Controlling Endogenous Enzyme Activity in IHC: A Complete Guide to Blocking, Troubleshooting, and Validation
This article provides researchers, scientists, and drug development professionals with a comprehensive guide to addressing endogenous enzyme activity in Immunohistochemistry (IHC).
Controlling Endogenous Enzyme Activity in IHC: A Complete Guide to Blocking, Troubleshooting, and Validation
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive guide to addressing endogenous enzyme activity in Immunohistochemistry (IHC). Endogenous enzymes like peroxidase and alkaline phosphatase are a major source of non-specific staining and high background in both chromogenic and fluorescent IHC, particularly in tissues such as liver, kidney, and spleen. We cover the foundational science behind enzyme interference, detail proven methodological blocking protocols, offer advanced troubleshooting strategies for complex cases, and outline rigorous validation frameworks to ensure assay reliability and reproducibility. This guide is essential for achieving accurate, interpretable, and publication-quality IHC results.
Understanding the Enemy: Foundational Concepts of Endogenous Enzymes in IHC
Endogenous Enzymes and Why Do They Interfere with IHC
What are endogenous enzymes?
Endogenous enzymes are proteins with catalytic activity that are naturally present in cells and tissues. In the context of Immunohistochemistry (IHC), the most relevant endogenous enzymes are peroxidases and alkaline phosphatases [1] [2]. These enzymes are intrinsic components of the biological samples being analyzed. For example, endogenous peroxidase activity is particularly found in red blood cells and tissues such as the kidney and liver, while endogenous alkaline phosphatase is common in the intestine, kidney, lymphoid tissue, and placenta [1] [2].
How do they interfere with IHC?
Endogenous enzymes interfere with IHC because they react with the same chromogenic substrates used in the detection system to visualize the target antigen. IHC often uses reporter enzymes, such as Horseradish Peroxidase (HRP) or Alkaline Phosphatase (AP), which are conjugated to antibodies. When a substrate is added, these reporter enzymes catalyze a reaction that produces a colored precipitate, pinpointing the location of the protein of interest [3].
If endogenous enzyme activity is not blocked, it will catalyze the same color-producing reaction, generating a precipitate indiscriminately throughout the tissue section. This results in non-specific staining and a high background signal, which can obscure the specific signal from the target antigen and lead to false-positive results [1] [4] [2].
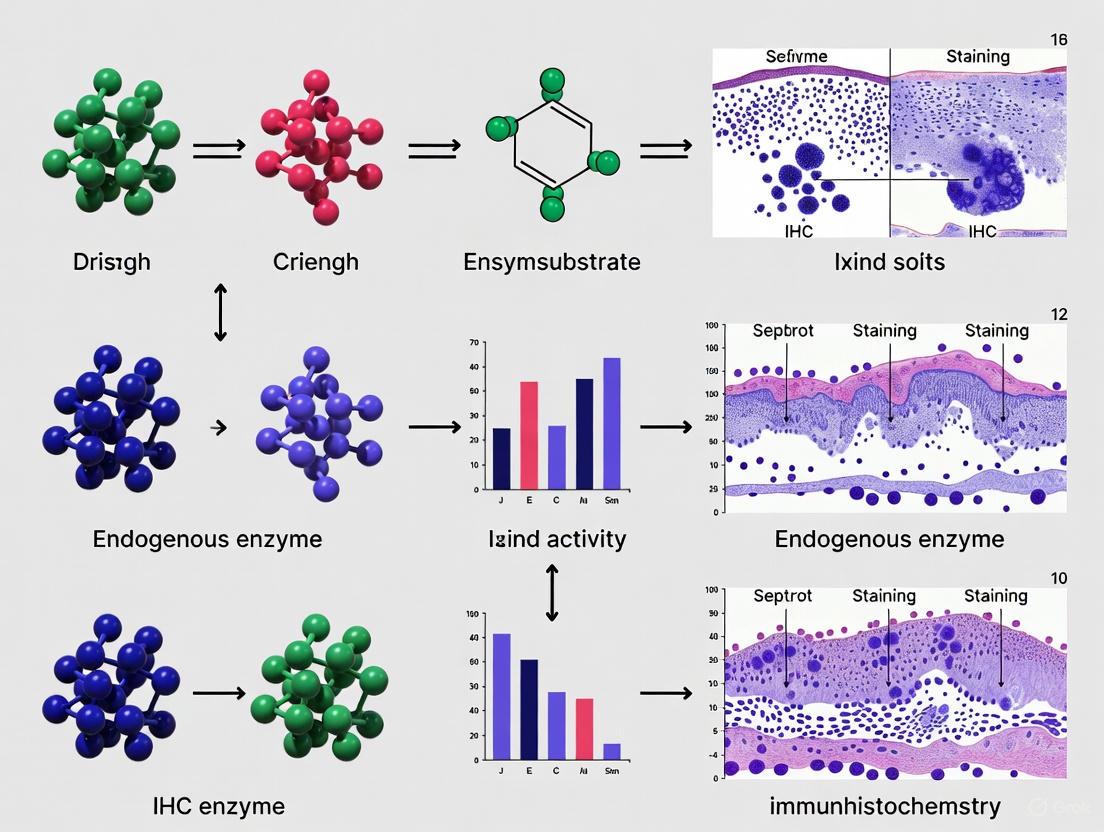
The diagram below illustrates this interference mechanism.
How can I detect endogenous enzyme activity in my samples?
Before beginning an IHC experiment, it is good practice to test for the presence of interfering endogenous enzymes. The methods are straightforward and involve incubating an untreated tissue section with the detection substrate alone.
| Enzyme Type | Test Substrate | Positive Result Indicated By | Common Tissue Locations |
|---|---|---|---|
| Peroxidase [1] [2] | 3,3'-Diaminobenzidine (DAB) | Brown-colored precipitate | Kidney, liver, red blood cells [1] [2] |
| Alkaline Phosphatase [1] [2] | BCIP/NBT | Blue-colored precipitate | Intestine, kidney, bone (osteoblasts), lymphoid tissue, placenta [1] [2] |
What are the specific methods for blocking endogenous enzymes?
Effective blocking is a critical step to eliminate non-specific signals. The standard methods for quenching endogenous enzyme activity are summarized in the table below.
| Enzyme to Block | Recommended Blocking Method | Typical Incubation Conditions | Key Considerations |
|---|---|---|---|
| Peroxidase [1] [4] [2] | Incubation with 0.3% - 3.0% hydrogen peroxide (H₂O₂) in methanol or water. | 10-15 minutes at room temperature [1] [4]. | Sodium azide is a potent inhibitor of HRP; do not use it in buffers if using an HRP-based detection system [3] [5]. |
| Alkaline Phosphatase [1] [2] [6] | Incubation with 1-2 mM levamisole in the substrate solution. | During the substrate development step [1] [2]. | Levamisole does not inhibit the intestinal form of AP; for these tissues, use a different inhibitor or detection system [2]. |
Experimental Protocol for Blocking Endogenous Peroxidases
The following is a generalized protocol for quenching endogenous peroxidase activity in formalin-fixed, paraffin-embedded (FFPE) tissue sections [1] [4].
- Deparaffinization and Rehydration: After baking the slides, completely deparaffinize tissue sections by immersing them in fresh xylene (or a xylene-substitute). Rehydrate the tissues through a series of graded alcohols (100%, 95%, 70%) and finish with a rinse in distilled water [7] [4].
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER) using an appropriate buffer (e.g., citrate or EDTA) in a microwave oven or pressure cooker, as optimized for your target antigen [7] [8].
- Peroxidase Blocking: Prepare a peroxidase blocking solution by diluting 30% hydrogen peroxide in methanol or water to a final concentration of 0.3% to 3% [1] [4]. Submerge the slides in this solution and incubate for 10-15 minutes at room temperature.
- Washing: Rinse the slides thoroughly with a wash buffer, such as PBS or TBS [4].
- Proceed with Staining: Continue with the standard IHC protocol, including protein blocking, and incubation with primary and secondary antibodies [4].
The overall workflow for addressing this common issue is outlined below.
The Scientist's Toolkit: Key Reagent Solutions
The following table lists essential reagents used to manage endogenous enzyme activity in IHC.
| Reagent | Function | Example Use Case |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) [1] [4] [2] | Quenches endogenous peroxidase activity by acting as a substrate for the enzyme, depleting it before the detection step. | Blocking peroxidases in tissues with high red blood cell content (e.g., spleen). |
| Levamisole [1] [2] | An alkaline phosphatase inhibitor that blocks the activity of most endogenous AP isoenzymes. | Blocking AP in tissues like kidney, bone, or placenta. |
| Polymer-Based Detection System [2] [8] | A detection method that does not rely on the biotin-streptavidin system, avoiding interference from endogenous biotin. | An alternative to HRP/AP systems for tissues rich in both endogenous enzymes and biotin (e.g., liver). |
| Sodium Azide [1] | A potent inhibitor of horseradish peroxidase (HRP). Warning: Do not use in buffers if using an HRP-based detection system. | Sometimes included in peroxidase blocking solutions from commercial manufacturers [1]. |
Frequently Asked Questions (FAQs)
What should I do if the standard peroxidase blocking with H₂O₂ damages my tissue or alters the epitope?
If a 3% H₂O₂ solution is too harsh, try reducing the concentration to 0.3% (v/v). You can also experiment with the incubation time or temperature. Additionally, for some surface antigens, performing the peroxidase blocking step after the primary or secondary antibody incubation can help preserve epitope integrity [1].
Why is there still high background staining after I've performed an endogenous enzyme block?
High background can have multiple causes. If you have confirmed that endogenous enzymes are blocked, consider these other common issues:
- Endogenous Biotin: Tissues like liver, kidney, and mammary gland are rich in endogenous biotin, which will bind to streptavidin in ABC detection systems. Use an endogenous biotin blocking kit or switch to a polymer-based detection system [1] [4] [2].
- Antibody Concentration: The concentration of your primary or secondary antibody may be too high, leading to non-specific binding. Perform an antibody titration to find the optimal dilution [4] [5].
- Insufficient Protein Blocking: Ensure you are using an appropriate protein block (e.g., normal serum or BSA) before applying the primary antibody [4] [2] [6].
My tissue is known to have high endogenous alkaline phosphatase activity, and levamisole isn't working. What are my options?
Levamisole is ineffective against the intestinal isoform of alkaline phosphatase. In this case, you have two main options:
- Use a Different Detection System: Switch to an HRP-based detection system instead of AP-based detection, provided you effectively block endogenous peroxidases [2].
- Use a Different Inhibitor: For the intestinal isoform of AP, other inhibitors like tetramisole hydrochloride can be effective [2].
Are frozen sections or FFPE sections more prone to interference from endogenous enzymes?
Frozen sections generally retain higher endogenous enzyme activity because the tissue is not subjected to the same extensive chemical processing as FFPE tissues. The cross-linking fixatives used for FFPE samples can partially destroy endogenous enzyme activity, but significant levels often remain, making blocking a necessary step for both sample types [1] [2].
In immunohistochemistry (IHC), the specific binding of an antibody to its target antigen is visualized using reporter enzymes, most commonly Horseradish Peroxidase (HRP) and Alkaline Phosphatase (AP) [9]. However, many cells and tissues naturally contain endogenous forms of these enzymes or related enzymatic activities. When these endogenous enzymes react with the chromogenic substrates used for detection—such as 3,3'-Diaminobenzidine (DAB) for HRP or Nitro Blue Tetrazolium/5-Bromo-4-Chloro-3-Indolyl Phosphate (NBT/BCIP) for AP—they generate insoluble colored precipitates indistinguishable from the specific signal [1]. This activity causes high background staining, obscures true results, and can lead to false-positive interpretations [4]. Effectively identifying and blocking these key culprits is therefore a critical prerequisite for successful IHC experiments.
Troubleshooting Guide: Identifying and Resolving Issues
Q: How can I determine if my background staining is caused by endogenous enzymes?
A: Perform a simple no-primary-antibody control test.
- Procedure: Run your standard IHC protocol on a test tissue section but omit the primary antibody. Instead, incubate the sample only with the detection substrate (e.g., DAB or NBT/BCIP) for the same duration as your normal antibody incubation [4].
- Interpretation: If a colored precipitate forms, it confirms the presence of interfering endogenous enzyme activity that must be quenched before running your experimental samples [1] [4].
Q: My tissue is rich in red blood cells, leading to high background with HRP. What can I do?
A: Erythrocytes contain high levels of endogenous peroxidases, making them a common source of background.
- Solution: Quench endogenous peroxidase activity by treating the rehydrated tissue sections with a hydrogen peroxide solution [1] [10].
- Standard Protocol: Incubate slides in a solution of 3% hydrogen peroxide (H₂O₂) in methanol or pure water for 10-15 minutes at room temperature [1] [4]. After incubation, wash the slides thoroughly with buffer before proceeding with the rest of your staining protocol [1].
- Alternative: If 3% H₂O₂ damages your tissue or alters epitopes, try a lower concentration, such as 0.3% H₂O₂ [1]. Commercial peroxidase blocking solutions are also available [4].
Q: I am using an AP-based detection system and see nonspecific staining. How do I block it?
A: Inhibit endogenous alkaline phosphatase activity with levamisole.
- Solution: Add levamisole to your AP substrate solution at a final concentration of 1 mM. The incubation is typically performed between the primary and secondary antibody steps [1].
- Note: Levamisole effectively inhibits most endogenous AP isoenzymes but will not inhibit the intestinal calf AP commonly conjugated to antibodies [1]. Boiling tissues during Heat-Induced Epitope Retrieval (HIER) can also destroy some endogenous phosphatase activity [1].
Q: I have blocked endogenous enzymes, but my background is still high. What else could it be?
A: Consider interference from endogenous biotin, especially when using avidin-biotin complex (ABC) detection methods.
- Context: Tissues such as liver, kidney, adipose tissue, and mammary gland are naturally rich in endogenous biotin [1]. This biotin binds to the streptavidin in your detection complex, creating punctate, nonspecific staining.
- Solution: Use an endogenous biotin-blocking kit. The basic procedure involves sequentially incubating the sample with unlabeled streptavidin (to bind endogenous biotin) followed by free biotin (to block any remaining unoccupied binding sites on the streptavidin) [1].
- Pro Tip: Since Heat-Induced Epitope Retrieval (HIER) can increase the detectable levels of endogenous biotin, your negative controls should also undergo HIER to avoid false positives [1].
The table below summarizes the key reagents and methods used to quench endogenous enzyme activity.
Table: Reagents for Blocking Endogenous Enzyme Activity
| Endogenous Element | Recommended Blocking Reagent | Standard Protocol | Additional Notes |
|---|---|---|---|
| Peroxidase (HRP) | 0.3% - 3% Hydrogen Peroxide (H₂O₂) [1] [4] | Incubate rehydrated sections for 10-15 min at room temperature [1]. | Can be prepared in methanol or water. Commercial peroxidase suppressor solutions are available [1] [4]. |
| Alkaline Phosphatase (AP) | 1 mM Levamisole [1] | Add to the AP substrate solution (e.g., NBT/BCIP) during incubation [1]. | Does not inhibit the antibody-conjugated calf intestinal AP. Heat from HIER can also destroy activity [1]. |
| Biotin | Endogenous Biotin Blocking Kit [1] [4] | Sequential incubation with unlabeled streptavidin, then free biotin [1]. | Crucial for liver, kidney, and frozen sections. Use streptavidin (not avidin) to avoid lectin binding [1] [4]. |
Experimental Workflow for Managing Endogenous Activity
The following diagram outlines a logical workflow for diagnosing and addressing background staining in IHC.
Diagram: Troubleshooting workflow for endogenous enzyme interference.
The Scientist's Toolkit: Essential Reagents
Table: Key Reagents for Blocking and Detection
| Reagent | Function/Purpose |
|---|---|
| Hydrogen Peroxide (H₂O₂) | Quenches endogenous peroxidase activity by acting as a substrate for the enzyme, depleting it before the detection step [1] [10]. |
| Levamisole | An inhibitor used to block the activity of most endogenous alkaline phosphatase isoenzymes without affecting the commonly used reporter enzyme, calf intestinal AP [1]. |
| Endogenous Biotin Blocking Kit | Contains sequential reagents (e.g., unlabeled streptavidin and free biotin) to saturate endogenous biotin binding sites in tissues, preventing nonspecific detection [1] [4]. |
| Sodium Azide | Often included in peroxidase blocking solutions. Critical Note: Do not use sodium azide in buffers if you are using an HRP-based detection system, as it is an potent inhibitor of HRP activity [9] [5]. |
| Streptavidin/NeutrAvidin | Preferred over avidin for biotin-based detection. They are not glycosylated and have a more neutral charge, resulting in significantly lower nonspecific background binding to tissue lectins [1] [4] [11]. |
Frequently Asked Questions (FAQs)
Q: Can I skip the endogenous enzyme blocking step if I use a polymer-based detection system?
A: Blocking is still necessary for peroxidase and phosphatase activity. Polymer systems are non-biotinylated, so they elegantly circumvent problems with endogenous biotin [11]. However, the enzymes (HRP or AP) conjugated to the polymer will still be activated by the endogenous enzymes in your tissue. Therefore, quenching endogenous HRP and AP remains a critical step.
Q: At what point in the IHC protocol should I perform the blocking step?
A: The standard practice is to block endogenous enzymes after deparaffinization and rehydration of your sections but before the application of the primary antibody or any detection reagents [1] [12]. This ensures the enzymes are inactivated before they can react with the detection substrate.
Q: The hydrogen peroxide block seems to be damaging my tissue. What should I do?
A: High concentrations of H₂O₂ can be damaging. First, try reducing the concentration from 3% to 0.3% or 0.5% [1]. You can also experiment with shortening the incubation time. If problems persist, ensure you are using a fresh hydrogen peroxide solution, as it decomposes over time.
Q: Why is my negative control clean, but my test slide still has background after blocking?
A: If your no-primary-antibody control is clean, the background in your test slide is likely due to issues unrelated to endogenous enzymes. Common causes include the primary antibody concentration being too high, nonspecific antibody binding, or insufficient blocking of non-specific protein interactions with serum or BSA [4] [5]. Re-optimize your antibody dilution and ensure your protein blocking step is effective.
In immunohistochemistry (IHC), accurate interpretation depends on specific antibody-antigen binding visualized through chromogenic reactions. However, high-risk tissues like liver, kidney, spleen, and red blood cell (RBC)-rich areas contain abundant endogenous enzymes that catalyze these reactions independently of primary antibody binding, generating false-positive signals [4] [13]. This background staining compromises data integrity, particularly in drug development research where precise biomarker localization is essential. This guide provides targeted methodologies for identifying and mitigating this interference, ensuring experimental reliability in IHC workflows [14].
Tissue-Specific Challenges and Identification
Liver Tissue
Hepatocytes and Kupffer cells possess high constitutive levels of endogenous peroxidases [4]. The liver's inherent bioactivation functions correlate with robust enzymatic activity, often resulting in diffuse, brown background staining that can obscure specific signals, particularly in central lobular regions [13].
Kidney Tissue
The proximal tubules contain high peroxidase concentrations related to their metabolic functions [4]. Glomeruli also contribute to background, complicating interpretation of glomerular disease markers. The medulla's RBC content introduces additional peroxidase activity from hemoglobin [14].
Spleen Tissue
The spleen's extensive RBC pool within red pulp produces intense peroxidase-mediated background [4]. White pulp regions, rich in immune cells, may also exhibit endogenous alkaline phosphatase activity, creating dual interference challenges for multi-enzyme detection strategies [13].
Red Blood Cell-Rich Areas
Intact and degenerating RBCs contain hemoglobin pseudoperoxidase activity, which catalyzes the same chromogenic reaction as horseradish peroxidase (HRP)-based detection systems [4]. This is particularly problematic in hemorrhagic tissues, highly vascularized tumors, and splenic tissues [14].
Troubleshooting Guide: FAQs and Solutions
FAQ 1: How can I distinguish true positive staining from endogenous peroxidase activity in liver sections?
Solution: Implement a negative control without primary antibody alongside your test sample [4] [13].
| Step | Procedure | Purpose |
|---|---|---|
| 1 | Include a control section processed identically but without primary antibody incubation. | Differentiates specific signal from background enzymatic activity [13]. |
| 2 | Apply detection substrate to this control for the same duration as test samples. | Reveals staining pattern caused solely by endogenous enzymes [4]. |
| 3 | Compare staining patterns between control and test sections. | True specific staining will be absent in the control [13]. |
FAQ 2: What is the most effective method to quench endogenous peroxidases in kidney tissue?
Solution: Use hydrogen peroxide blocking applied before primary antibody incubation [4] [14].
| Method | Procedure | Considerations |
|---|---|---|
| 3% H₂O₂ in Methanol | Incubate sections in 3% H₂O₂ in methanol for 15 minutes at room temperature [4]. | Effective for peroxidase quenching; methanol may affect some antigens [4]. |
| Aqueous H₂O₂ | Use 3% H₂O₂ in distilled water for 10-15 minutes at room temperature [4]. | Preferred for methanol-sensitive antigens [14]. |
| Commercial Blockers | Apply ready-to-use peroxidase blocking solutions per manufacturer instructions [4]. | Optimized for consistency; convenient for standardized workflows [4]. |
FAQ 3: How do I handle tissues with both endogenous peroxidase and biotin activity?
Solution: Employ sequential blocking for multiple interference sources [4].
| Order | Blocking Target | Procedure |
|---|---|---|
| 1 | Endogenous Peroxidases | 3% H₂O₂ in methanol or commercial peroxidase suppressor, 10-15 minutes [4]. |
| 2 | Endogenous Biotin | Avidin/Biotin blocking kit: incubate with avidin solution (15-20 minutes), then with biotin solution (15-20 minutes) [4]. |
| 3 | Non-Specific Binding | Block with 2-10% normal serum from secondary antibody species [4]. |
Experimental Protocols for Validation
Protocol 1: Comprehensive Endogenous Enzyme Blocking
This validated protocol effectively addresses multiple interference sources in high-risk tissues [4] [14].
