Solving Deparaffinization Problems in IHC: A Complete Guide for Reproducible Research
This article provides a comprehensive resource for researchers, scientists, and drug development professionals facing challenges with deparaffinization in immunohistochemistry (IHC).
Solving Deparaffinization Problems in IHC: A Complete Guide for Reproducible Research
Abstract
This article provides a comprehensive resource for researchers, scientists, and drug development professionals facing challenges with deparaffinization in immunohistochemistry (IHC). It covers the foundational role of deparaffinization in the IHC workflow, detailing how improper wax removal directly causes staining artifacts, high background, and false-negative results. The content delivers robust methodological protocols for both manual and automated systems, a systematic troubleshooting guide for common problems like spotty staining and weak signal, and finally, explores validation techniques and comparative analyses to ensure staining reproducibility and data integrity for preclinical and clinical research.
The Critical Role of Deparaffinization: Why This Foundational Step Can Make or Break Your IHC Results
Scientific Context: The Critical Role of Deparaffinization
In immunohistochemistry (IHC) research, Formalin-Fixed Paraffin-Embedded (FFPE) tissues are invaluable resources that combine excellent morphological preservation with vast clinical data, making them essential for translational research and biomarker discovery [1]. The FFPE process provides mechanical support for thin sectioning by embedding tissue in paraffin wax after formalin fixation, which stabilizes proteins and prevents degradation [2].
However, this process creates a fundamental accessibility challenge: the paraffin wax used for embedding forms a physical barrier that prevents antibody penetration and access to target antigens [1]. Deparaffinization is therefore the essential gateway procedure that removes this hydrophobic wax matrix to enable aqueous-based reagents, including antibodies and detection systems, to reach their cellular targets.
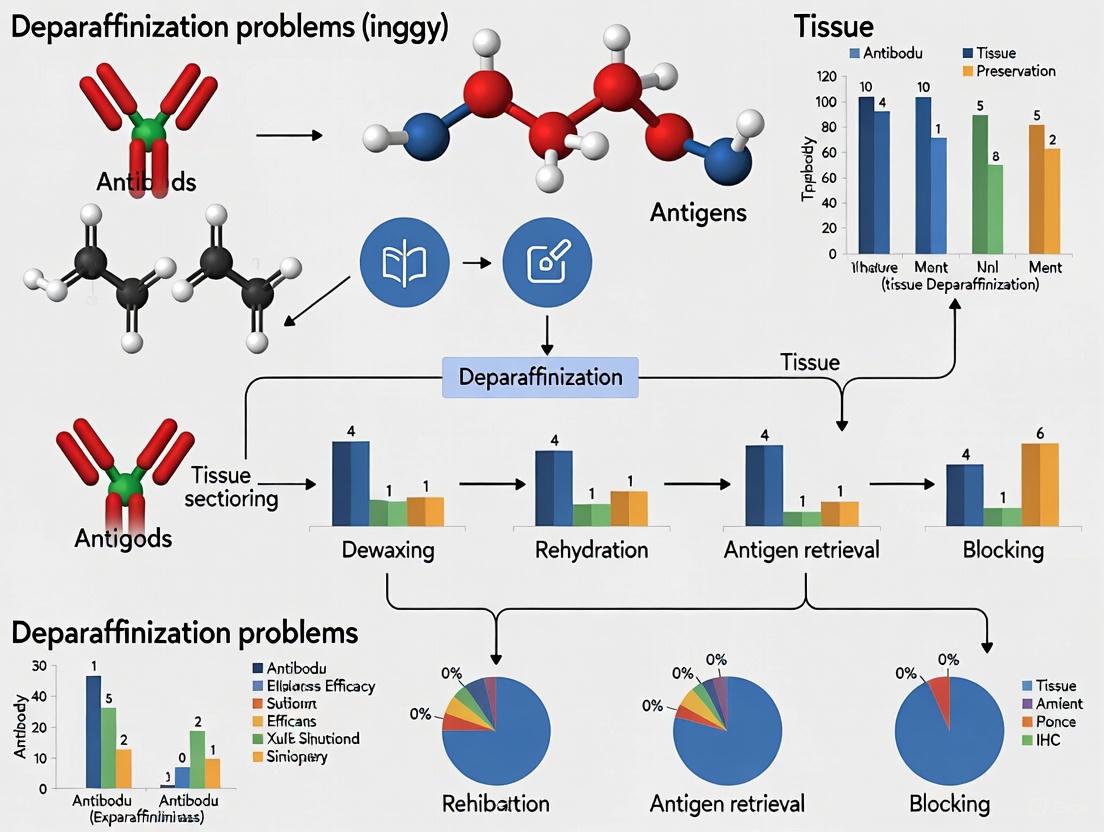
The relationship between deparaffinization and downstream IHC success can be visualized as a critical pathway where early failures compromise all subsequent steps:
Standard Deparaffinization Protocol
A rigorously executed deparaffinization protocol is fundamental to successful IHC outcomes. The following comprehensive workflow details each critical step:
Complete Deparaffinization and Rehydration Protocol
| Step | Solution | Incubation Time | Purpose | Critical Parameters |
|---|---|---|---|---|
| 1 | Xylene (or substitute) | 10-15 minutes | Initial paraffin dissolution | Use fresh solution for optimal efficiency |
| 2 | Xylene (or substitute) | 10-15 minutes | Complete wax removal | Second change ensures thorough clearing [2] |
| 3 | 100% Ethanol | 5 minutes | Removal of xylene | Prevents carryover into graded alcohols |
| 4 | 100% Ethanol | 5 minutes | Complete dehydration | Ensures no water contamination |
| 5 | 95% Ethanol | 5 minutes | Begin rehydration | Gradual water introduction |
| 6 | 95% Ethanol | 5 minutes | Continue rehydration | Prevents tissue stress |
| 7 | 85% Ethanol | 5 minutes | Further hydration | Stepwise dilution |
| 8 | 85% Ethanol | 5 minutes | Equilibrium | Consistent hydration |
| 9 | 75% Ethanol | 5 minutes | Near-final hydration | Prepares for aqueous buffer |
| 10 | 75% Ethanol | 5 minutes | Final alcohol step | Complete transition [2] |
| 11 | Distilled Water | 3 washes | Complete hydration | Ready for antigen retrieval [3] |
This meticulous progression from organic solvents to aqueous solutions is crucial for maintaining tissue architecture while ensuring complete paraffin removal. Incomplete deparaffinization may cause spotty, uneven background staining and poor antibody penetration, compromising experimental results [4].
Troubleshooting Guide: Common Deparaffinization Problems and Solutions
Researchers frequently encounter several specific challenges during deparaffinization that can dramatically affect IHC outcomes:
Deparaffinization Troubleshooting Reference Table
| Problem | Root Cause | Visual Indicators | Solution | Prevention |
|---|---|---|---|---|
| High Background Staining | Incomplete paraffin removal | Spotty, uneven background [4] | Repeat with fresh xylene and new sections [4] | Use fresh xylene changes; verify timing |
| Weak or Absent Staining | Residual wax blocking antibody access | No specific staining despite positive control | Optimize deparaffinization protocol [3] | Follow graded alcohol series precisely |
| Tissue Detachment from Slides | Inadequate slide preparation or harsh processing | Tissue loss during staining procedure | Use charged/adhesion slides [5] | Ensure proper slide coating and drying |
| Non-specific Staining | Tissue drying after rehydration | High background across entire section | Keep slides hydrated after rehydration [2] | Never allow slides to dry after step 11 |
Researcher's Toolkit: Essential Materials for Deparaffinization
Successful deparaffinization requires specific reagents and equipment to ensure consistent, reliable results:
Essential Deparaffinization Reagents and Equipment
| Item | Function | Technical Notes |
|---|---|---|
| Xylene or Xylene Substitutes | Primary paraffin solvent | Most common solvent; less hazardous alternatives available [2] |
| Ethanol (100%, 95%, 85%, 75%) | Gradual rehydration series | Prevents tissue damage from rapid water introduction [5] |
| Coplin Jars or Automated Stainers | Container for processing | Consistent solvent exposure; 30-slide capacity before changing [5] |
| Charged/Adhesion Microscope Slides | Tissue section support | Prevents detachment during processing [5] |
| Distilled Water | Final hydration | Preparation for antigen retrieval steps |
| 3'-Deoxy-3'-fluorothymidine-d3 | 3'-Deoxy-3'-fluorothymidine-d3, MF:C10H13FN2O4, MW:247.24 g/mol | Chemical Reagent |
| DBCO-N-bis(PEG4-acid) | DBCO-N-bis(PEG4-acid), MF:C41H56N2O14, MW:800.9 g/mol | Chemical Reagent |
Frequently Asked Questions
What are the consequences of using exhausted xylene solutions?
Exhausted xylene has reduced paraffin-dissolving capacity, leading to incomplete deparaffinization. This results in residual wax barriers that prevent antibody access to antigens, causing weak staining and high background [4]. Replace xylene after processing approximately 30 slides [5].
Why is the graded alcohol series necessary instead of direct water immersion?
Gradual rehydration through graded alcohols (100%→95%→85%→75%) prevents sudden osmotic shifts that can damage tissue morphology. This preserves cellular architecture while ensuring complete transition from organic to aqueous environments [2] [5].
How can I verify that deparaffinization was successful?
Visual inspection alone is insufficient. Include a positive control tissue known to express your target antigen. Successful staining in positive controls with appropriate negative controls confirms adequate deparaffinization. Persistent issues across multiple antibodies indicate processing problems [4].
What are the critical steps to prevent tissue detachment?
Use charged or adhesive slides, ensure sections are completely dry before deparaffinization (oven drying at 60°C for at least 2 hours or ideally overnight), and avoid aggressive fluid transfer during processing [5].
Are there alternatives to xylene for deparaffinization?
Yes, several commercially available xylene substitutes exist that are less hazardous. Follow the manufacturer's instructions for ethanol exchange and mounting procedures specific to the alternative agent [2].
What are the immediate staining artifacts caused by incomplete deparaffinization?
Incomplete deparaffinization directly causes specific, visible artifacts that compromise data interpretation. The primary issues include:
- Spotty, uneven background staining: Residual paraffin wax creates a physical barrier that prevents uniform reagent access to the tissue, leading to irregular staining patterns with high, uneven background [6] [7].
- Weak or absent target signal: Wax remnants block antibody binding to target antigens, resulting in false-negative results or significant signal loss, which can be misinterpreted as low target expression [7].
- Irregular DAB precipitation: The chromogenic 3,3'-Diaminobenzidine (DAB) reaction can become trapped in wax-containing areas, producing nonspecific, granular precipitate not associated with actual antigen presence [6].
These artifacts directly threaten experimental reproducibility by introducing variability in staining intensity and pattern between samples processed in different batches or by different personnel.
How does residual wax lead to non-reproducible data in multi-center studies?
Incomplete wax removal introduces critical pre-analytical variables that systematically undermine reproducibility:
- Variable antibody penetration: Residual wax creates unpredictable physical barriers that cause differential antibody access to epitopes across tissue sections and between experimental runs [7].
- Inconsistent antigen retrieval efficacy: Heat-induced epitope retrieval (HIER) solutions cannot properly penetrate wax-blocked areas, creating localized zones where antigens remain masked despite retrieval attempts [6] [8].
- Irreproducible quantification results: Automated image analysis systems misinterpret staining artifacts as true signal, generating falsely elevated background measurements or missing genuine positive signals in blocked areas [9].
For multi-center trials and longitudinal studies, these inconsistencies manifest as unacceptable inter-laboratory variation, potentially invalidating collaborative research findings and biomarker validation studies.
What validated protocols ensure complete paraffin removal?
The following standardized protocols guarantee complete deparaffinization for reproducible IHC results:
| Step | Reagent | Duration | Repetitions | Critical Control Points |
|---|---|---|---|---|
| 1 | Xylene | 10 minutes | 2-3 changes | Check solution clarity after each change |
| 2 | 100% Ethanol | 5-10 minutes | 2 changes | Ensure no water contamination |
| 3 | 95% Ethanol | 5 minutes | 1-2 changes | Gradual hydration |
| 4 | 70% Ethanol | 5 minutes | 1-2 changes | Prepare for aqueous buffers |
| 5 | 50% Ethanol | 5 minutes | 1-2 changes | Optional step |
| 6 | Deionized Water | 5 minutes | 2 changes | Complete rehydration |
| Platform | Dewax Solution | Temperature | Cycles | Additional Notes |
|---|---|---|---|---|
| Leica BOND RX | Bond Dewax Solution | Ambient | Programmed | Integrated with antigen retrieval |
| BioGenex i6000 | Clearify Clearing Agent | 25°C | 1-2 | Solvent-free options available |
| Ventana Ultra | Proprietary dewax | 37-72°C | System-defined | Full automation with minimal hands-on time |
Consequence Pathway of Incomplete Dewaxing
What quality control checks verify adequate deparaffinization?
Implement these essential quality control measures to validate complete wax removal:
- Visual inspection under polarized light: Residual paraffin appears birefringent under polarized microscopy, allowing direct visualization of incomplete deparaffinization before staining [10].
- Blank slide control: Process a control slide without primary antibody through the entire IHC procedure; any DAB development indicates nonspecific background from inadequate dewaxing [11].
- Hematoxylin-only staining: After deparaffinization, stain with hematoxylin only; clear, uniform nuclear staining without cytoplasmic speckling indicates successful wax removal [12].
- Solvent clarity monitoring: Note xylene/clearing agent turbidity during processing; cloudy solutions indicate wax saturation and need for fresh reagent changes [6].
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent Category | Specific Products | Function in Deparaffinization | Protocol Considerations |
|---|---|---|---|
| Clearing Agents | Xylene, Clearify Clearing Agent | Dissolves and removes paraffin wax | Use fresh solutions; 2-3 changes of 5-10 minutes each [8] [10] |
| Hydrophobic Barrier Pens | Dako Pen, Vector Pen | Creates liquid barrier around tissue | Apply after complete deparaffinization before aqueous steps [10] |
| Rehydration Alcohols | 100%-50% Ethanol graded series | Gradually replaces organic solvent with water | Ensure absolute alcohol is water-free; progressive concentration steps [12] |
| Automated Platform Solutions | Bond Dewax Solution, Leica dewax reagents | Platform-specific wax removal | Follow manufacturer cycles; integrated with staining platforms [8] |
| Vitronectin (367-378) | Vitronectin (367-378), MF:C70H122N32O16, MW:1667.9 g/mol | Chemical Reagent | Bench Chemicals |
| 20-Methyltetracosanoyl-CoA | 20-Methyltetracosanoyl-CoA, MF:C46H84N7O17P3S, MW:1132.2 g/mol | Chemical Reagent | Bench Chemicals |
Standardized Dewaxing and Rehydration Workflow
How do we troubleshoot persistent background after deparaffinization?
When background staining persists despite standard deparaffinization protocols:
- Extend xylene incubation: Increase initial xylene immersion to 15-20 minutes with 3-4 fresh changes, particularly for thick sections (>5μm) or densely packed tissues [12] [10].
- Incorporate solvent agitation: Gentle agitation during xylene incubation improves wax dissolution from tissue crevices and dense cellular areas [7].
- Verify reagent quality: Degraded or water-contaminated alcohols create incomplete hydration chains that trap wax; use fresh, high-grade solvents exclusively [6].
