automated IHC stainers introduce advanced capabilities for standardized control application and processing, directly affecting the sensitivity, specificity, and reproducibility of control outcomes [14] [13]. Within the context of a broader thesis on IHC controls, this guide objectively compares how different automated staining platforms and their integrated quality control modules impact the performance of traditional tissue controls and novel control materials. As one study notes, "The precise detection of low ALK expression mainly depends on the affinity of the antibody, the sensitivity of the detection system, and the quality control" [14], highlighting the critical interplay between detection systems and control reliability.
Comparison of Automated IHC Staining Systems
The selection of an automated IHC staining system is a critical decision that directly influences the consistency and quality of control performance. The table below compares several key platforms and their approaches to quality control.
| Company / Platform | Key Features | Impact on Control Performance |
|---|---|---|
| Roche (Ventana) | Established platform (e.g., BenchMark XT), extensive assay menu, robust regulatory support [71]. | High reproducibility and inter-laboratory consistency due to standardized, pre-validated protocols and integrated control tracking [72]. |
| Leica Biosystems | Known for integration capabilities with Laboratory Information Systems (LIS) [71]. | Streamlines control data management, ensuring traceability and reducing administrative errors in control documentation. |
| Biolynx (LYNX480 PLUS) | Integrated IHC QC module for automated application of Controls in Liquid Form (CLFs) [14] [13]. | Automates control application, yielding a "more regular circular shape and better cell distribution" than manual application, minimizing human variability [13]. |
| BioGenex & Sakura Finetek | Recognized for cost-effectiveness and operational simplicity [71]. | Suitable for smaller labs, though control performance may rely more heavily on stringent manual protocol adherence by technologists. |
| Celnovte (CNT360) | Full-automatic IHC & ISH stainer designed to improve accuracy and efficiency [73]. | Minimizes human error in the staining process itself, enhancing the reproducibility and reliability of control staining outcomes. |
Analysis of Comparative Experimental Data
A direct comparative study provides quantitative data on control performance across systems. Research evaluating the Biolynx LYNX480 PLUS system with its novel BP6165 anti-ALK antibody against the established VENTANA D5F3 system demonstrated excellent performance metrics [14] [13]. In 87 lung adenocarcinoma specimens with known ALK status, the LYNX480 PLUS/BP6165 combination achieved a sensitivity of 98.30% and a specificity of 100%, comparable to high-performing established systems [13].
A crucial finding was the superior performance of Controls in Liquid Form (CLFs) when applied via the system's automated QC module versus manual pipetting. The automated process produced controls with a more regular shape and even cell distribution, which is critical for consistent and accurate interpretation [14]. Furthermore, the CLFs were demonstrated to be robust indicators of staining conditions, as they "can show changes in the same pattern as tissue controls under different antibody concentrations and antigen retrieval conditions" [13]. This validates their utility as reliable sentinels for the entire IHC process.
Detailed Experimental Protocols from Cited Studies
Protocol: Validation of an Automated Stainer with Novel Controls
The following methodology was used to compare the LYNX480 PLUS system and its CLFs against a reference standard [14] [13].
- Tumor Samples: 87 archival formalin-fixed paraffin-embedded (FFPE) lung adenocarcinoma specimens (47 ALK-positive, 40 ALK-negative), with status previously confirmed by FISH, qRT-PCR, or IHC.
- Controls: ALK-positive and ALK-negative Controls in Liquid Form (CLFs) (Biolynx, BX30026P & BX30026N), prepared from genetically modified cell lines.
- Staining Platform Comparison:
- Test System: LYNX480 PLUS with BP6165 concentrated primary antibody (1:200 dilution).
- Reference System: VENTANA BenchMark XT with D5F3 antibody.
- IHC Staining Protocol on LYNX480 PLUS:
- Deparaffinization & Rehydration: Automated on-platform.
- Antigen Retrieval: EDTA retrieval solution (pH 9.0), 60 minutes at 100°C.
- Peroxidase Block: 5 minutes.
- Primary Antibody Incubation: BP6165 for 30 minutes at room temperature.
- Detection: Incubation with post-primary antibody (15 min) and secondary HRP compound (20 min).
- Visualization: DAB chromogen for 10 minutes.
- Counterstaining: Hematoxylin.
- Control Application: CLFs were applied to slides using the automated QC module of the LYNX480 PLUS, which uses a scanner to identify the correct controls via QR code and drips them onto slides. The droplets were then dried and fixed using an integrated heater.
- Interpretation: Five independent pathologists blindly reviewed all slides. Staining was considered positive with "tumor-specific cytoplasmic staining of any intensity... found to be superior to background staining" [13].
Protocol: Peptide-Based Control for HER-2 Testing
This study illustrates an alternative, non-tissue-based control method, highlighting a different aspect of control technology [5].
- Control Production:
- Slide Activation: Standard glass slides were chemically coated with a protected isocyanate.
- Peptide Printing: A custom automated printer deposited ~1-2 μL spots of synthetic peptides (representing the HER-2 epitope) onto activated slides.
- Formalin Fixation: Some slides underwent formalin vapor fixation overnight to mimic tissue fixation and create antigen retrieval dependency.
- IHC Staining: The peptide-spotted slides were stained alongside patient tissue sections using standard clinical protocols for HER-2 (CB11 or Herceptest), including antigen retrieval in a water bath at 98°C for 40 minutes.
- Quantification: A custom software application measured the color intensity of the stained peptide spots to provide an objective quality control metric.
Signaling Pathways and Workflows
IHC Control Performance Assurance Pathway
The following diagram illustrates the logical workflow and key factors for ensuring control performance within an IHC detection system, from input parameters to final validated output.
Automated QC Module Workflow
This diagram details the specific operational workflow of an integrated quality control module, as featured in the LYNX480 PLUS system, for automated control application.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the featured experiments for developing and deploying high-performance IHC controls.
| Item | Function / Description | Example from Research |
|---|---|---|
| Controls in Liquid Form (CLFs) | Cell suspensions from genetically modified cell lines providing a consistent source of positive and negative controls without consuming scarce tissue blocks [14] [13]. | ALK-positive (BX30026P) and ALK-negative (BX30026N) CLFs from Biolynx, used to validate ALK IHC staining on the LYNX480 PLUS platform [13]. |
| Synthetic Peptide Spots | Short amino acid sequences (≈20 aa) covalently bound to slides, representing specific antibody epitopes. They act as quantitative, reproducible controls for antibody specificity and staining performance [5]. | HER-2 peptide spots used in a multi-center study to monitor staining consistency and identify antigen retrieval failures [5]. |
| Formalin-Fixed, Paraffin-Embedded (FFPE) Tissue | The standard material for IHC, used for both test specimens and traditional "in-tissue" controls. Proper fixation is critical to preserve antigenicity and morphology [60]. | Archived FFPE lung adenocarcinoma samples used as the gold standard to validate the performance of the new BP6165 antibody and CLFs [14]. |
| Validated Primary Antibodies | Monoclonal or polyclonal antibodies whose specificity and affinity for a target antigen have been rigorously established for IHC use [74]. | Clone BP6165 (concentrated) on LYNX480 PLUS and clone D5F3 on VENTANA system, used for the comparative detection of ALK protein [14] [13]. |
| Detection Visualization System | The kit of reagents (e.g., secondary antibodies, enzyme conjugates, chromogens) used to generate a visible signal from antibody-antigen binding [14] [60]. | The BXV visualization system (I2003, Biolynx) used with DAB chromogen on the LYNX480 PLUS platform for signal development [14]. |
| Antigen Retrieval Solution | A buffer (e.g., EDTA-based, citrate-based) used to reverse the cross-links formed by formalin fixation, thereby exposing epitopes for antibody binding [60] [13]. | EDTA retrieval solution at pH 9.0, used for 60 minutes at 100°C to retrieve the ALK antigen on the LYNX480 PLUS system [13]. |
The evidence demonstrates that the choice of detection system is not merely a matter of convenience but a fundamental determinant of control performance. Automated systems from vendors like Roche, Leica, and Biolynx enhance reproducibility through standardization and integration [72] [71]. The data from the LYNX480 PLUS system specifically highlights how integrated quality control modules and novel control materials like CLFs can directly improve the physical characteristics and analytical reliability of controls, offering a viable solution to the challenges of scarce tissue resources and manual variability [14] [13]. For researchers and drug developers, selecting a detection system must extend beyond assessing its performance on test specimens to include a rigorous evaluation of its ability to ensure that positive and negative controls are performing optimally, thereby safeguarding the integrity of every IHC-based finding.
Validation, Quality Assurance, and Future Perspectives in IHC Control
Immunohistochemistry (IHC) serves as an essential tool in both diagnostic pathology and research, enabling the visualization of protein expression within the context of preserved tissue architecture. The transition of IHC assays from research tools to clinically actionable tests necessitates rigorous analytical validation to ensure their accuracy, reliability, and reproducibility. The College of American Pathologists (CAP) has established evidence-based guidelines to standardize these validation processes across laboratories. The 2024 guideline update affirms and expands upon previous recommendations, with a continued focus on ensuring analytical accuracy and reducing variation in IHC laboratory practices [15]. A core principle of this update is the establishment of a universal 90% overall concordance threshold for assay validation, harmonizing requirements across various marker types [15]. This guide objectively compares these updated CAP recommendations against previous standards and alternative approaches, providing a structured framework for their implementation within the broader context of IHC quality control.
