Solving IHC No Staining and Weak Signal: A Complete Troubleshooting Guide for Researchers
This comprehensive guide addresses the pervasive challenge of weak or absent staining in Immunohistochemistry (IHC), a critical technique for researchers and drug development professionals.
Solving IHC No Staining and Weak Signal: A Complete Troubleshooting Guide for Researchers
Abstract
This comprehensive guide addresses the pervasive challenge of weak or absent staining in Immunohistochemistry (IHC), a critical technique for researchers and drug development professionals. It systematically explores the foundational causes of signal failure, provides actionable methodological protocols for optimization, details a step-by-step troubleshooting framework for common pitfalls, and emphasizes the importance of rigorous validation and controls. By synthesizing insights from current best practices, this article equips scientists to diagnose and resolve IHC issues efficiently, saving valuable time and resources while ensuring the reliability of their experimental data for preclinical and biomedical research.
Understanding IHC Signal Failure: Core Principles and Common Culprits
The IHC Workflow and Critical Checkpoints for Signal Generation
Immunohistochemistry (IHC) is an antibody-based technique used to characterize protein expression in tissue while preserving its structural organization [1]. Despite its widespread use in research and clinical diagnostics, IHC experiments are prone to specific technical issues that can compromise results. This guide addresses the most frequent challenges—weak staining, high background, and uneven signal—providing targeted troubleshooting advice to ensure reliable, publication-quality data.
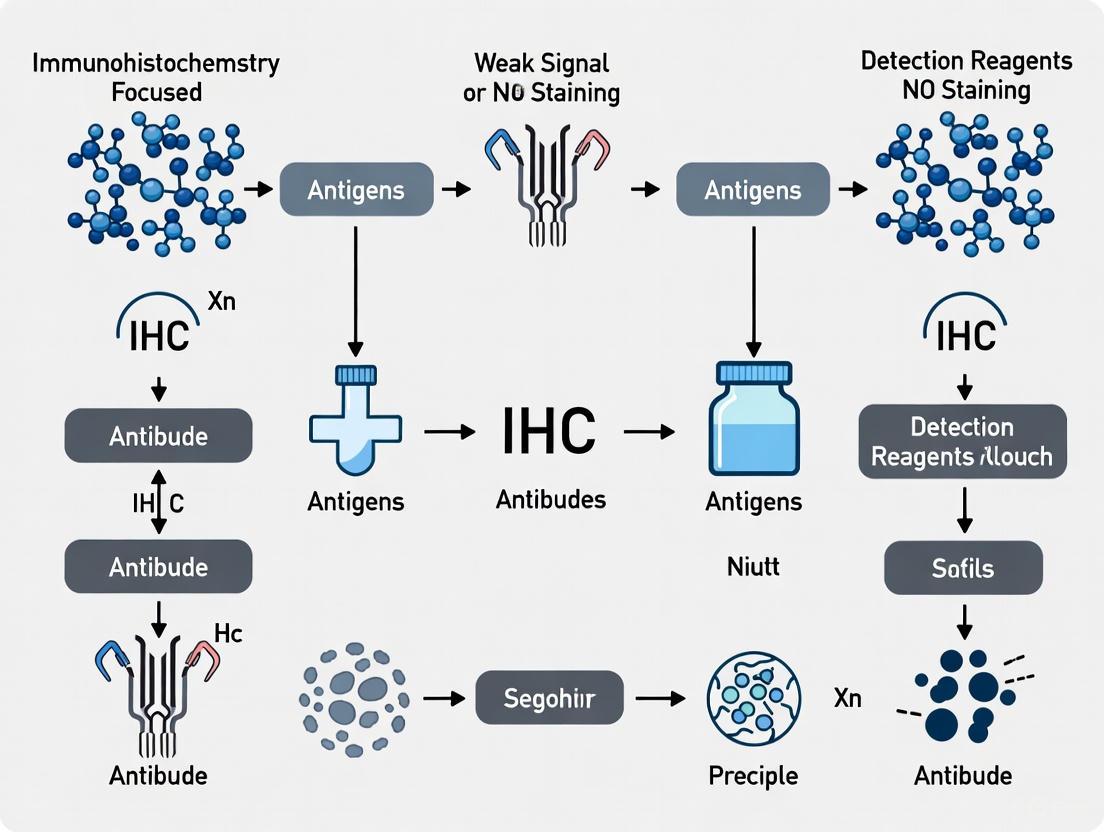
The Complete IHC Workflow: A Visual Guide
The diagram below illustrates the core IHC workflow and pinpoints critical checkpoints where failures most commonly occur.
Frequently Asked Questions & Troubleshooting Guides
FAQ 1: My IHC staining shows no signal or very weak signal. What should I check?
Weak or absent staining is one of the most common problems in IHC. The following table outlines the primary causes and evidence-based solutions.
Table 1: Troubleshooting Guide for No or Weak Staining
| Problem Cause | Recommended Solution | Key Experimental Checkpoints |
|---|---|---|
| Primary Antibody Issues | Confirm antibody is validated for IHC in your specific tissue type (e.g., FFPE). Perform a positive control with a known expressing tissue. Check storage conditions and expiration date [2]. | Always run a positive control tissue. Aliquot antibodies to avoid freeze-thaw cycles [3]. |
| Incorrect Antibody Concentration | Perform a titration experiment. Test a range of dilutions (e.g., 1:50, 1:100, 1:200) starting from the datasheet's recommendation. Increase concentration or incubation time if too dilute [2] [3]. | For CST antibodies, incubate overnight at 4°C as validated [4]. |
| Suboptimal Antigen Retrieval | This is a critical step. Optimize Heat-Induced Epitope Retrieval (HIER): ensure correct buffer (Citrate pH 6.0 or Tris-EDTA pH 9.0), temperature, and incubation time. A microwave oven is often preferred over a water bath [1] [4]. | If retrieval is too harsh, it can destroy the epitope. Optimize incubation length and method [3]. |
| Over-Fixation | Formalin over-fixation can over-mask epitopes. Increase the duration or intensity of antigen retrieval. Standardize fixation time across all samples (typically 2-24 hours for immersion) [5] [2]. | For phosphorylated targets, include phosphatase inhibitors in all buffers to prevent dephosphorylation [3]. |
FAQ 2: How can I reduce high background staining in my IHC experiments?
High background obscures specific signal and makes interpretation difficult. The solutions often involve optimizing blocking and washing steps.
Table 2: Troubleshooting Guide for High Background Staining
| Problem Cause | Recommended Solution | Key Experimental Checkpoints |
|---|---|---|
| High Primary Antibody Concentration | Titrate the antibody to find a lower concentration that maintains signal while reducing noise. This is the most common cause of background [2] [3]. | Decrease incubation time, particularly at room temperature, or perform incubations at 4°C [3]. |
| Insufficient Blocking | Block with normal serum from the secondary antibody host species for 1 hour. For HRP-based detection, quench endogenous peroxidases with 3% H2O2. For biotin-based systems, use an avidin/biotin block [2] [4]. | Use a polymer-based detection system (e.g., SignalStain Boost) instead of biotin-based systems for tissues with high endogenous biotin like liver and kidney [4]. |
| Tissue Drying | Never let tissue sections dry out during the protocol. Perform all incubation steps in a humidified chamber [2] [6]. | |
| Over-Development of Chromogen | Monitor DAB development under a microscope and stop the reaction as soon as specific signal is clear. Typically, this takes about 10 minutes [2]. | |
| Inadequate Washing | Increase wash length and frequency. Wash slides 3 times for 5 minutes with TBST or PBS containing 0.025% Triton X-100 after primary and secondary antibody incubations [7] [4]. | Ensure wash buffers contain a gentle detergent like Tween-20 or Triton X-100 to minimize hydrophobic interactions [2] [7]. |
FAQ 3: What causes uneven or patchy staining, and how can I fix it?
Uneven staining compromises the interpretation and quantification of your results. The causes are often related to reagent application or tissue handling.
Table 3: Troubleshooting Guide for Uneven or Patchy Staining
| Problem Cause | Recommended Solution | Key Experimental Checkpoints |
|---|---|---|
| Inconsistent Reagent Coverage | Ensure antibodies and other reagents fully cover the tissue section throughout incubation. Use a humidified chamber to prevent evaporation and ensure even distribution [2]. | Use a hydrophobic pen to draw a barrier around the section, which helps contain the liquid [7]. |
| Tissue Folding or Poor Adhesion | Check sections under a microscope before staining. Use positively charged, silanized, or gel-coated slides to ensure tissue adherence [2] [7] [3]. | For frozen sections, ensure tissue is dried properly on the slide before freezing or storage [3]. |
| Variable Fixation | Standardize fixation time and conditions for all samples. For immersion fixation, ensure tissue pieces are small (<10 mm) and sufficient time is allowed for full penetration [5] [2]. | Perfusion fixation can provide more uniform fixation than immersion for whole organs [5]. |
| Inadequate Deparaffinization | Spotty background can be caused by poor deparaffinization. Repeat the experiment with new sections and fresh xylene [4]. | Follow a strict rehydration series before immunostaining [7]. |
Essential Research Reagent Solutions
The choice of reagents is fundamental to a successful IHC experiment. The table below details key materials and their functions.
Table 4: Essential IHC Reagents and Their Functions
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Fixatives | Formalin, Paraformaldehyde (PFA), Ethanol, Methanol, Acetone | Preserves tissue integrity and morphology, prevents degradation, and maintains antigenicity. Cross-linking fixatives (aldehydes) provide better morphology but may mask epitopes, while precipitative fixatives (alcohols) better preserve antigenicity but compromise morphology [5]. |
| Antigen Retrieval Buffers | Citrate Buffer (pH 6.0), Tris-EDTA (pH 9.0), EDTA (pH 8.0), Proteases (Trypsin, Pepsin) | Reverses formaldehyde-induced cross-links, "unmasking" epitopes to make them accessible to the primary antibody. The optimal pH and method (HIER vs. PIER) are antibody-dependent [7] [1]. |
| Blocking Agents | Normal Serum, BSA, Commercial Protein Blockers | Reduces non-specific binding of antibodies to the tissue, thereby minimizing background staining. Normal serum from the secondary antibody host is commonly used [7] [4]. |
| Detection Systems | Polymer-based HRP/AP, Avidin-Biotin Complex (ABC), Fluorophore-conjugated secondaries | Amplifies the primary antibody signal for visualization. Polymer-based systems are more sensitive than biotin-based systems and avoid endogenous biotin background [4]. |
| Chromogens/ Fluorophores | DAB (brown), AEC (red), Fluorescein (FITC), Tetramethylrhodamine (TRITC), Alexa Fluor dyes | Generates the visible signal. DAB is a stable, permanent chromogen for brightfield microscopy. Fluorophores are chosen based on their excitation/emission spectra for fluorescence microscopy [5]. |
Detailed Experimental Protocols for Critical Steps
Protocol 1: Antigen Retrieval for FFPE Tissue Sections
Antigen retrieval is a critical, often problematic, step for formalin-fixed tissues. The following HIER protocol is widely applicable.
Heat-Induced Epitope Retrieval (HIER) Protocol [7]:
- Deparaffinize and Rehydrate: Follow standard procedures to bring slides to water.
- Choose Retrieval Buffer: Place slides in a coplin jar filled with retrieval buffer. Common buffers include:
- 10 mM Sodium Citrate, pH 6.0
- 1 mM EDTA, pH 8.0
- 10 mM Tris/1 mM EDTA, pH 9.0
- Heat the Slides: Using a microwave, pressure cooker, or steamer, boil the slides in buffer and maintain the temperature at approximately 98°C for 15-20 minutes. A microwave is generally recommended for best performance with many targets [1] [4].
- Cool the Slides: Allow the slides to cool completely in the buffer at room temperature for 20-30 minutes. This cooling step is essential for stabilizing the unmasked epitopes.
- Rinse and Proceed: Rinse the slides briefly in distilled water or PBS before moving to the immunostaining steps.
Protocol 2: Immunofluorescence Staining for Frozen Sections
This protocol is optimized for frozen tissue sections, a common preparation method for labile antigens.
Fluorescence-conjugated Antibody Staining [7] [6]:
- Fixation: Fix air-dried frozen sections in ice-cold acetone for 10 minutes.
- Rehydration & Permeabilization: Wash slides in PBS for 10 min. Permeabilize by incubating with wash buffer (PBS + 0.025% Triton X-100) for 10 minutes.
- Blocking: Incubate sections with a blocking buffer (e.g., 10% normal serum from the secondary antibody species in PBS) for 1 hour at room temperature in a humidified chamber. It is critical that the tissue does not dry out from this point forward.
- Primary Antibody: Dilute the primary antibody in blocking buffer. Apply to the tissue and incubate overnight at 4°C in a humidified chamber.
- Wash: Wash slides 3 times in wash buffer for 10 minutes each.
- Secondary Antibody: Dilute the fluorophore-conjugated secondary antibody in blocking buffer (typically 1:500-1:1000). Apply to the tissue and incubate for 1-2 hours at room temperature, protected from light.
- Wash and Counterstain: Wash slides 3 times for 10 minutes each. If desired, incubate with DAPI (0.5 μg/mL) for 5 minutes to stain nuclei, followed by a final 5-minute wash.
- Mounting: Rinse in dH2O, apply an anti-fade mounting medium, and coverslip. Seal the edges with nail polish and store at 4°C protected from light until imaging.
Frequently Asked Questions
1. What are the most common antibody-related causes of weak or no staining in IHC? The most common causes include using an antibody that is not validated for IHC or your specific application (e.g., FFPE tissue), incorrect antibody concentration (too dilute or, less commonly, too concentrated), loss of antibody potency due to improper storage or excessive freeze-thaw cycles, and insufficient antigen retrieval that prevents antibody access to the epitope [8] [2] [9].
2. How can I confirm that my primary antibody is specific for my target antigen? A key step is to run a positive control—a tissue known to express the target antigen—alongside your experiment. If the positive control stains correctly, your antibody is likely specific. If it does not, the antibody or protocol is at fault. For further validation, use a knockout tissue or cell line, or pre-absorb the antibody with its immunizing peptide; a specific signal should be greatly reduced or eliminated [8] [2] [10].
3. What is the best way to store antibodies to maintain their potency? Follow the manufacturer's storage instructions carefully. For long-term storage, divide the antibody into small, single-use aliquots to avoid repeated freeze-thaw cycles, which can cause denaturation. Store aliquots at the recommended temperature, typically -20°C or below. Always wear gloves and use sterile pipette tips when handling antibodies to prevent microbial contamination [9] [8].
4. Why is there high background staining even on my negative control slide? High background on a negative control slide (incubated without the primary antibody) indicates that the secondary antibody is binding non-specifically to the tissue. This can happen due to endogenous enzymes, endogenous biotin (if using a biotin-based detection system), or cross-reactivity. Use a secondary antibody that has been pre-adsorbed against the immunoglobulin of your sample species, and ensure thorough blocking and washing steps [8] [9] [11].
Antibody Types and Characteristics
The type of antibody you choose has a significant impact on the specificity, sensitivity, and overall success of your IHC experiment [10].
Table: Comparison of Common Antibody Types Used in IHC
| Antibody Type | Production | Advantages | Disadvantages |
|---|---|---|---|
| Conventional Polyclonal | Immunization with a large protein; contains a mix of antibodies against multiple epitopes [10]. | High affinity and signal amplification due to binding multiple epitopes; more tolerant of antigen variation and denaturation; stable over broad pH/salt conditions [10]. | Greater risk of cross-reactivity and high background; potential for batch-to-batch variability [10]. |
| Monoclonal | Generated from a single hybridoma cell line; recognizes one specific epitope [10]. | A renewable, consistent source with high reproducibility; generally lower background due to single specificity [10]. | Often lower affinity, requiring careful washing; highly susceptible to changes in pH/salt concentration; may not recognize epitopes altered by fixation [10]. |
| Monotypic (Anti-Peptide) | Immunization with a small synthetic peptide; polyclonal but against a single epitope [10]. | Can be tailored to specific protein domains; production is relatively quick and easy [10]. | Often has lower affinity, similar to monoclonals; risk of cross-reactivity if the peptide sequence is not unique [10]. |
Troubleshooting Antibody-Related Problems
Systematically investigating antibody-related factors is crucial for resolving IHC issues. The following workflow outlines a logical approach to diagnosing and fixing common problems.
Diagram: A logical workflow for troubleshooting antibody-related IHC problems.
Problem: No Staining or Very Weak Signal
Table: Causes and Solutions for Weak/No Staining
| Cause | Solution | Experimental Protocol Consideration |
|---|---|---|
| Incorrect Antibody Concentration [2] | Perform a titration experiment. Test a series of primary antibody dilutions (e.g., 1:50, 1:100, 1:200, 1:500) on positive control tissue to find the optimal concentration [2]. | Incubate primary antibody overnight at 4°C in a humidified chamber for optimal binding [8] [7]. |
| Loss of Antibody Potency [9] | Use a positive control to verify activity. Aliquot antibodies for storage to minimize freeze-thaw cycles. Check expiration dates [9] [2]. | Ensure antibody diluent pH is between 7.0 and 8.2 for optimal binding. Avoid buffers containing sodium azide with HRP-conjugated antibodies [9]. |
| Insufficient Antigen Retrieval [8] [2] | Optimize Heat-Induced Epitope Retrieval (HIER). Test different buffers (e.g., citrate pH 6.0, Tris-EDTA pH 9.0) and heating methods (microwave, pressure cooker). For over-fixed tissue, increase retrieval time [8] [2]. | For FFPE tissue, deparaffinize and rehydrate slides first. Cool slides completely after HIER before proceeding to immunostaining [7] [12]. |
| Incompatible or Inactive Detection System [8] [9] | Verify secondary antibody compatibility and activity. Use polymer-based detection systems for enhanced sensitivity over biotin-based systems [8]. | For HRP-based detection, quench endogenous peroxidase activity by incubating slides in 3% Hâ‚‚Oâ‚‚ for 10 minutes prior to primary antibody incubation [8] [7]. |
Problem: High Background Staining
Table: Causes and Solutions for High Background
| Cause | Solution | Experimental Protocol Consideration |
|---|---|---|
| Primary Antibody Concentration Too High [9] [2] | Titrate the primary antibody to find a lower concentration that provides specific signal with minimal background [9] [8]. | Dilute the primary antibody in a specialized antibody diluent or a buffer containing 1-5% normal serum and 0.025-0.05% detergent [9] [7]. |
| Secondary Antibody Cross-Reactivity [9] [8] | Use a secondary antibody that is pre-adsorbed against the immunoglobulin of the sample species. Always include a no-primary control [8] [11]. | Block nonspecific binding by incubating tissue with 5-10% normal serum from the species of the secondary antibody for 30-60 minutes at room temperature [9] [12]. |
| Endogenous Enzymes or Biotin [9] [8] | For HRP: block with 3% Hâ‚‚Oâ‚‚. For biotin: use a commercial avidin/biotin blocking kit or switch to a polymer-based detection system [9] [8] [13]. | Perform endogenous enzyme blocking after antigen retrieval and before applying the primary antibody [7] [14]. |
| Hydrophobic/ Ionic Interactions [9] [2] | Add a detergent like 0.05% Tween-20 to wash and antibody dilution buffers. For ionic interactions, add NaCl (0.15-0.6 M) to the antibody diluent [9]. | Wash slides thoroughly 3 times for 5 minutes each with a buffer like TBST or PBST after primary and secondary antibody incubations [8] [7]. |
The Scientist's Toolkit: Key Research Reagent Solutions
Having the right reagents is fundamental to successful IHC. The following table details essential solutions for addressing antibody-related issues.
Table: Essential Reagents for IHC Troubleshooting
| Reagent / Solution | Function | Application Note |
|---|---|---|
| Sodium Citrate Buffer (10 mM, pH 6.0) | A common buffer for Heat-Induced Epitope Retrieval (HIER) to unmask antigens in FFPE tissue [9] [7]. | Used in a microwave, pressure cooker, or water bath. Tris-EDTA (pH 9.0) is an alternative for certain targets [8] [12]. |
| Normal Serum | Used as a blocking agent to reduce non-specific binding of secondary antibodies. Should be from the same species as the secondary antibody [9] [12]. | A typical protocol is a 30-60 minute incubation at room temperature with 5-10% serum in buffer prior to primary antibody application [7] [8]. |
| Enzyme Blockers (3% Hâ‚‚Oâ‚‚) | Quenches endogenous peroxidase activity to prevent high background when using HRP-based detection systems [8] [9] [14]. | Incubate slides for 10-15 minutes at room temperature after antigen retrieval and before blocking [8] [7]. |
| Antibody Diluent | A optimized solution for diluting antibodies, often containing protein stabilizers and blockers of non-specific binding [8] [2]. | Superior to simple buffers like PBS. Using the manufacturer's recommended diluent can significantly improve signal-to-noise ratio [8]. |
| Polymer-Based Detection System | A sensitive detection method where multiple enzyme and secondary antibody molecules are conjugated to a polymer backbone. It replaces older biotin-avidin systems [8]. | Provides enhanced sensitivity and reduces background from endogenous biotin, which is found in tissues like liver and kidney [8]. |
| Gcase activator 3 | Gcase activator 3, MF:C23H20N4O2, MW:384.4 g/mol | Chemical Reagent |
| Ret-IN-9 | Ret-IN-9, MF:C26H27N9O, MW:481.6 g/mol | Chemical Reagent |
Essential Protocols for Validation and Titration
Experimental Protocol: Antibody Titration for Optimal Signal
- Sectioning: Cut consecutive sections from a positive control FFPE tissue block known to express your target [2].