Materials Required:
- 3% Hydrogen peroxide in methanol or distilled water
- Avidin/Biotin Blocking Solution (commercial kit)
- Normal serum from secondary antibody host species
- Protein block (BSA or commercial protein block)
Procedure:
- Deparaffinization and Rehydration: Process FFPE sections through xylene and graded alcohols to water [14].
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER) using appropriate buffer (e.g., 10mM sodium citrate, pH 6.0) and method (microwave: 8-15 minutes; pressure cooker: 20 minutes) [4] [13].
- Peroxidase Blocking: Incubate with 3% H₂O₂ for 10-15 minutes at room temperature [4].
- Biotin Blocking: Apply avidin solution for 15-20 minutes, rinse, then apply biotin solution for 15-20 minutes [4].
- Protein Blocking: Incubate with protein block containing 2-10% normal serum for 30 minutes to reduce non-specific binding [4].
- Primary Antibody: Apply optimized primary antibody dilution and incubate overnight at 4°C in humid chamber [4].
- Detection: Proceed with appropriate detection system per standard protocol [4].
Protocol 2: Endogenous Alkaline Phosphatase Blocking
For tissues with endogenous alkaline phosphatase activity (spleen, kidney, bone) [4].
Materials:
- Levamisole solution (1-5mM in buffer)
- Alternatively: Commercial AP blocking solution
Procedure:
- Following antigen retrieval, prepare levamisole solution in Tris buffer (pH 7.4-8.2).
- Incubate sections for 30-60 minutes at room temperature.
- Proceed directly to primary antibody application without rinsing. Note: Levamisole inhibits intestinal-type AP but not tissue-nonspecific AP; test efficacy for your specific tissue type [4].
Visual Workflows
Diagram 1: Endogenous Interference Identification and Blocking Strategy
Diagram 2: Sequential Blocking Protocol for High-Risk Tissues
The Scientist's Toolkit: Essential Research Reagents
| Reagent | Function | Application Notes |
|---|---|---|
| 3% Hydrogen Peroxide | Quenches endogenous peroxidase activity [4] | Use in methanol for standard applications; aqueous for sensitive antigens [4] |
| Avidin/Biotin Blocking Solution | Blocks endogenous biotin [4] | Essential for liver, kidney, spleen; apply as sequential avidin then biotin incubation [4] |
| Levamisole | Inhibits endogenous alkaline phosphatase [4] | Effective against intestinal-type AP; use at 1-5mM concentration [4] |
| Normal Serum | Reduces non-specific antibody binding [4] | Use serum from secondary antibody species; 2-10% concentration [4] |
| Sodium Borohydride | Reduces aldehyde-induced autofluorescence [4] | Use ice-cold (1mg/mL) for 10-30 minutes post-fixation [4] |
| Heat-Induced Epitope Retrieval Buffers | Unmasks antigens cross-linked by formalin fixation [13] | Citrate (pH 6.0) or EDTA/TRIS (pH 9.0) buffers; microwave or pressure cooker method [4] [13] |
Advanced Troubleshooting: Additional Considerations
Tissue Fixation Impact
Over-fixation in formalin increases antigen masking, potentially requiring more aggressive retrieval that may exacerbate background [14]. Under-fixation preserves endogenous enzyme activity. Optimize fixation time for each tissue type: 24-48 hours typically recommended [13].
Detection System Alternatives
When persistent background remains problematic despite blocking:
- Polymer-based systems: Eliminate biotin-related background by avoiding avidin-biotin chemistry [4]
- Tyramide signal amplification: Allows extreme antibody dilution, reducing nonspecific binding [13]
- Fluorescent detection: With borohydride treatment to reduce autofluorescence [4]
Validation Controls
Always implement comprehensive controls [13]:
- Positive control tissue: Known positive expression pattern
- Negative control: No primary antibody
- Internal controls: Normal tissue elements with known expression
- Background assessment control: Substrate-only application
Effective management of endogenous enzymes in high-risk tissues requires systematic validation of blocking protocols and controls specific to each tissue type and experimental condition. The methodologies presented herein provide a foundation for reliable IHC data generation in critical drug development research.
FAQs: Understanding Endogenous Enzyme Interference
What are endogenous enzymes, and why do they cause background in IHC?
Endogenous enzymes are enzymes naturally present in the cells and tissues you are studying. In Immunohistochemistry (IHC), you often use enzyme-conjugated antibodies (like Horseradish Peroxidase, HRP, or Alkaline Phosphatase, AP) to generate a detectable signal. If the endogenous versions of these enzymes are not blocked, they will react with the same detection substrates (e.g., DAB for HRP), producing a colored precipitate even where your target antigen is not present. This leads to false-positive signals and high background, obscuring your specific signal [1].
Which tissues are particularly prone to high endogenous enzyme activity?
Certain tissues have naturally high levels of these interfering enzymes and require extra care:
- Endogenous Peroxidase: Abundant in liver, spleen, tonsil, lymph nodes, kidney, and red blood cells [15] [1].
- Endogenous Biotin: High levels are found in the liver, kidney, mammary gland, and adipose tissue [1].
- Endogenous Alkaline Phosphatase: Present in many tissues, particularly intestinal mucosa, placenta, and bone [16].
How can I quickly test if my background is due to endogenous enzymes?
A simple "deletion control" can diagnose the source of background:
- Follow your standard staining protocol but omit the primary antibody.
- If you still see considerable staining after adding only the detection substrate, the signal is non-specific and likely originates from endogenous enzymes or other tissue components [15] [4].
Troubleshooting Guides
Guide 1: Systematic Workflow for Diagnosing Enzyme-Related Background
Follow this decision tree to identify and resolve the cause of high background in your IHC experiments.
Diagram: A systematic workflow for diagnosing the source of high background in IHC experiments.
Guide 2: Blocking Specific Endogenous Enzymes
Once you have diagnosed the likely cause, use these targeted protocols to block the interfering activity.
Detailed Experimental Protocols
Protocol 1: Blocking Endogenous Peroxidase Activity Peroxidases are a common source of background, especially in hematopoietic tissues [1] [17].
- Principle: Hydrogen peroxide (H₂O₂) inhibits the heme group in peroxidases, preventing it from reacting with your chromogenic substrate [1].
- Reagents:
- Methanol or absolute ethanol
- 30% Hydrogen Peroxide (H₂O₂) stock solution
- Phosphate-Buffered Saline (PBS)
- Procedure:
- After deparaffinization, rehydration, and antigen retrieval (if performing), wash slides in PBS.
- Prepare a 3% H₂O₂ solution by mixing 1 part 30% H₂O₂ with 9 parts pure methanol or PBS [1] [4].
- Submerge the tissue sections in this solution and incubate for 10-15 minutes at room temperature [1] [17].
- Wash the slides thoroughly with PBS or distilled water (2-3 times) before proceeding with the rest of your staining protocol [17].
- Note: For frozen sections or tissues with very high peroxidase activity (e.g., blood smears), a milder 0.3% H₂O₂ in methanol for 20-30 minutes may be preferable to preserve morphology [17].
Protocol 2: Blocking Endogenous Alkaline Phosphatase Activity
- Principle: Levamisole is a competitive inhibitor of alkaline phosphatase (except for the intestinal isoenzyme) [16] [1].
- Reagents:
- Levamisole
- Tris-buffered Saline (TBS) or your antibody diluent buffer
- Procedure:
- Prepare a 1-2 mM solution of levamisole in your buffer [16] [1].
- Add this solution directly to your alkaline phosphatase substrate solution immediately before use [1].
- Proceed with the detection step as usual. Levamisole will inhibit endogenous AP activity without affecting the enzyme conjugated to your antibody.
Protocol 3: Blocking Endogenous Biotin
- Principle: Tissues rich in endogenous biotin will bind streptavidin from your detection system. This is blocked by sequentially applying unlabeled avidin/streptavidin (to bind endogenous biotin) and then free biotin (to block any remaining binding sites on the avidin/streptavidin) [1].
- Reagents:
- Avidin or Streptavidin solution (unconjugated)
- D-biotin
- PBS or TBS buffer
- Procedure (using a commercial kit is recommended for ease):
- After peroxidase blocking and washing, apply an unlabeled avidin or streptavidin solution to the tissue. Incubate for 10-15 minutes and wash [1].
- Apply a D-biotin solution to the tissue. Incubate for 10-15 minutes and wash thoroughly [1].
- Proceed with your primary and secondary (biotinylated) antibody incubation.
Research Reagent Solutions
The table below summarizes key reagents used to overcome endogenous enzyme interference.
| Reagent | Function / Target | Mechanism of Action | Key Considerations |
|---|---|---|---|
| Hydrogen Peroxide (H₂O₂) [16] [1] [17] | Endogenous Peroxidases | Inactivates the heme group in peroxidases. | Use 0.3%-3% in methanol or PBS. Can damage some epitopes; test first. |
| Levamisole [16] [1] | Endogenous Alkaline Phosphatase (AP) | Competitive inhibitor of most tissue AP isoenzymes. | Add directly to the AP substrate solution. Ineffective against intestinal AP. |
| Avidin/Biotin Blocking Kit [15] [1] [4] | Endogenous Biotin | Sequentially blocks biotin binding sites and endogenous biotin. | Essential for liver, kidney, and brain tissues. Use before primary antibody. |
| Sodium Borohydride [4] | Aldehyde-Induced Autofluorescence | Reduces free aldehyde groups from formaldehyde/PFA fixation. | Use ice-cold 1 mg/mL solution in PBS. Helps reduce green autofluorescence. |
| Sudan Black B [15] [4] | Lipofuscin Autofluorescence | Lipophilic dye that quenches autofluorescence from lipids/lipofuscin. | Apply before antibody staining. Can stain tissues blue if overused. |
| BLOXALL Blocking Solution [15] [17] | Peroxidases & Alkaline Phosphatase | Ready-to-use solution that blocks both peroxidase and AP activity. | Useful for multiplexing or when the source of interference is unknown. |
The Critical Link Between Fixation and Endogenous Enzyme Activity
Troubleshooting Guides
FAQ: How does fixation affect endogenous enzyme activity?
Formalin fixation, the most common method for tissue preservation, directly influences the activity of endogenous enzymes. While fixation stabilizes tissue architecture, it does not necessarily destroy the enzymatic activity of peroxidases or phosphatases. These preserved enzymes can later react with detection substrates (like DAB or NBT/BCIP), generating false-positive signals and high background staining that obscures specific antigen detection [1]. The key issue is that fixation preserves the very enzymes that detection systems rely on, creating potential interference [4].
FAQ: What are the consequences of inadequate fixation on background staining?
Inadequate or delayed fixation leads to several problems that increase non-specific background:
- Diffusion of Antigens: Cellular antigens can leach out or diffuse into surrounding tissues [18].
- Poor Tissue Integrity: Damaged tissue structures are more prone to nonspecific antibody binding [4].
- Variable Enzyme Preservation: Inconsistently fixed tissues show patchy, uneven background staining [18] [19]. Proper fixation must strike a balance between optimal morphology and preserved antigenicity. Under-fixed tissues show proteolytic degradation, while over-fixed tissues have excessive cross-links that mask target epitopes [20].
Troubleshooting High Background from Endogenous Enzymes
| Problem | Cause | Solution | Protocol Details |
|---|---|---|---|
| High Background Staining [4] | Endogenous peroxidases reacting with HRP-based detection systems [1] | Quench with hydrogen peroxide solution [10] [4] | Incubate slides in 3% H₂O₂ in methanol or water for 10-15 min at room temperature [1] [21] |
| Nonspecific Chromogen Precipitation [1] | Endogenous phosphatases reacting with AP substrates (e.g., NBT/BCIP) [1] | Inhibit with levamisole [1] | Add levamisole to substrate solution at 1 mM final concentration [1] |
| False-Positive Signal in Liver/Kidney [1] [4] | Endogenous biotin in tissues [1] | Block with avidin/biotin blocking kit [4] | Sequentially incubate with avidin, then biotin solutions; use polymer-based detection to avoid issue [1] [21] |
Experimental Protocol: Validating Endogenous Peroxidase Activity
To test whether endogenous peroxidases are causing background, follow this control experiment before applying your primary antibody [1] [4]:
- After completing deparaffinization, rehydration, and antigen retrieval steps, take one control slide.
- Apply the peroxidase substrate (e.g., DAB) to the tissue section for the same duration used in your full IHC protocol.
- Observe the slide under a microscope.
- Result Interpretation: Any colored precipitate that forms indicates the presence of active endogenous peroxidases. If this occurs, you must include a peroxidase quenching step in your protocol [1].
Research Reagent Solutions
| Reagent | Function | Example Formulation |
|---|---|---|
| Peroxidase Blocking Solution [1] [10] | Quenches endogenous peroxidase activity to prevent false-positive signals with HRP-based detection. | 3% H₂O₂ in methanol or aqueous buffer; incubate for 10-15 min at room temperature [10]. |
| Alkaline Phosphatase Inhibitor [1] | Suppresses endogenous phosphatase activity when using AP-conjugated antibodies. | 1 mM levamisole in substrate buffer; add to NBT/BCIP chromogen solution [1]. |
| Avidin/Biotin Blocking Solution [1] [4] | Blocks endogenous biotin in tissues (e.g., liver, kidney) to prevent binding to avidin-biotin detection systems. | Commercial kits; sequential application of avidin then biotin solutions [1]. |
| Aldehyde Quencher [20] [22] | Neutralizes free aldehyde groups after glutaraldehyde fixation to prevent covalent antibody binding. | 0.1 M glycine, 50 mM NH₄Cl, or 1 mg/mL sodium borohydride in PBS; incubate for 10-30 min [20] [22]. |
Experimental Workflow for Managing Endogenous Activity
Advanced Troubleshooting: Fixation-Related Artifacts
FAQ: Why does background staining persist even after peroxidase blocking?
Persistent background after standard blocking protocols often indicates fixation-related issues:
- Incomplete Penetration: With thick tissue specimens, fixative penetration may be incomplete, creating zones of variable enzyme preservation [18] [22].
- Prolonged Fixation: Over-fixation (beyond 48 hours) can create excessive cross-linking that makes some epitopes inaccessible while preserving enzyme activity, requiring optimized antigen retrieval [18].
- Fixative pH Imbalance: Non-neutral buffered formalin can alter tissue charge characteristics, increasing non-specific ionic interactions with antibodies [22].
Solution: For tissues rich in endogenous peroxidases (e.g., hematopoietic tissues), combine multiple approaches:
- Increase H₂O₂ concentration to 3% and extend incubation to 20-30 minutes [1].
- Add a biotin block step, even with polymer-based detection systems [21].
- Use high-salt antibody diluents (0.15-0.6 M NaCl) to reduce non-specific ionic interactions [4].
Proven Blocking Protocols: Step-by-Step Methods for Clean IHC Staining
In immunohistochemistry (IHC), the accurate visualization of target antigens is paramount. However, endogenous enzymes present in tissues can catalyze the same chromogenic reactions used for detection, generating false-positive signals and obscuring specific staining. Addressing this endogenous enzyme activity is a critical foundation for reliable IHC results. This guide provides a detailed comparison of peroxidase and alkaline phosphatase inhibition strategies, offering researchers targeted solutions for optimizing their experiments.
# Why Blocking Endogenous Enzymes is Crucial
Endogenous enzymes are naturally present in many tissues and cell types. When using horseradish peroxidase (HRP) or alkaline phosphatase (AP)-based detection systems, these native enzymes react with the substrate, producing nonspecific background staining that compromises data interpretation [1] [23]. Effective blocking inactivates these endogenous activities, ensuring that the final signal originates solely from the antibody-target interaction.
# Comparative Analysis: Peroxidase vs. Alkaline Phosphatase Blocking
The choice of blocking strategy depends on your selected detection system and the tissue type. The table below summarizes the core considerations for each.
| Characteristic | Endogenous Peroxidase Blocking | Endogenous Alkaline Phosphatase Blocking |
|---|---|---|
| Primary Reagent | Hydrogen Peroxide (H₂O₂) [1] [2] | Levamisole [1] [23] [2] |
| Typical Working Concentration | 0.3% - 3% (v/v) [1] [23] | 1 mM - 10 mM (often added to substrate) [1] [23] |
| Standard Incubation | 10-15 minutes at room temperature [1] [4] | Incubated with the substrate solution [1] [24] |
| Tissues with High Endogenous Activity | Kidney, liver, tissues rich in red blood cells [1] [24] [2] | Kidney, intestine, bone, lymphoid tissue, placenta; higher in frozen sections [1] [2] |
| Mechanism of Action | Inactivates the heme group in peroxidases by oxidizing it to a non-reactive state [1] | Competitively inhibits the enzyme's activity [1] |
| Commercially Available Solutions | Peroxidase Suppressor, Hydrogen Peroxide Block [1] [4] | Pre-mixed NBT/BCIP substrate with levamisole [1] |
| Alternative Strategy | Switch to an AP-based detection system [1] | Use heat during antigen retrieval (HIER) to destroy activity [1] |
# Experimental Protocols for Effective Blocking
Protocol for Blocking Endogenous Peroxidase Activity
This protocol is designed for formalin-fixed, paraffin-embedded (FFPE) tissue sections after deparaffinization and rehydration.
- Prepare Blocking Solution: Use 3% hydrogen peroxide in methanol or pure water. For more sensitive tissues, a lower concentration of 0.3% can be effective [1].
- Apply Solution: Submerge or cover the tissue sections completely with the prepared hydrogen peroxide solution.
- Incubate: Incubate for 10 to 15 minutes at ambient temperature [1] [4].
- Wash: Rinse the slides thoroughly with buffer, such as phosphate-buffered saline (PBS), twice before proceeding with the rest of the staining protocol [1].
Troubleshooting Tip: If you are staining labile surface antigens (e.g., CD4, CD8), performing the peroxidase blocking step after the primary or secondary antibody incubation may be necessary to prevent epitope damage [1].
Protocol for Blocking Endogenous Alkaline Phosphatase Activity
Blocking endogenous AP is typically performed after the primary antibody incubation step and concurrently with the AP substrate application.
- Prepare Substrate with Inhibitor: Add levamisole hydrochloride to your AP substrate (e.g., BCIP/NBT) to achieve a final concentration of 1 mM to 10 mM [1] [23] [2].
- Apply and Incubate: Apply the substrate-levamisole mixture to the tissue sections and incubate for the required development time. Levamisole inhibits most endogenous AP isoenzymes but does not affect intestinal or bacterial AP commonly used in detection systems [1].
# Visual Guide to Blocking Strategy Selection
The following diagram outlines a logical workflow for diagnosing background issues and selecting the appropriate blocking strategy.
Decision Workflow for Enzyme Blocking
# The Scientist's Toolkit: Essential Reagents for Enzyme Blocking
The table below lists key reagents used for inhibiting endogenous enzyme activity in IHC.
| Reagent | Function | Key Consideration |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) | Oxidizes and inactivates the heme group in endogenous peroxidases [1]. | Aqueous solutions may damage tissue architecture in peroxidase-rich tissues; methanolic solutions are often preferred [24]. |
| Levamisole | Competitive inhibitor of endogenous alkaline phosphatase (except the intestinal isoenzyme) [1] [2]. | Typically added directly to the AP substrate solution just before use [1] [24]. |
| BLOXALL Solution | Ready-to-use commercial solution that blocks both endogenous peroxidase and alkaline phosphatase activity [24]. | A versatile option for labs using multiple detection systems or when the source of background is unclear. |
| Sodium Azide | A potent inhibitor of HRP activity; can be found in some pre-made peroxidase blockers [1]. | Do not use in buffers if you plan to use an HRP-based detection system later in the protocol, as it will inactivate the reporter enzyme [4]. |
# Frequently Asked Questions (FAQs)
Q1: How can I test if my tissue has problematic levels of endogenous peroxidase or alkaline phosphatase activity? A1: Incubate a representative test tissue section with the detection substrate (e.g., DAB for peroxidase, BCIP/NBT for alkaline phosphatase) alone, for the same duration as your standard protocol. The formation of a colored precipitate indicates significant endogenous activity that requires blocking [4] [2].
Q2: I've performed peroxidase blocking, but my positive control tissue (e.g., kidney) still shows high background. What should I do? A2: Tissues very rich in peroxidases, like kidney and liver, can be challenging. First, ensure you are using a methanolic solution of H₂O₂, which is less damaging and sometimes more effective. If background persists, consider switching your detection system to one based on alkaline phosphatase, as endogenous AP is less prevalent in these tissues [1] [24].
Q3: Are there any risks associated with the hydrogen peroxide blocking step? A3: Yes. High concentrations of H₂O₂ can damage tissue morphology and mask certain labile epitopes. If you experience this, try reducing the H₂O₂ concentration to 0.3% or shortening the incubation time. For sensitive epitopes, perform the blocking step after the primary antibody incubation [1].
Q4: My detection system is biotin-based. Do I only need to worry about endogenous enzymes? A4: No. Tissues such as liver, kidney, adipose, and mammary gland contain endogenous biotin, which will bind to avidin/streptavidin reagents and cause high background. When using biotin-based detection, you must employ a sequential blocking protocol for endogenous biotin, typically involving an avidin/streptavidin block followed by a free biotin block, prior to the primary antibody incubation [1] [24] [2].
Within the framework of advanced immunohistochemistry (IHC) research, addressing endogenous enzyme activity is a foundational step for ensuring assay specificity. Immunohistochemistry is a powerful technique that combines immunology, histology, and biochemistry to detect specific antigens within tissue sections, providing invaluable spatial context that methods like Western blot or ELISA cannot offer [20] [25]. However, the reliability of this data is heavily dependent on effective blocking of background interference.