- Pre-warm xylene: For difficult tissues, pre-warm xylene to 37°C (not higher) to improve wax solubility without damaging antigen integrity [8].
- Implement two-phase systems: Automated platforms like Biogenex i6000 use two-phase deparaffinization with specialized clearing agents for superior wax removal [8].
Complete paraffin removal is not merely a technical formality but a fundamental prerequisite for reproducible immunohistochemistry. The implementation of validated, rigorous deparaffinization protocols represents a critical control point in ensuring data integrity across research and diagnostic applications.
How does inadequate deparaffinization directly cause spotty background and weak staining?
Inadequate deparaffinization creates two primary failure modes in immunohistochemistry (IHC) experiments: spotty, uneven background staining and weak or absent specific signal [13]. These issues stem from a fundamental physical barrier preventing proper reagent penetration and interaction.
The following diagram illustrates the causal relationship between insufficient deparaffinization and the observed staining artifacts:
The mechanism is straightforward: residual paraffin wax acts as a physical barrier that blocks antibody access to target antigens within the tissue section [13] [14]. When primary antibodies cannot reach their epitopes, the result is weak or non-existent specific staining. Concurrently, this residual wax can trap detection reagents nonspecifically, leading to the characteristic spotty background pattern that obscures morphological detail and compromises data interpretation [13].
What is the experimental evidence linking deparaffinization to staining artifacts?
The connection between deparaffinization and staining quality is well-established in standardized IHC protocols and troubleshooting guides. The evidence comes from systematic observation and protocol optimization rather than a single definitive experiment.
- Direct Protocol Advisories: Technical resources explicitly state that "inadequate deparaffinization may cause spotty, uneven background staining" and recommend repeating experiments with new tissue sections using fresh xylene as the definitive solution [13].
- Signal Integrity Findings: Incomplete paraffin removal is identified as a leading cause of "weak or no staining," directly impeding antibody penetration and necessitating longer deparaffinization times or fresh solvents [14].
- Fixation Context: While prolonged formalin fixation (over weeks) minimally affects most antigens [15], improper deparaffinization causes immediate and severe artifacts. Proper deparaffinization is a prerequisite for effective subsequent steps like antigen retrieval, which reverses formalin-induced cross-links [16] [2].
The table below summarizes the key staining artifacts and their relationship to deparaffinization failures:
| Staining Artifact | Direct Cause | Impact on Interpretation | Recommended Solution |
|---|---|---|---|
| Spotty, Uneven Background [13] | Residual wax trapping detection reagents nonspecifically. | Obscures cellular morphology; compromises specific signal detection. | Repeat with new sections and fresh xylene [13]. |
| Weak or No Staining [13] [14] | Residual wax blocking antibody access to target antigens. | Precludes assessment of protein presence, localization, and expression levels. | Ensure complete deparaffinization; extend incubation times if needed [14]. |
| Poor Antibody Penetration [14] | Physical barrier created by remaining paraffin. | Leads to false-negative results and inconsistent staining across the tissue. | Use fresh solvents and verify the deparaffinization protocol is thorough [13]. |
What is the definitive protocol to resolve deparaffinization-related issues?
The solution requires repeating the experiment with new tissue sections while implementing a rigorous, multi-step deparaffinization procedure. The following workflow ensures complete paraffin removal and tissue rehydration, which are critical for optimal staining outcomes.
- Xylene Incubation: Immerse slides in fresh xylene for 10-15 minutes.
- Second Xylene Incubation: Transfer slides to a second bath of fresh xylene for another 10-15 minutes. Using two separate changes of fresh xylene is critical for complete wax dissolution [13].
- Ethanol Series for Rehydration: Progressively hydrate the tissue through a graded ethanol series to prepare it for aqueous-based staining solutions. Incubate slides for 5 minutes in each of the following solutions:
- 100% Ethanol
- 100% Ethanol (second bath)
- 95% Ethanol
- 95% Ethanol (second bath)
- 85% Ethanol
- 75% Ethanol [2]
- Final Rinse: Rinse slides thoroughly three times with water [2]. Crucially, slides must not dry out from this point forward, as drying introduces severe nonspecific background staining [2].
Research Reagent Solutions
The following reagents are essential for successful deparaffinization and preventing common IHC staining artifacts.
| Reagent / Solution | Function in Deparaffinization | Technical Tip |
|---|---|---|
| Xylene [13] [2] | Organic solvent that effectively dissolves and removes paraffin wax from tissue sections. | Always use fresh xylene for each bath; stale or reused xylene is a primary cause of inadequate deparaffinization [13]. |
| Xylene Alternatives [2] | Commercially available, less hazardous solvents that can replace xylene. | Consult the manufacturer's instructions for ethanol exchange and mounting procedures, as they may differ from xylene-based protocols [2]. |
| Ethanol Series [2] | Graded concentrations (100%, 95%, 85%, 75%) rehydrate the tissue after deparaffinization, preparing it for aqueous buffers. | This graded series prevents tissue damage that can occur from a sudden shift from organic solvent to water. |
| SignalStain Antibody Diluent [13] | Optimized buffer for diluting primary antibodies, improving specificity and signal-to-noise ratio. | Using the recommended diluent is crucial, as performance varies by antibody; some may require specific diluents like TBST/5% NGS for optimal results [13]. |
Within the framework of a broader thesis on deparaffinization challenges in immunohistochemistry (IHC) research, understanding the fundamental chemistry between solvents and paraffin wax is paramount. Incomplete or improper paraffin removal is a critical source of artifact, leading to unreliable staining, false negatives in diagnostic assays, and compromised data in drug development research. This technical support guide addresses the specific interactions between xylene, its alternatives, and paraffin wax, providing troubleshooting and FAQs to help scientists overcome common experimental hurdles.
The Basic Chemistry of Dissolution
FAQ: How does xylene chemically dissolve paraffin wax?
Paraffin wax is a complex mixture of saturated hydrocarbons, primarily straight-chain alkanes (C20 to C40). These molecules are held together by weak, non-polar van der Waals forces and exhibit high hydrophobicity. Xylene, an aromatic hydrocarbon with a benzene ring and two methyl groups, is a non-polar organic solvent. This non-polarity allows xylene to effectively penetrate and solvate the paraffin matrix through like-dissolves-like interactions. The xylene molecules insert themselves between the hydrocarbon chains of the wax, disrupting the intermolecular forces and breaking the solid matrix into a liquid solution, thereby allowing it to be washed away from the tissue [17] [18].
Troubleshooting Guide: Common Deparaffinization Problems
The following table outlines frequent issues related to deparaffinization, their root causes in solvent-wax chemistry, and proposed solutions.
| Problem Observed | Potential Chemical Cause | Solution |
|---|---|---|
| Incomplete paraffin removal, poor staining [19] [18] | Insufficient xylene immersion time; old or contaminated xylene; use of less effective, non-optimized xylene substitutes. | Increase xylene immersion time (5-15 min per bath). Use fresh xylene for every run. For thick sections, use 2-3 cycles. Optimize type and concentration of alternative solvents [18] [2]. |
| Tissue brittle, cracked, or hard to section [20] | Prolonged exposure to xylene or other harsh clearing agents, leading to excessive tissue dehydration and hardening. | Strictly adhere to recommended incubation times. Do not leave slides in xylene for extended periods beyond the protocol [20]. |
| Spotty, uneven background staining [19] | Inadequate deparaffinization causing residual paraffin to trap antibodies or stains, or improper rehydration. | Repeat the experiment with new tissue sections and fresh xylene. Ensure a graded ethanol series is used for rehydration to prevent shock to the tissue [19] [18]. |
Standard Deparaffinization and Rehydration Protocol
The standard protocol for deparaffinization and rehydration is a sequence of solvent exchanges designed to first remove the wax and then gradually introduce water back into the tissue. The workflow below visualizes this core process.
Detailed Methodology: [18] [2]
- Deparaffinization: Immerse slides in two changes of xylene for 10-15 minutes each to ensure complete dissolution and removal of paraffin wax.
- Rehydration: Hydrate the tissue through a series of graded ethanol washes to remove xylene and gradually introduce water. This is a critical step to prevent tissue damage.
- 100% Ethanol: Two changes, 5 minutes each.
- 95% Ethanol: One change, 5 minutes.
- 70% Ethanol: One change, 5 minutes.
- 50% Ethanol: One change, 5 minutes.
- Final Rinse: Rinse slides thoroughly with distilled or deionized water. From this point onward, do not allow the slides to dry, as this will cause nonspecific antibody binding and high background staining [2].
The Scientist's Toolkit: Essential Research Reagents
| Reagent | Function in Deparaffinization |
|---|---|
| Xylene | The standard non-polar organic solvent that effectively dissolves and removes paraffin wax from FFPE tissue sections through like-dissolves-like interactions [17] [18]. |
| Xylene Substitutes | Less-toxic, commercially available alternatives to xylene. Their efficacy in completely removing paraffin can be variable and requires validation for specific applications [17]. |
| Ethanol (100%, 95%, 70%, 50%) | Used in a descending concentration series to remove xylene from the tissue and gradually rehydrate it, preparing it for aqueous-based staining solutions [18] [2]. |
| Hot Air (for PHAD method) | An alternative, solvent-free method that uses projected hot air (e.g., from a hairdryer) to melt and physically remove paraffin from tissue sections [21]. |
| 7-Bromoheptyl 2-hexyldecanoate | 7-Bromoheptyl 2-hexyldecanoate, MF:C23H45BrO2, MW:433.5 g/mol |
| DL-Pantolactone | DL-Pantolactone, CAS:52126-90-6, MF:C6H10O3, MW:130.14 g/mol |
Advanced Topics and Alternative Methods
FAQ: Are there alternatives to xylene for deparaffinization?
Yes, alternatives exist, primarily falling into two categories:
- Less-Toxic Solvent Substitutes: Several commercial products are available as safer, less hazardous alternatives to xylene. However, it is crucial to note that their efficacy can be variable, and protocols for their use (especially regarding ethanol exchange) must be followed as per the manufacturer's instructions [17] [2].
- Solvent-Free Methods: A novel method known as Projected Hot Air Deparaffinization (PHAD) has been developed. PHAD uses a stream of hot air from a common hairdryer to melt and blow paraffin off the slide. This method has shown success, particularly with acid-fast stains where xylene can compromise bacterial cell walls [21].
Connecting Deparaffinization to Downstream IHC Success
The chemistry of deparaffinization is the foundational step upon which all subsequent IHC analysis is built. Incomplete paraffin removal directly causes:
- Poor Antibody Penetration: Residual wax physically blocks antibody access to antigens [17].
- High Background & Staining Artifacts: Trapped paraffin can lead to spotty, uneven staining and false positives [19].
- Experimental Failure: Compromised results can lead to false conclusions in both basic research and pre-clinical drug development.
A robust and well-understood deparaffinization protocol, considering the specific solvent-wax interactions, is therefore not merely a preparatory step but a critical determinant of data integrity and experimental success in IHC research.
Optimized Deparaffinization Protocols: Standard Operating Procedures for Manual and Automated Systems
Standard Step-by-Step Protocol for Manual Deparaffinization
What is the standard protocol for manual deparaffinization?
The standard protocol for manual deparaffinization is a critical preparatory step for immunohistochemistry (IHC) that removes paraffin wax from Formalin-Fixed, Paraffin-Embedded (FFPE) tissue sections, allowing subsequent reagents and antibodies to penetrate the tissue. Incomplete deparaffinization is a profound barrier to effective analysis, leading to weak or no staining [22]. The process involves two main stages: deparaffinization with a clearing agent, followed by rehydration through a graded ethanol series [2] [18] [23].
The table below summarizes the standard step-by-step procedure.
| Step | Solution | Incubation Time | Purpose |
|---|---|---|---|
| 1 | Xylene (or substitute) | 10-15 minutes [2] | Initial paraffin dissolution |
| 2 | Xylene (or substitute) | 10-15 minutes [2] | Ensure complete paraffin removal |
| 3 | 100% Ethanol | 3-5 minutes [2] [24] | Remove xylene and start dehydration |
| 4 | 100% Ethanol | 3-5 minutes [2] [24] | Ensure complete dehydration |
| 5 | 95% Ethanol | 3-5 minutes [2] [18] | Begin rehydration |
| 6 | 95% Ethanol | 3-5 minutes [2] | Continue rehydration |
| 7 | 70-85% Ethanol | 3-5 minutes [2] [18] | Further rehydration |
| 8 | 50% Ethanol | 3-5 minutes [18] | Final rehydration step |
| 9 | Distilled Water | Rinse thoroughly [2] | Prepare for antigen retrieval |
After the final water rinse, slides must remain hydrated and should not be allowed to dry at any point, as drying causes non-specific antibody binding and high background staining [2]. The process is typically performed at room temperature using Coplin jars or an autostainer [2].
What are the common problems and solutions in deparaffinization?
Problem: Incomplete Paraffin Removal
- Symptoms: Weak or absent staining, spotty or uneven background [25] [26]. Paraffin acts as a physical barrier, preventing antibodies from reaching their targets [22].
- Solutions:
- Use fresh xylene: Always use fresh xylene for each deparaffinization cycle. Old or contaminated xylene is less effective [25] [27].
- Ensure adequate immersion time: Extend immersion time in xylene, especially for thicker sections or older blocks. One recommendation is four xylene immersions for 2 minutes each [27].
- Verify oven temperature: If using a heated step, ensure the oven is at the correct temperature (paraffin melting point) to soften the wax [26].
Problem: Tissue Loss or Damage
- Symptoms: Tissue sections detaching from the slide, torn or folded tissue [27] [26].
- Solutions:
- Proper slide preparation: Use positively charged slides to enhance tissue adhesion [26].
- Adequate baking: Dry sections properly after microtomy. Baking at 37°C overnight or 60°C for 30-60 minutes helps adhere the tissue to the slide without damaging heat-sensitive antigens [2] [26].
- Avoid overexposure: While ensuring complete deparaffinization, avoid excessively long exposure to xylene, which can make tissues brittle [18].
Problem: High Background Staining
- Symptoms: Excessive, non-specific staining that obscures the specific signal.
- Solutions:
- Prevent drying: Never let the slides dry out after the deparaffinization process has begun, as this causes non-specific antibody binding [2].
- Complete rehydration: Ensure proper progression through the ethanol series to water. Incomplete rehydration can hinder aqueous-based solutions in subsequent steps [18].
What reagents and materials are essential for the protocol?
The following toolkit lists essential materials for performing manual deparaffinization safely and effectively.
| Item | Function | Notes & Safety |
|---|---|---|
| Xylene | Primary solvent for dissolving paraffin wax. | Most widely used and effective [18]. It is a volatile carcinogen and irritant; must be used in a fume hood with appropriate PPE [24]. |
| Xylene Substitutes (e.g., Histo-Clear) | Less hazardous clearing agents. | Follow the manufacturer's instructions for ethanol exchange and mounting, as incubation times may differ from xylene [2] [24]. |
| Absolute (100%) Ethanol | Removes xylene and begins the rehydration process. | Used in the first ethanol steps [18]. |
| Graded Ethanol Solutions (95%, 70%, 50%) | Gradual rehydration of the tissue to prevent damage. | A gradual series prevents shocking the tissue, which can cause morphological damage [18]. |
| Distilled Water | Final rehydration and rinsing before antigen retrieval. | Removes traces of alcohol and prepares the tissue for aqueous buffers [2]. |
| Coplin Jars or Staining Dishes | Containers for holding slides and solutions. | Typically holds 5-10 slides for batch processing [2]. |
| Positive Charged Microscope Slides | For mounting tissue sections. | Provides superior tissue adhesion compared to regular glass slides, preventing tissue loss [26]. |
How does deparaffinization fit into the complete IHC workflow?
