A Complete Guide to Validating Phospho-Specific Antibodies for Immunohistochemistry
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for the rigorous validation of phospho-specific antibodies in Immunohistochemistry (IHC).
A Complete Guide to Validating Phospho-Specific Antibodies for Immunohistochemistry
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for the rigorous validation of phospho-specific antibodies in Immunohistochemistry (IHC). It covers the foundational principles of protein phosphorylation, detailed methodological protocols for assay development, systematic troubleshooting for common pitfalls, and established validation standards to ensure specificity and reproducibility. The guide synthesizes current best practices to empower the development of robust, clinically relevant phospho-specific IHC assays for predictive biomarker discovery and signal transduction research.
Understanding Phospho-Specific Antibodies and Protein Phosphorylation
The Critical Role of Protein Phosphorylation in Cellular Signaling and Disease
Protein phosphorylation, the reversible addition of a phosphate group to serine, threonine, or tyrosine residues, represents one of the most crucial and extensively studied post-translational modifications in eukaryotic cells [1]. This fundamental mechanism regulates virtually every cellular process, including cell cycle progression, signal transduction, apoptosis, and metabolic pathways [2] [3]. The human genome encodes approximately 568 protein kinases that catalyze phosphorylation and 156 protein phosphatases that reverse this process, creating a dynamic regulatory system that controls biological function [2]. It is estimated that over one-third of all human proteins undergo phosphorylation at some point, highlighting the pervasive influence of this modification on cellular physiology [1].
The dysregulation of phosphorylation events constitutes a cornerstone of disease pathogenesis, particularly in oncology, where hyperactive kinase signaling drives tumor development and progression [2] [3]. This understanding has catalyzed the development of kinase inhibitors, with the United States Food and Drug Administration approving 68 small-molecule protein kinase inhibitors as of 2022 [3]. The critical importance of phosphorylation in health and disease has created an urgent need for precise research tools, particularly phosphorylation-specific antibodies that can detect specific phosphorylation events in their native cellular context using immunohistochemistry (IHC) [4] [5].
Phosphorylation-Specific Antibodies: Validation Challenges and Solutions
The Critical Importance of Antibody Validation
Validated phosphospecific antibodies provide invaluable tools for investigating phosphorylation events in situ, but their development and validation present unique challenges. Phospho-epitopes are often transient modifications that may be unstable during tissue processing, and antibodies must distinguish between the phosphorylated and non-phosphorylated forms of the same protein with exquisite specificity [5] [6]. For IHC applications, where cellular context is preserved, rigorous validation is essential to ensure that observed staining patterns accurately reflect the in vivo phosphorylation status rather than technical artifacts [7].
Several studies highlight the importance of comprehensive validation. Researchers validating antibodies against phosphorylated estrogen receptor α (ERα) epitopes emphasized that limited antibody validation might explain contradictory results in the literature regarding correlations with histopathological parameters and clinical outcomes [4]. Similarly, developers of a topoisomerase I phosphorylation (topoI-pS10) IHC assay noted that despite the proliferation of phosphorylation state-specific antibodies, many studies have failed to demonstrate their added value over general antibody IHC, often due to challenges in interpreting complex staining patterns in tissue samples [5].
Essential Validation Methodologies
Table 1: Key Validation Methods for Phosphorylation-Specific Antibodies
| Validation Method | Purpose | Experimental Approach |
|---|---|---|
| Phosphatase Treatment | Confirm phospho-specificity | Treat tissue sections or cell pellets with phosphatase enzymes; specific signal loss confirms antibody depends on phosphorylation [8] [7]. |
| Peptide Blocking | Verify epitope specificity | Pre-incubate antibody with phosphorylated target peptide; competitive binding should abolish specific staining [7]. |
| Cell Line Models | Assess target specificity | Use paraffin-embedded cell pellets with known phosphorylation status or genetically engineered knockout cells [7] [6]. |
| Western Blot Analysis | Demonstrate specificity for appropriate molecular weight | Identify specific bands of correct molecular weight with minimal cross-reactivity [7]. |
| Tissue Microarrays | Evaluate performance across diverse tissues | Test antibody on arrays containing multiple tissue types to assess consistency and specificity [4]. |
| Xenograft Models | Verify performance in tissue-like contexts | Assess antibody staining in xenografts from cell lines with known target expression levels [7]. |
The cornerstone of phospho-specific antibody validation involves demonstrating specificity for the phosphorylated epitope. The most definitive approach utilizes phosphatase treatment, where enzymatic removal of phosphate groups should abolish antibody binding [8] [7]. Cell Signaling Technology, for instance, subjects tissue sections and cell pellets to phosphatase treatment to verify target phospho-specificity as part of their comprehensive validation workflow [7]. Similarly, the Abcam dephosphorylation protocol uses calf intestinal alkaline phosphatase (CIP) to remove phosphate groups from proteins before or after membrane transfer, with successful dephosphorylation resulting in little or no staining compared to untreated samples [8].
Additional validation strategies include peptide blocking experiments, where pre-incubation with the phosphorylated target peptide competitively inhibits antibody binding; use of cell lines with known phosphorylation status; and genetic approaches including knockout validation [7] [6]. For GPCR phosphorylation studies, researchers have developed specialized protocols that maintain phosphorylation during routine immunohistochemical procedures through the inclusion of appropriate phosphatase inhibitors throughout both fixation and staining [6].
Experimental Data: Phosphorylation in Disease and Therapy
Phosphorylation Profiling in Breast Cancer
Comprehensive phosphorylation profiling has demonstrated significant clinical potential in stratifying patient populations and predicting therapeutic responses. A landmark study investigating multiple phosphorylated forms of estrogen receptor α (ERα) in breast cancer exemplifies this approach [4]. Researchers validated several phospho-ERα antibodies for IHC using tissue microarrays containing 450 primary invasive breast cancers, demonstrating for the first time the detection of multiple phosphorylated ERα forms in clinical samples (P-S104/106-ERα, P-S118-ERα, P-S167-ERα, P-S282-ERα, P-S294-ERα, P-T311-ERα, and P-S559-ERα) [4].
Table 2: Phospho-ERα Isoforms Detected in Breast Cancer Tissue Microarrays
| Phospho-ERα Isoform | Antibody Source | Dilution | Prevalence in Breast Cancers | Clinical Correlation |
|---|---|---|---|---|
| P-S104/106-ERα | Bethyl Laboratories | 1:200 | Not specified | Potential for patient stratification [4] |
| P-S118-ERα | Cell Signaling | 1:600 | 48% (177/370 cases) | Positively correlated with total ERα and PgR [4] |
| P-S167-ERα | Abcam | 1:700 | Not specified | Potential for patient stratification [4] |
| P-S282-ERα | Bethyl Laboratories | 1:700 | Not specified | Potential for patient stratification [4] |
| P-S294-ERα | Bethyl Laboratories | 1:800 | Not specified | Potential for patient stratification [4] |
| P-T311-ERα | Bethyl Laboratories | 1:100 | Not specified | Potential for patient stratification [4] |
| P-S559-ERα | Bethyl Laboratories | 1:150 | Not specified | Potential for patient stratification [4] |
The study found that P-S118-ERα expression, detected in 48% of breast tumors, showed a statistically significant positive correlation with total ERα expression and progesterone receptor status, suggesting this phosphorylation event may have particular functional significance in ERα signaling [4]. This comprehensive profiling approach revealed the potential for phosphorylation signatures to identify subgroups of breast cancer patients who might benefit from specific endocrine therapies, moving beyond conventional ERα testing to a more nuanced understanding of receptor activation status [4].
Phosphorylation as a Predictive Biomarker in Cancer Therapy
The development of P-topoIDx, an IHC-based test detecting topoisomerase I phosphorylation at serine 10 (topoI-pS10), exemplifies the translation of phosphorylation biology into clinically applicable predictive biomarkers [5]. This test addresses the critical need to identify patients who will respond to camptothecin analogue therapy (e.g., topotecan, irinotecan), where response rates vary from 13-32% depending on tumor type [5].
The molecular mechanism underpinning this biomarker involves DNA-PKcs-dependent phosphorylation of topoI at serine 10, which promotes ubiquitin proteasomal pathway-mediated degradation of topoI [5]. Cells with higher basal levels of topoI-pS10 rapidly degrade topoI and consequently exhibit resistance to camptothecin-based therapy [5]. During assay development, researchers utilized colon cancer cell lines with divergent topoI degradation phenotypes—HCT15 cells (rapid topoI degradation) versus Colo205 cells (minimal degradation)—to validate antibody specificity, confirming that HCT15 cells exhibited higher topoI-pS10 immunostaining [5].
This example demonstrates how understanding phosphorylation-mediated resistance mechanisms can yield robust predictive biomarkers. The developers established a standardized IHC protocol on an automated platform, optimized digital pathology quantitative analysis, and created a framework for implementing phosphospecific IHC in clinical decision-making [5].
Phospho-Tau in Alzheimer's Disease Treatment Response
Recent investigations into Alzheimer's disease therapeutics have highlighted the utility of phosphorylation biomarkers for predicting both treatment efficacy and adverse effects. A 2025 study examining lecanemab treatment for early Alzheimer's disease demonstrated that baseline cerebrospinal fluid (CSF) levels of phosphorylated tau (ptau181) predicted both cognitive decline and the occurrence of amyloid-related imaging abnormalities (ARIA) during treatment [9].
Patients with high CSF-ptau181 levels (above 78.6 pg/ml, the cutoff derived from ROC analysis for ARIA prediction) showed significantly greater cognitive decline on Mini-Mental State Examination scores at 6 and 12 months compared to the low ptau group [9]. This finding suggests that tau phosphorylation status may identify patient subgroups more likely to benefit from lecanemab therapy, with the low ptau group exhibiting better cognitive outcomes and fewer ARIA events [9]. This research exemplifies how phosphorylation biomarkers can guide therapeutic personalization in neurological diseases, similar to their application in oncology.
Experimental Protocols for Phosphorylation Analysis
Phosphospecific IHC Assay Development
The development of robust phosphospecific IHC assays requires meticulous optimization and validation. The protocol for topoI-pS10 IHC development illustrates key considerations [5]. Researchers established a standardized protocol on an automated stainer (Intellipath auto-stainer, Biocare Medical) with carefully optimized conditions: antigen retrieval in acidic pH citrate buffer (pH 6.0) at 85°C for 30 minutes followed by 75°C for 10 minutes, peroxidase blocking, universal blocking with Biocare Medical sniper block reagent, incubation with anti-topoI-pS10 primary antibody for 2 hours at room temperature, followed by mouse secondary antibody for 15 minutes, and DAB chromogen development for 5 minutes [5].
Critical protocol considerations for phosphospecific IHC include:
- Antigen retrieval optimization: Both time and pH significantly impact phospho-epitope detection
- Blocking conditions: Use of appropriate blocking reagents to minimize non-specific background
- Incubation parameters: Time and temperature optimization for specific antibody-antigen interactions
- Detection system selection: Ensuring sufficient sensitivity while minimizing background
- Control inclusion: Both positive and negative controls essential for interpretation
Protein Dephosphorylation Protocol for Specificity Validation
A fundamental protocol for validating phospho-specific antibody involvement involves enzymatic dephosphorylation [8]. The standard approach uses calf intestinal alkaline phosphatase (CIP) to remove phosphate groups from target proteins:
Pre-SDS-PAGE Dephosphorylation:
- Resuspend protein/lysate in CIP buffer (100 mM NaCl, 50 mM Tris-HCl, 10 mM MgCl2, 1 mM dithiothreitol, pH 7.9) with EDTA-free protease inhibitors
- Add 1 unit CIP per µg of protein to the "+phosphatase" sample
- Incubate for up to 60 minutes at 37°C
- Process samples for SDS-PAGE as usual
Post-transfer Dephosphorylation:
- Transfer proteins to membrane and block with 5% BSA in TBS containing 0.1% Triton X-100
- Cut membrane to obtain duplicate sample pieces
- Incubate one piece in CIP buffer with added CIP enzyme (2 hours at 37°C, overnight at 4°C, or overnight at 37°C)
- Wash membrane 3 times with 1x TBST before continuing with western blotting procedure
Critical considerations include avoiding phosphatase inhibitors (sodium orthovanadate inhibits CIP activity by 90% at 10 mM; 50 mM EDTA inactivates CIP almost completely) and using BSA instead of milk for blocking (as casein in milk is a phosphoprotein that may create background staining) [8].
Advanced Antibody Screening Using Yeast Biopanning
Emerging technologies for developing phosphorylation-specific antibodies include sophisticated screening approaches. A 2024 protocol describes yeast biopanning for screening antibodies specific to protein phosphorylation sites [10]. This method utilizes yeast surface display libraries to identify high-specificity binders through a structured process:
- Library Preparation: Grow and induce yeast cells expressing single-chain variable region fragments (scFv) or nanobodies
- Antigen Presentation: Immobilize phosphopeptides on a layer of biotinylated HEK293FT cell surface using streptavidin
- Negative Selection: Remove clones binding to non-phosphorylated protein using the same amino acid sequence without phosphorylation
- Selection Process: Iterative screening to isolate clones with specificity for the phosphorylated epitope
- Validation: High-throughput specificity analysis through whole-well image analysis in 96-well plates
This approach addresses the challenge of finding rare clones with high specificity for phosphorylated epitopes, which conventional methods often miss [10]. The method's advantage lies in using whole cells for peptide immobilization, which more closely mimics natural presentation compared to direct plate coating.
Signaling Pathways and Experimental Workflows
Phosphorylation-Dependent Signaling Cascades
Protein phosphorylation forms the backbone of intracellular signal transduction, with cascades of sequential kinase activation amplifying and specifying cellular responses to extracellular stimuli [1]. These pathways follow structured architectures:
Cellular Signal Transduction Cascade
These phosphorylation cascades enable cells to respond precisely to stimuli. The balance between kinase and phosphatase activities determines the duration and intensity of signaling events [1]. Dysregulation of these pathways, through kinase mutations, overexpression, or phosphatase loss, contributes significantly to disease states, particularly cancer [2] [3].
Phospho-Specific IHC Validation Workflow
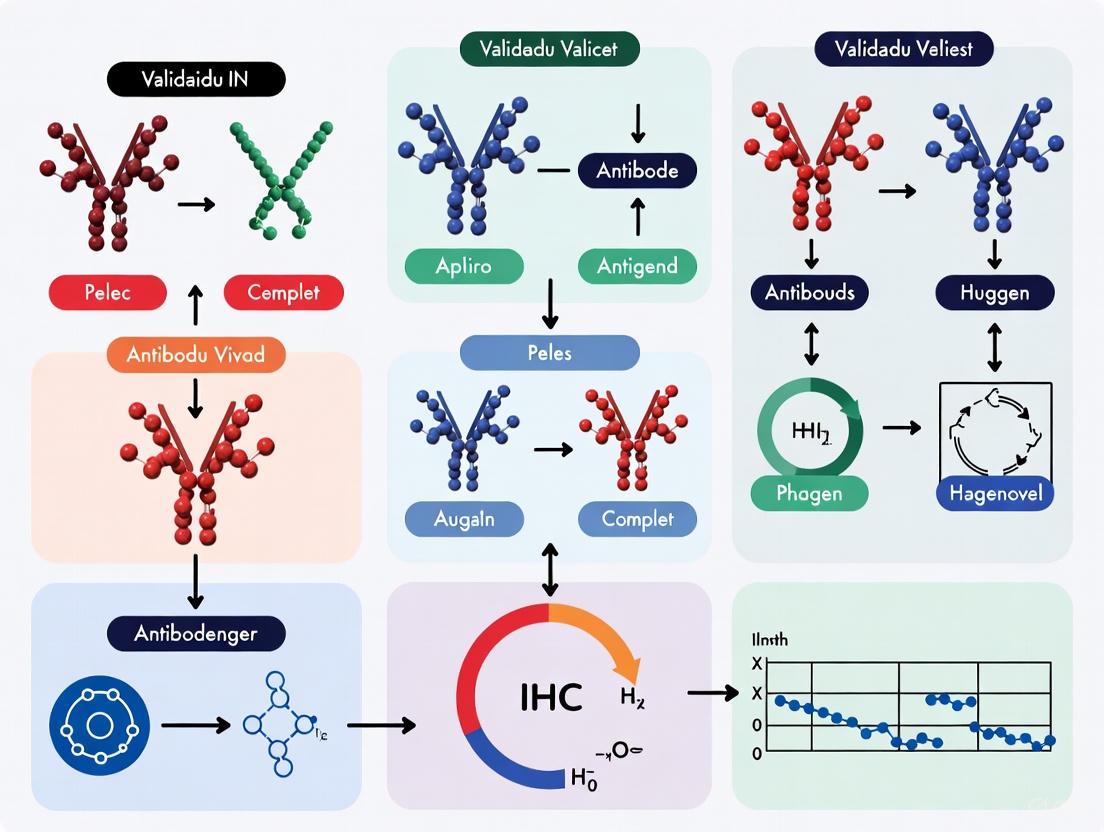
The development and validation of phosphorylation-specific antibodies for IHC follows a systematic workflow to ensure reliability and specificity:
Phospho-Specific IHC Antibody Validation
This comprehensive workflow ensures that phosphospecific antibodies produce accurate, reproducible results in IHC applications. Each validation step addresses specific potential pitfalls: phosphatase treatment confirms phosphorylation dependence, peptide blocking verifies epitope specificity, cell line testing establishes biological relevance, and tissue microarray assessment evaluates performance across diverse samples [5] [8] [7].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Phosphorylation Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Phospho-Specific Antibodies | P-S118-ERα [4], topoI-pS10 [5], pS375-MOP [6] | Detection of specific phosphorylation events in IHC, western blotting |
| Protein Kinase Inhibitors | Imatinib, Capivasertib, Afuresertib [3] | Inhibition of specific kinase activity for functional studies |
| Phosphatases | Calf intestinal alkaline phosphatase (CIP) [8] | Antibody validation through dephosphorylation controls |
| Cell Line Models | HCT15 and Colo205 colon cancer cells [5], transfected 293T cells [7] | Positive and negative controls for assay development |
| Phosphatase Inhibitors | Sodium orthovanadate, EDTA-free protease inhibitors [8] | Preservation of phosphorylation status during sample processing |
| Antigen Retrieval Reagents | Citrate buffer (pH 6.0) [5], CC1 buffer [4] | Optimization of epitope exposure in FFPE tissues |
| Detection Systems | HRP-conjugated secondaries, DAB chromogen [5] | Signal amplification and visualization |
The selection of appropriate research reagents fundamentally determines the success of phosphorylation studies. Phospho-specific antibodies serve as the primary detection tool, with validation being paramount [4] [5] [6]. Kinase inhibitors provide both therapeutic agents and research tools for manipulating phosphorylation states [3]. Phosphatase enzymes like CIP enable critical specificity controls through dephosphorylation [8]. Well-characterized cell line models with known phosphorylation status offer essential positive and negative controls [5] [7]. Phosphatase inhibitors maintain phosphorylation integrity during sample processing, while optimized antigen retrieval reagents ensure adequate epitope exposure in formalin-fixed tissues [4] [5] [8]. Finally, sensitive detection systems enable visualization of often low-abundance phosphorylation events [5].
Protein phosphorylation represents a central regulatory mechanism in cellular signaling, with profound implications for understanding disease mechanisms and developing targeted therapies. The critical role of phosphorylation in conditions ranging from cancer to Alzheimer's disease underscores the importance of robust research tools, particularly validated phosphospecific antibodies for immunohistochemistry. While significant challenges exist in antibody validation, including epitope instability and specificity requirements, comprehensive approaches incorporating phosphatase treatment, peptide blocking, and rigorous biological testing can ensure reliable performance. The continuing development of sophisticated screening methods, such as yeast biopanning, promises to yield increasingly specific research reagents. As phosphorylation-based biomarkers and therapies continue to transform personalized medicine, rigorous validation standards and optimized methodologies will remain essential for advancing both basic research and clinical applications.
How Phospho-Specific Antibodies Differ from Conventional Antibodies
Table 1: Fundamental Differences Between Phospho-Specific and Conventional Antibodies
| Characteristic | Phospho-Specific Antibodies | Conventional Antibodies |
|---|---|---|
| Antigen Recognition | Recognize a specific phosphorylated amino acid within a unique protein sequence (phosphoepitope) [11]. | Recognize an unmodified specific antigen, independent of its phosphorylation state [11]. |
| Biological Information | Detects the active, phosphorylated form of a protein, directly reporting on its functional state and signaling pathway activity [12] [11]. | Detects total protein expression, including both active and inactive forms; cannot discern protein activity [11]. |
| Production Process | Involves synthesis of phosphopeptides, conjugation to a carrier protein, immunization, and stringent screening for phospho-recognition [12] [11]. | Typically uses prokaryotically expressed proteins or unmodified peptides for immunization and antibody production [11]. |
| Experimental Requirements | Require specific conditions to preserve the labile phosphorylation state, including phosphatase and protease inhibitors during sample preparation [11]. | Requirements for sample inhibitors are relatively more lenient [11]. |
| Data Interpretation | Provides a direct readout of signaling activity and protein function; changes indicate pathway modulation [12] [11]. | Serves as an internal reference for total protein levels; changes indicate alterations in protein expression [11]. |
The Critical Role of Validation in IHC Research
For immunohistochemistry (IHC), which preserves the spatial context of protein activity within tissues, rigorous validation of phospho-specific antibodies is paramount [13] [14]. A single validation assay is insufficient; a comprehensive data package is required to confirm that the observed staining is specific and reliable [15] [14].