Updated CAP Validation Guidelines: Key Changes and Requirements
The 2024 "Principles of Analytic Validation of Immunohistochemical Assays: Guideline Update" introduces several critical modifications designed to address evolving complexities in IHC testing. Notably, the original guideline outlined distinct requirements for validation of predictive markers like HER2, ER, and PR. The updated version harmonizes validation requirements for all predictive markers, creating a more uniform standard [15]. The guideline also now includes specific statements for the validation of IHC assays performed on cytology specimens, which are often fixed differently than standard formalin-fixed, paraffin-embedded (FFPE) tissues [15]. Furthermore, it provides expanded guidance on validating predictive markers with distinct scoring systems, such as PD-L1 and HER2, stipulating that laboratories must separately validate each assay-scoring system combination [15].
Core Validation Requirements and Comparator Options
A fundamental mandate across all CAP guidelines is that laboratories must analytically validate all laboratory-developed IHC assays and verify all FDA-cleared/approved assays before reporting patient results [16]. For the validation study design, the guidelines provide a flexible set of comparator options, ordered here from most to least stringent [15]:
- Comparison to IHC results from cell lines with known protein amounts ("calibrators")
- Comparison with a non-immunohistochemical method (e.g., flow cytometry, FISH)
- Comparison with results from testing the same tissues in another laboratory using a validated assay
- Comparison with prior testing of the same tissues with a validated assay in the same laboratory
- Comparison with results from a laboratory that performed testing for a clinical trial
- Comparison with expected architectural and subcellular localization of the antigen
- Comparison against percent positive rates in published clinical trials
- Comparison with previously graded tissue challenges from formal proficiency testing
The table below summarizes the key quantitative requirements for initial analytic validation as outlined in the updated CAP guidelines, providing a clear comparison of standards for different assay types.
Table 1: CAP Guideline Requirements for Initial Analytic Validation/Verification
| Assay Type | Minimum Case Requirements | Concordance Threshold | Special Considerations |
|---|---|---|---|
| Laboratory-Developed Non-Predictive Assays | 10 positive + 10 negative cases [16] | ≥90% overall concordance [15] | Validation set should include high and low expressors when appropriate [16] |
| Laboratory-Developed Predictive Marker Assays | 20 positive + 20 negative cases [16] | ≥90% overall concordance [15] | Set must span expected range of clinical results/expression levels [16] |
| Unmodified FDA-Cleared/Approved Predictive Assays | Follow manufacturer instructions; if none, 20 positive + 20 negative cases [16] | ≥90% overall concordance [15] | Laboratory medical director may document rationale for fewer cases [16] |
| Assays with Distinct Scoring Systems | Separately validate each assay-scoring system combination with 20 positive + 20 negative cases [15] [16] | ≥90% overall concordance [15] | Challenges must be based on intended clinical use [16] |
| Cytology Specimens with Alternative Fixation | 10 positive + 10 negative cases recommended for each fixation method [15] [16] | ≥90% overall concordance [15] | Increase case numbers for predictive markers; document rationale if minimum not feasible [16] |
Evolution of Validation Practices: Survey Data on Guideline Adoption
The impact of CAP guidelines on laboratory practices is evident from historical survey data. A comparative analysis of surveys from 2010 and 2015 demonstrated significant improvement in validation compliance following the dissemination of evidence-based guidelines.
Table 2: Impact of Guidelines on Laboratory Validation Practices (2010 vs. 2015)
| Validation Practice Metric | 2010 Survey Results | 2015 Survey Results | P-Value |
|---|---|---|---|
| Laboratories with written validation procedures for predictive markers | 45.9% (299/651) [72] | 73.8% (795/1077) [72] | <0.001 |
| Laboratories that validated their most recently introduced predictive marker | 74.9% (326/435) [72] | 99.0% (101/102) [72] | <0.001 |
| Laboratories with written validation procedures for non-predictive markers | 68.3% (496/726) [72] | 80.4% (866/1077) [72] | <0.001 |
The most frequently cited challenges in implementing the guidelines were difficulty finding validation cases for rare antigens and resource limitations [72], highlighting specific areas where alternative strategies may be necessary.
Experimental Protocols for Implementing CAP Validation Standards
Protocol for Validating an Automated IHC Staining System
Recent research demonstrates protocols for validating novel IHC systems against established standards. A 2025 study evaluating a novel automated IHC staining system for ALK testing in lung adenocarcinoma provides a template for comparative validation [13].
Materials and Experimental Setup:
- Specimens: 87 archival FFPE tumor samples from patients with stage I-III NSCLC, with ALK status previously confirmed by FISH, qRT-PCR, or IHC [13].
- Control Materials: ALK-positive and ALK-negative Controls in Liquid Form (CLFs) prepared from genetically modified cell lines (BX30026P and BX30026N, Biolynx) [13].
- Staining Systems: Comparison between the established VENTANA BenchMark XT platform (using D5F3 antibody) and the investigational LYNX480 PLUS System (using BP6165 concentrated antibody) [13].
- Validation Protocol: IHC was performed on 3-μm FFPE sections using the LYNX480 PLUS system with conventional DAB staining without amplification. The protocol included EDTA-based antigen retrieval (pH 9.0, 60 min at 100°C), peroxidase blocking (5 min), incubation with primary antibody BP6165 (1:200 dilution, 30 min at room temperature), post-primary antibody (15 min), secondary antibody-HRP compound (20 min), and DAB chromogen application (10 min) [13].
- Interpretation and Analysis: Five independent pathologists blindly reviewed each stained slide. Positive ALK expression was defined as tumor-specific cytoplasmic staining of any intensity superior to background staining in the vast majority of tumor cells. Statistical analysis included Cohen's Kappa for interobserver variability [13].
Results and Performance Data: The BP6165 concentrated antibody on the LYNX480 PLUS platform demonstrated 98.30% sensitivity and 100% specificity compared to FISH in the 87 biopsy specimens. The automated CLFs application showed more regular circular shape and better cell distribution than manual application, providing a consistent quality control method without consuming scarce patient tissue [13].
Validating antibodies against rare antigens presents particular challenges in obtaining sufficient positive cases. CAP guidelines acknowledge this limitation, stating that when the laboratory medical director determines that fewer than the recommended validation cases are sufficient for a specific marker (e.g., rare antigen), the rationale for that decision must be documented [16]. Practical solutions include [38]:
- Internal Resources: Using the laboratory information system to retrospectively and prospectively search archival material.
- External Resources: Purchasing tissue microarray blocks, slides, or cell lines from commercial biobanks.
- Multitissue Blocks: Creating homemade multitissue blocks (MTBs) that combine multiple rare tissue samples into a single block.
- Literature Correlation: Conducting thorough literature searches and correlating staining patterns of the new test to expected results.
For extremely rare antigens such as TLE-1 (synovial sarcoma) or INI-1 (malignant rhabdoid tumors), which have incidences as low as 0.19-0.89 per million [38], these alternative approaches become necessary to achieve meaningful validation.
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing robust IHC validation requires specific reagents and tools. The following table details key materials and their functions in the validation process.
Table 3: Essential Research Reagent Solutions for IHC Validation
| Reagent/Tool | Function in Validation | Application Examples |
|---|---|---|
| Controls in Liquid Form (CLFs) | Cell suspensions from genetically modified cell lines; serve as consistent positive/negative controls without consuming scarce tissue [13] | ALK positive CLF (BX30026P) and ALK negative CLF (BX30026N) used in automated IHC system validation [13] |
| Automated IHC Staining System | Platforms that standardize staining procedures through automated reagent application, incubation times, and temperatures [13] | LYNX480 PLUS System with integrated QC module; VENTANA BenchMark XT [13] |
| Antigen Retrieval Buffers | Solutions that reverse formaldehyde-induced protein cross-linking to expose epitopes for antibody binding [75] | Citrate buffer (pH 6.0) and EDTA buffer (pH 8.0-9.0) for heat-induced epitope retrieval [13] [75] |
| Isotype Controls | Antibodies of the same class and host species but without target specificity; assess nonspecific antibody binding [76] | Used at same concentration as primary antibody to confirm staining specificity [76] |
| Cell Lines with Known Protein Expression | Characterized cells serving as calibrators with defined antigen levels for quantitative comparison [15] | Genetically modified cell lines expressing specific targets like ALK [13] |
| Multitissue Blocks | Blocks containing multiple tissue samples arrayed together; efficient screening of antibody performance across tissues [38] | Validation of antibodies against rare antigens by combining limited samples [38] |
Visualizing IHC Validation Pathways and Workflows
IHC Assay Validation Decision Pathway
This decision pathway illustrates the structured approach required for IHC assay validation based on CAP guidelines. The process begins with determining the assay type, which dictates specific case requirements. A critical common endpoint is achieving the 90% concordance threshold, with documentation required for any deviations from minimum case numbers, particularly relevant for rare antigens or challenging specimen types [15] [16].
IHC Quality Control Implementation Workflow
This workflow outlines the comprehensive quality control system necessary for reliable IHC validation. Each control type addresses specific potential artifacts: positive controls verify assay functionality; negative controls detect nonspecific binding; no primary controls identify secondary antibody issues; isotype controls assess Fc receptor interactions; absorption controls confirm antibody specificity; and background controls account for endogenous tissue properties [76]. Together, these controls form an integrated system that safeguards against misinterpretation of IHC results.