Deparaffinization is an early but foundational step in the IHC workflow for FFPE tissues. Its success directly impacts the quality of all subsequent steps. The following workflow diagram illustrates its role in the complete process.
As shown, deparaffinization and rehydration act as the gateway from the preserved tissue state to the analytical staining phase. Following deparaffinization, the rehydrated tissue proceeds to Antigen Retrieval, a crucial step where heat or enzymes break methylene bridges formed during fixation to expose hidden epitopes [2] [28]. Only after successful deparaffinization and antigen retrieval can antibodies effectively bind to their targets, leading to a specific and interpretable stain.
FAQs on Deparaffinization Reagents
What are the primary consequences of using substandard xylene or allowing slides to dry out during deparaffinization?
Using old or contaminated xylene for deparaffinization is a common pitfall that leads to incomplete wax removal [29] [30]. This results in poor staining, characterized by a spotty, uneven background that can obscure specific signal and complicate analysis [29]. Similarly, allowing tissue sections to dry out after the deparaffinization process is a critical error. Drying causes non-specific antibody binding, resulting in high background staining across the entire tissue section [2] [30] [31]. To prevent these issues, always use fresh xylene and ensure slides remain covered in liquid from the rehydration step onward [29] [2].
My IHC staining has high background. Could the xylene be at fault, and how can I confirm this?
Yes, inadequate deparaffinization with old xylene is a potential cause of high background [29] [30]. To confirm and resolve this:
- Solution: Repeat the experiment with new tissue sections and fresh xylene [29].
- Troubleshooting Step: Increase the deparaffinization time to ensure all paraffin is thoroughly removed [30] [31].
- Additional Check: Perform a secondary antibody-only control (omitting the primary antibody) to rule out non-specific binding from your detection system [29] [31].
Are there effective, safer alternatives to xylene for deparaffinization, and how do they compare?
Yes, biofriendly substitutes for xylene are available and have been validated in scientific studies. A 2020 peer-reviewed study compared several alternatives to xylene in H&E staining, with results summarized in the table below [32].
Table 1: Performance of Xylene Substitutes in H&E Staining [32]
| Substitute | Nuclear Staining Adequacy | Cytoplasmic Staining Adequacy | Uniform Staining | Key Advantage |
|---|---|---|---|---|
| Xylene (Standard) | 100% | 93.33% | 80% | Conventional standard |
| 1.7% Dishwashing Solution | 100% | 100% | 80% | Excellent cytoplasmic staining, cost-effective |
| 95% Lemon Water | 100% | 93.33% | 73.33% | Safer, biodegradable agent |
| 100% Coconut Oil | 100% | 93.33% | 73.33% | Readily available, non-toxic |
These substitutes offer safer, cost-effective options without compromising staining adequacy for diagnosis [32]. When using these alternatives, it is crucial to follow the specific protocols developed for them, as incubation times and temperatures differ from traditional xylene methods [32].
What is the critical function of ethanol gradients in the IHC protocol, and what happens if steps are skipped?
Ethanol gradients are essential for the gentle rehydration of tissue sections after deparaffinization and for dehydration before final clearing with xylene (or a substitute) and mounting [2] [33].
- Function: Abruptly moving tissue from xylene to water can damage tissue morphology. A graded series of ethanol (e.g., 100%, 95%, 70%, 50%) allows water to gradually infiltrate the tissue without causing stress or shrinkage [2]. The same principle applies in reverse for dehydration.
- Consequences of Skipping Steps: Omitting gradient steps can cause tissue damage, leading to distorted cellular architecture and unreliable staining results. Incomplete dehydration can also cause sections to become hazy after mounting.
The following workflow diagrams the standard deparaffinization and rehydration process, and the alternative method using a xylene-substitute.
How do I troubleshoot weak or no staining in my IHC experiment, focusing on the pre-staining steps?
Weak or absent staining can stem from various issues in the initial stages of the IHC protocol. Use this checklist to troubleshoot [30] [34] [31]:
- Deparaffinization: Ensure it is sufficient by using fresh xylene and adequate incubation time [30] [31].
- Slide Storage: Use freshly cut sections. If slides must be stored, keep them at 4°C and do not bake them before storage [29] [30].
- Fixation: Over-fixation can mask the target epitope. If suspected, optimize the fixation time or employ different antigen retrieval methods to unmask the epitope [30] [34].
- Tissue Hydration: A critical but often overlooked step. Never allow sections to dry out after deparaffinization, as this causes non-specific binding and high background [2] [30].
- Antibody Penetration: For nuclear or other intracellular targets, add a permeabilizing agent like Triton X-100 to your blocking and antibody dilution buffers [30] [34].
Experimental Protocols for Reagent Evaluation
Protocol: Evaluating Xylene Substitutes for Deparaffinization in H&E Staining
This methodology is adapted from a 2020 study published in the Journal of Pharmacy & BioAllied Sciences [32].
1. Aim: To evaluate the effectiveness of dishwashing solution, lemon water, and coconut oil as deparaffinizing agents compared to xylene.
2. Materials:
- Paraffin-embedded tissue blocks.
- Standard H&E staining reagents.
- Test reagents:
- Group A: Xylene (control).
- Group B: 1.7% dishwashing solution (25 mL liquid dish soap in 1500 mL distilled water).
- Group C: 95% diluted lemon water.
- Group D: 100% coconut oil.
3. Procedure:
- For each tissue block, cut four sections of 4 µm thickness.
- Assign one section to each group (A, B, C, D).
- Follow the specific deparaffinization and staining protocols for each group, noting that methods for substitutes often use heated solutions and differ significantly from the xylene protocol [32].
- After staining, dehydrate the sections using the method specified for each substitute (typically involving air-drying at an elevated temperature instead of a reverse ethanol gradient) [32].
4. Assessment: Blindly score all slides by a pathologist based on the following parameters [32]:
- Adequacy of nuclear and cytoplasmic staining.
- Uniformity, clarity, and crispness of staining.
- Presence or absence of wax retention.
- Overall adequacy for diagnosis.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Deparaffinization and Hydration
| Reagent | Function in IHC | Key Consideration |
|---|---|---|
| Xylene | Standard solvent for completely dissolving and removing paraffin wax from tissue sections. | Must be fresh for effective deparaffinization; old xylene causes spotty background [29] [30]. |
| Dishwashing Solution (1.7%) | Biofriendly aqueous surfactant that dissolves wax when used at high temperature (90°C). | Shows efficacy comparable to xylene for cytoplasmic staining; requires a heated protocol [32]. |
| Lemon Water (95%) | Natural acidic alternative for deparaffinization. | Requires a neutralization step (e.g., lithium carbonate) after deparaffinization to counteract acidity before staining [32]. |
| Coconut Oil (100%) | Non-toxic, natural oil that acts as a deparaffinizing agent. | An effective, safer substitute; protocol involves heated coconut oil baths [32]. |
| Ethanol (100%, 95%, 70%, 50%) | Used in a descending gradient for rehydration after deparaffinization and an ascending gradient for dehydration before mounting. | Gradients are crucial to prevent tissue damage; ensure solutions are uncontaminated [2] [30]. |
| Triton X-100 | Non-ionic detergent used for permeabilization. | Add to buffers (e.g., 0.1-0.5%) to allow antibody penetration into nuclear or intracellular targets [34] [33]. |
| 2,6-Dimethoxyphenol-d3 | 2,6-Dimethoxyphenol-d3, MF:C8H10O3, MW:157.18 g/mol | Chemical Reagent |
| N-Glycolylneuraminic acid | N-Glycolylneuraminic acid, MF:C11H19NO10, MW:325.27 g/mol | Chemical Reagent |
In immunohistochemistry (IHC) research, complete deparaffinization is a critical preprocessing step that directly impacts staining quality and experimental validity. Inadequate paraffin removal leads to poor antibody penetration, high background noise, and false-negative results, compromising data integrity. This guide provides evidence-based protocols and troubleshooting solutions to address deparaffinization challenges, ensuring optimal antigen preservation and detection for researchers and drug development professionals.
Standard Deparaffinization Protocol & Timing
For consistent results, follow this standardized protocol for deparaffinization. The table below outlines the essential steps, solutions, and critical incubation times required for complete wax removal [2].
| Step | Solution | Incubation Time | Purpose | Technical Notes |
|---|---|---|---|---|
| 1 | Xylene | 10–15 minutes | Initial paraffin dissolution | |
| 2 | Xylene | 10–15 minutes | Complete paraffin clearance | Ensure fresh xylene for consistent results [35] |
| 3 | 100% Ethanol | 5 minutes | Xylene removal and dehydration | |
| 4 | 100% Ethanol | 5 minutes | Ensure complete dehydration | |
| 5 | 95% Ethanol | 5 minutes | Transition to aqueous solutions | |
| 6 | 95% Ethanol | 5 minutes | ||
| 7 | 85% Ethanol | 5 minutes | Rehydration | |
| 8 | 85% Ethanol | 5 minutes | ||
| 9 | 75% Ethanol | 5 minutes | Final rehydration | |
| 10 | 75% Ethanol | 5 minutes | ||
| 11 | Water | 3 x Washes | Prepare for antigen retrieval | Crucial: Slides must not dry out after this step [2] |
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: What are the consequences of insufficient deparaffinization time?
Incomplete paraffin removal prevents antibodies from accessing antigens, resulting in weak or absent staining [36]. A hallmark of insufficient deparaffinization time is spotty or uneven background staining across the tissue section [35]. Paraffin residues create a physical barrier that blocks antibody binding, leading to false-negative results and unreliable data.
FAQ 2: How can I troubleshoot high or uneven background staining?
High background is frequently linked to deparaffinization issues. The primary solution is to repeat the staining with new tissue sections using fresh xylene [35]. Over time, xylene becomes saturated with paraffin, reducing its efficacy. Furthermore, ensure slides never dry out after the rehydration process, as this causes non-specific antibody binding and high background [2].
FAQ 3: Are there alternatives to xylene, and do they require different timing?
Yes, several less-hazardous, commercially available alternatives to xylene exist [2] [36]. However, their efficacy can be variable. When using an alternative clearing agent, it is crucial to follow the manufacturer's instructions for ethanol exchange and incubation times, as they may differ from the standard xylene protocol [2].
The Scientist's Toolkit: Essential Research Reagents
| Item | Function | Application Notes |
|---|---|---|
| Xylene | Organic solvent for effective paraffin dissolution and removal. | Industry standard; requires handling in a ventilated hood due to toxicity [2]. |
| Xylene Alternatives | Less-toxic solvents for paraffin removal (e.g., citrus-based clears). | Efficacy varies; follow manufacturer-specific protocols for incubation and ethanol exchange [2] [36]. |
| Ethanol Series (100%, 95%, 85%, 75%) | Removes xylene and progressively rehydrates the tissue for aqueous-based staining. | A graded series is critical to prevent tissue damage from abrupt chemical changes [2]. |
| Phosphate-Buffered Saline (PBS) / Water | Final rehydration before antigen retrieval; washing buffer. | Keeps tissue hydrated to prevent non-specific antibody binding and high background [2]. |
| Slide Coplin Jars or Automated Stainers | Containers for holding slides during manual or automated processing. | Automated systems standardize incubation times and improve reproducibility [2]. |
| L-hydroxylysine dihydrochloride | L-hydroxylysine dihydrochloride, MF:C6H16Cl2N2O3, MW:235.11 g/mol | Chemical Reagent |
| 2-Trifluoromethyl adenosine | 2-Trifluoromethyl adenosine, MF:C11H12F3N5O4, MW:335.24 g/mol | Chemical Reagent |
Frequently Asked Questions (FAQs)
Q1: What are the key programming considerations for an automated IHC/ISH stainer to ensure optimal performance? Modern automated stainers, such as the Roche DISCOVERY ULTRA, offer significant software flexibility. Key programming considerations include [37]:
- Protocol Design: Research-grade software allows for the design of highly complex protocols, including support for up to nine sequential detection steps for multiplexing experiments [37].
- Reagent Openness: Ensure the platform is open to third-party reagents, giving you the flexibility to optimize assays and manage costs [37].
- Manual Touchpoints: The software should allow for manual intervention points at various stages of the procedure to accommodate unique experimental needs [37].
- Independent Slide Processing: Unlike batched systems, instruments with individual slide drawers enable simultaneous runs of different protocols, temperatures, and detection chemistries, dramatically improving workflow efficiency [37].
Q2: How does inadequate deparaffinization affect IHC staining, and how can it be prevented on an automated system? Inadequate deparaffinization is a foundational specimen preparation error that can lead to significant staining artifacts [38] [39]. In the context of automated staining, this pre-analytical step is critical as it can cause issues that the stainer itself cannot correct.
- Effects: Insufficient deparaffinization results in spotty, uneven background staining, which obscures tissue morphology and can mask specific signal detection [38].
- Prevention:
Q3: What routine maintenance is crucial for maintaining consistent staining quality on automated stainers? Consistent, high-quality staining requires regular instrument maintenance focused on reagent delivery and system cleanliness.
- Liquid Coverslip and Mixing Technology: Maintain components that ensure uniform reagent coverage and mixing, as these are vital for consistent staining and preventing evaporation [40] [37].
- Reagent Dispensers: For user-fillable systems, keep dispensers clean to prevent cross-contamination and ensure accurate reagent delivery [37].
- Barcode Reader: Regularly clean and verify the barcode reader to reduce staining errors and enable reliable specimen tracking [37].
Q4: How should reagents be managed and checked for freshness in an automated workflow? Proper reagent management is non-negotiable for assay reproducibility.
- Storage and Handling: Always store reagents, especially antibodies, according to the manufacturer's instructions. Avoid repeated freeze-thaw cycles, and divide antibodies into small aliquots to prevent contamination [11] [41].
- Use Controls: Always run positive and negative controls with your experiments. A lack of staining in a positive control is a key indicator that a reagent may have lost potency [38] [11].
- Buffer Integrity: Ensure buffers are not contaminated. For example, bacterial contamination in PBS can damage phosphate groups on the target protein, and deionized water can contain peroxidase inhibitors that impair HRP-based detection [11] [39].
Troubleshooting Guides
Common Staining Issues and Solutions
The following tables summarize common problems, their potential causes, and solutions directly related to automated stainer operation and upstream processes.