Table 2: Key Validation Strategies for Phospho-Specific Antibodies in IHC
| Validation Method | Experimental Approach | Interpretation of Positive Result |
|---|---|---|
| Phosphatase Treatment | Treating tissue sections with alkaline phosphatase (AP) or lambda phosphatase to remove phosphate groups [16] [14]. | A significant reduction or complete loss of staining confirms that antibody binding is dependent on the phosphate group [16] [17]. |
| Peptide Blocking | Incubating the antibody with an excess of its target phosphopeptide prior to application on the tissue [4]. | Staining is competitively inhibited, demonstrating binding specificity. Pre-incubation with a non-phosphorylated peptide should not affect staining [4]. |
| Biological Modulation | Using cell or tissue models treated with kinase inhibitors, activators, or ligands known to modulate the target pathway [14]. | Staining intensity correlates with the expected increase or decrease in phosphorylation, confirming biological relevance [18]. |
| Genetic Validation | Using cell lines or tissues where the target protein is knocked down (e.g., via siRNA) or knocked out [15] [14]. | Loss of staining in knockout/knockdown models confirms antibody specificity for the target protein [15]. |
Signaling Pathways and Experimental Workflow
The following diagram illustrates the central role of protein phosphorylation in cellular signaling and the specific detection capability of phospho-specific antibodies.
Validating a phospho-specific antibody for IHC requires a systematic workflow, as outlined below.
Essential Reagents for Phospho-Specific IHC Research
Table 3: Research Reagent Solutions for Phospho-Specific IHC
| Reagent / Solution | Function in the Experimental Process |
|---|---|
| Phosphatase Inhibitors | Added to tissue lysis buffers and during sample preparation to prevent enzymatic removal of phosphate groups by endogenous phosphatases, thereby preserving the phospho-epitope [11]. |
| Phosphopeptides & Control Peptides | Synthetic peptides identical to the target phospho-epitope (for blocking assays) and its non-phosphorylated counterpart (as a negative control) are essential for demonstrating antibody specificity [4] [17]. |
| Alkaline Phosphatase (AP) / Lambda Phosphatase | Enzymes used in validation assays to dephosphorylate proteins on tissue sections; loss of staining confirms the antibody is phospho-specific [16] [18]. |
| Cell/Tissue Models with Modulated Pathways | Genetically modified cells (e.g., knockouts) or tissues treated with specific kinase inhibitors/activators provide biologically relevant systems for validation [15] [14]. |
| Validated Total Target Protein Antibodies | Antibodies that recognize the total protein (phosphorylated and non-phosphorylated) are crucial as loading controls and to correlate phosphorylation status with total protein expression [18]. |
Application in Disease Research: The Case of Phospho-ERα in Breast Cancer
The power of phospho-specific IHC is exemplified by research on Estrogen Receptor α (ERα) in breast cancer. ERα is phosphorylated at multiple sites (e.g., S104, S106, S118, S167), which regulates its activity [4]. Studies using validated phospho-specific antibodies on formalin-fixed, paraffin-embedded breast tumor samples have successfully detected these distinct phosphorylated ERα forms [4]. This capability opens the door to profiling phosphorylation patterns to better understand tumor biology and predict patient response to endocrine therapies, moving beyond simple analysis of total ERα expression [4].
Immunohistochemistry (IHC) is an indispensable technique for visualizing protein distribution and abundance within tissue samples, playing a vital role in both research and clinical diagnostics [19]. However, the detection of phosphorylated proteins introduces specific technical hurdles that can compromise data reliability. This guide objectively compares the core challenges—epitope masking, epitope lability, and low antigen abundance—faced when validating phospho-specific antibodies for IHC, providing experimental data and methodologies to aid researchers and drug development professionals.
Phospho-specific antibodies are designed to detect proteins that have been modified by phosphorylation at specific amino acid residues (serine, threonine, or tyrosine). This post-translational modification is a key regulator of cellular signaling, and its accurate detection in situ provides critical insights into biological processes and disease states [20]. Unlike antibodies against total protein, phospho-specific antibodies are particularly challenging to validate due to the transient nature of phosphorylation, the low stoichiometry of the target, and the fragility of the phosphoester bond [20] [21]. Successful IHC depends on a multi-step workflow where each stage—from tissue collection to imaging—can significantly impact the final result. The table below outlines the primary vulnerabilities for phospho-epitopes at each stage.
Table: Key Vulnerabilities for Phospho-Epitopes in the IHC Workflow
| IHC Workflow Stage | Primary Vulnerability | Impact on Phospho-Epitope |
|---|---|---|
| Tissue Collection & Fixation | Delay in fixation, improper fixative choice [4] [20] | Rapid dephosphorylation and proteolysis (Lability) [20] |
| Fixation | Over-fixation with strong cross-linkers [22] [19] | Epitope masking due to cross-linking [19] |
| Embedding & Sectioning | Antigen retrieval inefficiency [19] | Persistent epitope masking [19] |
| Antibody Incubation | Low abundance of target [23] | Weak or false-negative signal [23] |
Challenge 1: Epitope Masking
Epitope masking occurs when the target antigenic site is physically obscured, primarily by formaldehyde-induced protein cross-links during fixation. This prevents antibody binding and leads to false-negative results [19].
Experimental Evidence and Protocols
A comprehensive study validating phospho-ERα antibodies highlighted that fixation is a critical parameter. While 10% neutral buffered formalin is standard, over-fixation can mask epitopes, requiring optimization for each specific phospho-antibody [4]. The study utilized an automated tissue immunostainer with heat-induced antigen retrieval in a citrate buffer (CC1) to reverse the cross-linking for multiple phospho-ERα epitopes, including P-S118-ERα and P-S167-ERα [4].
Detailed Protocol: Antigen Retrieval for Unmasking Phospho-Epitopes [4]
- Tissue Sectioning: Cut formalin-fixed, paraffin-embedded (FFPE) tissue sections to 5 μm thickness.
- Deparaffinization and Rehydration: Process slides through xylene and a graded ethanol series to water.
- Heat-Induced Epitope Retrieval (HIER):
- Use a citrate-based antigen retrieval buffer (e.g., CC1, Ventana Medical Systems).
- Perform retrieval using an automated stainer or a water bath/steamer at 95-100°C for 20-30 minutes.
- Cooling: Allow slides to cool to room temperature in the retrieval buffer for approximately 20 minutes.
- Immunostaining: Proceed with standard blocking and antibody incubation steps.
Comparative Data on Fixation and Retrieval
The choice of fixative fundamentally impacts the success of antigen retrieval. The following table compares common fixatives based on their mechanism and effect on phospho-epitope detection.
Table: Impact of Fixative Choice on Epitope Masking and Retrieval
| Fixative | Mechanism | Tissue Penetration | Impact on IHC | Compatibility with Phospho-IHC |
|---|---|---|---|---|
| Formaldehyde/PFA | Creates methylene cross-links between proteins [19] | Strong [19] | Can mask epitopes through cross-linking; reversible with HIER [19] | High (Standard for most protocols) |
| Glutaraldehyde | Strong dialdehyde cross-linker [22] [19] | Slower than formaldehyde [19] | Extensive masking; often incompatible with paraffin embedding; high autofluorescence [22] [19] | Low (Typically reserved for EM) |
| Ethanol/Methanol | Precipitates proteins by altering dielectric points [19] | Medium [19] | Poor preservation of morphology; antigen retrieval usually not effective [19] | Variable (Antibody-dependent) |
Epitope Masking and Retrieval Workflow
Challenge 2: Epitope Lability
Phospho-epitopes are highly labile due to the activity of endogenous phosphatases that remain active after tissue excision. The time between surgical resection and tissue fixation (cold ischemia time) is a critical variable that directly impacts the detectability of phosphorylation signals [20].
Experimental Evidence and Protocols
A key study investigating phospho-ERα in breast tumors explicitly examined the effect of tissue collection time. The research used the Manitoba Breast Tumor Bank (MBTB) cohort, where the time from removal to freezing/fixation was documented. The study assessed total ERα and phospho-epitopes (P-S118-ERα, P-S167-ERα) and highlighted that the detection of these phospho-forms could vary with biospecimen collection time, underscoring the instability of these modifications [4].
Detailed Protocol: Preserving Labile Phospho-Epitopes during Tissue Procurement [20]
- Rapid Processing: Minimize the time between tissue devitalization (surgical removal or sacrifice) and immersion in fixative. The target should be less than 30 minutes.
- Use of Inhibitors: Include phosphatase and protease inhibitors in the lysis or initial wash buffer if the tissue is to be frozen. For example, use a commercial Protease/Phosphatase Inhibitor Cocktail (100X).
- Cold Chain: Keep samples on ice whenever possible to slow enzymatic activity.
- Fixative Choice: Rapidly penetrate tissue with fixative. A mixture of paraformaldehyde with a low concentration of glutaraldehyde (0.01–0.05%) can be used, but requires optimization to balance preservation with antigenicity [22].
Quantitative Data on Phospho-Epitope Stability
The following table summarizes factors influencing epitope lability and validated solutions to mitigate this challenge.
Table: Factors and Solutions for Managing Epitope Lability
| Factor | Impact on Lability | Validated Mitigation Strategy | Supporting Experimental Data |
|---|---|---|---|
| Cold Ischemia Time | Direct negative correlation; longer times reduce signal [4] | Standardize and document collection-to-fixation time (<30 min ideal) [4] | Study of 100 ER+ breast tumors showed variability in P-S118-ERα and P-S167-ERα detection linked to collection time [4] |
| Phosphatase Activity | Active phosphatases remove phosphate groups post-excision [20] | Immediate immersion in fixative or lysis buffer containing phosphatase inhibitors [20] | Western blot protocols mandate phosphatase inhibitors in lysis buffer to preserve signal [20] |
| Temperature | Higher temperatures accelerate enzymatic degradation [20] | Maintain cold chain (ice) during tissue procurement [20] | Standard recommendation for preserving phosphorylation state in protein extracts [20] |
Phospho-Epitope Lability and Preservation
Challenge 3: Low Antigen Abundance
Phosphorylated proteins often exist in very low stoichiometric abundance, meaning that at any given time, only a small fraction of the total target protein is phosphorylated. In a background of highly abundant total protein, detecting this low-abundance signal is a significant challenge [23] [20].
Experimental Evidence and Protocols
The dynamic concentration range of proteins in biological samples can span over 12 orders of magnitude. High-abundance proteins can obscure the signal of low-abundance phosphoproteins, making them undetectable without enrichment or signal amplification strategies [23]. For instance, Combinatorial Peptide Ligand Library (CPLL) technology can be used to normalize protein concentrations by reducing high-abundance proteins and concentrating low-abundance ones, making previously undetectable phosphoproteins visible for analysis [23].
Detailed Protocol: Enhancing Detection of Low-Abundance Phospho-Antigens [20]
- Signal Amplification: Use high-sensitivity detection systems such as tyramide signal amplification (TSA) or enzyme conjugates that generate precipitates with high signal-to-noise ratios.
- Controlled Antibody Incubation:
- Incubate primary phospho-specific antibody overnight at 4°C to improve binding.
- Dilute the primary antibody in 5% BSA (not milk) to prevent potential interference.
- Multiplexed Fluorescent Detection: If equipment allows, use fluorescent reporters to multiplex the phospho-protein detection with the total protein simultaneously, providing an internal control for abundance [20].
- Antigen Concentration: For very low abundance targets, consider initial concentration steps such as immunoprecipitation of the target protein before IHC analysis [20].
Comparison of Enrichment and Detection Methods
The table below evaluates different strategies for overcoming the low abundance challenge.
Table: Strategies for Detecting Low-Abundance Phospho-Proteins
| Strategy | Principle | Advantages | Drawbacks |
|---|---|---|---|
| Combinatorial Peptide Ligand Libraries (CPLLs) | Equalizes protein concentrations by saturating binding sites for abundant proteins and concentrating rare ones [23] | Concentration of LAPs; no sample restriction; can be applied to various proteomes [23] | Requires large sample volumes; relatively expensive; typically single-use [23] |
| Immunofluorescence with Signal Amplification | Uses enzymatic or chemical methods to deposit multiple fluorophores or reporters at the antigen site [19] | High sensitivity; allows for multiplexing; compatible with standard IHC workflows [19] [20] | Can increase background noise; requires optimization to avoid over-amplification [19] |
| Prolonged Primary Antibody Incubation | Increases antibody-antigen binding equilibrium by extending incubation time [20] | Simple, low-cost optimization; can significantly enhance signal for rare epitopes [20] | Extends protocol duration; potential for increased non-specific binding [20] |
Overcoming Low Antigen Abundance
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the right reagents is fundamental to developing a robust and validated phospho-specific IHC assay. The following table details essential materials and their functions.
Table: Essential Reagents for Phospho-Specific IHC Validation
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Phosphatase Inhibitors | Preserves labile phospho-epitopes by inhibiting endogenous phosphatases during tissue lysis or processing [20]. | Essential in lysis buffers for Western blotting; should be considered during initial tissue washes for IHC [20]. |
| Citrate-Based Antigen Retrieval Buffer (e.g., CC1) | Reverses formaldehyde-induced cross-links (epitope masking) in FFPE tissues via heat-induced retrieval [4]. | pH and buffer composition are critical for effectiveness; requires optimization for different antibody-antigen pairs [4] [19]. |
| BSA (Bovine Serum Albumin) | Used as a blocking agent and diluent for phospho-specific primary antibodies [20]. | Preferred over milk-based blockers to prevent potential interference with phospho-epitope recognition [20]. |
| Phospho-Peptide for Neutralization | Validates antibody specificity by pre-adsorbing the antibody with its target phospho-peptide [4]. | A reduction in staining upon pre-adsorption confirms specificity. The non-phosphorylated peptide should be used as a control [4]. |
| Combinatorial Peptide Ligand Libraries (CPLLs) | Enriches low-abundance proteins from complex samples prior to analysis, normalizing the dynamic concentration range [23]. | Useful for discovering very low-abundance phospho-targets but may require sample volumes and processing not typical for routine IHC [23]. |
| Phospho-Specific Primary Antibodies | Binds specifically to the phosphorylated form of a protein at a defined amino acid residue [4] [24]. | Requires rigorous validation for IHC. Sources include Bethyl Laboratories, Cell Signaling Technology, and Abcam [4]. |
The journey to a validated phospho-specific IHC assay is fraught with technical challenges, but each can be systematically addressed. Epitope masking demands careful optimization of fixation and antigen retrieval. Epitope lability requires strict control over pre-analytical variables, particularly cold ischemia time. Finally, the inherent low abundance of phospho-targets necessitates sensitive detection methods and potentially sample enrichment.
For researchers, the key to success lies in a rigorous, evidence-based validation workflow that includes appropriate positive and negative controls, such as using isogenic cell lines or peptide neutralization assays [4] [13]. Furthermore, as IHC assays move toward clinical applications, understanding the regulatory landscape—including CLIA validation and FDA submissions for companion diagnostics—becomes paramount [25]. By acknowledging and proactively managing these three core challenges, scientists can generate reliable, reproducible, and biologically meaningful data from phospho-specific IHC, ultimately accelerating biomarker discovery and therapeutic development.
Developing a Robust Phospho-Specific IHC Assay: From Protocol to Platform
The accurate assessment of protein phosphorylation status in tissue specimens has become indispensable for basic research and drug development, particularly in the context of targeted cancer therapies and neurodegenerative disease research. Phospho-proteins serve as direct indicators of signaling pathway activation and represent valuable biomarkers with significant therapeutic and prognostic implications [26]. However, phospho-epitopes present unique challenges for immunohistochemical (IHC) detection due to their exceptional lability during the preanalytical phase of sample processing. The dynamic balance between kinase and phosphatase activities continues ex vivo, and phospho-epitopes are particularly vulnerable to degradation during delays in tissue preservation [27]. Furthermore, the chemical modifications introduced by standard fixatives can mask these epitopes, requiring optimized retrieval methods for successful detection [26] [28]. This guide objectively compares fixation, embedding, and sectioning methodologies to identify optimal protocols that preserve phospho-epitopes while maintaining tissue morphology, providing researchers with evidence-based recommendations for reliable phospho-specific IHC.
Comparative Analysis of Fixation Methods for Phospho-Epitope Preservation
Crosslinking vs. Non-Crosslinking Fixatives
The choice of fixative fundamentally impacts phospho-epitope preservation by determining the extent of protein modification and the subsequent requirements for antigen retrieval.
Table 1: Comparison of Fixation Methods for Phospho-Epitope Preservation
| Fixation Method | Mechanism of Action | Impact on Phospho-Epitopes | Antigen Retrieval Requirements | Morphology Preservation |
|---|---|---|---|---|
| Formalin (Crosslinking) | Forms methylene bridges between amino acid side chains, creating protein crosslinks [28] | Masks epitopes through crosslinking; phospho-epitopes vulnerable to extended fixation [26] [28] | Requires harsh HIER conditions (45 min at 97°C, pH 9.0) [26] | Excellent preservation of cellular structure and tissue architecture [26] |
| PAXgene (Non-Crosslinking) | Combination of alcohols and acid; stabilizes biomolecules without crosslinks [28] | Better preserves phospho-epitopes; less epitope masking [28] | Requires less harsh HIER conditions (shorter microwave treatment) [28] | Good preservation, allowing application of standard diagnostic criteria [28] |
| Acetone/Methanol | Precipitates proteins through dehydration [29] [30] | Good preservation without masking; ideal for frozen sections [30] | No antigen retrieval typically required [30] | Moderate preservation; may cause shrinkage or hardening |
The Critical Variable of Cold Ischemic Time
The time between tissue resection and fixation (cold ischemic time) profoundly affects phospho-epitope integrity. Quantitative studies using automated quantitative analysis (AQUA) technology have demonstrated that phospho-epitopes degrade at different rates during this period [27].
Table 2: Impact of Cold Ischemic Time on Specific Phospho-Epitopes
| Phospho-Epitope | Stability Profile | Quantitative Change | Implications for Research |
|---|---|---|---|
| p-HSP27, p-S6 RP | Increase with prolonged ischemic time | Expression levels rise with increasing delay to fixation [27] | May reflect stress response pathways activated post-resection |
| p-AKT, p-ERK1/2, p-Tyrosine, p-MET | Highly labile | Significant antigenicity loss within 1-2 hours [27] | Require strict ischemic time control (≤1 hour) |
| p-JAK2, p-ER | Relatively stable | Minimal change with increasing ischemic time [27] | More suitable for retrospective studies with variable fixation delays |
Experimental data indicate that delays in formalin fixation as short as 30 minutes can significantly alter the detection of certain phospho-epitopes, necessitating rigorous standardization of tissue collection protocols [27]. For the most labile phospho-epitopes, such as p-AKT and p-ERK1/2, specimen collection should be closely monitored with cold ischemic time not exceeding 60 minutes to ensure accurate measurement [27].
Embedding and Sectioning Methodologies Comparative Data
Paraffin Embedding Versus Frozen Section Preparation
The choice between paraffin embedding and frozen section preparation represents a critical decision point in experimental design, with significant implications for phospho-epitope preservation and detection sensitivity.
Frozen sections are frequently preferred when studying phosphorylated epitopes as the avoidance of formalin fixation and high-temperature processing prevents epitope masking and preserves phosphorylation status [30]. The protocol involves snap-freezing tissue in liquid nitrogen, isopentane, or dry ice, followed by cryostat sectioning and storage at -80°C for up to one year [30]. Frozen sections are typically fixed with alcohols (methanol or acetone) which do not mask epitopes, thereby eliminating the need for antigen retrieval [30]. This approach provides maximum preservation of phospho-epitopes but may compromise morphological detail.
Paraffin embedding following formalin fixation remains the gold standard for morphological preservation but introduces significant challenges for phospho-epitope detection [26] [29]. The embedding process involves dehydration through graded ethanol series (50%-100%), clearing with xylene or substitutes, and infiltration with molten paraffin at 50-60°C [29]. The transition from aqueous to hydrophobic environments at elevated temperatures causes protein unfolding and refolding influenced by formalin-induced crosslinks, potentially further masking epitopes [28]. While this method offers superior morphology and tissue architecture preservation, it necessitates optimized antigen retrieval methods to reverse the masking effects.