The updated CAP guidelines for IHC assay validation represent a significant advancement in standardizing laboratory practices and ensuring patient safety. The harmonization of a 90% concordance threshold across all assay types, coupled with clear case requirements for different testing scenarios, provides laboratories with a structured framework for demonstrating analytical validity. The incorporation of new recommendations for cytology specimens and assays with distinct scoring systems addresses evolving complexities in IHC testing. Implementation of these guidelines, while challenging particularly for rare antigens, is essential for producing reliable, interpretable, and reproducible IHC results. As survey data demonstrates, widespread adoption of evidence-based validation guidelines has already significantly improved laboratory practices, ultimately enhancing the quality of patient care and the validity of research findings.
In the era of personalized medicine, predictive immunohistochemistry (IHC) has become indispensable for guiding targeted cancer therapies. Assays for markers such as p16 and HER2 provide critical information for treatment selection, directly impacting patient outcomes. Within this context, the implementation of robust control strategies forms the foundation of reliable and reproducible IHC testing. Proper controls verify both the analytical sensitivity and specificity of an IHC test, ensuring that staining results accurately reflect the true biomarker status of patient tissues [19]. The standardization of these controls, however, remains challenging due to variations in practice, reagents, and interpretation criteria across laboratories.
This case study examines the control strategies for two critical predictive markers: p16, a surrogate marker for high-risk human papillomavirus (hrHPV) in gynecologic cancers and also relevant in breast cancer, and HER2, a well-established therapeutic target in breast cancer [77] [78] [79]. We will objectively compare performance data across different antibody clones and detection systems, provide detailed experimental methodologies, and analyze how proper control implementation ensures assay validity within the broader framework of IHC quality assurance.
Comparative Performance Data of IHC Assays
p16 IHC Assay Performance Comparison
Table 1: Comparative Performance of p16 Antibody Clones in Gynecologic Tumors
| Antibody Clone | Manufacturer/Platform | Concordance with E6H4 (%) | Interobserver Reproducibility (Cohen's κ) | Staining Performance & Morphology |
|---|---|---|---|---|
| E6H4 | Ventana/Roche | 100 (Reference) | 1.00 (95% CI: 0.94-1.00) | Excellent, minimal background |
| JC8 | Agilent/Dako | 100 (95% CI: 97.9-100) | 1.00 (95% CI: 0.94-1.00) | Excellent, preserved morphology |
| 6H12 | Leica | 100 (95% CI: 97.9-100) | 1.00 (95% CI: 0.94-1.00) | Excellent, minimal artifacts |
A recent 2025 comparative study evaluating three fully automated p16 IHC assays demonstrated perfect concordance (100%) across E6H4, JC8, and 6H12 clones in 176 gynecologic tumor specimens, supporting their practical interchangeability in clinical settings [77]. The study utilized 42 whole slide sections and 134 tissue microarray cores from cervical, endometrial, vulvar, and ovarian tumors, with 21 positive and 21 negative cases as determined by two board-certified pathologists. All clones showed excellent staining performance with preserved tissue morphology and minimal background artifacts, achieving perfect interobserver reproducibility (κ=1.00) [77].
HER2 IHC and HER2-low Scoring Concordance
Table 2: HER2-low Scoring Concordance Among Expert Pathologists
| Assessment Category | Concordance Rate (%) | Fleiss Kappa Statistic | Primary Challenges Identified |
|---|---|---|---|
| Overall absolute agreement | 6 | - | All perfectly concordant cases were HER2 3+ |
| Challenging cases (HER2-low/ultralow) | 10 | Fair to moderate | Heterogeneous expression, cytoplasmic staining, expression around 10% cut-off |
| Clustered as 0 vs. others | 86 | - | Improved concordance when combining 1+ and 2+ scores |
The reproducibility of HER2-low scoring presents particular challenges. A 2023 study assessing concordance among 16 expert breast pathologists in the UK and Ireland found only 6% absolute agreement across 50 digitally scanned HER2 IHC slides, with all perfectly concordant cases being HER2 3+ [80]. Approximately 10% of cases (particularly HER2-low and ultralow) showed poor agreement due to heterogeneous HER2 expression, cytoplasmic staining, and expression levels spanning the 10% cut-off value. Concordance improved to 86% when scores were clustered as 0 versus others (1+/2+/3+), and further improvement was observed when 1+ and 2+ scores were combined [80].
External Quality Assessment (EQA) Performance Data
Table 3: EQA Pass Rates for Key Predictive Markers (2017-2021)
| Biomarker Category | Specific Marker | Mean Pass Rate (%) | Key Influencing Factors |
|---|---|---|---|
| Established Predictive Biomarkers | ER, PR, HER2 (Breast) | 89-92 | Standardized testing guidelines, extensive validation |
| Diagnostic IHC Biomarkers | PAX8, SOX10, Cytokeratins | 75 (range: 37-95) | Antibody sensitivity/specificity, test purpose, validation |
| New Diagnostic Biomarkers | 7 newly introduced markers | Below average | Optimization and implementation challenges |
| Programmed Death-Ligand 1 (PD-L1) | PD-L1 TPS/CPS (NSCLC) | 65 | "3-dimensional" approach complexity |
| PD-L1 IC (TNBC) | 79 | "3-dimensional" approach complexity |
Data from the Nordic Immunohistochemical Quality Control (NordiQC) program from 2017-2021, which evaluated over 31,967 results from more than 600 laboratories across 65 biomarkers, provides valuable insights into real-world performance [81]. Established predictive biomarkers for breast carcinoma (ER, PR, HER2) showed the highest pass rates (89-92%), while diagnostic IHC biomarkers demonstrated a wider spectrum of performance (37-95%, mean 75%). Newly introduced diagnostic biomarkers consistently showed inferior pass rates compared to the average, emphasizing the challenges of optimizing, validating, and implementing new IHC biomarkers [81].
Experimental Protocols and Methodologies
Protocol for p16 Antibody Comparison Study
The 2025 p16 clone comparison study followed a rigorous validation protocol [77]:
Sample Preparation: 42 cases of gynecological tumors were selected from routine diagnostic practice, including cervical cancer, vulvar cancer, endometrial cancer, and ovarian cancer. All tissue specimens were fixed in 10% neutral buffered formalin for 12-48 hours and processed without decalcification. From FFPE tissue blocks, 4-5 µm thick sections were cut within three weeks of staining.
IHC Staining Procedure: Three primary antibody clones were employed according to manufacturers' instructions on fully automated platforms:
- E6H4 on Ventana/Roche Benchmark series
- JC8 on Agilent/Dako Omnis series
- 6H12 on Leica Biosystems BOND series
Validation Design: The study followed CAP guidelines for validation of IHC, utilizing a minimum of 10 positive and 10 negative cases for non-predictive markers. The final validation set included 21 positive and 21 negative cases, as determined independently by at least two board-certified pathologists.
Assessment Methodology: Two pathologists independently reviewed each case blinded to the antibody clone used. staining patterns were evaluated for intensity, distribution, and cellular localization. Concordance and interobserver agreement were analyzed using Cohen's κ statistics.
Protocol for AI-Assisted Quality Monitoring
A 2025 study established a novel protocol for monitoring IHC staining variations using artificial intelligence [12]:
Control Material: Standardized cell lines designed as controls for HER2 and PD-L1 IHC staining were used instead of traditional tissue controls to ensure consistency.
Staining Protocol: Five IHC autostainers from the same manufacturer and type were used for parallel staining over a 24-month period with weekly measurements.
AI Analysis: Qualitopix, an AI algorithm for measuring stain quality control, was employed to quantify cell membrane expression levels. The algorithm provided objective quantification of staining intensity and distribution.
Variance Assessment: The study assessed both interstainer variations (differences between stainers) and intrarun variations (differences between slide slots within stainers). Calibrator slides were used to measure the limit of detection and identify variance per stainer and slot.
This protocol demonstrated that AI could effectively monitor IHC stain quality of standardized control cell lines and trace underlying errors, with the study identifying unexpected variations particularly in low- and medium-expressing cell lines [12].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for IHC Control Strategies
| Reagent/Material | Function in IHC Control | Application Examples |
|---|---|---|
| E6H4 p16 Antibody Clone | FDA-approved primary antibody for p16 IHC | Surrogate marker for hrHPV in cervical biopsies [77] |
| JC8 p16 Antibody Clone | Alternative p16 primary antibody | Interchangeable with E6H4 in gynecologic pathology [77] |
| 6H12 p16 Antibody Clone | Alternative p16 primary antibody | Comparable performance to E6H4 and JC8 clones [77] |
| Polymer-based Detection Systems | Signal amplification without avidin-biotin | Reduces background staining; enables discretion on NRC use [19] |
| Ready-To-Use (RTU) Antibodies | Pre-diluted, standardized reagents | Increases laboratory efficiency, better quality control [7] |
| Standardized Cell Lines | Consistent control material for quality monitoring | Enables AI-assisted quality control for HER2 and PD-L1 [12] |
| Immunohistochemical Critical Assay Performance Controls (iCAPCs) | Pseudo reference materials | Evaluates test performance for LLOD and reproducibility [81] |
| DAB Chromogen | Chromogenic substrate for HRP | Provides strong, permanent brown stain; most applications [7] |
| Hematoxylin Counterstain | Nuclear counterstain | Provides contrast to chromogen; visualizes tissue structure [7] |
Signaling Pathways and Experimental Workflows
p16/RB Pathway in HER2+ Breast Cancer Brain Metastases
Pathway Title: p16/RB Pathway in HER2+ Breast Cancer Brain Metastases
Recent research has revealed that p16INK4A deficiency predicts response to combined HER2 and CDK4/6 inhibition in HER2+ breast cancer brain metastases (BCBMs) [78]. The CDKN2A gene locus encodes the p16INK4A protein, which functions as a tumor suppressor by binding to CDK4/6 and preventing their interaction with cyclin D1, thereby inhibiting G1/S cell cycle progression [78]. In HER2+ BCBMs, genomic analysis of patient-derived xenografts revealed that loss of CDKN2A and CDKN2B by copy number variation is prevalent (11/18 cases), leading to p16INK4A deficiency in the majority of HER2+ BCBMs [78]. This deficiency creates therapeutic vulnerability to combined HER2-targeted therapy (tucatinib) and CDK4/6 inhibition (abemaciclib), resulting in marked tumor regression and significantly prolonged survival in orthotopic PDX models [78].