- Deparaffinization and Antigen Retrieval: Process all slides simultaneously through deparaffinization and a standardized HIER protocol [7] [12].
- Blocking: Block all sections with an appropriate protein block (e.g., 5% normal serum) and any necessary enzyme blockers [8] [13].
- Primary Antibody Incubation: Prepare a series of primary antibody dilutions (e.g., 1:50, 1:100, 1:200, 1:500) in the recommended diluent. Apply each dilution to a separate section and incubate overnight at 4°C [8] [2].
- Detection and Analysis: Process all slides with the same detection system and development time. Examine under a microscope to identify the dilution that gives the strongest specific signal with the cleanest background [2].
Experimental Protocol: Verification of Antibody Specificity
- Positive Control: Always include a tissue known to express the target protein in every experiment. This validates that the entire IHC protocol is functioning correctly [8] [9].
- Negative Control: Run a duplicate of your test tissue where the primary antibody is omitted or replaced with a non-immune immunoglobulin from the same species. This identifies non-specific binding from the secondary antibody or detection system [12] [8].
- Adsorption Control (Peptide Blocking): Pre-incubate the primary antibody with a 5-10 fold molar excess of the immunizing peptide for 1-2 hours at room temperature. Then, use this pre-adsorbed antibody for IHC. A significant reduction or loss of staining compared to the standard protocol strongly indicates antibody specificity [10].
In the context of a broader thesis on troubleshooting no staining and weak signals in immunohistochemistry (IHC) research, proper sample preparation emerges as the most critical determinant of success. This initial phase establishes the foundation for all subsequent steps, and failures here are often the root cause of experimental failure. For researchers and drug development professionals, understanding that a significant proportion of IHC problems originate from pre-analytical variables is essential [15]. This guide addresses the major pitfalls in fixation, tissue processing, and the management of epitope masking, providing targeted solutions to preserve antigenicity and ensure reliable, reproducible results.
Frequently Asked Questions (FAQs)
FAQ 1: How does the time between tissue resection and fixation impact my IHC results? Prolonged ischemia time between tissue resection and fixation initiates protein degradation, autolysis, and enzyme activation, leading to a significant loss of antigenicity [15]. This is particularly crucial for labile antigens such as phospho-proteins and Ki-67, where delays can drastically alter staining outcomes for key biomarkers like estrogen receptor, progesterone receptor, and HER2 [15]. Rapid fixation is essential to preserve the native state of these targets.
FAQ 2: What are the consequences of over-fixation, and how can I avoid it? While under-fixation causes poor morphology and antigen loss, over-fixation, typically with formalin beyond 24-48 hours, creates excessive protein cross-links that can permanently mask epitopes [15] [2] [16]. This makes antigens inaccessible to antibodies, even with aggressive antigen retrieval. The solution is to standardize fixation in 10% Neutral Buffered Formalin (NBF) for a consistent, recommended duration of 24 hours at room temperature, ensuring a proper tissue-to-fixative volume ratio of 1:10 to 1:20 [15] [16].
FAQ 3: Why is my antigen retrieval inconsistent, and how can I optimize it? Inconsistency often arises from using a suboptimal method or buffer for your specific antibody-epitope pair. The fixation process forms methylene bridges that cross-link proteins, physically obscuring the epitope from antibody binding [15]. Heat-Induced Epitope Retrieval (HIER) is designed to break these cross-links. Optimization requires empirical testing of different retrieval buffers (e.g., citrate at pH 6.0 vs. Tris-EDTA at pH 9.0) and heating methods (microwave, pressure cooker, water bath) to find the most effective combination for unmasking your target [9] [15] [17].
Troubleshooting Guides
Troubleshooting Fixation & Processing Problems
Fixation and processing set the stage for successful staining. The table below outlines common pitfalls and their solutions.
Table 1: Troubleshooting Guide for Fixation and Tissue Processing
| Problem | Primary Cause | Recommended Solution | Preventive Measure |
|---|---|---|---|
| Weak/No Staining | Prolonged Ischemia: Antigen degradation prior to fixation [15]. | Compare staining with a rapidly fixed control sample. | Fix tissue immediately after dissection; for large specimens, slice into thin sections to ensure rapid penetrance [15] [3]. |
| Epitope Masking | Over-fixation: Excessive cross-linking from extended formalin exposure [15] [2]. | Increase the duration or intensity of antigen retrieval (e.g., use a pressure cooker) [2]. | Standardize fixation time to 24 hours in 10% NBF for all samples [15]. |
| Poor Morphology & Antigen Loss | Under-fixation or use of inappropriate fixative [3]. | For soluble antigens, switch to a cross-linking fixative like formalin [3]. | Use 10% NBF and ensure adequate tissue-to-fixative volume ratio (1:10 to 1:20) [15]. |
| High Background & Artifacts | Incomplete Deparaffinization or tissue drying during processing [17] [16]. | Repeat staining with new sections and fresh xylene for deparaffinization [17] [16]. | Perform all incubation steps in a humidified chamber to prevent sections from drying out [2] [16]. |
Troubleshooting Epitope Masking & Antigen Retrieval
Even with perfect fixation, epitope masking is common in FFPE tissues. The following workflow diagram illustrates the logic and options for resolving epitome masking issues.
When troubleshooting, the first decision point is whether the tissue was formalin-fixed. If not, antigen retrieval may be unnecessary. For formalin-fixed tissues, HIER is the primary method, and optimization involves testing different buffers and heating modalities. If HIER fails, Protease-Induced Epitope Retrieval (PIER) is an alternative pathway for certain antigens [15] [16].
Table 2: Troubleshooting Antigen Retrieval for Epitope Masking
| Symptom | Possible Reason | Solution & Experimental Protocol |
|---|---|---|
| Complete Lack of Staining | Ineffective or no antigen retrieval for a tightly masked epitope [18]. | Protocol: Perform HIER using 10 mM sodium citrate buffer (pH 6.0). Heat in a microwave for 8-15 minutes or a pressure cooker for 20 minutes. Allow slides to cool in buffer for 20-30 minutes before proceeding [9] [15]. |
| Persistent Weak Signal | Suboptimal retrieval conditions for the specific antibody [3] [17]. | Protocol: Empirically test multiple retrieval buffers. Compare citrate (pH 6.0) against Tris-EDTA (pH 9.0). Use a pressure cooker for 10-20 minutes, as it often provides stronger signal than a microwave for difficult targets [17]. |
| Destroyed Morphology / No Signal | Overly harsh retrieval has destroyed the epitope or tissue architecture [3]. | Protocol: Optimize by reducing heating time or switching to a milder method. Try a water bath at a lower temperature (e.g., 90-95°C for 30 minutes) or a shorter protease incubation (e.g., trypsin for 10 min at 37°C) [15] [3]. |
| Inconsistent Staining Between Runs | Variable retrieval due to inconsistent heating or old buffer [17]. | Protocol: Standardize the process. Use a pressure cooker for even heating. Always prepare fresh 1X retrieval solution daily and ensure slides are fully submerged in the same volume of buffer for every run [17]. |
The Scientist's Toolkit: Key Research Reagents
The following reagents are essential for overcoming sample preparation challenges.
Table 3: Essential Reagents for Managing Sample Preparation Pitfalls
| Reagent | Function in Sample Preparation | Specific Application Note |
|---|---|---|
| 10% Neutral Buffered Formalin (NBF) | Standard cross-linking fixative that preserves morphology and stabilizes proteins for long-term storage [15]. | The gold standard for FFPE tissues. Avoid over-fixation beyond 24-48 hours to prevent severe epitope masking [15]. |
| Sodium Citrate Buffer (pH 6.0) | A common low-pH buffer for Heat-Induced Epitope Retrieval (HIER) [9]. | Ideal for many targets. Compare with high-pH buffers (e.g., Tris-EDTA, pH 9.0) empirically for optimal results [2]. |
| Tris-EDTA Buffer (pH 9.0) | A common high-pH buffer for HIER, effective for a different set of masked epitopes [2]. | Often superior for nuclear antigens and some phosphorylated epitopes [2]. |
| Proteinase K / Trypsin | Enzymes for Protease-Induced Epitope Retrieval (PIER), which digests proteins to expose epitopes [15]. | Use for specific antigens where HIER fails (e.g., some immunoglobulins). Incubation time and concentration must be tightly controlled to avoid tissue damage [15]. |
| Triton X-100 | A detergent used for permeabilizing cell membranes, especially in frozen sections or for intracellular targets [16] [19]. | Add at 0.1-0.5% to wash and/or blocking buffers to aid antibody penetration, particularly for nuclear proteins [16] [19]. |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) | Blocks endogenous peroxidase activity, which causes high background in HRP-based detection systems [9] [15]. | Incubate sections with 3% Hâ‚‚Oâ‚‚ in methanol or water for 10-15 minutes at room temperature prior to primary antibody incubation [9] [17]. |
| Wee1-IN-7 | Wee1-IN-7, MF:C28H28N10O, MW:520.6 g/mol | Chemical Reagent |
| Autophagy inducer 2 | Autophagy inducer 2, MF:C41H58N6O, MW:650.9 g/mol | Chemical Reagent |
The Critical Role of Antigen Retrieval in Unmasking Epitopes
â– FAQs on Antigen Retrieval and Epitope Unmasking
1. Why is antigen retrieval a critical step in IHC? Formalin or paraformaldehyde fixation creates methylene bridges that cross-link proteins, masking antigenic epitopes and making them inaccessible to antibodies [12]. Antigen retrieval reverses these cross-links, thereby unmasking the epitopes and restoring the antibody's ability to bind to its target [12]. Without this step, staining may be weak or absent even if the target antigen is present [20].
2. My IHC staining is weak or absent, even though my positive control worked. Could the problem be antigen retrieval? Yes, this is a common cause. Suboptimal antigen retrieval is a frequent source of weak or absent staining [21] [20] [2]. Issues can include:
- Insufficient Retrieval Intensity: The heating time or temperature during Heat-Induced Epitope Retrieval (HIER) may be too low to fully unmask the epitope [2].
- Incorrect Buffer pH: The optimal pH of the retrieval buffer (e.g., citrate at pH 6.0 vs. Tris-EDTA at pH 9.0) is highly antigen-dependent [21] [2].
- Over-fixation of Tissue: Prolonged fixation can over-cross-link tissues, requiring a more aggressive retrieval protocol [2].
3. What are the main methods of antigen retrieval, and how do I choose? The two primary methods are Heat-Induced Epitope Retrieval (HIER) and Protease-Induced Epitope Retrieval (PIER). The choice depends on the specific antibody and target antigen [12] [20].
Table: Comparison of Antigen Retrieval Methods
| Method | Type | Mechanism | Common Uses & Considerations |
|---|---|---|---|
| HIER | Physical/Chemical | Uses heat and buffer to break protein cross-links [12]. | Most commonly used; provides good tissue morphology [12]. |
| Microwave Oven | HIER | Heats buffer to ~100°C [12]. | Preferred method for many targets; provides a good balance of performance and convenience [21]. |
| Pressure Cooker | HIER | Heats buffer above 100°C. | Can enhance signals beyond microwave for some stubborn antigens [21]. |
| Water Bath | HIER | Heats buffer below 100°C. | Not generally recommended; can result in weaker staining [21]. |
| PIER | Chemical | Uses enzymes (e.g., proteases) to digest proteins and expose epitopes [12]. | For epitopes that may lose antigenicity with heat; may destroy some epitopes and compromise tissue morphology [12]. |
4. How can I optimize my antigen retrieval protocol? Optimization is often necessary for best results. Key variables to test include [21] [22] [2]:
- Buffer pH: Test a citrate-based buffer (pH 6.0) and a Tris-EDTA-based buffer (pH 9.0).
- Heating Method: Compare microwave and pressure cooker performance for your specific antibody.
- Heating Time: Optimize incubation time at the retrieval temperature. Always refer to the primary antibody's datasheet for a recommended starting protocol [21] [22].
5. Can antigen retrieval cause high background staining? While typically associated with weak staining, improper antigen retrieval can contribute to background issues. Overly aggressive retrieval can damage tissue morphology and increase non-specific antibody binding. If high background appears after changing the retrieval protocol, titrate the retrieval time or temperature downward [9] [20].
â– Antigen Retrieval Troubleshooting Guide
Table: Troubleshooting Weak or No Staining Related to Antigen Retrieval
| Problem | Possible Cause | Solution |
|---|---|---|
| No Staining | Complete failure to unmask the epitope due to incorrect retrieval method or buffer. | Use a positive control tissue. Switch the retrieval buffer pH (e.g., from pH 6.0 to 9.0) or method (e.g., from microwave to pressure cooker) [21] [2]. |
| Weak Staining | Partial or insufficient epitope unmasking. | Increase the duration or intensity of HIER [20] [2]. Ensure retrieval buffer is fresh and slides are fully submerged [21]. |
| Patchy Staining | Inconsistent retrieval across the tissue section. | Ensure the slide is fully submerged in retrieval buffer and that the container is properly placed in the heating unit to ensure even heating [2]. |
| Tissue Damage | Overly aggressive retrieval (especially with PIER). | For HIER, reduce heating time. For PIER, reduce enzyme concentration and/or incubation time [12] [20]. |
â– Antigen Retrieval Workflow and Decision Pathway
The following diagram illustrates the logical workflow for establishing and troubleshooting an antigen retrieval protocol.
â– The Scientist's Toolkit: Key Reagents and Equipment for Antigen Retrieval
Table: Essential Research Reagent Solutions for Antigen Retrieval
| Item | Function & Application |
|---|---|
| Sodium Citrate Buffer (10mM, pH 6.0) | A common, mildly acidic retrieval buffer suitable for a wide range of antigens [9] [12]. |
| Tris-EDTA Buffer (pH 9.0) | A common, alkaline retrieval buffer often used for more challenging antigens or when citrate buffer fails [2]. |
| Proteinase K | An enzyme used for Protease-Induced Epitope Retrieval (PIER), necessary for certain epitopes that are sensitive to heat [12] [20]. |
| Microwave Oven or Pressure Cooker | Standard equipment for performing Heat-Induced Epitope Retrieval (HIER). Pressure cookers can often retrieve more stubborn antigens due to higher achievable temperatures [12] [21]. |
| Charged or Adhesion Slides | Microscope slides coated to promote tissue adhesion, preventing sections from detaching during the rigorous heating and washing steps of antigen retrieval [12]. |
| Humidity Chamber | A sealed container that maintains a humid environment during incubation steps to prevent tissue sections from drying out, which can cause high, uneven background [2]. |
| p53 Activator 10 | p53 Activator 10, MF:C26H28F3N5O2S, MW:531.6 g/mol |
| Piperlactam S | Piperlactam S, CAS:188546-49-8, MF:C17H13NO4, MW:295.29 g/mol |
FAQ: Addressing Common Detection System Problems
1. My IHC experiment shows no signal, even though I confirmed my primary antibody is good. Could the problem be with my detection system?
Yes, this is a common issue. An inactive detection system is a frequent cause of no or weak staining [2]. To troubleshoot, first verify that your enzyme and substrate are reacting properly. You can perform a simple test: place a drop of the enzyme (e.g., HRP) onto a piece of nitrocellulose and then immediately dip it into the prepared substrate. A colored spot should form if they are reacting correctly [9]. Furthermore, ensure you are not using a buffer incompatible with your enzyme, such as sodium azide with HRP systems or phosphate buffer with AP systems [23].
2. I am getting a high background with my HRP-based detection. What are the potential causes and solutions?
High background can stem from several sources related to the detection system. A common cause is endogenous enzyme activity; for example, endogenous peroxidases in the tissue can produce signal even in the absence of your primary antibody [9] [24]. To resolve this, quench slides in a 3% Hâ‚‚Oâ‚‚ solution for about 10 minutes before applying the primary antibody [24]. If you are using a biotin-based detection system (like ABC), high levels of endogenous biotin in tissues such as kidney and liver can also cause background. Switching to a polymer-based detection system or using an avidin/biotin blocking kit can mitigate this [9] [24].
3. The staining in my fluorescent IHC experiment is obscured by high background autofluorescence. How can I reduce this?
Autofluorescence is a common challenge in fluorescent IHC [9] [2]. This can be inherent to the tissue (e.g., from lipofuscin in aged tissue) or induced by aldehyde-based fixatives like formalin [3] [2]. Several strategies can help:
- Chemical Quenching: Treat the tissue sample with autofluorescence quenching reagents such as Sudan Black B, pontamine sky blue, or trypan blue before imaging [9] [2].
- Fixative Reduction: If aldehyde fixation is the cause, you can treat the sample with ice-cold sodium borohydride (1 mg/mL) in PBS or TBS [9].
- Fluorophore Selection: Choose fluorescent markers that emit in the red or near-infrared wavelengths (e.g., Alexa Fluor 647, Alexa Fluor 750), as these are less affected by the common green spectral range of tissue autofluorescence [9] [3].
Troubleshooting Guide: Weak or No Staining
The following table outlines common detection system failures that lead to weak or no staining and provides actionable solutions.
| Possible Cause | Specific Issue | Recommended Solution |
|---|---|---|
| Inactive Enzyme or Substrate | Enzyme conjugate has lost activity; substrate is degraded or prepared incorrectly [2]. | Test enzyme and substrate activity separately with a positive control or a spot test on nitrocellulose [9]. Use fresh aliquots of substrate and check expiration dates. |
| Buffer Incompatibility | Using sodium azide in buffers with HRP, as azide inhibits HRP activity [9] [23]. Using phosphate buffer with Alkaline Phosphatase (AP) systems [23]. | Prepare fresh buffers without sodium azide for HRP-based systems. Use Tris-based buffers instead of phosphate buffers for AP systems [23]. |
| Suboptimal Substrate pH | The pH of the substrate buffer is inappropriate for the specific enzyme-substrate reaction, impairing precipitate formation [9]. | Prepare the substrate at the proper pH specified by the manufacturer. Ensure deionized water used in buffers does not contain peroxidase inhibitors [9] [23]. |
| Insufficient Signal Amplification | The detection system (e.g., standard HRP-conjugated secondary) is not sensitive enough for the target abundance [24]. | Switch to a more sensitive detection system, such as a polymer-based system which offers enhanced sensitivity compared to avidin-biotin or direct conjugate systems [24]. |
| Over-fixation or Masked Epitopes | Chemical crosslinks from formalin fixation prevent antibody access, and antigen retrieval is insufficient for the detection system to work [24] [2]. | Optimize antigen retrieval conditions (method, buffer, time, and temperature) to effectively unmask the epitope [24] [2]. |
Experimental Protocol: Verification of Enzyme-Substrate Functionality
Purpose: To confirm that the enzyme (e.g., HRP) and its chromogenic substrate (e.g., DAB) are active and reacting properly, ruling them out as the source of a no-signal problem.
Materials:
- Enzyme-conjugated antibody (e.g., HRP-conjugated secondary antibody)
- Chromogenic substrate (e.g., DAB solution)
- Piece of nitrocellulose membrane
- Pipette and tips
Methodology:
- Prepare the substrate solution according to your standard protocol.
- Pipette a single drop of the enzyme-conjugated antibody directly onto the dry nitrocellulose membrane.
- Immediately dip the membrane, with the antibody drop, into the prepared substrate solution.
- Observe the membrane for the rapid formation of a colored spot at the location of the enzyme drop.
Interpretation:
- Positive Result: A colored spot forms, confirming that both the enzyme and substrate are active and compatible.
- Negative Result: No color develops, indicating a failure in either the enzyme conjugate, the substrate, or the buffer used. You should then test components individually (e.g., test a new vial of substrate with a known active enzyme) to identify the failed reagent [9].
Experimental Workflow for Detection System Troubleshooting
The following diagram outlines a logical workflow for diagnosing and resolving detection system failures in IHC experiments.