Sectioning and Slide Storage Considerations
For paraffin-embedded tissues, sections of 3-10μm thickness are recommended, with drying temperatures not exceeding 37°C overnight to prevent damage to heat-sensitive antigens [29]. For phospho-epitope studies, section drying at 37°C overnight is preferable to higher temperatures as it is less likely to damage heat-sensitive antigens [29]. Storage of pre-cut sections introduces another pre-analytical variable that differentially affects various antigens and epitopes, potentially particularly relevant for retrospective analyses [28].
Experimental Protocols for Optimal Phospho-Epitope Detection
Optimized Antigen Retrieval for Phospho-Proteins
Comprehensive comparative studies have systematically evaluated antigen retrieval methods specifically for phospho-protein detection. The following protocol, validated across 15 different survival phosphoproteins, has demonstrated significant improvements in unmasking efficiency compared to conventional methods:
Superior Retrieval Buffer: Tris-EDTA buffer (pH 9.0) outperforms traditional citrate buffer (pH 6.0) for most phospho-epitopes [26]. In direct comparisons, Tris-EDTA at pH 9.0 unmasked and significantly enhanced the staining of 9 out of 15 phosphoproteins tested (p<0.0001) [26].
Extended Heating Duration: Heating for 45 minutes at 97°C provides superior results compared to the standard 20-minute protocol [26]. This extended duration more effectively reverses the effects of prolonged formalin fixation, which is particularly problematic for phospho-epitope detection [26].
Validation Data: This optimized protocol has been successfully applied to various phospho-epitopes including p-STAT3Tyr705, p-STAT5Tyr694, p-ERK1/2Thr202/Tyr204, and p-AKTSer473, among others [26]. The method is cost-effective and feasible for both clinical and research settings [26].
Comprehensive Workflow for Phospho-Epitope Preservation
The following diagram illustrates the critical decision points in the sample preparation workflow that determine success in phospho-epitope preservation:
Antibody Validation Requirements for Phospho-Specific IHC
Robust validation of phospho-specific antibodies is essential for generating reliable data. Recommended validation steps include:
- Phosphatase Treatment: Pre-treatment of tissue sections with lambda protein phosphatase should significantly reduce or eliminate staining, confirming phospho-specificity [27].
- Western Blot Analysis: Demonstration of specific bands at appropriate molecular weights with minimal cross-reacting bands [31].
- Cell Line Models: Use of paraffin-embedded cell pellets with known target expression levels to verify specificity [31].
- Blocking Peptides: Staining in the presence of control versus phospho-specific peptides to confirm epitope specificity [31].
Research Reagent Solutions for Phospho-Epitope Studies
Table 3: Essential Research Reagents for Phospho-Epitope Studies
| Reagent Category | Specific Product/Formulation | Research Application | Performance Considerations |
|---|---|---|---|
| Fixatives | 10% Neutral Buffered Formalin (NBF) [29] | Standard crosslinking fixation | Requires optimized antigen retrieval for phospho-epitopes [26] |
| Fixatives | PAXgene Tissue System [28] | Non-crosslinking alternative | Better phospho-epitope preservation; milder retrieval needed [28] |
| Fixatives | 100% Acetone or Methanol [29] [30] | Frozen section preparation | Ideal for phospho-epitopes; no retrieval required [30] |
| Antigen Retrieval Buffers | Tris-EDTA Buffer, pH 9.0 [26] | Heat-induced epitope retrieval | Superior for unmasking phospho-epitopes [26] |
| Antigen Retrieval Buffers | Citrate Buffer, pH 6.0 [29] [27] | Conventional antigen retrieval | Less effective for many phospho-epitopes [26] |
| Validation Reagents | Lambda Protein Phosphatase [27] | Antibody specificity testing | Confirms phospho-specificity through enzymatic dephosphorylation [27] |
| Validation Reagents | Phospho-specific Peptides [31] | Antibody blocking controls | Verifies epitope specificity and rules out non-specific binding [31] |
Integrated Workflow for Phospho-Specific Antibody Validation
The following framework integrates sample preparation methodologies within the broader context of phospho-specific antibody validation:
The comparative analysis of sample preparation methodologies demonstrates that phospho-epitope preservation requires integrated optimization across all preanalytical phases. Based on experimental evidence, the following recommendations emerge:
For maximum phospho-epitope preservation, frozen section preparation with alcohol fixation provides superior results, though with compromised morphology.
When morphology is essential, formalin fixation with rigorous control of cold ischemic time (≤60 minutes) and optimized antigen retrieval (Tris-EDTA pH 9.0, 45 minutes at 97°C) offers the best compromise.
For novel fixative approaches, non-crosslinking systems like PAXgene show promise for phospho-epitope preservation but require protocol re-optimization and extensive validation.
Antibody validation must include phospho-specificity testing through phosphatase treatment and appropriate controls, with validation conducted using the same sample preparation methods intended for research use.
The optimal sample preparation strategy depends on the specific phospho-epitopes under investigation, their stability characteristics, and the balance required between morphological preservation and antigen detection sensitivity. By implementing these evidence-based protocols, researchers can significantly enhance the reliability and reproducibility of phospho-specific IHC data for drug development and translational research applications.
Antigen retrieval (AR) is a cornerstone technique in immunohistochemistry (IHC), essential for unlocking antigens masked by formalin fixation and cross-linking in paraffin-embedded tissues. For researchers validating phospho-specific antibodies, mastering AR is not merely a procedural step but a critical determinant of experimental success. These antibodies target specific, often transient, phosphorylation sites—epitopes that are particularly susceptible to masking and conformational changes. The choice between heat-induced epitope retrieval (HIER) and proteolytic-induced epitope retrieval (PIER), the buffer pH, and the heating methodology directly impact the sensitivity, specificity, and reliability of the resulting data. This guide provides a comparative analysis of AR strategies, supported by experimental data and detailed protocols, to equip scientists with the knowledge to optimize IHC for the most demanding targets, including phospho-proteins central to signaling pathway analysis.
The Critical Role of Antigen Retrieval in IHC
Formalin fixation preserves tissue morphology by creating methylene bridges that cross-link proteins. While excellent for structural preservation, this process obscures epitopes, making them inaccessible to antibodies. AR techniques reverse this masking, dramatically enhancing the capability of IHC on formalin-fixed paraffin-embedded (FFPE) tissues [32]. The development of AR in the 1990s effectively divided IHC for FFPE tissues into two eras: pre- and post-AR, marking it as a fundamental milestone that enabled the extensive use of archival tissues for both diagnostics and translational research [32].
For phospho-specific antibodies, which are powerful tools for investigating cell signaling pathways, AR is especially crucial. These antibodies detect specific phosphorylation events on proteins, such as kinases and transcription factors, providing insights into the dynamic regulation of cellular processes [17]. The phospho-epitopes they recognize are often transient, low-abundance, and can be easily altered or hidden by fixation. Therefore, a poorly optimized AR protocol can lead to false-negative results or non-specific background, compromising the validity of the entire experiment. The rigorous validation of these antibodies, as demonstrated in high-throughput studies, often involves genetic strategies (e.g., CRISPR/Cas9 knockout cells) and orthogonal methods to confirm that the signal is specific to the intended phosphorylated epitope [33].
Comparative Analysis of Antigen Retrieval Methods
There are two primary approaches to AR: Heat-Induced Epitope Retrieval (HIER) and Proteolytic-Induced Epitope Retrieval (PIER). The choice between them depends on the nature of the antigen, the tissue type, and the specific antibody.
Heat-Induced Epitope Retrieval (HIER)
HIER is the most widely used AR technique. It involves heating tissue sections in a buffer solution at high temperatures (95-100°C) to break the formaldehyde-induced cross-links [34].
- Advantages: HIER is suitable for a broad range of antigens, is less likely to disrupt tissue morphology, and produces less non-specific staining compared to enzymatic methods [34].
- Disadvantages: Overheating can damage tissues and destroy antigenicity, while insufficient heating may lead to inadequate retrieval. The process requires careful optimization of time, temperature, and buffer pH [34].
Proteolytic-Induced Epitope Retrieval (PIER)
PIER employs proteolytic enzymes like proteinase K, trypsin, or pepsin to digest proteins surrounding the epitopes, thereby exposing the masked antigens [35] [34].
- Advantages: PIER can be more effective for certain difficult-to-recover epitopes, particularly in dense extracellular matrices, and may be less damaging to delicate tissues [35] [34].
- Disadvantages: The technique carries a risk of destroying both the antigen of interest and the tissue morphology if the enzyme concentration and incubation time are not meticulously calibrated. It generally has a lower success rate for restoring immunoreactivity across a wide antibody panel compared to HIER [34].
Head-to-Head Comparison: HIER vs. PIER
A direct comparison of these methods was demonstrated in a study focusing on the detection of Cartilage Intermediate Layer Protein 2 (CILP-2) in osteoarthritic cartilage, a tissue with a voluminous and dense extracellular matrix [35].
Table 1: Comparison of Antigen Retrieval Methods for CILP-2 Staining
| Antigen Retrieval Method | Staining Outcome for CILP-2 | Practical Considerations |
|---|---|---|
| No Retrieval (Control) | Inadequate staining | Confirms the necessity of AR for masked epitopes |
| HIER Only | Suboptimal results | Potential antigen destruction or insufficient unmasking |
| PIER Only | Best results | Effective for glycoproteins in a dense matrix |
| HIER + PIER Combined | No improvement over PIER alone; frequent section detachment | Application of heat reduced the positive effect of enzymes |
This study concluded that for the specific experimental setting of a minor cartilage glycoprotein, PIER alone provided the most abundant and specific staining [35]. The combination of HIER and PIER did not yield better outcomes and, in fact, frequently caused sections to detach from the slides. This highlights the importance of tailoring the AR method to the specific protein and tissue context, rather than assuming that more aggressive retrieval will be beneficial.
Buffer Selection for HIER
The choice of retrieval buffer is a critical variable in HIER, with the pH often being as important as the heating method itself.
Common Buffers and Their Applications
The three most commonly used buffers are citrate, EDTA, and Tris-EDTA, each with different pH profiles and suitability for various antigen classes [36].
Table 2: Common Antigen Retrieval Buffers for HIER
| Buffer | Typical pH | Best Suited For | Experimental Notes |
|---|---|---|---|
| Sodium Citrate | 6.0 | Many cytoplasmic antigens; a traditional, widely used buffer. | May be less effective for some nuclear antigens [34]. |
| EDTA | 8.0 - 9.0 | A broad range of antigens, particularly nuclear proteins. | Often yields stronger staining intensity than citrate buffer [37] [38]. |
| Tris-EDTA | 9.0 | Challenging antigens; often requires robust retrieval. | Recommended when a high-pH buffer is needed [36]. |
The Impact of Buffer pH
The effect of buffer pH on staining results can be categorized into several patterns, which should guide selection when prior information is limited [34]:
- Stable Type: Staining is largely unaffected by pH (e.g., PCNA, CD20).
- V Type: Good staining is achieved at both high and low pH, with poor results at mid-range pH (e.g., ER, Ki-67).
- Increasing Type: Staining improves progressively with increasing pH (e.g., HMB45).
- Decreasing Type: Staining weakens as pH increases (this is rare).
A comprehensive evaluation of AR buffer systems for 29 common diagnostic antibodies found that borate (pH 8.0) and Tris (pH 9.5) buffers yielded the highest retrieved antigen immunoreactivity for most antibodies tested [38]. Furthermore, Cell Signaling Technology, a leader in antibody production, notes that "antibodies that yield an acceptable signal with low pH retrieval (citrate buffer) will generally work well with high pH retrieval (EDTA or Tris-EDTA), but the optimal concentration may not be the same. Antibodies that require the more robust high pH retrieval are unlikely to work as well with low pH retrieval" [37]. Consequently, many experts recommend starting optimization with a high-pH buffer, such as EDTA or Tris-EDTA.
Optimization of Heating Methods for HIER
The method of applying heat during HIER significantly influences the efficiency and uniformity of antigen retrieval.
Pressure Cooking
Pressure cooking is highly effective as it allows the buffer temperature to exceed 100°C, leading to more robust and rapid retrieval.
- Protocol: After bringing the buffer to a boil in a pressure cooker, slides are added, and the lid is secured. Timing begins once full pressure is reached. A typical protocol is 3 minutes at full pressure, followed by rapid cooling under cold water [36].
- Advantages: Faster retrieval and often more potent unmasking, making it suitable for difficult antigens [38].
Microwave Heating
Microwave heating is a common laboratory method, though it can suffer from uneven heating ("hot and cold spots").
- Protocol: Slides are heated in retrieval buffer using a microwave. A typical protocol involves heating at 95°C for 20 minutes (or until boiling in a domestic microwave, then boiling for 20 minutes), followed by a 20-minute cooling period [36].
- Advantages: Rapid heat generation and simplicity.
- Disadvantages: Risk of uneven retrieval and buffer evaporation, which can lead to section drying and detachment [36]. The use of a scientific microwave with temperature control is advised over a domestic microwave.
Steamer and Water Bath Methods
These methods provide gentler, more uniform heating at around 95-100°C.
- Protocol: A vegetable steamer or water bath is pre-heated. Slides in pre-heated buffer are placed inside for 20 minutes, followed by cooling [36].
- Advantages: Reduced risk of section damage and detachment compared to vigorous boiling. A water bath set to 60°C for overnight incubation is a gentle alternative for fragile tissues like bone and skin [36].
Table 3: Comparison of HIER Heating Methods
| Heating Method | Typical Conditions | Advantages | Disadvantages |
|---|---|---|---|
| Pressure Cooker | ~3 min at full pressure | Rapid, highly effective, consistent | Can be too harsh for some tissues/antigens |
| Microwave | 20 min at 95-100°C | Fast, simple, accessible | Uneven heating, high evaporation risk |
| Steamer/Water Bath | 20 min at 95-100°C | Gentle, even heating, low evaporation | Longer processing time |
Experimental Protocols for Antigen Retrieval
Detailed Protocol: HIER Using a Pressure Cooker
This protocol is adapted from Abcam's guidelines and is an excellent starting point for robust antigen retrieval [36].
Materials:
- Domestic stainless steel pressure cooker
- Hot plate
- Slide rack and vessel
- Antigen retrieval buffer (e.g., Tris-EDTA, pH 9.0, or Sodium Citrate, pH 6.0)
Steps:
- Fill the pressure cooker with the chosen AR buffer and place it on a hot plate set to full power. Do not secure the lid yet.
- While the buffer is heating, deparaffinize and rehydrate the tissue sections using standard xylene and ethanol washes.
- Once the buffer is boiling, carefully transfer the slides from the water bath to the pressure cooker.
- Secure the lid as per the manufacturer's instructions. Once full pressure is achieved, start the timer for 3 minutes.
- After 3 minutes, turn off the hotplate, move the pressure cooker to a sink, and activate the pressure release valve. Run cold water over the cooker to depressurize and cool it rapidly.
- Open the lid and run cold tap water into the cooker for 10 minutes to cool the slides further.
- Proceed with the subsequent IHC steps, such as peroxidase blocking and antibody incubation.
Detailed Protocol: Enzymatic Retrieval (PIER)
This protocol is based on the method that proved optimal for CILP-2 retrieval [35].
Materials:
- Proteinase K (e.g., Merck KGaA)
- Bovine hyaluronidase (e.g., Fertipro NV)
- 50 mM Tris/HCl, 5 mM CaCl2 solution (pH 6.0)
- HEPES-buffered medium
- 37°C incubator
- Humidified chamber
Steps:
- Prepare a 30 µg/mL Proteinase K solution in the Tris/HCl/CaCl2 buffer and pre-warm it to 37°C.
- Pipette the enzyme solution onto the tissue section and place the slides in a humidified container.
- Incubate for 90 minutes at 37°C.
- Prepare a 0.4% solution of bovine hyaluronidase in HEPES-buffered medium.
- Treat the same sections with the hyaluronidase solution for 3 hours at 37°C.
- After the enzymatic treatments, rinse the slides under running tap water for several minutes.
- Continue with the standard IHC protocol.
The Scientist's Toolkit: Essential Reagents and Materials
A successful IHC workflow relies on high-quality, specific reagents. The following table details key materials referenced in the protocols and studies above.
Table 4: Essential Research Reagent Solutions for Antigen Retrieval
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Recombinant Phospho-specific Antibodies | High-affinity detection of phosphorylated proteins in signaling pathways. | Sino Biological's Phospho-ERK1/2 (Thr202, Tyr204) antibody used to map MAPK activation in virus-infected cells [17]. |
| Proteinase K | Proteolytic enzyme for PIER; digests cross-linking proteins to unmask epitopes. | Key component in the optimal retrieval protocol for CILP-2 in cartilage matrix [35]. |
| Bovine Hyaluronidase | Enzyme that degrades hyaluronic acid, a major component of the extracellular matrix. | Used in combination with Proteinase K to improve antibody penetration in dense cartilage tissues [35]. |
| Tris-EDTA Buffer (pH 9.0) | High-pH retrieval buffer for HIER; effective for a wide range of antigens. | A commonly recommended starting buffer for AR optimization [37] [36]. |
| EDTA Buffer (pH 8.0) | High-pH retrieval buffer; particularly effective for nuclear antigens. | Identified as a top-performing buffer in comparative studies [38]. |
| Sodium Citrate Buffer (pH 6.0) | Low-pH retrieval buffer; a traditional standard for many antigens. | A widely used buffer, though high-pH alternatives may be more effective for many targets [34]. |
| CRISPR/Cas9 KO Cell Lines | Gold-standard control for validating antibody specificity, including phospho-antibodies. | Used to confirm the absence of signal in knockout cells, ensuring the antibody is not binding non-specifically [33]. |
Visualizing the Antigen Retrieval Optimization Workflow
The following diagram outlines a systematic approach to optimizing antigen retrieval for a new antibody, particularly a phospho-specific one, integrating the concepts and methods discussed in this guide.
Mastering antigen retrieval is a fundamental requirement for rigorous IHC, especially when working with finicky but information-rich phospho-specific antibodies. There is no universal "best" protocol; success lies in a systematic, empirical optimization process. As the comparative data shows, while HIER with a high-pH buffer is a powerful starting point, alternative methods like PIER can be superior for specific antigens in challenging microenvironments. The experimental protocols and optimization workflow provided here serve as a strategic framework. By carefully selecting retrieval buffers, heating methods, and validating results with appropriate controls, researchers can confidently unmask critical epitopes, ensuring that their IHC data is both reliable and reproducible, thereby unlocking the full potential of archival tissue samples for cutting-edge research in signaling biology and drug development.
Immunohistochemistry (IHC) is an indispensable technique in biomedical research and clinical diagnostics, allowing for the specific visualization of protein distribution within the context of preserved tissue architecture. For researchers and drug development professionals, particularly those working with phospho-specific antibodies, standardized staining protocols are not merely a convenience but a necessity. These protocols ensure the reproducibility, reliability, and accurate interpretation of data, which is crucial for validating biomarkers and making informed decisions in therapeutic development. The unique challenge in validating phospho-specific antibodies lies in the lability of the phosphorylation epitope and the potential for subtle changes in fixation or handling to significantly alter staining outcomes. This guide provides a comparative analysis of key protocol variables—antibody dilution, incubation conditions, and detection systems—to establish a robust foundation for IHC research.
Core IHC Protocol Variables: A Comparative Analysis
The journey from a tissue sample to a meaningful IHC result is governed by a series of critical steps. Each step introduces variables that must be carefully controlled to optimize the signal-to-noise ratio, especially for sensitive targets like phospho-epitopes.
Antibody Dilution and Diluents
The concentration of the primary antibody and the composition of its diluent are fundamental to achieving specific staining with minimal background.
- Diluent Composition: A standard antibody diluent stabilizes the antibody and reduces non-specific binding. It often contains a buffered saline solution like PBS at pH 7-7.5, a carrier protein such as 0.2–5% Bovine Serum Albumin (BSA), and a gentle detergent (e.g., 0.01–0.1% Tween 20) to ensure uniform wetting of the sample [39]. For phospho-specific antibodies, using a diluent with dedicated blocking reagents can further enhance specificity.
- Optimization Strategy: The working dilution for a primary antibody must be determined empirically through titration. Using too high a concentration can increase background staining, while too low a concentration may result in a weak or absent signal [40]. The specification sheet provided by the antibody manufacturer should serve as a starting point.
Incubation Parameters
Incubation conditions directly impact the efficiency of the antigen-antibody reaction.
- Time and Temperature: Primary antibody incubation can vary widely, from 1 hour at room temperature to overnight at 4°C [41] [42]. Longer, cooler incubations (overnight at 4°C) are often preferred for phospho-specific antibodies as they can enhance specificity and signal strength [43]. All incubation steps should be performed in a humidity chamber to prevent evaporation and uneven staining [19].
- Washing Steps: Thorough washing between steps is critical to remove unbound and weakly bound antibodies, thereby reducing background [39]. This is typically done with a buffer containing a surfactant, such as PBS with 0.05% Tween 20 (PBS-T), with multiple rinses (e.g., 3 times for 5 minutes each) [41] [44].