Dual-Modality AI Framework for Biomarker Prediction
Workflow Title: Dual-Modality AI Framework for Biomarker Prediction
A 2025 study developed DuoHistoNet, an efficient dual-modality transformer-based framework that integrates both H&E and IHC stained images for enhanced biomarker prediction [82]. This AI framework operates through a three-stage pipeline: (1) data preprocessing involving tissue segmentation and patch extraction, (2) feature extraction using a transformer-based model, and (3) aggregation of features to produce the final WSI-level prediction [82]. The system achieved clinical-grade performance, with AUROC exceeding 0.97 for MSI/MMRd prediction in colorectal cancer and 0.96 for PD-L1 prediction in breast cancer. Patients with biomarker-positive model predictions demonstrated prolonged time-on-treatment and overall survival when treated with pembrolizumab, suggesting the model's potential to enhance prognostic precision beyond current biomarker assessments [82].
This case study demonstrates that robust control strategies are fundamental to reliable predictive marker assays in IHC. The comparative data shows that while different p16 antibody clones can achieve excellent concordance and reproducibility when properly validated [77], significant challenges remain in scoring interpretation, particularly for emerging categories like HER2-low [80]. The integration of new technologies—including AI-assisted quality monitoring [12] and dual-modality biomarker prediction [82]—offers promising avenues for enhancing standardization and reproducibility.
Future directions should focus on the adoption of "Fit-For-Purpose" principles throughout the IHC testing lifecycle [81], implementation of standardized control materials like cell lines and iCAPCs [81] [12], and the development of integrated AI tools that can augment pathologist interpretation [82]. As personalized medicine continues to evolve, with an increasing number of predictive markers guiding therapy selection, the implementation of rigorous, standardized control strategies will remain paramount to ensuring accurate patient results and optimal therapeutic outcomes.
The Role of Controls in Validating Assays for Cytology Specimens
In the field of diagnostic pathology and biomedical research, the validation of immunohistochemistry (IHC) assays for cytology specimens presents unique challenges that demand rigorous control strategies. Unlike traditional histology samples, cytology specimens often undergo different fixation and processing methods, introducing variability that can compromise assay accuracy and reproducibility. The College of American Pathologists (CAP) emphasizes that laboratories must perform separate validations for IHC assays used on cytology specimens fixed in alternative fixatives compared to conventional formalin-fixed, paraffin-embedded (FFPE) tissues [15]. This article explores the critical role of positive and negative controls in validating IHC assays for cytology specimens, examining current guidelines, implementation challenges, and emerging solutions that enhance reliability in both diagnostic and research settings.
The Critical Importance of Controls in Cytology IHC
Fundamental Principles of IHC Controls
Immunohistochemistry relies on appropriate controls to ensure the validity of interpretations. Controls serve as internal checks that help differentiate between true positive signals and artifacts caused by nonspecific binding, autofluorescence, or protocol errors [83]. In cytology specimens, where material is often limited and fixation methods vary, implementing proper controls becomes even more crucial.
The essential premise is that an immunohistochemical assay lacking controls cannot be validly interpreted [1]. Both false-positive and false-negative results can lead to erroneous scientific conclusions and clinical misdiagnoses, making properly designed controls indispensable for building a convincing case for the presence or absence of a probed molecule [1].
Unique Challenges in Cytology Specimens
Cytology specimens present distinct challenges for IHC validation due to differences in specimen collection, processing, and fixation methods compared to surgical pathology samples. According to the 2024 CAP guideline update, laboratories must perform separate validations with a minimum of 10 positive and 10 negative cases for IHC performed on specimens fixed in alternative fixatives [15]. This recognition stems from literature showing variable sensitivity of IHC assays performed on specimens collected in fixatives often used in cytology laboratories compared with FFPE tissues [15].
Types and Applications of Essential IHC Controls
Positive Controls
Positive controls in immunohistochemistry protocols are specimens containing the target molecule in its known location [1]. For cytology specimens, these controls verify that the entire IHC process has functioned correctly.
- Positive Tissue Controls: These involve staining a tissue or cytology sample known to express the target protein. Lack of staining indicates an issue with the protocol that requires troubleshooting [83].
- Internal Positive Controls: The most rigorous positive control is the positive anatomical control where the presence of the antigen in the specimen is known a priori and is not the target of the experimental treatment [1].
- External Positive Controls: Separate specimens (e.g., a slide) that are known to contain the molecule targeted by the antibody [1].
Negative Controls
Negative controls demonstrate that the reaction visualized is due to the interaction of the epitope of the target molecule and the paratope of the antibody/affinity reagent [1].
- Negative Tissue Controls: These controls use tissues or cytology samples that do not express the target protein. Any observed staining suggests non-specific binding [83].
- Knockdown (KD) and Knockout (KO) Samples: These tissues significantly reduce or eliminate expression of the target protein, providing a reliable baseline for comparison [83].
- Isotype Controls: An antibody of the same class, clonality, and host species as the primary antibody, but with no specificity to the target antigen [83].
Specialized Control Types
- No Primary Controls (Secondary Antibody Only Control): Used to assess nonspecific binding by the secondary antibody by omitting the primary antibody [83].
- Absorption Controls: Utilize antibodies pre-incubated with the immunogen to test binding specificity [83].
- Endogenous Tissue Background Controls: Identify inherent biological properties that emit natural fluorescence or cause background staining [83].
Current Guidelines and Validation Requirements
CAP Analytic Validation Guidelines
The 2024 "Principles of Analytic Validation of Immunohistochemical Assays: Guideline Update" affirms and expands on previous publications to ensure accuracy and reduce variation in IHC laboratory practices [15]. Key recommendations include:
- Distinct Validation for Cytology: Separate validation/verification requirements for IHC assays performed on cytology specimens not fixed identically to tissues used for initial assay validation [15].
- Minimum Case Requirements: A minimum of 10 positive and 10 negative cases for IHC performed on specimens fixed in alternative fixatives [15].
- Harmonized Concordance Requirements: A uniform 90% concordance requirement for all IHC assays, including predictive markers [15].
Implementation Challenges
The CAP guideline panel recognizes that these new recommendations impose an added burden to laboratories, particularly for cytology specimens where appropriate positive control tissues may be rare and come with ethical issues [15] [14]. This challenge is especially pronounced for markers like ALK in lung adenocarcinoma, where positive control tissue is scarce [14].
Experimental Data and Validation Protocols
Case Requirements for Cytology Validation
Table 1: CAP Validation Requirements for Cytology IHC Assays
| Validation Parameter | Traditional FFPE Tissue | Cytology Specimens (Alternative Fixatives) |
|---|---|---|
| Minimum Positive Cases | Varies by assay type | 10 cases |
| Minimum Negative Cases | Varies by assay type | 10 cases |
| Concordance Requirement | 90% for all IHC assays | 90% for all IHC assays |
| Fixation Consistency | Standardized | Must validate for each alternative fixative |
Performance Metrics in Automated Systems
Table 2: Performance Comparison of ALK IHC Detection Systems
| Parameter | VENTANA D5F3 System | LYNX480 PLUS BP6165 System |
|---|---|---|
| Sensitivity | Established standard | 98.30% |
| Specificity | Established standard | 100% |
| Sample Size (N) | Varies by study | 87 biopsy specimens |
| Platform Type | Traditional automated | Automated with QC module |
| Control Method | Conventional tissue | Controls in Liquid Form (CLFs) |
Data extracted from studies comparing the established D5F3 antibody on the VENTANA system with the BP6165 concentrated antibody on the LYNX480 PLUS platform in 87 lung adenocarcinoma specimens with known ALK status [14].
Innovative Solutions for Control Challenges
Controls in Liquid Form (CLFs)
Recent advances address the challenge of scarce control tissues through the development of Controls in Liquid Form (CLFs). These are cell suspensions prepared from genetically modified cell lines that can either express or not express the target protein [14]. When applied using an automated system, CLFs demonstrate more regular circular shapes and better cell distribution than manually applied controls [14].
Automated Quality Control Systems
Integrated automated IHC staining systems with dedicated quality control modules now enable batch processing of multiple slides with consistent application of controls [14]. These systems automatically drip CLFs onto target slides, with features that prevent evaporation and contamination while tracking the entire QC procedure [14].