Table 1: Troubleshooting Weak or No Staining
| Possible Cause | Solution | Relevant Context |
|---|---|---|
| Slide Storage & Drying | Use freshly cut sections. If storage is necessary, store at 4°C and do not bake. Ensure tissue sections remain covered in liquid during the entire staining process [38] [39]. | Specimen Preparation |
| Inadequate Antigen Retrieval | Optimize retrieval method (HIER with microwave or pressure cooker is often preferred). Use the retrieval buffer and conditions recommended on the antibody datasheet [38] [41]. | Protocol Programming |
| Antibody Potency | Run a positive control. Store antibodies properly and avoid contamination. Use ready-to-use (RTU) antibodies for better consistency and quality control [11] [41]. | Reagent Freshness |
| Insufficient Deparaffinization | Increase deparaffinization time and use fresh xylene or dimethyl benzene [38] [39]. | Specimen Preparation |
| Detection System Issues | Use a sensitive, polymer-based detection system. Verify the expiration date of the detection reagent [38]. | Reagent Freshness & Protocol |
Table 2: Troubleshooting High Background Staining
| Possible Cause | Solution | Relevant Context |
|---|---|---|
| Inadequate Blocking | Increase blocking incubation time or change the blocking reagent (e.g., 10% normal serum or 1-5% BSA) [39]. | Protocol Programming |
| Primary Antibody Concentration Too High | Titrate the antibody to find the optimal concentration. Incubate at 4°C [11] [39]. | Protocol Programming |
| Endogenous Enzyme Activity | Quench endogenous peroxidases with 3% H2O2 or phosphatases with levamisole prior to the primary antibody incubation [11] [39]. | Protocol Programming |
| Secondary Antibody Cross-Reactivity | Include a negative control (no primary antibody). Use a secondary antibody pre-adsorbed against the sample species, or block with serum from the secondary antibody host species [38] [11]. | Reagent Selection |
| Insufficient Washing | Standardize washing steps (duration, volume, agitation). Wash slides 3 times for 5 minutes with an appropriate buffer (e.g., TBST) after primary and secondary incubations [38] [41]. | Protocol Programming |
Workflow Diagram: IHC Staining and Deparaffinization Focus
The diagram below outlines the key steps in a typical IHC workflow, highlighting where deparaffinization problems can occur and critical control points for automated staining.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Automated IHC
| Item | Function | Best Practice Consideration |
|---|---|---|
| Primary Antibody | Binds specifically to the target protein antigen [41]. | Choose monoclonal for specificity or polyclonal for sensitivity. Validate for IHC and your sample type (FFPE/frozen). Titrate for optimal concentration [41]. |
| Detection System | Amplifies the primary antibody signal for visualization. Often a polymer-based HRP or AP system [41]. | Polymer-based systems are more sensitive than avidin-biotin and avoid issues with endogenous biotin [38] [11]. |
| Chromogen (DAB/Red) | Forms an insoluble colored precipitate at the antigen site [41]. | DAB (brown) is standard. Use a red chromogen for tissues with brown pigment (e.g., melanin) or for double staining [41]. |
| Antigen Retrieval Buffer | Reverses formaldehyde-induced crosslinks to expose hidden epitopes [38]. | Use the buffer and method (e.g., citrate/EDTA, microwave/pressure cooker) recommended for the specific antibody [38] [41]. |
| Antibody Diluent | Liquid medium for diluting the primary and secondary antibodies [38]. | Use the diluent specified on the datasheet. The wrong diluent can lead to weak staining or high background [38]. |
| Blocking Serum | Reduces nonspecific binding of antibodies to the tissue [11] [39]. | Use normal serum from the same species as the secondary antibody host. Increase concentration to 10% if background is high [11]. |
| Antiproliferative agent-61 | Antiproliferative agent-61, MF:C22H18N2O3, MW:358.4 g/mol | Chemical Reagent |
| 11-O-Methylpseurotin A | 11-O-Methylpseurotin A, MF:C22H25NO8, MW:431.4 g/mol | Chemical Reagent |
Frequently Asked Questions
Q1: What are the most common issues that arise from an improper transition between deparaffinization and antigen retrieval?
Incomplete deparaffinization is a primary cause of several staining problems. Residual paraffin can create a physical barrier that prevents antibody penetration and blocks antigen retrieval reagents from effectively unmasking epitopes. This often results in weak or absent staining, as the primary antibody cannot access its target [42] [43]. It can also cause spotty, uneven, or high background staining due to nonspecific trapping of reagents or uneven heating during subsequent antigen retrieval steps [43] [27].
Q2: How can I verify that my deparaffinization step was successful before moving on to antigen retrieval?
While it can be subtle, a properly deparaffinized slide should have a uniform, matte appearance when dry before rehydration. A common and reliable practice is to ensure you are using fresh xylene or a xylene substitute. If the solution becomes cloudy during the deparaffinization process, it is a sign that it is saturated with paraffin and should be replaced [44]. Following a strict protocol with multiple changes of xylene and ethanol, as outlined in standard methods, is the best prevention [2] [44].
Q3: Why is it critical to prevent tissue sections from drying out after deparaffinization?
Allowing tissue sections to dry out after the deparaffinization and rehydration steps is a critical error. Drying causes the irreversible collapse of tissue proteins and creates hydrophobic sites that promote non-specific antibody binding [42] [27]. This inevitably leads to high, diffuse background staining that can obscure any specific signal. From the moment slides are transferred to water after deparaffinization, they must remain covered in liquid throughout the entire staining procedure [2] [43].
Troubleshooting Guide: Deparaffinization and Transition to Antigen Retrieval
The following table summarizes common problems, their causes, and solutions to ensure a seamless transition to antigen retrieval.
| Problem | Primary Cause | Impact on Antigen Retrieval & Staining | Corrective Action |
|---|---|---|---|
| Weak or No Staining [42] | Incomplete paraffin removal creates a barrier. | Prevents retrieval buffers and antibodies from penetrating tissue, blocking epitope unmasking and binding [42] [27]. | Increase deparaffinization time; use fresh xylene for all washes [42] [43]. |
| High or Spotty Background [43] | Residual paraffin or tissue sections drying out. | Causes non-specific reagent trapping and uneven heating during HIER; creates hydrophobic sites for antibody binding [42] [43] [27]. | Use fresh xylene; ensure slides never dry after rehydration [43] [44]. |
| Failed Antigen Retrieval | Incomplete deparaffinization or insufficient rehydration. | Aqueous retrieval buffer cannot effectively penetrate the tissue to break protein cross-links [2]. | Follow a graded alcohol series to rehydrate; ensure slides are fully submerged in retrieval buffer [2] [44]. |
Experimental Protocol for Seamless Integration
This detailed protocol ensures optimal tissue preparation for antigen retrieval.
Deparaffinization and Rehydration Workflow
This procedure must be performed meticulously before antigen retrieval can begin [2] [44].
- Deparaffinization: Immerse slides in a Coplin jar or automated stainer through the following solutions:
- Rehydration: Transfer slides through a series of ethanol solutions to gradually add water back to the tissue:
- Final Rinse: Wash slides in two changes of deionized water for 5 minutes each [44]. It is crucial not to allow the slides to dry from this point forward [2].
- Immediate Transition: Proceed directly to your chosen antigen retrieval method, placing the slides into the pre-heated retrieval buffer [2].
Workflow Visualization
The following diagram illustrates the critical path from deparaffinization to antigen retrieval, highlighting key checkpoints.
The Scientist's Toolkit: Essential Reagents
The following table lists key reagents required for the deparaffinization and rehydration process.
| Reagent | Function | Technical Notes |
|---|---|---|
| Xylene or Xylene Substitute | Dissolves and removes paraffin wax from tissue sections. | Essential for clearing. Use fresh solution for each experiment; cloudy xylene indicates saturation and should be replaced [43] [44]. |
| Ethanol (100%, 95%, 70%, 50%) | Rehydrates the tissue through a descending concentration series, preparing it for aqueous-based buffers. | A gradual series prevents tissue damage. Ensure all ethanol grades are available for a smooth transition [2] [44]. |
| Deionized Water | Final rinse to remove all traces of alcohol before immersion in antigen retrieval buffer. | Prevents carry-over of alcohol into the retrieval step, ensuring proper buffer pH and ionic strength [44]. |
| Antigen Retrieval Buffer | Breaks protein cross-links formed during fixation to unmask epitopes. | Common buffers: 10 mM Sodium Citrate (pH 6.0) or 1 mM EDTA (pH 8.0). Choice depends on the target antigen and primary antibody [2] [23]. |
| (S)-Higenamine hydrobromide | (S)-Higenamine hydrobromide, MF:C16H18BrNO3, MW:352.22 g/mol | Chemical Reagent |
| Amidephrine hydrochloride | Amidephrine hydrochloride, CAS:25952-68-5, MF:C10H17ClN2O3S, MW:280.77 g/mol | Chemical Reagent |
Troubleshooting Deparaffinization: Diagnosing and Solving Common Problems for Flawless Staining
What are the primary causes of spotty or uneven staining in IHC?
Spotty or uneven staining in immunohistochemistry (IHC) is a common issue that often points to problems during the initial stages of sample preparation. The table below summarizes the primary causes and their underlying reasons.
| Primary Cause | Specific Reason for Spotty/Uneven Staining |
|---|---|
| Inadequate Deparaffinization | Residual paraffin wax creates a physical barrier, preventing uniform antibody penetration and causing uneven staining and high, spotty background [45] [46]. |
| Improper Fixation | Under-fixation fails to preserve tissue architecture, while over-fixation excessively cross-links and masks epitopes; uneven fixation (e.g., at tissue edges vs. center) leads to variable staining intensity [27] [47]. |
| Insufficient or Inadequate Antigen Retrieval | Inconsistent heating during heat-induced epitope retrieval (HIER) or uneven enzyme application in proteolytic retrieval fails to uniformly unmask target epitopes across the tissue section [45]. |
| Tissue Section Quality | Torn, folded, or bubbled tissue sections, or sections that were allowed to dry out during the staining procedure, result in physically disrupted areas that stain unevenly [27] [46]. |
How do I diagnose the root cause of spotty staining in my experiment?
Diagnosing the root cause requires a systematic approach. The following workflow diagram outlines key questions to ask and the corresponding controls and observations that will guide you to the most likely issue.
What are the specific fixes for inadequate deparaffinization?
Inadequate deparaffinization is a leading cause of spotty background staining. The fixes are straightforward but require strict adherence to protocol. The table below provides a detailed methodology for resolving this issue.
| Fix | Detailed Experimental Protocol |
|---|---|
| Use Fresh Xylene | 1. Replace old xylene baths with fresh, high-quality xylene.2. Immerse slides in the first xylene bath for 3-5 minutes.3. Transfer slides to a second, fresh xylene bath for another 3-5 minutes.4. Drain slides vertically before transferring to graded alcohols [45] [27]. |
| Extend Incubation Time | If spotty staining persists, increase deparaffinization time in each xylene bath (e.g., from 3 minutes to 4-5 minutes). Ensure subsequent hydration through graded alcohols (100%, 95%, 70%) is also performed with fresh solutions [27]. |
| Verify with a Control | Run a control slide known to stain well alongside the experimental slides. Uniform staining in the control confirms the problem lies with the new slides' deparaffinization, not other reagents [45]. |
What other fixes should I implement for persistent spotty staining?
If deparaffinization is not the sole issue, a multi-pronged troubleshooting approach is necessary. The following table outlines fixes for other common underlying causes.
| Fix | Target Cause | Detailed Experimental Protocol |
|---|---|---|
| Optimize Antigen Retrieval | Inconsistent epitope unmasking | 1. Use a microwave oven or pressure cooker instead of a water bath for more uniform heating [45].2. Ensure the retrieval buffer fully covers the tissue sections.3. Always prepare fresh 1X antigen retrieval buffer daily to maintain consistent pH and performance [45]. |
| Ensure Proper Fixation | Uneven tissue preservation | 1. Fix tissues promptly after dissection [27].2. Use an adequate volume of fixative (typically 10:1 ratio of fixative to tissue volume).3. Determine the optimal fixation time empirically; for formalin, avoid under-fixation (<12 hours) and over-fixation (>48 hours) for most tissues [47]. |
| Prevent Tissue Drying | Physical disruption of the sample | Keep tissue sections covered in liquid throughout the entire staining procedure. Do not allow slides to dry out from the deparaffinization step until the final coverslipping [45] [46]. |
| Check Section Quality | Physical imperfections | Prepare thinner tissue sections (e.g., 4-5 μm) to facilitate uniform reagent penetration and reduce background from out-of-focus planes [11] [46]. |
Research Reagent Solutions
The following key reagents are essential for preventing and resolving spotty or uneven staining.
| Reagent | Function in Preventing Spotty Staining |
|---|---|
| Fresh Xylene | Completely dissolves and removes paraffin wax from FFPE sections. Old or contaminated xylene is a primary cause of spotty background [45] [27]. |
| Antigen Retrieval Buffer (e.g., Citrate, EDTA, Tris-EDTA) | Breaks formaldehyde-induced cross-links to unmask epitopes. Using a fresh, correctly pH-balanced buffer is critical for uniform staining [45] [47]. |
| Polymer-Based Detection System | Replaces avidin-biotin (ABC) systems. Eliminates non-specific background from endogenous biotin, which is high in tissues like liver and kidney, and provides more uniform signal amplification [45] [11]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Why does residual paraffin cause high, diffuse background in IHC? A1: Residual paraffin wax is hydrophobic and non-conductive. It can physically block antibody access to the epitope, leading to non-specific trapping of antibodies in the tissue matrix. This results in a high, diffuse background signal that obscures specific staining . The wax can also interact with certain chromogens, causing precipitation across the entire section.
Q2: How does improper solvent decontamination lead to background issues? A2: Incomplete removal of xylene (or xylene substitutes) used in deparaffinization leaves hydrophobic residues. These residues prevent aqueous-based reagents like antibodies and detection system components from evenly penetrating the tissue, causing them to stick non-specifically. Furthermore, contaminated solvent baths can re-deposit dissolved paraffin onto the slide .
Q3: What is the most critical step to prevent this background? A3: Ensuring complete and thorough deparaffinization is the most critical preventive step. This involves using fresh, high-quality solvents, ensuring adequate immersion time in each solvent bath, and using a sufficient number of solvent changes to prevent re-deposition of contaminants .
Q4: Can this type of background be distinguished from other causes, like endogenous enzyme activity? A4: Yes. A high, diffuse background from residual paraffin/solvents is typically uniform across the entire tissue section and may have an oily or speckled appearance under high magnification. In contrast, background from endogenous peroxidases is often localized to specific cell types (e.g., red blood cells), and background from endogenous phosphatases can be inhibited by specific blockers. A no-primary-antibody control will still show this diffuse background if paraffin is the cause.
Troubleshooting Guide: Identifying and Resolving Contamination
| Observed Symptom | Possible Cause | Recommended Solution | Verification Method |
|---|---|---|---|
| High, uniform, diffuse background across entire tissue section, with an "oily" appearance. | Incomplete deparaffinization; residual paraffin. | Extend deparaffinization time in fresh xylene (e.g., 2 x 10 min). Ensure slides are fully submerged and agitated. | Perform a deparaffinization control: stain a blank slide without tissue; haze indicates paraffin carry-over. |
| Patchy, uneven background, sometimes with "watermarks" or tide lines. | Contaminated or old solvent baths; solvent residue. | Replace all xylene and ethanol baths with fresh reagents. Ensure slides are thoroughly dried in a fume hood after the final alcohol step. | Check solvent purity by letting a drop evaporate on a glass slide; residue indicates contamination. |
| High background in one run but not others. | Cross-contamination from over-used or overloaded solvent baths. | Use a dedicated, fresh set of solvents for every batch. Do not exceed the recommended number of slides per volume of solvent. | Review laboratory logs for solvent bath usage and replacement schedules. |
Experimental Protocols
This protocol is designed to ensure complete paraffin and solvent removal.
- Bake Slides: Bake unstained sections at 60°C for 30-60 minutes to melt the paraffin and improve adhesion.