Detection System Selection
The choice of detection system is a major determinant of assay sensitivity and signal amplification. The table below compares the most common chromogenic reporters and detection methodologies.
Table 1: Comparison of Common Chromogenic Detection Systems
| Enzyme Label | Common Substrates | Resulting Color | Key Features & Best For |
|---|---|---|---|
| Horseradish Peroxidase (HRP) | 3,3'-Diaminobenzidine (DAB) [39] | Brown to Black [39] | Pros: High turnover rate, good stability, low cost, most popular method [39]. Permanent stain [40]. Cons: Inhibited by cyanides, sulfides, and azides [39]. Endogenous peroxidase must be blocked [44]. |
| Aminoethyl carbazole (AEC) [39] | Red [39] | Alcohol-soluble; requires aqueous mounting media. | |
| Alkaline Phosphatase (AP) | Fast Red [39] | Red [39] | Pros: Optimal activity at basic pH (8-10) [39]. Cons: Inhibited by cyanides, arsenate, inorganic phosphate, and EDTA [39]. Endogenous AP must be blocked with levamisol [44]. |
| NBT/BCIP [39] | Black to Purple [39] | Provides a sharp, precipitate. |
Table 2: Comparison of Detection Methodologies and Their Amplification Efficiency
| Detection Methodology | Principle | Relative Sensitivity | Key Considerations |
|---|---|---|---|
| Direct Detection [39] | Primary antibody is directly conjugated to an enzyme or fluorophore. | Low | Simple and rapid; minimal amplification; suitable for high-abundance targets. |
| Indirect Detection [39] | A labeled secondary antibody binds to the primary antibody. | Medium | Good signal amplification as multiple secondaries bind to a single primary; most common method. |
| Avidin-Biotin Complex (ABC) [39] | Biotinylated secondary is detected by a pre-formed complex of enzyme-linked avidin and biotin. | High | High amplification due to multiple enzyme molecules per complex; can suffer from high background or endogenous biotin interference. |
| Labeled Streptavidin-Biotin (LSAB) [39] | Biotinylated secondary is detected by enzyme-conjugated streptavidin. | High (up to 8x ABC) [39] | Very high sensitivity; smaller complex size than ABC allows better penetration to difficult-to-reach epitopes. |
| Polymer-Based Systems [42] | Multiple secondary antibodies and enzymes are conjugated to a polymer backbone. | Very High | Excellent sensitivity and low background; eliminates endogenous biotin issues; widely used in automated platforms. |
The following diagram illustrates the logical progression and key decision points for selecting and optimizing a detection system for an IHC experiment.
Experimental Protocol for Phospho-Specific IHC
Developing a standardized protocol for phospho-specific IHC requires extra vigilance at every step to preserve the labile phospho-epitope. The following workflow, derived from published methodologies [41] [42] [5], provides a robust foundation.
Standardized IHC Staining Protocol
- Deparaffinization and Rehydration: Bake paraffin sections (4 µm) at 50-60°C. Deparaffinize in xylene and rehydrate through a graded ethanol series to distilled water [41] [42].
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER) using a pressure cooker or decloaking chamber. Heat slides in citrate buffer (pH 6.0) or Tris-EDTA buffer (pH 9.0) at 95-120°C for 10-20 minutes. Cool slides to room temperature before proceeding [39] [42]. The optimal buffer and pH must be determined empirically for each phospho-specific antibody.
- Endogenous Enzyme Blocking: For HRP-based systems, incubate sections with 3% hydrogen peroxide (H₂O₂) in methanol or buffer for 10 minutes to quench endogenous peroxidase activity [41] [44].
- Protein Blocking: Incubate sections with a protein block (e.g., 5-10% normal serum from the secondary antibody species, BSA, or commercial blocking reagents) for 30 minutes to reduce non-specific background [44] [42].
- Primary Antibody Incubation: Apply the optimized dilution of phospho-specific primary antibody in diluent. Incubate for 1 hour at room temperature or, for better sensitivity and specificity, overnight at 4°C in a humidified chamber [43] [41].
- Washing: Rinse slides thoroughly with wash buffer (e.g., PBS-T) 3 times for 5 minutes each [41].
- Secondary Antibody and Detection: Apply the appropriate detection system as per the manufacturer's instructions. For a standard indirect method, incubate with a biotinylated or polymer-based secondary antibody for 30 minutes, followed by another wash step [41] [42]. Then, apply the enzyme (HRP or AP) complex for 30 minutes.
- Chromogenic Development: Incubate sections with the chromogen/substrate (e.g., DAB for HRP) for 1-5 minutes. Monitor development under a microscope and stop the reaction by immersing in distilled water once optimal signal is achieved [41] [42].
- Counterstaining and Mounting: Counterstain with hematoxylin (∼1 minute) to visualize nuclei. Rinse in tap water, dehydrate through graded alcohols, clear in xylene, and mount with a permanent mounting medium [41] [42].
The Scientist's Toolkit: Essential Reagents for IHC
Table 3: Key Research Reagent Solutions for IHC
| Reagent / Solution | Function / Purpose | Examples / Key Components |
|---|---|---|
| Fixatives [19] [44] | Preserves tissue morphology and antigenicity by forming cross-links (formalin) or precipitating proteins (alcohols). | 10% Neutral Buffered Formalin (NBF); Paraformaldehyde (PFA); Acetone/Methanol (for frozen sections). |
| Antigen Retrieval Buffers [42] | Reverses formaldehyde-induced cross-links to unmask epitopes, critical for FFPE tissues. | Citrate Buffer (pH 6.0); Tris-EDTA Buffer (pH 9.0). |
| Antibody Diluent [39] | Stabilizes the antibody during incubation and storage; reduces non-specific binding. | PBS, BSA (0.2-5%), and Tween 20 (0.01-0.1%). |
| Wash Buffer [39] | Removes unbound reagents between steps to minimize background staining. | PBS or TBS with 0.05% Tween 20 (PBS-T/TBS-T). |
| Blocking Solutions [44] | Blocks charged sites and Fc receptors to prevent non-specific antibody binding. | Normal Serum, BSA, or commercial protein blocks. |
| Detection Kits | Provides the components for signal amplification and visualization. | HRP/DAB Kits; Polymer-Based Detection Systems; ABC/LSAB Kits. |
Experimental Data and Performance Comparison
Case Study: Validating a Phospho-Specific Assay
The development of a predictive IHC test for topoisomerase I phosphorylation at serine 10 (topoI-pS10) provides a robust model for phospho-specific antibody validation [5]. The experimental protocol involved:
- Antibody Generation: Mice were immunized with a phosphorylated peptide, and hybridomas were screened via ELISA against both phosphorylated and non-phosphorylated peptides to isolate clones with high specificity [5].
- IHC Specificity Screening: Early hybridoma supernatants were tested on two colon cancer cell lines (HCT15 and Colo205) with known differential levels of topoI-pS10. Clone 1C1.H5.H7 was selected for its ability to differentiate between them [5].
- Protocol Optimization: The finalized IHC assay used acidic pH citrate buffer (pH 6.0) for antigen retrieval at 85°C for 30 min, followed by incubation with the anti-topoI-pS10 mAb for 2 hours at room temperature. Detection was achieved with a mouse secondary antibody and DAB chromogen [5].
Comparative Antibody Performance in Research
A 2023 study aimed at capturing the pathological diversity of alpha-synuclein (aSyn) in Lewy body diseases underscores the importance of using a panel of well-characterized antibodies [45]. The researchers developed and characterized an expanded antibody toolbox targeting different sequences and post-translational modifications (e.g., phosphorylation at Serine 129). They demonstrated that antibodies targeting the C-terminal region could miss N-terminal truncations or other modifications, leading to an incomplete picture of the pathology. This work highlights that for complex targets, a single "standard" antibody may be insufficient, and performance must be validated in the context of the specific biological question.
The path to reliable and reproducible IHC data, especially with phospho-specific antibodies, is paved with rigorous standardization. As demonstrated, the interplay between antibody dilution, incubation conditions, and the choice of detection system profoundly influences experimental outcomes. The adoption of polymer-based detection systems offers a compelling combination of sensitivity and low background, while the validation pipeline for phospho-specific antibodies—exemplified by the topoI-pS10 case study—is non-negotiable. For researchers in drug development, where decisions hinge on accurate biomarker detection, a meticulous, well-documented, and optimized protocol is not just best practice; it is the cornerstone of scientific integrity and translational success.
Protein phosphorylation is the most extensively studied post-translational modification, with approximately 500 kinases in the human genome regulating virtually every aspect of cell function [5]. Deregulated kinase cascades are implicated in numerous disease pathologies, particularly in oncology, creating an urgent need for phosphospecific tests with prognostic or predictive value [5]. However, developing robust phospho-specific immunohistochemistry (IHC) assays presents unique challenges, including the preservation of unstable phosphorylation states during tissue processing and the validation of antibody specificity [5] [6]. This case study examines the systematic development of a predictive phospho-biomarker assay for topoisomerase I (topoI) inhibitor therapy, providing researchers with a framework for assay development while objectively comparing critical reagents and methodologies.
Background: The Therapeutic Challenge and Biological Rationale
Human topoisomerase I inhibitors, including camptothecin and its analogues (topotecan, irinotecan), are used extensively to treat various solid tumors, including metastatic colon cancer, small cell lung cancer, ovarian, pancreatic, gastric, and non-small cell lung cancer [5]. A significant clinical challenge exists as response rates vary considerably by tumor type, ranging from only 13% to 32% [5]. A key mechanism of resistance to this drug class involves the ubiquitin proteasomal pathway (UPP)-mediated degradation of topoI, wherein cells that degrade topoI rapidly demonstrate resistance to camptothecin analogues [5].
Research revealed that DNA-PKcs-dependent basal phosphorylation of topoI at serine 10 (topoI-pS10) enables rapid degradation of topoI and confers camptothecin resistance [5]. This phosphorylation is linked to continual activation of DNA-PKcs, potentially due to failure of upstream effector phosphatases such as PTEN [5]. This molecular understanding provided the foundation for developing P-topoIDx, an IHC-based test that stratifies responder and non-responder patient populations [5].
Table 1: Key Biological Components in the TopoI Phosphorylation Pathway
| Component | Role in Pathway | Therapeutic Significance |
|---|---|---|
| DNA-topoisomerase I (topoI) | Essential enzyme relieving torsional DNA stress during transcription/replication | Molecular target of camptothecin analogues |
| Serine 10 phosphorylation site (topoI-pS10) | Phosphorylation site critical for ubiquitination and degradation | Predictive biomarker for therapy response |
| DNA-PKcs | Kinase that phosphorylates topoI at serine 10 | Central to DNA double-strand break response pathway |
| Ubiquitin Proteasomal Pathway (UPP) | Mediates degradation of phosphorylated topoI | Mechanism of drug resistance |
| PTEN phosphatase | Potential upstream regulator of DNA-PKcs activation | Possible contributor to pathway dysregulation |
Materials and Methods: Systematic Assay Development
Antibody Generation and Validation
The development of a topoI-pS10 mouse monoclonal antibody followed a rigorous multi-stage process [5]:
- Immunogen Design: Four Balb/c mice were immunized with a synthetic 14 amino acid peptide containing phosphorylated serine 10 of topoI conjugated to keyhole limpet hemocyanin (KLH) carrier protein [5].
- Immunization Protocol: Primary immunization used 100 µg of peptide with Freund's Complete Adjuvant, followed by two boosts every two weeks with 50 µg of peptide in Freund's Incomplete Adjuvant [5].
- Hybridoma Development: Spleens from mice with the best immune response were harvested for polyethylene glycol (PEG)-assisted fusions with SP2/0 mouse myeloma cells at a 2:1 ratio [5].
- Screening Strategy: Hybridoma supernatants were screened by indirect ELISA on BSA-conjugated p-topoI peptide, with counter-screening on non-phosphorylated topoI peptide and irrelevant phosphopeptides to determine specificity [5].
- Clone Selection: The 357.3.1C1.H5.H7 clone (designated 1C1.H5.H7) was selected based on superior performance in both ELISA and IHC specificity tests, particularly its ability to differentially stain HCT15 cells (high topoI-pS10) versus Colo205 cells (low topoI-pS10) [5].
IHC Assay Development and Optimization
An indirect IHC assay was developed using the Intellipath auto-stainer (Biocare Medical) with the following optimized parameters [5]:
- Antigen Retrieval: Performed at 85°C for 30 minutes followed by 75°C for 10 minutes in acidic pH citrate buffer (pH 6.0) [5].
- Blocking Steps: Sequential peroxidase blocking for 10 minutes followed by universal blocking (Biocare Medical sniper block reagent) for 30 minutes [5].
- Antibody Incubation: Anti-topoI-pS10 primary antibody incubation for 2 hours at room temperature [5].
- Detection System: Mouse secondary antibody for 15 minutes at room temperature followed by universal horseradish peroxidase (HRP) reagent and diaminobenzidine tetrahydrochloride (DAB) chromagen incubation for 5 minutes [5].
- Counterstaining and Mounting: Hematoxylin counterstaining followed by dehydration and mounting with permanent mounting media [5].
Diagram 1: Molecular mechanism of CPT resistance.
Assay Validation Framework
Comprehensive validation followed established best practices for phospho-specific antibody validation [46] [47]:
- Specificity Verification: Western blot analysis demonstrated specific bands at appropriate molecular weights with minimal cross-reactivity [46].
- Phospho-Specificity Confirmation: Tissue sections and cell pellets were subjected to phosphatase treatment to verify phospho-specificity [46].
- Peptide Blocking: Use of blocking peptides verified specificity and ruled out Fc-mediated binding and other non-specific staining [46].
- Cell Line Models: Paraffin-embedded cell pellets of known target expression levels verified target specificity [46].
- Tissue Cross-Reactivity: Human cancer tissue arrays demonstrated antibody performance across multiple tissue types [46].
- Lot Consistency: Thorough lot testing ensured reproducibility necessary for accurate IHC results [46].
Comparative Performance Analysis
Phospho-Specific IHC Assay Comparison
The development of phospho-specific IHC assays extends beyond topoI-pS10 to other biologically relevant targets, each with unique technical considerations and applications.
Table 2: Comparison of Phospho-Specific IHC Assay Applications
| Assay Target | Biological Context | Technical Challenges | Clinical/Research Utility |
|---|---|---|---|
| topoI-pS10 [5] | DNA damage response to topoisomerase I inhibitors | Preservation of phospho-epitopes during FFPE processing | Predictive biomarker for camptothecin analogue response |
| Phospho-ERα isoforms [4] | Estrogen receptor signaling in breast cancer | Multiple phosphorylation sites requiring individual validation | Profiling for endocrine therapy selection; correlation with total ERα expression |
| GPCR phospho-sites [6] | G protein-coupled receptor activation states | Extreme instability of phosphorylation during routine IHC | Visualization of receptor activation in response to physiological/pharmacological stimulation |
| Plasma p-tau variants [48] | Alzheimer's disease neurodegeneration | Differential performance across assay platforms | Detection of abnormal amyloid-β status and prediction of dementia progression |
Quantitative Performance Metrics
The P-topoIDx assay demonstrated significant differential staining capabilities that correlated with drug response phenotypes. In validation studies, HCT15 cells (known to degrade topoI rapidly and exhibit camptothecin resistance) showed significantly higher basal topoI-pS10 levels compared to Colo205 cells (which show minimal topoI degradation and maintain drug sensitivity) [5]. This differential immunostaining formed the basis for patient stratification.
For other phospho-biomarker applications, performance varies significantly by target and detection method:
- In Alzheimer's biomarker development, mass spectrometry-based p-tau217 demonstrated Area Under Curve (AUC) = 0.947 for detecting abnormal amyloid-β status, significantly outperforming several immunoassay-based p-tau181 formats (AUC range 0.642–0.813) [48].
- The Quanterix Simoa ALZpath p-tau217 assay achieved ROC-AUC of 82.82% for distinguishing Alzheimer's disease from healthy controls in a Peruvian cohort, demonstrating consistent performance across ethnic populations [49].
- Phospho-ERα detection in breast cancer showed varying prevalence across phosphorylation sites, with P-S118-ERα detected in 48% of breast tumors (177/370 cases) and positively correlating with total ERα expression (r = 0.352, P < 0.0001) [4].
Technical Comparison of Detection Methodologies
Different detection platforms offer distinct advantages for phospho-specific assay development:
Diagram 2: IHC assay workflow for phospho-biomarker detection.
Research Reagent Solutions
Successful development of phospho-specific IHC assays requires carefully selected reagents and methodologies to address the unique challenges of phospho-epitope preservation and detection.
Table 3: Essential Research Reagents for Phospho-Specific IHC
| Reagent Category | Specific Examples | Function in Assay Development |
|---|---|---|
| Phospho-Specific Antibodies | topoI-pS10 mouse monoclonal; Phospho-ERα rabbit polyclonals; GPCR phospho-antibodies [5] [4] [6] | Target detection with phosphorylation state specificity |
| Antigen Retrieval Solutions | Citrate buffer (pH 6.0); CC1 buffer (Ventana) [5] [4] | Exposure of masked phospho-epitopes in FFPE tissues |
| Detection Systems | MACH 4 Universal HRP-Polymer; Avidin-biotin-peroxidase complex (ABC); Labeled streptavidin-biotin (LSAB) [5] [50] | Signal amplification with minimal background |
| Specificity Controls | Phosphopeptide blocks; Phosphatase-treated tissues; Isotype controls [46] | Verification of antibody specificity and staining relevance |
| Validation Tools | Transfected cell pellets; Xenograft models; Tissue microarrays [46] | Assessment of antibody performance across biological contexts |
Discussion: Implementation Challenges and Technical Considerations
The implementation of phospho-specific IHC assays in both research and potential clinical settings presents several critical considerations that impact assay performance and interpretation.
Pre-Analytical Variables
Pre-analytical factors significantly influence phospho-epitope detection [4] [50]:
- Tissue Collection Time: Studies of phospho-ERα epitopes investigated whether detection varied with biospecimen collection times (time from surgical excision to processing), recognizing that phosphorylation states can be transient [4].
- Fixation Protocols: Prolonged formaldehyde fixation can result in variably reversible loss of immunoreactivity by masking antibody binding sites, while delays in fixation may cause loss of immunoreactivity for some phospho-epitopes [50].
- Phosphatase Activity: Endogenous phosphatase activity remains a significant challenge, with specialized protocols incorporating phosphatase inhibitors throughout fixation and staining procedures required for optimal detection of unstable phosphorylation events, particularly for GPCRs [6].
Validation Requirements
Comprehensive validation of phospho-specific antibodies follows tiered evidence-based approaches [47]. Level 1 validation requires evidence of usage in IHC applications, while Levels 2-3 require increasingly rigorous specificity testing. Key validation steps include [46]:
- Demonstration of appropriate bands on Western blot with minimal cross-reactivity
- Verification using paraffin-embedded cell pellets with known target expression
- Assessment in relevant disease models (xenografts, genetically engineered models)
- Use of peptide blocking to confirm specificity
- Consistent performance across production lots
Comparison to Alternative Methodologies
While IHC provides valuable spatial information in tissue context, other phospho-biomarker detection platforms offer complementary advantages:
- Immunoassays: Platforms like Simoa and Lumipulse provide quantitative results from liquid samples but lose spatial context [48].
- Mass Spectrometry: Considered the "gold standard" for protein identification, with p-tau217 measures demonstrating superior performance (AUC = 0.947) but requiring specialized instrumentation and expertise [48].
- Digital Pathology: Quantitative analysis of IHC staining patterns enables objective assessment of heterogeneous phosphorylation in tissue samples [5].
The systematic development of the P-topoIDx assay for topoI-pS10 detection demonstrates a validated framework for creating predictive phospho-biomarker tests. This case study highlights critical success factors: rigorous antibody validation, optimization of pre-analytical conditions, implementation of appropriate controls, and comprehensive performance assessment. The comparison of reagent solutions and methodologies provides researchers with practical guidance for developing robust phospho-specific IHC assays. As personalized medicine advances, such carefully validated phospho-biomarker assays will play increasingly important roles in stratifying patient populations for targeted therapies, ultimately improving treatment outcomes through precise targeting of dysregulated kinase pathways. Future developments should focus on standardizing protocols across laboratories, improving phospho-epitope preservation methods, and expanding quantitative digital pathology applications to enhance reproducibility and accuracy in phospho-biomarker detection.