Research Reagent Solutions
Table 3: Essential Reagents for Cytology IHC Validation
| Reagent Type | Function | Examples/Specifications |
|---|---|---|
| Primary Antibodies | Specifically bind to target antigens | Clone BP6165 for ALK detection [14] |
| Detection System | Visualize antibody-antigen interactions | BXV visualization system [14] |
| Controls in Liquid Form | Provide standardized positive/negative controls without tissue consumption | ALK positive CLF (BX30026P), ALK negative CLF (BX30026N) [14] |
| Automated Staining Platform | Ensure consistent processing and staining | LYNX480 PLUS System with QC module [14] |
| Antigen Retrieval Reagents | Unmask epitopes altered by fixation | EDTA retrieval solution at pH 9.0 [14] |
Experimental Workflow for Cytology IHC Validation
The following diagram illustrates the complete workflow for validating IHC assays on cytology specimens, incorporating essential control steps:
The validation of IHC assays for cytology specimens demands meticulous attention to control strategies tailored to the unique challenges of these samples. Current guidelines explicitly require separate validation for cytology specimens fixed in alternative fixatives, with minimum case requirements and harmonized performance standards. Emerging technologies, including Controls in Liquid Form and automated quality control systems, offer promising solutions to the practical challenges of implementing appropriate controls while conserving scarce tissue resources. By adhering to these principles and leveraging innovative tools, researchers and diagnosticians can ensure the reliability, accuracy, and reproducibility of IHC assays on cytology specimens, ultimately supporting both valid research conclusions and accurate clinical diagnoses.
Digital Pathology and AI in the Automated Assessment of Control Slides
In immunohistochemistry (IHC), controls form the fundamental basis for validating staining accuracy and ensuring experimental reproducibility. Proper controls distinguish specific staining from artifacts, verify protocol performance, and confirm antibody specificity, ultimately determining whether research results are reliable [84] [2]. The transition from manual microscopy to digital pathology has introduced artificial intelligence (AI) and computational methods that are revolutionizing how these essential controls are assessed and quantified. This transformation addresses long-standing challenges in traditional pathology, including human variability, subjective interpretation, and the labor-intensive nature of manual slide review [85].
Digital pathology converts physical glass slides into high-resolution whole-slide images (WSIs), creating the foundational data layer for AI algorithms to analyze [85]. These AI-powered tools now demonstrate remarkable capabilities in detecting cancer, predicting molecular alterations, and quantifying biomarkers directly from standard H&E-stained slides [86] [87]. Within this technological framework, the automated assessment of control slides represents a critical application area, ensuring that the underlying staining and experimental conditions meet rigorous quality standards before proceeding with diagnostic interpretation or research analysis. This guide examines the current landscape of digital pathology and AI tools for control slide assessment, providing objective performance comparisons and detailed experimental methodologies relevant to researchers, scientists, and drug development professionals working within the context of IHC controls research.
Fundamental IHC Controls: A Research Framework
Core Control Types for Validated IHC
The foundation of any reliable IHC experiment rests on implementing appropriate controls. These controls systematically address potential variables and artifacts, ensuring observed staining patterns accurately reflect antigen-antibody interactions rather than technical artifacts.
Table 1: Essential Controls for IHC Experiments
| Control Type | Purpose | Interpretation of Results |
|---|---|---|
| No Primary Control | Detects non-specific binding of the secondary antibody or detection system [84]. | Any positive staining indicates false positives from the detection system [2]. |
| Blocking Peptide Control (Pre-absorption) | Confirms primary antibody specificity by blocking its binding sites [84]. | Significant reduction or loss of specific staining validates antibody specificity [84]. |
| Positive Tissue Control | Verifies the entire IHC protocol is functioning correctly [84] [2]. | Expected staining confirms protocol validity; lack of staining indicates technical failure [2]. |
| Negative Tissue Control | Identifies non-specific binding and false positives from the primary antibody [84]. | Any positive staining suggests non-specific antibody binding [84] [2]. |
| Isotype Control | Assesses non-specific Fc receptor or protein binding by the primary antibody [2]. | Staining similar to specific antibody indicates significant non-specific background [2]. |
| Endogenous Background Control | Evaluates inherent tissue autofluorescence or enzymatic activity [84] [2]. | Baseline staining levels guide interpretation thresholds for specifically stained samples. |
The Scientist's Toolkit: Essential Research Reagents
Successful IHC control experiments require specific reagents and materials. The following table details key components of the research toolkit for control slide preparation and assessment.
Table 2: Essential Research Reagent Solutions for IHC Controls
| Reagent/Material | Function | Application Example |
|---|---|---|
| Validated Primary Antibodies | Specifically binds the target antigen of interest. | Used in all test samples; omitted in "No Primary" controls [84]. |
| Blocking Peptide | The specific antigen used to generate the antibody. | Pre-incubated with primary antibody for blocking peptide controls [84]. |
| Isotype Control | A non-immune immunoglobulin matching the primary antibody's class and subtype. | Replaces the primary antibody in isotype controls to assess non-specific binding [2]. |
| Signal Detection System | Enzymatic (e.g., HRP) or fluorescent system that generates the detectable signal. | Must be tested in "No Primary" controls to rule out system-generated background [88]. |
| Validated Control Tissue | Tissues with known expression (positive) or absence (negative) of the target. | Serves as positive and negative tissue controls to validate the assay [84]. |
| Antigen Retrieval Buffers | Solutions that break protein cross-links from fixation, exposing epitopes. | Critical for optimizing signal in formalin-fixed, paraffin-embedded (FFPE) controls [88]. |
Digital Pathology and AI Fundamentals
From Microscopy to Digital Workflows
The field of pathology is undergoing a profound transformation, moving from a 140-year-old technology based on stained thin tissue sections viewed under a microscope to a modern paradigm powered by high-performance computing and machine learning [89]. Digital pathology addresses key limitations of conventional microscopy, including reliance on physical slides, difficulties in remote collaboration, and limited scalability [85]. This shift creates the essential technological foundation for AI applications by converting physical slides into standardized, high-quality digital whole-slide images (WSIs) that serve as input for computational algorithms [85].
Key technological advancements driving this field include high-performance computing with AI accelerator chips, robust image management systems integrated with laboratory information systems (LIS), advanced deep learning architectures, cloud computing solutions, and secure communication protocols that maintain data privacy compliance [85]. These innovations have collectively enabled the development and deployment of AI tools that can analyze control slides with consistency, speed, and quantitative precision beyond human capabilities.
AI Approaches and Applications in Pathology
Artificial intelligence, particularly deep learning, has emerged as a transformative force in pathology. These algorithms can recognize complex patterns in digitized slides, enabling large-scale image analysis and quantification of features that may be subtle or inconsistent when assessed manually [90] [91]. The applications are broad, spanning from cancer diagnosis and grading to predicting treatment response and inferring molecular status from standard H&E stains [92] [86].
A significant trend is the emergence of "foundation models" – AI models pre-trained on vast collections of whole-slide images (e.g., tens of thousands) that serve as a backbone for developing more specific diagnostic tools [86]. This approach democratizes AI development, allowing researchers with smaller datasets to build clinically useful applications by fine-tuning these pre-trained models for specific tasks such as control slide assessment [86]. The integration of AI in pathology workflows increasingly follows a "human-in-the-loop" paradigm where pathologists remain the final decision-makers, but AI guides them to work more efficiently and with greater accuracy [89].
Comparative Performance Analysis of AI Digital Pathology Tools
Objective Performance Metrics in Validation Studies
Rigorous validation studies demonstrate the measurable impact of AI on pathology assessment quality and efficiency. The following table summarizes key performance metrics from recent studies and implementations relevant to control slide assessment.
Table 3: AI Digital Pathology Tool Performance Comparison
| AI Tool / Study | Primary Function | Performance Metrics | Validation Context |
|---|---|---|---|
| Digital PATH Project [91] | HER2 status evaluation in breast cancer | High agreement with experts at high expression levels; greatest variability at low (1+) levels | 1,100 breast cancer samples; 10 AI tools compared |
| Nuclei.io [89] | Adaptive AI framework for pathologist workflow | Improved diagnostic efficiency and accuracy; rapid plasma cell identification (seconds vs. 5-10 minutes manually) | Stanford Medicine implementation; user studies with pathologists |
| CAPAI Biomarker [86] | Risk stratification in stage III colon cancer | Identified high-risk patients among ctDNA-negative cases (35% vs. 9% 3-year recurrence) | Combined analysis of pathologists and AI for prognostication |
| Mindpeak HER2 Assessment [86] | Digital HER2 IHC assessment in breast cancer | Boosted diagnostic agreement: 86.4% from 73.5% for HER2-low; 80.6% from 65.6% for HER2-ultralow | Six global academic centers; international multicenter study |
| Paige Prostate Detect [85] | Prostate cancer detection | 7.3% reduction in false negatives; improved sensitivity | FDA-cleared AI tool; diverse scanner platform compatibility |
Experimental Protocols for AI Validation
The development and validation of AI tools for pathology follow rigorous methodological frameworks to ensure reliability and generalizability.
Data Collection and Whole-Slide Imaging: Studies typically utilize formalin-fixed, paraffin-embedded (FFPE) tissue sections stained with H&E or IHC markers [91] [92]. Slides are digitized using high-resolution slide scanners from multiple vendors to ensure platform diversity. For example, the Digital PATH Project involved digitizing approximately 1,100 breast cancer samples stained with both H&E and HER2 IHC [91]. This approach captures the broad spectrum of variation in histological preparation and scanning instruments across different clinical sites, which is crucial for developing robust AI models [92].