The Scientist's Toolkit: Research Reagent Solutions
This table details key reagents used to prevent and resolve enzyme and substrate issues in IHC.
| Reagent | Function | Key Consideration |
|---|---|---|
| Polymer-Based Detection Reagents | More sensitive than avidin/biotin-based systems; avoids background from endogenous biotin [24]. | Ideal for low-abundance targets and tissues with high endogenous biotin (e.g., liver, kidney). |
| HRP Blockers (e.g., 3% Hâ‚‚Oâ‚‚) | Quenches endogenous peroxidase activity to reduce high background [9] [24]. | Essential for HRP-based systems; incubate for 10-15 minutes at room temperature before primary antibody. |
| Biotin/Avidin Blocking Kits | Blocks endogenous biotin and avidin to prevent nonspecific staining in ABC methods [9] [24]. | Use when a polymer system is not an option and you are working with biotin-rich tissues. |
| Optimized Antibody Diluent | A ready-to-use solution with the correct pH and carrier proteins to maintain antibody and enzyme stability [24]. | Prevents issues related to improper pH or ionic strength that can impede antibody binding or enzyme activity [9]. |
| Fresh Substrate Kits (e.g., DAB) | Provides fresh, active chromogen and buffer for the enzyme reaction, ensuring optimal signal generation [24]. | Always check the expiration date and protect from light; development time should be monitored under a microscope to prevent over-staining [2]. |
| Crenulatin | Crenulatin, MF:C11H20O6, MW:248.27 g/mol | Chemical Reagent |
| Hdac6-IN-52 | Hdac6-IN-52, MF:C23H17F2N5O3, MW:449.4 g/mol | Chemical Reagent |
Optimized IHC Protocols to Prevent and Resolve Weak Staining
The Scientist's Toolkit: Essential Reagents for IHC Specimen Preparation
The following reagents are fundamental for successful specimen preparation and fixation in immunohistochemistry (IHC).
| Reagent | Function & Application |
|---|---|
| Paraformaldehyde (PFA) [7] [25] | A cross-linking fixative that preserves tissue morphology by creating methylene bridges between proteins. It is the most common fixative for IHC, ideal for preserving small peptides and enzymes [26]. |
| Formalin [5] [25] | A liquid containing 37-40% formaldehyde, commonly used as a 10% solution (equivalent to ~4% PFA) for perfusion and immersion fixation [5]. |
| Methanol & Ethanol [5] [26] | Precipitative fixatives that dehydrate tissues and precipitate proteins. They are often used for frozen sections and are preferred for large or nuclear proteins [26]. |
| Acetone [26] [25] | A strong dehydrating agent that causes irreversible precipitation of proteins. It is typically used on unfixed, snap-frozen tissues [25]. |
| OCT Compound [7] | An embedding medium used to support tissue structure during cryosectioning of frozen tissue samples. |
| Sucrose (in PBS) [7] | A cryoprotectant used to permeate tissues before freezing, preventing the formation of destructive ice crystals during the freezing process. |
| Citrate, EDTA, and Tris-EDTA Buffers [7] | Common buffers used for Heat-Induced Epitope Retrieval (HIER) to reverse the cross-links formed by aldehyde fixation and unmask epitopes. |
| Andropanolide | Andropanolide, MF:C20H30O5, MW:350.4 g/mol |
| Conduritol A | Conduritol A, MF:C20H32O6, MW:368.5 g/mol |
Foundational Concepts: Fixation Principles and Selection
What is the primary goal of fixation in IHC? Fixation preserves tissue morphology and prevents proteolytic degradation. Crucially, it must retain the antigenicity of the target molecules, enabling antibodies to bind to their specific epitopes. A balance must be struck, as under-fixation leads to tissue degradation, while over-fixation can mask epitopes through excessive cross-linking [5] [25].
How do I choose the right fixative for my antigen? The choice of fixative is critical and depends on the nature of your target antigen. The table below provides a guide for selecting a fixative based on your experimental needs [26].
| Antigen Type | Recommended Fixative |
|---|---|
| Low molecular weight peptides, enzymes | 4% Paraformaldehyde |
| Large or delicate tissues, meiotic chromosomes | Bouin's Fixative |
| Large proteins, nuclear/compartmentalized proteins | Acetone or Methanol |
Diagram: IHC Specimen Preparation Workflow. This flowchart outlines the key decision points for preparing tissue samples for IHC analysis.
Detailed Protocols for Specimen Preparation
Protocol 1: Preparation of Frozen Tissue Sections (Snap-Freezing Followed by Fixation)
This protocol is ideal for preserving labile antigens, such as phosphorylated proteins [7] [3].
- Dissection & Embedding: Dissect tissue (<10 mm in size) and place it in a pre-labeled tissue mold. Cover the tissue completely with cryo-embedding media (OCT) [7].
- Snap-Freezing: Freeze the tissue block by slowly submerging it in liquid nitrogen or placing it on dry ice. Store the frozen block at -80°C until sectioning [7].
- Sectioning: Equilibrate the tissue block in a cryostat set at -20°C for 15 minutes. Section the block into 6–15 μm thick slices and transfer them onto positively charged glass slides [7].
- Fixation: Air-dry slides briefly, then fix sections in ice-cold acetone for 10 minutes. Acetone fixation is common for frozen sections as it precipitates proteins without requiring antigen retrieval [7] [25].
- Storage: Wash slides in PBS and store at -80°C for several months [7].
Protocol 2: Preparation of Formalin-Fixed, Paraffin-Embedded (FFPE) Tissue Sections
FFPE provides excellent morphological detail and is the standard for clinical archives. However, the process requires reversing formalin-induced cross-links through antigen retrieval [7] [27].
- Fixation: Fix tissue via perfusion or immersion in 4% paraformaldehyde for 2–24 hours at 4°C or room temperature [7].
- Dehydration: Rinse tissue in PBS, then dehydrate in a graded series of ethanol solutions (50%, 70%, 80%, 95%, 100%) [7].
- Clearing & Infiltration: Clear the tissue in xylene, then infiltrate with molten paraffin wax [7].
- Embedding & Sectioning: Embed tissue in a paraffin block. Section the block into 5–15 μm slices using a microtome and transfer sections to coated glass slides [7].
- Deparaffinization & Rehydration: Before staining, deparaffinize slides in xylene and rehydrate through a descending ethanol series to water [7].
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER). Boil slides in 10 mM sodium citrate buffer (pH 6.0) for 20 minutes, then allow them to cool completely [7] [27].
Frequently Asked Questions (FAQs) & Troubleshooting
Q: My IHC staining shows no signal or a very weak signal. Could this be related to specimen preparation? A: Yes, this is a common problem often stemming from the preparation and fixation steps [2].
- Cause 1: Over-fixation. Excessive cross-linking from prolonged formalin fixation can mask epitopes [2] [25].
- Cause 2: Inappropriate fixative. The antibody may not recognize the epitope after certain fixation methods [3].
- Solution: If using an alcohol-based fixative, switch to formaldehyde. Alternatively, if epitope masking is suspected with formaldehyde, try methanol or acetone fixation [25].
- Cause 3: Antigen degradation. This can occur due to a delay in fixation or under-fixation [3].
Q: I am observing high background staining. What steps during specimen preparation can help reduce this? A: High background, or non-specific signal, can be mitigated with proper blocking and handling [2] [9].
- Cause 1: Tissue drying. Allowing tissue sections to dry out at any point causes irreversible non-specific antibody binding [2].
- Cause 2: Inadequate blocking. Endogenous enzymes or biotin in the tissue can cause background [2] [9].
- Solution: Use a blocking buffer containing normal serum from the secondary antibody host species. For HRP-based detection, include a peroxidase blocking step (3% Hâ‚‚Oâ‚‚). For tissues with high endogenous biotin (e.g., liver, kidney), use a biotin block or a polymer-based detection system [27] [9].
Q: What is the difference between immersion and perfusion fixation, and when should I use each? A: The choice depends on your tissue type and experimental goals [26].
- Immersion Fixation: The most common method. Suitable for small tissue pieces (<10 mm) dissected from the organism. The tissue is simply immersed in a large volume of fixative (50-100x the tissue volume) [7] [26].
- Perfusion Fixation: This method involves flushing the vascular system of a sacrificed animal with fixative. It provides rapid and uniform fixation of all internal organs, preserving morphology and reducing background from blood vessels. It is necessary for large tissues or when analyzing multiple organs from one animal [5] [26].
Antigen retrieval is a critical pre-analytical step in immunohistochemistry (IHC), essential for reversing the epitope masking caused by formalin fixation [28]. This process restores the accessibility of antigens to antibodies, enabling accurate detection and reliable results [29]. For researchers and drug development professionals troubleshooting issues like no staining or weak signal, selecting and optimizing the correct antigen retrieval method is often the key to success. This guide provides a detailed comparison of the two primary techniques—Heat-Induced Epitope Retrieval (HIER) and Proteolytic-Induced Epitope Retrieval (PIER)—and offers practical protocols and troubleshooting advice to refine your IHC experiments.
The choice between HIER and PIER depends on the target antigen, tissue type, and fixation method. The table below summarizes the core characteristics of each method.
Table 1: Core Characteristics of HIER and PIER
| Feature | Heat-Induced Epitope Retrieval (HIER) | Proteolytic-Induced Epitope Retrieval (PIER) |
|---|---|---|
| Fundamental Principle | Uses heat to break protein crosslinks via thermal unfolding [29] | Uses enzymes to digest and degrade protein crosslinks [29] |
| Standard Mechanism | Thermal disruption of crosslinks and chelation of calcium ions [28] | Enzymatic cleavage of protein crosslinks [30] |
| Typical Temperature | 95-120°C [29] [28] | 37°C [28] [31] |
| Standard Incubation Time | 10-30 minutes (heat application) [28] [32] | 5-30 minutes (commonly 10-15 minutes) [31] [32] |
| Key Advantage | Gentler on tissue morphology; more definable and controllable parameters [28] [31] | Can be effective for epitopes that are difficult to retrieve with heat alone [31] |
| Primary Disadvantage | Potential for tissue detachment from slides; can destroy some heat-labile epitopes [30] | Risk of tissue damage and epitope degradation; harder to control [30] [28] |
Selecting and Optimizing Antigen Retrieval Buffers
The chemical environment during antigen retrieval significantly impacts its efficacy. The pH of the retrieval buffer is a critical factor that must be optimized for each specific antibody-antigen pair [28].
Table 2: Common Antigen Retrieval Buffers and Their Applications
| Buffer Solution | Typical pH | Common Applications & Notes |
|---|---|---|
| Sodium Citrate [32] | 6.0 | A widely used low-pH buffer. A common starting point for optimization [28] [32]. |
| Tris-EDTA [32] | 8.0 - 9.0 | A common high-pH buffer. Often effective for many targets and is a standard alternative to citrate [28] [32]. |
| EDTA [32] | 8.0 | Another high-pH option. Can be particularly effective for certain nuclear antigens [32]. |
Decision Workflow for Antigen Retrieval Optimization
The following diagram outlines a systematic approach to selecting and optimizing an antigen retrieval protocol, which is crucial for resolving issues of weak or no staining.
Detailed Experimental Protocols
Standardized HIER Protocol Using a Pressure Cooker
This protocol is a common and effective method for HIER [32].
- Deparaffinization and Rehydration: Process slides through xylene and graded ethanol series to water [32].
- Buffer Preparation: Fill a domestic stainless steel pressure cooker with an appropriate antigen retrieval buffer (e.g., Sodium Citrate pH 6.0 or Tris-EDTA pH 9.0) [32].
- Heating: Place the open pressure cooker on a hot plate set to full power until the buffer boils. Transfer the slide rack from tap water into the boiling buffer, secure the lid, and bring to full pressure [32].
- Retrieval: Once full pressure is reached, maintain the heat for 3 minutes [32].
- Cooling: Turn off the heat. Place the pressure cooker in a sink, activate the pressure release valve, and run cold water over it to depressurize and cool. Once open, run cold water into the cooker for 10 minutes to cool the slides and allow epitopes to re-form [32].
- Staining: Proceed with the standard IHC staining protocol [32].
Enzymatic Antigen Retrieval (PIER) Protocol
This protocol uses proteinase K as an example enzyme [30].
- Deparaffinization and Rehydration: Process slides to water.
- Enzyme Solution: Prepare a solution of 30 µg/mL Proteinase K in a 50 mM Tris/HCl buffer with 5 mM CaCl₂ at pH 6.0 [30].
- Digestion: Incubate the tissue sections in the Proteinase K solution for 90 minutes at 37°C in a humidified chamber [30].
- Optional Secondary Digestion: For dense tissues like cartilage, a subsequent incubation with 0.4% bovine hyaluronidase for 3 hours at 37°C may be beneficial [30].
- Washing: Rinse slides gently with PBS or distilled water [30].
- Staining: Continue with the standard IHC protocol.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Antigen Retrieval and IHC
| Reagent / Tool | Primary Function | Application Notes |
|---|---|---|
| Citrate Buffer (pH 6.0) | Low-pH retrieval solution for HIER [32]. | A standard first-choice buffer for many antibody targets [28]. |
| Tris-EDTA Buffer (pH 9.0) | High-pH retrieval solution for HIER [32]. | A standard second-choice buffer; often effective where citrate fails [28]. |
| Proteinase K | Proteolytic enzyme for PIER [30]. | Requires careful optimization of time and concentration to prevent tissue damage [30] [28]. |
| Polymer-Based Detection System | Amplifies signal for visualization [33]. | More sensitive than avidin-biotin (ABC) systems; reduces background in tissues with endogenous biotin [33]. |
| Sodium Borohydride | Reduces autofluorescence [9]. | Used to treat aldehyde-induced autofluorescence in fluorescent IHC (1 mg/mL in PBS) [9]. |
| Normal Serum | Blocks non-specific antibody binding [33]. | Use serum from the species of the secondary antibody (e.g., Normal Goat Serum) [33]. |
| Excisanin B | Excisanin B, MF:C22H32O6, MW:392.5 g/mol | Chemical Reagent |
| Regaloside I | Regaloside I, MF:C20H26O11, MW:442.4 g/mol | Chemical Reagent |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: What is the single best antigen retrieval buffer to use? A: There is no universal "best" buffer. The optimal buffer is antibody-specific. A systematic approach, starting with both a low pH (Citrate, pH 6.0) and a high pH (Tris-EDTA, pH 9.0) buffer, is recommended to determine the best condition for your target [28] [32].
Q: How can I fix weak or absent IHC staining? A: Weak or no staining is frequently caused by under-retrieval [28]. First, verify that your primary antibody is validated for IHC and your fixation method [2]. Then, try increasing the heating time during HIER, switching to a higher pH retrieval solution, or testing a PIER approach [2] [28].
Q: Is antigen retrieval always necessary? A: No. It is primarily required for formalin-fixed, paraffin-embedded (FFPE) tissues. Frozen tissues fixed with alcohol or fresh frozen sections typically do not require antigen retrieval, as alcohols do not create the same protein crosslinks [29] [28] [31].
Q: My staining has high background. Could antigen retrieval be the cause? A: Yes. Over-retrieval, either from excessive heating during HIER or over-digestion during PIER, can damage tissue and cause high, non-specific background staining [28]. Optimizing the retrieval time and intensity is crucial.
Troubleshooting Common Artifacts
The following flowchart helps diagnose and resolve common staining problems related to antigen retrieval.
Antibody Titration and Diluent Selection for Optimal Signal
Core Principles of Antibody Titration
Antibody titration is the process of determining the optimal dilution of an antibody that provides the strongest specific signal with the lowest background noise. The optimum antibody titer is the highest dilution that results in maximum positive signal without background or nonspecific reactions [34].
Performing titration is essential because using an antibody at too high a concentration can increase background staining and nonspecific binding, while too low a concentration may yield weak or no detectable signal [35] [36]. The optimal dilution must be determined empirically for each antibody and application, even when manufacturer recommendations are available [34].
Quantitative Dilution Ranges by Antibody Type
The table below summarizes typical working dilution ranges for different antibody preparation types, which serves as a starting point for titration experiments [34].
| Antibody Preparation Type | Typical Working Dilution Range |
|---|---|
| Polyclonal antiserum | 1:100 - 1:2,000 |
| Chromatographically purified antibodies | 1:500 - 1:10,000 |
| Monoclonal antibodies (cell culture supernatants) | 1:10 - 1:1,000 |
| Monoclonal antibodies (ascites fluid) | 1:1,000 - 1:100,000 |
Experimental Protocol: Antibody Titration for IHC
Recommended Titration Approach
To determine the optimal working concentration for a primary antibody in IHC, follow this systematic titration protocol [34]:
- Select fixed incubation time and temperature for the experiment
- Prepare a series of antibody dilutions in a recommended diluent (e.g., PBS with 1-5% BSA) [35] [36]
- If the datasheet suggests 1:200, test: 1:50, 1:100, 1:200, 1:400, and 1:500
- Apply each dilution to identical tissue sections with the same experimental conditions
- Process all slides simultaneously using the same reagents and timing
- Evaluate results to identify the dilution with the strongest specific signal and lowest background
Titration Workflow and Signal Optimization
The following diagram illustrates the antibody titration optimization process and its effect on signal quality:
Diluent Selection and Composition
The choice of antibody diluent significantly impacts staining quality by affecting antibody stability and binding characteristics. An appropriate diluent maintains antibody activity while minimizing nonspecific interactions.
Key Diluent Components and Functions
| Component | Function | Considerations |
|---|---|---|
| Buffered Saline (PBS or TBS) | Maintains physiological pH (7.0-8.2) | Provides stable environment for antibody-antigen binding [36] |
| Carrier Proteins (BSA, serum) | Reduces nonspecific binding | 1-5% BSA or 2-10% normal serum from secondary antibody species [35] [36] [15] |
| Salts (NaCl) | Reduces ionic interactions | 0.15M-0.6M NaCl can decrease background staining [36] |
| Preservatives (sodium azide) | Prevents microbial growth | Avoid with HRP systems; use 0.01% azide in storage buffers [35] [36] |
Specialized Diluent Formulations
For challenging applications, specialized diluent modifications may be necessary:
- High Salt Diluent: Adding 0.15M-0.6M NaCl to the blocking buffer/antibody diluent helps reduce ionic interactions that cause background staining [36]
- Permeabilization Diluent: For nuclear targets, add 0.2% Triton X-100 or other permeabilizing agents to the blocking buffer and antibody dilution buffer to improve antibody penetration [35] [37]
- Commercial Antibody Diluents: Specifically formulated to maintain enzymatic activity and prevent peroxidase inhibitors present in some deionized water [35]
Frequently Asked Questions (FAQs)
How do I troubleshoot weak or no staining after antibody titration?
Weak or absent staining despite proper titration can result from several issues [35] [37]:
- Epitope Masking: Fixation procedures (especially with formalin/PFA) may mask the epitope
- Solution: Use antigen retrieval methods (HIER or PIER) to unmask epitopes
- Antibody Incompatibility: Confirm the antibody is validated for IHC and your specific sample type (FFPE vs. frozen)
- Improper Antibody Storage: Repeated freeze-thaw cycles can degrade antibodies
- Solution: Aliquot antibodies and store according to manufacturer instructions
- Insufficient Deparaffinization: Incomplete removal of paraffin prevents antibody access
- Solution: Increase deparaffinization time and use fresh xylene
- Endogenous Enzyme Interference: Contaminated buffers or enzyme inhibitors in water
- Solution: Use fresh sterile PBS and commercial antibody diluents
What causes high background staining even with optimized titration?
Excessive background staining often relates to nonspecific antibody binding or insufficient blocking [35] [36]:
- Insufficient Blocking: Increase blocking incubation period or change blocking reagents
- Tissue sections: 10% normal serum (1 hour)
- Cell cultures: 1-5% BSA (30 minutes)
- Endogenous Enzyme Activity: Unquenched peroxidases or phosphatases
- Solution: Quench with 3% Hâ‚‚Oâ‚‚ in methanol or 2mM Levamisole for phosphatases
- Secondary Antibody Cross-reactivity: Use secondary antibodies pre-adsorbed against the species of your samples
- Excessive Antibody Concentration: Despite titration, further dilution may be needed
- Endogenous Biotin: Particularly problematic in liver, kidney, and spleen tissues
- Solution: Block with avidin/biotin blocking solutions
How do incubation time and temperature affect antibody binding?