Solving Common Problems in Phospho-Specific IHC: Weak Staining, High Background, and Specificity Issues
In the study of cellular signaling pathways, phospho-specific antibodies provide invaluable insight by detecting post-translational modifications that indicate protein activation status. However, their application in immunohistochemistry (IHC) presents unique challenges, with no or weak staining being a frequent obstacle that compromises data integrity. For researchers and drug development professionals validating these reagents, addressing poor staining is not merely technical troubleshooting but a fundamental requirement for generating biologically relevant data. The validation of phospho-specific antibodies for IHC demands rigorous optimization of two interdependent parameters: antibody titration, which determines reagent specificity and sensitivity, and antigen retrieval, which reverses formaldehyde-induced epitope masking and is especially critical for revealing labile phosphorylation sites [4] [51] [52]. This guide systematically compares optimization approaches, providing experimental data and protocols to ensure reliable detection of phosphorylated epitopes in formalin-fixed paraffin-embedded (FFPE) tissues.
Antibody Titration: Establishing Specificity and Sensitivity
Antibody titration determines the optimal concentration that maximizes specific signal while minimizing background. For phospho-specific antibodies, this process requires additional controls to verify phosphorylation-dependent recognition.
Experimental Data and Comparative Performance
In a comprehensive validation study of phospho-specific estrogen receptor α (ERα) antibodies, researchers established specific working concentrations for multiple phosphorylation sites (Table 1) [4]. This systematic approach demonstrates that different phospho-epitopes require individualized optimization even within the same target protein.
Table 1: Optimized Working Conditions for Phospho-Specific ERα Antibodies
| Phospho-Epitope | Antibody Supplier | Optimal Dilution | Incubation Conditions | Antigen Retrieval Method |
|---|---|---|---|---|
| P-S104/106-ERα | Bethyl Laboratories | 1:200 | 1 hour at 42°C | CC1 (Citrate Buffer) |
| P-S118-ERα | Cell Signaling | 1:600 | 1 hour at 42°C | CC1 (Citrate Buffer) |
| P-S167-ERα | Abcam | 1:700 | 1 hour at 42°C | CC1 (Citrate Buffer) |
| P-S282-ERα | Bethyl Laboratories | 1:700 | 1 hour at 42°C | CC1 (Citrate Buffer) |
| P-S294-ERα | Bethyl Laboratories | 1:800 | 1 hour at 42°C | CC1 (Citrate Buffer) |
| P-S559-ERα | Bethyl Laboratories | 1:150 | 1 hour at 42°C | CC1 (Citrate Buffer) |
| P-T311-ERα | Bethyl Laboratories | 1:100 | 1 hour at 42°C | CC1 (Citrate Buffer) |
Detailed Titration Protocol
Initial Dilution Series: Prepare a range of antibody concentrations flanking the manufacturer's recommendation (e.g., 1:50, 1:100, 1:200, 1:400, 1:800) using an appropriate antibody diluent [53] [54].
Control Tissues: Include both positive and negative control tissues in the experiment. Positive controls should express the target phospho-epitope, while negative controls may utilize:
Specificity Verification: Perform peptide blocking experiments where the antibody is pre-incubated with the phospho-specific peptide used for immunization. Compare this to pre-incubation with non-phosphorylated peptide [54] [51]. Only the phospho-peptide should abolish staining.
Assessment and Selection: Evaluate staining intensity and specificity. The optimal dilution provides strong specific nuclear staining with minimal background when compared to negative controls [4].
The following workflow illustrates the systematic approach to antibody titration and validation:
Antigen Retrieval Re-optimization: Recovering Masked Epitopes
Antigen retrieval is particularly crucial for phospho-specific antibodies because formalin fixation creates methylene bridges that can mask the very epitopes these antibodies recognize [52]. Without proper retrieval, even perfectly titrated antibodies may fail to bind their targets.
Comparison of Antigen Retrieval Methods
Table 2: Performance Comparison of Antigen Retrieval Methods for IHC
| Method | Mechanism | Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| Heat-Induced Epitope Retrieval (HIER) | High-temperature breakdown of formalin cross-links [36] [52] | - Broad effectiveness- Good tissue morphology preservation- Wide pH buffer options | - Potential tissue damage- Equipment-dependent variability | Most phospho-specific antibodies; general IHC work [4] [52] |
| Proteolytic-Induced Epitope Retrieval (PIER) | Enzymatic cleavage of protein cross-links [52] | - Effective for some epitopes resistant to HIER- Lower temperature (37°C) | - Risk of tissue morphology damage- Potential epitope destruction- Narrow optimal concentration window | Epitopes resistant to heat retrieval; specific targets requiring enzymatic unmasking [52] |
| Combination Approaches | Sequential or simultaneous application of heat and enzymes | - Potentially superior for difficult epitopes- Can rescue otherwise undetectable targets | - Complex optimization- Increased risk of artifacts | Stubborn epitopes; phospho-sites particularly vulnerable to masking |
Buffer Selection and Experimental Optimization
The choice of retrieval buffer significantly impacts staining success. Research indicates that different phospho-epitopes may respond differently to buffer pH and composition:
- Low-pH Buffers (e.g., Sodium citrate, pH 6.0): Effective for many nuclear antigens and phospho-epitopes [4] [36]
- High-pH Buffers (e.g., Tris-EDTA, pH 8.0-9.0): Often superior for membrane proteins and some phosphorylated targets [36] [52]
The phospho-ERα study utilized citrate buffer (pH 6.0) for all epitopes, demonstrating that a single retrieval condition can work for multiple phosphorylation sites within the same protein [4]. However, initial optimization should test multiple buffers.
Detailed HIER Protocol Using a Pressure Cooker
Deparaffinization and Rehydration:
Retrieval Solution Preparation:
- Prepare 1-3 L of appropriate buffer (e.g., 10 mM sodium citrate, pH 6.0, or Tris-EDTA, pH 9.0)
- Add to pressure cooker and begin heating [36]
Heat-Induced Retrieval:
- When buffer is boiling, transfer slides to pressure cooker
- Secure lid and bring to full pressure
- Maintain at full pressure for 3-20 minutes (optimization required) [36]
Cooling and Washing:
- Depressurize cooker and run cold water over it for 10 minutes
- Cool slides in buffer for 20 additional minutes
- Transfer to wash buffer [36]
The relationship between antigen retrieval methods and their applications can be visualized as follows:
Integrated Troubleshooting Approach
When facing no or weak staining with phospho-specific antibodies, a systematic integrated approach is essential:
Sequential Optimization Strategy
Begin with Antigen Retrieval: Test both low-pH and high-pH buffers using a standard HIER protocol [52]. Include both positive and negative control tissues.
Proceed to Antibody Titration: Once optimal retrieval is established, titrate the antibody using the retrieval conditions identified in step 1.
Validate Specificity: Confirm phosphorylation-dependent staining through:
Assess Tissue Quality: For phospho-epitopes, consider tissue collection time and ischemia effects, as phosphorylation states can change rapidly post-excision [4] [55].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Phospho-Specific IHC Validation
| Reagent Category | Specific Examples | Function in Validation | Considerations |
|---|---|---|---|
| Validation Controls | Phospho-specific blocking peptides [54] [51] | Verify antibody specificity through competition | Should abolish staining while non-phospho peptide should not |
| Cell pellets with known expression [54] | Provide consistent positive and negative controls | Can be transfected to express target phospho-protein | |
| Phosphatase enzymes [54] | Generate negative controls by dephosphorylation | Must be validated for activity on FFPE tissues | |
| Retrieval Buffers | Sodium citrate buffer (pH 6.0) [4] [36] | Low-pH retrieval for many nuclear phospho-epitopes | Effective for many phosphorylation sites |
| Tris-EDTA buffer (pH 8.0-9.0) [36] [52] | High-pH retrieval for challenging epitopes | May reveal epitopes resistant to low-pH retrieval | |
| Detection Systems | Polymer-based detection [53] | Enhanced sensitivity for low-abundance targets | Reduced background compared to avidin-biotin systems |
| Tyramine amplification [55] | Signal amplification for very weak signals | Requires careful optimization to prevent background |
Addressing no or weak staining in phospho-specific IHC requires methodical optimization of both antibody concentration and antigen retrieval conditions. The experimental data presented demonstrates that different phospho-epitopes require individualized validation, with optimal results achieved through systematic testing of retrieval buffers and antibody dilutions. By implementing these protocols and utilizing appropriate controls, researchers can overcome the technical challenges associated with phospho-specific antibody validation, ensuring reliable detection of phosphorylation events critical for understanding cellular signaling pathways in both research and drug development contexts.
In phospho-specific immunohistochemistry (IHC), achieving high signal-to-noise ratio is paramount for accurate data interpretation. The detection of phosphorylated epitopes presents unique challenges, as these transient post-translational modifications often exist at low stoichiometry amidst a background of abundant non-phosphorylated proteins. Inadequate blocking and suboptimal washing represent two primary sources of high background staining that can compromise data quality and lead to false-positive interpretations in research and drug development contexts [56] [57]. The validation of phospho-specific antibodies for IHC research demands rigorous optimization of these fundamental steps to ensure that observed signals genuinely reflect the phosphorylation status of the target protein rather than technical artifacts.
The broader thesis of phospho-specific antibody validation acknowledges that these reagents are exceptionally prone to non-specific binding due to the charged nature of phosphate groups and the often-similar chemical properties of related epitopes. For instance, during the development of a predictive IHC test for topoisomerase I phosphorylation (topoI-pS10), researchers implemented a comprehensive blocking protocol using a commercial blocking reagent followed by careful wash optimization to distinguish between camptothecin-responsive and non-responsive patient populations [5]. This highlights how methodological precision in blocking and washing directly translates to clinically relevant assay performance.
Systematic Blocking Strategies for Background Reduction
Mechanism and Selection of Blocking Agents
Blocking functions by occupying non-specific binding sites within tissue sections before antibody incubation, thereby preventing subsequent non-specific interactions between detection reagents and tissue components. Effective blocking agents compete with antibodies for charge-based, hydrophobic, and other non-specific interactions that would otherwise contribute to background staining [58]. The selection of appropriate blocking agents should be guided by the specific experimental context, including the tissue type, primary antibody host species, and detection system.
The table below summarizes the primary categories of blocking agents and their optimal use cases:
Table 1: Comparison of Blocking Agent Categories and Applications
| Blocking Agent Category | Specific Examples | Mechanism of Action | Optimal Use Cases | Key Limitations |
|---|---|---|---|---|
| Normal Serum | Serum from secondary antibody host species (e.g., goat serum for anti-goat secondary) | Antibodies in serum bind non-specific epitopes; other serum proteins block protein-binding sites | Ideal for polyclonal primary antibodies; reduces Fc receptor binding [59] [60] | Must match secondary antibody species, not primary antibody species [59] |
| Protein Solutions | 1-5% BSA, gelatin, or non-fat dry milk | Proteins compete with antibodies for non-specific binding sites | Cost-effective for monoclonal antibodies; compatible with various detection systems [58] | Non-fat dry milk contains biotin and interferes with avidin-biotin detection systems [58] |
| Commercial Blocking Buffers | Proprietary protein-based or protein-free formulations | Optimized proprietary mixtures designed for maximal non-specific site coverage | When traditional methods yield high background; standardized formulations [58] [59] | Higher cost; variable performance across different tissue types |
Specialized Blocking Considerations for Phospho-Specific Detection
Phospho-specific IHC introduces additional complexities that demand specialized blocking approaches. The charged nature of phosphate groups increases the potential for non-specific ionic interactions, necessitating more stringent blocking conditions. Furthermore, the often low abundance of phosphorylated epitopes relative to their non-phosphorylated counterparts means that even minimal non-specific binding can generate significant background relative to the specific signal.
For phospho-specific antibodies, incorporating phosphatase inhibitors throughout tissue processing is critical to preserve the phosphorylation epitope. As noted in IHC troubleshooting guides, "the primary antibody is specific to a phosphorylated target, which has been dephosphorylated," recommending to "include protein phosphatase inhibitors (PPIs) in fixative, wash buffers and staining buffers to prevent dephosphorylation" [56]. This epitope preservation represents a unique prerequisite for successful phospho-specific IHC that precedes conventional blocking methods.
When working with mouse monoclonal antibodies on mouse tissues (a common scenario for transgenic models), additional blocking strategies are required to prevent the secondary antibody from binding to endogenous immunoglobulins. Using F(ab) fragment secondary antibodies and specialized mouse-on-mouse blocking protocols can significantly reduce this specific source of background [60].
Wash Optimization Parameters and Methodologies
Composition, Timing, and Volume Considerations
While often overlooked in protocol development, washing steps are equally critical as blocking for background reduction. Inadequate washing fails to remove unbound antibodies and detection reagents, allowing them to deposit non-specifically throughout the tissue section. Optimization requires careful attention to buffer composition, pH, ionic strength, detergent content, volume, duration, and frequency [56] [57].
The buffer composition significantly influences washing efficiency. Phosphate-buffered saline (PBS) and Tris-buffered saline (TBS) are the most common bases for wash buffers, with TBS generally providing better performance for phospho-epitopes due to its enhanced capacity to maintain stable pH. The addition of detergents such as Tween-20 (typically at 0.05-0.1%) significantly improves removal of unbound antibodies by reducing surface tension and disrupting hydrophobic interactions. However, detergent concentration requires optimization, as excessively high concentrations may potentially elute specifically bound antibodies.
Table 2: Wash Optimization Parameters and Their Effects on Background Reduction
| Parameter | Optimal Range | Effect on Background | Experimental Considerations |
|---|---|---|---|
| Buffer pH | 7.2-7.6 (physiological) | Prevents charge-based non-specific interactions | Phospho-epitopes may require specific pH for stability |
| Ionic Strength | 150-200 mM NaCl | Reduces ionic interactions without disrupting specific binding | High salt can elute low-affinity antibodies |
| Detergent Concentration | 0.05-0.1% Tween-20 | Disrupts hydrophobic interactions | Excessive detergent may decrease specific signal |
| Wash Volume | 50-100x slide volume | Ensures complete exchange of reagents | Larger volumes improve efficiency but increase reagent use |
| Wash Duration | 5-10 minutes per wash | Allows diffusion of unbound reagents from tissue | Longer washes may be needed for thick sections |
| Wash Frequency | 3-5 washes after each incubation step | Cumulative effect removes progressively bound reagents | Critical after secondary antibody and detection steps |
Technical Execution of Washes
The mechanical aspects of washing significantly impact effectiveness. Simple immersion of slides may not sufficiently displace reagents from the tissue section. Agitated washing using orbital shakers at low to moderate speeds improves reagent exchange throughout the tissue. For high-throughput applications, automated stainers provide highly consistent washing through precisely controlled buffer exchange, contributing to improved reproducibility [5].
The implementation of cascading washes (sequential transfers through fresh buffer baths) can enhance removal of unbound reagents compared to single-bath immersion. Additionally, incorporating a final rinse in detergent-free buffer immediately before developing can prevent detergent interference with certain detection chemistries.
Integrated Workflow: Combining Blocking and Wash Strategies
The diagram below illustrates the strategic position of blocking and optimized washing within the comprehensive IHC workflow for phospho-specific detection:
Figure 1. Comprehensive IHC Workflow with Integrated Blocking and Wash Steps. This workflow highlights the sequential application of different blocking strategies (yellow) and optimized washing steps (green) within the complete IHC procedure. Note that multiple washing steps are strategically positioned after each critical incubation to systematically reduce background.
Experimental Validation and Controls for Background Assessment
Essential Control Experiments
Rigorous validation of blocking and washing efficacy requires implementation of appropriate controls that can distinguish specific signal from background staining. The table below outlines critical controls for assessing background in phospho-specific IHC:
Table 3: Essential Controls for Assessing Background in Phospho-Specific IHC
| Control Type | Implementation | Interpretation of Results | Utility for Background Assessment |
|---|---|---|---|
| No Primary Antibody Control | Omit primary antibody; incubate with antibody diluent only | Any staining indicates secondary antibody non-specific binding | Directly assesses secondary antibody-related background [61] |
| Isotype Control | Replace primary antibody with same concentration of non-specific immunoglobulin from same species | Staining indicates non-specific Fc-mediated binding | Identifies background from antibody-protein interactions [61] |
| Phosphatase-Treated Control | Treat tissue sections with alkaline phosphatase prior to immunostaining | Reduced or eliminated staining confirms phospho-specificity | Validates that detection depends on phosphorylation status [16] |
| Absorption Control | Pre-absorb primary antibody with immunizing phospho-peptide | Specific staining should be abolished | Confirms antibody specificity to target phospho-epitope [61] |
| Tissue Negative Control | Use tissue known to lack target phospho-epitope | Staining indicates non-specific binding to tissue components | Assesses tissue-specific background issues [61] |
Quantitative Assessment of Background Reduction
The development of the P-topoIDx assay exemplifies how systematic optimization of blocking and washing enables the creation of clinically applicable phospho-specific IHC tests. Researchers employed a semi-automated IHC platform with standardized blocking using a commercial "background sniper" reagent and carefully timed washes after each incubation step [5]. This methodological rigor allowed for precise quantification of topoI-pS10 levels that could stratify patient responders from non-responders to camptothecin analogues.
In a reverse-phase protein array study investigating phospho-antibody performance, researchers established quantitative metrics for antibody validation, including signal-to-noise ratio and dilution linearity score, which directly reflect the effectiveness of background reduction strategies [16]. Implementing similar quantitative assessments in IHC, through image analysis software that measures signal intensity in specific cellular compartments relative to background in adjacent areas, provides objective evaluation of blocking and washing efficacy.
The Scientist's Toolkit: Essential Reagents for Background Reduction
Successful implementation of the strategies discussed requires access to specific high-quality reagents. The following table catalogues essential materials for optimizing blocking and washing in phospho-specific IHC:
Table 4: Essential Research Reagent Solutions for Background Reduction in Phospho-Specific IHC
| Reagent Category | Specific Examples | Function | Key Considerations |
|---|---|---|---|
| Protein Blocking Agents | Normal serum (species-matched to secondary), BSA (1-5%), casein-based blockers | Occupy non-specific protein-binding sites in tissue | Serum must be from secondary antibody species; BSA is versatile for most applications [58] [60] |
| Commercial Blocking Buffers | Biocare Medical "Background Sniper", Thermo Scientific Blocker BSA | Proprietary formulations for maximal background reduction | Particularly valuable for challenging antibodies or tissues with high endogenous background [5] [58] |
| Wash Buffer Components | PBS or TBS, Tween-20 detergent | Remove unbound antibodies while maintaining epitope integrity | Detergent concentration requires optimization (typically 0.05-0.1%) [56] [57] |
| Endogenous Enzyme Blockers | 0.3% hydrogen peroxide (peroxidase), levamisole (alkaline phosphatase) | Quench endogenous enzymatic activity that causes background | Essential for chromogenic detection; concentration and incubation time require optimization [60] |
| Phosphatase Inhibitors | Sodium fluoride, sodium orthovanadate, β-glycerophosphate | Preserve phosphorylation epitopes during processing | Must be included in fixatives and wash buffers for phospho-specific IHC [56] |
| Species-Specific Blockers | Mouse-on-Mouse blocking reagents, F(ab) fragment secondary antibodies | Reduce background when using mouse antibodies on mouse tissue | Critical for studies in genetically engineered mouse models [60] |
Effective elimination of high background in phospho-specific IHC requires a systematic, integrated approach combining strategic blocking with rigorous wash optimization. The fundamental principle involves both preemptively occupying non-specific binding sites through appropriate blocking agents and methodically removing unbound reagents through optimized washing protocols. For researchers validating phospho-specific antibodies, implementing the structured framework presented here—incorporating appropriate controls, quantitative assessment metrics, and specialized reagents—will significantly enhance assay specificity and reliability. The resulting improvement in signal-to-noise ratio directly translates to increased confidence in experimental results and more meaningful biological interpretations in both basic research and drug development contexts.
In immunohistochemistry (IHC) research, the accurate detection of protein phosphorylation states represents a formidable technical challenge. Phospho-epitopes are highly unstable modifications that can be rapidly erased by endogenous phosphatases released during tissue preparation and processing. For researchers validating phospho-specific antibodies, this instability poses a significant threat to experimental reliability and reproducibility. The essential defense against this threat lies in the strategic implementation of phosphatase inhibitors throughout the experimental workflow.
Cellular homeostasis maintains a precise balance between kinase and phosphatase activity. However, cell lysis during sample preparation disrupts this balance, releasing phosphatases that can swiftly remove phosphate groups from proteins, thereby obliterating the very signals researchers aim to detect [62] [63]. This degradation occurs rapidly and can lead to biologically meaningless representations of protein activation states, compromising data integrity and potentially leading to erroneous conclusions in both basic research and drug development [62]. This guide examines the essential role of phosphatase inhibitors in preventing phospho-epitope loss, providing a comparative analysis of inhibitor efficacy and detailed protocols for their application in phospho-specific IHC workflows.
The Science of Phospho-Epitope Instability
Understanding the Threat: Phosphatase Activity in Sample Preparation
In living cells, phosphatases are tightly regulated through compartmentalization and natural inhibitors to prevent indiscriminate damage to cellular proteins and maintain proper signaling pathway function [62] [63]. This careful regulation is catastrophically disrupted during cell lysis and tissue processing for IHC. The disruption of cellular architecture distorts the in vivo state by making all proteins potentially accessible for modification by endogenous phosphatases [62]. The consequence is rapid dephosphorylation of phospho-epitopes, which can occur within minutes of tissue collection [4].