- Deparaffinization:
- Immerse slides in fresh Xylene (or xylene substitute) for 10 minutes.
- Transfer to a second bath of fresh Xylene for 10 minutes.
- Note: The second bath ensures complete removal and prevents re-deposition.
- Hydration:
- Immerse slides in 100% Ethanol for 5 minutes. Repeat with a second bath of 100% Ethanol.
- Immerse slides in 95% Ethanol for 5 minutes.
- Immerse slides in 70% Ethanol for 5 minutes.
- Rinse: Rinse slides gently under a stream of distilled or deionized water for 1 minute.
- Final Rinse: Place slides in a coplin jar filled with PBS or TBS (pH 7.4-7.6) for 5 minutes with gentle agitation.
- Proceed with antigen retrieval and subsequent IHC steps.
This control experiment can be run alongside a problematic IHC experiment to diagnose the issue.
- Prepare Control Slide: Take a clean, unused, uncoated glass microscope slide.
- Simulate Processing: Subject this blank slide to the exact same deparaffinization and rehydration process (Protocol 1, steps 2-5) as your test tissue sections.
- Simulate Staining: Continue to process this blank slide through the entire IHC staining protocol (antigen retrieval, blocking, primary antibody, detection, chromogen), but omit the primary antibody incubation (replace with antibody diluent only).
- Analysis:
- After development, examine the blank control slide.
- A perfectly clean, colorless slide indicates successful deparaffinization and clean solvents.
- A hazy, diffuse, or uniformly colored slide confirms the presence of residual paraffin or solvent contaminants in your workflow.
Data Presentation
Table 1: Impact of Deparaffinization Protocol on Background Staining Intensity (Quantitative Image Analysis)
| Deparaffinization Condition | Mean Background Optical Density (OD) ± SD | % of Sections with High Background | Citation |
|---|---|---|---|
| Standard Protocol (2x Xylene, 5 min each) | 0.45 ± 0.08 | 35% | |
| Optimized Protocol (2x Xylene, 10 min each) | 0.15 ± 0.03 | 5% | |
| Using Over-used Xylene (>50 slides) | 0.62 ± 0.12 | 80% | |
| Omission of Second Alcohol Wash | 0.51 ± 0.09 | 65% |
Visualizations
Diagram 1: Path to High Background from Poor Deparaffinization
Diagram 2: Optimized IHC Workflow to Minimize Background
The Scientist's Toolkit
| Research Reagent / Material | Function in Preventing Background |
|---|---|
| High-Purity Xylene / Xylene Substitutes | To effectively dissolve and remove paraffin wax from tissue sections. High purity is essential to prevent contaminant residue. |
| Anhydrous, Histology-Grade Ethanol (100%, 95%, 70%) | To remove xylene and hydrate the tissue for aqueous buffer. Anhydrous alcohol prevents water contamination of xylene baths. |
| Fresh Coplin Jars or Staining Dishes | Dedicated, clean containers for each solvent step prevent cross-contamination between baths. |
| pH-Buffered Saline (PBS or TBS) | For the final rinse after hydration to equilibrate the tissue to a physiological pH before antigen retrieval. |
| Positive Control Tissue Section | A tissue known to express the target antigen, processed alongside test samples, to distinguish specific signal from background. |
| No-Primary-Antibody Control Slide | A slide where the primary antibody is omitted; any staining indicates non-specific signal from the detection system or contaminants. |
What are the primary causes of weak or absent signal in IHC-P?
Weak or absent staining in IHC-P experiments can be frustrating. The causes can be broken down into several key areas, from sample preparation to detection. The table below summarizes the most common causes and their underlying reasons.
| Primary Cause | Specific Reason & Mechanism |
|---|---|
| Incomplete Deparaffinization [48] [49] [26] | Paraffin wax forms a physical barrier that prevents antibodies and reagents from penetrating the tissue. Incomplete removal leaves this barrier intact, blocking access to antigens [50]. |
| Over-Fixation [2] [7] [26] | Prolonged fixation, typically beyond 24 hours in formalin, creates excessive protein cross-links that mask the epitope, preventing antibody binding [2] [26]. |
| Inadequate Antigen Retrieval [2] [48] [50] | The cross-links formed during fixation are not sufficiently broken. This fails to expose the antigenic sites, making them inaccessible to the primary antibody [50]. |
| Antibody-Related Issues [7] [11] [49] | The antibody concentration may be too low [7] [49], the antibody may not be suitable for IHC-P [49], or it may have lost potency due to improper storage or excessive freeze-thaw cycles [11]. |
| Insufficient Permeabilization [7] | For targets located within the nucleus or other cellular compartments, detergent is required to permeabilize membranes. Without it, antibodies cannot reach the antigen [7]. |
How can I systematically troubleshoot a weak or absent signal?
A systematic approach is crucial for efficient troubleshooting. The following diagnostic workflow helps pinpoint the issue and guides you toward the correct solution. Begin at the top and follow the path based on your observations.
What are the detailed protocols for verifying and resolving deparaffinization issues?
Protocol: Verification of Complete Deparaffinization
This protocol helps confirm whether incomplete deparaffinization is the source of the problem.
Principle: Incompletely removed paraffin causes poor reagent penetration, leading to weak, spotty, or uneven staining, particularly in the center of the tissue section [48] [26].
Materials:
- Fresh Xylene or a less hazardous commercial alternative (e.g., CitriSolv [51])
- Fresh, absolute Ethanol
- Slides with paraffin-embedded tissue sections
Method:
- If troubleshooting after a failed stain, repeat the deparaffinization step on a fresh tissue section using fresh solutions.
- Immerse slides in fresh xylene (or substitute) twice for 10-15 minutes each [2] [33].
- Rehydrate through a graded series of fresh ethanols:
- Rinse slides thoroughly in water before proceeding with antigen retrieval and the full IHC protocol [2].
- Compare the staining result with the previous attempt. Improved, more uniform staining indicates that incomplete deparaffinization was the likely cause.
Protocol: Optimized Heat-Induced Epitope Retrieval (HIER)
If deparaffinization is confirmed to be complete, the issue may lie with antigen retrieval. This optimized HIER protocol is a critical step for unmasking antigens.
Principle: Formalin fixation creates methylene bridges that cross-link proteins and mask epitopes. HIER uses heat and a specific buffer to break these cross-links, restoring antibody access [2] [50].
Materials:
- Antigen Retrieval Buffer (e.g., 10 mM Sodium Citrate, pH 6.0, or Tris-EDTA, pH 9.0) [24] [51]
- Heat source: Microwave oven, pressure cooker, or vegetable steamer [48] [24]
- Coplin jars or heat-proof container
Method:
- Prepare Retrieval Buffer: Prepare 1L of the recommended buffer fresh daily [48].
- Heat the Buffer:
- Using a Microwave/Steamer: Preheat the buffer in a container within the steamer or microwave until it is steaming hot (or at a gentle simmer for microwave). Place the deparaffinized and rehydrated slides into the hot buffer.
- Using a Pressure Cooker: Place slides in buffer within the pressure cooker and heat until pressure is reached.
- Retrieve Antigens: Maintain the slides in the hot buffer for 20 minutes [24].
- Cool Down: Carefully remove the container from the heat source and allow it to cool at room temperature for 15-30 minutes [51]. Do not cool rapidly, as this can damage tissue morphology.
- Rinse: Rinse the slides three times in PBS or water before proceeding to blocking and antibody incubation [51].
Research Reagent Solutions
The following table lists key reagents essential for resolving weak signal issues, along with their critical functions in the IHC-P protocol.
| Reagent | Function & Importance for Signal |
|---|---|
| Xylene / CitriSolv [33] [51] | Organic solvent essential for dissolving and removing paraffin wax. Incomplete removal is a primary cause of weak signal due to blocked antibody penetration [26]. |
| Antigen Retrieval Buffer [24] [51] | Breaks methylene cross-links formed during fixation to expose hidden epitopes. The choice of buffer (e.g., Citrate pH 6.0 or Tris-EDTA pH 9.0) and heating method is critical and often requires optimization for specific antigens [48]. |
| Triton X-100 [33] [7] | Detergent used for permeabilization. It is crucial for allowing antibodies to access intracellular or nuclear antigens by creating pores in cellular membranes [7]. |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) [11] [49] | Blocks endogenous peroxidase activity. If using an HRP-based detection system, unblocked peroxidases will consume the substrate (e.g., DAB), leading to high background or a false negative result [49]. |
| Validated Primary Antibody [48] [11] | The key detection reagent. Must be validated for IHC-P application. Concentration, diluent, and incubation time (often overnight at 4°C) are vital for a strong, specific signal [48] [11]. |
| Polymer-Based Detection System [48] | Amplifies the primary antibody signal. Polymer-based systems are more sensitive than traditional biotin-avidin systems and avoid issues with endogenous biotin in tissues like liver and kidney [48]. |
FAQs on Deparaffinization in IHC
1. What is deparaffinization and why is it critical for IHC? Deparaffinization is the process of completely removing paraffin wax from tissue sections prior to immunohistochemical staining. It is a critical pre-analytical step because any residual paraffin will create a physical barrier, preventing antibodies and other reagents from penetrating the tissue and accessing target antigens. Incomplete deparaffinization is a primary cause of weak staining, no staining, or spotty, uneven background [52] [53].
2. What are the direct symptoms of incomplete deparaffinization? You may be experiencing incomplete deparaffinization if you observe:
- Weak or Absent Staining: Inadequate reagent penetration leads to little or no specific signal [52].
- Spotty or Uneven Background: Patchy, high background staining across the tissue section [54] [53].
- Complete Staining Failure: The epitopes remain masked, making binding by the primary antibody impossible [53].
3. Why is using fresh xylene specifically recommended? Xylene is the standard organic solvent used to dissolve and remove paraffin wax. Over time and with repeated use, xylene becomes saturated with dissolved paraffin, drastically reducing its efficacy. Using fresh, pure xylene is recommended because it ensures the solvent has the full capacity to completely clear the tissue of wax, thereby exposing the epitopes for antibody binding [52] [54].
4. When should I cut new tissue sections? If the original tissue sections were subjected to an inadequate deparaffinization process, it is very difficult to reverse the effects on those same slides. Starting with newly cut tissue sections provides a clean slate, ensuring that the tissue is pristine and has not been compromised by prior processing errors [54].
Troubleshooting Guide: Deparaffinization and Staining Issues
The table below summarizes the common problems, their causes, and the ultimate solutions related to deparaffinization.
| Observed Problem | Primary Cause | Recommended Solution |
|---|---|---|
| No or Weak Staining [52] [53] | Insufficient deparaffinization; old or contaminated xylene [52]. | Repeat experiment with fresh xylene and new tissue sections [54]. |
| High, Spotty Background [54] [53] | Incomplete paraffin removal causing uneven reagent penetration. | Repeat experiment with fresh xylene and new tissue sections [54]. |
| Tissue Damage or Loss | Aggressive processing of under-fixed tissue or use of uncoated slides [7] [26]. | Ensure proper tissue fixation. Use positively charged or coated slides. Be gentle during antigen retrieval and washing steps [7] [53]. |
Experimental Protocol: Correct Deparaffinization and Staining
The following workflow details the correct procedure for deparaffinization and rehydration, which is foundational for all subsequent IHC steps.
Detailed Methodology
Dewaxing:
- Immerse the slides carrying new tissue sections in a first bath of fresh xylene for 5-10 minutes [53].
- Transfer the slides to a second bath of fresh xylene for another 5-10 minutes to ensure all paraffin is removed.
Rehydration through Ethanol Gradients:
- Hydrate the dewaxed sections through a series of ethanol solutions to prepare them for aqueous-based staining reagents.
- Immerse slides in 100% ethanol (two changes, 2-5 minutes each).
- Transfer to 95% ethanol for 2-5 minutes.
- Transfer to 70% ethanol for 2-5 minutes.
- Rinse the slides gently under a stream of distilled or deionized water. Crucially, do not allow the sections to dry out at any point from here onward, as this can create severe, irreversible background staining [52] [53].
Proceed to Antigen Retrieval:
The Scientist's Toolkit: Essential Research Reagent Solutions
The table below lists key materials required to execute the optimized deparaffinization protocol successfully.
| Reagent/Material | Function | Key Consideration |
|---|---|---|
| Fresh Xylene [52] [54] | Organic solvent that completely dissolves and removes paraffin wax from tissue sections. | Always use fresh, pure solvent. Do not reuse saturated xylene from previous runs. |
| Positively Charged or Coated Slides [7] [26] | Provides superior tissue adhesion, preventing tissue loss during rigorous deparaffinization and antigen retrieval steps. | Check slide expiration dates, as the charged coating can degrade over time. |
| Ethanol Gradients (100%, 95%, 70%) [53] | Rehydrates the tissue after dewaxing, preparing it for water-based buffers and antibodies. | Ensure solutions are prepared correctly and not contaminated. |
| Polymer-Based Detection System [54] | A detection method that does not rely on avidin-biotin chemistry, eliminating background from endogenous biotin. | Recommended over avidin-biotin (ABC) systems for tissues like liver and kidney with high endogenous biotin. |
FAQs on Deparaffinization and Quality Control
Q1: What are the common signs of incomplete deparaffinization, and how does it affect my IHC results? Incomplete deparaffinization presents as spotty, uneven background staining and can cause weak or absent target signal [55] [26]. Paraffin forms a physical barrier that prevents antibodies from reaching their targets, leading to failed experiments [22] [56]. This occurs because residual paraffin blocks antigen retrieval and antibody binding.
Q2: How can I verify that paraffin has been completely removed from my FFPE sections? While routine microscopy may not detect minimal residue, research indicates that conventional solvent protocols often leave paraffin contamination [22]. For critical work, specialized methods like Raman microspectroscopy can detect residual paraffin. A practical quality control check is to ensure fresh xylene appears clear after slide processing and does not become cloudy [26].
Q3: What are the best practices for storing reagents and slides to maintain purity and activity?
- Xylene: Use fresh, pure xylene and replace it regularly. Avoid using diluted solutions unless specified [26].
- Antibodies: Store according to manufacturer instructions. Aliquot to minimize freeze-thaw cycles and avoid contamination [57] [56].
- Prepared Slides: For IHC, use freshly cut sections whenever possible. If storage is necessary, keep slides at 4°C and do not bake them before storage [55] [56].
- Buffers: Prepare with pure water (check pH if using tap water for rinsing) and ensure proper sterility to prevent bacterial growth that can damage proteins [26] [56].
Q4: My positive controls are staining correctly, but my experimental slides show no signal. Could this be a deparaffinization issue? Yes. If controls confirm your antibodies and detection system are functional, the problem likely lies in sample preparation prior to antibody incubation [55]. Incomplete deparaffinization is a prime suspect, as it prevents antigen retrieval and antibody access [26] [56]. Verify your deparaffinization protocol, especially solution freshness and incubation times.