A primary source of such interference is endogenous peroxidase activity, which is naturally present in many tissues, particularly red blood cells [1]. When using horseradish peroxidase (HRP)-based detection systems, this endogenous activity will react with chromogenic substrates (e.g., DAB), generating widespread nonspecific staining that obscures the true signal and compromises experimental integrity [4] [1]. Therefore, the implementation of a robust, gold standard protocol for quenching endogenous peroxidases using hydrogen peroxide (H₂O₂) is not merely a preliminary step but a critical determinant of IHC success.
Core Protocol: The Gold Standard H₂O₂ Quenching Method
This section details the established, most reliable protocol for effectively inhibiting endogenous peroxidase activity in formalin-fixed, paraffin-embedded (FFPE) tissue sections.
Reagents and Solution Preparation
- Hydrogen Peroxide Stock Solution: 30% (v/v) laboratory grade.
- Working Quenching Solution: 3% (v/v) Hydrogen Peroxide. Prepare by adding one part of 30% H₂O₂ to nine parts of pure methanol or deionized water [4] [1]. Note: The choice of diluent (methanol or water) can be tailored based on the sensitivity of your target antigen, as methanol can be harsher on some epitopes.
Step-by-Step Procedure
- Deparaffinization and Rehydration: Following standard protocol, deparaffinize FFPE tissue sections in xylene and rehydrate through a graded series of ethanol (100%, 95%, 70%) to water [26]. Inadequate deparaffinization can cause spotty, uneven background [26].
- Peroxidase Quenching: Submerge the slides in the freshly prepared 3% H₂O₂ solution. Incubate for 10-15 minutes at room temperature [4] [1] [26].
- Washing: Rinse the slides thoroughly by washing three times with phosphate-buffered saline (PBS) or distilled water for 5 minutes each [4] [26].
- Protocol Continuation: Proceed immediately with subsequent steps in your IHC workflow, such as antigen retrieval and antibody incubation.
Workflow and Decision Path
The following diagram illustrates the quenching protocol's place in the overall IHC process and key decision points:
Troubleshooting Guide: FAQs on H₂O₂ Blocking
Q1: I am still observing high background staining after using the 3% H₂O₂ block. What could be the cause?
High background post-quenching can result from several factors:
- Insufficient Quenching: Tissues with very high endogenous peroxidase content (e.g., liver, kidney, spleen) may require a longer incubation time (up to 30 minutes) or a slight increase in H₂O₂ concentration [1]. However, high concentrations can damage epitopes.
- Alternative Background Sources: The background may not be from peroxidases. Consider other common sources and their solutions:
- Endogenous Biotin: Tissues like liver, kidney, and adipose are rich in biotin. Use a polymer-based detection system (non-biotin) or perform an endogenous biotin block after the peroxidase quenching step [1] [26].
- Non-specific Antibody Binding: Optimize primary antibody concentration and use appropriate blocking serum (e.g., 5% normal serum from the host species of your secondary antibody) [4].
- Inadequate Washing: Ensure thorough washing after all incubation steps (e.g., 3 x 5 min with TBST) [26].
Q2: The target signal has become weak after H₂O₂ treatment. Is H₂O₂ damaging my antigen?
Yes, this is a known possibility. The oxidizing nature of H₂O₂ can damage certain sensitive epitopes, leading to reduced or abolished signal [4] [1].
- Solution: Titrate the H₂O₂ concentration downward. A concentration of 0.3% H₂O₂ is often effective for quenching with minimal antigen damage and is recommended if 3% is too harsh [1]. Always perform a pilot experiment to balance effective blocking with signal preservation.
Q3: How can I confirm that endogenous peroxidase activity is truly the source of my background?
Perform a simple control experiment [1]:
- Prepare a test tissue section (known to have high peroxidase activity, like liver).
- Process it through the IHC protocol but omit the primary antibody.
- Continue with the rest of the protocol, including incubation with your HRP-conjugated secondary and the chromogenic substrate (e.g., DAB). The appearance of a colored precipitate indicates residual endogenous peroxidase activity that needs to be quenched. A clean slide confirms the blocking was effective.
Q4: Are there alternatives to H₂O₂ for blocking endogenous peroxidases?
If endogenous peroxidase activity cannot be sufficiently quenched without antigen damage, the most effective alternative is to switch your detection system. Use an alkaline phosphatase (AP)-based detection system and corresponding chromogenic substrates (e.g., NBT/BCIP) instead of an HRP-based one [1]. Note that endogenous phosphatases must then be blocked with levamisole.
Quantitative Data and Reagent Selection
Comparison of Peroxidase Quenching Methods
The table below summarizes the key parameters for different approaches to handling endogenous peroxidase interference.
| Method | Typical Concentration | Incubation Time | Key Considerations |
|---|---|---|---|
| H₂O₂ in Methanol [4] [1] | 3% | 10-15 min, RT | Pros: Highly effective. Cons: Methanol can be harsh on some epitopes. |
| H₂O₂ in Aqueous Buffer [1] [26] | 0.3% - 3% | 10-15 min, RT | Pros: Gentler on antigens. Cons: May be less effective for high-peroxidase tissues. |
| Commercial Peroxidase Suppressors [4] [1] | As per mfr. (often ~0.3%) | 10-15 min, RT | Pros: Pre-optimized, reliable. Cons: Higher cost than in-house preps. |
| Detection System Switch [1] | N/A | N/A | Use Alkaline Phosphatase (AP) system if HRP quenching fails. Block endogenous AP with levamisole. |
The Scientist's Toolkit: Key Research Reagents
This table lists essential reagents for implementing this protocol and their critical functions.
| Reagent / Tool | Function / Explanation |
|---|---|
| Hydrogen Peroxide (30% stock) | Active ingredient for quenching; decomposes to water and oxygen, inactivating endogenous heme groups in peroxidases [1]. |
| Methanol or Deionized Water | Diluent for preparing working H₂O₂ solution; methanol provides a slightly harsher fixation which can help reduce background [4]. |
| Positive Control Tissue | Tissue known to express your target antigen and contain peroxidases (e.g., tonsil, liver); essential for protocol validation [26] [25]. |
| Polymer-based Detection Reagents | Non-biotin detection systems that avoid background from endogenous biotin, a common confounding factor after peroxidase block [26]. |
| Sodium Azide | A potent inhibitor of HRP; Warning: Never include in buffers when using HRP-based detection, as it will inactivate the enzyme label [4]. |
The gold standard protocol for blocking endogenous peroxidases with hydrogen peroxide is a cornerstone technique for achieving publication-quality IHC data. Its successful implementation hinges on understanding the balance between complete quenching and antigen preservation. As IHC continues to evolve with multiplexed techniques and digital/AI-driven analysis [25], the principles of rigorous validation and controlled background remain paramount. Always include the appropriate positive and negative controls to verify that your staining is specific, and do not hesitate to titrate conditions to optimize the protocol for your specific tissue and target antigen.
Effective Alkaline Phosphatase Blocking with Levamisole
In immunohistochemistry (IHC), chromogenic detection often relies on enzymes such as alkaline phosphatase (AP) to visualize target antigens. However, many tissues contain endogenous alkaline phosphatase, which can react with the substrate and cause high background staining, obscuring specific signals and leading to false-positive results [27] [2]. Endogenous AP is found in various tissues, including the kidney, intestine, bone, lymphoid tissue, and placenta, with its activity being notably higher in frozen tissues [27] [2]. Effectively blocking this endogenous activity is, therefore, a critical step for ensuring the accuracy and interpretability of IHC experiments. This guide focuses on the use of levamisole, a specific inhibitor, to suppress endogenous AP activity, and provides troubleshooting advice for researchers.
Mechanism of Action: How Levamisole Blocks Endogenous AP
Levamisole acts as a reversible, competitive inhibitor of alkaline phosphatase [28]. Its key characteristic is its selective inhibition profile. Mammalian tissues express different isoenzymes of alkaline phosphatase. Levamisole effectively inhibits the widely distributed non-intestinal (tissue-specific) forms of AP but does not inhibit the intestinal isoenzyme [29] [30]. This selectivity is strategically exploited in IHC because the enzyme conjugates used in detection systems (e.g., those conjugated to secondary antibodies) are typically derived from calf intestinal alkaline phosphatase [29]. Consequently, when levamisole is added to the substrate solution, it suppresses background staining from endogenous tissue AP without affecting the activity of the detector AP conjugate [28] [29].
The following diagram illustrates the mechanism and workflow for using levamisole in an IHC detection system.
Standard Experimental Protocol for Using Levamisole
Preparation and Application
Levamisole is typically supplied as a concentrated solution (e.g., 125 mM) [28]. The standard method of use is to add it directly to the alkaline phosphatase chromogenic substrate solution immediately before application to the tissue section.
A common and convenient protocol is to add one drop of levamisole concentrate to every 5 mL of substrate solution [28]. The solution is mixed, and then applied to the tissue section for the standard development time. Incubation with the substrate-levamisole mixture is usually performed at room temperature.
Quantitative Usage Guidelines
The table below summarizes the key quantitative parameters for using levamisole effectively.
Table 1: Levamisole Usage Specifications
| Parameter | Typical Specification | Notes & References |
|---|---|---|
| Stock Concentration | 125 mM | Supplied as a 100X concentrate [28]. |
| Final Working Concentration | 1 - 2 mM | This achieves a 1 mM final concentration [31]; other sources use 1-2 mM [1]. |
| Dilution Factor | 1:100 (or 1X) | The 100X concentrate is diluted to its final working concentration in the substrate solution [28]. |
| Volume Guidance | 1 drop per 5 mL substrate | A convenient dispensing method for the concentrated solution [28]. |
| Storage Conditions | 2-8°C | Store the concentrated solution in a refrigerator [28]. |
Troubleshooting Guide: FAQs on Levamisole Use
Q1: I am still observing high background staining even after using levamisole. What could be the cause?
- Confirm the Presence of Endogenous AP: First, verify that the background is due to alkaline phosphatase and not another source, such as endogenous peroxidase or non-specific antibody binding. Perform a control experiment by incubating the tissue with the BCIP/NBT substrate alone. The development of a blue color indicates endogenous AP activity [27] [2].
- Check Levamisole Effectiveness: Ensure the levamisole solution is not expired and has been stored correctly at 2-8°C [28]. Confirm that the final working concentration in the substrate is correct (1-2 mM).
- Consider the Tissue Type: Levamisole is ineffective against the intestinal isoform of alkaline phosphatase [29] [30]. If you are working with intestinal tissue or a tissue that contains this specific isoenzyme, an alternative blocking method, such as a brief incubation with 1% acetic acid, may be necessary [27] [30].
- Evaluate Other Causes: High background can also stem from other issues, such as insufficient protein blocking, primary antibody concentration being too high, or non-specific binding of the secondary antibody. Refer to the general troubleshooting table in Section 4.1 [4] [31].
Q2: Can levamisole be used in all alkaline phosphatase-based detection systems?
Yes, levamisole is compatible with most commercial AP-based detection systems. This is because these kits commonly use calf intestinal alkaline phosphatase as the reporter enzyme, which is not inhibited by levamisole [28] [29]. The inhibitor specifically targets the non-intestinal, tissue-derived isoenzymes. It is considered a standard and safe practice to include levamisole in the substrate step for any AP-based IHC detection to preemptively quench endogenous activity.
Q3: At which precise step in the IHC protocol should levamisole be introduced?
Levamisole is added during the final detection step. Specifically, it is mixed into the chromogenic substrate solution just before that solution is applied to the tissue sections [28]. The incubation occurs simultaneously with the substrate development. There is no need for a separate blocking step or wash prior to this.
Q4: Does heat-induced epitope retrieval (HIER) affect endogenous alkaline phosphatase activity?
Yes, a significant benefit is that the standard heat-induced epitope retrieval (HIER) procedure used for FFPE tissues often destroys endogenous phosphatase activity [1]. This means that for many FFPE samples, extensive blocking with levamisole may be less critical. However, it remains a best practice to include it, as activity can persist in some tissues or under certain retrieval conditions. For frozen sections, which are not subjected to the same harsh processing, endogenous AP activity is much higher and levamisole blocking is essential [27] [2].
General IHC Background Staining Troubleshooting
While this guide focuses on alkaline phosphatase, background staining can have multiple causes. The table below provides a broader troubleshooting framework.
Table 2: Troubleshooting High Background Staining in IHC
| Possible Cause | Recommended Solution | References |
|---|---|---|
| Endogenous Alkaline Phosphatase | Add levamisole (1-2 mM final) to the substrate solution. | [4] [31] [2] |
| Endogenous Peroxidase | Quench with 3% H2O2 in methanol or water for 10-15 minutes. | [4] [27] [1] |
| Endogenous Biotin | Use an avidin/biotin blocking kit or switch to a polymer-based detection system. | [4] [27] [1] |
| Primary Antibody Concentration Too High | Titrate the antibody to find the optimal, lower concentration. | [4] [31] |
| Non-specific Secondary Antibody Binding | Increase serum blocking concentration (up to 10%); use a secondary antibody that is pre-adsorbed against the host species. | [4] |
| Insufficient Protein Blocking | Increase blocking time or change the blocking reagent (e.g., use 1-5% BSA or 10% normal serum). | [27] [31] |
The Scientist's Toolkit: Key Reagents for AP Blocking and Detection
A successful IHC experiment requires more than just an effective AP blocker. The following table lists essential reagents and their functions related to AP-based detection and background reduction.
Table 3: Essential Research Reagents for AP-based IHC
| Reagent / Solution | Function / Purpose | Key Considerations |
|---|---|---|
| Levamisole Hydrochloride | Competitive inhibitor of tissue-nonspecific AP. | Ineffective against intestinal AP; add directly to substrate. [29] [30] |
| Calf Intestinal Alkaline Phosphatase | Reporter enzyme in detection conjugates. | Resistant to levamisole inhibition, enabling specific detection. [28] [29] |
| BCIP/NBT Chromogen Substrate | Enzymatic substrate for AP; produces an insoluble blue/purple precipitate. | Used to visualize the target antigen and to test for endogenous AP activity. [27] [2] |
| Normal Serum | Protein blocking agent to reduce non-specific antibody binding. | Should ideally be from the same species as the secondary antibody. [27] [2] |
| Acetic Acid | Alternative blocking agent for intestinal alkaline phosphatase. | Used when levamisole is ineffective (e.g., 1% acetic acid). [27] [30] |
| Bovine Serum Albumin (BSA) | Common protein component of blocking and antibody dilution buffers. | Helps reduce non-specific background by occupying charged sites. [27] [2] |
The management of endogenous enzyme activity is a cornerstone of robust and reliable IHC. Levamisole provides a highly specific and effective solution for the problem of endogenous alkaline phosphatase. By integrating it correctly into the detection protocol—adding it directly to the substrate solution at a final concentration of 1-2 mM—researchers can achieve a significant reduction in background staining. Understanding its mechanism, its limitations regarding the intestinal isoenzyme, and its place within a comprehensive troubleshooting workflow empowers scientists and drug development professionals to produce clean, interpretable, and high-quality data in their research.
In immunohistochemistry (IHC), the sequence of blocking steps is not a mere formality but a critical determinant of experimental success. Endogenous enzyme activity and other tissue constituents can generate significant background noise, obscuring specific signals and leading to false-positive interpretations. This guide addresses the pivotal question of sequencing in blocking protocols, providing clear methodologies to optimize signal-to-noise ratio for accurate and reproducible results.
FAQ: Sequencing of Blocking Steps
Q: When should I block endogenous peroxidases, and why is the sequence important? A: Block endogenous peroxidases BEFORE incubating with the primary antibody. [1] [32]
This sequence is crucial because the hydrogen peroxide solution used to quench peroxidases can be damaging. Performing this step early, often immediately after deparaffinization and rehydration, prevents potential damage to your primary antibody and the target antigens themselves [1] [32]. If you are staining particularly sensitive surface antigens (e.g., CD4, CD8), some protocols adjust this timing, but for the vast majority of targets, blocking first is the standard.
Q: What about blocking endogenous Alkaline Phosphatase (AP)? A: The inhibitor for endogenous AP, levamisole, is typically added directly to the substrate solution used for detection, which occurs AFTER the primary and secondary antibody incubations [1] [2] [33]. Unlike peroxidases, endogenous AP is effectively inhibited by levamisole in real-time during the color development reaction.
Q: Does the sequence for blocking endogenous biotin differ? A: Yes, absolutely. Blocking endogenous biotin is a two-step process that should be performed BEFORE the primary antibody is applied [1] [2].
The standard protocol is:
- Incubate the sample with an excess of unlabeled avidin or streptavidin to bind all endogenous biotin.
- Incubate with an excess of free biotin to block any remaining binding sites on the avidin/streptavidin molecules [1] [2].
This sequential blocking ensures your detection system later only sees the biotin on your secondary antibody.
Q: What is the consequence of incorrect sequencing? A: Incorrect sequencing can lead to two primary issues:
- High Background: Failure to block enzymes like peroxidase before antibody incubation results in widespread chromogen deposition, masking your specific signal [1] [4].
- Destroyed Antigens: Performing harsh blocking steps after antibody incubation can damage the already-bound antibodies or the epitopes themselves, leading to weak or false-negative staining [1].
Troubleshooting Guide: Blocking Sequence and Background Staining
| Problem | Possible Cause Related to Sequence | Recommended Solution |
|---|---|---|
| High background throughout the entire tissue section | Endogenous peroxidase activity was not blocked before primary antibody incubation [1] [4]. | Quench with 3% H₂O₂ in methanol or water for 10-15 minutes after tissue rehydration but before any antibody steps [1] [32]. |
| Endogenous biotin was not blocked prior to using a biotin-streptavidin detection system [1] [4]. | Use a commercial avidin/biotin blocking kit before the primary antibody. For biotin-rich tissues (liver, kidney), consider switching to a polymer-based detection system [4] [32]. | |
| Specific false-positive staining in tissues known to be rich in endogenous enzymes or biotin | Blocking step was incomplete or omitted due to incorrect sequence [1]. | For liver, kidney, intestine: ensure complete peroxidase and biotin blocking before primary antibody. For alkaline phosphatase, add levamisole to the substrate solution [2] [33]. |
| Weak or absent target-specific signal | Harsh peroxidase blocking with H₂O₂ was performed after the primary antibody, damaging the antibody-antigen complex [1]. | Always perform peroxidase quenching before the primary antibody incubation step. |
| Unexpected staining in negative controls (no primary antibody) | The secondary antibody is binding non-specifically, indicating insufficient protein blocking [4] [33]. | Ensure protein blocking with serum or BSA is performed immediately before the primary antibody step. Use a serum from the same species as the secondary antibody [23] [2]. |
Experimental Protocols for Determining Optimal Blocking
Protocol 1: Validating the Need for Endogenous Peroxidase Blocking
Purpose: To empirically confirm whether your tissue contains interfering peroxidase activity that requires blocking prior to primary antibody incubation.
Materials:
- Prepared tissue sections (deparaffinized and rehydrated)
- Phosphate-Buffered Saline (PBS)
- 3,3'-Diaminobenzidine (DAB) Substrate [2]
- Hydrogen Peroxide (3%)
Methodology:
- Take one control tissue section and proceed with your standard IHC protocol but OMIT the primary and secondary antibodies.
- After the rehydration step, incubate the section directly with the prepared DAB substrate solution for the same duration you plan to use in your full experiment.
- Observe the tissue under a microscope.
- Result Interpretation: The development of a brown precipitate indicates the presence of endogenous peroxidase activity [2]. This confirms that a peroxidase blocking step (using 3% H₂O₂ for 10-15 minutes) is necessary and must be performed before the primary antibody in your main protocol.
Protocol 2: A Standard IHC Workflow with Correct Blocking Sequence
The following diagram illustrates the critical path and correct sequence for key blocking steps in a standard IHC protocol.
The Scientist's Toolkit: Key Reagents for Blocking
| Reagent | Function in Blocking | Key Consideration |
|---|---|---|
| Hydrogen Peroxide (3%) | Quenches endogenous peroxidase activity by converting the enzyme to an inactive form [1] [32]. | Use before primary antibody. Can be prepared in methanol or aqueous buffer; methanol helps preserve tissue morphology in peroxidase-rich tissues [33]. |
| Levamisole Hydrochloride | Inhibits endogenous alkaline phosphatase (AP) activity [1] [2]. | Typically added to the AP substrate solution just before the detection step, not during initial blocking [2] [33]. |
| Avidin/Biotin Blocking Kit | Sequentially blocks endogenous biotin and its binding sites to prevent detection by streptavidin-based systems [1] [4]. | A two-step process (avidin first, then biotin) performed before the primary antibody. Critical for tissues like liver, kidney, and brain [1] [2]. |
| Normal Serum | Reduces non-specific background by blocking charged sites and Fc receptors on the tissue [23] [2]. | Use serum from the species in which the secondary antibody was raised. Apply after enzyme blocks but immediately before the primary antibody. |
| Bovine Serum Albumin (BSA) | A protein-based blocking agent that occupies non-specific hydrophobic binding interactions [23] [33]. | A versatile, animal-free alternative. Do not use non-fat dry milk if using a biotin-streptavidin system, as it contains biotin [23] [4]. |
| Polymer-Based Detection System | A detection method that does not rely on the avidin-biotin complex, thus avoiding issues with endogenous biotin [4] [32]. | An excellent alternative to biotin-based systems, eliminating the need for biotin blocking steps and often providing superior sensitivity [32]. |
Within the broader context of managing endogenous enzyme activity in immunohistochemistry (IHC) research, addressing endogenous biotin interference represents a critical technical challenge. The avidin-biotin complex (ABC) method is a powerful amplification system used to enhance detection sensitivity in IHC. However, this system is compromised by the presence of endogenous biotin, a vitamin and essential coenzyme naturally present in many tissues. Tissues rich in endogenous biotin—including liver, kidney, mammary gland, adipose tissue, and heart—are particularly prone to high background staining, which can generate false-positive results and obscure specific signals [1] [34]. This background occurs because the streptavidin or avidin conjugates used for detection bind indiscriminately to both the biotinylated antibodies and the endogenous biotin present in tissue carboxylase enzymes [35]. Effective blocking is therefore not optional but essential for producing reliable, interpretable data in biotin-streptavidin based IHC systems.