The vulnerability of phospho-epitopes is particularly pronounced for G protein-coupled receptors (GPCRs), where phosphorylation is very unstable during routine immunohistochemical procedures [6]. This instability necessitates the presence of appropriate phosphatase inhibitors throughout both fixation and staining procedures to visualize receptor activation states accurately [6]. The challenge extends beyond GPCRs to critical signaling proteins including estrogen receptor α, retinoblastoma protein, topoisomerase I, and numerous kinases central to oncogenic pathways [4] [5] [64].
Comparative Analysis of Phosphatase Inhibitors
Inhibitor Specificity and Performance Data
Effective protection of phospho-epitopes requires a strategic approach to phosphatase inhibition based on the specific phosphatase classes present in samples. No single chemical is effective for all types of phosphatases; rather, a mixture or inhibitor cocktail of several different compounds is typically required to ensure comprehensive protection [62]. The table below summarizes the key characteristics and performance data for commonly used phosphatase inhibitors:
Table 1: Commonly Used Phosphatase Inhibitors and Their Applications
| Inhibitor | Target Class | Inhibition Type | Solubility | Typical Working Concentration | Mechanism of Action |
|---|---|---|---|---|---|
| Sodium Fluoride | Ser/Thr and acidic phosphatases | Irreversible | Water (40 mg/mL) | 1-20 mM | Inhibits enzymatic activity through irreversible binding |
| Sodium Orthovanadate | Tyr and alkaline phosphatases | Irreversible | Water (20 mg/mL) | 1-100 mM | Competitive inhibition at enzyme active site |
| β-Glycerophosphate | Ser/Thr phosphatases | Reversible | Water (10 mg/mL) | 1-100 mM | Reversible binding to enzyme active site |
| Sodium Pyrophosphate | Ser/Thr phosphatases | Irreversible | Water (65 mg/mL) | 1-100 mM | Irreversible enzyme inactivation |
Experimental Evidence of Inhibitor Efficacy
The critical importance of phosphatase inhibition is demonstrated in studies validating phospho-specific antibodies for IHC. Research on estrogen receptor α (ERα) phosphorylation in breast cancer specimens revealed that the detection of multiple phosphorylated ERα forms (including P-S118-ERα and P-S167-ERα) was highly dependent on proper tissue collection and processing methods that incorporated phosphatase inhibitors [4]. Similarly, in developing an IHC-based test for topoisomerase I phosphorylation (topoI-pS10), researchers maintained phosphatase inhibitors throughout sample processing to preserve the phosphorylation signal that serves as a predictive biomarker for camptothecin-based therapy response [5].
The consequence of inadequate phosphatase inhibition is clearly demonstrated in validation protocols for phospho-specific antibodies. In one such protocol for validating a phospho-specific antibody against retinoblastoma (Rb) protein phosphorylated at Serine 249, researchers used bovine intestinal phosphatase treatment to confirm antibody specificity [64]. The successful de-phosphorylation resulted in either complete abrogation of immunoreactivity or an altered electrophoretic mobility of the protein of interest, highlighting how rapidly phosphatases can erase critical research signals [64].
Essential Methodologies for Phospho-Epitope Preservation
Integrated Workflow for Phospho-Specific IHC
Preserving phospho-epitopes requires an integrated approach that incorporates phosphatase inhibitors at multiple stages of sample processing. The following workflow visualization outlines the critical steps where phosphatase inhibition is essential:
Validation Protocol: Phosphatase Treatment for Antibody Specificity
A critical methodology in phospho-specific antibody validation involves using phosphatase treatment to confirm antibody specificity. This protocol, adapted from established validation procedures [64] [16], serves as both a validation method and a dramatic demonstration of what occurs when phospho-epitopes are lost due to inadequate phosphatase inhibition:
Table 2: Phosphatase Treatment Protocol for Antibody Validation
| Step | Reagents | Procedure | Purpose | Expected Outcome |
|---|---|---|---|---|
| 1. Sample Preparation | Cell lysates or tissue homogenates | Divide sample into two aliquots | Create paired samples for comparison | Identical starting material |
| 2. Phosphatase Treatment | Bovine intestinal phosphatase (BIP), Dephosphorylation buffer | Treat one aliquot with BIP (100 units) for 30-60 minutes at 37°C | Remove phosphate groups from proteins | Experimental group: dephosphorylated |
| 3. Control Treatment | BIP inhibitor cocktail (NaF, Na3VO4, NaPP) | Treat second aliquot with BIP + inhibitors under same conditions | Prevent dephosphorylation | Control group: phosphorylation intact |
| 4. Analysis | Phospho-specific antibody, Detection system | Process both samples in parallel using IHC or immunoblotting | Compare signal intensity | >70% signal reduction in experimental group confirms antibody specificity |
This protocol demonstrates that without proper phosphatase inhibition, the critical phospho-epitopes detected by phospho-specific antibodies would be lost, leading to false-negative results and potentially invalid conclusions.
The Researcher's Toolkit: Essential Reagents for Phospho-Epitope Preservation
Successful preservation of phospho-epitopes requires strategic implementation of specific reagents throughout the IHC workflow. The following table details essential solutions and their applications:
Table 3: Research Reagent Solutions for Phospho-Epitope Preservation
| Reagent Solution | Composition | Function | Application Point |
|---|---|---|---|
| Complete Phosphatase Inhibitor Cocktail | Sodium fluoride (10-20 mM), Sodium orthovanadate (1-10 mM), β-Glycerophosphate (10-50 mM) | Broad-spectrum inhibition of Ser/Thr and Tyr phosphatases | Lysis buffers, tissue homogenization |
| Acidic Phosphatase Inhibitor Solution | Sodium fluoride (10-20 mM), Tartrate (1-5 mM) | Specifically targets acid phosphatases released from lysosomes | Fixation solutions, processing buffers |
| Alkaline Phosphatase Blocking Solution | Levamisole (1-5 mM) or specific anti-alkaline phosphatase inhibitors | Inhibits endogenous alkaline phosphatase activity | Pre-incubation steps before detection |
| Stabilized Lysis Buffer with Inhibitors | RIPA or similar buffer with fresh phosphatase inhibitors added immediately before use | Immediate inhibition upon cell disruption while maintaining protein integrity | Initial tissue/cell lysis |
| Phosphatase-Free Validated Antibody Diluent | PBS or TBS with carrier protein and phosphatase inhibitors | Maintains phosphorylation state during antibody incubation steps | Antibody dilution and incubation |
Advanced Applications: Phospho-Specific IHC in Drug Development
The strategic implementation of phosphatase inhibitors enables critical applications in drug development and precision oncology. For instance, the development of P-topoIDx, an IHC-based test that stratifies responder and non-responder patient populations to topoisomerase I inhibitors, depended entirely on maintaining the topoI-pS10 phosphorylation state during tissue processing [5]. Similarly, profiling multiple phosphorylated ERα forms in breast cancer tissues has revealed potential for selecting subgroups of patients who would benefit from endocrine therapy [4].
These advanced applications share a common requirement: the preservation of inherently unstable phosphorylation states throughout complex tissue processing workflows. The essential strategy in each case involves comprehensive phosphatase inhibition from the moment of tissue collection through final detection. As one study emphasized, "GPCR phosphorylation is very unstable during routine immunohistochemical procedures, necessitating the presence of appropriate phosphatase inhibitors throughout both fixation and staining procedures" [6]. This principle extends beyond GPCRs to virtually all phospho-specific detection systems.
The validation of phospho-specific antibodies for IHC research depends fundamentally on preventing phospho-epitope loss through strategic phosphatase inhibition. The experimental data and methodologies presented demonstrate that without proper inhibitor cocktails targeting all relevant phosphatase classes, research outcomes may reflect artifact rather than biological reality. As phosphatase research advances and new inhibitors with improved specificity and bioavailability emerge, the precision of phospho-specific detection will continue to improve. For researchers, drug developers, and clinical scientists, maintaining rigorous standards for phosphatase inhibition represents not merely a technical consideration, but an essential prerequisite for generating meaningful, reproducible data on protein phosphorylation states in health and disease.
In the field of immunohistochemistry (IHC) research, particularly in the development and application of phosphospecific antibodies, the use of appropriate controls is not merely a recommendation—it is an absolute necessity for generating valid, interpretable, and reproducible data. Phosphorylation-state-specific antibodies (PSSAs) are invaluable tools for investigating cell signaling pathways in situ, offering potential for predictive biomarkers in oncology [5]. However, the unique challenges associated with validating IHC assays for these antibodies, including the lability of phosphorylation epitopes and potential for cross-reactivity, make robust experimental design paramount [5]. Without proper controls, investigators risk erroneous scientific conclusions and clinical misdiagnoses, contributing to irreproducible findings in the literature [65]. This guide outlines the essential controls required for validating phosphospecific IHC assays, providing a framework that researchers can apply to their own experimental designs to ensure data integrity.
The Non-Negotiable Minimum: Essential Controls for IHC Experiments
Positive Controls
A positive control is a specimen known to express the target protein or phospho-epitope of interest [66]. Its purpose is to verify that the entire IHC procedure is working and optimized. When a positive control yields the expected staining pattern, it confirms that any negative results in test samples are truly due to the absence of the target and not technical failure [65]. The most rigorous positive control is the positive anatomical control—an internal or external specimen where the presence and location of the antigen is established a priori through other validated methods [65].
For phosphospecific antibodies, this might involve using cell lines with known phosphorylation status or tissue sections with documented expression of the phospho-epitope. For instance, in developing a topoI-pS10 phosphospecific immunohistochemical assay, researchers utilized HCT15 cells known to have higher basal topoI-pS10 levels compared to Colo205 cells as a positive control during hybridoma screening [5].
Negative Controls
Negative controls are equally critical and come in several forms, each serving a distinct purpose:
- Tissue Negative Control: A specimen known not to express the target antigen, used to check for non-specific signals and false-positive results [66].
- No Primary Antibody Control: This involves incubating the sample with antibody diluent alone, followed by the detection system. It confirms that observed staining is not produced by the detection system or non-specific binding of secondary antibodies [66].
- Isotype Control: When working with monoclonal antibodies, the tissue is incubated with a non-immune antibody of the same isotype and concentration as the primary antibody. This controls for non-specific interactions between the antibody and tissue components [66].
Absorption Control
An absorption control demonstrates that the antibody binds specifically to the antigen of interest. The primary antibody is pre-incubated with a large molar excess (e.g., 10-fold) of the immunizing peptide before application to the tissue [66]. A significant reduction or elimination of staining suggests specificity. This control is particularly reliable when using peptide immunogens, as protein immunogen mixtures may themselves cause high background [66]. For phosphospecific antibodies, this should be performed using both the phosphorylated and non-phosphorylated forms of the peptide to confirm phosphorylation-dependent recognition [4].
Experimental Protocols: Implementing Controls in Phosphospecific IHC Validation
The following workflow diagram outlines a comprehensive experimental approach for validating phosphospecific antibodies using appropriate controls:
Detailed Methodology for Control Implementation
Based on published protocols for phospho-specific IHC assay development [4] [5], the following steps are critical:
1. Antibody Specificity Validation Before IHC optimization, confirm antibody specificity using Western blot analysis with proteins from the same tissue or cells used for IHC [65]. For phosphospecific antibodies, test against both phosphorylated and non-phosphorylated forms of the target protein. Additionally, using cell lines with genetically confirmed expression or knockout of the target provides strong evidence of specificity [65].
2. Tissue Microarray (TMA) Construction and Processing As demonstrated in the validation of multiple phospho-ERα antibodies [4], TMAs containing both known positive and negative tissues are invaluable for standardized testing. Key steps include:
- Selection of cases with previously characterized status (e.g., by ligand binding assay or mass spectrometry)
- Re-review of hematoxylin and eosin (H&E) sections by a pathologist
- Standardized formalin-fixed paraffin-embedded (FFPE) processing
- Use of automated stainers with consistent antigen retrieval conditions [4]
3. Controlled Staining Protocol The IHC protocol should be carefully optimized and consistently applied:
- Antigen retrieval using standardized buffers (e.g., citrate buffer pH 6.0)
- Controlled incubation times and temperatures for primary antibody
- Consistent detection system (e.g., HRP-polymer with DAB chromogen)
- Hematoxylin counterstaining [4] [5]
4. Specificity Assessment for Phosphoepitopes For phosphospecific antibodies, additional validation steps are crucial:
- Parallel staining with antibodies immunoabsorbed with phosphorylated vs. non-phosphorylated peptides [4]
- Treatment of tissues with phosphatases to abolish staining
- Correlation with other markers in signaling pathway when possible
Quantitative Data Analysis: Comparing Control Performance
The table below summarizes quantitative data from phospho-ERα antibody validation, demonstrating how proper controls enable reliable assessment of antibody performance [4]:
Table 1: Performance Characteristics of Validated Phospho-ERα Antibodies in Breast Cancer TMAs
| Phospho-ERα Epitope | Positive Cases/Total | Percentage Positive | Correlation with Total ERα (r-value) | Correlation with PgR Status (r-value) |
|---|---|---|---|---|
| P-S104/106-ERα | Data not reported | Data not reported | Data not reported | Data not reported |
| P-S118-ERα | 177/370 | 48% | 0.352 | 0.163 |
| P-S167-ERα | Data not reported | Data not reported | Data not reported | Data not reported |
| P-S282-ERα | Data not reported | Data not reported | Data not reported | Data not reported |
| P-S294-ERα | Data not reported | Data not reported | Data not reported | Data not reported |
| P-T311-ERα | Data not reported | Data not reported | Data not reported | Data not reported |
| P-S559-ERα | Data not reported | Data not reported | Data not reported | Data not reported |
The validation approach for these antibodies included running positive and negative controls in parallel, with specificity confirmed by peptide absorption. The significant correlation between P-S118-ERα and total ERα (r=0.352, P<0.0001) provides evidence of specificity, while the imperfect correlation highlights that phosphorylation represents a distinct regulatory mechanism [4].
For the topoI-pS10 IHC assay development, researchers used a different quantitative approach, comparing two colon cancer cell lines with known differential topoI-pS10 levels (HCT15 vs. Colo205) to screen hybridoma clones for IHC specificity [5]. This controlled comparison enabled selection of a clone (1C1.H5.H7) that differentially stained the two cell lines, confirming its utility as a predictive biomarker.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Essential Reagents for Controlled Phosphospecific IHC Experiments
| Reagent Category | Specific Examples | Function in Experimental Controls |
|---|---|---|
| Phosphospecific Antibodies | P-S118-ERα [4], TopoI-pS10 [5] | Primary detection reagents targeting specific phospho-epitopes; require validation with controls. |
| Positive Control Tissues/Cells | Cell lines with known phosphorylation status (HCT15 for topoI-pS10) [5], Tissue Microarrays with characterized cases [4] | Verify assay performance; essential for interpreting test results. |
| Negative Control Tissues/Cells | Cell lines lacking target phosphorylation (Colo205 for topoI-pS10) [5], Knockout tissues [65] | Establish staining specificity; identify non-specific background. |
| Isotype Controls | Non-immune IgG of same species and isotype as primary antibody [66] | Control for non-specific antibody binding to tissue components. |
| Absorption Peptides | Phosphorylated and non-phosphorylated peptides corresponding to target epitope [4] | Confirm antibody specificity through competitive inhibition. |
| Detection System | HRP-polymer systems, DAB chromogen [4] [5] | Amplify signal while minimizing background; consistent application across controls and tests is critical. |
| Antigen Retrieval Buffers | Citrate buffer (pH 6.0) [4] [5] | Unmask epitopes in FFPE tissue; optimization required for each antibody. |
Critical Considerations for Experimental Design
Control for Pre-Analytical Variables
For phosphospecific IHC, pre-analytical variables significantly impact results. Studies investigating estrogen receptor α phosphorylation examined the effect of tissue collection time—the interval between surgical removal and processing—on the detection of phospho-epitopes [4]. Such variables must be controlled through standardized operating procedures to ensure reproducible results.
Avoid Common Control Missteps
A frequent error in IHC reporting is omitting the primary antibody and claiming this demonstrates antibody specificity [65]. This control only addresses non-specific binding of the secondary antibody, not the specificity of the primary antibody. The proper negative control uses isotype-specific immunoglobulins or preimmune serum at the same concentration as the primary antibody [65].
Quantitative Scoring with Established Cutoffs
When evaluating controlled experiments, use semi-quantitative scoring systems (e.g., IHC-scores combining intensity and percentage of positive cells) and establish clinically relevant cutoffs [4]. For novel phospho-markers where clinical cutoffs don't exist, percentiles based on distribution in study cohorts can provide initial thresholds [4].
The development of robust, clinically relevant phosphospecific IHC tests depends fundamentally on the implementation of appropriate positive and negative controls at every validation stage. From initial antibody characterization to final clinical application, controls provide the foundation for interpreting staining patterns and building a convincing case for the presence or absence of specific phospho-epitopes in tissue samples [65]. As the field moves toward increasingly personalized medicine approaches, with tests like the P-topoIDx assay aiming to stratify patient responders [5], the rigorous use of controls will remain the key to generating reliable, reproducible data that can confidently inform therapeutic decisions.
Establishing Confidence: Rigorous Validation and Specificity Testing for Clinical and Research Applications
The validation of phospho-specific antibodies represents a critical challenge in biomedical research, particularly for immunohistochemistry (IHC) applications where accurate detection of protein phosphorylation states can inform diagnostic and therapeutic decisions. The complexity of phosphorylation-dependent epitopes, combined with the potential for cross-reactivity and the influence of pre-analytical variables, necessitates a rigorous, multi-technique approach to antibody validation. Without comprehensive characterization, research findings may be irreproducible, potentially misleading drug development efforts. This guide objectively compares the performance of various validation methodologies and antibody products, providing researchers with experimental data and protocols to inform their reagent selection and validation workflows.
The Critical Need for Phospho-Specific Antibody Validation
Phosphorylation is the most extensively studied post-translational modification of proteins, with approximately 500 kinases identified in the human genome regulating virtually every aspect of cell function [5]. Deregulated kinase cascades are implicated in numerous disease pathways, particularly in oncology and neurodegenerative disorders. Despite this importance, the development of reliable phosphospecific immunohistochemical tests has proven challenging due to the lability of phosphorylation epitopes and technical difficulties in preserving these modifications throughout tissue processing [5].
The consequences of inadequate antibody validation are significant. Recent systematic evaluations have revealed that over half of commercially available Tau antibodies demonstrate non-selective binding to other proteins, with several cross-reacting with the related MAP2 protein [67]. Similarly, studies of tissue factor antibodies found substantial variability in quality, with some reagents detecting nonspecific bands in knockout cell lines [68]. These validation failures directly impact research reproducibility and therapeutic development, emphasizing the necessity of robust, multi-pronged validation strategies.
Comparative Analysis of Validation Methodologies
The table below summarizes the key characteristics, advantages, and limitations of principal antibody validation techniques:
Table 1: Performance Comparison of Antibody Validation Methods
| Method | Key Applications | Advantages | Limitations | Typical Validation Criteria |
|---|---|---|---|---|
| Western Blot | Specificity assessment, molecular weight confirmation, cross-reactivity screening | Determines target specificity, identifies cross-reacting bands, establishes molecular weight | Denaturing conditions may not reflect native protein conformation; limited for IHC validation alone | Single band at expected molecular weight; loss of signal in knockout controls [67] |
| Immunohistochemistry (IHC) | Tissue localization, subcellular distribution, pathological assessment | Preserves tissue architecture and cellular context; clinically relevant | Subject to pre-analytical variables (fixation, processing); semi-quantitative | Appropriate cellular/subcellular staining pattern; agreement with known expression patterns [69] |
| Tissue Microarrays (TMAs) | High-throughput validation across multiple tissue types, cancer profiling | Enables simultaneous screening of 50+ tissue types; efficient use of resources | Limited sampling per tissue; may miss heterogeneity | Consistent staining across biological replicates; tissue-specific patterns match literature [70] |
| Phosphatase Treatment | Specificity confirmation for phospho-antibodies | Directly tests phosphorylation dependency; clear negative control | May require optimization of lysis buffer composition; cannot distinguish between specific phospho-sites | Significant signal reduction after phosphatase treatment [16] |
| Cell Line Models (Overexpression/Knockout) | Specificity controls, optimal protocol development | Provides defined positive/negative controls; amenable to experimental manipulation | May not fully recapitulate native tissue context; potential adaptive changes in knockouts | Strong signal in overexpressors; absent signal in knockouts [67] |
Quantitative Performance Metrics
Recent systematic validations provide quantitative insights into antibody performance across different methodologies:
Table 2: Quantitative Performance Metrics from Systematic Antibody Validations
| Study Focus | Antibodies Tested | Success Rate | Key Failure Modes | Reference |
|---|---|---|---|---|
| Tau antibodies (WB) | 79 reagents | ~50% showed non-selective binding | Cross-reactivity with MAP2; phosphorylation sensitivity of "total" Tau antibodies | [67] |
| Tau antibodies (IHC) | 35 reagents | Varied; subset performed well | Poor performance at endogenous expression levels; fixation sensitivity | [67] |
| RPPA phospho-antibodies | 106 phospho-antibodies | 85% confirmed by WB after pre-screening | 15% showed unexpected bands or no signal | [16] |
| Commercial tissue factor antibodies | Multiple vendors | Variable; some detected nonspecific bands | Recognition of nonspecific proteins in knockout lines; species cross-reactivity issues | [68] |
Experimental Protocols for Comprehensive Validation
Western Blot Validation with Knockout Controls
Protocol Objective: To establish antibody specificity by demonstrating appropriate molecular weight detection and absence of signal in genetically validated knockout cells.