Troubleshooting Guides
Common Deparaffinization and Reagent Problems
| Problem & Manifestation | Possible Cause | Solution |
|---|---|---|
| Weak or No Staining [57] [56] | Incomplete paraffin removal creates a physical barrier [26] [56]. | Increase deparaffinization time; use fresh xylene or alternative solvents [55] [56]. |
| High Background Staining [11] [57] | Inadequate deparaffinization causes spotty, uneven background [55]. | Repeat with new sections and fresh xylene [55]. Ensure slides do not dry out after deparaffinization [2]. |
| Poor Antigen Retrieval [55] [2] | Residual paraffin prevents retrieval buffers from effectively unmasking epitopes [22]. | Standardize fixation; optimize retrieval method (microwave/pressure cooker) [55] [58]. |
| Loss of Tissue Sections [26] | Underlying issue is often improper fixation or slide treatment, not deparaffinization itself. | Ensure adequate fixation volume/time; use properly charged slides; control baking time/temperature [26]. |
Reagent Purity and Quality Control Checks
| Problem | Quality Control Check | Corrective Action |
|---|---|---|
| Ineffective Xylene [26] [56] | Check if solution becomes cloudy after use; verify preparation (if not ready-to-use). | Replace with fresh, pure xylene. Follow manufacturer's dilution instructions precisely [26]. |
| Antibody Degradation [57] [56] | Always run a positive control tissue with known expression. | Store antibodies correctly in aliquots; avoid repeated freeze-thaw cycles; do not use expired reagents [57] [56]. |
| Buffer Contamination [26] [56] | Check for cloudiness or microbial growth; monitor pH of tap water used for rinsing. | Use sterile buffers; add 0.01% sodium azide to PBS for storage; use filtered, pH-corrected water [26] [56]. |
| Inactive Detection Enzymes [11] [56] | Test system independently by applying enzyme to substrate. | Ensure deionized water lacks peroxidase inhibitors; never use sodium azide with HRP systems [11] [56]. |
Experimental Protocols for Quality Control
Protocol 1: Standardized Deparaffinization and Hydration
This protocol is critical for preventing common staining issues [58] [2].
Materials:
- Fresh Xylene
- Ethanol (100%, 95%, 85%, 75%)
- Coplin Jars or Automated Stainer
Steps:
- Xylene Incubation: Immerse slides in fresh xylene for 10-15 minutes. Repeat with a second bath of fresh xylene for another 10-15 minutes [2].
- Ethanol Hydration Series: Transfer slides through a graded ethanol series to rehydrate the tissue:
- Final Rinse: Rinse slides thoroughly in deionized or distilled water [2].
- Crucial Note: From this point onward, do not allow the slides to dry, as this causes nonspecific antibody binding and high background [2].
Protocol 2: Verification of Deparaffinization Efficacy
This method uses IHC staining intensity as a functional readout of paraffin removal.
Materials:
- FFPE tissues with known, robust antigen expression (e.g., human tonsil for CD3)
- Optimized IHC protocol for a target in the control tissue
- Fresh and old/contaminated xylene for comparison
Steps:
- Cut serial sections from the control FFPE block.
- Subject slides to different deparaffinization conditions:
- Group A (Optimal): Fresh xylene, two changes of 10-15 minutes each.
- Group B (Suboptimal): Overused or diluted xylene.
- Process all slides simultaneously using the same IHC protocol.
- Compare staining intensity and background between groups. A clear reduction in signal in Group B indicates inadequate deparaffinization.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Deparaffinization & QC |
|---|---|
| High-Purity Xylene | Primary solvent for dissolving and removing paraffin wax from tissue sections. Must be fresh and uncontaminated [55] [26]. |
| Xylene Substitutes | Less hazardous, commercially available alternatives for paraffin removal. Follow manufacturer's instructions for use [2]. |
| Charged Microscope Slides | Positively charged slides enhance tissue adhesion, preventing section loss during aggressive deparaffinization and retrieval steps [26]. |
| Positive Control FFPE Tissue | Tissue with known expression of your target. Essential for verifying that the entire IHC process, including deparaffinization, worked correctly [55] [57]. |
| SignalStain Antibody Diluent | Optimized commercial diluent. Can enhance signal-to-noise ratio compared to homemade buffers like TBST/5% NGS for certain antibodies [55]. |
| Polymer-Based Detection Kits | Systems like SignalStain Boost provide enhanced sensitivity and avoid background from endogenous biotin present in tissues like liver and kidney [55] [11]. |
Workflow and Troubleshooting Diagrams
Deparaffinization Quality Control Workflow
Troubleshooting Logic for Staining Failure
Validation and Quality Control: Ensuring Deparaffinization Efficacy for Robust and Reproducible Data
FAQs on Deparaffinization Protocol Validation
What are the critical steps in a standard deparaffinization protocol? A standard deparaffinization protocol involves immersing paraffin-embedded tissue sections in xylene (or a xylene-substitute) twice, typically for 10-15 minutes each time, followed by rehydration through a graded series of ethanol washes (100%, 95%, 85%, 75%) and finally water before antigen retrieval [2]. The key is to ensure complete wax removal without letting the sections dry out.
Why is validating the deparaffinization protocol so important for IHC? Incomplete deparaffinization is a primary cause of poor immunohistochemistry (IHC) staining. It creates a physical barrier that prevents antibodies and other reagents from penetrating the tissue, leading to weak or absent staining, high background noise, and spotty, uneven staining patterns [59] [60]. A validated protocol ensures consistent, reliable results essential for accurate data interpretation and diagnosis [61].
What are the direct consequences of incomplete deparaffinization on staining quality? Incomplete deparaffinization directly causes several specific staining artifacts [59] [60] [62]:
- Weak or No Staining: The antibody cannot access the target antigen.
- High, Spotty Background: Reagents trap unevenly in the wax, causing non-specific precipitation.
- Non-specific Staining: Uneven reagent penetration leads to false-positive signals.
How can I troubleshoot a deparaffinization protocol that is failing? If you suspect deparaffinization failure, implement these troubleshooting steps [59] [62]:
- Use Fresh Reagents: Always use fresh xylene (or substitute) and ethanol solutions for each run. Old, contaminated solvents are a common failure point.
- Increase Incubation Time: Extend the immersion time in xylene, especially for thicker sections or densely packed tissues.
- Verify Technique: Ensure slides are agitated during washes to improve solvent action and are never allowed to dry after the process begins.
Key Performance Indicators (KPIs) for Validation
When validating a deparaffinization protocol, monitor these quantitative and qualitative KPIs to objectively assess performance.
Table 1: Key Performance Indicators for Deparaffinization Validation
| KPI Category | Specific Metric | Target Performance Value | Method of Assessment |
|---|---|---|---|
| Staining Quality | Overall Concordance with Expected Result | ≥90% [61] | Visual & digital comparison to validated control |
| Signal-to-Noise Ratio | High, clear specific staining over minimal background [59] | Microscopy & image analysis | |
| Specific Artifacts | Incidence of Weak/No Staining | 0% [61] | Visual scoring of all stained sections |
| Incidence of High/Spotty Background | 0% [61] | Visual scoring of all stained sections | |
| Protocol Robustness | Inter-Batch Consistency | >95% concordance between batches [61] | Compare KPIs across multiple validation runs |
| Control Tissue Performance | Consistent staining in known control tissues [61] | Track staining intensity of controls over time |
The Scientist's Toolkit: Essential Reagents & Materials
Table 2: Essential Materials for Deparaffinization Protocol Validation
| Item | Function in Validation | Key Considerations |
|---|---|---|
| Xylene or Xylene-Substitute | Primary solvent for dissolving and removing paraffin wax. | Must be fresh; old solvent is a primary cause of protocol failure [60] [62]. |
| 100% Ethanol | Removes xylene and begins tissue rehydration. | Used in two changes to ensure complete xylene removal [2]. |
| Graded Ethanol Series (95%, 85%, 75%) | Hydrates the tissue gradually to prevent morphological damage. | Prepares tissue for aqueous-based buffers and antibody solutions [2] [3]. |
| Positive Control Tissue | Tissue with known, consistent antigen expression. | Serves as a benchmark for optimal staining after deparaffinization [61] [60]. |
| Negative Control Tissue | Tissue known not to express the target antigen. | Helps identify non-specific background staining caused by insufficient deparaffinization [61]. |
Experimental Validation Workflow
The following diagram outlines a systematic workflow for validating a deparaffinization protocol.
Detailed Methodology for Validation Experiments
1. Select Control Tissues:
- Choose a set of FFPE control tissues that include both known positive and known negative cases for the target antigen [61]. For predictive markers, CAP guidelines recommend a minimum of 20 positive and 20 negative cases for a robust validation [61].
- Ensure control tissues have experienced similar pre-analytic conditions (fixation, processing) as patient samples [61].
2. Execute Deparaffinization Protocol:
- Follow the established deparaffinization steps meticulously. A typical manual protocol involves [2]:
- Xylene: 2 changes, 10-15 minutes each.
- Ethanol Series: 100% (2x, 5 min), 95% (2x, 5 min), 85% (5 min), 75% (5 min).
- Final Rinse: Distilled water (2x, 5 min).
- Crucial Note: From the moment slides enter the rehydration series, they must never be allowed to dry, as this causes irreversible non-specific antibody binding and high background [2].
3. Perform Full IHC Staining:
- Continue with the complete IHC procedure immediately after deparaffinization and rehydration. This includes antigen retrieval, blocking, primary and secondary antibody incubation, and detection [2] [3].
- Run all controls (positive, negative, no-primary) simultaneously to ensure any issues can be correctly attributed [60].
4. Microscopic Evaluation & KPI Analysis:
- Pathologists or trained scientists should evaluate the stained slides blinded to the expected outcome.
- Score slides based on the KPIs in Table 1, specifically looking for the absence of artifacts linked to poor deparaffinization (weak staining, high spotty background) [61] [59].
- An overall concordance of 90% or higher with the expected results is typically considered acceptable for validation [61].
Troubleshooting Guide: Common Deparaffinization Issues
Table 3: Troubleshooting Common Deparaffinization Problems
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Weak or No Staining | Incomplete wax removal creating a barrier to antibody penetration. | Increase deparaffinization time; always use fresh xylene [59] [62]. |
| High, Spotty Background | Insufficient deparaffinization causing uneven reagent trapping and precipitation. | Repeat experiment with new sections and fresh xylene [60]. |
| Non-specific Staining | Tissue sections dried out during or after the rehydration process. | Ensure slides are covered in liquid at all times after deparaffinization begins [59] [2]. |
| Inconsistent Results Between Runs | Degraded or contaminated solvent batches; variable immersion times. | Standardize protocol timing; use fresh, high-quality reagents for every run [61]. |
Using Positive and Negative Controls to Monitor Deparaffinization Efficiency
The Critical Role of Controls in Deparaffinization
In immunohistochemistry (IHC) research, proper deparaffinization is a foundational step that directly impacts experimental outcomes. Incomplete paraffin removal compromises antibody penetration and epitope accessibility, leading to weak staining, high background, or false-negative results [63] [18]. While these problems are well-documented, many researchers struggle to determine whether poor staining results from antibody issues versus inadequate sample preparation.
Positive and negative controls provide the objective data needed to isolate deparaffinization efficiency as an experimental variable. A properly functioning positive control tissue with known antigen expression should display robust, specific staining when deparaffinization is complete. Conversely, a negative control (primary antibody omitted) should show minimal background, helping distinguish true signal from paraffin-induced artifacts [63]. Implementing this control system enables researchers to troubleshoot systematically rather than guessing at the root cause of staining problems.
The following diagram illustrates how controls integrate into the troubleshooting workflow for identifying deparaffinization issues:
Figure 1: A control-based workflow isolates deparaffinization as the staining problem source.
Troubleshooting Guide: Deparaffinization Issues
Common Problems and Solutions
| Problem | Observable Effects | Recommended Solution | Control Observation |
|---|---|---|---|
| Incomplete Deparaffinization | Spotty, uneven background staining; weak or absent target signal [63] [26] | Repeat with fresh xylene (2-3 cycles, 5-10 min each) [18] [2] | Positive control shows weak staining; negative control may show high background |
| Overexposure to Solvents | Tissue brittleness, distortion, or detachment [18] | Optimize immersion times; ensure proper ethanol rehydration series [18] [2] | Tissue damage visible in both test and control samples |
| Old or Contaminated Xylene | Variable staining across sections; crystalline deposits [63] [26] | Replace with fresh xylene; use multiple fresh baths [63] [64] | Inconsistent staining between control slides |
| Inadequate Rehydration | Poor aqueous reagent penetration; uneven staining [18] | Implement graded ethanol series (100%-95%-85%-70%-50%) [18] [2] | Positive control shows patchy staining pattern |
Advanced Troubleshooting Scenarios
Persistent Background After Apparent Deparaffinization
- Issue: High background continues despite fresh xylene treatment
- Investigation: Check if detection system uses biotin-streptavidin in tissues with endogenous biotin (liver, kidney) [63] [11]
- Solution: Switch to polymer-based detection systems or perform biotin blocking [63]
Edge Artifacts and Variable Staining
- Issue: Strong staining on tissue edges with weak central staining
- Root Cause: Possible under-fixation combined with paraffin trapping [26] [2]
- Solution: Extend fixation time and verify deparaffinization completeness with controls
Experimental Protocols
Standardized Deparaffinization Protocol for IHC
This protocol ensures complete paraffin removal while maintaining tissue integrity for optimal immunohistochemical staining [18] [2]:
Materials Required:
- Xylene or xylene substitutes
- 100%, 95%, 85%, 70%, and 50% ethanol solutions
- Coplin jars or automated stainer
- Distilled water
Procedure:
- Xylene Immersion: Place slides in fresh xylene for 10-15 minutes
- Second Xylene Bath: Transfer to second xylene bath for additional 10-15 minutes
- Ethanol Series:
- 100% ethanol: 5 minutes (two changes)
- 95% ethanol: 5 minutes (two changes)
- 85% ethanol: 5 minutes
- 70% ethanol: 5 minutes
- 50% ethanol: 5 minutes
- Hydration: Rinse slides three times with distilled water
- Critical Note: Do not allow slides to dry after rehydration, as this causes nonspecific antibody binding and high background [2]
Validation with Controls:
- Include known positive control tissue sections in each run
- Process negative control (no primary antibody) alongside test samples
- Acceptable results: Positive control shows robust specific staining; negative control shows minimal background
Control-Based Quality Assessment Method
Quantitative Assessment Using Image Analysis: For precise quality monitoring, researchers can employ image analysis software to quantify staining intensity in control samples:
- Image Acquisition: Capture whole slide images at consistent magnification
- Color Deconvolution: Use Fiji/ImageJ to separate hematoxylin and DAB signals [65]
- Threshold Setting: Establish consistent thresholds for positive staining
- Quantification: Measure percentage of DAB-positive area in control tissues
- Documentation: Record values for quality tracking over time
Acceptance Criteria:
- Positive controls should maintain consistent staining intensity (≤20% variance from historical controls)
- Negative controls should show <2% background staining in target tissues
- Investigate any deviations from these parameters as potential process failures
Research Reagent Solutions
| Reagent | Function | Technical Notes |
|---|---|---|
| Xylene | Primary solvent for dissolving paraffin wax | Use fresh solutions; multiple baths recommended; toxic requiring ventilation [18] |
| Xylene Substitutes | Less hazardous paraffin solvents | Follow manufacturer's instructions for ethanol compatibility [2] |
| Ethanol Series (100%-50%) | Rehydration while preventing tissue damage | Gradual concentration changes prevent structural damage [18] |
| SignalStain Antibody Diluent | Optimal antibody performance | Specific diluents can significantly enhance signal-to-noise ratio [63] |
| Polymer-Based Detection Reagents | Enhanced sensitivity detection | Superior to avidin/biotin systems; avoids endogenous biotin issues [63] |
Frequently Asked Questions
Q1: How can I determine if my deparaffinization is complete using controls? A: Process your positive control tissue through the deparaffinization protocol. If staining is weak or absent in the positive control while the negative control shows high background, deparaffinization is likely incomplete. Properly deparaffinized controls should show robust specific staining (positive) with minimal background (negative) [63].