FAQs and Troubleshooting Guides
How do I identify high background caused by endogenous biotin?
Answer: High background from endogenous biotin typically appears as a diffuse, nonspecific stain across the tissue section, which can be distinguished from the specific, localized signal of your target antigen [1]. This background is often most pronounced in frozen sections and can be intensified by heat-induced epitope retrieval (HIER) methods [1]. To confirm that endogenous biotin is the source of your background problem, run a control where you omit the primary antibody but include all subsequent steps, including the biotinylated secondary antibody and the streptavidin-enzyme conjugate. If this control shows significant staining, endogenous biotin or another component of the detection system is likely causing nonspecific background [4] [36].
What are the most effective methods for blocking endogenous biotin?
Answer: Researchers have two primary strategies for blocking endogenous biotin, each with its own advantages.
1. Sequential Avidin/Biotin Blocking: This is the most common and widely recommended method.
- Procedure: The tissue section is first incubated with an excess of unlabeled avidin or streptavidin, which binds to all endogenous biotin. This is followed by an incubation with free biotin, which saturates all remaining unoccupied biotin-binding sites on the avidin/streptavidin molecules [1] [34]. The result is that all endogenous biotin is masked, and the detection complex has nothing to bind to except the biotinylated secondary antibody.
- Considerations: While highly effective, this two-step process can be time-consuming and may require optimization for different tissues [35].
2. Pre-Hybridization of Detection Reagents: This innovative method prevents the detection system from interacting with endogenous biotin in the first place.
- Procedure: The biotinylated secondary antibody is pre-incubated with the streptavidin-enzyme conjugate to form saturated complexes before they are applied to the tissue. These pre-formed complexes can no longer bind to endogenous biotin; their only available interaction is with the primary antibody [35] [37].
- Advantages: This method efficiently suppresses endogenous biotin binding without a separate, lengthy blocking step and has been shown to reduce background without compromising the specific signal [35].
Why am I still seeing high background even after a biotin block?
Answer: Persistent high background after a biotin block can stem from several sources:
- Inadequate Blocking: The concentration or incubation time for the avidin and biotin solutions may be insufficient for the specific tissue type. Tissues with very high biotin content may require more rigorous blocking [38].
- Lectins Binding to Avidin: If your ABC complex is made with avidin (from egg white), its high carbohydrate content can bind to lectins in the tissue, causing background. Solution: Replace avidin with its non-glycosylated alternatives, recombinant streptavidin or NeutrAvidin (de-glycosylated avidin), which exhibit much lower nonspecific binding [39] [4].
- Other Sources of Background: Ensure you have also blocked other potential sources of interference, such as:
- Endogenous Enzymes: Quench peroxidase activity with hydrogen peroxide (e.g., 3% H₂O₂ in methanol) and alkaline phosphatase with levamisole [1] [4] [36].
- Non-specific Protein Binding: Use protein blockers like normal serum, bovine serum albumin (BSA), or commercial animal-free blockers [38] [34].
- Secondary Antibody Cross-reactivity: Always include a no-primary-antibody control to check for secondary antibody nonspecific binding [4] [36].
Are there detection systems that avoid endogenous biotin entirely?
Answer: Yes. A highly effective way to circumvent the issue of endogenous biotin is to use polymer-based detection systems [36]. These systems consist of a secondary antibody directly conjugated to a polymer backbone that carries many enzyme molecules (e.g., HRP). Since these systems do not rely on the biotin-streptavidin interaction, they are completely unaffected by endogenous biotin, eliminating the need for a biotin-blocking step and significantly reducing background in problematic tissues [36].
Quantitative Data and Reagent Comparison
The choice of biotin-binding protein is crucial for minimizing background. The table below compares the key properties of the most common options.
| Protein (Source) | Molecular Weight (kDa) | Isoelectric Point (pI) | Biotin Affinity (Kd) | Non-Specific Binding | Key Characteristics |
|---|---|---|---|---|---|
| Avidin (Egg White) | 67-68 | 10.0 - 10.5 | ~1.3 x 10⁻¹⁵ M | High | Glycosylated, basic pI; high lectin binding. |
| Streptavidin (Recombinant) | ~53 | 6.8 - 7.5 | ~0.04 x 10⁻¹⁵ M | Low | Non-glycosylated, near-neutral pI; preferred for IHC. |
| NeutrAvidin (From Avidin) | ~60 | 6.3 | ~1.3 x 10⁻¹⁵ M | Lowest* | De-glycosylated; near-neutral pI; lowest nonspecific binding. |
*Depending upon the application or circumstances.
Experimental Protocols
Protocol 1: Standard Sequential Blocking for Endogenous Biotin
This is a fundamental method for suppressing background from endogenous biotin [1] [34].
Materials Needed:
- Unlabeled avidin or streptavidin solution
- Free biotin solution
- Phosphate-buffered saline (PBS) or Tris-buffered saline (TBS)
Detailed Methodology:
- After deparaffinization, rehydration, and antigen retrieval (if required), wash the tissue sections with buffer.
- Incubate with Avidin/Streptavidin: Cover the tissue with a solution of unlabeled avidin or streptavidin (e.g., from a commercial kit). Incubate for 15-20 minutes at room temperature.
- Wash: Rinse the slides thoroughly with buffer (e.g., 2 x 5 minutes in PBS) to remove unbound avidin/streptavidin.
- Incubate with Biotin: Cover the tissue with a solution of free biotin. Incubate for 15-20 minutes at room temperature.
- Wash: Rinse the slides thoroughly with buffer (e.g., 2 x 5 minutes in PBS).
- Proceed with the standard IHC protocol, starting with serum or protein blocking and primary antibody application.
Protocol 2: Pre-Hybridization Method for Western Blot and IHC
This method, adapted from a Western blot protocol, pre-forms the detection complexes to prevent binding to endogenous biotin [35] [37].
Materials Needed:
- Biotinylated secondary antibody
- Streptavidin-enzyme conjugate (e.g., HRP)
- Standard antibody dilution buffer
Detailed Methodology:
- Calculate Reagents: Determine the total volume of detection reagent needed for your experiment.
- Pre-hybridize: In a microcentrifuge tube, mix the biotinylated secondary antibody and the streptavidin-enzyme conjugate at their optimal working concentrations. A typical starting ratio is 5:1 (biotinylated antibody : streptavidin conjugate) [35].
- Incubate: Allow the mixture to incubate for 15-60 minutes at room temperature to form stable complexes.
- Apply to Tissue: After the primary antibody step and washing, apply the pre-hybridized detection complex directly to the tissue section. Incubate as you normally would.
- Wash and Develop: Wash the slides and proceed with chromogenic or fluorescent substrate development.
The following diagram illustrates the logical workflow of this pre-hybridization method.
The Scientist's Toolkit: Essential Reagents for Blocking
| Item | Function | Example/Note |
|---|---|---|
| NeutrAvidin or Streptavidin | High-affinity biotin-binding protein with low nonspecific binding used for blocking and detection. | Preferred over avidin due to lack of glycosylation and neutral pI [39]. |
| Free Biotin | Small molecule that saturates remaining binding sites on avidin/streptavidin after initial blocking. | Essential for a complete sequential block [1]. |
| Polymer-Based Detection System | HRP-labeled polymer linked directly to a secondary antibody; avoids biotin system entirely. | Ideal for tissues with extremely high endogenous biotin [36]. |
| Endogenous Enzyme Block | Suppresses activity of endogenous peroxidases (H₂O₂) and phosphatases (levamisole). | Required when using HRP or AP-based detection [1] [4]. |
| Protein Blocking Serum/BSA | Reduces nonspecific hydrophobic and ionic binding of antibodies to tissue. | Use serum from the same species as the secondary antibody [38] [34]. |
| Pre-made Blocking Kits | Provide optimized, ready-to-use reagents for sequential avidin/biotin blocking. | Saves time and ensures proper reagent formulation [4]. |
Visualization of Techniques
The following workflow diagram contrasts the standard ABC method with the pre-hybridization method, highlighting how the latter prevents background.
Endogenous enzyme activity represents a significant source of false-positive results and high background in immunohistochemistry (IHC), directly compromising experimental reliability and reproducibility. Within the context of a broader thesis on optimizing IHC for research and diagnostic applications, this guide addresses the critical need for systematic enzyme blocking protocols. When using enzyme-based detection systems such as horseradish peroxidase (HRP) or alkaline phosphatase (AP), endogenous enzymes present in tissues can react with the detection substrate, generating signal independent of antibody binding [4]. This technical resource provides researchers, scientists, and drug development professionals with a comprehensive, practical workflow for integrating effective enzyme blocking into standard IHC protocols, ensuring specific signal detection and accurate biological interpretation.
FAQs: Fundamental Principles of Enzyme Blocking
Q1: What is endogenous enzyme activity, and why does it interfere with IHC? Endogenous enzymes are proteins naturally present in tissues that possess catalytic activity similar to the enzymes conjugated to detection antibodies in IHC. For example, peroxidases and phosphatases found in various cell types, particularly in blood cells and some epithelial cells, can catalyze the same chromogenic or fluorescent reactions as HRP or AP conjugates [4]. This activity leads to non-specific signal generation, obscuring the true antigen-specific staining and resulting in high background that compromises data interpretation [40].
Q2: When is enzyme blocking absolutely necessary in the IHC workflow? Enzyme blocking is a mandatory step when using enzyme-conjugated detection systems and should be performed after antigen retrieval but before the application of the primary antibody [41]. The necessity is determined by the detection method:
- HRP-based detection: Requires blocking of endogenous peroxidases [42] [40].
- AP-based detection: Requires blocking of endogenous phosphatases [42] [4].
- Biotin-Streptavidin amplification systems: Require blocking of endogenous biotin, which is found primarily in mitochondria [41]. It is good practice to always include this step when the tissue type is known to have high endogenous levels, such as in liver, kidney, or brain tissues [4].
Q3: How can I quickly test if my tissue has problematic endogenous enzyme activity? A simple control experiment can diagnose endogenous enzyme interference. Incubate an untreated tissue section with only the detection substrate (e.g., DAB for HRP) for the standard development time, omitting all antibody incubation steps [4]. The development of a colored or fluorescent signal indicates that endogenous enzymes are active and must be blocked before proceeding with your experiment.
Step-by-Step Experimental Protocol for Enzyme Blocking
Workflow Integration
The following diagram illustrates the precise point for enzyme blocking within a standard IHC protocol.
Detailed Blocking Methodologies
After antigen retrieval and subsequent cooling of slides, follow these specific protocols based on your detection system.
For Endogenous Peroxidases (HRP Systems)
- Prepare Blocking Solution: Use 3% hydrogen peroxide (H₂O₂) in methanol or pure water [4] [40]. Commercially available peroxidase suppressor solutions can also be used [41].
- Apply Solution: Completely cover the tissue sections with the prepared H₂O₂ solution.
- Incubate: Incubate for 10–15 minutes at room temperature [4].
- Rinse: Rinse the slides thoroughly with distilled water, followed by a wash in your standard buffer (e.g., PBS or TBS).
For Endogenous Phosphatases (AP Systems)
- Prepare Blocking Solution: Use 2 mM levamisole in the appropriate buffer. Levamisole is an effective inhibitor for many types of endogenous alkaline phosphatase [42] [4] [40].
- Apply and Incubate: Cover the tissues and incubate for the recommended time (typically 10-30 minutes) at room temperature.
- Wash: Proceed with a standard buffer wash.
For Endogenous Biotin (Biotin-Streptavidin Systems)
- Sequential Blocking: Use a commercial avidin/biotin blocking kit [41].
- Procedure: Follow the manufacturer's instructions, which typically involve sequential incubation with an avidin solution to block endogenous avidin-binding sites, followed by a biotin solution to block any remaining endogenous biotin [42].
Troubleshooting Guide: Enzyme Blocking Issues
The table below summarizes common problems, their causes, and verified solutions related to enzyme blocking.
Table: Troubleshooting Enzyme Blocking in IHC
| Problem & Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| High Background (General) | Incomplete quenching of endogenous enzymes [40]. | Ensure fresh H₂O₂ is used; increase incubation time slightly; confirm levamisole is active [4]. |
| High Background (Brown Tissues) | Endogenous biotin not blocked [4]. | Implement a biotin/avidin blocking step prior to applying biotinylated secondary antibodies [41]. |
| Weak or No Target Signal | Over-blocking or enzyme inhibitor carried over into detection step. | Increase wash steps and volume after blocking; ensure inhibitors are thoroughly removed [40]. |
| Persistent Background in Control | Wrong blocking reagent for detection system. | Verify compatibility: use H₂O₂ for HRP, levamisole for AP. Run a substrate-only control to confirm [4]. |
Research Reagent Solutions
Selecting the correct reagents is fundamental to successful enzyme blocking. The following table lists essential reagents and their functions.
Table: Essential Reagents for Enzyme Blocking in IHC
| Reagent | Function in Protocol | Key Consideration |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) | Inactivates endogenous peroxidases by consuming the enzyme's cofactor [4]. | Use a fresh 3% solution for reliable results; old or diluted stocks are ineffective [40]. |
| Levamisole | Inhibits endogenous alkaline phosphatase activity [42] [4]. | Effective against many intestinal and placental-type AP isozymes, but may not block all [42]. |
| Avidin/Biotin Blocking Kit | Sequentially blocks endogenous biotin and avidin binding sites to prevent non-specific signal [41]. | Critical for tissues with high biotin levels (liver, kidney); use before applying biotinylated antibodies [4]. |
| Normal Serum | Blocks non-specific binding sites for antibodies, reducing general background [42]. | Should be from the same species as the host of the secondary antibody for optimal effect [43]. |
| BSA (IgG-Free) | Serves as an inert protein to block non-specific binding and as a carrier in antibody diluents [42]. | Use IgG-free and protease-free BSA to prevent interference with antibody binding [42]. |
Solving Staining Problems: Advanced Troubleshooting for Persistent Background
FAQ: How can I tell if my high background is from endogenous enzymes?
To determine if endogenous enzymes are causing your high background staining, follow this diagnostic protocol:
- Prepare a Control Slide: For your experimental tissue section, prepare an additional control slide.
- Omit Primary Antibody: On this control slide, skip the incubation with the primary antibody. Instead, incubate the tissue with just the detection substrate (e.g., DAB for HRP or NBT/BCIP for AP) for the same duration as your standard antibody incubation [4].
- Interpret the Results: If a strong background signal develops on this control slide, it confirms that endogenous enzyme activity in your tissue is interfering with your assay [4]. If no signal develops, the background is likely due to another cause, such as non-specific antibody binding.
A Step-by-Step Diagnostic Workflow
When you encounter high background in your IHC experiment, follow the logical troubleshooting path outlined in the diagram below to determine if endogenous enzymes are the culprit or if you should investigate other common issues.
Experimental Protocol: Quenching Endogenous Enzymes
If your diagnostic test confirms endogenous enzyme activity, use these standard protocols to quench it.
1. Quenching Endogenous Peroxidase Activity [4] [1] [44]
- Reagent: 3% Hydrogen Peroxide (H₂O₂) in methanol or water.
- Procedure:
- After deparaffinization, rehydration, and antigen retrieval, submerge the slides in the 3% H₂O₂ solution.
- Incubate for 10-15 minutes at room temperature.
- Wash the slides thoroughly with buffer (e.g., PBS or TBS) before proceeding to the blocking step.
- Note: If 3% H₂O₂ damages tissue or epitopes, try a lower concentration (e.g., 0.3%) [1].
2. Quenching Endogenous Alkaline Phosphatase Activity [4] [45]
- Reagent: 1-2 mM Levamisole in the detection substrate buffer.
- Procedure:
- Add levamisole directly to the alkaline phosphatase substrate solution (e.g., NBT/BCIP) immediately before use.
- Proceed with the detection step as usual. Levamisole will inhibit most endogenous phosphatases without affecting the commonly used calf intestinal alkaline phosphatase reporter [1].
The Scientist's Toolkit: Key Reagents for Blocking
The following table lists essential reagents used to mitigate endogenous interference and reduce non-specific background in IHC.
| Item | Function | Key Considerations |
|---|---|---|
| 3% Hydrogen Peroxide (H₂O₂) | Quenches endogenous peroxidase activity [4] [45] [1]. | Use fresh solution; can be prepared in methanol or water [1]. |
| Levamisole | Inhibits endogenous alkaline phosphatase activity [4] [45]. | Add directly to the substrate solution; ineffective on intestinal-type phosphatases [1]. |
| Avidin/Biotin Blocking Kit | Blocks endogenous biotin, prevalent in tissues like liver and kidney [4] [1]. | Essential when using avidin-biotin complex (ABC) detection systems [1]. |
| Normal Serum | Blocks non-specific protein-binding sites to reduce background [4] [44]. | Should be from the same species as the host of the secondary antibody [4]. |
| Sodium Azide | Inhibits microbial growth in buffers; can also inhibit HRP activity [4]. | Do not use in buffers if an HRP-based detection system is employed [4] [45]. |
FAQ: What are other common causes of high background?
If you have ruled out endogenous enzymes as the problem, consider and troubleshoot these other frequent causes:
- Primary Antibody Concentration is Too High: This is a very common cause. An excessively high antibody concentration increases non-specific binding. Solution: Perform an antibody titration experiment to find the optimal dilution that provides a strong specific signal with minimal background [45] [46].
- Insufficient Blocking: If non-specific sites on the tissue are not adequately blocked, antibodies can bind to them. Solution: Increase the concentration of your blocking agent (e.g., normal serum or BSA) and/or the blocking incubation time [45] [44].
- Inadequate Washing: Residual, unbound antibodies can contribute to a diffuse background. Solution: Increase the number and duration of washes between steps, using a buffer containing a mild detergent like 0.05% Tween-20 [44].
- Over-development: Leaving the chromogenic substrate (e.g., DAB) on the tissue for too long can produce a high, diffuse background. Solution: Carefully monitor the development reaction under a microscope and stop it immediately once the specific signal is clear [46].
- Tissue Drying Out: Allowing the tissue section to dry at any point after the primary antibody is applied can cause irreversible, high background staining. Solution: Always keep slides in a humidified chamber during incubation steps and ensure they are fully covered by liquid [46] [44].
Why is Blocking Critical in IHC?
Immunohistochemistry (IHC) combines immunological, biochemical, and histological techniques to detect specific antigens in tissue sections using labeled antibodies [25]. Despite an antibody's high specificity, non-specific binding can occur due to intermolecular forces, such as Van der Waals interactions or net charges on amino acid groups [47]. This binding prevents clear visualization of the true antigen-antibody interaction.
The primary purpose of the blocking step is to occupy these non-specific sites within the tissue sample before the primary antibody is applied [47]. Effective blocking is fundamental for reducing background staining and preventing false-positive results, ensuring that the final stain accurately reflects the target antigen's presence and location [2].
FAQ: Troubleshooting Persistent Background Staining
Q1: I have performed blocking, but my slides still show high background. What are the most common causes?
Persistent background after blocking is a frequent challenge, and the causes can be multifaceted. The table below summarizes the common issues and their initial diagnostic checks.
Table: Common Causes of Persistent Background Staining
| Cause Category | Specific Issue | Quick Check |
|---|---|---|
| Endogenous Enzymes | Incomplete blocking of endogenous peroxidase or alkaline phosphatase [1] [4]. | Incubate a tissue section with only the substrate (e.g., DAB); development of color indicates a problem [4]. |
| Endogenous Biotin | High endogenous biotin levels in tissues like liver, kidney, or mammary gland [1] [2]. | Most problematic in frozen sections; use a control without a biotinylated antibody to assess [1]. |
| Protein Blocking | Inadequate blocking serum concentration or incubation time [43]. | Ensure you are using serum from the same species as the secondary antibody and try increasing the concentration to 5-10% [2] [4]. |
| Antibody Issues | Primary or secondary antibody concentration is too high [43] [48]. | Perform an antibody titration experiment to find the optimal dilution [43]. |
| Cross-Reactivity | Secondary antibody binding to endogenous immunoglobulins in the tissue [48] [4]. | Include a no-primary-antibody control; background staining here suggests secondary antibody cross-reactivity [48]. |
Q2: How do I systematically optimize blocking concentration and incubation time?
Optimization is a iterative process. The following workflow provides a logical sequence for diagnosing and resolving background issues, with a focus on blocking parameters.
Diagram: A systematic workflow for troubleshooting persistent background staining.
Q3: What are the specific experimental protocols for optimizing blocking parameters?
After running controls to identify the likely cause, use these targeted experimental protocols.
A. Optimizing Protein Blocking Conditions
Objective: To determine the optimal concentration and incubation time of a protein blocking agent (e.g., normal serum or BSA) to minimize non-specific hydrophobic and ionic interactions.
Materials:
- Protein blocking agent (e.g., Normal Serum, BSA)
- Antibody Diluent
- Wash Buffer (e.g., PBS or TBST)
- Test tissue section known to have moderate target expression
Method:
- Prepare Blocking Solutions: Create a series of blocking solutions with varying concentrations of your chosen agent. For example:
- Normal Serum: 2%, 5%, and 10% (v/v) in wash buffer.
- BSA: 1%, 3%, and 5% (w/v) in wash buffer.
- Apply Block: Divide your slides into groups. Apply the different blocking solutions to separate slides. For each concentration, test two incubation times: 30 minutes and 60 minutes at room temperature.
- Proceed with Staining: Continue with your standard IHC protocol (primary antibody, secondary antibody, detection, etc.).
- Analysis: Compare the signal-to-noise ratio across the slides. The optimal condition is the one that yields strong specific staining with the cleanest background.
B. Optimizing Primary Antibody Concentration
Objective: To find the antibody dilution that provides strong specific signal with minimal background, as overly high concentrations are a common cause of background [43] [48].