AI Model Development and Training: Deep neural networks form the core architecture for most modern pathology AI systems [92]. The specific design—including image preprocessing steps, model architecture, and training approach—is optimized for each diagnostic task. For prostate cancer assessment, one protocol involves developing multiple AI models tailored for specific objectives: Gleason grading, perineural invasion detection, cribriform cancer identification, and cancer length measurement [92]. These models integrate to form a comprehensive AI system. Training typically employs carefully partitioned datasets with separate cohorts for development and validation to prevent information leakage [92].
Validation and Statistical Analysis: Robust validation follows predefined statistical analysis plans adhering to emerging guidelines such as TRIPOD+AI (Transparent Reporting of a multivariable prediction model of Individual Prognosis Or Diagnosis+AI) and CLAIM (Checklist for AI in Medical Imaging) [92]. The primary objective is typically to assess concordance between AI models and pathologists in diagnosing and scoring specimens. For example, in the Digital PATH Project, each participating digital pathology tool evaluated the same set of breast cancer samples, enabling direct comparison of their results with expert human pathologists and with each other [91]. This approach allows researchers to determine if different AI tools produce consistent and accurate results while characterizing performance using an independent reference set of samples.
Implementation in Research and Clinical Trials
AI for Quality Control and Standardization
In the context of IHC controls research, AI tools are increasingly deployed for quality control monitoring in both diagnostic and clinical trial settings. For example, research presented at ASCO 2025 highlighted how AI can significantly improve consistency in assessing HER2 expression levels, particularly for the challenging HER2-low and ultralow categories [86]. This capability is crucial for ensuring that IHC staining and interpretation meet quality standards across multiple testing sites in large clinical trials.
The implementation of AI for control slide assessment follows two primary paradigms: (1) automated quality control checks that flag staining irregularities or protocol failures before pathologist review, and (2) decision-support systems that provide quantitative assessments to guide final interpretation. These applications directly address the longstanding challenge of inter-observer variability in pathology, which in the case of Gleason scoring for prostate cancer, shows Cohen's kappa statistics varying from 0.30 to 0.70 between pathologists [92]. By providing consistent, quantitative assessments of control slides, AI systems help establish standardized baselines against which experimental staining quality can be objectively measured.
Regulatory Considerations and Future Directions
The regulatory landscape for AI in pathology is evolving rapidly, though adoption has historically lagged behind technological capabilities. As of March 2024, only three AI/ML Software as a Medical Device tools had received FDA clearance, highlighting the validation dataset gap rather than an absence of regulatory pathways [90]. Recent developments show progress, with the FDA granting Breakthrough Device Designation to AI-based computational pathology devices, including the first such designation for a cancer companion test [86].
Future directions in the field point toward increased use of multimodal AI that integrates whole-slide images with clinical and genomic data, the expansion of foundation models pretrained on massive diverse datasets, and the development of more sophisticated human-in-the-loop interfaces that optimize collaboration between pathologists and AI systems [86] [89]. These advancements will further enhance the role of automated control slide assessment in ensuring IHC quality and reliability, ultimately supporting more reproducible research and effective clinical trials in precision oncology.
Standardizing Controls for Multiplex IHC and Future Biomarkers
Multiplex immunohistochemistry and immunofluorescence (mIHC/IF) represent a transformative advancement in tissue-based diagnostics, enabling simultaneous detection of multiple antigens on a single tissue section to define complex immunophenotypes, quantify immune cell subsets, and assess spatial relationships within the tumor microenvironment [93]. Unlike conventional IHC, which is limited to single-marker assessment, mIHC/IF technologies can simultaneously detect anywhere from 3-5 markers using chromogenic methods to over 60 markers with advanced cyclic approaches [94] [95]. This capability is particularly valuable in immuno-oncology, where multiplex assays have demonstrated superior performance in predicting response to immune checkpoint inhibitors compared to PD-L1 IHC alone, tumor mutational burden, or gene expression profiling [93] [94].
However, the increased complexity of mIHC/IF introduces substantial challenges in standardization, particularly regarding positive and negative controls. Traditional IHC validation frameworks, as outlined by the College of American Pathologists, require rigorous validation of each assay-scoring system combination with harmonized concordance requirements set at 90% for predictive markers [15]. For mIHC/IF, these challenges are multiplied due to factors including antibody cross-reactivity, spectral overlap, signal amplification variability, and complex data analysis workflows [93] [95]. The Society for Immunotherapy of Cancer has recognized these challenges and convened task forces to establish best practice guidelines for both staining validation and image analysis to ensure robust, reproducible results across laboratories [93]. This guide examines the current landscape of control standardization in mIHC/IF, comparing emerging solutions and their applications in biomarker development.
Platform Comparisons: Control Strategies Across Multiplex IHC Technologies
The appropriate selection of controls for mIHC/IF varies significantly across different technological platforms. Each platform presents unique advantages and limitations for control implementation, influencing their suitability for specific research or clinical applications. The table below provides a systematic comparison of major mIHC/IF platforms and their control considerations.
Table 1: Comparison of Multiplex IHC/IF Platforms and Control Strategies
| Platform | Technology Principle | Plexing Capacity | Control Requirements | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Multiplexed IHC (Chromogenic) | Simultaneous/sequential application without removal of previous marker [93] | 3-5 markers [93] | Individual antibody controls, color deconvolution validation [93] [95] | Compatibility with brightfield microscopy, stable slides for archiving [95] | Limited plexing capacity, challenging co-localization studies due to color mixing [95] |
| MICSSS | Iterative cycles of staining, scanning, and stripping [93] | 10+ markers [93] | Control for epitope stability across cycles, antibody stripping efficiency [93] | Whole slide imaging, high plexing capacity [93] | Time-intensive process, potential cumulative tissue damage [95] |
| Multiplex IF (TSA-based) | Tyramide signal amplification with fluorophore-conjugated tyramides [93] [95] | 5-8 markers [93] | Spectral unmixing validation, autofluorescence controls, TSA titration [93] [95] | High sensitivity (100-fold amplification), same-species antibody compatibility [95] | Signal diffusion risk, photobleaching, complex optimization [95] |
| DNA-Barcoded Technologies | Antibodies conjugated to oligonucleotide barcodes [94] | 30-60+ markers [93] | Hybridization controls, barcode specificity validation [94] | Ultra-high plexing, minimal spectral overlap [94] | Specialized instrumentation required, high cost [94] |
| Digital Spatial Profiling | UV-cleavable oligonucleotide tags, region-of-interest analysis [93] | 40-50 markers [93] | ROI selection standardization, cleavage efficiency controls [93] | Targeted analysis, digital quantification [93] | Limited imaging area (0.28mm²), expensive platform [93] |
Innovative Control Methodologies: Automated Systems and Liquid Controls
Recent advancements in control methodologies focus on addressing the critical challenge of scarce positive control tissues, particularly for rare biomarkers. Automated IHC staining systems with integrated quality control modules represent a significant innovation in standardization. The LYNX480 PLUS System exemplifies this approach, featuring an IHC quality control module that automatically applies controls in liquid form (CLFs) to slides before the staining procedure [13].
CLFs are cell suspensions prepared from genetically modified cell lines designed to express or not express the target antigen, such as ALK for lung adenocarcinoma testing [13]. These controls demonstrate several advantages over traditional tissue-based controls:
- Circular Morphology and Even Cell Distribution: Automated application produces more regular circular shapes with better cell distribution compared to manual application [13].
- Staining Pattern Consistency: CLFs show changes in the same pattern as tissue controls under different antibody concentrations and antigen retrieval conditions [13].
- Reduced Tissue Consumption: Provides a convenient solution without consuming scarce patient tissue for daily quality control [13].
- Traceability: The entire QC procedure, including patient information and staining records, can be recorded and tracked via barcode scanning [13].
In validation studies, this automated approach combined with the BP6165 concentrated antibody demonstrated excellent sensitivity (98.30%) and specificity (100%) in 87 lung adenocarcinoma biopsy specimens when compared to fluorescence in situ hybridization [13]. This performance highlights the potential of automated control systems to enhance reproducibility while addressing ethical concerns related to rare patient tissue consumption.
Experimental Protocols for Control Validation
Orthogonal Validation of IHC Assays
Comprehensive validation of therapy-guiding IHC biomarker assays requires a multi-step approach that extends beyond typical diagnostic validations. The validation framework developed for the NCI-MATCH EAY131 trial provides a robust model, incorporating both analytical and clinical validation components [96]. The process includes:
- Primary Antibody Selection: Selection based on epitope location within the protein structure, with preference for segments infrequently impacted by mutations or deletions. Peer-reviewed studies demonstrating sensitivity and specificity using orthogonal protein detection methods provide supporting evidence [96].
- Assay Optimization: Determination of optimal antibody dilution, antigen retrieval conditions, and incubation time using automated platforms. The ideal antibody dilution represents the lowest concentration yielding optimal sensitivity and specificity balance [96].
- Interpretation Criteria Development: Establishment of clear guidelines for staining patterns (nuclear, cytoplasmic, membranous) based on biological knowledge of the protein. This includes definitions for handling indeterminate results and standardized reporting terminology that unambiguously describes assay results rather than clinical implications [96].
- Orthogonal Validation: Comparison of IHC results with non-immunohistochemical methods such as flow cytometry or fluorescent in-situ hybridization [15] [96].