Q2: Can I reuse xylene for multiple batches of slides? A: No, xylene should be fresh for optimal results. Used xylene becomes saturated with paraffin, reducing efficiency. Multiple cycles (2-3) of fresh xylene are recommended for complete paraffin removal [63] [64].
Q3: What is the most common mistake in deparaffinization that affects IHC results? A: The most common error is insufficient immersion time in xylene or using old, saturated xylene solutions. This leads to residual paraffin that blocks antibody access to epitopes, causing weak staining or high background [63] [26].
Q4: How does improper deparaffinization specifically affect my positive control? A: Incomplete deparaffinization physically blocks antibody access to epitopes, resulting in false-negative staining in your positive control. This occurs even when the antibody and detection systems are functioning properly [63] [18].
Q5: Can automated stainers reliably deparaffinize tissues? A: Yes, but regular maintenance is essential. Check that heating elements are functioning properly and solution lines aren't clogged. Always validate automated systems with control tissues to ensure complete paraffin removal [26].
Q6: What should I do if my controls indicate deparaffinization problems? A: First, replace all xylene and ethanol solutions with fresh reagents. Repeat the deparaffinization protocol with increased immersion times. If problems persist, check that your oven temperature reaches the paraffin melting point (56-58°C) during baking [26].
Within the framework of a broader thesis on deparaffinization problems in immunohistochemistry (IHC) research, this guide addresses a critical, yet often overlooked, initial step in the processing of formalin-fixed, paraffin-embedded (FFPE) tissue sections. Effective deparaffinization is foundational to all subsequent staining and interpretation phases. Incomplete paraffin removal creates a hydrophobic barrier that prevents aqueous-based staining reagents from penetrating the tissue, leading to a cascade of experimental artifacts, compromised data, and erroneous conclusions. This technical support document provides a comparative analysis of suboptimal versus optimized practices, offering researchers and drug development professionals clear troubleshooting and protocols to safeguard data integrity.
FAQs: Understanding Deparaffinization Fundamentals
1. Why is deparaffinization specifically critical for IHC compared to routine H&E staining? IHC relies on the precise antigen-antibody binding, which is highly sensitive to physical barriers. Incomplete deparaffinization prevents antibodies and other large detection molecules (e.g., polymer-based HRP) from accessing the tissue matrix, leading to false-negative results. While H&E staining can also be affected, the smaller molecular size of the dyes makes it somewhat more tolerant of minor paraffin residues, meaning IHC failure can occur even when H&E appears normal.
2. What are the definitive signs that my staining issues originate from deparaffinization? The primary indicators are spatial and irregular staining patterns [66] [49]:
- Weak or No Staining: A complete lack of expected signal in positive control tissues [66].
- Uneven, Patchy, or Spotty Background: Staining is not consistent across the tissue section and appears blotchy [66] [49].
- High, Irregular Background: This occurs when reagents pool in areas where paraffin has been partially, but not completely, removed [49].
3. How can I troubleshoot a suspected deparaffinization problem? First, ensure you are using fresh xylene or a suitable substitute, as old, contaminated solvents lose efficacy [66] [49]. Second, extend the incubation time in the deparaffinization solutions, particularly for thicker sections or tissues with dense connective tissue. Finally, always include a well-characterized positive control tissue processed in the same batch to isolate the problem to the protocol rather than the antibody or tissue itself.
Troubleshooting Guide: Suboptimal vs. Optimized Deparaffinization
The table below summarizes the direct impact of deparaffinization quality on IHC outcomes, providing a clear framework for diagnosis and resolution.
Table 1: Impact of Deparaffinization on IHC Staining and Interpretation
| Aspect | Suboptimal Deparaffinization | Optimized Deparaffinization | Corrective Action |
|---|---|---|---|
| Staining Intensity | Weak, faint, or complete absence of specific signal [66] [49]. | Strong, clear specific staining. | Repeat staining with new sections using fresh xylene [66] [49]. |
| Staining Uniformity | Irregular, patchy, or spotty staining across the tissue section [66] [49]. | Even and consistent staining throughout the entire tissue. | Increase deparaffinization time; ensure slides are fully submerged and agitated. |
| Background Staining | High, uneven background; nonspecific speckling [66] [49]. | Low, clean background with high signal-to-noise ratio. | Use fresh xylene and ethanol solutions; ensure proper hydration before antibody incubation [49]. |
| Data Interpretation | Risk of false negatives; inaccurate quantification of protein expression; unreliable data [66]. | Accurate and reliable interpretation of protein localization and expression levels. | Always validate staining protocol with controls and repeat if irregular patterns are observed. |
| Tissue Integrity | Potential for tissue damage if sections are exposed to harsh, old solvents for extended periods. | Tissue morphology is well-preserved for accurate pathological assessment. | Follow a graded series of solvents and avoid prolonged exposure to harsh chemicals. |
Experimental Protocols for Validation
To objectively assess and validate deparaffinization efficiency within a research setting, the following experimental approaches can be employed.
Protocol for Direct Visualization of Residual Paraffin
Purpose: To visually confirm the complete removal of paraffin before proceeding with immunostaining. Method:
- After the final absolute ethanol step in the deparaffinization series, incubate the slide in a xylene substitute containing a water-soluble fluorescent dye (e.g., Nile red) for 2-5 minutes.
- Rinse briefly in fresh absolute ethanol.
- Observe the slide under a fluorescence microscope. The presence of fluorescent patches indicates areas where residual paraffin has trapped the hydrophobic dye.
- If fluorescence is observed, return the slide to fresh xylene and repeat the deparaffinization and hydration steps.
Protocol for Comparative Staining Analysis
Purpose: To systematically compare the impact of different deparaffinization conditions on final IHC outcome [66] [49]. Method:
- Sectioning: Cut consecutive sections from the same FFPE tissue block.
- Experimental Groups:
- Group A (Optimized): Deparaffinize in fresh xylene (2 changes, 5-10 minutes each).
- Group B (Suboptimal): Deparaffinize in old, saturated xylene (1 change, 3 minutes).
- Group C (Control): Include a known positive control tissue processed with the optimized method.
- Staining: Process all groups through the exact same, validated IHC protocol simultaneously.
- Analysis: Compare staining intensity, uniformity, and background across groups using digital pathology software or semi-quantitative scoring by a pathologist. The expected outcome, as demonstrated in practice, is that Groups B will show significantly weaker and more irregular staining compared to Group A [66] [49].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents used in the deparaffinization and subsequent IHC workflow, with an emphasis on their specific function and importance for success.
Table 2: Essential Reagents for Deparaffinization and Initial IHC Steps
| Reagent | Function | Critical Consideration |
|---|---|---|
| Xylene / Xylene Substitutes | Dissolves and removes paraffin wax from tissue sections [47]. | Freshness is critical. Exhausted xylene leaves a paraffin film, blocking antibody access [66] [49]. |
| Ethanol (100%, 95%, 70%) | Forms a graded series for rehydration after xylene, preparing tissue for aqueous buffers [47]. | Must be reagent grade and used in a strict descending concentration series to prevent tissue dehydration artifacts. |
| Target Antigen Retrieval Buffer | Unmasks epitopes cross-linked by formalin fixation; common buffers include Citrate (pH 6.0) and EDTA (pH 8.0/9.0) [67] [47]. | Ineffective deparaffinization will render this step useless, as the buffer cannot penetrate the tissue [47]. |
| Primary Antibody Diluent | Stable buffer for diluting the primary antibody, often containing protein and stabilizers. | Antibodies diluted in this solution cannot penetrate paraffin residues, leading to false negatives. |
Workflow Visualization: The Role of Deparaffinization in IHC
The diagram below illustrates the IHC workflow, highlighting how suboptimal deparaffinization creates a critical failure point that compromises all downstream steps.
Technical Support Center
Troubleshooting Guides & FAQs
FAQ: What are the most critical steps to standardize across multiple laboratories to ensure consistent IHC staining? The most critical steps are tissue fixation, antigen retrieval, and primary antibody incubation. Variation in fixation time and the antigen retrieval method (e.g., microwave vs. pressure cooker) are major sources of staining variability between sites. Standardizing the specific protocols for these steps is essential [28] [68].
FAQ: Our multi-center study shows high background staining. What are the common causes and solutions? High background often results from inadequate deparaffinization, insufficient blocking, or endogenous enzyme activity.
- Cause: Inadequate deparaffinization.
- Cause: Endogenous peroxidase activity when using HRP-based detection.
- Cause: Endogenous biotin, especially in kidney and liver tissues.
- Cause: Nonspecific binding from the primary antibody.
FAQ: We are experiencing weak or absent target staining. How can we resolve this? Weak or absent staining can be due to several factors, with antigen retrieval being a primary suspect.
- Cause: Suboptimal antigen retrieval.
- Solution: Re-optimize the antigen retrieval method (e.g., using a microwave oven or pressure cooker) and buffer for your specific antibody and tissue type. Using a microwave oven is often preferred over a water bath [68].
- Cause: Loss of antigenicity due to prolonged slide storage.
- Cause: Primary antibody potency.
- Solution: Ensure the antibody is stored correctly and test its potency on a known positive control sample. Always include a positive control in your experiments [11].
FAQ: How does tissue fixation impact IHC results, and what is the best practice? Ischemia time before fixation and the duration of fixation itself can significantly alter IHC results. Proteins and antigens, such as Ki-67 and phosphoproteins, are particularly vulnerable to ischemic time. Best practice is to use 10% neutral buffered formalin (NBF) for 24 hours at room temperature with a tissue-to-fixative ratio between 1:1 and 1:20. Rapid fixation after specimen resection is critical to prevent protein degradation [28].
Key IHC Troubleshooting Table
The following table summarizes common IHC problems, their causes, and recommended solutions.
| Potential Problem | Primary Cause | Recommended Solution |
|---|---|---|
| Little to No Staining [68] | Suboptimal antigen retrieval | Re-optimize retrieval method (use microwave/pressure cooker) and buffer [68]. |
| Loss of antigenicity | Use freshly cut tissue sections; avoid prolonged slide storage [28] [68]. | |
| Inadequate deparaffinization | Use fresh xylene and new tissue sections [68] [11]. | |
| High Background Staining [68] [11] | Endogenous peroxidase activity | Quench with 3% H2O2 for 10 minutes [68] [11]. |
| Endogenous biotin | Use polymer-based detection or a biotin block [68] [11]. | |
| Inadequate blocking | Increase concentration of blocking serum (e.g., to 5-10%) [28] [11]. | |
| Variable Staining Between Labs [28] [69] | Non-standardized fixation | Standardize ischemic and formalin fixation time (e.g., 24hrs in NBF) [28]. |
| Different antibody clones/platforms | Harmonize antibodies, platforms, and positivity thresholds [69]. |
Experimental Protocols & Data
Standardized IHC Protocol for Multi-Center Studies
Below is a detailed, standardized protocol developed to minimize inter-laboratory variability, based on methodologies from the search results.
Standardized IHC Workflow for Multi-Center Studies
Detailed Procedure:
- Deparaffinization and Rehydration:
Antigen Retrieval:
Blocking:
Primary Antibody Incubation:
- Apply the optimized dilution of primary antibody in a recommended diluent.
- Incubate overnight at 4°C in a humidified chamber [68].
Detection:
Chromogenic Development and Counterstaining:
Quantitative Data from Standardization Studies
The table below summarizes performance data from studies that highlight the impact of protocol standardization.
| Study Focus | Key Parameter Measured | Result Before Standardization | Result After Standardization/Harmonization |
|---|---|---|---|
| Pan-Trk IHC Harmonization [69] | Rate of False Negatives (with ≥1% positivity threshold) | Significant variability and higher false-negative rates observed with different antibodies/platforms. | False-negative cases were reduced after harmonization of antibodies and platforms. |
| GEP vs. IHC Diagnostic Accuracy [70] | Overall Diagnostic Accuracy | IHC accuracy: 83% (across all specimens). | N/A (High accuracy of >90% was linked to cases requiring only a single round of IHC stains, implying a more straightforward, robust protocol) [70]. |
| Antigen Retrieval Method Comparison [68] | Staining Performance (Signal Intensity) | Water bath method: weak staining. | Microwave oven or pressure cooker methods: robust, enhanced staining [68]. |
The Scientist's Toolkit
Research Reagent Solutions
This table details essential materials and reagents for a standardized IHC protocol.
| Item | Function / Explanation | Example / Specification |
|---|---|---|
| Primary Antibody Diluent | Optimized solution to dilute the primary antibody for maximum signal-to-noise ratio. Using the manufacturer's recommended diluent is critical [68]. | SignalStain Antibody Diluent or TBST/5% Normal Goat Serum [68]. |
| Polymer-Based Detection System | A highly sensitive detection method that avoids issues with endogenous biotin, which is common in avidin-biotin (ABC) systems [68] [11]. | SignalStain Boost IHC Detection Reagents (HRP) [68]. |
| Antigen Retrieval Buffer | A solution used in HIER to break protein cross-links formed during fixation, thereby "unmasking" epitopes for antibody binding [28]. | 10 mM Sodium Citrate Buffer, pH 6.0 [11]. |
| Blocking Serum | Normal serum from the species in which the secondary antibody was raised. It blocks nonspecific binding sites to reduce background staining [28]. | 5-10% Normal Goat Serum (if using goat-anti-rabbit secondary) [28] [68]. |
| Endogenous Enzyme Block | Chemical inhibitors that neutralize endogenous enzymes in tissues that could react with the detection system, causing high background [28] [11]. | 3% H2O2 (for peroxidases); Levamisole (for alkaline phosphatase) [28] [11]. |
IHC Problem-Solving Decision Workflow
The following diagram provides a logical pathway for troubleshooting common IHC issues.
FAQs: Deparaffinization in IHC Research
1. What is the fundamental purpose of deparaffinization in IHC, and why is it so critical? Deparaffinization is the process of removing paraffin wax from formalin-fixed, paraffin-embedded (FFPE) tissue sections. Its primary purpose is to return the tissue to its original pre-embedded state, allowing antibodies and staining reagents to penetrate the tissue and access target antigens. This step is crucial because incomplete paraffin removal hinders reagent penetration, leading to weak or absent staining, high background noise, and unreliable results [18].
2. What are the most common indicators of deparaffinization failure? The most frequent symptoms of inadequate deparaffinization are:
- Weak or No Staining: Incomplete wax removal physically blocks antibody binding [71] [72].
- Spotty or Uneven Background: This appears as irregular, non-specific staining across the tissue section, often caused by residual paraffin [71] [72].
- Non-specific Staining: Residual paraffin can cause antibodies to bind to unintended sites [49].
3. How can I troubleshoot a protocol that I suspect is yielding incomplete deparaffinization? The standard troubleshooting approach involves checking the following:
- Freshness of Solvents: Always use fresh xylene or xylene substitutes. Overused solvents become saturated with paraffin and lose effectiveness [71] [72].