Materials:
- Primary Antibody
- Recommended Antibody Diluent
Method:
- Prepare Antibody Dilutions: Prepare a series of primary antibody dilutions. A typical range could be 1:50, 1:100, 1:200, 1:500, and a no-antibody control.
- Incubate: Apply these dilutions to serial sections of the same test tissue.
- Standardize Protocol: Keep all other steps (blocking, retrieval, detection, incubation times) identical.
- Analysis: Identify the dilution where the specific staining is strong but the background is minimal. The signal intensity may plateau at higher concentrations, while background will continue to increase.
Table: Optimization of Key IHC Parameters to Reduce Background
| Parameter | Typical Range | Protocol Variation | Objective & Analysis |
|---|---|---|---|
| Protein Block Concentration | 2-10% serum [4] [49] or 1-5% BSA [49]. | Test 2%, 5%, 10% serum; 1%, 3%, 5% BSA. | Find concentration that minimizes general background without quenching specific signal. |
| Block Incubation Time | 30 - 60 minutes [48]. | Compare 30 min vs. 60 min at room temperature. | Ensure complete coverage and binding to all non-specific sites. |
| Primary Antibody Concentration | Manufacturer's recommendation as starting point. | Test a series (e.g., 1:50, 1:100, 1:200, 1:500). | Identify the highest dilution (lowest concentration) that gives a strong specific signal [43]. |
| Primary Antibody Incubation | Overnight at 4°C (common) [48]. | Compare 1 hr at RT vs. overnight at 4°C. | Overnight incubation often improves specificity and allows for higher antibody dilution. |
Advanced Blocking: Addressing Specific Interferences
Beyond general protein blocking, specific tissue components require targeted blocking strategies.
A. Blocking Endogenous Enzymes
When using enzyme-based detection systems (e.g., HRP or AP), endogenous versions of these enzymes must be blocked.
Table: Protocols for Blocking Endogenous Enzymes
| Enzyme | Tissues with High Activity | Blocking Solution | Incubation Protocol |
|---|---|---|---|
| Peroxidase (HRP) | Kidney, liver, red blood cells [2] [50]. | 0.3% - 3.0% H₂O₂ in methanol or aqueous buffer [1] [2] [49]. | 10-15 minutes at room temperature [1] [50]. |
| Alkaline Phosphatase (AP) | Kidney, intestine, placenta, lymphoid tissue [2]. | 1-2 mM Levamisole in buffer [1] [2]. | Incubate with the substrate solution (e.g., during the detection step) [1]. |
B. Blocking Endogenous Biotin
Tissues rich in endogenous biotin can cause severe background when using avidin-biotin complex (ABC) detection methods. The most effective strategy is a sequential two-step block [1] [2]:
- Incubate with an excess of avidin (or streptavidin) to bind all endogenous biotin.
- Incubate with an excess of free biotin to block any remaining binding sites on the avidin/streptavidin molecules [1].
For tissues with very high biotin, consider switching to a polymer-based detection system that does not rely on biotin chemistry [48] [2].
The Scientist's Toolkit: Essential Reagents for Effective Blocking
Table: Key Research Reagent Solutions for IHC Blocking
| Reagent | Function | Example & Notes |
|---|---|---|
| Normal Serum | Protein block; provides antibodies and proteins to bind non-specific sites. | Use serum from the species of the secondary antibody (e.g., Normal Goat Serum if secondary is goat anti-rabbit) [2]. |
| Bovine Serum Albumin (BSA) | Protein block; alternative to serum, especially in multiplexing. | Often used at 1-5% in buffer. Can be combined with detergents like Triton X-100 [47] [49]. |
| Hydrogen Peroxide (H₂O₂) | Blocks endogenous peroxidase activity. | Use 0.3% for frozen sections, 3% for paraffin sections [1] [49]. |
| Levamisole | Inhibits endogenous alkaline phosphatase activity. | Ineffective on intestinal alkaline phosphatase [1]. |
| Avidin/Biotin Blocking Kit | Sequentially blocks endogenous biotin. | Essential for biotin-rich tissues (liver, kidney) when using ABC methods [1] [2]. |
| Sodium Azide | Preservative for blocking buffers. | Warning: Inhibits HRP activity; do not use in buffers for HRP-conjugated antibodies [49]. |
Quality Control and Validation
No troubleshooting guide is complete without emphasizing controls. Always include:
- A no-primary-antibody control: This identifies background caused by the secondary antibody or detection system [48] [4].
- A positive control tissue: This confirms your entire protocol is working and helps distinguish specific signal from background [48].
- Use of calibrated slides: For quantitative analysis and to control for staining and scanning variations, specially designed IHC calibrator slides can be used [51].
The relationship between key reagents, their targets, and the resulting output in a well-controlled IHC experiment can be visualized as follows.
Diagram: The role of blocking agents in promoting specific signal by reducing background noise.
Troubleshooting High Background in Specific Tissue Types (e.g., Kidney, Liver)
FAQ: Why do kidney and liver tissues often present high background in IHC?
Kidney and liver tissues are particularly prone to high background staining in Immunohistochemistry (IHC) due to their high levels of endogenous bioactive substances. These substances interfere with common detection systems, leading to non-specific signal that can mask the true antigen-antibody reaction.
The primary challenges in these tissues are:
- High Endogenous Biotin: Liver and kidney tissues naturally contain high concentrations of biotin, which will bind to avidin or streptavidin in biotin-based detection systems, creating widespread background staining [52] [4].
- Active Endogenous Enzymes: These tissues possess endogenous peroxidase (in red blood cells) and alkaline phosphatase activities. When using enzyme-based detection (e.g., HRP or AP), these endogenous enzymes will catalyze the chromogenic substrate, producing a false-positive signal [16] [4].
- Tissue Autofluorescence: Fixed tissues, especially with aldehyde-based fixatives like formalin, can exhibit autofluorescence, which creates a high background when using fluorescence detection [53] [43].
FAQ: What are the specific strategies to reduce background in liver and kidney?
The table below summarizes the primary causes of high background in kidney and liver tissues and the recommended solutions.
| Challenge | Recommended Solution | Alternative or Complementary Approach |
|---|---|---|
| High Endogenous Biotin (Liver, Kidney) | Use polymer-based detection systems instead of avidin-biotin complex (ABC) methods [52]. | Perform a biotin block using a commercial Avidin/Biotin Blocking Kit [16] [4]. |
| Endogenous Peroxidase | Quench with 3% H₂O₂ in methanol or water for 10 minutes at room temperature [52] [16] [4]. | Use an endogenous enzyme blocking solution, readily available commercially [4]. |
| Endogenous Alkaline Phosphatase | Inhibit with 2 mM levamisole added to the substrate solution [16] [4]. | Use a different enzyme-label, such as HRP, and ensure thorough blocking. |
| Autofluorescence (from fixatives) | Switch to a fluorophore in the red or infrared range to avoid formalin's green autofluorescence [53] [43]. | Treat samples with autofluorescence quenching dyes like Sudan black or Pontamine sky blue [4]. |
| Non-specific Antibody Binding | Optimize blocking with 5-10% normal serum from the secondary antibody host for 30-60 minutes [52] [16]. | Titrate the primary and secondary antibodies to find the optimal concentration [53] [43]. |
Detailed Experimental Protocols
Protocol for Blocking Endogenous Biotin
For tissues with high endogenous biotin, a sequential blocking step is highly effective [4].
- After the standard blocking step with serum or protein.
- Incubate slides with an Avidin solution for 10-15 minutes.
- Wash thoroughly with buffer (e.g., PBS or TBST).
- Incubate slides with a Biotin solution for 10-15 minutes.
- Wash thoroughly before proceeding with the primary antibody application.
- Recommended Reagent: Commercial Avidin/Biotin Blocking Kits [4].
Protocol for Quenching Endogenous Peroxidase
This is a critical step when using HRP-based detection systems [52] [4].
- After deparaffinization, rehydration, and antigen retrieval (if performed).
- Incubate the slides in a solution of 3% H₂O₂ in methanol or RODI water.
- Incubate for 10 minutes at room temperature.
- Wash slides thoroughly with distilled water, followed by wash buffer (e.g., PBS or TBST).
- Proceed with the standard blocking and immunostaining protocol.
The following troubleshooting workflow synthesizes the key decision points and actions for resolving high background in these challenging tissues.
The Scientist's Toolkit: Key Research Reagent Solutions
The following reagents are essential for effectively managing background in complex tissue types like kidney and liver.
| Reagent | Function in Troubleshooting | Example Application |
|---|---|---|
| Polymer-Based Detection Kits | Replaces biotin-based systems to avoid interference from endogenous biotin. Superior sensitivity [52]. | SignalStain Boost IHC Detection Reagents [52]. |
| Avidin/Biotin Blocking Kits | Sequentially blocks endogenous biotin, preventing its binding to the detection system [16] [4]. | ReadyProbes Avidin/Biotin Blocking Solution [4]. |
| Endogenous Enzyme Blockers | Inhibits peroxidase (H₂O₂) or alkaline phosphatase (levamisole) activity to prevent false-positive chromogen deposition [16] [4]. | 3% H₂O₂ in methanol for peroxidase blocking; 2 mM levamisole for AP blocking. |
| Pre-adsorbed Secondary Antibodies | Secondary antibodies that have been adsorbed against immunoglobulins of multiple species to minimize cross-reactivity and non-specific binding [4] [43]. | Using anti-rabbit secondary pre-adsorbed against mouse and human IgG for staining human tissue with a rabbit primary. |
| Specialized Antibody Diluent | Optimized buffer to maintain antibody stability and reduce non-specific ionic interactions that cause background [52]. | SignalStain Antibody Diluent [52]. |
| Autofluorescence Quenchers | Chemical dyes that reduce natural tissue fluorescence, improving signal-to-noise ratio in fluorescence IHC [4]. | Treating fixed tissue sections with Sudan black or Pontamine sky blue. |
FAQs: Troubleshooting Formalin-Induced Autofluorescence
What causes formalin-induced autofluorescence in FFPE tissues?
Formalin and other aldehyde-based fixatives (like paraformaldehyde and glutaraldehyde) create methylene cross-links between proteins. An unfortunate consequence of this process is the formation of Schiff bases, which are highly fluorescent compounds. This fixation-induced autofluorescence has a broad emission spectrum, occurring across the blue, green, and red spectral ranges. Glutaraldehyde causes the most severe autofluorescence, followed by paraformaldehyde, then formaldehyde [54] [55].
How can I confirm that background signal is due to autofluorescence?
Always perform control experiments to diagnose autofluorescence [54] [55]:
- Tissue Autofluorescence Control: Process a tissue section without adding any primary or secondary antibodies.
- Secondary Antibody Control: Process a tissue section with the secondary antibody only (no primary antibody). A persistent fluorescent signal in these controls indicates inherent tissue or fixation-induced autofluorescence [4].
My autofluorescence is still high after treatment. What are my options?
If chemical and dye-based treatments are insufficient, the most effective strategy is to switch your detection to a spectral range where the autofluorescence is minimal.
- Use Far-Red Fluorophores: Autofluorescence from formalin and endogenous elements like collagen and NADH is strongest in the blue/green spectra. Choosing fluorophores that emit in the far-red (e.g., Alexa Fluor 647, CoraLite 647) will help distinguish your specific signal from the background [54] [55] [53].
- Leverage Multispectral Imaging: Advanced imaging systems can separate the specific fluorophore signal from the background autofluorescence based on their distinct spectral signatures [56].
Experimental Protocols for Autofluorescence Reduction
Protocol 1: Treatment with Sodium Borohydride
Sodium borohydride (NaBH₄) is a chemical quencher that reduces the fluorescent Schiff bases formed during formalin fixation [57] [4].
Detailed Methodology:
- Reagent Preparation: Prepare a 1 mg/mL solution of sodium borohydride in 1X Tris-Buffered Saline (TBS). Keep this solution on ice [57].
- Tissue Preparation: Deparaffinize and rehydrate your FFPE tissue sections through a graded series of alcohols to water. Perform standard antigen retrieval [57].
- Treatment Application: Apply the cold sodium borohydride solution to cover the tissue section. Perform three consecutive 10-minute incubations. Do not perform washes between incubations [57].
- Washing: After the final incubation, wash the slides thoroughly with 1X TBSt (TBS with 0.02% Tween-20) to remove the reagent [57].
- Proceed with Staining: Continue with your standard immunofluorescence protocol (e.g., blocking, antibody incubation) [57].
Protocol 2: Treatment with Sudan Black B
Sudan Black B (SB) is a lipophilic dye that effectively masks autofluorescence, particularly from lipids and the age-related pigment lipofuscin [57] [54] [55].
Detailed Methodology:
- Reagent Preparation: Prepare a 0.3% (w/v) solution of Sudan Black B in 70% ethanol. Stir the solution in the dark for 2 hours to ensure it is fully dissolved [57].
- Tissue Preparation: Deparaffinize, rehydrate, and perform antigen retrieval on FFPE tissue sections as standard.
- Treatment Application: Apply the Sudan Black B solution to cover the tissue. Incubate for 10 minutes at room temperature [57].
- Rinsing: Briefly rinse the slides in 70% ethanol to remove excess dye, followed by additional washing with buffer (e.g., 1X TBS or PBS) [57].
- Proceed with Staining: Mount the slides or continue with your immunofluorescence staining protocol.
Protocol 3: Treatment with Eriochrome Black T
Eriochrome Black T (EBT) is a dye that can shift or mask the autofluorescence emission profile [57].
Detailed Methodology:
- Reagent Preparation: Prepare a 1.65% (w/v) solution of Eriochrome Black T in deionized water [57].
- Tissue Preparation: Deparaffinize, rehydrate, and perform antigen retrieval on FFPE tissue sections.
- Treatment Application: Apply the Eriochrome Black T solution to the tissue. Incubate for 5 minutes at room temperature [57].
- Washing: Wash the slides with 1X TBSt to remove the reagent [57].
- Proceed with Staining: Continue with the standard immunofluorescence procedure.
Data Presentation: Comparison of Autofluorescence Reduction Treatments
The table below summarizes key treatments for diminishing autofluorescence, based on a systematic study of FFPE human respiratory tissue [57].
| Treatment | Mechanism | Concentration | Incubation Time | Key Considerations |
|---|---|---|---|---|
| Sodium Borohydride | Chemical quenching (reduces Schiff bases) | 1 mg/mL in TBS | 3 x 10 minutes (on ice) | Variable efficacy; requires cold temperature and multiple applications [57] [54]. |
| Sudan Black B | Masking (lipophilic dye) | 0.3% in 70% Ethanol | 10 minutes (room temp) | Also effective against lipofuscin; fluoresces in far-red channel—avoid for far-red multiplexing [57] [54] [55]. |
| Eriochrome Black T | Masking / Shifting emission | 1.65% in DI Water | 5 minutes (room temp) | One of the three most efficacious treatments identified [57]. |
| Trypan Blue | Masking | 250 µg/mL in TBS (pH 4.4) | 1 minute | Short incubation time [57]. |
| Ammonium Chloride | Chemical quenching | 50 mM in TBS | 10 minutes (room temp) | [57] |
Autofluorescence Reduction Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Reagent | Primary Function in Autofluorescence Reduction |
|---|---|
| Sodium Borohydride (NaBH₄) | Chemical quencher; reduces fluorescent Schiff bases formed by aldehyde fixation [57] [4] [54]. |
| Sudan Black B | Lipophilic dye; masks autofluorescence from lipids and lipofuscin [57] [54] [55]. |
| Eriochrome Black T | Dye; masks or shifts the emission profile of general tissue autofluorescence [57]. |
| TrueVIEW Autofluorescence Quenching Kit | Commercial reagent; designed to reduce autofluorescence from multiple causes [54]. |
| TrueBlack Lipofuscin Autofluorescence Quencher | Commercial reagent; specifically used to quench lipofuscin autofluorescence prior to imaging [58]. |
| Pontamine Sky Blue / Trypan Blue | Dyes; mask autofluorescence by absorbing light and re-emitting at a longer, less interfering wavelength [57] [4]. |
Troubleshooting Autofluorescence Strategy
This guide addresses frequent challenges in Immunohistochemistry (IHC), providing targeted solutions to ensure specific staining and reliable results.
Troubleshooting Common IHC Issues
Q: What are the primary causes of high background staining, and how can they be resolved?
High background staining, which results in a poor signal-to-noise ratio, can stem from several sources related to endogenous substances, antibodies, and protocol execution [4].
| Possible Cause | Specific Issue | Recommended Solution |
|---|---|---|
| Endogenous Enzymes | Peroxidase or phosphatase activity in tissue [4] | Quench with 3% H₂O₂ in methanol/water (10-15 min, RT) or use commercial blocking solutions [4] [59] [60]. For AP, use levamisole [4]. |
| Endogenous Biotin | High in kidney, liver tissues [59] | Use a polymer-based detection system instead of avidin-biotin. Block with commercial avidin/biotin blocking solutions [4] [59]. |
| Primary Antibody | Concentration too high; nonspecific binding [4] [60] | Titrate antibody to find optimal dilution. Incubate at 4°C. Add NaCl (0.15-0.6 M) to diluent to reduce ionic interactions [4]. |
| Secondary Antibody | Cross-reactivity or nonspecific binding [4] [59] | Include a negative control (no primary). Increase blocking serum concentration to 10%. Use cross-adsorbed secondary antibodies [4] [60]. |
| Inadequate Blocking | Non-specific sites remain exposed [12] [60] | Block with 5-10% normal serum (from secondary host species) or 1-5% BSA for 30 minutes at room temperature [12] [59] [60]. |
| Inadequate Washes | Unbound antibodies remain [59] [60] | Wash slides 3 times for 5 minutes with TBST or PBST after primary and secondary incubations [59]. |
Q: How do I troubleshoot weak or absent staining?
A lack of signal can be due to issues with the antigen, antibody, or detection system [59] [60].
| Possible Cause | Specific Issue | Recommended Solution |
|---|---|---|
| Antigen Masking | Over-fixation, especially with formalin, cross-links and masks epitopes [20] [59] | Optimize Antigen Retrieval. Use Heat-Induced Epitope Retrieval (HIER) with citrate buffer (pH 6.0) in a microwave or pressure cooker [4] [59]. |
| Antibody Potency | Loss of affinity from degradation, contamination, or excessive freeze-thaw cycles [4] | Always run a positive control. Store antibodies in small aliquots as per manufacturer instructions. Avoid contaminants [4] [60]. |
| Insufficient Antibody | Concentration too low for target abundance [60] | Increase antibody concentration or extend incubation time (e.g., overnight at 4°C) [59] [60]. |
| Slide Storage | Antigen loss over time in stored slides [59] | Use freshly cut sections. If storing is necessary, keep slides at 4°C and do not bake them before storage [59] [60]. |
| Detection System | Low sensitivity; expired reagents; incompatible buffers [59] | Use sensitive polymer-based detection. Ensure substrate pH is correct. Do not use sodium azide with HRP systems [4] [59] [60]. |
Q: What are the specific consequences of over-fixation, and how can they be corrected?
Over-fixation, particularly with aldehyde-based fixatives like formalin, causes excessive protein cross-linking. This can mask the target epitope, preventing antibody binding and leading to weak or false-negative results [20] [61].
- Mechanism: Formaldehyde creates methylene bridges between amino acids like lysine, arginine, and tyrosine, which can alter the protein's structure and hide the antibody-binding site [61].
- Prevention: Standardize fixation time. A general guideline is 18-24 hours in 10% Neutral Buffered Formalin (NBF) at room temperature. The fixative volume should be 10-20 times the tissue volume [12] [61].
- Correction: The primary method to reverse the effects of over-fixation is robust antigen retrieval [20] [59]. Heat-induced methods using a microwave or pressure cooker are highly effective at breaking cross-links and restoring antigenicity [59].
Experimental Protocols for Validation
Detailed Protocol: Blocking Endogenous Peroxidase Activity
Endogenous peroxidases are present in red blood cells, liver, and kidney tissues and must be blocked when using HRP-based detection to prevent high background [12] [59].
- After deparaffinization, rehydration, and antigen retrieval, rinse slides in distilled water.
- Prepare a 3% H₂O₂ solution in methanol or deionized water. Note: Prepare fresh for best results [59].
- Cover the tissue sections completely with the H₂O₂ solution and incubate for 10-15 minutes at room temperature [12] [59].
- Rinse slides thoroughly with distilled water followed by wash buffer (PBS or TBS).
- Proceed with the standard blocking and immunostaining steps.
Detailed Protocol: Antibody Titration for Optimal Concentration
Using the correct antibody concentration is critical for balancing strong specific signal with low background [62].
- Prepare a dilution series of the primary antibody (e.g., 1:100, 1:250, 1:500, 1:750, 1:1000) in the recommended diluent [62].
- Apply each dilution to consecutive, nearly identical tissue sections on the same slide, if possible. Include a negative control (no primary antibody) for each.
- Process all slides with the same secondary antibody and detection conditions.
- Evaluate staining under a microscope. The optimal dilution provides strong specific staining in the expected cellular location with a clean, low background.
Detailed Protocol: Using a Blocking Peptide Control
This control is the gold standard for confirming antibody specificity by competing for the binding site [63].
- Prepare two identical tubes of diluted primary antibody (at the optimized concentration).
- To one tube, add a 10-fold mass excess of the specific blocking peptide. To the other, add an equal volume of buffer. Incubate both for 1 hour at room temperature with rotation [63].
- Apply the "antibody alone" solution to one tissue section and the "antibody + peptide" solution to an adjacent section.
- Complete the IHC staining protocol for both sections in parallel.
- Interpret results: Specific staining is indicated by a significant loss of signal in the peptide-blocked section compared to the one stained with antibody alone [63].