Incubation conditions significantly impact staining results and should be standardized during titration [38]:
- Overnight at 4°C: Typically provides optimal signal-to-noise ratio for most antibodies
- Shorter Incubations at Higher Temperatures: May require increased antibody concentrations
- Temperature Sensitivity: Some epitopes/antibodies are sensitive to higher temperatures (37°C), which can reduce binding efficiency
- Consistency: Maintain consistent incubation conditions across experiments once optimized
Research Reagent Solutions
The table below outlines essential reagents for antibody titration and IHC staining optimization:
| Reagent | Function | Application Notes |
|---|---|---|
| Primary Antibody | Binds specifically to target antigen | Must be validated for IHC; titration required for optimal dilution [35] [34] |
| Species-Matched Secondary Antibody | Binds to primary antibody for detection | Should be raised against species of primary antibody [35] [37] |
| Blocking Serum | Reduces nonspecific binding | Use normal serum from secondary antibody species (5-10%) [35] [36] |
| BSA | Carrier protein in diluents | 1-5% in buffer reduces nonspecific binding [35] [36] |
| Antigen Retrieval Solutions | Unmasks epitopes cross-linked by fixation | Citrate (pH 6.0) or EDTA/Tris (pH 9.0) buffers for HIER [35] [15] |
| Enzyme Substrates (DAB, AEC) | Generates detectable signal | Choose based on application; DAB provides permanent staining [5] [39] |
| Permeabilization Agents (Triton X-100) | Enables antibody penetration | 0.1-0.5% for membrane permeabilization; critical for nuclear targets [35] [37] |
In the field of Immunohistochemistry (IHC), the choice of detection system is pivotal for achieving clear, specific, and reproducible results. When researchers are confronted with the common challenges of no staining or a weak signal, the detection method is a primary area for investigation. This guide provides a detailed comparison between two major classes of detection systems—polymer-based and biotin-based—to help you select the optimal methodology for your experiments and effectively troubleshoot issues.
Detection Systems at a Glance
The following table summarizes the core characteristics, advantages, and disadvantages of the primary detection systems used in IHC.
Comparison of IHC Detection Systems
| Feature | Direct Method | Indirect Method | Biotin-Based (ABC/LSAB) | Polymer-Based |
|---|---|---|---|---|
| Complex Formed | Labeled primary antibody | Labeled secondary antibody | Avidin-Biotin-Enzyme complex [40] [41] | Polymer backbone with multiple enzymes & antibodies [40] |
| Sensitivity | Low (no amplification) [41] [42] | Moderate (some amplification) [41] | High [40] [41] | Very High (highest enzyme-to-antibody ratio) [40] [41] |
| Steps | 1-step [41] | 2-step [41] | 3-step [41] | 2-step [41] |
| Key Advantage | Fast, minimal nonspecific binding [42] | Flexible, more sensitive than direct [41] | High signal amplification, well-established [40] [41] | High sensitivity & specificity, fast, no endogenous biotin interference [40] [41] |
| Key Disadvantage | Low sensitivity, requires labeled primary for each target [41] [42] | Lower sensitivity than amplified methods [41] | Endogenous biotin causes background; large complex size may hinder penetration [40] [41] | Can be more expensive; dextran polymers may have steric interference [41] |
Fig 1. A workflow diagram for selecting an IHC detection system. The diagram maps the relationship between the type of method and key operational characteristics, such as protocol steps, sensitivity, and background risk, helping researchers narrow their choices based on experimental priorities.
Troubleshooting FAQs: No Staining & Weak Signal
Q1: My IHC experiment shows no staining. What should I check first in my detection system?
A systematic approach is crucial for diagnosing a complete lack of signal.
- Verify Detection System Activity: A simple test can check if your enzyme and substrate are working. Place a drop of the enzyme (e.g., HRP) onto a piece of nitrocellulose and dip it into the prepared substrate. A colored spot should form immediately if they are reacting properly [9].
- Confirm Antibody Compatibility: Ensure your secondary antibody is raised against the host species of your primary antibody (e.g., an anti-rabbit secondary for a rabbit primary) [43].
- Check for Incompatible Buffers: Sodium azide is a potent inhibitor of Horseradish Peroxidase (HRP) and must not be present in any buffers used with HRP-based systems [9] [43]. Similarly, phosphate buffers should be avoided with Alkaline Phosphatase (AP) systems [43].
- Assay the Positive Control: Always run a positive control tissue known to express your target antigen concurrently with your experimental sample. A lack of staining in the positive control indicates a problem with the antibody or detection reagents, whereas staining only in the positive control points to an issue with the experimental tissue itself, such as antigen absence or suboptimal retrieval [9] [44].
Q2: I have a weak signal. Should I increase my primary antibody concentration?
Increasing the primary antibody concentration is a common instinct, but it can often increase background without improving the signal [2]. Before adjusting the primary, optimize your detection system:
- Switch to a Higher-Sensitivity System: If you are using a direct or simple indirect method, switching to an amplified system like polymer-based detection can dramatically increase signal strength. Polymer-based systems are more sensitive than biotin-based systems and are the modern standard for many applications [44] [40].
- Troubleshoot Biotin-Based Systems: If using a biotin-based system (ABC or LSAB), be aware that extremely high concentrations of the biotinylated secondary antibody can paradoxically reduce antigen detection. Perform a titration experiment with decreasing concentrations of the secondary antibody to find the optimum [9].
- Review the Chromogen Development Time: Insufficient time in the chromogen substrate solution can result in a weak signal. Monitor the development under a microscope and stop the reaction only when the specific signal is clearly visible [2].
Q3: My staining has high background. How can I determine if it's caused by my detection system?
High background staining obscures your specific signal and is a frequent challenge.
- Test for Secondary Antibody Cross-Reactivity: Run a negative control by omitting the primary antibody. If staining is observed, it suggests the secondary antibody is binding non-specifically to the tissue. To resolve this, use a secondary antibody that has been pre-adsorbed against the immunoglobulin of the species from which your sample was obtained, and ensure adequate blocking with serum from the secondary antibody's host species [44] [43].
- Block Endogenous Enzymes: For HRP-based systems, endogenous peroxidases in tissues (especially erythrocytes and granulocytes) can produce background. Quench this activity by incubating slides in 3% Hâ‚‚Oâ‚‚ for 10 minutes before applying the primary antibody [44] [22].
- Block Endogenous Biotin (Critical for Biotin-Based Systems): Tissues such as liver and kidney have high levels of endogenous biotin, which will bind the avidin/streptavidin in ABC/LSAB systems, causing significant background [40] [41]. This is less of an issue with polymer-based systems, which are biotin-free. If using a biotin-based system, you must perform an endogenous biotin block after the normal blocking procedure [44].
- Optimize Washes: Inconsistent or insufficient washing after primary and secondary antibody incubations is a common source of high background. Wash slides 3 times for 5 minutes with a buffer containing a mild detergent like Tween-20 (e.g., TBST or PBST) with standardized agitation [44] [22].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table lists key reagents and their specific functions for troubleshooting detection-related issues in IHC.
Research Reagent Solutions for IHC Detection
| Reagent / Kit | Primary Function | Key Application Note |
|---|---|---|
| Polymer-Based Detection Kits (e.g., SignalStain Boost [44]) | High-sensitivity, biotin-free detection. | Preferred for avoiding endogenous biotin background; offers a streamlined 2-step protocol [44] [40]. |
| Endogenous Enzyme Block (3% Hâ‚‚Oâ‚‚ [9] [44]) | Quenches endogenous peroxidase activity. | Essential for HRP-based systems to reduce background in tissues with high peroxidase activity [22]. |
| Endogenous Biotin Blocking Kit [9] [44] | Blocks endogenous biotin. | Mandatory when using ABC or LSAB methods, especially for liver, kidney, or frozen sections [40] [41]. |
| Ready-To-Use (RTU) Antibodies | Provides consistency and saves time. | Eliminates dilution errors and simplifies protocol validation; ideal for standardized workflows [22]. |
| Normal Serum (from secondary host species) | Blocks nonspecific protein binding sites. | Reduces background caused by hydrophobic or ionic interactions; typically used at 5-10% concentration [9] [44]. |
| Buffered Detergent Washes (e.g., TBST, PBST) | Removes unbound reagents. | Critical for reducing background; 3x5 minute washes with agitation are recommended [9] [44]. |
| Rediocide A | Rediocide A, MF:C44H58O13, MW:794.9 g/mol | Chemical Reagent |
| Cryptofolione | Cryptofolione, MF:C19H22O4, MW:314.4 g/mol | Chemical Reagent |
Fig 2. A troubleshooting flowchart for common IHC detection problems. This diagram outlines a logical path from identifying a core problem (weak signal or high background) to implementing targeted, practical solutions based on the principles of detection systems.
Protocol for Overnight Primary Antibody Incubation at 4°C
Standard Operating Procedure: Overnight Incubation at 4°C
The overnight incubation of the primary antibody at 4°C is a critical step in immunohistochemistry (IHC) that enhances specificity and signal intensity for challenging targets [45]. This protocol details the optimal procedure for this incubation within the broader context of IHC troubleshooting for resolving issues of no staining or weak signal.
Materials and Reagents
- Primary Antibody: Validated for IHC and specific to your target [2].
- Antibody Diluent: A suitable buffer such as PBS or TBS with carrier protein (e.g., 1-5% BSA) [46] [47]. Using the same buffer for blocking and antibody dilution is recommended [47].
- Humidity Chamber: A sealed container with a moistened paper towel to prevent sections from drying out [2].
- Fixed and processed tissue sections on slides, already undergone deparaffinization, antigen retrieval, and blocking steps [48].
Step-by-Step Workflow
- Preparation: Following the blocking step, remove the blocking buffer from the tissue sections.
- Application: Apply the optimally diluted primary antibody solution to the tissue sections, ensuring complete coverage [2].
- Incubation: Place the slides in a humidity chamber and incubate overnight (typically 12-16 hours) in a refrigerator at 4°C [46] [45].
- Washing: The next day, wash the slides thoroughly (e.g., three times for 10 minutes each) with an appropriate wash buffer like TBS or PBS to remove unbound antibody [46].
- Proceed with the application of the secondary antibody and the remainder of your detection protocol.
Troubleshooting Guide: Resolving Common Incubation Issues
Weak or No Staining
| Possible Cause | Solution | Experimental Protocol / Notes |
|---|---|---|
| Inactive Primary Antibody | Run a positive control tissue known to express the target. Aliquot antibodies to avoid freeze-thaw cycles and store according to manufacturer instructions [9] [2] [49]. | Always include a positive control slide with a known validated antibody to confirm the entire procedure is functional [9] [45]. |
| Suboptimal Antibody Concentration | Perform a titration experiment. Test a range of dilutions (e.g., 1:50, 1:100, 1:200) to find the optimal concentration for your specific tissue and protocol [2] [49]. | Incubate a series of slides with different antibody dilutions overnight at 4°C. Compare signal strength and background to identify the dilution with the best signal-to-noise ratio. |
| Inadequate Antigen Retrieval | Optimize the antigen retrieval method (HIER). Ensure the correct buffer (e.g., Citrate pH 6.0, Tris-EDTA pH 9.0) is used with sufficient heating time and temperature [9] [2] [45]. | If weak staining persists, test a different retrieval buffer pH or method (e.g., pressure cooker vs. microwave) on consecutive sections, followed by the standard overnight incubation [45]. |
| Tissue Drying | Use a properly sealed humidity chamber and ensure the tissue section is fully covered with antibody solution throughout the incubation [2] [49]. | Drying causes irreversible non-specific binding and loss of signal. Check the chamber seal and the volume of antibody applied. |
High Background Staining
| Possible Cause | Solution | Experimental Protocol / Notes |
|---|---|---|
| Primary Antibody Concentration Too High | Titrate the antibody to find a lower concentration that maintains a strong specific signal while reducing background [2] [49]. | As with weak staining, a dilution series is essential. High concentrations promote non-specific binding. |
| Insufficient Blocking | Increase the concentration of the blocking serum (up to 10%) or extend the blocking incubation time. Ensure the normal serum used for blocking is from the same species as the secondary antibody [9] [47]. | Block with 10% normal serum from the secondary antibody host species for 1 hour at room temperature before applying the primary antibody [46] [49]. |
| Non-specific Binding | Add NaCl to the antibody diluent to a final concentration of 0.15-0.6 M to reduce ionic interactions, or include a gentle detergent like 0.05% Tween-20 [9] [2]. | Empirically determine the best NaCl concentration. Prepare diluent with varying NaCl levels and compare background on control tissues. |
| Secondary Antibody Cross-reactivity | Always run a negative control slide incubated without the primary antibody. If staining is observed, use secondary antibodies that are cross-adsorbed against the species of your tissue sample [9] [45]. | The negative control (secondary antibody only) is critical for diagnosing background from the detection system. |
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function in Overnight Incubation |
|---|---|
| Humidity Chamber | Prevents evaporation and drying of the primary antibody solution on the tissue section, which is critical for a long incubation and prevents high background [2]. |
| Antibody Diluent Buffer | Stabilizes the primary antibody, provides the correct pH (typically 7.0-8.2), and can contain proteins (BSA) or sera to minimize non-specific binding during the long incubation [9] [45]. |
| Normal Serum | Used in blocking buffers and/or antibody diluents. Serum from the secondary antibody species blocks non-specific binding sites, reducing background caused by the secondary antibody [9] [47]. |
| Cross-Adsorbed Secondary Antibodies | Secondary antibodies that have been purified to remove reactivity against immunoglobulins from other species. This is crucial for multiplex experiments or when working with tissue endogenous immunoglobulins, minimizing false-positive signals [46] [50]. |
| Tatsinine | Tatsinine, MF:C22H35NO6, MW:409.5 g/mol |
| Ganoderic acid I | Ganoderic acid I, MF:C30H44O8, MW:532.7 g/mol |
Visualized Workflows and Decision Pathways
Overnight Primary Antibody Incubation Workflow
Troubleshooting Weak Staining & High Background
Frequently Asked Questions (FAQs)
Q1: Why is an overnight incubation at 4°C preferred over a shorter incubation at room temperature? A1: The prolonged incubation at a lower temperature increases the binding affinity and specificity of the primary antibody for its target antigen. This is particularly beneficial for low-abundance targets or antibodies with lower affinity, as it enhances the signal while often reducing non-specific binding, leading to a better signal-to-noise ratio [45].
Q2: Can I incubate the primary antibody for longer than overnight (e.g., over a weekend)? A2: It is not generally recommended. While an overnight incubation (12-16 hours) is optimal, excessively long incubations can increase the risk of non-specific binding, tissue degradation, or microbial growth, potentially leading to high background.
Q3: My positive control stains well, but my experimental tissue does not. What does this indicate? A3: This is a critical observation. A good positive control confirms that your antibody and protocol are functioning correctly [9]. The lack of staining in your experimental tissue likely indicates a true biological result—that the target antigen is not present or is present at levels below the detection threshold in that specific sample [45].
Q4: What is the most critical control for diagnosing high background? A4: The most critical control is a no-primary control (incubating with diluent and secondary antibody only). If this control shows staining, the background is caused by non-specific binding of your secondary antibody or endogenous activity in the tissue, and you should focus on improving blocking and using cross-adsorbed secondaries [9] [45].
IHC Troubleshooting Protocol: A Step-by-Step Diagnostic Framework
FAQ: Addressing Common IHC Staining Problems
What are the primary causes of no staining in IHC experiments?
A complete lack of staining often stems from issues related to the antibody, antigen accessibility, or specimen preparation [18] [51]. The following table summarizes the common causes and their respective investigative approaches.
| Possible Cause | Diagnostic Question or Action |
|---|---|
| Antibody Issues | Has the antibody been validated for IHC on your specific sample type (e.g., FFPE)? Are storage conditions correct, and is it past its expiration date? [2] [51] |
| Ineffective Antigen Retrieval | Was the appropriate Heat-Induced Epitope Retrieval (HIER) method used? Check the buffer pH, temperature, and incubation time [52] [2]. |
| Specimen Preparation | Was the tissue fixed promptly and for a correct duration? Has deparaffinization been complete? [15] [51] |
| Incompatible Detection System | Are the primary and secondary antibodies compatible? Is the detection system active and appropriate for the target abundance? [52] [51] |
What leads to weak or faint staining signals?
Weak staining signals typically result from suboptimal protocol conditions or reagent potency [9] [51]. A systematic check of key parameters is essential for resolution.
| Possible Cause | Diagnostic Question or Action |
|---|---|
| Suboptimal Antibody Concentration | Is the primary antibody too dilute? Has a titration experiment been performed to find the optimal concentration? [2] [51] |
| Loss of Antibody Potency | Has the antibody been subjected to multiple freeze-thaw cycles or improper storage? Always run a positive control [9] [51]. |
| Over-fixation | Has prolonged formalin fixation masked the epitope, requiring a more robust antigen retrieval step? [15] [2] |
| Insufficient Detection Sensitivity | Is an amplification step included? Would a polymer-based detection system provide greater sensitivity than a biotin-based one? [52] |
Diagnostic Flowchart for IHC Staining Issues
The following diagram outlines a systematic troubleshooting pathway for resolving issues of no signal to weak staining in IHC. This workflow synthesizes diagnostic checks and remedial actions from the provided research.
Research Reagent Solutions for IHC Troubleshooting
The table below details essential reagents and their specific functions in resolving no or weak staining issues, as highlighted in the troubleshooting literature.
| Reagent / Material | Function in Troubleshooting |
|---|---|
| Sodium Citrate Buffer (pH 6.0) | A common buffer for heat-induced epitope retrieval (HIER) to unmask antigens cross-linked by formalin fixation [9]. |
| Tris-EDTA Buffer (pH 9.0) | An alternative high-pH retrieval buffer used for a different subset of antigens that do not unmask effectively with citrate buffer [2]. |
| Protein Blocking Serum | Normal serum from the species of the secondary antibody reduces nonspecific binding, improving signal-to-noise ratio [15] [52]. |
| Polymer-Based Detection System | Provides superior sensitivity and signal amplification compared to avidin-biotin complex (ABC) systems, crucial for low-abundance targets [52]. |
| Triton X-100 | A permeabilizing agent added to buffers to allow antibody penetration into nuclear or intracellular epitopes [51]. |
| Ready-To-Use (RTU) Antibodies | Pre-optimized antibodies that enhance run-to-run consistency and eliminate dilution errors, improving reproducibility [22]. |
Detailed Experimental Protocols for Key Troubleshooting Steps
Protocol 1: Standardized Heat-Induced Epitope Retrieval (HIER)
Antigen retrieval is a critical step for recovering signals in formalin-fixed, paraffin-embedded (FFPE) tissues [15]. The following protocol is a common starting point for optimization.
- Buffer Selection: Begin with 10 mM Sodium Citrate buffer, pH 6.0, or Tris-EDTA, pH 9.0, depending on the primary antibody's validation data [9] [2].
- Heating Method: A microwave oven is generally recommended. Heat slides in retrieval buffer for 8-15 minutes at a high power setting (750-800 W) to achieve and maintain a near-boiling temperature [15] [52]. Alternatively, a pressure cooker can be used for 20 minutes for more challenging targets [9] [52].
- Cooling: After heating, allow the slides to cool in the buffer for 20-30 minutes at room temperature before proceeding to immunostaining [15].
Protocol 2: Primary Antibody Titration
Using an incorrect antibody concentration is a primary cause of both no signal and high background [9] [2]. A titration experiment is essential for optimization.
- Preparation: Prepare a series of primary antibody dilutions (e.g., 1:50, 1:100, 1:200, 1:500) in the recommended antibody diluent [2] [51].
- Application: Apply the different dilutions to consecutive tissue sections from the same FFPE block, preferably one known to express the target (positive control tissue).
- Incubation and Development: Process all slides simultaneously using the same detection system and chromogen development time.
- Analysis: Examine the slides microscopically to identify the dilution that provides the strongest specific signal with the cleanest background.
Protocol 3: Enhancing Detection Sensitivity
Weak signals can often be resolved by improving the detection method rather than altering primary antibody conditions [52].
- System Choice: Switch from a standard streptavidin-biotin (ABC) system to a modern polymer-based system. These systems conjugate multiple enzyme molecules directly to the secondary antibody, providing greater amplification and avoiding issues with endogenous biotin [52].
- Signal Development: Ensure the chromogen substrate (e.g., DAB) is fresh and prepared correctly. Monitor the development reaction under a microscope and stop it promptly by immersing slides in water once the desired signal intensity is achieved to prevent high background [2].
Why is there no staining or a very weak signal in my experiment?