Materials:
- Wild-type and knockout cell lines (e.g., HAP1 wild-type and MAPT knockout cells [67])
- Recombinant target protein (positive control)
- Lysis buffer (RIPA or similar)
- Electrophoresis and transfer systems
- Primary antibody of interest
- Species-appropriate secondary antibodies
Methodology:
- Culture wild-type and knockout cells under standard conditions
- Prepare lysates in appropriate lysis buffer with phosphatase and protease inhibitors
- Separate 20-40μg total protein by SDS-PAGE based on target molecular weight
- Transfer to nitrocellulose or PVDF membrane
- Block membrane with 5% non-fat milk or BSA in TBST
- Incubate with primary antibody at manufacturer-recommended dilution (typically 1:500-1:5000) overnight at 4°C
- Wash and incubate with HRP-conjugated secondary antibody (1:2000-1:10000) for 1 hour at room temperature
- Develop with enhanced chemiluminescence substrate
- Validate results: Single band at expected molecular weight in wild-type but not knockout lysates [67]
Phosphatase Treatment for Phospho-Specificity Confirmation
Protocol Objective: To confirm that antibody recognition depends on phosphorylation status.
Materials:
- Cell or tissue lysates
- Alkaline phosphatase (AP) and compatible lysis buffer (e.g., AGLyse [16])
- Phosphatase inhibitors
- RPPA or Western blot equipment
Methodology:
- Divide lysates into two aliquots
- Treat one aliquot with alkaline phosphatase (concentration and duration optimized per system)
- Maintain second aliquot with phosphatase inhibitors as untreated control
- Process both samples simultaneously through RPPA or Western blot
- Compare signals: Phospho-specific antibodies should show significant signal reduction (typically >70%) in AP-treated samples [16]
- Calculate log fold-change (logFC); antibodies with logFC ≤ -0.792 typically demonstrate high specificity [16]
Tissue Microarray Validation for IHC
Protocol Objective: To assess antibody performance across multiple tissue types in a single experiment.
Materials:
- Custom-built TMAs with 50+ different tissue types from human, mouse, and rat [70]
- FFPE sections (4-5μm thickness)
- Automated staining platform (e.g., BOND RX, DISCOVERY ULTRA)
- Antigen retrieval solutions
- Appropriate detection systems
Methodology:
- Cut TMA sections at standard thickness
- Perform antigen retrieval optimized for target epitope (citrate buffer, pH 6.0, 85°C for 30 minutes [5])
- Block endogenous peroxidase activity
- Apply primary antibody with optimized concentration and incubation conditions (e.g., 2 hours at room temperature [5])
- Detect using HRP-conjugated secondaries and DAB chromogen
- Counterstain with hematoxylin
- Scan slides using high-throughput scanners (e.g., NanoZoomer S360)
- Analyze staining patterns across tissues; compare to expected expression patterns from literature and databases [70]
Integrated Validation Workflow
The following diagram illustrates a comprehensive, multi-pronged validation strategy that integrates these methodologies:
Research Reagent Solutions for Phospho-Antibody Validation
Table 3: Essential Research Reagents and Their Applications in Antibody Validation
| Reagent/Category | Specific Examples | Primary Function | Validation Role |
|---|---|---|---|
| Knockout Cell Lines | MAPT knockout HAP1 cells [67] | Definitive negative controls | Confirm absence of signal in true negative background |
| Phosphatase Enzymes | Alkaline phosphatase [16] | Phospho-group removal | Verify phosphorylation dependency of antibody binding |
| Reference Antibodies | Well-characterized clones (e.g., Tau-5 [67]) | Benchmark comparators | Establish performance standards across laboratories |
| Tissue Microarrays | Custom TMAs with 50+ tissues [70] | Multi-tissue screening platform | Assess staining patterns across diverse biological contexts |
| Automated Staining Platforms | BOND RX, DISCOVERY ULTRA [70] | Standardized IHC processing | Minimize technical variability during validation |
| Phospho-Specific Peptides | BSA-conjugated phosphopeptides [5] | Blocking controls | Demonstrate epitope specificity via competitive inhibition |
Case Studies in Methodological Integration
Case Study 1: Development of P-topoIDx IHC Assay
The development of a phosphospecific IHC assay for topoisomerase I phosphorylation at serine 10 (topoI-pS10) demonstrates effective methodological integration. Researchers began by generating a mouse monoclonal antibody through immunization with a synthetic 14 amino acid peptide containing phosphorylated serine 10 [5]. Initial screening used ELISA against both phosphorylated and non-phosphorylated peptides to establish phosphorylation dependence. Subsequently, IHC specificity was evaluated using colon cancer cell lines (HCT15 and Colo205) with known differential topoI-pS10 levels and CPT response profiles [5]. Finally, the assay was transferred to a fully automated IHC platform with optimized antigen retrieval (citrate buffer, pH 6.0, 85°C for 30 minutes) and detection protocols, creating a clinically applicable test capable of stratifying patient responders and non-responders to camptothecin analogues [5].
Case Study 2: Validation of Phospho-Tau Antibodies
A comprehensive validation of 79 Tau antibodies for Western blot and 35 for IHC revealed critical insights into phospho-antibody performance [67]. Researchers employed multiple validation techniques including:
- Recombinant Tau proteins with defined phosphorylation states
- MAPT knockout cell lines to establish specificity
- Brain tissues from wild-type and transgenic Tau models
- Comparison with mass spectrometry proteomics data
This systematic approach demonstrated that phosphorylation significantly inhibits binding for many "total" Tau antibodies, including the popular Tau-5 clone, highlighting the importance of context-specific validation [67]. The study ultimately identified a validated panel of high-performing antibodies capable of reliably detecting Tau proteoforms at physiological expression levels.
The reliable validation of phospho-specific antibodies for IHC research demands an integrated, multi-pronged strategy that combines Western blot analysis, knockout controls, phosphatase treatment, and tissue microarray screening. The experimental data presented in this guide demonstrates that no single method suffices to establish antibody specificity, with each approach contributing unique and complementary information. By implementing these comprehensive validation workflows, researchers can significantly improve the reproducibility of their findings, accelerate drug development pipelines, and ensure that critical diagnostic and therapeutic decisions are based on reliable research reagents. As antibody validation technologies continue to evolve, the standardization of these multi-technique approaches will be essential for advancing precision medicine initiatives across oncology, neuroscience, and other fields dependent on accurate protein phosphorylation detection.
The reliability of immunohistochemistry (IHC) data hinges on antibody specificity. For phospho-specific antibodies, which detect proteins modified at specific serine, threonine, or tyrosine residues, validation is particularly crucial as phosphorylation is a dynamic and transient post-translational modification regulating numerous cellular activities [12] [18]. Without rigorous validation, false positive or negative results can lead to erroneous conclusions. This guide objectively compares the experimental data from two foundational methods—phosphatase treatment and peptide blocking—used to prove phospho-specificity for IHC research, providing drug development professionals and researchers with a framework for rigorous antibody validation.
Core Principles of Phospho-Specific Antibody Validation
Phosphorylation state-specific antibodies (PSSAs) provide invaluable insight into dynamic signaling events within the spatially complex context of cells and tissues [12]. Their production typically involves immunizing animals with synthetic phosphopeptides corresponding to the amino acid sequence surrounding the phosphorylation site of the target protein [12] [18]. The resulting antisera are then affinity-purified to isolate antibodies monospecific for the phosphorylated epitope [51]. The College of American Pathologists (CAP) provides updated guidelines for the analytical validation of IHC assays, emphasizing the need to ensure accuracy and reduce variation [71]. For phospho-specific antibodies, this entails demonstrating that the observed signal is dependent on the presence of the phosphate group at a specific residue on the target protein.
Key Experimental Methods for Proving Specificity
Two of the most critical wet-lab experiments for establishing phospho-specificity are phosphatase treatment and peptide blocking. Each method tests the antibody's dependency on the phosphorylated state through a different mechanism.
Phosphatase Treatment
This method validates specificity by enzymatically removing phosphate groups from the target protein.
- Concept: Pre-incubating tissue sections or protein lysates with a phosphatase enzyme, such as lambda phosphatase (λ-PPase), should abolish the antibody's binding signal by dephosphorylating the epitope. This serves as a direct functional test for phosphate dependency [18].
- Protocol:
- Sample Preparation: Generate tissue sections or cell lysates from formalin-fixed, paraffin-embedded (FFPE) or frozen samples.
- Phosphatase Incubation: Treat serial sections or lysate aliquots with an active phosphatase (e.g., λ-PPase) in the appropriate reaction buffer. Include control sections treated with buffer alone or with phosphatase inhibitors.
- Inactivation: Terminate the phosphatase reaction, often by heating or adding specific inhibitors.
- Immunodetection: Process both phosphatase-treated and control samples for IHC or western blotting using the phospho-specific antibody in question.
- Interpretation: A significant reduction in immunostaining in the phosphatase-treated sample, compared to the control, confirms the signal is phosphorylation-dependent.
Peptide Blocking (Immunoneutralization)
This method validates specificity by competitive binding, using the phosphorylated peptide antigen to block the antibody's paratope.
- Concept: Pre-absorbing the antibody with an excess of the phosphopeptide used as the immunogen should competitively inhibit its binding to the target epitope in the tissue. This confirms the antibody's specificity for that exact phosphorylated sequence [4] [51].
- Protocol:
- Peptide Preparation: Obtain the specific phosphopeptide and its non-phosphorylated counterpart.
- Antibody Pre-absorption: Incubate the phospho-specific antibody with a ~30-fold molar excess of either the phosphopeptide or the non-phosphorylated peptide [4]. A third aliquot is left untreated as a control.
- Immunostaining: Apply the pre-absorbed and control antibody solutions to serial tissue sections.
- Interpretation: Specificity is demonstrated when staining is abolished only in the section stained with the phosphopeptide-pre-absorbed antibody. Staining should persist with the non-phosphorylated peptide and the untreated antibody, proving that recognition requires the phosphorylated form of the sequence [51].
The logical relationship and outcomes of these experiments are summarized in the workflow below.
Comparative Experimental Data Analysis
The following tables summarize the quantitative and qualitative outcomes of applying these validation methods, as reported in the scientific literature.
Table 1: Validation Data from Peer-Reviewed Studies
| Target Protein | Validation Method | Key Experimental Finding | Outcome | Citation |
|---|---|---|---|---|
| Phospho-p53 (S15) | Phosphatase Treatment | Western blot signal in UV-irradiated CEM cells was abolished by λ-phosphatase treatment. | Specificity Confirmed | [18] |
| Multiple pERα sites (e.g., P-S118-ERα) | Peptide Blocking | IHC staining was specifically neutralized only with the corresponding phospho-peptide, not the non-phosphorylated peptide. | Specificity Confirmed | [4] |
| Phospho-ERK1/2 (Thr202, Tyr204) | Peptide Blocking | Western blot signal was blocked only by the specific phospho-peptide; generic phospho-peptides or non-phospho peptide had no effect. | Specificity Confirmed | [51] |
| S499-pFMRP (abcam antibody) | Knockout Control | A band was present in Fmr-1 KO mice, which lack the target protein, indicating non-specific binding. | Specificity Failed | [72] [73] |
Table 2: Advantages and Limitations of Key Validation Methods
| Method | Key Advantage | Key Limitation | Suitable for IHC? |
|---|---|---|---|
| Phosphatase Treatment | Directly demonstrates phosphate dependency of the signal. | Potential for incomplete dephosphorylation or non-specific effects on tissue antigenicity. | Yes, on tissue sections |
| Peptide Blocking | Directly confirms specificity for the exact immunogen sequence. | Requires synthesis of high-purity peptides; a negative result can be difficult to interpret. | Yes |
| Knockout Tissue Control | Provides the most rigorous negative control by completely removing the target antigen. | Requires access to genetically modified tissue, which can be costly and time-consuming. | Yes |
| Cell Line with Mutated Site | Excellent for confirming site-specificity by mutating the phosphorylatable serine/threonine to alanine. | Requires validated cell models and may not account for tissue-specific context. | Indirectly (via cell pellets) |
The Scientist's Toolkit: Essential Reagents & Materials
Successful validation requires specific, high-quality reagents. The following table details key solutions and materials required for these experiments.
Table 3: Essential Research Reagent Solutions for Phospho-Specificity Validation
| Reagent / Material | Function / Purpose | Example from Literature |
|---|---|---|
| Phosphatase Enzymes | Enzymatically removes phosphate groups from proteins to test signal dependency. | Lambda phosphatase (λ-PPase) [18]. |
| Phospho-Specific Peptides | Used for competitive blocking experiments to confirm antibody specificity. | Synthetic peptides matching the phosphorylated epitope [4] [51]. |
| Non-Phosphorylated Peptides | Critical control for peptide blocking experiments to ensure blocking is phosphorylation-dependent. | Synthetic peptides with an identical sequence but lacking the phosphate group [51]. |
| Cell Penetrating Peptide Inhibitors | Used in functional studies to probe the role of specific phosphatases in signaling pathways. | TAT-Y127WT peptide used to inhibit PP2A activation [74] [75]. |
| Validated Positive Control Tissues/Cells | Provides a known positive sample to ensure the antibody and assay are working correctly. | FFPE breast cancer tissue microarrays with known ERα phosphorylation status [4]. |
Rigorously validating phospho-specific antibodies with phosphatase treatment and peptide blocking experiments is not merely a best practice but a fundamental requirement for generating reliable IHC data. The experimental evidence consistently shows that antibodies validated with these methods, such as those for phospho-ERα and phospho-ERK1/2, yield specific and interpretable results [4] [51]. In contrast, antibodies that fail these or similar controls, as seen with a commercial pFMRP antibody, can produce misleading, non-specific signals [72] [73]. For researchers and drug developers, investing in this level of analytical validation is paramount for accurately profiling signaling pathways in human disease and for the credible development of new anti-fibrotic therapies or kinase-targeted treatments.
The validation of phospho-specific antibodies for immunohistochemistry (IHC) research represents a critical frontier in biomedical science, enabling precise visualization of dynamic cellular signaling events directly in tissue architecture. For researchers and drug development professionals, assessing antibody performance through the trifecta of sensitivity, specificity, and consistency is not merely procedural but fundamental to data integrity. Phospho-specific antibodies detect proteins only at specific phosphorylation sites, serving as essential tools for understanding active signaling pathways in fields from cancer biology to neuroscience [76]. This guide provides an objective comparison of antibody performance metrics and methodologies, framed within the broader context of validating these crucial reagents for IHC applications.
Performance Comparison of Phospho-Specific Antibodies
The following tables synthesize quantitative performance data for commercially available phospho-specific antibodies, focusing on key metrics relevant to IHC applications.
Table 1: Key Performance Metrics for Phospho-Specific Antibodies
| Antibody Target | Clone/Product # | Species Reactivity | IHC Dilution | Specificity Notes | Supplier |
|---|---|---|---|---|---|
| Phospho-TAZ (Ser89) | (E1X9C) Rabbit mAb #59971 | H, M, R | 1:500 - 1:2000 [77] | Detects TAZ p-Ser89; may cross-react with YAP p-Ser127 [77] | Cell Signaling Technology |
| Phospho-ERK1/ERK2 (Thr185, Tyr187) | 15H10L7 #700012 | Human, Mouse, Rat, Dog [78] | 5 µg/mL [78] | Predicted reactivity with bovine, chicken, zebrafish [78] | Thermo Fisher Scientific |
Table 2: Comparative Assessment of Antibody Consistency and Validation
| Characteristic | Recombinant Monoclonal Antibodies | Traditional Monoclonal Antibodies | Polyclonal Antibodies |
|---|---|---|---|
| Lot-to-Lot Consistency | Superior consistency due to in vitro expression systems [77] [78] | Good, but subject to biological variability in hybridomas | Low consistency due to heterogeneous immune response |
| Production Method | In vitro expression systems (e.g., Expi293) [78] | Hybridoma technology | Animal immunization |
| Key Advantages | Animal-free production, continuous supply, defined sequence [77] [78] | Well-established technology, stable clones | Potential for higher signal in some applications |
| IHC Validation | Often highly validated with application-specific data | Requires careful lot-specific validation | Requires extensive batch-specific validation |
Experimental Protocols for Antibody Validation
Robust experimental protocols are essential for establishing antibody performance in IHC. The following methodologies are critical for validating sensitivity, specificity, and consistency.
Standard Immunohistochemistry Protocol
A generalized IHC protocol forms the foundation for all antibody validation workflows [19]:
- Sample Fixation: Fix tissue samples in 4% Paraformaldehyde (PFA) for 10 minutes to several hours, depending on tissue size. Formaldehyde-based fixatives preserve tissue integrity while maintaining antigenicity, though over-fixation can mask epitopes and require antigen retrieval [19].
- Permeabilization: Treat samples with 0.1% Triton X-100 for 10 minutes to allow antibody penetration [78].
- Blocking: Incubate tissues with 1-5% BSA or serum for 1 hour at room temperature to prevent non-specific antibody binding [19] [78].
- Primary Antibody Incubation: Apply phospho-specific antibody at optimized dilution (e.g., 1:500 to 1:2000 for #59971 [77]) and incubate in a humidity chamber. Incubation times vary from 1 hour at room temperature to overnight at 4°C.
- Secondary Antibody Incubation: Add enzyme-conjugated (e.g., HRP) or fluorophore-conjugated secondary antibody for 1 hour at room temperature.
- Detection: Use chromogenic substrates (e.g., DAB) for brightfield microscopy or directly image fluorophores [19].
- Counterstaining: Apply nuclear counterstains such as Hematoxylin (for chromogenic) or DAPI (for fluorescence) to provide cellular context [79].
- Mounting and Imaging: Mount slides with appropriate media and image using brightfield or fluorescence microscopy.
Specificity Validation Protocols
- Peptide Competition Assay: Pre-incubate the phospho-specific antibody with an excess of the immunizing phosphopeptide. Specific staining should be significantly reduced or abolished, while non-specific staining remains [77].
- Cell-Based Specificity Controls: Treat cells with phosphatase enzymes to dephosphorylate the target protein, which should eliminate antibody binding. Conversely, using cells known to express the phosphorylated target provides a positive control.
- Genetic Validation:
- Knockdown/Knockout: Use siRNA, CRISPR, or other genetic methods to reduce or eliminate the target protein. A specific antibody should show significantly reduced signal.
- Constitutively Active Mutants: Transfert cells with plasmids encoding phospho-mimetic (e.g., aspartic acid) or constitutively active (e.g., TAZ S89A [77]) mutants of the target protein to confirm antibody recognition.
Sensitivity and Lot-to-Lot Consistency Protocols
- Titration Series: Perform IHC with a range of antibody concentrations (e.g., from 1:100 to 1:10,000) to determine the optimal dilution that provides strong specific signal with minimal background.
- Multi-Lot Testing: Compare at least three different production lots of the same antibody on serial sections of the same tissue sample under identical experimental conditions. Consistent staining intensity and pattern indicate high lot-to-lot consistency [77].
Signaling Pathways and Experimental Workflows
Understanding the biological context of phosphorylation targets and the procedural flow of IHC validation is crucial for appropriate antibody application and data interpretation.
Hippo Signaling Pathway and TAZ Regulation
The diagram below illustrates the Hippo signaling pathway, a key regulatory network controlling cell growth and organ size, and the central role of TAZ phosphorylation.
Diagram 1: Hippo pathway regulates TAZ activity.
This pathway highlights the functional significance of TAZ phosphorylation at Ser89, the target of the Phospho-TAZ (Ser89) antibody [77]. Phosphorylation by LATS1/2 kinases promotes TAZ binding to 14-3-3 proteins, leading to its cytoplasmic sequestration and degradation, thereby inactivating its transcriptional co-activator function [77]. Conversely, non-phosphorylated TAZ translocates to the nucleus and drives gene expression programs linked to stem cell phenotypes, a mechanism exploited in cancers [77].