Workflow and Relationship Diagrams
IHC Background Staining Troubleshooting
Fixation Time vs. Antigen Integrity Relationship
The Scientist's Toolkit: Research Reagent Solutions
| Reagent | Function | Key Considerations |
|---|---|---|
| Sodium Citrate Buffer (pH 6.0) | Common buffer for heat-induced antigen retrieval (HIER). Breaks formaldehyde cross-links to unmask epitopes [4] [59]. | The pH and retrieval method (microwave, pressure cooker) are critical and target-dependent [59]. |
| Normal Serum | Used for blocking. Serum from the host species of the secondary antibody occupies non-specific binding sites [12] [64]. | Use at 5-10% concentration. Do not use serum from the same species as the primary antibody host [4] [60]. |
| Hydrogen Peroxide (H₂O₂) | Quenches endogenous peroxidase activity to prevent false-positive signals in HRP-based detection [4] [12] [59]. | Use a 3% solution in methanol or water. Prepare fresh and protect from light [59] [60]. |
| Polymer-Based Detection Reagents | Non-biotin detection system. Polymer chains conjugated with multiple enzyme molecules provide high sensitivity and avoid endogenous biotin [59]. | Preferred over avidin-biotin (ABC) systems for tissues with high endogenous biotin (e.g., liver, kidney) [4] [59]. |
| Antibody Diluent | Buffer for diluting primary and secondary antibodies. May contain stabilizers and mild detergents to promote specific binding [59]. | Using the manufacturer's recommended diluent is crucial for optimal performance, especially for phospho-specific antibodies [59]. |
For best practices, always include appropriate positive and negative controls, carefully validate each new antibody and protocol, and ensure consistent sample processing to achieve reliable and reproducible IHC results.
FAQ: Addressing Endogenous Enzyme Activity
What are endogenous enzymes, and why do they interfere with IHC?
Endogenous enzymes are naturally occurring enzymes present within the tissue sample itself. In IHC, the most common reporters used for chromogenic detection are Horseradish Peroxidase (HRP) and Alkaline Phosphatase (AP). If the tissue contains its own active peroxidases or phosphatases (e.g., in erythrocytes, leukocytes, or liver tissues), these enzymes will react with the added detection substrate (e.g., DAB). This reaction generates a colored precipitate independently of your target antigen, leading to high background staining, false-positive signals, and a poor signal-to-noise ratio that can obscure your specific results [4] [1] [23].
How can I quickly diagnose if endogenous enzymes are causing my high background?
A simple and effective diagnostic test is to incubate a test tissue sample with the detection substrate alone, omitting both the primary and secondary antibodies. If a colored precipitate forms after adding the substrate, it confirms the presence of interfering endogenous enzyme activity that must be blocked before proceeding with your experiment [4]. Similarly, you can use your secondary antibody alone (without the primary) as a control; staining in this case can indicate issues with endogenous enzymes or non-specific binding of the secondary antibody [65].
What is the definitive solution for endogenous peroxidase activity?
The standard and most effective method is to quench the activity with hydrogen peroxide (H₂O₂) [4] [1] [23].
Detailed Protocol:
- After deparaffinization, rehydration, and antigen retrieval (if performed), wash slides in PBS or distilled water.
- Prepare a 3% H₂O₂ solution in methanol or pure water. Using methanol can help permeabilize the tissue, but for delicate tissues, a lower concentration of 0.3% H₂O₂ in aqueous solution is recommended to prevent damage [4] [1] [65].
- Submerge the slides in this solution and incubate for 10-15 minutes at room temperature.
- Wash the slides thoroughly with buffer (e.g., PBS or TBS) before proceeding to the blocking or primary antibody incubation step.
Note: Sodium azide is a potent inhibitor of HRP and should never be used in buffers if you are using an HRP-based detection system [4] [5].
How do I handle endogenous alkaline phosphatase activity?
Endogenous AP can be effectively inhibited with levamisole [4] [1] [66].
Detailed Protocol:
- Prepare a working solution containing 1-2 mM levamisole and add it directly to your AP substrate solution just before use [1] [66].
- Incubate the tissue with this substrate-levamisole mixture as per your standard detection protocol. Levamisole will suppress most endogenous AP activity (particularly the intestinal type) without affecting the activity of the calf-intestinal AP enzyme commonly conjugated to antibodies [1].
Are there alternative strategies if quenching is insufficient?
Yes. If background remains high despite quenching, consider these strategies:
- Switch the Detection System: The most straightforward alternative is to switch your detection enzyme. If you are using HRP and getting high background, switch to an AP-based detection system, and vice versa [1].
- Use Polymer-Based Detection Systems: Modern polymer-based systems do not rely on avidin-biotin chemistry (which has its own background issues from endogenous biotin) and can offer cleaner backgrounds with high sensitivity [67] [65] [68].
- Optimize Incubation Conditions: Incubating the primary antibody at 4°C overnight promotes slower, more specific binding, which can reduce non-specific background [4] [5].
Troubleshooting Table: Endogenous Enzyme Issues
The following table summarizes the key problems, their confirmation tests, and recommended solutions.
| Problem | Confirmatory Test | Recommended Solution | Key Parameters |
|---|---|---|---|
| Endogenous Peroxidase Activity | Incubate tissue with DAB substrate only. Brown precipitate indicates activity. | Quench with H₂O₂ [4] [1] [23]. | - Solution: 3% H₂O₂ in methanol or 0.3% H₂O₂ in water- Incubation: 10-15 min at RT |
| Endogenous Alkaline Phosphatase Activity | Incubate tissue with NBT/BCIP substrate only. Purple/black precipitate indicates activity. | Inhibit with Levamisole added to the substrate [4] [1] [66]. | - Solution: 1-2 mM Levamisole- Application: Add directly to substrate solution |
| Persistent High Background | Use a secondary antibody-only control. Staining indicates system-level issues. | Switch detection enzyme (HRP to AP, or vice versa) or use a polymer-based detection system [1] [67] [65]. | - System Change: HRP AP- Alternative: Biotin-free polymer systems |
Experimental Workflow for Diagnosis and Resolution
The diagram below outlines a systematic workflow for diagnosing and resolving endogenous enzyme issues in IHC.
Systematic troubleshooting workflow for endogenous enzyme issues in IHC.
Research Reagent Solutions
The following table lists key reagents essential for preventing and troubleshooting endogenous enzyme interference.
| Reagent | Function in Troubleshooting | Example/Note |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) | Oxidizing agent that quenches endogenous peroxidase activity by consuming the enzyme's substrate [4] [1]. | Typically used at 0.3% - 3% concentration in methanol or water [1] [65]. |
| Levamisole | Inhibitor of endogenous alkaline phosphatase, particularly the intestinal isoenzyme [4] [1]. | Added to the substrate solution at a final concentration of 1-2 mM [66]. |
| Polymer-Based Detection Kits | Biotin-free detection systems that avoid background from endogenous biotin and can provide cleaner results with high sensitivity [67] [65] [68]. | Examples include Enzo's POLYVIEW PLUS and CST's SignalStain Boost IHC Detection Reagents [67] [65]. |
| Normal Serum | Used in blocking step to reduce non-specific antibody binding, which can compound background issues [4] [23]. | Should be from the same species as the secondary antibody [23]. |
| Ready-to-Use Blocking Solutions | Commercial blends of proteins and/or synthetic polymers designed for effective blocking of non-specific interactions [4] [5]. | Often optimized for low background and compatibility with various detection systems. |
Ensuring Assay Reliability: Validation, Controls, and Comparative Analysis
FAQs on Negative Controls for IHC
What is the purpose of a "no primary antibody" control?
The "no primary antibody" control is designed to detect nonspecific binding caused by your detection system. In this control, the tissue is incubated with antibody diluent but without the primary antibody, followed by the normal incubation with the secondary antibody and detection reagents [69]. Any staining you see indicates that the secondary antibody is binding nonspecifically to components in the tissue, leading to false-positive results [69]. This control specifically validates that your secondary antibody and detection system are not creating background signal.
Why is an isotype control necessary if I already use a "no primary antibody" control?
While the "no primary antibody" control tests for secondary antibody issues, the isotype control specifically tests for nonspecific binding caused by the primary antibody itself [69]. An isotype control is an antibody that has the same immunoglobulin class (e.g., IgG, IgM) and is from the same host species as your primary antibody, but it targets an antigen that is not present in your sample [69]. When you use this control instead of your primary antibody, any staining observed indicates that your primary antibody could be binding nonspecifically through non-immunological interactions, rather than specifically to your target epitope.
Can I use the "no primary antibody" control to prove my primary antibody is specific?
No, this is a common misconception. The absence of staining when the primary antibody is omitted only serves as a control for nonspecific binding of the secondary antibody [70]. It does not provide evidence for the specificity of staining with your primary antibody [70]. A proper negative control for primary antibody specificity requires substitution with serum or isotype-specific immunoglobulins at the same concentration as your primary antibody [70].
What should I do if my negative controls show staining?
If your negative controls show staining, your results are compromised. The table below outlines common problems and solutions:
| Problem Identified | Possible Cause | Recommended Solution |
|---|---|---|
| Staining in "no primary antibody" control | Non-specific binding of secondary antibody [4] | Increase blocking serum concentration to 10%; reduce secondary antibody concentration; ensure adequate washing [4] [71] |
| Staining in isotype control | Non-specific binding of primary antibody [69] | Titrate primary antibody to optimal concentration; add NaCl (0.15-0.6 M) to antibody diluent to reduce ionic interactions [4] |
| Background across all slides, including controls | Endogenous enzyme activity [4] | Quench endogenous peroxidases with 3% H2O2 [4] [71] or block endogenous biotin [4] |
Troubleshooting Guide: Addressing Endogenous Enzyme Activity
Endogenous enzymes present in tissues can react with your detection system's enzyme substrates (like HRP or AP), causing high background that obscures specific signal. This issue must be addressed for your controls and experimental slides to be valid.
How to Identify and Remedy Endogenous Enzyme Interference
- Identification Test: Incubate a test tissue section with only the detection substrate (no antibodies). If a signal develops, it indicates interference from endogenous peroxidases or phosphatases [4].
- Remedies:
- For endogenous peroxidases: Quench with 3% H2O2 in methanol or water for 10 minutes at room temperature before antibody incubation [4] [71].
- For endogenous alkaline phosphatases: Use the inhibitor levamisole in your substrate solution [4].
- For endogenous biotin (especially in kidney, liver): Use a polymer-based detection system instead of avidin-biotin complexes (ABC), or perform a biotin block [4] [71].
Experimental Protocol: Establishing Valid Negative Controls
Follow this detailed protocol to ensure your negative controls are properly set up within the context of your full IHC experiment.
Materials Needed:
- Tissue sections on slides (FFPE or frozen)
- Primary antibody and matching isotype control at the same concentration
- Normal serum from the species of your secondary antibody
- Blocking buffer (e.g., TBST with 5% normal serum)
- Antibody diluent
- Appropriate detection kit (HRP or AP-based)
Workflow:
Diagram 1: Workflow for negative control setup.
Procedure:
- Slide Preparation: Perform antigen retrieval (if using FFPE tissue) and permeabilization as optimized for your target [72].
- Endogenous Enzyme Blocking: Immediately after rehydration, quench endogenous peroxidases by incubating slides in 3% H2O2 in methanol or RODI water for 10 minutes at room temperature [4] [71].
- Serum Blocking: Block all slides with a suitable blocking buffer (e.g., TBST with 5% normal goat serum) for 30 minutes to reduce nonspecific binding [71].
- Antibody Application:
- Slide 1 (Experimental): Apply the optimized dilution of your primary antibody.
- Slide 2 (Isotype Control): Apply the isotype control antibody at the same concentration as the primary antibody.
- Slide 3 (No Primary Control): Apply only antibody diluent.
- Detection: Incubate all slides with the same secondary antibody and detection system (e.g., polymer-based HRP with DAB).
- Interpretation:
- A clean isotype control slide confirms your primary antibody's specificity.
- A clean no primary antibody control confirms your secondary antibody and detection system are not causing background.
- Specific staining should only be present in your experimental slide.
The Scientist's Toolkit: Essential Reagents for Valid IHC Controls
The table below details key reagents required for implementing proper negative controls in IHC.
| Reagent | Function in Control Experiments | Example |
|---|---|---|
| Isotype Control Antibody | Matches the primary antibody's species, isotype, and conjugation; confirms specificity. | Mouse IgG2a for a mouse IgG2a primary antibody [69]. |
| Normal Serum | Blocks nonspecific protein-binding sites; used in blocking buffers and antibody diluents. | Normal goat serum when using a goat-derived secondary antibody [4] [71]. |
| Hydrogen Peroxide (H₂O₂) | Quenches endogenous peroxidase activity to prevent false-positive signals. | 3% solution in methanol or water, applied for 10 minutes [4] [71]. |
| Polymer-Based Detection Kit | A biotin-free detection system that avoids background from endogenous biotin. | SignalStain Boost IHC Detection Reagents [71]. |
| Antibody Diluent | A protein-rich, buffered solution for stabilizing antibody concentrations. | SignalStain Antibody Diluent or TBST/5% NGS [71]. |
Key Takeaways for Robust IHC Data
Proper use of both "no primary antibody" and isotype controls is fundamental for validating your IHC results. These controls help you distinguish specific signal from artifacts caused by your detection system or nonspecific antibody binding. Always integrate these controls into your IHC workflow, especially when troubleshooting high background, to ensure your conclusions about protein localization and expression are reliable and reproducible.
This technical support center provides a framework for validating immunohistochemistry (IHC) assays in accordance with the latest College of American Pathologists (CAP) guidelines. A properly validated assay is the foundation for reliable and reproducible results, which are critical for both research and drug development. A key aspect of this validation involves addressing technical challenges, such as endogenous enzyme activity, which can cause high background staining and compromise data integrity. The following guides and FAQs are designed to help you navigate the validation process and troubleshoot specific experimental issues.
FAQs: CAP IHC Assay Validation
1. What are the core sample size requirements for validating a new IHC assay according to CAP?
The CAP guidelines provide specific, evidence-based recommendations for the number of samples required for assay validation. The exact number depends on whether the assay is being validated for a new biomarker or verified for an established one in your lab. The table below summarizes the key quantitative requirements [73]:
Table 1: CAP Validation Sample Size Requirements
| Validation Scenario | Minimum Positive Cases | Minimum Negative Cases | Total Minimum Samples | Target Concordance |
|---|---|---|---|---|
| Standard IHC Assay Validation | 20 | 20 | 40 | ≥90% |
| Validation for Alternative Fixatives (e.g., cytology) | 10 | 10 | 20 | Not specified |
| Predictive Marker Assays (e.g., HER2, PD-L1) | Varies by scoring system | Varies by scoring system | Varies | ≥90% |
Note: For predictive markers with distinct scoring systems (e.g., PD-L1, HER2), the CAP guideline stipulates that laboratories should separately validate/verify each assay-scoring system combination [73].
2. What are the acceptable comparator methods for IHC assay validation?
CAP Statement 1 outlines several options for validation study design, ordered here from most to least stringent [73]:
- Comparison to IHC results from cell lines with known protein amounts ("calibrators").
- Comparison with a non-IHC method (e.g., flow cytometry, FISH).
- Comparison with results from testing the same tissues in another laboratory using a validated assay.
- Comparison with prior testing of the same tissues with a validated assay in the same laboratory.
3. How do we validate IHC assays performed on cytology specimens?
The 2024 CAP guideline update provides explicit guidance for cytology specimens not fixed identically to the tissues used for initial validation. It requires laboratories to perform separate validations with a minimum of 10 positive and 10 negative cases for IHC performed with alternative fixatives [73].
Troubleshooting Guides
Guide 1: Resolving High Background Staining
High background, or non-specific staining, is a common issue that can obscure results and is often related to endogenous enzyme activity or antibody non-specificity.
Table 2: Troubleshooting High Background Staining
| Problem Cause | Specific Issue | Recommended Solution |
|---|---|---|
| Endogenous Enzyme Activity | High levels of endogenous peroxidase in tissues like RBCs, granulocytes, and liver/kidney. | Use a peroxidase-blocking step (e.g., 3% H2O2 for 10 minutes) before primary antibody incubation [74] [75]. |
| Endogenous Biotin | Prevalent in tissues like liver and kidney; interferes with biotin-based detection systems. | Use a polymer-based detection system that does not rely on biotin-streptavidin chemistry. Alternatively, perform a biotin-blocking step after the normal serum block [75]. |
| Inadequate Blocking or Washing | Non-specific antibody binding or residual reagents on the slide. | Use an appropriate protein block (e.g., 5% normal serum). Ensure standardized, thorough washing (e.g., 3 x 5 min with TBST) after each incubation step [74] [75]. |
| Antibody Concentration Too High | Excessive antibody leads to non-specific binding. | Titrate the primary antibody to find the optimal dilution that provides strong specific signal with minimal background [76]. |
| Insufficient Antigen Retrieval | Masked antigens cause antibodies to bind non-specifically. | Optimize the antigen retrieval method (e.g., pH, buffer, heating conditions: microwave, water bath, or pressure cooker) for your specific antibody and tissue [75]. |
The following workflow diagram outlines a logical approach to diagnosing and resolving high background issues:
Guide 2: Addressing No or Faint Staining
A complete lack of signal can be just as problematic as high background. The issues often lie in assay conditions or reagent integrity.
Table 3: Troubleshooting No or Faint Staining
| Problem Cause | Specific Issue | Recommended Solution |
|---|---|---|
| Antigen Masking or Loss | Over-fixation (especially in formalin) or suboptimal antigen retrieval. | Optimize antigen retrieval buffer (e.g., citrate vs. EDTA) and retrieval method (microwave, pressure cooker). Ensure fixation time is consistent and not excessive [75]. |
| Antibody or Detection Issues | Inactive primary antibody, improper dilution, or expired detection reagents. | Use a known positive control tissue to verify antibody and protocol. Check expiration dates. Titrate the primary antibody. Ensure detection kits are stored and used correctly [75]. |
| Insufficient Epitope Exposure | The protocol does not adequately expose the target epitope. | Ensure complete deparaffinization with fresh xylenes. Follow optimized antigen retrieval protocols, which may require a pressure cooker for some difficult targets [75]. |
| Incompatible Buffer Systems | Using phosphate buffers with Alkaline Phosphatase (AP) detection systems. | If using an AP-based system, avoid phosphate-buffered saline (PBS) for washing and incubation, as phosphate ions inhibit AP activity. Use Tris-based buffers instead [77]. |
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the right reagents is critical for a robust and validated IHC assay. The following table details essential materials and their functions.
Table 4: Essential Reagents for IHC Assay Validation
| Reagent Category | Specific Examples | Function in IHC & Validation |
|---|---|---|
| Detection Systems | Polymer-based HRP systems; Avidin-Biotin Complex (ABC) | Amplifies the primary antibody signal. Polymer systems are highly sensitive and avoid endogenous biotin interference, which is valuable for validation [75]. |
| Antigen Retrieval Buffers | Citrate Buffer (pH 6.0), EDTA Buffer (pH 8.0-9.0) | Reverses formaldehyde-induced cross-links to expose epitopes. The optimal pH and buffer must be determined during validation for each antibody [75]. |
| Blocking Reagents | Normal Serum, Protein Block, BSA | Reduces non-specific background staining by occupying reactive sites on the tissue. Essential for achieving a high signal-to-noise ratio [75]. |
| Enzyme Blockers | 3% Hydrogen Peroxide (H2O2), Levamisole (for AP) | Quenches endogenous peroxidase or alkaline phosphatase activity to prevent false-positive background [74] [75]. |
| Primary Antibody Diluents | Commercial Antibody Diluents, PBS/BSA | Preserves antibody stability and can contain additives to reduce non-specific binding. Using a consistent, optimized diluent is key to assay reproducibility [75]. |
| Validation Controls | FFPE Cell Pellets, Multi-tissue Microarrays (TMAs) | Provide consistent positive and negative controls for run-to-run monitoring of assay performance. Critical for both initial validation and ongoing quality control [73] [75]. |
Visualizing the IHC Assay Validation Workflow
A successful validation follows a structured process from planning to implementation. The diagram below outlines the key stages.
In immunohistochemistry (IHC) research, accurate detection of target antigens is paramount. However, the presence of endogenous enzymes, such as peroxidases and alkaline phosphatases, can catalyze the same chromogenic substrates used for detection, leading to false-positive results and compromised data integrity. A critical step in validating any IHC experiment is to confirm the efficiency of the blocking procedures for these endogenous enzymes. This guide details a pre-incubation protocol using 3,3'-Diaminobenzidine (DAB) or 5-Bromo-4-chloro-3-indolyl phosphate/Nitro blue tetrazolium (BCIP/NBT) substrates to test blocking efficiency, ensuring that observed staining is specific to the antibody-antigen interaction.
FAQ: Understanding Pre-Testing for Blocking Efficiency
Q1: Why is it necessary to test for endogenous enzyme activity before starting my IHC experiment? Endogenous peroxidases and alkaline phosphatases are present in many tissues. If not effectively blocked, they will react with the HRP or AP substrate used for detection, generating nonspecific background staining that obscures the true signal and leads to false-positive interpretation of results [1] [2]. Pre-testing verifies that your blocking step was successful.
Q2: When should I perform this pre-incubation test? This test should be performed after you have completed the blocking step for endogenous enzymes but before you add your primary antibody [1] [2]. It serves as a quality control checkpoint for your protocol.
Q3: My pre-test shows positive staining. What does this mean? A positive result—the formation of a colored precipitate upon substrate addition—indicates that endogenous enzyme activity is still present and has not been sufficiently quenched by your blocking method. You should not proceed with your main IHC experiment until you have optimized the blocking step [1] [4].
Q4: What are the recommended solutions if my blocking is inefficient?
- For Peroxidases (DAB staining): Ensure you are using a fresh solution of 0.3% to 3% hydrogen peroxide for quenching. Incubate for 10-15 minutes at room temperature [1] [78]. If the problem persists, consider increasing the incubation time or concentration within limits that do not damage epitopes.
- For Alkaline Phosphatase (BCIP/NBT staining): Add 1 mM levamisole to your substrate solution. Levamisole is an effective inhibitor for many types of endogenous alkaline phosphatase [1] [2].