- Tissue Validation: Use of patient samples and cell lines for analytical validation, including sensitivity and specificity calculations using various gold standard references [96].
Control Procedures for Multiplex IHC Workflows
For multiplex IHC workflows, the Society for Immunotherapy of Cancer recommends additional quality control measures specific to the complexities of multiplex staining:
- Image Acquisition Controls: Implementation of calibrated scanners, well-focused images, and reduced tiling effects. The appropriate per-pixel resolution must be determined based on the specific research question and technology [93].
- Color Deconvolution and Spectral Unmixing Validation: For both mIHC and mIF, these processes are essential for accurate marker expression assignment and significantly impact downstream cell segmentation and phenotyping [93].
- Region of Interest Selection Standardization: Documentation of the number of ROIs analyzed per specimen, selection methodology, and ROI inclusion/exclusion criteria. For heterogeneous markers, extended sampling strategies or whole slide imaging may be necessary [93].
- Batch-to-Batch Correction: Quality control measures to address variation between different staining batches [93].
- Algorithm Verification: Validation of image analysis algorithms for tissue segmentation, cell segmentation, and phenotyping [93].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of standardized controls for multiplex IHC requires carefully selected reagents and tools. The following table outlines essential research reagent solutions and their functions in ensuring robust, reproducible multiplex IHC experiments.
Table 2: Essential Research Reagent Solutions for Multiplex IHC Controls
| Reagent/Tool | Function | Application Notes | Validation Requirements |
|---|---|---|---|
| Genetically Modified Cell Lines | Provide consistent positive/negative controls for target antigens [13] | Can be formatted as controls in liquid form (CLFs) for automated application [13] | Expression stability across passages, comparison to clinical samples [13] |
| Tyramide Signal Amplification Reagents | Enable high-sensitivity detection for low-abundance targets [95] | Fluorophore or chromogen-conjugated tyramides for sequential staining [95] | Titration to prevent over-amplification, validation of stripping efficiency [95] |
| Multispectral Imaging Systems | Acquire images with spectral separation for multiplex analysis [93] [94] | Platforms include Vectra (PerkinElmer), CODEX (Akoya), and others [94] | Spectral library validation, unmixing algorithm verification [93] |
| Automated Staining Platforms | Standardize staining procedures across multiple runs [13] [96] | Systems include DISCOVERY ULTRA (Roche), LYNX480 PLUS (Biolynx) [13] [94] | Inter-instrument concordance, lot-to-lot reagent variation [96] |
| Image Analysis Software | Quantify marker expression, cell segmentation, and spatial relationships [93] | Includes inForm (PerkinElmer), Definiens, and custom algorithms [93] [94] | Algorithm verification against manual counts, reproducibility assessment [93] |
| Reference Standard Tissues | Provide benchmark for expected staining patterns and intensity [15] [96] | Multi-tissue blocks with known expression patterns for multiple markers [96] | Inter-laboratory concordance, stability over time [15] |
Future Directions: Emerging Technologies and Standardization Initiatives
The future of controls for multiplex IHC is evolving toward increased automation, artificial intelligence integration, and novel control materials. The global IHC market, expected to reach $5.14 billion by 2030, is driving innovation in quality control solutions [97]. Several key trends are shaping this evolution:
Artificial Intelligence in Quality Control: AI-powered image analysis algorithms are increasingly being integrated into IHC workflows to quantify biomarker expression, detect rare cell types, and identify tissue abnormalities with greater precision than manual methods [97]. These systems can learn from control samples to establish acceptance criteria for staining quality.
Virtual Staining Approaches: Deep generative models are being developed to virtually generate IHC images from H&E-stained samples, potentially reducing the need for physical controls and multiple staining procedures [18]. While not yet replacements for experimental controls, these approaches may transform control strategies in the future.
Multi-institutional Harmonization Efforts: Organizations like the Society for Immunotherapy of Cancer are leading harmonization initiatives to establish standardized protocols, share raw outputs and processed results, and develop representative photomicrographs for mIHC/IF assays [93].
Integrated Quality Management Systems: Automated platforms with built-in quality control modules, such as the LYNX480 PLUS system, represent a movement toward fully integrated quality management that tracks the entire testing process from sample receipt to result reporting [13].
These advancements, combined with comprehensive validation frameworks like those implemented in the NCI-MATCH trial, are paving the way for more reliable, reproducible multiplex IHC assays that will support both research and clinical applications in the era of precision medicine and immunotherapy [96].
Conclusion
The rigorous implementation of positive and negative controls is the cornerstone of reliable and interpretable IHC data, forming a direct link between experimental integrity and confident scientific and diagnostic conclusions. By systematically applying the controls outlined across the foundational, methodological, troubleshooting, and validation intents, researchers can effectively verify assay specificity, diagnose protocol failures, and meet evolving accreditation standards like the 2024 CAP guideline update. The future of IHC controls lies in their integration with digital pathology and AI for automated interpretation, enhanced standardization for complex multiplex assays, and their critical role in validating novel biomarkers, ultimately ensuring that IHC remains a robust pillar in both drug development and clinical diagnostics.
References
- 1. Controls for Immunohistochemistry: The Histochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4212362/]
- 2. Controls in IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/controls-in-ihc]
- 3. How to Design Positive and Negative Controls [https://www.bosterbio.com/how-to-design-positive-negative-controls-ihc-western-blot-elisa?srsltid=AfmBOooUaWf-oOxyYQ-rfa7SI3e6U2FOJbtEfxFLmppa-9UdN9M2UMTv]
- 4. Histopathological Considerations for IHC-based Studies [https://waxitinc.com/histopathological-considerations-for-ihc-based-studies/]
- 5. Experimental Validation Of Peptide Immunohistochemistry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2672113/]
- 6. Frequently Asked Questions from Immunohistochemistry ... [https://www.cap.org/member-resources/councils-committees/immunohistochemistry-topic-center/frequently-asked-questions-from-immunohistochemistry-laboratories]
- 7. Intro to Immunohistochemistry (IHC) Staining: Steps & Best ... [https://www.leicabiosystems.com/us/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 8. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOoonErnlyX4GTWwonqIPD1isiC2TOUR7AUbBvpxWU9XwK9Ovc6ub]
- 9. Overview of Immunohistochemistry (IHC) [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-immunohistochemistry.html]
- 10. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 11. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOorrd4YeNrkCu3iNDXr4ALaDCHleioiw223q0-33XmTZ8Le2A7ei]
- 12. Monitoring Immunohistochemical Staining Variations Using ... [https://www.sciencedirect.com/science/article/pii/S0023683725000157]
- 13. A novel automated IHC staining system for quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11864879/]
- 14. A novel automated IHC staining system for quality control ... [https://www.por-journal.com/journals/pathology-and-oncology-research/articles/10.3389/pore.2025.1611964/full]
- 15. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 16. Principles of Analytic Validation of Immunohistochemical ... [https://www.guidelinecentral.com/guideline/24377]
- 17. Reagents for Reliable Immunohistochemistry (IHC) Results [https://www.cellsignal.com/applications/immunohistochemistry/solutions-for-consistent-ihc-results?srsltid=AfmBOopZW4ypuEwR-Q6OahejG83j_2AhC3F0w9Xobiz9_xdwDy_oqdoU]
- 18. H&E to IHC virtual staining methods in breast cancer [https://www.nature.com/articles/s41746-025-01741-9]
- 19. Standardization of Negative Controls in Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4206554/]
- 20. Beginner's Guide to Choosing Isotype Controls [https://nordicbiosite.com/blog/beginners-guide-to-choosing-isotype-controls]
- 21. Isotype Controls [https://www.antibodies.com/primary-antibodies/isotype-controls]
- 22. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOorHxT7mw7mL-WqDuemlfhE7sktEpMn1fAe70FpmUsG8g1PLYj8O]
- 23. Immunohistochemistry Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/immunohistochemistry-market]
- 24. Designing a Successful IHC/ICC Experiment [https://www.rndsystems.com/resources/technical/designing-successful-ihc-icc-experiment]
- 25. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOopKZ-TI2Mi_IbZ-4LaTkfne_FGqgICTUnz_VN0j79J_UJ9i2_YR]
- 26. Peptide Blocking [https://www.novusbio.com/support/blocking-with-immunizing-peptide?srsltid=AfmBOopYAxirMFIpW31KqvK9HFrgSI2NauxW65by0xzzIiyC7xfv1be9]