- Immersion Time: Ensure slides are immersed in xylene for an adequate duration, typically 5-10 minutes per bath, with multiple cycles (2-3) for complete removal [18].
- Agitation: Gently agitating the slides during immersion can improve solvent contact and paraffin dissolution.
- Tissue Thickness: Thicker sections may require longer immersion times in xylene [18].
4. What emerging technologies are improving the deparaffinization process? The field is moving towards full automation and integration with digital pathology.
- Automated Stainers: Automated platforms perform deparaffinization, rehydration, and subsequent staining with high precision, reducing human error and variability [2] [73].
- AI-Assisted Quality Control: Emerging workflows use whole-slide scanners and AI-supported software (e.g., QuPath) to digitize slides and automatically assess staining quality, which indirectly evaluates sample preparation, including deparaffinization [73].
- High-Throughput Workflows: Semi-automated systems like tissue microarrayers integrate deparaffinization into streamlined processes for analyzing large sample cohorts efficiently, significantly saving time and resources [73].
5. Are there safer alternatives to xylene for deparaffinization? Yes, several less hazardous commercial alternatives to xylene are available. These are often citrus-based or aliphatic hydrocarbon solvents. When using these substitutes, it is essential to follow the manufacturer's specific instructions for ethanol exchange and mounting procedures [2].
Troubleshooting Guide: Common Deparaffinization Problems and Solutions
The following table summarizes frequent issues, their causes, and evidence-based solutions.
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Weak or No Staining [72] [49] | Incomplete deparaffinization blocking antibody access. | Increase deparaffinization time; use fresh xylene or substitutes; ensure adequate number of xylene baths (2-3 cycles) [71] [72] [18]. |
| Spotty/Uneven Background [71] | Inadequate deparaffinization causing irregular reagent flow. | Repeat experiment with new sections and fresh xylene [71]. |
| Non-specific Staining [49] | Residual paraffin leading to nonspecific antibody trapping. | Increase deparaffinization time and use fresh dimethyl benzene (xylene) [72] [49]. |
| Tissue Damage [18] | Overexposure to harsh solvents like xylene. | Optimize immersion time; avoid excessively long exposure to xylene, especially for delicate tissues [18]. |
Experimental Protocol: Standard Deparaffinization and Rehydration
This detailed protocol is essential for preparing FFPE tissue sections for subsequent IHC staining [23] [2] [18].
Materials Required:
- FFPE tissue sections on glass slides
- Xylene or a certified xylene substitute
- 100%, 95%, 85%, 75%, and 50% Ethanol
- Deionized or distilled water
- Coplin jars or automated stainer racks
- Fume hood (if using xylene)
Methodology:
- Deparaffinization:
- Rehydration (Gradual Hydration through Ethanol Series):
- Immerse slides in 100% ethanol for 5 minutes [2].
- Transfer to a second bath of 100% ethanol for 5 minutes [2].
- Sequentially immerse slides through a descending ethanol series to rehydrate the tissue:
- Rinse slides gently in running tap water or deionized water for 10 minutes to remove all traces of ethanol [23].
- Critical Note: From this point onward, do not allow the slides to dry out, as drying causes irreversible non-specific antibody binding and high background [2]. Proceed directly to antigen retrieval.
Workflow Visualization: Traditional vs. Emerging Deparaffinization
The diagram below contrasts the manual and automated/AI-assisted workflows for deparaffinization and quality assessment.
The Scientist's Toolkit: Essential Research Reagent Solutions
This table details key materials and their functions for effective deparaffinization.
| Item | Function | Technical Notes |
|---|---|---|
| Xylene [71] [18] | Organic solvent that effectively dissolves and removes paraffin wax. | Industry standard; requires careful handling in a fume hood due to toxicity. |
| Xylene Substitutes [2] | Safer, less toxic solvents (e.g., citrus-based, aliphatic hydrocarbons) for paraffin removal. | Follow manufacturer-specific protocols for ethanol exchange and mounting. |
| Ethanol (100%, 95%, 70%, 50%) [23] [18] | Used in a descending series to rehydrate tissue after deparaffinization, removing xylene and preparing tissue for aqueous-based staining. | A gradual series is critical to prevent tissue damage. |
| Automated Stainer [2] | Instrument that automates deparaffinization, rehydration, and staining protocols. | Ensures consistency, reduces manual labor, and improves reproducibility. |
| Positively Charged Glass Slides [23] | Microscope slides with a charged coating to enhance tissue section adhesion. | Prevents tissue loss during rigorous deparaffinization and washing steps. |
Conclusion
Deparaffinization is not merely a preliminary step but a critical determinant of success in IHC. Inadequate removal of paraffin wax is a primary, yet often overlooked, cause of staining failures, introducing significant variability that can compromise research reproducibility and clinical diagnostic accuracy. By understanding its foundational importance, adhering to optimized methodological protocols, systematically applying troubleshooting principles, and rigorously validating the process, researchers can eliminate a major source of error. Mastering this essential technique ensures the generation of robust, reliable, and high-quality IHC data, which is fundamental for advancing drug development, biomarker discovery, and translational clinical research.
References
- 1. FFPE in modern tissue analysis: Applications and ... [https://www.abcam.com/en-us/knowledge-center/immunohistochemistry/ffpe-in-modern-tissue-analysis]
- 2. IHC-P protocols [https://www.abcam.com/en-us/technical-resources/protocols/ihc-with-samples-in-paraffin]
- 3. IHC Protocol [https://www.bostonbioproducts.com/resources/ihc-protocol/]
- 4. Immunohistochemistry ( IHC ) Troubleshooting & the... Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide]
- 5. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 6. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOorR5DIleMYixpXtW5z5ZuScvvgdcHF97TILXJ19UU0oMqolaZBm]
- 7. Immunohistochemistry Paraffin Troubleshooting: IHC-P Help [https://www.bio-techne.com/applications/imaging/immunohistochemistry/ihc-paraffin-troubleshooting]
- 8. Automated IHC protocols for Anti-PD-L1 [clone 28-8] | Abcam [https://www.abcam.com/en-us/technical-resources/protocols/automated-ihc]
- 9. å¤å‘性æµäº§ä¸4ç§å宫内膜å…疫细胞类型的多é‡è§å…‰å…疫组织 ... [https://app.jove.com/cn/t/62931/multiplexed-fluorescent-immunohistochemical-staining-four-endometrial]
- 10. Chromogenic Immunohistochemistry (IHC) Paraffin Protocol [https://www.novusbio.com/support/support-by-application/immunohistochemistry-paraffin/protocol.html?srsltid=AfmBOoqhQeX4d8s2hAf8wXEIvXlENCgCSZzTt9T4fFH97ASV67op93Y_]
- 11. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 12. IHC On Paraffin Sections [https://www.ptglab.com/support/immunohistochemistry-protocol/ihc-on-paraffin-sections/?srsltid=AfmBOoryp__An52vSgPwzs6DOIcI3dpioBfib1VeDaNMy5MlFJtjG3ng]
- 13. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOorKhKlfiaSG0MfYl7LktQGmqWEOCoTRaRb3Mmg9VSa-Nxxz7R_a]
- 14. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/?srsltid=AfmBOopz3nr_5p7R--hAN_QKwX3q7m1S-b_t_dMSezKaoLTjoobLOYVR]
- 15. Effects of Prolonged Formalin Fixation on Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2713075/]
- 16. Proteomic analysis of formalin-fixed paraffin embedded ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3516368/]
- 17. Paraffin Removal and Antigen Retrieval [https://www.thermofisher.com/ar/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/paraffin-removal-antigen-retrieval.html]
- 18. Deparaffinization & Rehydration of FFPE Tissue Samples [https://superiorbiodx.com/blog/deparaffinization-protocol/]
- 19. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooffM79-6kPs-H2Sy6BK721Ipku0JXEvzYP6iEsBKWIgRtr-pc0]
- 20. A review of artifacts in histopathology - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6097380/]
- 21. A simple heat-based alternative method for ... [https://www.sciencedirect.com/science/article/pii/S2215016123000821]
- 22. Rapid and complete paraffin removal from human tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7677988/]
- 23. Immunohistochemistry Protocols [https://www.antibodies.com/applications/immunohistochemistry/ihc-protocol]
- 24. Paraffin Embedded Immunohistochemistry Protocol (IHC-P) [https://hellobio.com/ihc-p-protocol/]
- 25. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOop8MooYTvoD6XOeKk6A4JmbGj-vyMcx0BFJbM3HE3IFd5s3IglT]
- 26. Troubleshooting Immunohistochemistry [https://www.nsh.org/blogs/alisha-yocum/2023/04/13/troubleshooting-ihc]
- 27. Immunohistochemistry Troubleshooting Guide [https://www.enzo.com/note/immunohistochemistry-troubleshooting-guide/]
- 28. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 29. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqRazGJbJBcIlSqGhBp1PBxt9m2JW2Aw-57HKBimN66MKiBA9Eg]
- 30. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOooP_M_K3ytVLQzpthvChiOAUE1WqBtocWD3Z2-INKh7l2_cK53r]
- 31. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/?srsltid=AfmBOorSyU2fDeGfuRc_lJlFBl0XJff-vimXuUGJ9M5DN_D1r5jYdPBL]
- 32. Biofriendly Substitutes for Xylene in Deparaffinization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7595545/]
- 33. Fluorescent IHC Protocol: Paraffin-embedded Tissue ... [https://www.rndsystems.com/resources/protocols/protocol-preparation-and-fluorescent-ihc-staining-paraffin-embedded-tissue]
- 34. Immunohistochemistry Paraffin Troubleshooting: IHC-P Help [https://www.novusbio.com/support/support-by-application/immunohistochemistry-paraffin/troubleshooting.html?srsltid=AfmBOop7dThAPDSj2ljxCxe4JwejWHFq7vXxVPqFSQnc29q8ZD9XaZDl]
- 35. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoql_Mlj99rIkk0m5OICd7CB4LhZtTB80GFm8Ci5yR2AUE6JwVFh]
- 36. Paraffin Removal and Antigen Retrieval [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/paraffin-removal-antigen-retrieval.html]
- 37. DISCOVERY ULTRA IHC/ISH research platform [https://diagnostics.roche.com/us/en/products/instruments/discovery-ultra-research.html]
- 38. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOookWhWbYygomairJESoQ3RGPYJ5SolbEHnZQFJaUrCB02B4npuy]
- 39. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOorcPnvoqQIw3Zhf4NzTry5E1B5EOgFzz1DcwroL3h7Rb0wtMFUL]
- 40. And ISH Automated in the Real World: 5 Uses You'll... IHC Stainer [https://www.linkedin.com/pulse/automated-ihc-ish-stainer-real-world-5-uses-youll-actually-15vbc]
- 41. Intro to Immunohistochemistry ( IHC ) Staining : Steps & Best Practices [https://www.leicabiosystems.com/us/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 42. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOorAKsvH0uvlipsmjqJRDoRWiLWr-JafnnHr4uj16rLzQce6o6pl]
- 43. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOorndneOj39Tor-AT9sdmHStb9aAoBrE_oBYuWg4-SJktsKB7IOA]
- 44. Chromogenic Immunohistochemistry (IHC) Paraffin Protocol [https://www.novusbio.com/support/support-by-application/immunohistochemistry-paraffin/protocol.html?srsltid=AfmBOoqWDnoGIfyRbofveT4nZ6bMB9RROTVYMv7WVU10MuCKH-riv5S7]
- 45. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopIRqMgpzFLKc9XbGC_BA_peE4bWd99tH2Cal3b7GGYTeEn3I-j]
- 46. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/?srsltid=AfmBOoq7gcGTChBzC7q2HPt03bKb2OA7ZvsC1nXw083mi7n-1N4UrPSN]
- 47. A Guide to Better IHC Staining: Steps, Troubleshooting, ... [https://www.celnovte.com/solution/a-guide-to-better-ihc-staining-steps-troubleshooting-and-optimization/]
- 48. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOorqoOn0d94K9dgvayUJFw_GEcey0cfIpn_WWr4vgS0s4Xz5XVKS]
- 49. IHC Troubleshooting [https://www.origene.com/research-areas/ihc/ihc-troubleshooting]
- 50. Immunohistochemistry (IHC) Workflow [https://www.rockland.com/resources/immunohistochemistry-workflow/?srsltid=AfmBOopPatE7InSm6F_1vVZjjRyR018LbapmvRST2almLon4YCNHzLyq]
- 51. Paraffin Embedding - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/paraffin-embedding]
- 52. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoo_CpesDRs4FcE5JLqToDIrWA66huUW7aAFCfuJSliYLmGi2kHM]
- 53. Immunohistochemistry-Paraffin Protocol & Troubleshooting [https://www.creativebiolabs.net/immunohistochemistry-paraffin.htm]
- 54. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooY1_ErObPGCHIinrZ3owJqZ1MxobZ043Lcw2bWm5Xq3N4jw_Hi]
- 55. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOop9sf8YSD3Cl5RTRj6jrMFDU6N9JAeXSjTarayHKQBkKzkS57_w]
- 56. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoouwrgmtvHishDTa2JdmDAHP582Kl4L33g4-WuSWkWr5x1cyvHK]
- 57. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 58. IHC (Immunohistochemistry) Procedure + Tips and Precautions [https://www.absin.net/article-1367.html]
- 59. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoqmqaR5pgGBHpbXrGdlRXH5Npq7jpypm-dVwKyUe3iu9kSfqDpQ]
- 60. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOop8bhujx83A0r6O8ObyQXgi5oCoMBZLdfs-z-rfnI1YYUBjLG1z]
- 61. Frequently Asked Questions from Immunohistochemistry ... [https://www.cap.org/member-resources/councils-committees/immunohistochemistry-topic-center/frequently-asked-questions-from-immunohistochemistry-laboratories]
- 62. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/?srsltid=AfmBOoo6NyYdlj4cRw68k8Au8kcShn1rl4xN3jpncCtBPzwFom83Bx81]
- 63. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoq9cRBfjKtKBWEspdC1RzkNcJBarE-G3DAFL6aEpYODjXr281I7]
- 64. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/?srsltid=AfmBOopViHuPSFVzlLUDz5Jo27eWfhtaqicr0c7c4iBOXbVKDqI3YfQM]
- 65. Semi-quantitative Determination of Protein Expression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6924920/]
- 66. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqPB2XkyW_wHP9fCsA-9_5-Syc8QxtM4nt3dpq0qU9lv-KMQy1R]
- 67. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOorvqxwGs0SGSfJ5uGGv-ATF_TKGji-QOjhWcicVIJHvQZpYWBy3]
- 68. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopBrEBJhAQDRdAA4MWqDvsTZieK238TBFuOxRjT-zVJR0Qdx6oC]
- 69. Multicenter Harmonization Study of Pan-Trk ... [https://www.sciencedirect.com/science/article/pii/S0893395223000972]
- 70. A multicenter study directly comparing the diagnostic accuracy ... [https://pubmed.ncbi.nlm.nih.gov/23648464/]
- 71. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoplex1nMEfjua-UXI2YYvSrE4Er0NFWE8fEnViiXURJHRSddWFw]
- 72. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOop7Bm9pQoebKk-FfcreEEf5hm-KEC_xie-BnzknfwD1g3FplE42]
- 73. AI-Assisted High-Throughput Tissue Microarray Workflow [https://pmc.ncbi.nlm.nih.gov/articles/PMC11678066/]