- Alternative Approach: If blocking remains problematic for a particular enzyme, consider switching to a detection system based on the other enzyme (e.g., use an AP-based kit if endogenous peroxidase is too high) [1].
Experimental Protocol: Pre-Incubation Test
The following table summarizes the core procedural steps for testing blocking efficiency against endogenous peroxidases and alkaline phosphatases.
Table 1: Protocol for Testing Endogenous Enzyme Blocking Efficiency
| Step | Parameter | Test for Peroxidase (HRP) | Test for Alkaline Phosphatase (AP) |
|---|---|---|---|
| 1. Sample Preparation | Tissue Section | Deparaffinized and rehydrated FFPE or frozen section. | Deparaffinized and rehydrated FFPE or frozen section. |
| 2. Blocking | Treatment | Incubate with 0.3% - 3% H₂O₂ for 10-15 min [1] [78]. | Incubate with 1 mM levamisole or proceed without for the test [1] [2]. |
| 3. Pre-Incubation Test | Substrate | Apply DAB substrate for 10-15 min [1] [2]. | Apply BCIP/NBT substrate for 10-15 min [1] [2]. |
| 4. Result Interpretation | Positive Result | Development of a brown precipitate [1] [79]. | Development of a dark blue/purple precipitate [80] [79]. |
| Negative Result | No color change. Blocking is successful [1]. | No color change. Blocking is successful [1]. |
Detailed Methodology
- Tissue Preparation: Begin with your prepared tissue sections (formalin-fixed paraffin-embedded or frozen) that have been deparaffinized (if applicable) and rehydrated.
- Apply Blocking Agent: Perform your standard endogenous enzyme blocking step. For peroxidases, this is typically incubation with a hydrogen peroxide solution (e.g., 0.3% H₂O₂ in methanol or aqueous solution for 10-15 minutes). For alkaline phosphatases, this may involve the use of levamisole [1] [2] [78].
- Pre-Incubation with Substrate: After blocking and a subsequent buffer wash, directly apply the prepared chromogenic substrate solution (DAB for HRP or BCIP/NBT for AP) to the tissue section. Do not add any primary or secondary antibodies.
- Incubate and Monitor: Allow the substrate to incubate for a time equal to your planned detection step (typically 10-15 minutes). Monitor for the development of color.
- Interpret Results:
- No Color Development: The test is negative. This indicates that endogenous enzyme activity has been successfully blocked, and you can proceed with your IHC experiment with confidence.
- Color Development: The test is positive. This indicates residual endogenous enzyme activity. You must troubleshoot and optimize your blocking protocol before proceeding with the main experiment. Refer to the FAQ section for solutions.
Workflow for Testing Blocking Efficiency
The following diagram illustrates the decision-making process for validating blocking efficiency using the pre-incubation test.
The Scientist's Toolkit: Essential Reagents
Table 2: Key Reagents for Blocking Endogenous Enzymes and Testing Efficiency
| Reagent | Function | Example Application |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) | Quenches endogenous peroxidase activity by acting as an oxidizing agent in the presence of the enzyme [1] [78]. | Used as a 0.3% - 3% solution in methanol or buffer for 10-15 minute incubation. |
| Levamisole | Inhibits endogenous intestinal-like alkaline phosphatase activity by acting as an alkaline phosphatase inhibitor [1] [2]. | Added to the substrate solution (e.g., BCIP/NBT) at a final concentration of 1 mM to block during detection. |
| DAB Substrate | Chromogenic substrate for Horseradish Peroxidase (HRP); produces a brown, insoluble precipitate upon oxidation [1] [79]. | Used to detect HRP-conjugated antibodies or to test for residual endogenous peroxidase activity. |
| BCIP/NBT Substrate | Chromogenic substrate combination for Alkaline Phosphatase (AP); produces an insoluble dark blue/purple precipitate [80] [79]. | Used to detect AP-conjugated antibodies or to test for residual endogenous alkaline phosphatase activity. |
| Polymer-Based Detection System | A detection method that does not rely on biotin-streptavidin chemistry, avoiding issues with endogenous biotin [4] [78]. | Recommended as an alternative to avidin-biotin complex (ABC) methods in tissues with high endogenous biotin (e.g., liver, kidney). |
In immunohistochemistry (IHC), the blocking step is critical for reducing non-specific background staining and false-positive results. This process involves inhibiting endogenous enzymes, blocking non-specific protein binding sites, and saturating endogenous molecules like biotin that can interfere with detection systems. Researchers must choose between commercially prepared blocking kits and traditional laboratory-made solutions, each with distinct advantages and limitations. This technical guide provides a comparative analysis and troubleshooting support to help scientists optimize their IHC protocols for reliable results.
## Troubleshooting Guides
### FAQ: Addressing Common Blocking Issues
1. What are the primary causes of high background staining in IHC? High background, or noise, can stem from multiple sources related to inadequate blocking. Key causes include:
- Endogenous Enzymes: Peroxidase activity (in red blood cells, kidney, liver) or alkaline phosphatase activity (in intestine, bone, placenta) reacts with chromogenic substrates [4] [2] [81].
- Endogenous Biotin: Prevalent in tissues like liver, kidney, mammary gland, and brain, leading to non-specific signal in avidin-biotin complex (ABC) detection systems [4] [1] [2].
- Non-specific Antibody Binding: Primary or secondary antibodies may bind to charged particles, Fc receptors on cells, or other non-target tissue elements [4] [81].
- Inadequate Protein Blocking: Insufficient blocking with serum or protein buffers allows antibodies to adhere to non-specific sites [23] [2].
2. How can I determine if my background is caused by endogenous enzymes? To test for endogenous peroxidase activity, incubate a control tissue section with the peroxidase substrate (e.g., DAB) alone. The development of a colored precipitate indicates the presence of active endogenous enzymes that require blocking [1] [2]. A similar test for alkaline phosphatase uses a BCIP/NBT substrate, where a blue precipitate indicates endogenous activity [2].
3. When should I use a commercial blocking kit over a lab-made solution? Commercial kits are often preferable when:
- Standardization is key: Kits offer consistent, pre-optimized formulations for reproducible results across experiments and users [1] [81].
- Working with challenging tissues: Tissues rich in endogenous biotin (e.g., liver) or endogenous enzymes benefit from specialized, potent blockers found in kits [82] [1].
- Efficiency is a priority: Kits save preparation time and can combine multiple blocking actions (e.g., blocking both peroxidase and alkaline phosphatase with a single reagent like BLOXALL) [81]. Lab-made solutions offer flexibility for protocol fine-tuning and can be more cost-effective for high-volume routine blocking where parameters are already well-established [23] [2].
4. Why is there still high background after I performed a protein block? This can occur if:
- The serum used for blocking does not match the host species of the secondary antibody [23] [2].
- The concentration of the blocking agent is too low, or the incubation time is too short [43].
- The primary antibody concentration is too high, leading to non-specific binding [4] [83].
- There is cross-reactivity, especially when using mouse-primary antibodies on mouse tissue ("mouse-on-mouse" effect), which requires specific MOM blockers or F(ab')2 fragments [82] [2].
### Troubleshooting Blocking Problems
| Observed Problem | Potential Cause | Recommended Solution |
|---|---|---|
| High Background Staining | Inadequate blocking of endogenous peroxidase/alkaline phosphatase [4] [2]. | Quench with 3% H2O2 (in methanol or water) or a commercial peroxidase suppressor. For AP, use 1-10 mM levamisole [4] [1] [2]. |
| High levels of endogenous biotin [4] [1]. | Use an avidin/biotin blocking kit or switch to a polymer-based (non-biotin) detection system [82] [1] [2]. | |
| Non-specific binding of secondary antibody [4] [82]. | Include a no-primary-antibody control. Increase the concentration of the normal serum block (up to 10%) from the secondary antibody host species [4] [43]. | |
| Primary antibody concentration too high [4] [43]. | Titrate the antibody to find the optimal dilution that minimizes background while retaining specific signal [43] [83]. | |
| Weak or No Specific Staining | Over-blocking or epitope damage from harsh blocking steps [43]. | For HRP-conjugated primary antibodies, perform peroxidase blocking after the primary antibody incubation to protect epitopes [1] [84]. |
| Blocking serum contains neutralizing antibodies [4]. | Change to a different diluent or blocking solution, such as BSA or a commercial protein block [4] [81]. | |
| Endogenous enzyme quenching destroyed the target antigen [83]. | Change the order of steps: block endogenous enzymes after primary antibody incubation [83]. |
## Comparative Data Analysis
### Comparison of Blocking Reagent Types
The table below summarizes the key characteristics of commercial kits versus laboratory-made solutions for different blocking needs.
| Blocking Need | Commercial Kits | Laboratory Solutions |
|---|---|---|
| General Protein Block | Formulation: Pre-mixed synthetic peptide cocktails or optimized protein buffers [23] [81].Consistency: High batch-to-batch reproducibility [81].Examples: Animal-Free Blocker, specialized antibody diluents [81]. | Formulation: Normal serum (5-10%), BSA (1-5%), or non-fat dry milk [23] [2].Flexibility: Concentration and serum source can be adjusted.Note: Non-fat dry milk contains biotin and is unsuitable for ABC methods [2]. |
| Endogenous Biotin Block | Protocol: Sequential application of avidin/streptavidin followed by free biotin [1] [2].Efficacy: Highly effective and reliable for biotin-rich tissues [1].Examples: Endogenous Biotin-Blocking Kits [1]. | Protocol: Lab-prepared avidin and biotin solutions.Alternative: Switch to non-biotin polymer detection systems to avoid the issue entirely [82] [2]. |
| Endogenous Peroxidase Block | Formulation: Ready-to-use hydrogen peroxide solutions, sometimes with stabilizers [1].Convenience: Saves preparation time.Examples: Peroxidase Suppressor, Hydrogen Peroxide Block [4] [1]. | Formulation: 0.3%-3.0% H2O2 in methanol or aqueous buffer [4] [1] [83].Consideration: Methanol-based helps preserve tissue architecture in peroxidase-rich tissues [81]. |
| Endogenous Alkaline Phosphatase Block | Formulation: Ready-to-use levamisole solutions or pre-added to substrates [2] [81].Comprehensiveness: Some kits (e.g., BLOXALL) block both AP and peroxidase [81]. | Formulation: 1-10 mM levamisole hydrochloride added to the substrate solution or used as a separate block [4] [2]. |
## Experimental Protocols
### Detailed Protocol: Blocking Endogenous Biotin with a Commercial Kit
This protocol is designed for formalin-fixed, paraffin-embedded (FFPE) tissue sections and uses a typical sequential avidin/biotin blocking kit [1] [2].
Principle: Endogenous biotin binding sites are saturated with unconjugated avidin/streptavidin. Any remaining unoccupied binding sites on the avidin/streptavidin molecules are then filled with free biotin, preventing subsequent binding of the detection complex [1].
Procedure:
- Deparaffinization and Rehydration: Process slides through xylene and graded alcohols to water.
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER) as required for your target antigen. Note: HIER can increase the detectability of endogenous biotin, making this block essential [1].
- Rinse slides in wash buffer (e.g., PBS).
- Apply Unlabeled Avidin/Streptavidin: Cover the tissue section with the avidin or streptavidin solution from the kit. Incubate for 10-15 minutes at room temperature.
- Wash slides gently with buffer to remove excess reagent.
- Apply Free Biotin: Cover the tissue section with the biotin solution from the kit. Incubate for 10-15 minutes at room temperature.
- Wash slides thoroughly with buffer.
- Proceed with the standard IHC protocol starting from the protein blocking or primary antibody incubation step.
### Detailed Protocol: Blocking with Laboratory-Made Serum and Protein
This is a standard protocol for reducing non-specific antibody binding via protein blocking [23] [2].
Principle: Normal serum and proteins like BSA physically occupy hydrophobic and charged sites on the tissue, as well as Fc receptors, preventing non-specific interactions with the primary and secondary antibodies [2] [81].
Reagent Preparation:
- Protein Block Buffer: 2-5% Normal Serum (from the same species as the secondary antibody) and 1-3% BSA in PBS or Tris-buffered saline [4] [2].
Procedure:
- After any required endogenous enzyme blocking steps, tap off excess liquid from the slide.
- Apply Blocking Solution: Completely cover the tissue section with the prepared protein block buffer.
- Incubate: Place slides in a humidified chamber to prevent evaporation. Incubate for 30 minutes to 1 hour at room temperature. For challenging specimens, incubation can be extended or performed at 4°C [23].
- Tip: Do not wash the blocking buffer off vigorously. Instead, tap off the excess solution and proceed directly to the next step (usually primary antibody application). This ensures the blocking agents remain in place during antibody incubation [23].
## Visualization of Workflows
### Blocking Strategy Selection
### Troubleshooting High Background
## The Scientist's Toolkit
### Essential Research Reagent Solutions
| Reagent / Solution | Function / Purpose |
|---|---|
| Normal Serum | A primary protein blocking agent. Serum from the host species of the secondary antibody is used to block Fc receptors and non-specific binding sites [23] [2]. |
| Bovine Serum Albumin (BSA) | A common protein used in blocking buffers to occupy non-specific hydrophobic binding sites on tissues [23] [2]. |
| Hydrogen Peroxide (H₂O₂) | Used at 0.3% - 3% concentration to quench endogenous peroxidase activity, typically before primary antibody incubation [4] [1] [83]. |
| Levamisole Hydrochloride | An inhibitor of endogenous alkaline phosphatase activity, often added to the substrate solution at 1-10 mM concentration [4] [2]. |
| Avidin/Biotin Blocking Kit | A sequential kit used to block endogenous biotin in tissues, preventing non-specific signal in ABC detection systems [1] [2]. |
| Sodium Borohydride | Used to reduce autofluorescence caused by aldehyde fixation (e.g., with formalin), often by treating tissue with a 1 mg/mL solution in PBS [4] [2]. |
| Animal-Free Blocker | A commercial, universal protein-blocking reagent suitable for researchers avoiding animal-derived products [81]. |
| BLOXALL Blocking Solution | A commercial solution that blocks both endogenous peroxidase and alkaline phosphatase activity in a single 10-minute step [81]. |
FAQs on Endogenous Enzyme Activity in IHC
1. Why is blocking endogenous enzymes critical for reproducible IHC, especially in multi-center studies?
Endogenous enzymes, such as peroxidases and phosphatases, are naturally present in tissues and can react with the chromogenic substrates used for detection in IHC [1]. This reaction generates unwanted background staining or false-positive signals that falsely indicate the presence of a target antigen [1]. In multi-institutional studies, inconsistencies in blocking protocols are a major source of irreproducibility, as even slight variations in the concentration of blocking solutions can lead to dramatically different staining outcomes [85]. Establishing and adhering to a harmonized blocking protocol is therefore foundational for generating comparable and trustworthy data across different laboratories.
2. What is the recommended concentration of hydrogen peroxide (H₂O₂) for quenching endogenous peroxidases, and why is this specific concentration important?
The established and recommended concentration for quenching endogenous peroxidase activity is a 3% (v/v) solution of hydrogen peroxide [1] [85]. This concentration is crucial because lower concentrations, such as 0.9% or 0.3%, have been scientifically demonstrated to be insufficient for complete inhibition [85]. For example, one study showed that a breast carcinoma specimen falsely stained positive for a specific protein when a 0.3% H₂O₂ solution was used, but stained negative when the proper 3% solution was applied, with all other conditions remaining identical [85]. Adopting this standardized concentration across laboratories prevents such false-positive artifacts and enhances data comparability.
3. Which tissues have high levels of endogenous biotin, and how should they be handled?
Tissues rich in endogenous biotin include the liver, kidney, mammary gland, and adipose tissue [1]. When using avidin-biotin complex (ABC) detection methods, this endogenous biotin must be blocked to avoid high background staining [1]. The recommended procedure is a two-step block: first, incubate the sample with an excess of unlabeled streptavidin (or avidin) to bind the endogenous biotin; second, add an excess of free biotin to fill all the remaining binding sites on the streptavidin molecules [1]. An alternative and effective solution is to avoid biotin-based detection systems altogether for these tissues and instead use polymer-based detection systems, which eliminate the problem at its source [86].
4. How can we validate that our blocking protocol for endogenous enzymes is effective?
A simple and effective validation test is to run a control where the tissue sample is incubated with the detection substrate alone (e.g., DAB for HRP) for the same duration as the antibody incubation, but without the primary antibody [4]. The development of a colored precipitate in this control indicates residual endogenous activity, signaling that your blocking step is inadequate and needs optimization [4]. Incorporating this check during assay validation and periodically during routine staining is a key practice for robust quality control.
Troubleshooting Guide: Endogenous Enzyme Interference
Here are common issues related to endogenous activity and steps to resolve them.
Table 1: Troubleshooting Background Staining
| Problem & Possible Cause | Diagnostic Test | Recommended Solution |
|---|---|---|
| High Background from Endogenous Peroxidases [1] [4] | Incubate a tissue section with peroxidase substrate (e.g., DAB) alone. Development of color indicates problematic activity. | Quench with 3% H₂O₂ in methanol or water for 10-15 minutes [1] [85] [86]. |
| High Background from Endogenous Biotin (e.g., in liver, kidney) [1] [4] | Staining persists with biotin-streptavidin detection system in susceptible tissues. | Use a sequential avidin/biotin blocking kit, or switch to a polymer-based detection system (non-biotin) [4] [86]. |
| High Background from Endogenous Alkaline Phosphatase (AP) [1] | Incubate a tissue section with AP substrate (e.g., NBT/BCIP) alone. Color development indicates AP activity. | Inhibit by adding 1 mM levamisole to the substrate solution [1]. |
| False Positive Staining due to Inadequate Peroxidase Block [85] | Compare staining with 0.3% vs. 3% H₂O₂ block; false positives may disappear with the stronger block. | Strictly adhere to using a 3% H₂O₂ blocking solution and re-optimize the step if false positives occur [85]. |
Experimental Protocols for Harmonized Blocking
Protocol 1: Standardized Blocking of Endogenous Peroxidases
This protocol is designed for formalin-fixed, paraffin-embedded (FFPE) tissue sections and should be performed after deparaffinization, rehydration, and antigen retrieval.
Materials:
- 3% (v/v) Hydrogen Peroxide (H₂O₂) in deionized water or methanol
- Phosphate-Buffered Saline (PBS) or Tris-Buffered Saline (TBS)
- Humidified slide chamber
Method:
- After antigen retrieval and cooling, wash slides twice in buffer (PBS/TBS) for 5 minutes each.
- Submerge the slides completely in freshly prepared 3% H₂O₂ solution.
- Incubate for 10-15 minutes at room temperature [1] [86].
- Wash the slides thoroughly with buffer (e.g., three times for 5 minutes each) to remove all traces of H₂O₂.
- Proceed with the subsequent blocking and antibody incubation steps.
Note for Multi-institutional Reproducibility: The 3% concentration and incubation time must be strictly adhered to. Laboratories should confirm the efficacy of their stock H₂O₂ and document the specific supplier and catalog number in their Standard Operating Procedures (SOPs).
Protocol 2: Standardized Blocking of Endogenous Biotin
Use this protocol when an avidin-biotin detection system must be used on tissues known to have high endogenous biotin.
Materials:
- Avidin Solution (from a commercial blocking kit or prepared)
- Biotin Solution (from a commercial blocking kit or prepared)
- Protein Block (e.g., serum or BSA)
Method:
- After peroxidase blocking (if applicable) and washing, incubate the sections with a ready-to-use avidin solution for 10-15 minutes [4].
- Wash slides with buffer to remove unbound avidin.
- Incubate the sections with a ready-to-use biotin solution for 10-15 minutes [4].
- Wash slides thoroughly with buffer.
- Proceed with the standard protein block and primary antibody incubation.
Note for Multi-institutional Reproducibility: For maximum consistency, the use of a commercial avidin/biotin blocking kit is recommended. The use of streptavidin or NeutrAvidin (a deglycosylated form) instead of avidin for detection can further reduce background from lectin binding and is considered a best practice [1].
Workflow Visualization
The following diagram illustrates the critical decision points for managing endogenous enzyme activity within a standardized IHC workflow, ensuring consistent results across different laboratories.
Research Reagent Solutions
This table details essential reagents for effectively managing endogenous enzyme activity, providing a common reference for procurement and protocol harmonization.
Table 2: Essential Reagents for Blocking Endogenous Activity
| Reagent | Function & Rationale | Example |
|---|---|---|
| Hydrogen Peroxide (3%) | Quenches endogenous peroxidase activity by providing a substrate that is consumed before the detection step, preventing reaction with the chromogen (e.g., DAB) [1] [85]. | Thermo Fisher Peroxidase Suppressor [1]. |
| Levamisole (1 mM) | Inhibits endogenous alkaline phosphatase (AP) activity. It is added directly to the AP substrate solution to prevent non-specific staining without affecting the activity of the commonly used calf intestinal AP enzyme [1]. | Pre-formulated NBT/BCIP/levamisole mixtures [1]. |
| Avidin/Biotin Blocking Kit | Sequentially blocks endogenous biotin. Unlabeled avidin binds free biotin sites, followed by free biotin which saturates the avidin's remaining binding sites, preventing detection reagent binding [1] [4]. | Invitrogen ReadyProbes Avidin/Biotin Blocking Solution [4]. |
| Polymer-Based Detection System | A superior alternative to avidin-biotin systems. Uses a dextran polymer backbone conjugated with enzymes and antibodies, completely bypassing issues with endogenous biotin and thus eliminating the need for biotin blocking [86]. | SignalStain Boost IHC Detection Reagents [86]. |
| Normal Serum | Used in the protein block step to reduce non-specific binding of secondary antibodies by occupying hydrophobic and charged sites on the tissue. Serum should be from the same species as the secondary antibody [4] [12]. | Normal Goat Serum, Normal Donkey Serum. |
In immunohistochemistry (IHC) research, effectively addressing endogenous enzyme activity is crucial for generating reliable, interpretable data. While specific techniques for blocking endogenous peroxidases and phosphatases are well-established, a comprehensive quality assurance strategy extends far beyond these fundamental steps. This technical support resource provides a systematic framework for integrating multiple control types to validate staining specificity, minimize artefacts, and ensure experimental reproducibility. By adopting this holistic approach, researchers can confidently distinguish true positive signals from background staining and technical artefacts, thereby enhancing the scientific rigor of their IHC experiments.