A lack of expected signal is one of the most common frustrations in IHC. The issue often originates with the primary antibody's concentration, specificity, or activity [2] [18].
| Possible Cause | Specific Tests & Solutions |
|---|---|
| Incorrect Antibody Concentration [2] [53] | - Titration Experiment: Systematically test a range of antibody dilutions (e.g., 1:50, 1:100, 1:200) to find the optimal concentration [2].- General Guidance: For monoclonal antibodies, test 5-25 µg/mL; for polyclonals, test 1.7-15 µg/mL [54]. |
| Loss of Antibody Activity [9] [55] | - Run a Positive Control: Always stain a tissue known to express the target antigen concurrently with your experimental samples [9] [56].- Proper Storage: Aliquot antibodies to avoid repeated freeze-thaw cycles and store according to the manufacturer's instructions [55] [57]. |
| Insufficient Epitope Exposure [55] [2] | - Optimize Antigen Retrieval: Ensure the correct buffer (e.g., Citrate pH 6.0, Tris-EDTA pH 9.0) and method (microwave or pressure cooker is preferred over water bath) are used [56] [58].- Address Over-fixation: If standard retrieval fails, increase the duration or intensity of the retrieval step [2]. |
| Antibody is Not IHC-Validated [55] [2] | - Check the Datasheet: Confirm the antibody has been validated for your specific application (e.g., FFPE, frozen sections) [55] [2].- Use a Primary Antibody that is Compatible with Your Secondary Antibody: Ensure the secondary antibody was raised against the host species of the primary antibody [55] [53]. |
Experimental Protocol: Primary Antibody Titration
A well-designed titration is the most reliable method to optimize antibody concentration for strong specific signal with minimal background [2] [54].
- Slide Preparation: Use consecutive sections of a positive control tissue that is known to express your target protein.
- Standard Protocol: Follow your established IHC protocol through the antigen retrieval and blocking steps.
- Primary Antibody Dilution: Prepare a series of primary antibody dilutions. A common starting range is 1:50, 1:100, 1:200, 1:500, and a negative control (no primary antibody) [2].
- Incubation: Apply the different dilutions to the respective tissue sections and incubate overnight at 4°C [54].
- Detection and Analysis: Complete the protocol with your standard detection method. Analyze the slides to identify the dilution that provides the strongest specific signal with the cleanest background.
Why is my background staining too high?
High background staining, which obscures specific signal, is frequently caused by the primary antibody binding non-specifically to off-target sites [9] [55].
| Possible Cause | Specific Tests & Solutions |
|---|---|
| Primary Antibody Concentration Too High [9] [2] | - Titrate the Antibody: Find the lowest concentration that still gives a strong specific signal. High concentrations promote non-specific binding [55] [2]. |
| Insufficient Blocking [55] [53] | - Increase Blocking: Extend the blocking incubation time or change the reagent (e.g., 10% normal serum, 1-5% BSA) [55].- Block Endogenous Enzymes: Quench endogenous peroxidases with 3% H2O2 [9] [56]. |
| Hydrophobic/Ionic Interactions [9] [57] | - Modify Buffers: Add a gentle detergent like 0.05% Tween-20 to wash and dilution buffers to reduce hydrophobic interactions [9].- Adjust Ionic Strength: Add NaCl (0.15M - 0.6M) to the antibody diluent to reduce ionic-based non-specific binding [9]. |
| Cross-Reactivity or Species Mismatch [56] [53] | - Run a Negative Control: Always include a control stained with secondary antibody only. If staining appears, the secondary antibody is the source [55] [56].- Use Cross-Absorbed Secondaries: For mouse-on-mouse staining, use secondary antibodies that have been pre-adsorbed against mouse IgG [56]. |
The Scientist's Toolkit: Essential Reagents for Troubleshooting
| Reagent | Function in Troubleshooting |
|---|---|
| Positive Control Tissue [9] [56] | Verifies antibody activity and protocol performance. Essential for diagnosing weak staining. |
| Normal Serum [9] [55] | Used for blocking to prevent non-specific binding of secondary antibodies. Should be from the same species as the secondary antibody host. |
| Antigen Retrieval Buffers (e.g., Citrate pH 6.0, EDTA pH 9.0) [9] [58] | Critical for unmasking epitopes cross-linked by formalin fixation, directly impacting signal strength. |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) [9] [55] | Quenches endogenous peroxidase activity in tissues, a major cause of high background in HRP-based detection. |
| Detergent (e.g., Tween-20) [9] [2] | Added to wash buffers to reduce hydrophobic interactions and improve washing efficiency, lowering background. |
| Polymer-Based Detection System [56] | Provides high sensitivity and avoids background from endogenous biotin, which is problematic with avidin-biotin (ABC) systems. |
How do I know if my primary antibody has lost activity, and what can I do?
Antibody activity can be compromised by improper storage, contamination, or repeated freeze-thaw cycles, leading to a sudden drop in staining intensity [9] [57].
- Test for Potency: The definitive test is to use the antibody to stain a positive control tissue that has previously worked well. If the positive control fails to stain, the antibody has likely lost potency [9] [55].
- Proper Storage and Handling:
- Aliquot: Upon receipt, divide the antibody into small, single-use aliquots to minimize freeze-thaw cycles and prevent contamination of the entire stock [55] [57].
- Storage Conditions: Follow the manufacturer's instructions precisely. Most antibodies are stored at -20°C or 4°C. Avoid frost-free freezers which undergo temperature cycles [55].
- Diluent pH: Ensure the antibody diluent has a pH between 7.0 and 8.2 for optimal antibody binding [9].
What is the difference between monoclonal and polyclonal antibodies for IHC?
The choice between monoclonal and polyclonal antibodies involves a trade-off between specificity and robustness [54].
| Characteristic | Monoclonal Antibody | Polyclonal Antibody |
|---|---|---|
| Epitope Recognition | A single, specific epitope on the target antigen [54]. | Multiple, different epitopes on the same antigen [54]. |
| Advantages | - Lower lot-to-lot variability [54].- Generally lower background [54].- High specificity for a single epitope. | - More tolerant to changes in antigen conformation caused by fixation [54].- Recognition of multiple epitopes can enhance signal [54]. |
| Disadvantages | - Vulnerable to epitope masking if the specific epitope is damaged or cross-linked during fixation [54]. | - Higher potential for background and cross-reactivity [54].- Higher lot-to-lot variability [54]. |
In immunohistochemistry (IHC), the ability to obtain clear, specific, and reproducible staining results hinges on the effective reversal of formalin-induced epitope masking. Formalin fixation, while essential for preserving tissue morphology, creates methylene bridges between proteins that alter epitope conformation and render antigens inaccessible to primary antibodies [28]. Antigen retrieval is therefore not merely a procedural step but a foundational technique that determines the success or failure of an entire IHC experiment. For researchers and drug development professionals, understanding how to systematically troubleshoot failures in this process—particularly relating to buffer pH, heating methods, and duration—is essential for generating reliable data.
This guide addresses the most common antigen retrieval failures by providing evidence-based troubleshooting strategies, quantitative optimization data, and practical protocols. The recommendations are framed within the broader context of IHC troubleshooting for resolving issues of no staining or weak signal, offering a structured approach to diagnose and rectify suboptimal retrieval conditions.
Understanding Antigen Retrieval Methods
Heat-Induced Epitope Retrieval (HIER)
HIER is the most widely used antigen retrieval method for formalin-fixed paraffin-embedded (FFPE) tissues. It employs high temperatures (typically 95-100°C) to disrupt protein crosslinks, restoring epitope accessibility [28] [32]. The mechanism involves both thermal disruption of crosslinks and chelation of calcium ions from protein cross-linking structures [28].
Proteolytic-Induced Epitope Retrieval (PIER)
PIER utilizes proteolytic enzymes (such as trypsin, proteinase K, or pepsin) to cleave protein crosslinks and restore antigenic accessibility. This method typically operates at 37°C with incubation periods of 10-20 minutes in humidified chambers [28]. While considered a gentler approach suitable for fragile tissues, PIER presents limitations including potential morphological tissue damage and epitope degradation if over-digested [28] [59].
Comparative Analysis: HIER vs. PIER
The table below summarizes the key characteristics, advantages, and disadvantages of each primary retrieval method:
Table: Comparison of Antigen Retrieval Methods
| Feature | Heat-Induced Epitope Retrieval (HIER) | Proteolytic-Induced Epitope Retrieval (PIER) |
|---|---|---|
| Principle | Uses heat to break protein crosslinks | Uses enzymes to digest proteins around epitopes |
| Typical Conditions | 95-100°C for 10-30 minutes [28] [32] | 37°C for 10-30 minutes [28] [59] |
| Common Agents | Citrate buffer (pH 6.0), Tris-EDTA (pH 8.0-9.0) [32] | Trypsin, proteinase K, pepsin [28] |
| Primary Advantages | Broader range of antigens, better morphology preservation [59] | Effective for difficult-to-recover epitopes, less heating damage [59] |
| Primary Disadvantages | Potential tissue damage from overheating, equipment-dependent [28] | Risk of destroying antigen and morphology, requires precise optimization [28] |
| Best Applications | Most nuclear and high-molecular-weight proteins [59] | Fragile tissues, specific interstitial antigens [59] |
Diagram: Systematic Troubleshooting Pathway for Antigen Retrieval Failures. This flowchart guides users through a logical decision-making process to diagnose and address common antigen retrieval problems based on observed staining outcomes.
Buffer pH Optimization Strategies
The Impact of pH on Antigen Retrieval Efficiency
The pH of the retrieval buffer significantly influences staining results by affecting the electrostatic charge of epitopes and the efficiency of crosslink reversal [32]. Different antigens demonstrate distinct responsiveness to pH variations, which can be categorized into four primary patterns [59]:
- Stable Type: pH has minimal effect on staining results (e.g., PCNA, CD20)
- V Type: Both high and low pH values yield good staining, while intermediate pH (4-5) results in poorer staining (e.g., ER, Ki-67)
- Increasing Type: Staining improves progressively with increasing pH (e.g., HMB45)
- Decreasing Type: Staining weakens as pH increases (rare, e.g., MOC31)
Buffer Formulations and Selection Guidelines
The table below provides preparation details for common HIER buffers and their typical applications:
Table: Common Antigen Retrieval Buffers and Applications
| Buffer Type | Composition | pH Range | Primary Applications | Preparation Guide |
|---|---|---|---|---|
| Citrate Buffer | 10 mM Sodium citrate, 0.05% Tween 20 [32] | 6.0 | Widely used general purpose buffer; effective for many cytoplasmic and membrane antigens [59] | 2.94 g tri-sodium citrate in 1L distilled water; adjust pH with HCl [32] |
| Tris-EDTA Buffer | 10 mM Tris base, 1 mM EDTA, 0.05% Tween 20 [32] | 8.0-9.0 | Superior for nuclear antigens and phospho-specific targets; often provides stronger staining than citrate [28] [59] | 1.21 g Tris + 0.37 g EDTA in 1L water; adjust to pH 9.0 [32] |
| EDTA Buffer | 1 mM EDTA [32] | 8.0 | Effective for challenging nuclear antigens; particularly useful when citrate fails [59] | 0.37 g EDTA in 1L water; adjust to pH 8.0 with NaOH [32] |
Systematic Buffer Optimization Approach
When optimizing antigen retrieval for a new antibody, follow this structured approach:
- Initial Testing: Begin with HIER at both low pH (citrate buffer, pH 6.0) and high pH (Tris-EDTA buffer, pH 8.0-9.9) [28]
- Matrix Optimization: If initial results are suboptimal, conduct preliminary matrix studies testing various combinations of time, temperature, and pH [28] [59]
- Enzymatic Retrieval: Evaluate PIER using different enzymatic approaches (trypsin, proteinase K, pepsin) if HIER fails [28]
Heating Methods and Duration Optimization
Comparison of Heating Modalities
The choice of heating method significantly impacts antigen retrieval efficiency and consistency. The table below compares the most common HIER heating methods:
Table: Comparison of HIER Heating Methods and Parameters
| Heating Method | Typical Temperature | Optimal Duration | Advantages | Limitations |
|---|---|---|---|---|
| Pressure Cooker | 120°C [28] | 1-5 minutes at full pressure [28] | Faster retrieval, superior for difficult epitopes, more uniform heating [32] | Potential for over-retrieval, requires careful timing [32] |
| Microwave | 95-100°C [32] | 15-20 minutes after reaching temperature [32] | Rapid heat generation, simple to use [59] | Uneven heating (hot/cold spots), potential for buffer evaporation [32] |
| Steamer | 95-100°C [32] | 20 minutes after returning to temperature [32] | Gentle boiling action, reduced evaporation risk [32] | Longer retrieval times, less intense than pressure cooking [32] |
| Water Bath | 95-100°C [32] | 20-30 minutes or overnight at 60°C [32] | Suitable for delicate tissues prone to detachment [32] | Significantly longer incubation times [32] |
Duration Optimization Framework
Retrieval duration must be optimized based on the heating method and target antigen:
- Pressure Cooker: 1-5 minutes at full pressure once pressurization is achieved [28]
- Microwave: 15-20 minutes of maintained heating after the solution reaches boiling temperature [32]
- Water Bath: 20-30 minutes at 95-100°C, or alternatively overnight incubation at 60°C for delicate tissues [32]
Troubleshooting Guide: FAQs and Solutions
Problem: Weak or No Staining
Q: Despite antigen retrieval, I'm getting weak or no signal. What should I adjust?
A: Weak or absent staining typically indicates insufficient epitope unmasking. Implement these solutions:
- Extend Retrieval Duration: Increase heating time by 5-10 minute increments [28] [60]
- Switch Buffer pH: Transition from low pH (citrate, pH 6.0) to high pH (Tris-EDTA, pH 8.0-9.0), particularly for nuclear antigens [28] [59]
- Verify Temperature: Confirm your heating equipment maintains correct temperature throughout retrieval [28]
- Intensify Heating Method: Change from microwave to pressure cooker for more effective retrieval of difficult epitopes [32] [61]
- Address Over-fixation: For over-fixed tissues, increase duration or intensity of antigen retrieval [2]
Problem: High Background Staining
Q: My staining shows high background that obscures specific signal. How can I reduce it?
A: High background often results from over-retrieval or non-specific binding:
- Reduce Retrieval Time: Decrease heating duration by 5-minute increments to minimize over-unmasking [28]
- Lower Buffer pH: Switch from high pH to citrate buffer (pH 6.0) if possible [28]
- Optimize Antibody Concentration: Titrate primary antibody to find optimal dilution that maintains signal while reducing background [2] [9]
- Enhance Blocking: Increase blocking serum concentration to 10% or extend blocking time to 1 hour [60]
- Implement Washes: Increase wash stringency with 0.05% Tween-20 in buffers to reduce hydrophobic interactions [2]
Problem: Tissue Morphology Damage
Q: After antigen retrieval, my tissue morphology appears damaged. How can I preserve it?
A: Morphological damage suggests overly harsh retrieval conditions:
- Reduce Enzymatic Digestion: For PIER, decrease enzyme concentration and/or incubation time [28]
- Switch to Gentler Method: Transition from PIER to HIER, or from pressure cooker to microwave/steamer [28] [32]
- Lower Temperature: For delicate tissues, use water bath method at 60°C overnight [32]
- Optimize Protease Concentration: For PIER, systematically test enzyme concentrations to find minimal effective level [59]
Problem: Inconsistent Staining Between Runs
Q: I get good staining sometimes but not others, even with the same protocol. Why?
A: Inconsistency typically stems from technical variability:
- Standardize Equipment: Use the same validated heating equipment for all experiments [28]
- Monitor Buffer Volume: Maintain consistent buffer volume across runs to ensure equivalent heating efficiency [32]
- Prepare Fresh Buffer: Always prepare fresh 1X retrieval solutions daily to maintain consistent pH and composition [61]
- Control Cooling Phase: Implement standardized cooling protocol (15-20 minutes at room temperature) after retrieval [32]
- Verify Timing: Begin timing only after the retrieval solution reaches the target temperature [32]
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Antigen Retrieval Optimization
| Reagent/Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| HIER Buffers | Citrate (pH 6.0), Tris-EDTA (pH 9.0), EDTA (pH 8.0) [32] | Break protein crosslinks through heat-mediated hydrolysis | EDTA often more effective for nuclear antigens [59] |
| Proteolytic Enzymes | Trypsin, Proteinase K, Pepsin [28] [59] | Digest proteins surrounding epitopes | Enzyme concentration and time require precise optimization [28] |
| Heating Equipment | Pressure cooker, microwave, steamer, water bath [32] | Provide controlled heating for HIER | Pressure cookers reduce retrieval time significantly [28] |
| Detection Enhancement | Polymer-based detection systems [61] | Amplify signal without biotin-related background | Superior to avidin-biotin systems for sensitive targets [61] |
| Blocking Reagents | Normal serum, BSA, commercial blocking solutions [9] [61] | Reduce non-specific antibody binding | Use serum from secondary antibody species [9] |
Effective troubleshooting of antigen retrieval failures requires a systematic approach that methodically addresses buffer pH, heating methodology, and duration parameters. By understanding the underlying principles of epitope unmasking and implementing the structured optimization strategies presented in this guide, researchers can transform inconsistent or failed IHC experiments into robust, reproducible staining outcomes. The integration of quantitative optimization matrices with empirical validation creates a foundation for reliable immunohistochemical data generation, ultimately supporting the rigorous research standards required in scientific discovery and drug development.
FAQs on Secondary Antibody Compatibility
Why is my negative control (no primary antibody) showing staining?
If your negative control shows staining, it indicates that your secondary antibody is binding non-specifically to something in the tissue. This is a clear sign of secondary antibody cross-reactivity. To resolve this, you should block the tissue using normal serum from the same species as the host in which the secondary antibody was raised. Alternatively, use a secondary antibody that has been pre-adsorbed against the immunoglobulins of the species from which your tissue sample was obtained. Including this negative control in every experiment is crucial for accurate troubleshooting [62] [3].
How do I confirm my primary and secondary antibodies are compatible?
Compatibility is determined by the host species of your primary antibody and the targeting species of your secondary antibody. For example, if your primary antibody was raised in a mouse, you must use an anti-mouse secondary antibody. Before starting your experiment, always check the datasheets of both antibodies to confirm this relationship. A common cause of failed experiments is using a secondary antibody that does not recognize the host species of the primary antibody [62] [3].
What causes high background from my secondary antibody, and how can I reduce it?
High background from a secondary antibody is typically caused by its concentration being too high, which can lead to non-specific binding. To fix this, titrate the secondary antibody to determine the optimal, lower concentration. Furthermore, extremely high concentrations of secondary antibody can paradoxically reduce antigen detection by causing steric hindrance. If background persists, switch to a polymer-based detection system, which is more sensitive and produces less background than traditional biotin-avidin systems [9] [62] [63].
FAQs on Enzyme-Substrate Reactions
My antibodies are compatible, but I still get no signal. What's wrong with my substrate reaction?
The enzyme-substrate reaction is a critical point of failure. Deionized water can sometimes contain peroxidase inhibitors that impair enzyme activity. Additionally, buffers containing sodium azide are incompatible with HRP-based detection systems. A simple test to verify the functionality of your HRP enzyme and substrate is to place a drop of the enzyme onto a piece of nitrocellulose and then immediately dip it into the prepared substrate. A colored spot should form promptly if they are reacting properly [9] [62].
Why is my chromogenic signal weak or developing too slowly?
A weak or slow-developing signal can result from an incorrect pH of the substrate buffer, as the enzyme requires a specific pH for optimal activity. Always prepare the substrate according to the manufacturer's instructions. Also, check the expiration date of your detection reagent, as expired substrates lose potency. If using a fluorescent system, ensure that the secondary antibody was stored in the dark, as exposure to light can degrade the fluorophore [9] [62] [18].
How can I enhance a weak substrate signal?
To enhance a weak signal, first ensure you are using a highly sensitive detection system. Polymer-based detection reagents are more sensitive than avidin/biotin-based systems and can provide significant signal amplification. You can also try increasing the incubation time with the substrate during the development step, but monitor this carefully under a microscope to prevent over-staining [63].
Troubleshooting Tables for Common Issues
Table 1: Troubleshooting Secondary Antibody Problems
| Possible Cause | Specific Issue | Recommended Solution |
|---|---|---|
| Cross-reactivity | Secondary antibody binds to endogenous immunoglobulins in the tissue. | Use a secondary antibody pre-adsorbed against the species of your tissue sample. [62] [3] |
| High Concentration | Non-specific binding causes high background staining. | Titrate to find the optimal dilution; reduce concentration. [9] [62] |
| Incompatible Host | Secondary antibody does not recognize the primary antibody's host species. | Confirm the secondary antibody targets the host species of your primary (e.g., anti-rabbit for rabbit primary). [62] [3] |
| Endogenous Enzymes | Peroxidase or phosphatase activity creates background with enzyme-based substrates. | Quench activity before primary antibody incubation: use 3% Hâ‚‚Oâ‚‚ for peroxidases or levamisole for phosphatases. [9] [62] [63] |
Table 2: Troubleshooting Substrate Reaction Problems
| Possible Cause | Specific Issue | Recommended Solution |
|---|---|---|
| Inhibited Enzyme | HRP activity is impaired by sodium azide or contaminated water. | Avoid azide in buffers; use fresh, high-purity water. Perform a functionality test on nitrocellulose. [9] [62] |
| Incorrect Buffer | The substrate buffer pH is suboptimal for the enzyme. | Prepare the substrate at the proper pH specified in the protocol. [9] |
| Incompatible Buffer | Using phosphate buffer with an Alkaline Phosphatase (AP) system. | Use the recommended buffer system for your enzyme (e.g., avoid phosphate buffers for AP). [62] |
| Weak Sensitivity | Insufficient signal amplification from the detection system. | Switch to a more sensitive polymer-based detection system. [63] |
Experimental Protocols for Verification
Protocol 1: Verifying Enzyme-Substrate Functionality
This test checks if your enzyme and substrate are working together properly.