IHC Antibody Validation Workflow
A systematic, multi-stage workflow is essential for rigorous antibody validation.
Diagram 2: IHC antibody validation workflow.
The Scientist's Toolkit: Essential Research Reagents
Successful IHC experimentation relies on a suite of carefully selected reagents and tools.
Table 3: Essential Reagents for Phospho-Specific IHC
| Reagent/Tool | Function/Purpose | Examples & Key Considerations |
|---|---|---|
| Phospho-Specific Antibody | Detects the phosphorylated form of a target protein; core reagent. | Clone #59971 for TAZ p-Ser89 [77]; recombinant monoclonals offer superior consistency [78]. |
| Primary Antibody | Unconjugated antibody generated against the target phospho-epitope. | Must be validated for IHC application and species. |
| Secondary Antibody | Enzyme- or fluorophore-conjugated antibody that binds the primary antibody for detection. | HRP-conjugated for chromogenic (DAB) detection; fluorophore-conjugated (e.g., Alexa Fluor) for IF. |
| Counterstain | Provides contrast by staining cellular components not targeted by the primary antibody. | Hematoxylin: blue nuclear stain for chromogenic IHC [79].DAPI: blue fluorescent nuclear stain for IF [79]. |
| Fixative | Preserves tissue architecture and antigenicity by cross-linking or precipitating proteins. | 4% Paraformaldehyde (PFA): common cross-linking fixative [19] [78]. |
| Mounting Medium | Preserves the sample and secures the coverslip for microscopy. | Use anti-fade mounting media for fluorescent samples to prevent photobleaching [79]. |
| Detection System | Generates a visible signal at the antigen-antibody binding site. | DAB Chromogen: produces a brown precipitate [79].Fluorescence Microscope: required to visualize fluorophores. |
The rigorous assessment of sensitivity, specificity, and lot-to-lot consistency is paramount for leveraging phospho-specific antibodies as precise tools in IHC research. As the data demonstrate, recombinant monoclonal antibody technology offers significant advantages for experimental reproducibility, a critical concern for both basic research and drug development. The integration of standardized validation protocols, such as those outlined here, along with a clear understanding of the underlying signaling pathways, provides a framework for generating reliable, interpretable data. The continued advancement and careful validation of these reagents will undoubtedly fuel future discoveries in cell signaling and the development of targeted therapeutics.
For researchers, scientists, and drug development professionals, the selection of appropriate antibodies is a critical step in experimental design, particularly for demanding applications like immunohistochemistry (IHC). The choice between rabbit and mouse monoclonal antibodies can significantly impact the specificity, sensitivity, and overall success of your research, especially within the nuanced field of phospho-specific antibody validation. This guide provides an objective comparison of these two clonal types, underpinned by experimental data, to inform your selection process and support the generation of reliable, reproducible results.
Biological and Structural Foundations
The performance differences between rabbit and mouse monoclonal antibodies are rooted in the distinct biological mechanisms of their immune systems. Understanding these foundational aspects is key to making an informed choice.
Rabbit Monoclonal Antibodies (RabMAbs) originate from a species belonging to the order Lagomorpha, which is evolutionarily distinct from the rodents [80]. This evolutionary distance contributes to their ability to recognize epitopes on human antigens that may not be immunogenic in mice [81] [80]. A key biological advantage is their antibody maturation process; rabbits utilize both somatic hypermutation (SHM) and an additional mechanism called somatic gene conversion (SGC) to generate their secondary antibody repertoire [81]. This dual mechanism often produces antibodies with exceptionally high affinity, typically in the picomolar range (10^-10 to 10^-12 M), which is significantly higher than the nanomolar or sub-nanomolar affinity common for most mouse monoclonals [81] [80].
Mouse Monoclonal Antibodies (MMs), in contrast, are derived from a well-established model organism where the hybridoma technology for monoclonal antibody production was first pioneered [82]. Their immune system relies heavily on somatic hypermutation for affinity maturation. While this can produce high-affinity binders, the typical affinity range for mouse mAbs is often reported between 30–300 pM, which may be generally lower than that achieved by rabbits, though direct comparative studies on a wide variety of antigens are still needed [80].
The following diagram illustrates the critical divergence in the B-cell and antibody development pathways between these two species.
Performance Comparison in Key Applications
The structural and biological differences between rabbit and mouse monoclonals translate directly into varied performance across laboratory applications. The table below summarizes quantitative and qualitative data for easy comparison.
| Feature | Rabbit Monoclonal Antibodies | Mouse Monoclonal Antibodies |
|---|---|---|
| Typical Affinity (Kd) | Picomolar range (10^-10-10^-12 M) [81] | Nanomolar/Sub-nanomolar range (10^-7-10^-9 M) [81] |
| Epitope Recognition | Can recognize epitopes inaccessible to murine mAbs; strong response to small molecules/haptens [81] [80] | Standard epitope recognition; may not generate immune response to some conserved human antigens [80] |
| Specificity | High specificity for a single epitope [82] [83] | High specificity for a single epitope [82] [83] |
| Sensitivity in IHC | Consistently higher sensitivity in multiple IHC studies [84] [80] | Good, but may suffer from background in mouse tissues [85] |
| Batch Consistency | Excellent, with minimal lot-to-lot variability [82] | Excellent, with minimal lot-to-lot variability [82] |
| Cross-reactivity with Mouse Tissues | Ideal for mouse model studies, eliminating background from endogenous Igs [85] | Can cause high background in mouse tissues due to secondary antibody binding to endogenous Igs [85] |
A pivotal consideration in pre-clinical research is the use of mouse models. When performing IHC on mouse tissue with a mouse primary antibody, the secondary anti-mouse antibody will inevitably bind to endogenous immunoglobulins throughout the tissue, creating high background staining [85]. Rabbit monoclonal antibodies provide an elegant solution to this problem, as an anti-rabbit secondary antibody will not recognize mouse immunoglobulins, thereby yielding a much cleaner signal with lower background [85]. This makes RabMAbs the superior choice for immunohistochemical analysis in syngeneic mouse models or studies of normal mouse tissue.
For phospho-specific antibodies, which are critical for signaling research, rigorous validation is non-negotiable. Key experimental protocols for validating these reagents in IHC include:
- Phosphatase Treatment: Tissue sections or cell pellets are treated with phosphatases to remove phosphate groups. A valid phospho-specific antibody should show a significant reduction or complete loss of staining after this treatment, confirming that the signal depends on the phosphorylated state of the target [86].
- Blocking Peptides: Staining is performed in the presence of the phospho-specific peptide used to generate the antibody. The peptide should competitively inhibit antibody binding and eliminate the specific staining signal. A control with a non-phosphorylated or irrelevant peptide should not affect the staining, ruling out non-specific Fc-mediated binding [4] [86].
- Cell Line Models: Using xenografts or cell pellets from isogenic cell lines that differ only in the phosphorylation status of the target protein (e.g., stimulated vs. unstimulated, or wild-type vs. kinase-dead) provides a robust system for confirming specificity [86].
The Scientist's Toolkit: Essential Reagents for IHC Validation
Successful IHC, particularly with phospho-specific antibodies, relies on a suite of carefully selected reagents and controls. The following table details essential components of a rigorous IHC workflow.
| Reagent / Material | Function in IHC Validation |
|---|---|
| Phosphatase Enzymes | Enzymes (e.g., lambda phosphatase) used to dephosphorylate tissue antigens; loss of signal confirms antibody specificity for the phosphorylated epitope [86]. |
| Blocking Peptides | Synthetic peptides identical to the phosphorylated immunogen. They compete with the epitope for antibody binding; loss of signal confirms specificity [4] [86]. |
| Recombinant Protein/ Cell Pellet Controls | Paraffin-embedded pellets of cells with known expression (or knockout) of the target protein. They serve as essential positive and negative controls for antibody performance [86]. |
| Isotype Control Antibodies | Non-immune IgGs of the same species and isotype as the primary antibody. They help distinguish specific staining from non-specific background caused by Fc receptor binding [83]. |
| Xenograft Tissues | Human tumor xenografts grown in mice, with known protein expression levels, used to verify antibody specificity in a complex tissue context [86]. |
| Multi-rAb Recombinant Secondaries | Mixtures of recombinant monoclonal secondary antibodies that recognize multiple epitopes on the primary antibody. They offer high sensitivity, low background, and exceptional lot-to-lot consistency [83]. |
| Tissue Microarrays (TMAs) | Slides containing small sections of dozens of different tissue types. They allow for high-throughput validation of antibody performance across a broad spectrum of normal and pathological tissues [4]. |
The logical workflow for selecting and validating an antibody for IHC, incorporating these key reagents, can be visualized as follows.
The decision between rabbit and mouse monoclonal antibodies is not a matter of one being universally superior, but rather which is optimal for a specific research context. Rabbit monoclonal antibodies often hold a distinct advantage for IHC due to their high affinity, ability to recognize a broader set of epitopes, and superior performance in mouse model systems by eliminating background from endogenous immunoglobulins. This makes them particularly valuable for phospho-specific IHC research. However, the ultimate key to success lies in rigorous validation. Regardless of the clonal type selected, researchers must employ a comprehensive strategy—including phosphatase treatment, blocking peptides, and appropriate biological controls—to ensure antibody specificity and generate reliable, reproducible data for drug development and scientific discovery.
Conclusion
The successful validation of phospho-specific antibodies for IHC is a multi-faceted process that demands a deep understanding of phosphorylation biology, meticulous optimization of staining protocols, proactive troubleshooting, and uncompromising validation standards. By adhering to the rigorous frameworks outlined for foundational knowledge, methodological application, problem-solving, and validation, researchers can develop reliable, reproducible assays. These robust tools are pivotal for advancing our understanding of cellular signaling in physiological and pathological states, accelerating the discovery of predictive biomarkers, and ultimately paving the way for more personalized therapeutic strategies in oncology and other diseases. Future directions will likely involve greater automation, standardization, and the integration of digital pathology for quantitative analysis, enhancing the translational potential of phospho-specific IHC.
References
- 1. Phosphorylation | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/phosphorylation.html]
- 2. The crucial role of protein phosphorylation in cell signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5500920/]
- 3. Role of protein phosphorylation in cell signaling, disease, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9632491/]
- 4. Immunohistochemical validation of multiple phospho ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3448371/]
- 5. Developing a Phosphospecific IHC Assay as a Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6071180/]
- 6. Phospho-IHC-7TM-Antibodies [https://7tmantibodies.com/phospho-ihc-7tm-antibodies]
- 7. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOoo4yb9xQJXM4hGmz63SGURlsElq-vRaJ9AHLrfHT5pKQhRj4S4k]
- 8. Protein dephosphorylation protocol [https://www.abcam.com/en-us/technical-resources/protocols/protein-dephosphorylation]
- 9. Higher phosphorylated tau levels predict cognitive decline ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-025-01912-6]
- 10. Protocol for screening and validating antibodies specific to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11345596/]
- 11. Phospho Specific Antibodies: A Powerful Tool for Protein ... [https://www.sinobiological.com/resource/antibody-technical/phospho-specific-antibody]
- 12. Phosphorylation State-Specific Antibodies - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC1892416/]
- 13. A critical evaluation of strategies used for validation ... [https://www.sciencedirect.com/science/article/pii/S1574789114000568]
- 14. Can You Trust Your Immunohistochemistry Results? [https://www.cellsignal.com/learn-and-support/videos-and-webinars/webinar-can-you-trust-your-ihc-results?srsltid=AfmBOooUpizMmq5xedkpw_IzDu8q0AiANGOq3gILaNjzsO52L3l0LP6J]
- 15. Antibody validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3891910/]
- 16. A reverse phase protein array based phospho-antibody ... [https://www.nature.com/articles/s41598-022-26715-9]
- 17. Phospho-specific Antibodies [https://www.sinobiological.com/activities/antibodies-of-the-month-202511]
- 18. Methods for Detecting Protein Phosphorylation [https://www.rndsystems.com/resources/articles/methods-detecting-protein-phosphorylation]
- 19. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 20. What Are Phospho-Specific Antibodies? - CST Blog [https://blog.cellsignal.com/have-you-ever-wondered-whats-the-lowdown-on-phospho-specific-antibodies]
- 21. Antigenic Dark Matter: Unexplored Post-Translational ... [https://www.mdpi.com/2072-6694/17/21/3506]
- 22. Immunoelectron microscopy: a comprehensive guide from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420552/]
- 23. Low-Abundance Protein Enrichment for Medical Applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC10299117/]
- 24. Novel method for the high-throughput production of ... [https://www.nature.com/articles/srep25174]
- 25. Optimizing Immunohistochemistry Validation and ... [https://www.precisionformedicine.com/blog/optimizing-ihc-validation-regulatory-strategies]
- 26. Enhancing Antigen Retrieval To Unmask Signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9096965/]
- 27. Preanalytical variables and phosphoepitope expression in ... [https://www.nature.com/articles/labinvest2014139]
- 28. The impact of crosslinking and non-crosslinking fixatives ... [https://www.sciencedirect.com/science/article/abs/pii/S1871678419300792]
- 29. IHC-P protocols [https://www.abcam.com/en-us/technical-resources/protocols/ihc-with-samples-in-paraffin]
- 30. Sample preparation [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/sample-preparation-for-ihc]
- 31. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOoqoZiIdDHWTkQ2ERA_wxfOcIRQ6vtdBfH28cuucH8M4FJt1Q7XW]
- 32. Antigen Retrieval Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC3201121/]
- 33. High-throughput screening and validation of antibodies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7900253/]
- 34. IHC Antigen Retrieval Protocol | Heat & Enzyme Methods [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-optimization/antigen-retrieval?srsltid=AfmBOooQXJ9aISrKnsz5Nyg5AHOf4qa7ujuRVLuwd6Y2mIZcRqysh2AD]
- 35. Comparison of Antigen Retrieval Methods for ... [https://www.mdpi.com/2409-9279/7/5/67]
- 36. IHC antigen retrieval protocol [https://www.abcam.com/en-us/technical-resources/protocols/ihc-antigen-retrieval]
- 37. Will an antibody recommended for IHC-P with one retrieval ... [https://www.cellsignal.com/learn-and-support/technical-support/will-an-antibody-recommended-for-ihc-p-with-one-retrieval-buffer-work-with-another/000001379?srsltid=AfmBOopS6LnrkwDc4qvMLaAvZzr2Y_tRQWep8A9gafgInNHl2dIQrvvo]
- 38. Evaluation of Antigen Retrieval Buffer Systems [https://link.springer.com/article/10.1023/B:HIJO.0000039854.17808.e0]
- 39. IHC Immunodetection (Staining) [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-immunodetection.html]
- 40. Intro to Immunohistochemistry (IHC) Staining: Steps & Best ... [https://www.leicabiosystems.com/us/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 41. Standard Immunohistochemistry Staining Method [https://ihcworld.com/2024/01/23/standard-immunohistochemistry-staining-method/]
- 42. IHC Standard Protocol [https://www.atlasantibodies.com/knowledge-hub/protocols-for-antibody-applications/ihc-standard-protocol/]
- 43. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOoqxiVY-8lTrGGkvWBF_xIsvs5spqmKicYs1TMXuPNh1pKms_K5a]
- 44. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 45. Development and validation of an expanded antibody ... [https://www.nature.com/articles/s41531-023-00604-y]
- 46. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOoq_roFpXrjk0dBsExdmgOzS6u9EHdZP4vNd3B52zIpG7-TZRPY9]
- 47. Antibody validation of immunohistochemistry for biomarker ... [https://www.sciencedirect.com/science/article/pii/S1046202314000280]
- 48. Head-to-head comparison of 10 plasma phospho-tau ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10115176/]
- 49. Plasma phospho-tau217 as a predictive biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11694372/]
- 50. Immunohistochemistry as an Important Tool in Biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2832341/]
- 51. An Overview of Phosphospecific Antibodies [https://www.thermofisher.com/us/en/home/life-science/antibodies/antibodies-learning-center/antibodies-resource-library/antibody-methods/overview-phosphospecific-antibodies.html]
- 52. Antigen Retrieval in IHC: Why It Matters and How to Get ... [https://www.atlasantibodies.com/knowledge-hub/blog/antigen-retrieval-in-ihc-why-it-matters-and-how-to-get-it-right/]
- 53. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 54. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOooRcgOS9_O3Y5WJE_6HwkkZh37UaRiK9-TQ-Qs5g_1bQuDt6e1j]
- 55. Antibody validation of immunohistochemistry for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4240800/]
- 56. Immunohistochemistry Troubleshooting [https://www.antibodies.com/applications/immunohistochemistry/ihc-troubleshooting]
- 57. How to Avoid or Reduce High Background in ... [https://www.linkedin.com/pulse/how-avoid-reduce-high-background-immunohistochemistry-huang-md-phd-xtvpe]
- 58. Blocking Strategies for IHC [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/blocking-strategies-ihc.html]
- 59. Immunohistochemistry Basics: Blocking Non-Specific ... [https://bitesizebio.com/13466/immunohistochemistry-basics-blocking-non-specific-staining/]
- 60. Blocking in IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/blocking-in-ihc]
- 61. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOoqLCYrQRVJ6go5nnJBS55lU__HcXZ9ngWBuo-W0Kdcn07OeKy6A]
- 62. Overview of Protease and Phosphatase Inhibition for ... [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/protease-phosphatase-inhibitors.html]
- 63. Protease and Phosphatase Inhibitors in Protein Preparation [https://www.creative-proteomics.com/resource/protease-phosphatase-inhibitors-protein-preparation.htm]
- 64. Immunoblot validation of phospho-specific antibodies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8034249/]
- 65. Controls for Immunohistochemistry: The Histochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4212362/]
- 66. Controls in IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/controls-in-ihc]
- 67. Identification of high-performing antibodies for the reliable ... [https://link.springer.com/article/10.1007/s00401-024-02729-7]
- 68. Evaluation of different commercial antibodies for their ... [https://www.sciencedirect.com/science/article/pii/S2475037922020672]
- 69. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOopphjquUkntb3jSpB6xav-y5mrBTDEdlfjkO13Q9zLDCTb_FQwy]
- 70. Inside our application testing [https://www.abcam.com/en-us/stories/articles/inside-our-application-testing]
- 71. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 72. Comparison of Equivalence between Two Commercially ... [https://pubmed.ncbi.nlm.nih.gov/26580204/]
- 73. Comparison of Equivalence between Two Commercially ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0143134]
- 74. Blocking protein phosphatase 2A with a peptide protects ... [https://pubmed.ncbi.nlm.nih.gov/32584210/]
- 75. Blocking protein phosphatase 2A signaling prevents ... [https://www.nature.com/articles/srep19821]
- 76. Guide to Phospho-Specific Antibodies [https://businessoutstanders.com/biotech/phospho-antibodies-cell-signaling-research-guide]
- 77. -TAZ (Ser89) (E1X9C) Rabbit mAb | Cell Signaling Technology Phospho [https://www.cellsignal.com/products/primary-antibodies/phospho-taz-ser89-e1x9c-rabbit-mab/59971]
- 78. -ERK1/ERK2 (Thr185, Tyr187) Recombinant Monoclonal... Phospho [https://www.thermofisher.com/antibody/product/Phospho-ERK1-ERK2-Thr185-Tyr187-Antibody-clone-15H10L7-Recombinant-Monoclonal/700012]
- 79. Counterstains in Immunohistochemistry: Principles, ... [https://www.bosterbio.com/blog/post/counterstains-in-immunohistochemistry-principles-options-and-troubleshooting?srsltid=AfmBOoqcowfLzdVZQGps-2SGvALh6IrcoyLL8o_2sTbPCjC1CaWFcaEa]
- 80. From rabbit antibody repertoires to rabbit monoclonal ... [https://www.nature.com/articles/emm201723]
- 81. Rabbit monoclonal antibodies: Synergistic innovation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0927776525006861]
- 82. Mouse Monoclonal vs. Rabbit Polyclonal Antibodies [https://greenmoab.com/resources/mouse-monoclonal-vs-rabbit-polyclonal-antibodies-which-is-right-for-your-research/]
- 83. Selecting Antibodies For IHC [https://www.ptglab.com/support/immunohistochemistry-protocol/selecting-antibodies-for-ihc/?srsltid=AfmBOooRS8vFrKWwWSwcLJmyz6tqYVFaL_P8H3cBYWU3SIFa_DVtLPLQ]
- 84. Comparison of rabbit monoclonal and mouse ... [https://pubmed.ncbi.nlm.nih.gov/16130992/]
- 85. Pre-Clinical IHC Tools for Mouse Models [https://www.cellsignal.com/applications/immunohistochemistry/preclinical-ihc-tools-for-mouse-models?srsltid=AfmBOopZRJ9HJRl7c0J0Wz70XrLT51vzuIYn2FqlMgL1r5HftZHfLgZ-]
- 86. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOoprsR_OqvcFsd2bIKimhBX4GHUR5x7Pi8-Phd7BDR8qWB0Vw_hM]