- 27. 4 controls for immunohistochemistry (IHC) you need to use [https://www.alomone.com/4-controls-for-immunohistochemistry-ihc-you-need-to-use?srsltid=AfmBOooYdzPPGBZj401MtNtvZzRI1n407CmhcPtvV8dAC-mCyiJhlUcI]
- 28. The Importance of IHC/ICC Controls [https://www.rndsystems.com/resources/protocols/importance-ihcicc-controls]
- 29. Blocking with immunizing peptide protocol [https://www.abcam.com/en-us/technical-resources/protocols/blocking-with-immunizing-peptides]
- 30. Blocking Peptide Protocols for Immunohistochemistry (IHC) ... [https://www.alomone.com/info/peptide-blocking-protocols-for-immunostaining?srsltid=AfmBOor0tjMCK9fzSzjFMnIdD1OlYQuGV1SnEuZ-auD7o88y35O0DHE0]
- 31. Specificity Controls for Immunocytochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC3351124/]
- 32. Autofluorescence [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/autofluorescence/]
- 33. 5 Sources Of Non-specific Staining And Background In IHC ... [https://vectorlabs.com/blog/5-sources-of-non-specific-staining-and-background-in-ihc-and-if/?srsltid=AfmBOopj3EkkxeTagSjBUyYXPGlatf6blZxjUyI5XF8Y9D3K5vpEGd5C]
- 34. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467]
- 35. 4 controls for immunohistochemistry (IHC) you need to use [https://www.alomone.com/4-controls-for-immunohistochemistry-ihc-you-need-to-use?srsltid=AfmBOorFJLB-pBXcd-sp9weEz7_8T6caF2oD_dm4TyUwSW34Os-YOnhQ]
- 36. 5 Sources Of Non-specific Staining And Background In IHC ... [https://vectorlabs.com/blog/5-sources-of-non-specific-staining-and-background-in-ihc-and-if/?srsltid=AfmBOooJJ0bzU8MeqSjtZd9hQh5zGpScXkCbnlzUimrWt9dwpRzgWFNP]
- 37. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOor3JADTkH3haY6xsHja3ChQZST6NxqLAJzqjihTncgNCVenwDa8]
- 38. Immunohistochemical Validation of Rare Tissues and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8143380/]
- 39. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOorjx6BD7zaRMUnS0f4CkyRIInTtn0OKch9aK1DWYFvjiNJCHqR3]
- 40. Mouse-on-mouse for Immunohistochemistry: tips and tricks [https://www.ptglab.com/news/blog/mouse-on-mouse-for-immunohistochemistry-tips-and-tricks/?srsltid=AfmBOoqyXa2Sp7Tx8lhcAEGMBi7cdfJtA2vfwMEngyrdKmditnXplAhS]
- 41. Antibodies 101: Avoiding the Mouse on Mouse Mess in IHC [https://blog.addgene.org/antibodies-101-avoiding-the-mouse-on-mouse-mess-in-ihc]
- 42. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOop22xahZ6gOBtaY6YdmT8V1TngcFHES3AFvV8F4RWhn-mQKPWHR]
- 43. Troubleshooting and choosing the right type of slides. [https://www.statlab.com/news/troubleshooting-and-choosing-the-right-type-of-slides]
- 44. What Controls are Necessary for Immunohistochemistry? [https://www.enzo.com/note/what-controls-are-necessary-for-immunohistochemistry/]
- 45. Antibody validation of immunohistochemistry for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4240800/]
- 46. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOor5jE2pwqpdEYpo2KRrauY0KCTSNqYqNi4pXPCODoXvgdXsGEFS]
- 47. Blocking Peptide Protocols for Immunohistochemistry (IHC) ... [https://www.alomone.com/info/peptide-blocking-protocols-for-immunostaining?srsltid=AfmBOop9nUv_up3JX4OkwR03bEGBlTpi0_EKSoXJRiQYwtZXRVizpmh0]
- 48. Peptide Blocking [https://www.novusbio.com/support/blocking-with-immunizing-peptide?srsltid=AfmBOoo0HpKr1xK_KRtu5fLVdNrcjhMygAPfO_p_gcHap9BrT0UUrla-]
- 49. Accelerated instability testing reveals quantitative mass ... [https://www.nature.com/articles/s41374-019-0366-y]
- 50. Blocking Strategies for IHC [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/blocking-strategies-ihc.html]
- 51. Methods to Block Endogenous Detection [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/methods-block-endogenous-detection.html]
- 52. Tips for Reducing Non-specific Staining in IHC [https://www.biossusa.com/blogs/news/tips-for-reducing-non-specific-staining-in-ihc?srsltid=AfmBOooF3hJEOiUvCCUSD1GJjk4gfDHeJILLFLQaTln6-GBsmiYY6UFB]
- 53. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 54. Strept(avidin)–Biotin Complex Method for IHC Detection [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/avidin-biotin-complex-method-ihc-detection.html]
- 55. How to Design Positive and Negative Controls [https://www.bosterbio.com/how-to-design-positive-negative-controls-ihc-western-blot-elisa?srsltid=AfmBOoqdo9ngU19yPIB50G93JtEDvNFlI1jy6nbhWW-4qcvE-qFrsZFo]
- 56. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOorz73NgWJ1l001zx-jz6jkTxvXUVXo3BvmZiytbKnWvaeLFflmo]
- 57. Quantitative comparison of immunohistochemical staining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3379953/]
- 58. Deep Learning–Based H-Score Quantification of ... [https://www.sciencedirect.com/science/article/pii/S0893395223003034]
- 59. A novel quantitative immunohistochemistry method for ... [https://www.nature.com/articles/modpathol2016176]
- 60. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467?utm_source=chatgpt.com]
- 61. Selecting an Optimal Positive IHC Control for Verifying ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6437345/]
- 62. Recommended controls for flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/recommended-controls-for-flow-cytometry]
- 63. Positive and negative controls for antibody validation [https://www.euromabnet.com/guidelines/positive-negative-controls.php]
- 64. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOopg7ViU16Y2uAkZqDP222ItVyh7zxgM9i6BTa14FKugsGlNQo9l]
- 65. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 66. Troubleshooting Immunohistochemistry [https://bitesizebio.com/13392/troubleshooting-immunohistochemistry/]
- 67. Primary Antibody Selection & Optimization [https://www.rndsystems.com/resources/protocols/primary-antibody-selection-optimization]
- 68. Comparison of different scoring systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC501013/]
- 69. How Antibody Diluent For IHC Works — In One Simple ... [https://www.linkedin.com/pulse/how-antibody-diluent-ihc-works-one-simple-flow-2025-h0rff/]
- 70. Antibody Diluent For IHC in the Real World: 5 Uses You'll ... [https://www.linkedin.com/pulse/antibody-diluent-ihc-real-world-5-uses-youll-actually-see-ug1ie/]
- 71. Top Automated IHC And ISH Stainer Companies & How to ... [https://www.linkedin.com/pulse/top-automated-ihc-ish-stainer-companies-how-compare-qdqne/]
- 72. Analytic Validation of Immunohistochemical Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938252/]
- 73. IHC Stainer Outcomes: Decoding the Significance of Your ... [https://www.celnovte.com/solution/ihc-stainer-outcomes-decoding-the-significance-of-your-test-results/]
- 74. A critical evaluation of strategies used for validation ... [https://www.sciencedirect.com/science/article/pii/S1574789114000568]
- 75. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOophc0wFNfzGrsrrtdF0HH0J8oYyZVO5iDno_x3CBRidvhkrODMI]
- 76. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOorj7E5YFAx3V1Y7uoSTH5ZDVIFRhpfIMrSZ3PVAJdkLqB5A2V8n]
- 77. Comparative Evaluation of Three Primary Antibody Clones ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452752/]
- 78. p16INK4A-deficiency predicts response to combined HER2 ... [https://www.nature.com/articles/s41467-022-29081-2]
- 79. Immunohistochemistry staining [https://www.abcam.com/en-us/knowledge-center/immunohistochemistry/ihc-staining]
- 80. Concordance of HER2-low scoring in breast carcinoma ... [https://www.sciencedirect.com/science/article/pii/S096097762300509X]
- 81. Lessons Learned, Challenges Taken, and Actions Made for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10396077/]
- 82. Synergistic H&E and IHC image analysis by AI predicts ... [https://www.nature.com/articles/s43856-025-01045-9]
- 83. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOooA1vd5ty1733eSB2eMLRQcXPKSBMZH-UT8oheTtlRhMnBSq9mH]
- 84. 4 controls for immunohistochemistry (IHC) you need to use [https://www.alomone.com/4-controls-for-immunohistochemistry-ihc-you-need-to-use?srsltid=AfmBOooSmlzkVYcjA75qrCjpCvDwMXLz7VAvpMi9DOMuZQNS9788Q4rT]
- 85. The Rise of AI-Assisted Diagnosis: Will Pathologists Be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468387/]
- 86. Digital Pathology and AI Highlights from ASCO 2025 [https://proscia.com/digital-pathology-and-ai-highlights-from-asco-2025/]
- 87. PathAI Publications [https://www.pathai.com/publications]
- 88. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOootTcsrBERWy_6mSAMP1VEdg37IFlFWMj1469OgBdUU8HIqQR3w]
- 89. AI tool gives pathologists speed, accuracy and a new way to ... [https://med.stanford.edu/news/all-news/2025/09/ai-tool-pathology.html]
- 90. Digital pathology imaging artificial intelligence in cancer ... [https://www.sciencedirect.com/science/article/pii/S2153353925001178]
- 91. Diagnostics World - Comparison of AI Digital Pathology ... [https://friendsofcancerresearch.org/news/diagnostics-world-comparison-of-ai-digital-pathology-tools-finds-means-to-measure-performance/]
- 92. Development and retrospective validation of an artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12258300/]
- 93. Society for Immunotherapy of Cancer - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11749220/]
- 94. Overview of multiplex immunohistochemistry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7170662/]
- 95. Multiplex immunohistochemistry (mIHC): A technical deep ... [https://www.abcam.com/en-us/knowledge-center/immunohistochemistry/multiplex-immunohistochemistry-mihc]
- 96. Validation of Immunohistochemical Assays for Integral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5796858/]
- 97. Immunohistochemistry Market Growth Accelerates with AI & ... [https://www.marketsandmarkets.com/blog/HC/immunohistochemistry-market-growth]