- Materials: Detection enzyme (e.g., HRP-conjugated antibody), prepared substrate (e.g., DAB), piece of nitrocellulose membrane.
- Method: Place a single drop of the detection enzyme directly onto the nitrocellulose membrane. Immediately dip the membrane into the prepared substrate solution.
- Interpretation: A colored precipitate should form rapidly at the spot where the enzyme was applied. If no color develops, the enzyme, substrate, or both are inactive or incompatible. Replace with fresh reagents [9].
Protocol 2: Testing for Secondary Antibody Cross-Reactivity
This control experiment is essential to identify non-specific binding.
- Materials: Tissue section, all reagents except the primary antibody.
- Method: Run your IHC protocol in parallel on two tissue sections. For the test slide, apply the primary and secondary antibodies as usual. For the negative control slide, apply the blocking solution and then the secondary antibody only (omit the primary antibody).
- Interpretation: If the test slide shows staining but the negative control slide is clean, the signal is specific. If the negative control shows staining, your secondary antibody is binding non-specifically, and you must implement better blocking or find a more specific secondary antibody [63] [3].
Workflow for Systematic Diagnosis
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Detection Troubleshooting
| Reagent | Function in Troubleshooting | Key Consideration |
|---|---|---|
| Pre-adsorbed Secondary Antibody | Reduces non-specific cross-reactivity with serum proteins in the studied tissue. | Ensure it is adsorbed against the species of your tissue sample (e.g., mouse-adsorbed for mouse tissue). [62] [3] |
| Polymer-Based Detection System | Increases sensitivity and reduces background compared to avidin-biotin (ABC) systems. | Ideal for targets with low abundance or when endogenous biotin is high. [63] |
| Normal Serum | Used for blocking non-specific binding sites. | Should be from the same species as the host of the secondary antibody. [9] [3] |
| Enzyme Inhibitors | Quenches endogenous enzyme activity that causes high background. | Use 3% Hâ‚‚Oâ‚‚ for peroxidases; Levamisole for alkaline phosphatases. [9] [62] [63] |
| Signal Amplification Kits | Enhances weak signals from low-abundance targets. | Can be used when primary antibody titration and sensitive detection are insufficient. [62] |
FAQs on Deparaffinization
What are the consequences of incomplete deparaffinization?
Incomplete deparaffinization prevents antibodies and detection reagents from accessing the tissue, leading to weak staining, no staining, or high, spotty background [64] [65] [66]. Paraffin acts as a physical barrier, and if not thoroughly removed, it will block epitope exposure during retrieval and antibody binding during subsequent steps.
How can I ensure my deparaffinization is effective?
- Use Fresh Xylene: Always use fresh xylene solutions for de-waxing [64] [65] [67]. Old, contaminated xylene is less effective.
- Verify Oven and Heat Pad Function: If using an automated system, ensure the heating elements for the deparaffinization step are working correctly to fully melt the paraffin [66].
- Increase Incubation Time: If problems persist, increase the deparaffinization time in xylene to ensure complete paraffin removal [65] [67].
FAQs on Permeabilization
Why is permeabilization necessary, and when is it required?
Permeabilization is essential for antibodies to access intracellular targets located within the cell, such as those in the nucleus or cytoplasm [67]. It creates pores in the cell membrane, allowing large antibody molecules to pass through.
- For FFPE tissues, permeabilization is typically required if you are using formaldehyde-based fixatives, which do not adequately permeabilize membranes [65].
- For frozen tissues fixed with methanol or acetone, these fixatives themselves permeabilize the cells, so an additional step is often unnecessary [68].
How do I troubleshoot failed permeabilization?
- Add a Permeabilization Agent: Incorporate a detergent into your blocking buffer or antibody dilution buffer. Common agents include 0.2% Triton X-100 or 0.5% Tween-20 [65] [67].
- Optimize Concentration and Time: The concentration of the detergent and the incubation time may require optimization. Excessive permeabilization can damage tissue morphology.
FAQs on Tissue Drying
Why is it critical to prevent tissue sections from drying out?
Allowing tissue sections to dry at any point during the staining procedure causes irreversible, non-specific antibody binding, leading to excessive background staining across the entire tissue section [2] [3].
What are the best practices to keep tissues hydrated?
- Use a Humidified Chamber: Perform all incubation steps in a sealed humidity chamber to prevent evaporation [2] [3].
- Ensure Full Coverage: Always verify that liquid reagents fully cover the tissue section and that slides are kept level during incubations [65] [68].
- Avoid Long Intervals: Do not leave slides exposed to air for extended periods between protocol steps.
Troubleshooting Tables for Sample Preparation Errors
Table 1: Troubleshooting Deparaffinization and Permeabilization
| Potential Problem | Root Cause | Recommended Solution |
|---|---|---|
| Weak or No Staining | Incomplete deparaffinization creating a paraffin barrier [64] [65]. | Increase deparaffinization time; always use fresh xylene [67]. |
| Antibodies cannot access intracellular/nuclear targets [67]. | Add a permeabilizing agent (e.g., 0.2% Triton X-100) to blocking and antibody buffers [65] [67]. | |
| Epitopes masked by formalin fixation cross-links [9] [2]. | Perform robust Heat-Induced Epitope Retrieval (HIER) [9] [64]. | |
| High Background Staining | Incomplete deparaffinization causing spotty, uneven staining [64] [66]. | Repeat with new sections and fresh xylene; check automated system heaters [66]. |
| Tissue sections dried out during staining, causing non-specific binding [2] [3]. | Perform all steps in a humidified chamber; ensure tissues stay fully covered [65]. |
Table 2: The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Solution | Primary Function in Troubleshooting |
|---|---|
| Fresh Xylene [64] [65] | Ensures complete removal of paraffin wax from FFPE sections, preventing barriers to reagent penetration. |
| Triton X-100 or Tween-20 [65] [67] | Permeabilizes cell membranes to allow antibody access to intracellular epitopes. |
| Sodium Citrate Buffer (pH 6.0) [9] | A common buffer for Heat-Induced Epitope Retrieval (HIER) to reverse formalin cross-linking. |
| Humidity Chamber [2] [3] | Prevents evaporation and tissue drying during long incubation steps, avoiding high background. |
| Normal Serum (e.g., Goat, Donkey) [64] [69] | Blocks non-specific binding sites to reduce background; should match the host species of the secondary antibody. |
| Hydrogen Peroxide (Hâ‚‚Oâ‚‚) [9] [64] | Quenches endogenous peroxidase activity, reducing false-positive signals in HRP-based detection. |
Workflow Diagrams for Error Correction
Deparaffinization Troubleshooting Logic
Permeabilization and Staining Process
Validating Your IHC Results: Controls, Comparisons, and Specificity
The Essential Role of Positive and Negative Controls in IHC
Why are controls absolutely essential in IHC experiments?
Controls are the foundation of any valid immunohistochemistry (IHC) experiment. They are necessary to confirm that the observed staining pattern is accurate and reliable, and they help distinguish specific signal from artifacts [70] [71]. Simply put, an immunohistochemical assay that lacks controls cannot be validly interpreted [70]. Controls help build a convincing case for the presence or absence of a probed molecule, which is critical for both accurate research conclusions and clinical diagnostics [70].
What are the different types of controls, and what does each one tell you?
Controls in IHC can be broadly divided into tissue controls and reagent controls. Each serves a distinct purpose in validating your experiment.
- Tissue Controls verify that the staining protocol is working correctly and that the results are specific to the target antigen.
- Reagent Controls help identify non-specific binding caused by the detection system or the antibodies themselves.
The table below summarizes the key controls and their interpretations.
Table 1: Types of Controls in IHC and Their Purpose
| Control Type | Description | Purpose | Interpretation of Result |
|---|---|---|---|
| Positive Control [71] | A tissue or cell sample known to express the target antigen. | Verifies the entire IHC procedure is working correctly. | Staining in the positive control validates the protocol. Lack of staining indicates a problem with the protocol or reagents [72]. |
| Negative Control [71] | A tissue or cell sample known not to express the target antigen. | Checks for non-specific signals and false positives. | No staining should be observed. Any staining indicates non-specific binding or background [71]. |
| No Primary Antibody Control [71] | The primary antibody is omitted and replaced with buffer. | Controls for non-specific binding of the secondary antibody and detection system. | Any staining indicates the secondary antibody is binding non-specifically to the tissue [70] [71]. |
| Isotype Control [71] | A non-immune antibody of the same isotype and concentration as the primary antibody is used. | Controls for non-specific binding caused by the primary antibody. | Staining should be negligible. Significant staining indicates non-specific interaction of the primary antibody with the tissue [71]. |
The relationships between these controls and the experimental result are crucial for correct interpretation.
What are the best practices for selecting and using controls?
Selecting Controls
- Positive Controls: The most rigorous is a positive anatomical control—a site within your specimen known to express the antigen [70]. Alternatively, an external control (a separate slide with a known positive tissue) is used. For example, an antibody for insulin should stain the beta cells in a pancreas control section [70].
- Negative Controls: These can be tissues known to lack the antigen or, more commonly, reagent controls like the isotype control or the no-primary-antibody control run on your experimental tissue [71] [73].
Common Missteps to Avoid
- Omission is not a control: Omitting the primary antibody only checks for secondary antibody specificity; it does not prove the primary antibody is binding specifically to your target [70].
- Beware of absorption controls: While sometimes used, absorption controls (pre-incubating the antibody with its immunogen) only demonstrate the antibody binds to that specific molecule, not that it is binding to that same target in the tissue. It is considered a weak control for identity [70].
How do controls help troubleshoot common IHC problems like no staining or high background?
Controls are your first line of defense when troubleshooting. They help you pinpoint where in the complex IHC protocol a problem has occurred.
Table 2: Using Controls for IHC Troubleshooting
| Problem | Control Results | Likely Cause | Solution |
|---|---|---|---|
| No or Weak Staining [72] [2] [74] | Positive Control: No stainingExperimental Tissue: No staining | The IHC protocol or reagents have failed. The issue is not with the sample itself. | Check antibody activity and storage conditions [2] [74]. Verify detection system is functional [2]. Optimize antigen retrieval methods [72] [2]. |
| Positive Control: Good stainingExperimental Tissue: No staining | The target protein may not be present in the experimental tissue, or there may be sample-specific issues like over-fixation [72] [2]. | Run a different positive control to confirm. Check literature for protein expression. Optimize antigen retrieval for that specific tissue [2]. | |
| High Background Staining [9] [72] [74] | No Primary Control: High background | The background is caused by non-specific binding of the secondary antibody or detection system. | Ensure adequate blocking [72] [74]. Use a secondary antibody that has been pre-adsorbed against the sample species [9] [74]. Increase wash stringency and time [72]. |
| Isotype Control: High backgroundNo Primary Control: Clean | The background is caused by non-specific binding of the primary antibody. | Titrate the primary antibody to a lower concentration [9] [2]. Add NaCl to the antibody diluent to reduce ionic interactions [9]. Change to a more specific antibody. |
The following workflow provides a systematic approach to diagnosing these issues using your control results.
What are the essential reagent solutions for implementing proper controls?
Having the right reagents is crucial for executing the controls described. The following table lists key materials and their functions.
Table 3: Research Reagent Solutions for IHC Controls
| Reagent / Material | Function in Controls | Key Considerations |
|---|---|---|
| Validated Positive Control Tissues [70] [73] | Provides a known biological reference for expected staining pattern. | Can be external (separate slide) or an internal area within the test specimen [70]. |
| Isotype Control Antibody [71] | Matches the primary antibody's species and immunoglobulin class to identify non-specific Fc-mediated binding. | Must be used at the same concentration as the primary antibody [71]. |
| Normal Serum [9] [72] | Used as a blocking agent to reduce non-specific background staining. | Should be from the same species as the secondary antibody [9]. |
| Antibody Diluent [72] | The solution used to dilute the primary and secondary antibodies. | The composition (e.g., presence of NaCl, BSA) can affect specificity and background [9] [72]. |
| Polymer-Based Detection Reagents [72] | Used for signal detection; often more sensitive and produce less background than biotin-based systems. | Helps avoid background from endogenous biotin in tissues like liver and kidney [72]. |
Validating Antibody Specificity for IHC Applications (FFPE vs. Frozen)
A foundational challenge in immunohistochemistry (IHC) research is ensuring that an antibody specifically binds to its intended target protein within the complex milieu of a tissue sample. This challenge is magnified when comparing results across different sample preparation methodologies, particularly formalin-fixed paraffin-embedded (FFPE) versus frozen tissues. The core thesis of this technical support guide is that systematic troubleshooting of "no staining" or "weak signal" problems must begin with rigorous, application-specific antibody validation. The chemical modifications induced by formalin fixation and paraffin embedding can alter protein epitopes, meaning an antibody validated for frozen sections may fail entirely on FFPE tissues. This guide provides detailed protocols and troubleshooting frameworks to help researchers and drug development professionals confidently verify antibody performance, ensuring reliable and reproducible experimental outcomes in their IHC experiments.
Understanding Your Sample: FFPE vs. Frozen Tissues
The choice between FFPE and frozen tissue preparation involves a fundamental trade-off between superior morphological preservation and optimal antigenicity. Understanding the inherent properties and processing requirements of each sample type is the first step in selecting and validating an appropriate antibody.
- Frozen Tissues are snap-frozen, typically in liquid nitrogen or on dry ice, which rapidly preserves the tissue in a state close to its native condition. This process helps retain the native structure of protein epitopes, making it often easier to achieve successful antibody binding without additional retrieval steps. A key advantage is that it is the preferred method for detecting labile post-translational modifications, such as protein phosphorylation [75]. The primary disadvantage is the potential for ice crystal formation during freezing, which can damage tissue morphology [75].
- FFPE Tissues undergo fixation (usually in formalin) and a dehydration process before being embedded in a paraffin block. This method provides excellent preservation of tissue architecture and allows for long-term storage at room temperature. The major drawback is that formalin fixation creates protein cross-links that can mask the very epitopes that antibodies are designed to recognize. Consequently, a critical and often optimization-heavy step for FFPE tissues is antigen retrieval, which is designed to break these cross-links and expose the hidden epitopes [75].
The table below summarizes the key characteristics of each method:
Table 1: Comparison of Frozen and FFPE Tissue Sample Preparation
| Characteristic | Frozen Tissue | FFPE Tissue |
|---|---|---|
| Tissue Morphology | Can be compromised by ice crystals [75] | Excellent long-term preservation [75] |
| Antigen Preservation | High; epitopes remain in a native state [75] | Often masked by formalin-induced cross-links [75] |
| Antigen Retrieval Required | Typically not required [75] | Almost always required [75] |
| Long-Term Storage | Short-term at -80°C [75] | Indefinite at room temperature [75] |
| Key Advantage | Ideal for phospho-specific targets and labile epitopes [75] | Superior morphology and storage convenience [75] |
Core Methodology: Experimental Protocol for Antibody Validation
A robust validation protocol confirms that an antibody is specific, sensitive, and fit-for-purpose for a specific application and sample type. The following workflow provides a systematic approach.
Detailed Experimental Protocols
1. Sample Preparation and Sectioning
- FFPE Tissues: Cut 4-5 μm thick sections using a microtome. Mount sections on charged slides and dry thoroughly. Deparaffinize and rehydrate the sections by sequential washing in fresh xylene, followed by graded ethanol (100%, 95%, 70%) and finally distilled water [76] [77].
- Frozen Tissues: Cut 5-10 μm thick sections using a cryostat. Mount sections on slides and allow to air dry. After drying, fix the sections in pre-cooled acetone or methanol for 5-10 minutes [75].
2. Antigen Retrieval (Critical for FFPE Tissues) For FFPE tissues, antigen retrieval is mandatory to break protein cross-links formed during fixation [75].
- Heat-Induced Epitope Retrieval (HIER): This is the most common and recommended method.
- Place the deparaffinized and rehydrated slides in a suitable retrieval buffer (e.g., 10 mM Sodium Citrate, pH 6.0, or 1 mM EDTA, pH 8.0-9.0) [75] [76].
- Heat the slides using a microwave oven, water bath, or pressure cooker. A microwave oven is often preferred, though a pressure cooker may enhance signals for some targets [76].
- Heat for 8-20 minutes at ~95-100°C, then allow the slides to cool in the buffer for 20-30 minutes at room temperature [75] [9].
- Rinse slides in distilled water followed by wash buffer (e.g., PBS) [9].
3. Blocking and Permeabilization
- Blocking: To minimize non-specific background staining, incubate the tissue sections with a blocking solution for 30 minutes at room temperature. Common blockers include 5% normal serum (from the species of the secondary antibody), 1-5% BSA, or commercial blocking buffers [75] [76] [77].
- Quenching: If using an HRP-based detection system, quench endogenous peroxidase activity by incubating with 3% Hâ‚‚Oâ‚‚ in methanol or water for 10-30 minutes at room temperature [9] [76].
- Permeabilization: For intracellular targets, especially nuclear proteins, add a permeabilizing agent like Triton X-100 or Tween-20 to the blocking buffer or wash buffer to allow antibody penetration [18] [77].
4. Antibody Incubation and Titration
- Primary Antibody Titration: A key to successful IHC is optimizing the primary antibody concentration.
- Prepare a series of dilutions (e.g., 1:50, 1:100, 1:200, 1:500) of the primary antibody in the recommended diluent [76] [2].
- Incubate the slides with the different antibody dilutions. For many antibodies, incubation overnight at 4°C in a humidified chamber provides the best signal-to-noise ratio [76].
- Wash slides thoroughly 3 times for 5 minutes each with a wash buffer containing a mild detergent like Tween-20 (e.g., PBST or TBST) [76].
- Secondary Antibody Incubation: Incubate with a compatible, species-specific secondary antibody conjugated to an enzyme (e.g., HRP) or a fluorophore for 30-60 minutes at room temperature. Ensure the secondary antibody is validated for IHC [2] [77].
5. Detection and Visualization
- For chromogenic detection (e.g., with HRP), incubate with a substrate such as DAB. Monitor the color development under a microscope and stop the reaction by immersing the slides in water as soon as the specific signal is clear. Over-development can lead to high background [9] [2].
- For fluorescent detection, protect the slides from light after adding the fluorophore-conjugated antibody.
- Counterstain with hematoxylin (for chromogenic) or DAPI (for fluorescent), dehydrate, clear, and mount with an appropriate mounting medium [75] [9].
Troubleshooting Guide: No Staining and Weak Signal
When faced with a lack of expected signal, a systematic investigation of the most common causes is required. The following table outlines the primary culprits and their solutions.
Table 2: Troubleshooting Guide for No Staining or Weak Signal
| Possible Cause | Solution / Corrective Action |
|---|---|
| Incorrect Antibody Selection | Confirm the antibody is validated for IHC and your specific sample type (FFPE vs. frozen) on the manufacturer's datasheet. Always run a positive control tissue known to express the target [76] [2]. |
| Suboptimal Antigen Retrieval (FFPE) | This is a very common cause. Ensure the correct HIER buffer (e.g., citrate vs. Tris-EDTA) is used. Optimize the heating method (microwave vs. pressure cooker), time, and temperature. For some targets, a protease-induced method (PIER) may be more effective [75] [76] [2]. |
| Incorrect Antibody Concentration | The antibody may be too dilute. Perform a titration experiment to determine the optimal concentration. Start with the datasheet recommendation and test a range of dilutions [2] [77]. |
| Antibody Inactivation | Ensure the antibody was stored correctly and is not past its expiration date. Avoid repeated freeze-thaw cycles. Run a positive control to confirm antibody activity [9] [2] [77]. |
| Insufficient Deparaffinization | Incomplete removal of paraffin from FFPE sections can prevent reagent access. Increase deparaffinization time and always use fresh xylene [76] [18] [77]. |
| Incompatible Detection System | Ensure your secondary antibody is compatible with the primary antibody's host species. Test the detection system (e.g., HRP-DAB) on its own to ensure it is active. Polymer-based detection systems often provide greater sensitivity than biotin-based systems [76] [77]. |
| Over-fixation | Prolonged formalin fixation can over-mask epitopes. If possible, reduce fixation time. If dealing with over-fixed tissue, increase the duration or intensity of antigen retrieval [2]. |
| Target Protein Not Present | Verify that your tissue of interest expresses the target protein at detectable levels using a positive control sample [77]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents that are fundamental to successful IHC antibody validation and troubleshooting.