Section 1: The Core Control Framework for IHC
A robust IHC control strategy systematically addresses different potential sources of error through multiple control types, each serving a distinct validation purpose.
Comprehensive Control Types and Their Applications
Table 1: Essential IHC Controls for Quality Assurance
| Control Type | Purpose | Experimental Setup | Interpretation of Results |
|---|---|---|---|
| Positive Tissue Control [87] | Verifies assay functionality | Stain a known antigen-expressing tissue alongside test samples | Proper Assay: Expected staining pattern in control.Assay Issue: Lack of staining indicates protocol problems. |
| Negative Tissue Control [87] | Reveals non-specific binding | Use tissue known to lack the target antigen (e.g., KD/KO samples) | Specific Staining: No staining in negative control.Non-specific Binding: Staining indicates antibody or protocol issues. |
| No Primary Antibody Control [87] | Assesses secondary antibody specificity | Omit primary antibody; incubate with diluent then secondary only | Clean Secondary: No staining confirms secondary specificity.Problematic Secondary: Staining indicates non-specific binding. |
| Isotype Control [87] | Evaluates antibody non-specific binding | Replace primary antibody with same-isotype non-specific antibody at identical concentration | Specific Binding: No staining confirms primary antibody specificity.Non-specific Binding: Staining indicates Fc receptor or protein interaction issues. |
| Absorption Control [87] | Confirms antibody-antigen specificity | Pre-absorb primary antibody with excess immunogen before application | Specific Interaction: Significant staining reduction confirms antibody specificity.Limited Reduction: Suggests non-specific antibody binding. |
| Endogenous Background Control [87] | Identifies inherent tissue background | Examine unstained tissue section for autofluorescence or endogenous activity | Low Background: Minimal inherent signal.High Background: Requires blocking strategies or detection system change. |
Experimental Protocols for Key Controls
Protocol 1: No Primary Antibody Control
Purpose: To verify that secondary antibodies do not bind non-specifically to tissue components [87].
- Follow standard IHC protocol through deparaffinization and antigen retrieval steps.
- Instead of applying primary antibody, incubate sections with antibody diluent only for the duration normally used for primary incubation.
- Apply secondary antibody and complete standard detection protocol.
- Interpret results: Any staining indicates non-specific binding of the secondary antibody detection system.
Protocol 2: Isotype Control
Purpose: To confirm that observed staining results from specific antigen recognition rather than non-specific antibody interactions [87].
- Prepare identical tissue sections as for test samples.
- Replace specific primary antibody with an immunoglobulin of the same isotype, host species, and conjugation at the same concentration.
- Process test and control sections in parallel through identical conditions.
- Interpret results: Lack of staining in isotype control validates specificity of test staining.
Protocol 3: Endogenous Peroxidase Blocking
Purpose: To quench endogenous peroxidase activity that causes background in HRP-based detection [1].
- Following deparaffinization and rehydration, prepare peroxidase blocking solution (3% hydrogen peroxide in methanol, or commercial peroxidase suppressor).
- Incubate sections for 10-15 minutes at room temperature.
- Wash twice with buffer before proceeding with primary antibody application.
- Note: For surface antigen staining, perform blocking after primary or secondary antibody incubation to preserve epitopes [1].
Section 2: The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for IHC Quality Control
| Reagent Category | Specific Examples | Function in Quality Assurance |
|---|---|---|
| Enzyme Blockers | Hydrogen peroxide, sodium azide [1], levamisole [1] | Quench endogenous enzyme activities that cause false positives |
| Biotin Blockers | Free avidin/streptavidin, excess biotin [1] | Block endogenous biotin in tissues like liver, kidney, mammary gland |
| Protein Blockers | Normal serum, BSA, commercial protein blocks [50] | Reduce non-specific antibody binding to tissue components |
| Validated Controls | Known positive tissues, knockout tissues [87], cell lines [88] | Provide benchmarks for assay performance and specificity |
| Detection Modulators | Alternative enzymes (AP instead of HRP) [1] [89], different chromogens [89] | Circumvent persistent background issues through system switching |
| Antigen Retrieval Reagents | Citrate buffer, EDTA, Tris-EDTA [50] | Reverse formaldehyde-induced epitope masking while managing background |
Section 3: Troubleshooting Guide: FAQs for Common Experimental Issues
Background and Specificity Problems
Q: I observe high background staining in tissues known to have endogenous biotin (liver, kidney). How can I resolve this?
A: Implement a biotin blocking protocol [1]:
- After antigen retrieval, incubate sections with free avidin or streptavidin (25-100 μg/mL) for 20 minutes.
- Wash and then incubate with free biotin (25-100 μg/mL) for 20 minutes.
- Proceed with standard IHC protocol.
- Consider using non-biotin detection systems if background persists.
Q: My negative control shows staining pattern similar to my test sample. What could be wrong?
A: This indicates non-specific binding. Troubleshoot using this systematic approach:
- Verify antibody concentration is not too high (titrate if necessary).
- Ensure proper protein blocking step is included [50].
- Check for antibody cross-reactivity by reviewing specification sheets [50].
- Confirm that the negative control tissue truly lacks the target antigen.
- Validate secondary antibody specificity using no-primary control [87].
Optimization and Validation Challenges
Q: How can I validate my IHC results when no commercial knockout tissue is available?
A: Employ multiple complementary approaches:
- Use absorption control by pre-incubating antibody with immunogen peptide [87].
- Compare staining patterns across multiple tissues with known expression profiles.
- Utilize alternative negative control methods such as isotype controls [87].
- Correlate with other detection methods (e.g., Western blot) if possible.
- Employ siRNA knockdown in cell line controls if feasible.
Q: What is the optimal fixation time to balance morphology and antigen preservation?
A: Fixation time critically impacts IHC results [88]:
- Ideal formalin fixation: 24-48 hours [88].
- Under-fixation (<24 hours): Causes proteolytic degradation and false negatives.
- Over-fixation (>48 hours): Masks epitopes through excessive cross-linking.
- Always standardize fixation conditions across compared samples.
- Begin fixation within 30 minutes of tissue collection to prevent autolysis [88].
Section 4: Advanced Integration in Experimental Design
Implementing External Quality Assurance
For laboratories performing clinical or translational IHC, participation in external quality assurance programs provides critical validation [88]:
- Programs like UK NEQAS, NordiQC, and QuIP (Germany) circulate standardized samples for inter-laboratory comparison.
- These initiatives help standardize staining interpretation and establish consensus scoring methods.
- They are particularly crucial for predictive biomarkers (e.g., HER2, hormone receptors) where staining accuracy directly impacts patient treatment.
Multiplex IHC Considerations
When designing multiplex IHC experiments to detect multiple antigens simultaneously:
- Select chromogens with contrasting colors and ensure compatibility in detection order [89].
- Use different enzyme systems (HRP and AP) to prevent cross-reaction during sequential detection [89].
- Include controls for each primary antibody individually to verify specificity of multiplex results.
- Consider substrate heat resistance if protocols require heating between detection steps [89].
Quantitative IHC and Standardization
For semi-quantitative or quantitative IHC applications:
- Implement rigorous standardization of all processing steps from fixation to counterstaining [50].
- Use cell line controls with known antigen expression levels as reference standards [88].
- Establish consistent scoring criteria among multiple observers to minimize inter-observer variability [88].
- Document all control results systematically to enable longitudinal quality tracking.
A holistic quality assurance strategy in IHC extends far beyond simple enzyme blocking to encompass a comprehensive system of controls that validate every aspect of the experimental process. By systematically implementing positive and negative controls, specificity assessments, and background evaluations, researchers can confidently interpret their results and generate robust, reproducible data. This integrated approach ensures that observed staining patterns truly reflect biological reality rather than technical artefacts, ultimately strengthening the scientific conclusions drawn from IHC experiments.
Conclusion
Effectively managing endogenous enzyme activity is not merely a technical step but a foundational requirement for robust and reliable IHC. Mastering the interplay between foundational knowledge, precise methodological application, systematic troubleshooting, and rigorous validation is key to eliminating false positives and achieving high-quality, interpretable data. As IHC continues to evolve, particularly with the rise of multiplexed techniques and its expanding role in clinical diagnostics and drug development, the principles of proper enzyme blocking remain paramount. Future directions will likely involve the development of more potent and specific inhibitors, integrated automated blocking protocols, and standardized validation frameworks that ensure reproducibility across laboratories, ultimately strengthening the critical link between IHC results and scientific and clinical conclusions.
References
- 1. Methods to Block Endogenous Detection [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/methods-block-endogenous-detection.html]
- 2. Blocking in IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/blocking-in-ihc]
- 3. What are the Common Reporter Enzymes used in IHC [https://www.enzo.com/note/what-are-the-common-reporter-enzymes-used-in-ihc/]
- 4. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 5. Immunohistochemistry Troubleshooting Guide [https://www.enzo.com/note/immunohistochemistry-troubleshooting-guide/]
- 6. IHC Blocking | Proteintech Group [https://www.ptglab.com/support/immunohistochemistry-protocol/ihc-blocking/?srsltid=AfmBOopQ32azyL22ytMTbECn74akmEE2brUrF9yg6I6daT7P_hP3A1cx]
- 7. Overview of Immunohistochemistry (IHC) [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-immunohistochemistry.html]
- 8. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqAZbOU8GC7anjpm4JH7e9SVtBD5nAAUud7DW80HXpJY1DX2z6B]
- 9. IHC Immunodetection (Staining) [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-immunodetection.html]
- 10. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 11. Detection and amplification systems [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/detection-and-amplification-systems]
- 12. Immunohistochemistry (IHC): Experimental Protocols and ... [https://www.antibodysystem.com/archive/387.html]
- 13. Useful Immunohistochemical Markers of Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3439132/]
- 14. Immunohistochemistry Troubleshooting [https://ihcworld.com/2024/01/26/immunohistochemistry-troubleshooting/]
- 15. Background Staining In IHC And IF [https://vectorlabs.com/blog/my-staining-didnt-work-part-1-background-staining-in-ihc-and-if/?srsltid=AfmBOoqU-0vk03UrcKe34I_RpmBMUR_qG0zxyxnHWxjMcOAREKRpg4W3]
- 16. High background in immunohistochemistry [https://www.abcam.com/en-us/technical-resources/troubleshooting/high-background-in-immunohistochemistry]
- 17. Application Guides / Peroxidase Blocking Methods [https://www.2bscientific.com/resources/application-guides/immunohistochemistry-guide/immunohistochemistry-walkthrough/blocking-steps/peroxidase-blocking-methods]
- 18. Effects of Fixation and Tissue Processing on ... [https://www.leicabiosystems.com/us/knowledge-pathway/effects-of-fixation-and-tissue-processing-on-immunocytochemistry/]
- 19. A Guide to Better IHC Staining: Steps, Troubleshooting, ... [https://www.celnovte.com/solution/a-guide-to-better-ihc-staining-steps-troubleshooting-and-optimization/]
- 20. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 21. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooMcWzXe8vXnSEXhjZPxedl52ExVUCXQFJfDdevBQo2qHdbiZli]
- 22. Fixation Strategies and Formulations Used in IHC Staining [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/fixation-strategies-formulations.html]
- 23. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 24. Getting To The Specifics: Blocking For Immunohistochemistry [https://vectorlabs.com/blog/blocking-for-immunohistochemistry/?srsltid=AfmBOooLoy22_WllyjKjX2zThiVnxJZkZMkf9DFpg1cfmHxqaxWg6vhg]
- 25. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467?utm_source=chatgpt.com]
- 26. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOop1rp_Csgpqvgy7Ain2ZTiUG_JHuTvoGaaLWTAVOwtmQxUuu4vS]
- 27. - Creative Diagnostics IHC Blocking [https://www.creative-diagnostics.com/blog/index.php/ihc-blocking/]
- 28. Levamisole Solution [https://vectorlabs.com/products/levamisole-solution/?srsltid=AfmBOorRuIqhUIMvqWgfAtCAPRsIuzZnIGWLbXgBFkwqi-sKGn_pK0vw]
- 29. Inhibition of endogenous tissue alkaline phosphatase with ... [https://pubmed.ncbi.nlm.nih.gov/7024402/]
- 30. Basics of the Blocking Step in IHC [https://www.nsh.org/blogs/natalie-paskoski/2021/02/19/basics-of-the-blocking-step-in-ihc]
- 31. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoqAVYngYiCYoIA2Ol5ADpIC8w0OYqZnm4E9s-4zFLCj1b934Fut]
- 32. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooa4KLBI-R_uRWKftMVM93JUbJEHVG8KY2huIrJbWtU6MZzkCCL]
- 33. Getting To The Specifics: Blocking For Immunohistochemistry [https://vectorlabs.com/blog/blocking-for-immunohistochemistry/?srsltid=AfmBOopZ8HZiD3Uj3KvAFc14ZS8GLV-E4nDvyZ_Jhza3KXs4JAn9xzPE]
- 34. ICC/IHC Non-Specific Binding / Staining Prevention Protocol [https://www.rndsystems.com/resources/protocols/preventing-non-specific-staining]
- 35. An efficient way of suppressing endogenous biotin-binding ... [https://www.sciencedirect.com/science/article/abs/pii/S0022175914000842]
- 36. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqweVjkh-a55Qdyajqsi9MS1lRRXUUSrWdIp3P1x44cXnpqnJRM]
- 37. an efficient way of suppressing endogenous biotin-binding ... [https://pubmed.ncbi.nlm.nih.gov/24657589/]
- 38. Getting To The Specifics: Blocking For Immunohistochemistry [https://vectorlabs.com/blog/blocking-for-immunohistochemistry/?srsltid=AfmBOoqHqwAyXu1G9fB37vJ_FEDoR8ims4IZGtuEOQAfU_jTkyvMQzx8]
- 39. Strept(avidin)–Biotin Complex Method for IHC Detection [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/avidin-biotin-complex-method-ihc-detection.html]
- 40. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoqFtEzL4NR2wApOsukzRZSXYm3kePBOohyZB0Z1RPPTizjX4891]
- 41. Immunohistochemistry-IHC | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cellular-imaging/ihc.reg.my.html]
- 42. A guide to selecting control and blocking reagents. [https://www.jacksonimmuno.com/secondary-antibody-resource/technical-tips/controls-diluents-blocking/]
- 43. Immunohistochemistry Troubleshooting [https://www.antibodies.com/applications/immunohistochemistry/ihc-troubleshooting]
- 44. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooYxGdOvDuX_BmuoPqNPke3KMp6AJuNSvXMl0E6mnPM9iTpJYyp]
- 45. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoprgKR6teFuc9QbxiD3oi2Yl7WVCbZ_e7xr366uwMjn3slcDQRE]
- 46. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 47. IHC Blocking | Proteintech Group [https://www.ptglab.com/support/immunohistochemistry-protocol/ihc-blocking/?srsltid=AfmBOooJ0v5xwd5MP-wn9ZdXAL-9rCRv9ujoSqZ9sg6kCJoXUW_rQcRB]
- 48. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOor-ThenRdSsTsgUAphiFXLIheAcsLY1W5oMZbqiUPUARfKpB7b_]
- 49. Blocking Solutions [https://ihcworld.com/2024/01/20/blocking-solutions/]
- 50. Intro to Immunohistochemistry (IHC) Staining: Steps & Best ... [https://www.leicabiosystems.com/us/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 51. calibration of color and intensity variation in whole slide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10499734/]
- 52. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooIR1rYRLX9NHF_a31Txk17kl_21x4WF9vfBU8e7x4nYeTa4LDp]
- 53. How to Reduce Background Noise in IHC [https://www.azolifesciences.com/article/How-to-Reduce-Background-Noise-in-IHC.aspx]
- 54. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOoqhXNIlmrCBjxL8B8I8cBBmPQ8hfzntLZyjWAwEqS13Abo2ssFH]
- 55. How to Reduce Autofluorescence [https://www.labcompare.com/10-Featured-Articles/577255-How-to-Reduce-Autofluorescence/]
- 56. Automated Multiplex Immunofluorescence Panel for Immuno-oncology... [https://www.jove.com/t/58390/automated-multiplex-immunofluorescence-panel-for-immuno-oncology]
- 57. Characterizing and Diminishing Autofluorescence in Formalin -fixed... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4174629/]
- 58. Optimizing immunofluorescence with high-dynamic-range ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11219731/]
- 59. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopa_q9I_eBqpV6efmf9xse4yym2XlmGRy4bekK6MGqSLFn6g8k0]
- 60. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOopi-XLTCf7s194xCAPBdrCa4Mb9UxGrboqGLpNsrBNCgo3H8b5o]
- 61. Tissue fixation and the effect of molecular fixatives on downstream... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4240801/]
- 62. Immunolabeling Using Secondary Antibodies Protocol [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/molecular-probes-school-of-fluorescence/imaging-basics/protocols-troubleshooting/protocols/immunolabeling-using-secondary-antibodies.html]
- 63. Blocking Peptide Protocols for Immunohistochemistry (IHC) ... [https://www.alomone.com/info/peptide-blocking-protocols-for-immunostaining?srsltid=AfmBOooRYaghKV3oXX0Qf0S-erXx0Us1J0nXBYtGsuODIvhapVmjxmhz]
- 64. Tips and Techniques for Troubleshooting ... [https://www.merckmillipore.com/HN/es/technical-documents/protocol/protein-biology/immunohistochemistry/antibody-immunohistochemistry-expert-tips-and-techniques]
- 65. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOop8JoSZ3ZoweDwv1PUuvZXUGbU8OUEw9t6z50aP4U6Oz6woevf8]
- 66. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOopc9yzEHUcSlFhwgD5El-fZz9mdKC-FdNvvX78MmL2UAohs-Xpg]
- 67. What are the different detection methods for IHC? [https://www.enzo.com/note/what-are-the-different-detection-methods-for-ihc/]
- 68. IHC Detection Systems: Advantages and Disadvantages [https://www.novusbio.com/ihc-detection?srsltid=AfmBOoqVCvScXGS2XXn-_fOXuBZjBPQCwUkosavLevDxJfBf4QteYdR9]
- 69. What Controls are Necessary for Immunohistochemistry? [https://www.enzo.com/note/what-controls-are-necessary-for-immunohistochemistry/]
- 70. Controls for Immunohistochemistry: The Histochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4212362/]
- 71. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOorDGUWSAgTHlm_br82kOKA_vGr6oMPQ46HkRGPM23qGjbqBqzSi]
- 72. Immunohistochemistry Techniques, Strengths, Limitations ... [https://www.technologynetworks.com/analysis/articles/immunohistochemistry-techniques-strengths-limitations-and-applications-363107]
- 73. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 74. 免疫组化: 改善IHC 染色的概述+ 步骤 [https://www.leicabiosystems.com/zh/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 75. 免疫组织化学(IHC) 疑难排除指南和使用对照的重要性 [https://www.cellsignal.cn/learn-and-support/troubleshooting/ihc-troubleshooting-guide]
- 76. 如何解决背景染色问题:一抗滴定和洗涤技巧 [https://www.celnovte.com/zh-CN/news/how-to-troubleshoot-background-staining-primary-antibody-titration-washing-tricks/]
- 77. 酶免疫组织化学技术 [https://www.detaibio.com/topics/enzyme-immunohistochemistry-technique.html]
- 78. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopdO0mT4yIvPncEYamW6lCw6e9jmGuCCRxgNp2mNN2GtjE_yMom]
- 79. Assay Substrate Selection Guide [https://www.rockland.com/resources/assay-substrate-selection-guide/?srsltid=AfmBOopJRZ28QcqpzpgpW5fMUfmZJDKg9KBjsY5Y9EGYwMdAdPro1Gad]
- 80. The Differences between ECL,NBT/BCIP and DAB [https://www.yacooscience.com/blog/the-differences-between-ecl-nbt-bcip-and-dab_b15]
- 81. Getting To The Specifics: Blocking For Immunohistochemistry [https://vectorlabs.com/blog/blocking-for-immunohistochemistry/?srsltid=AfmBOoo_fK_Ou2acUb8YM0dzCzTnnEQUTJ1xiB1eUi35cs1CjAoPXWlg]
- 82. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOor5tmRIyGZCg1ILTI1id-UoRnznmjLHgQ9X7auZvd5vIc7lYxCx]
- 83. Immunohistochemistry Troubleshooting Guide [https://www.rndsystems.com/resources/technical/immunohistochemistry-troubleshooting-guide]
- 84. IHC Staining | Antibodies Inc. [https://www.antibodiesinc.com/pages/ihc-staining?srsltid=AfmBOorOp2vO6tCQQ_pWzYfSs-tN2eDCVza2xwe_JQKxd2Zms2J11bW_]
- 85. Blocking endogenous peroxidases: a cautionary note for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4401301/]
- 86. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopY7DshcDhTsXVjm8gRwtKHmdBN3-BaYfxojSCJXmU4kul0Z2-c]
- 87. 6 Essential IHC Controls for Reliable Staining Results [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know?srsltid=AfmBOooDqEZG1he42K0stloKPGbC87ZT06wj-f5JSVVisuM3dBA57Qcc]
- 88. External Quality Assurance in Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC2931078/]
- 89. A Simple Guide To Immunohistochemistry Substrate ... [https://vectorlabs.com/blog/simple-ihc-substrate-selection/?srsltid=AfmBOooF7Nz6bYj2qbE1LLDHEPnM7aePUxDj03yGOt-OJD31xRHpkzgv]