Table 3: Essential Research Reagents for IHC Antibody Validation
| Reagent / Material | Function and Importance in Validation |
|---|---|
| Validated Primary Antibodies | The core reagent. Must be specifically validated for IHC and the sample type (FFPE/frozen). Look for antibodies with Advanced Verification or similar specificity data [9] [2]. |
| Antigen Retrieval Buffers | Critical for FFPE tissues. Common buffers include Sodium Citrate (pH 6.0) and Tris-EDTA (pH 9.0). The optimal buffer can be target-specific [75] [76]. |
| Blocking Reagents | Reduce non-specific background. Options include Normal Serums, BSA, or commercial blocking buffers. The choice can affect the signal-to-noise ratio [75] [76]. |
| Polymer-based Detection Kits | Used for signal amplification and visualization. Often provide higher sensitivity and lower background compared to traditional biotin-avidin systems [76]. |
| Specific Antibody Diluents | Optimized buffers for diluting antibodies. Using the manufacturer's recommended diluent can prevent loss of antibody activity and reduce non-specific binding [76]. |
| Endogenous Enzyme Blockers | Quench the activity of native enzymes in tissues (e.g., peroxidases with Hâ‚‚Oâ‚‚, phosphatases with levamisole) to prevent false-positive signals [75] [9] [76]. |
| Permeabilization Agents | Detergents like Triton X-100 or Tween-20 that create pores in cell membranes, allowing antibodies to access intracellular targets [18] [77]. |
Frequently Asked Questions (FAQs)
Q1: My antibody works perfectly in Western Blot (WB). Why does it fail to stain my FFPE tissue in IHC? This is a common issue. WB uses denatured proteins, while IHC on FFPE tissues requires an antibody to recognize its epitope on a protein that has been cross-linked and conformationally altered by formalin. The epitope recognized by the antibody in WB may be linear, but in IHC, it might be buried or structurally compromised. Always use an antibody that has been specifically validated for IHC applications [77].
Q2: What are the most critical controls to include when validating an antibody for IHC? The most critical controls are:
- Positive Control Tissue: A tissue known to express the target protein at moderate to high levels. This confirms the entire staining protocol is working.
- Negative Control (No Primary Antibody): The primary antibody is omitted and replaced with buffer or an isotype control. This identifies background caused by the detection system or non-specific secondary antibody binding [9] [76].
- Biological Negative Control: A tissue known to lack the target protein, which helps confirm the specificity of the signal observed.
Q3: How can I reduce high background staining in my IHC experiments? High background is often due to non-specific antibody binding. Key solutions include:
- Titrate the primary antibody: Excessive concentration is a primary cause [9] [2].
- Ensure adequate blocking: Use the appropriate serum or protein block for a sufficient duration [75] [77].
- Optimize washing: Increase the number and duration of washes with a buffer containing a mild detergent (e.g., Tween-20) [76].
- Quench endogenous enzymes: Use Hâ‚‚Oâ‚‚ to block endogenous peroxidase activity [9] [76].
- Avoid tissue drying: Never let the tissue sections dry out during the procedure, as this causes irreversible non-specific binding [2] [77].
Q4: Where can I find the specific experimental protocol and recommended dilutions for my antibody? The product datasheet from the manufacturer is the primary resource. Reputable antibody suppliers provide detailed, product-specific protocols that include the recommended antigen retrieval method, antibody dilution, diluent, incubation time, and appropriate controls [76].
Immunohistochemistry (IHC) is a critical technique for visualizing protein expression within tissue architecture, providing essential diagnostic, prognostic, and predictive information in pathology and research [12]. The detection system chosen for IHC experiments significantly impacts both the sensitivity and background of the final stain, making the selection process crucial for obtaining reliable, interpretable results. This guide provides a comparative analysis of available detection systems, focusing on their sensitivity characteristics and propensity for background noise, to assist researchers in selecting optimal methodologies for their specific experimental needs.
Types of Detection Systems
Direct Detection Method
The direct detection method represents the simplest approach, utilizing a primary antibody directly conjugated to a reporter molecule such as an enzyme or fluorophore [42]. This one-step process involves applying the labeled primary antibody directly to the tissue section, where it binds specifically to the target antigen.
Advantages:
- Rapid procedure: Eliminates secondary antibody incubation, reducing total assay time
- Minimal background: Fewer reagent layers decrease potential for nonspecific binding
- Species compatibility: Ideal for tissues with endogenous immunoglobulins (e.g., mouse lymph nodes) where secondary antibodies would cause background [42]
- Multiplexing suitability: Wide fluorochrome availability facilitates multicolor experimental designs [42]
Disadvantages:
- Lower sensitivity: Limited signal amplification makes it unsuitable for low-abundance antigens [42]
- Cost inefficiency: Each primary antibody requires individual conjugation [42]
- Potential antibody impairment: Labeling process may affect antibody affinity, particularly problematic for monoclonal antibodies [42]
Indirect Detection Method
The indirect method employs an unlabeled primary antibody followed by a labeled secondary antibody raised against the species of the primary antibody [22] [42]. This two-step approach provides significant signal amplification as multiple secondary antibodies can bind to each primary antibody molecule.
Advantages:
- Enhanced sensitivity: Signal amplification enables detection of low-abundance targets [42]
- Cost effectiveness: Same secondary antibody can be used with multiple primaries from the same species [42]
- Preserved antibody affinity: Primary antibodies remain unmodified, maintaining full avidity [42]
- Flexibility: Secondary antibodies with different labels can be selected based on experimental needs [42]
Disadvantages:
- Increased background potential: Additional layers increase risk of nonspecific binding [42]
- Additional controls required: More extensive blocking steps are necessary to prevent background [42]
- Species limitations: Secondary antibodies must be carefully matched to primary antibody host species
Enhanced Sensitivity Methods
For challenging targets with very low expression levels, more sophisticated detection systems provide additional signal amplification:
Avidin-Biotin Complex (ABC) Method:
- Utilizes the high-affinity interaction between avidin and biotin
- Biotinylated secondary antibodies are bound by preformed complexes of avidin and biotinylated enzyme
- Provides exceptional sensitivity but may suffer from background due to endogenous biotin in some tissues [9] [42]
Polymer-Based Methods:
- Multiple enzyme molecules and secondary antibodies are attached to a polymer backbone [12] [42]
- Eliminates background from endogenous biotin
- Offers high sensitivity with reduced background compared to ABC methods [12]
Tyramide Signal Amplification (TSA):
- Utilizes the catalytic activity of horseradish peroxidase to deposit numerous labeled tyramide molecules near the antigen-antibody complex [42]
- Provides extremely high sensitivity for detecting minimally expressed markers
- Requires careful optimization to prevent excessive background [42]
Diagram: IHC Detection System Pathways. This flowchart illustrates the different methodological approaches for IHC detection, from simple direct methods to complex amplification systems.
Comparative Analysis of Detection Systems
The table below provides a systematic comparison of the major IHC detection systems based on sensitivity, background potential, and appropriate applications.
Table: Comprehensive Comparison of IHC Detection Systems
| Detection System | Sensitivity Level | Background Issues | Optimal Applications | Protocol Complexity |
|---|---|---|---|---|
| Direct Method | Low [42] | Minimal [42] | High-abundance antigens; tissues with endogenous Igs; multiplexing [42] | Low (one-step) [42] |
| Indirect Method | Moderate [42] | Moderate (requires blocking) [42] | Routine IHC; general laboratory use [22] [42] | Medium (two-step) [42] |
| Polymer-Based | High [12] | Low (no endogenous biotin issues) [12] | Low-abundance targets; FFPE tissues [12] | Medium to High |
| ABC Method | Very High [42] | High (endogenous biotin) [9] | Research applications requiring maximum sensitivity [42] | High (multiple steps) |
| Tyramide Signal Amplification | Very High [42] | Variable (requires optimization) [42] | Minimally expressed markers; demanding targets [42] | High (specialized protocol) |
Troubleshooting Guide: FAQs on Sensitivity and Background Issues
FAQ: How can I improve weak or absent staining in my IHC experiments?
Weak or absent staining represents one of the most common challenges in IHC. The following systematic approach addresses the primary causes and solutions:
Primary Antibody Issues:
- Validate antibody suitability: Confirm the antibody is validated for IHC and your specific application (e.g., FFPE tissue) [2]
- Check antibody storage and expiration: Ensure proper storage conditions and that the antibody is not past its expiration date [2]
- Run positive controls: Always include tissue known to express your target to confirm antibody activity [2]
Antibody Concentration Optimization:
- Perform titration experiments: Test a range of concentrations (e.g., 1:50, 1:100, 1:200) starting from the manufacturer's recommendation [2]
- Consider ready-to-use antibodies: RTU formats provide consistent performance with minimal optimization [22]
Detection System Problems:
- Verify detection system activity: Test secondary antibodies and detection reagents separately to ensure functionality [2]
- Ensure species compatibility: Confirm secondary antibody is matched to primary antibody host species [2]
Antigen Retrieval Optimization:
- Evaluate retrieval method: Heat-induced epitope retrieval (HIER) should use appropriate buffer (citrate pH 6.0 or Tris-EDTA pH 9.0) and sufficient heating [2] [78]
- Adjust retrieval intensity: Over-fixed tissues may require extended retrieval time or higher temperature [2]
FAQ: What strategies effectively reduce high background staining?
High background staining obscures specific signal and compromises interpretation. The table below summarizes common causes and evidence-based solutions.
Table: Troubleshooting High Background Staining in IHC
| Problem Cause | Specific Solutions | Supporting Evidence |
|---|---|---|
| Excessive Primary Antibody Concentration | Titrate to find optimal concentration; reduce antibody concentration [2] [9] | High antibody concentration leads to non-specific binding [2] |
| Insufficient Blocking | Increase blocking serum concentration (up to 10%); use avidin/biotin blocking kits for biotin-based systems; block with normal serum from secondary antibody species [2] [9] | Endogenous enzymes and biotin cause non-specific signal without proper blocking [2] [79] |
| Endogenous Enzyme Activity | Quench peroxidases with 3% H2O2; inhibit phosphatases with levamisole [2] [79] [9] | Endogenous peroxidases and phosphatases contribute significantly to background [9] |
| Hydrophobic Interactions | Add detergent (0.05% Tween-20) to wash buffers and antibody diluents [2] | Detergents minimize non-specific antibody binding to tissue components [2] |
| Secondary Antibody Cross-Reactivity | Use pre-adsorbed secondary antibodies; increase serum blocking concentration; reduce secondary antibody concentration [79] [9] | Secondary antibodies may show affinity for non-target epitopes [9] |
| Chromogen Over-Development | Monitor development microscopically; stop reaction as soon as specific signal is visible [2] | Extended chromogen incubation causes diffuse background [2] |
FAQ: How do I select the appropriate detection system for my specific experiment?
Choosing the optimal detection system requires balancing multiple factors:
Consider Antigen Abundance:
- High abundance targets: Direct or simple indirect methods are typically sufficient [42]
- Low to moderate abundance: Standard indirect or polymer-based systems provide adequate sensitivity [12]
- Minimally expressed targets: High-sensitivity systems like polymer-based, ABC, or tyramide amplification are necessary [42]
Evaluate Tissue Considerations:
- Endogenous biotin-rich tissues (liver, kidney): Avoid ABC methods or implement thorough biotin blocking [9]
- Tissues with endogenous immunoglobulins: Direct methods prevent secondary antibody background [42]
- FFPE versus frozen sections: FFPE tissues generally require more sensitive detection systems [12]
Balance Sensitivity and Background:
- Select the simplest system that provides adequate detection of your target
- Remember that increased sensitivity typically comes with greater background potential [42]
- Polymer systems often offer the best compromise for routine applications [12]
Standardized Experimental Protocols
Protocol: Optimal IHC Staining Procedure for Maximum Sensitivity with Minimal Background
The following protocol incorporates best practices for achieving high-quality IHC results with optimal signal-to-noise ratio [78] [12]:
Sample Preparation:
- Use high-quality sections: Cut thin (4-7 μm), flat sections using charged or adhesive slides to ensure even adhesion [22] [12]
- Ensure optimal fixation: Standardize fixation conditions (type, pH, time, temperature) to preserve antigenicity without over-fixation [22]
- Deparaffinize thoroughly: Use fresh xylene and graded alcohols for complete paraffin removal [79] [12]
Antigen Retrieval:
- Select appropriate retrieval method: Heat-induced epitope retrieval (HIER) using microwave (5-10 minutes at 100°C) or pressure cooker (20 minutes) [78] [12]
- Choose optimal buffer: Citrate buffer (pH 6.0) works for most epitopes; EDTA (pH 8.0-9.0) may be needed for others [2] [78]
- Cool slides properly: Allow 15-30 minutes cooling after retrieval before proceeding [12]
Blocking and Antibody Incubation:
- Block endogenous enzymes: Treat with 3% H2O2 for 10 minutes to quench peroxidases [9] [12]
- Apply protein block: Use 2-10% normal serum from secondary antibody species or BSA for 1-2 hours [9] [12]
- Incubate with primary antibody: Dilute in appropriate buffer; incubate overnight at 4°C for optimal specificity [2] [80]
- Apply detection system: Follow manufacturer recommendations for polymer-based or other detection systems
Detection and Counterstaining:
- Develop chromogen carefully: Monitor development microscopically to prevent over-development [2]
- Apply counterstain judiciously: Use hematoxylin or other counterstain at appropriate concentration to avoid obscuring specific staining [22]
- Dehydrate and mount: Process through graded alcohols, xylene, and mount with appropriate medium [12]
Diagram: Comprehensive IHC Workflow. This flowchart outlines the critical steps in IHC processing, highlighting key decision points that affect sensitivity and background.
Protocol: Systematic Optimization of Detection Systems
When implementing a new detection system or troubleshooting existing methods, follow this systematic optimization approach:
Initial Setup:
- Include comprehensive controls: Always run positive control (tissue with known antigen expression), negative control (no primary antibody), and isotype control simultaneously [22] [12]
- Standardize washing procedures: Use consistent wash duration, volume, and agitation between all steps [22]
- Prevent section drying: Use humidity chambers for extended incubations to prevent irreversible non-specific binding [2]
Titration Experiments:
- Primary antibody titration: Test at least three concentrations bracketing the manufacturer's recommendation [2]
- Secondary antibody/detection system titration: Optimize concentration based on manufacturer guidelines and empirical testing [9]
- Incubation time optimization: Compare room temperature (30-60 minutes) versus overnight (4°C) primary antibody incubation [80]
Troubleshooting Assessment:
- Evaluate signal-to-noise ratio: Assess whether specific staining is sufficiently above background
- Adjust retrieval intensity: If signal remains weak, increase retrieval time or temperature
- Modify blocking conditions: If background persists, increase blocking serum concentration or duration
The Researcher's Toolkit: Essential Reagents and Materials
The table below summarizes key reagents and materials referenced in this guide that are essential for successful IHC detection system optimization.
Table: Essential Reagents for IHC Detection System Optimization
| Reagent/Material | Primary Function | Application Notes |
|---|---|---|
| Charged/Adhesive Slides | Tissue section adhesion | Prevents section loss and ensures even reagent coverage [22] [12] |
| Antigen Retrieval Buffers (Citrate pH 6.0, EDTA pH 8.0-9.0) | Epitope unmasking | Buffer selection depends on specific antibody-epitope requirements [2] [78] |
| Normal Serum (from secondary host species) | Blocking non-specific binding | Reduces background by saturating non-specific binding sites [9] [12] |
| Endogenous Enzyme Blockers (3% H2O2, levamisole) | Quench endogenous enzymes | Critical for reducing background in peroxidase/phosphatase systems [2] [79] [9] |
| Avidin/Biotin Blocking Solutions | Block endogenous biotin | Essential when using ABC detection systems [2] [9] |
| Detergents (Tween-20, Triton X-100) | Reduce hydrophobic interactions | Minimize non-specific antibody binding (0.05-0.1% concentration) [2] [81] |
| Polymer-Based Detection Systems | Signal generation and amplification | Provide high sensitivity without endogenous biotin background [12] |
| Chromogens (DAB, AP Red) | Visualize target antigen | DAB (brown) most common; AP Red useful for melanin-rich tissues [22] |
Question: What is the first thing I should check when my test tissue shows no staining, but my positive control tissue stains correctly?
This result indicates that your immunohistochemistry (IHC) protocol and detection reagents are functioning properly, but an issue is preventing specific antibody binding in your test sample. Your troubleshooting should focus on sample-specific variables [82].
Systematic Troubleshooting Guide for Isolated No Staining
| Possible Cause | Investigation Method | Recommended Solution |
|---|---|---|
| Antigen Availability | Check literature for antigen expression in your specific tissue type and cell population [3]. | Confirm the target is expressed in your test tissue; use a different sample known to express the target. |
| Suboptimal Antigen Retrieval | Test different retrieval buffers (e.g., citrate pH 6.0, Tris-EDTA pH 9.0) or heating methods (microwave, pressure cooker) [2] [82]. | Optimize retrieval conditions: increase heating duration or try a higher-pH buffer [2]. |
| Primary Antibody Concentration | Perform an antibody titration experiment on the test tissue [2] [3]. | Increase the primary antibody concentration or extend the incubation time [3]. |
| Over-fixation | Review fixation time; over-fixation can mask epitopes [5] [2]. | Increase the duration or intensity of the antigen retrieval step [2]. |
| Inappropriate Antibody | Verify the antibody datasheet for validation in IHC and your specific tissue type (e.g., FFPE) [2] [3]. | Use an antibody that is rigorously validated for your specific application and sample type [2]. |
Question: What if both my test sample and positive control show no staining?
A lack of staining in both your test and positive control samples points to a general failure of the IHC protocol itself [82]. The problem lies with the reagents or core procedure, not the specific test sample.
Systematic Troubleshooting Guide for Universal No Staining
| Possible Cause | Investigation Method | Recommended Solution |
|---|---|---|
| Primary Antibody Potency | Check expiration date; test a new aliquot on a known positive sample [9] [2]. | Aliquot antibodies to avoid freeze-thaw cycles; store according to manufacturer's instructions [9]. |
| Detection System Failure | Test the detection system alone (e.g., place a drop of enzyme on nitrocellulose and add substrate) [9]. | Use fresh detection reagents; ensure buffers (e.g., substrate buffer pH) are prepared correctly [9]. |
| Inactive Enzyme Substrate | Verify the substrate is active and prepared correctly; check for inhibitors in deionized water [9]. | Prepare fresh substrate solution with the proper pH; avoid sodium azide in buffers with HRP [9]. |
| Secondary Antibody Inhibition | Test with decreasing concentrations of the secondary antibody [9]. | Reduce the concentration of the secondary antibody if signal increases at lower concentrations [9]. |
| Incorrect Reagent Order or Omission | Carefully review protocol steps for accidental skips or use of wrong reagents [3]. | Include a positive control tissue in every run to monitor overall protocol performance [82]. |
Question: What detailed experiments can I perform to diagnose the root cause?
Experimental Protocol 1: Antibody Titration and Validation
Purpose: To determine the optimal primary antibody concentration that provides strong specific signal with minimal background [2].
Methodology:
- Prepare a series of primary antibody dilutions (e.g., 1:50, 1:100, 1:200, 1:500) in the recommended diluent [82].
- Apply each dilution to consecutive sections of your test tissue and a known positive control tissue.
- Process all slides with the same IHC protocol simultaneously.
- Compare staining intensity and background across the dilution series.
Interpretation: The optimal dilution is the one that yields the strongest specific signal with the cleanest background. A concentration that is too high can cause background, while one that is too low results in weak or no signal [2].
Experimental Protocol 2: Antigen Retrieval Optimization
Purpose: To unmask the target epitope that may have been cross-linked during formalin fixation [5] [82].
Methodology:
- Buffer Selection: Test different antigen retrieval buffers, such as sodium citrate (pH 6.0) and Tris-EDTA (pH 9.0) [2].
- Method Selection: Compare different heating methods: microwave, pressure cooker, or water bath [82]. A microwave oven is often preferred, though a pressure cooker may enhance signals for some targets [82].
- Incubation Time: If staining is weak, increase the retrieval time incrementally (e.g., from 10 minutes to 20 minutes) [2].
Interpretation: The correct retrieval condition will expose the epitope, leading to a strong specific signal. Ineffective retrieval is a common cause of false-negative results [82].
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in IHC Troubleshooting |
|---|---|
| Positive Control Tissue | Verifies that the entire IHC protocol and all reagents are working correctly; essential for interpreting results [82]. |
| Antigen Retrieval Buffers | Reverses formaldehyde-induced cross-links to expose epitopes for antibody binding; critical for FFPE tissues [9] [82]. |
| Antibody Diluent | A specialized buffer for diluting antibodies; its composition (e.g., salts, proteins) can significantly impact signal and background [9] [82]. |
| Polymer-Based Detection System | Offers high sensitivity and avoids background from endogenous biotin, which is common in tissues like liver and kidney [82]. |
| Endogenous Enzyme Block | Quenches activity of endogenous peroxidases (with Hâ‚‚Oâ‚‚) or phosphatases (with levamisole) to reduce high background [9] [82]. |
| Serum Blocking Solution | Reduces nonspecific binding of secondary antibodies; should be from the same species as the secondary antibody host [9] [3]. |
Best Practices for Antibody Validation and Storage to Maintain Potency
For researchers, scientists, and drug development professionals working with immunohistochemistry (IHC), achieving reliable and reproducible results hinges on two fundamental practices: rigorous antibody validation and proper antibody storage. Failures in either area directly manifest in common experimental frustrations such as weak staining, no signal, or high background, compromising data integrity. This guide provides a detailed, actionable framework for establishing robust antibody validation and storage protocols, serving as a critical resource for maintaining reagent potency and ensuring the accuracy of your IHC research.
Antibody Validation: Ensuring Specificity and Reproducibility
Antibody validation is the process of confirming that an antibody is specific, sensitive, and reproducible for its intended application [83]. For IHC, this is not a one-time event but a continuous practice essential for data quality.
Validation vs. Verification: Understanding the Difference
Knowing whether to perform a validation or a verification is the critical first step. The table below outlines the key distinctions.
Table: Key Differences Between Antibody Validation and Verification
| Aspect | Validation | Verification |
|---|---|---|
| Definition | The ultimate test drive; confirms a new test is specific, accurate, and reproducible [83]. | A quality check; ensures changes to an already validated test still meet quality expectations [83]. |
| When to Perform | Introducing a new test, antibody, clone, fixative, detection kit, or platform [83]. | Switching manufacturers for an established clone, changing antigen retrieval methods, moving platforms, or checking new antibody lots [83]. |
| Regulatory Status | Regulated by CAP and CLIA standards [83]. | Regulated by CAP and CLIA standards [83]. |
| Example | Bringing a novel antibody into the lab for the first time for an IHC assay. | Changing the antigen retrieval buffer for a previously validated antibody. |
Key Principles for Validating IHC Assays
The College of American Pathologists (CAP) provides evidence-based guidelines for the analytic validation of IHC assays. Adhering to these principles is critical for clinical and high-stakes research applications [84].
- Use Appropriate Comparators: Validation should involve comparing the new assay's results to a reliable standard. CAP lists several options, ordered here from most to least stringent:
- IHC results from cell lines with known protein amounts ("calibrators") [84].
- Results from a non-immunohistochemical method (e.g., flow cytometry, FISH) [84].
- Results from testing the same tissues in another laboratory using a validated assay [84].
- Expected architectural and subcellular localization of the antigen [84].
- Set Concordance Requirements: For predictive markers, the updated CAP guideline harmonizes the required concordance rate to 90% for all IHC assays when comparing to a validated method [84].
- Validate for Specific Specimen Types: Separate validation is required for IHC performed on cytology specimens or specimens fixed in alternative fixatives, using a minimum of 10 positive and 10 negative cases [84].
- Validate All Scoring Systems: For assays with distinct scoring systems based on tumor site or clinical indication (e.g., PD-L1, HER2), each assay-scoring system combination must be validated separately [84].
Antibody Storage: Preserving Potency and Longevity
Proper storage is fundamental to maintaining an antibody's affinity for its target. Primary antibodies can lose potency due to protein degradation or denaturation caused by improper storage, microbial contamination, pH changes, or repeated freeze-thaw cycles [9].
Best Practices for Storage Conditions
Table: Guidelines for Optimal Antibody Storage
| Factor | Recommendation | Rationale |
|---|---|---|
| Aliquoting | Divide antibodies into small, single-use aliquots [9]. | Prevents contamination and preserves the entire stock from repeated freeze-thaw damage. |
| Temperature | Store lyophilized antibodies at -20°C. For liquid antibodies, consult the datasheet; many are best stored at -20°C or -80°C, but some are stable at 4°C [85]. | Cold temperatures slow degradation. Follow the manufacturer's instructions for the specific product. |
| Buffer & pH | Use the recommended antibody diluent and ensure the pH is within the specified range (typically 7.0 to 8.2) for optimum binding [9]. | Incorrect pH or buffer composition can lead to protein aggregation, loss of function, or high background. |
| Contamination Prevention | Wear gloves and use sterile pipette tips when handling antibodies [9]. For buffers, add 0.01% sodium azide to prevent bacterial growth (Note: DO NOT use azide with HRP-based detection systems) [85]. | Microbial contamination can degrade antibodies and destroy the target epitope. |
| Documentation | Record the date of receipt, opening, and each use. Monitor and document expiration dates [83]. | Ensures traceability and prevents the use of compromised reagents. |
FAQs and Troubleshooting Guide
Frequently Asked Questions
Q1: What is the single most important step to ensure good IHC results? Starting with a highly validated antibody specific for your application is the most critical step. No amount of protocol optimization can compensate for a fundamentally poor or non-specific primary antibody [2].
Q2: How can I test if my antibody has lost potency? Test the primary antibody by staining a tissue sample known to contain the target antigen (a positive control) using various antibody concentrations concurrently with your test sample. If the positive control shows no staining, the antibody has likely lost potency [9].
Q3: We are changing to a new autostainer platform. Is this a validation or verification? Moving to a new platform is considered a major change and requires a full validation to confirm the assay's performance on the new system [83].
Q4: How long can I store cut slides before staining? Slide storage can be variable, but as a best practice, slides should be freshly cut before use. If slides must be stored, keep them at 4°C and ensure the tissue sections never dry out [86] [85].
Troubleshooting Common Problems Related to Antibodies
Table: Troubleshooting Weak Staining and High Background
| Problem | Possible Cause Related to Antibody | Solutions |
|---|---|---|
| Weak or No Staining | Antibody not validated for IHC or specific application (e.g., FFPE) [2]. | Check the datasheet for application validation. Run a positive control tissue [2]. |
| Antibody concentration is too dilute [2]. | Perform a titration experiment to find the optimal concentration [2]. | |
| Antibody has lost potency due to improper storage or excessive freeze-thaw cycles [9] [85]. | Test antibody potency with a positive control. Aliquot antibodies to minimize freeze-thaw cycles [9]. | |
| Inactive secondary antibody or detection system [2]. | Ensure secondary antibody is compatible with the primary host species. Test the detection system separately [2]. | |
| High Background | Primary antibody concentration is too high [2] [9]. | Titrate the antibody to find a lower concentration that reduces non-specific binding [2]. |
| Non-specific binding of the primary or secondary antibody [9]. | Use a secondary antibody that has been pre-adsorbed against the immunoglobulin of the sample species. Increase blocking time [85]. | |
| Insufficient blocking [2]. | Use normal serum from the secondary antibody species for blocking. For biotin-based systems, use an avidin/biotin block [2] [86]. |
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for Antibody Validation and IHC
| Reagent / Material | Function |
|---|---|
| Positive Control Tissues | Tissues known to express the target protein. Critical for validating antibody functionality and potency in every run [2] [86]. |
| Negative Control Tissues | Tissues known not to express the target protein, or using a negative control (e.g., no primary antibody) to assess specificity and background [86]. |
| Cell Pellets (FFPE) | Fixed and paraffin-embedded cell lines with known protein expression levels. Can serve as calibrated controls for validation [86] [84]. |
| Antibody Diluent | A optimized buffer solution to dilute antibodies. Superior to simple buffers like TBST as it often contains stabilizers and blockers to enhance signal and reduce background [86]. |
| SignalStain Boost / Polymer-Based Detection | A highly sensitive polymer-based detection system. More sensitive than avidin-biotin (ABC) systems and avoids background from endogenous biotin [86]. |
| Sodium Azide | A bacteriostatic agent added to antibody stocks (typically 0.01-0.02%) to prevent microbial contamination [85]. |
Conclusion
Resolving IHC no staining and weak signal issues requires a systematic approach that integrates foundational knowledge, optimized methodologies, rigorous troubleshooting, and robust validation. The key takeaways emphasize that successful IHC begins with proper sample preparation and fixation, relies critically on optimized antigen retrieval and antibody concentration, and is validated through the consistent use of appropriate controls. By adopting the diagnostic framework and best practices outlined across the four intents, researchers can transform a frustrating technical hurdle into a reliable, reproducible assay. The future of IHC in biomedical research, particularly in drug development and clinical diagnostics, depends on this level of rigor to ensure that data is both accurate and meaningful, ultimately accelerating the pace of scientific discovery and therapeutic innovation.
References
- 1. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOorLl6z3rjjddx5aMAs2XEhZimFc2LoTJfx0l_ZIw6xrH8edaD-g]
- 2. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 3. Immunohistochemistry Troubleshooting [https://www.antibodies.com/applications/immunohistochemistry/ihc-troubleshooting]
- 4. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOor3l0YwZ36tDNLFxadqTIZm7D9NyQ4WuiRnoVajwl9pHe3iGY3L]
- 5. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 6. BestProtocols: IHC Frozen Tissue—Indirect Method (purified) [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/ihc-frozen-tissue-indirect-method-purified-ab.html]
- 7. Immunohistochemistry Protocols [https://www.antibodies.com/applications/immunohistochemistry/ihc-protocol]
- 8. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooRgvGxjwTJqnRcSOmwvhH47p1WAZDdeCWwk83GoNDWBqLKTqkR]
- 9. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 10. Proper Application of Antibodies for Immunohistochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3929726/]
- 11. Troubleshooting in IHC [https://www.bma.ch/en/blogs/troubleshooting-in-ihc]
- 12. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 13. Immunohistochemistry-IHC | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cellular-imaging/ihc.html]
- 14. IHC Protocol | Step-by-Step Immunohistochemistry Guide [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-protocol?srsltid=AfmBOoqg8WGMYmCCAt4JUWWQgalU6OcIuWxB_cvIZIPfERpMoPGTEN56]
- 15. Immunohistochemistry for Pathologists: Protocols, Pitfalls , and Tips... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 16. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOopFHWqOH3SW9RyP1vVFXIwwVkK8A_LNYU3zZkXvt-H_iSTaS6zX]
- 17. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqHYmJQ8_S8mH5vv08j65vn4mSW-RizEwVFOaTAZoJu0_u13RUO]
- 18. IHC Troubleshooting: No Staining [https://www.sinobiological.com/category/ihc-troubleshooting-no-staining]
- 19. Immunohistochemistry Frozen Troubleshooting: IHC-Fr Help [https://www.novusbio.com/support/support-by-application/immunohistochemistry-frozen/troubleshooting.html?srsltid=AfmBOop2YwmOmx40C84qjWLEhX12lxFu5uaZImvPdHZ3FLKsO8TjEGtG]
- 20. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOooj-CgGIfNnLILHQ1CudB5kcuUdWvArVd9wnQJn0gSWY7naw5C4]
- 21. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoomWkYTnEUNgAjICsZ-hN9RgdQg9Jp1dWpvaT7-ZtoQkm4IJ4fY]
- 22. Intro to Immunohistochemistry (IHC) Staining: Steps & Best ... [https://www.leicabiosystems.com/us/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 23. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOooZdMQDO5fqhUaJXGf29t0351zRa0kA7heCO_heOcA-_nUI5UdF]
- 24. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoo2uuwwWfR1UD9IV-RslAZ3u_yHdoL_fKb6zP45BazBnM3_BgNJ]
- 25. Appropriate Fixation of IHC/ICC Samples [https://www.rndsystems.com/resources/protocols/appropriate-fixation-ihcicc-samples]
- 26. IHC Fixation Optimization: Best Practices for Tissue ... [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-optimization/fixation?srsltid=AfmBOopC-tTDiohgdmyQP1kOiSV6BeA_Io9Jxs4U4dIQZfo_6tZB0A-O]
- 27. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoq-Xijmzj52_aABEzHkg3dsmQilBvOd-WvvUZV_ANMbvo1GY4CJ]
- 28. Antigen Retrieval in IHC: Why It Matters and How to Get ... [https://www.atlasantibodies.com/knowledge-hub/blog/antigen-retrieval-in-ihc-why-it-matters-and-how-to-get-it-right/]
- 29. IHC Epitope Retrieval (HIER vs. PIER) [https://www.novusbio.com/epitope-retrieval?srsltid=AfmBOoq0uWyjdSGxW9K50Nhgw3G2txoyqLfJDZchQUIkBiziDONiNiBV]
- 30. Comparison of Antigen Retrieval Methods for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11417793/]
- 31. Antigen retrieval and permeabilization for IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/antigen-retrieval-and-permeabilization]
- 32. IHC antigen retrieval protocol [https://www.abcam.com/en-us/technical-resources/protocols/ihc-antigen-retrieval]
- 33. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOop4_HYlf5hSjdt7mHlq-41EQkhMob59bAeAm9VpeOgO228XOdnZ]
- 34. Tips for Diluting Antibodies [https://www.rockland.com/resources/tips-for-diluting-antibodies/?srsltid=AfmBOopFpmh9s0tJ4coWjxGautkFuk68lBSOq6DEgY05chvb65Io-BJX]
- 35. IHC Troubleshooting Guide | Common Issues & Fixes | Boster Bio [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting]
- 36. IHC Troubleshooting Guide | Thermo Fisher Scientific - IN [https://www.thermofisher.com/in/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 37. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/]
- 38. Immunofluorescence: Antibody Dilution and Incubation ... [https://blog.cellsignal.com/successful-immunofluorescence-antibody-dilution-and-incubation]
- 39. To select the optimal immunohistochemical staining ... [https://pubmed.ncbi.nlm.nih.gov/40825985/]
- 40. IHC Detection Systems: Advantages and Disadvantages [https://www.novusbio.com/ihc-detection?srsltid=ARcRdnppTkTbNi8vuSnQbDIwGoSXHvb8JiqoYVwDc5HZP9iBGNaaUqHT]
- 41. What are the different detection methods for IHC? [https://www.enzo.com/note/what-are-the-different-detection-methods-for-ihc/]
- 42. Detection Systems in Immunohistochemistry [https://www.intechopen.com/chapters/64808]
- 43. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoru69toUBYsGmVRLpBeWUEhclwmE-FVHIfE3p1cfYwALwS3LgaU]
- 44. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=ARcRdnqC9jpfbvlYCG-6DvMnVNisj9iG_gVEZjm4mjqHDT9ogrW4zoZL]
- 45. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopAG53g62F6gCJ21pRV0OkXGO5xhNIzUQkuOO4r5qcvUf2Szp5f]
- 46. IHC: Staining Protocol - Slide Mounted [https://www.sysy.com/protocols/protocol-ihc-slide]
- 47. Blocking Strategies for IHC [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/blocking-strategies-ihc.html]
- 48. A Guide to Better IHC Staining: Steps, Troubleshooting, ... [https://www.celnovte.com/solution/a-guide-to-better-ihc-staining-steps-troubleshooting-and-optimization/]
- 49. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoofejj1MMU5-6ZEEgQg3UCOddeuPBfO0fgn91mAepT7fAeUpSxr]
- 50. Improving Signal Strength [https://www.jacksonimmuno.com/technical/products/faq/weak-signal]
- 51. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoq-4XxP8Zjj6vj_C9ge97plyKNtA5G_9Kz3JToQClVt5OrI5OR-]
- 52. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoo5Leur42hBKJrlbHwGen7Wnh-askX7ukIdltEkbgRmEivOWBNd]
- 53. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/?srsltid=AfmBOooltx2fU38EFxm5lDUkkyRc6Cs0cdSC8leZvld1LqPfxeBpuFnD]
- 54. IHC Primary Antibody Selection & Optimization [https://www.novusbio.com/primary-antibody-selection-optimization?srsltid=AfmBOoptclncVYJozK0tQ9EE1KIVaYbE9pdGzYhYO99FKs8H-sLx0_hA]
- 55. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOooTqgXZYodytYrzfSwyV8iEOKFJQ7GzxXpIKnmiTpKky1ORKN1X]
- 56. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqUnlal3uu7jQGokDRUSq2ewxzm_bzYx03gzTxibOunM_zYl-rQ]
- 57. Troubleshooting Guide: Immunohistochemistry [https://www.rndsystems.com/resources/technical/troubleshooting-guide-immunohistochemistry]
- 58. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOoqEHdErMOskyi17uj6Khk5LnI_3enq-1F7flz7j4LZrhqX9hqMs]
- 59. Antigen Retrieval in Immunohistochemistry [https://www.bosterbio.com/blog/post/antigen-retrieval-in-immunohistochemistry?srsltid=AfmBOoo5hL28YbVYlOKJlDuSrggdcaWQuEQoZ2r4UZoEFM6izF8xOWcJ]
- 60. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOopmg9C0OZ3YJWwsM9U4pPOr-k2HZELtDPMjK4rVBzSR6_wTOhjN]
- 61. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqVgHCVQXcNzxnqTQGyGjoqRRUp9LzEdIFb7pxibRsqZPIJb6g5]
- 62. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoq6bpkSFatc2K-RKbwC9CRqcjqvheTFZcXaKXBPaaK31T_oteFn]
- 63. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqaDX1WM8dDVSjD1bixPuirLEMonTY1Bg0rs_9mKxmn-F-X51Fu]
- 64. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqTYflVunYkL7afu1ls7e4G14MjlydQ5IPTxQJJWtXtyGxO1aDc]
- 65. Immunohistochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunohistochemistry-troubleshooting/?srsltid=AfmBOorZmxWvjkKob0HDsBziK4eRufIbjyvQKkEWw7CjaUITD4R8CUQK]
- 66. Troubleshooting Immunohistochemistry [https://www.nsh.org/blogs/alisha-yocum/2023/04/13/troubleshooting-ihc]
- 67. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoo7PS4Ja62J0cJakL9bnyLlh5l2VoRBTuakrcsATS4joVRjEU6Y]
- 68. Overcoming Common Challenges with Fluorescent IHC [https://fluorofinder.com/challenges-fluorescent-ihc/]
- 69. Tips and Techniques for Troubleshooting ... [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/protein-biology/immunohistochemistry/antibody-immunohistochemistry-expert-tips-and-techniques?srsltid=AfmBOool7AfrPE48fUgiHFmJYFy0XkSggSp_OSB2bIVmWLccIE4csK3W]
- 70. Controls for Immunohistochemistry: The Histochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4212362/]
- 71. Controls in IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/controls-in-ihc]
- 72. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqsq1Ln6JjrQoZZsH4RJifXl2CsxnYuyNNauVqr370IK1729_9z]
- 73. Positive and negative controls for antibody validation [https://www.euromabnet.com/guidelines/positive-negative-controls.php]
- 74. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoryhGvyB2E882PEVV0DtiAevaTFVonipK8MU9lf0FJkswfLamOD]
- 75. å…疫组化-IHC-å…疫组织化å¦æŠ€æœ¯ - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/life-science/cell-analysis/cellular-imaging/ihc.html]
- 76. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopJu3badegLna46aOvJh4f2QYfNSnn3yzfzwayRj35Vpfxd5ZQd]
- 77. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOopBtYFCxdKhcviSTzkgzX1EgDjHhn0E_UstdmEz-yAk-GiMeIoV]
- 78. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOopxxZa7h8smXHPtdBJ64K6JhVp6OqbykwjR6gUEmltbvtG7wJ_7]
- 79. How to Reduce Background Noise in IHC [https://www.azolifesciences.com/article/How-to-Reduce-Background-Noise-in-IHC.aspx]
- 80. Immunocytochemistry Troubleshooting: ICC Help & ... [https://www.bio-techne.com/applications/imaging/immunocytochemistry/troubleshooting]
- 81. Immunocytochemistry protocol [https://www.abcam.com/en-us/technical-resources/protocols/icc-protocol]
- 82. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqVKgSAi8wAB4er0LNnNfi2mydcnCZz2SskmuNwbpb2K2XZJ4Lm]
- 83. Validation, verification, or optimization? Don't guess [https://www.statlab.com/news/validation-verification-or-optimization]
- 84. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 85. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOopBIALDrnPFs0hsKI348vnCM74dJIp_DDhm6aX8cE0mPTCyNW9a]
- 86. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoozt12F5Rpz2bHrtMXa4Na5_kOy9EYPA68mns1lOmJYxsoRv6CM]