Immunochemistry Principles and Techniques: From Basic Concepts to Advanced Applications in Biomedical Research
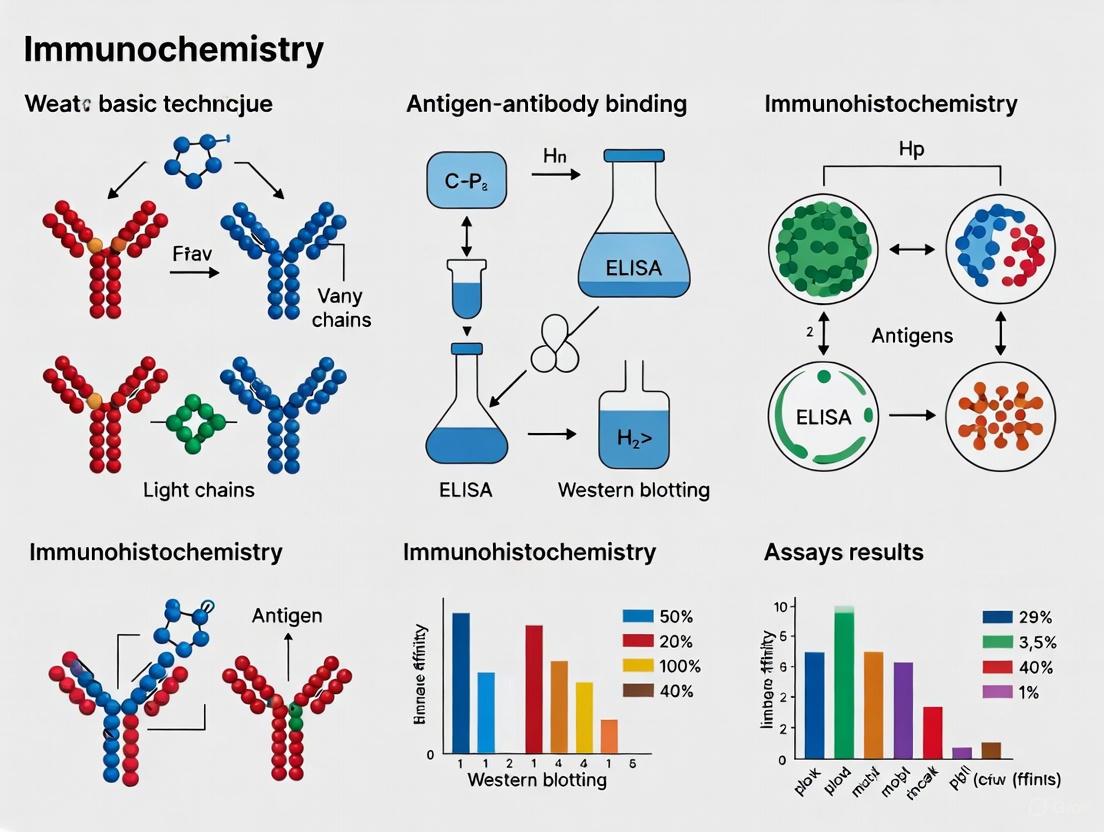
This article provides a comprehensive overview of immunochemistry, a cornerstone technique that combines anatomical, immunological, and biochemical principles to detect specific antigens within cells and tissues.
Immunochemistry Principles and Techniques: From Basic Concepts to Advanced Applications in Biomedical Research
Abstract
This article provides a comprehensive overview of immunochemistry, a cornerstone technique that combines anatomical, immunological, and biochemical principles to detect specific antigens within cells and tissues. Tailored for researchers, scientists, and drug development professionals, it covers the foundational concepts of antibody-antigen interactions, detailed methodological protocols for applications in disease diagnosis and drug development, practical troubleshooting for common issues, and rigorous standards for assay validation. By synthesizing current methodologies with emerging trends like artificial intelligence and multiplexed analysis, this guide serves as an essential resource for leveraging immunochemistry in both research and clinical settings.
Core Principles and Evolutionary Journey of Immunochemistry
Immunochemistry represents the interdisciplinary fusion of immunology, anatomy, and biochemistry, employing antibody-based techniques to detect and localize specific antigens within their anatomical context. This technical guide explores the core principles, methodologies, and applications of immunohistochemistry (IHC) as a quintessential immunochemical technique. We examine the complete workflow from tissue fixation to quantitative analysis, highlighting the critical convergence of disciplinary knowledge required for successful experimental outcomes. Recent advances in digital image analysis and automated quantification demonstrate the evolving sophistication of the field, offering enhanced reproducibility over traditional pathologist visual scoring. This whitepaper provides detailed protocols and resource guidance to support researchers in implementing robust immunochemical analyses for basic research and drug development applications.
Immunochemistry operates at the unique intersection of three fundamental biological disciplines. From immunology, it derives the exquisite specificity of antibody-antigen interactions. From anatomy, it incorporates the critical importance of structural and spatial context within tissues and cells. From biochemistry, it applies principles of molecular interactions, enzyme kinetics, and chemical staining reactions. This convergence enables the precise localization and quantification of specific molecules within their native morphological environment, providing insights that cannot be gleaned from techniques that homogenize tissues.
The foundational technique of immunohistochemistry (IHC) exemplifies this interdisciplinary approach. IHC exploits the specific recognition of an epitope by an antibody to visualize protein expression in situ while preserving the anatomical and structural features of a tissue sample [1]. First developed in the 1940s by Albert Coons, who created a fluorescein-labeled anti-pneumococcal antibody, the technique has evolved through numerous technical optimizations including enzyme-conjugated antibodies, antigen retrieval methods, and now digital quantification [2]. IHC's exceptional utility lies in its ability to bridge discovery research with clinical application, particularly in biomarker validation and cancer diagnostics [3] [4].
Core Principles and Methodological Framework
Antibody-Antigen Interactions: The Immunological Foundation
The specificity of immunochemical techniques stems from fundamental antibody-antigen interactions. Antibodies are immunoglobulins capable of binding specifically to a wide array of natural and synthetic antigens, including proteins, carbohydrates, and nucleic acids [5]. The strength of this interaction is defined by two key properties: affinity, referring to the thermodynamic energy of interaction between a single antibody-combining site and its corresponding epitope, and avidity, describing the overall binding strength including all combining sites on an antibody molecule [5].
Two principal types of antibodies are used in immunochemistry:
- Polyclonal antibodies: Heterogeneous mixtures derived from different B-cell clones, recognizing multiple epitopes on a target antigen.
- Monoclonal antibodies: Products of a single clone or plasma cell line, recognizing a single epitope with uniform specificity [5].
The antigen-to-antibody ratio significantly impacts complex formation, with optimal precipitation occurring at the equivalence zone where neither free antibody nor free antigen remains in solution [5].
Anatomical Preservation: Tissue Integrity and Architecture
Preservation of tissue architecture is paramount in immunochemistry, distinguishing it from solution-based immunoassays. Proper tissue fixation maintains anatomical relationships while preventing degradation. The choice of fixative represents a critical balance: under-fixed tissues may undergo proteolytic degradation, while over-fixed tissues can experience epitope masking through excessive cross-linking [2].
Common fixation approaches include:
- Formaldehyde-based fixatives: Create methylene cross-links between proteins, offering strong tissue penetration with relatively low background [2].
- Precipitative fixatives (e.g., methanol, ethanol): Cause protein precipitation by altering dielectric points but preserve cell morphology less effectively than cross-linking fixatives [2].
- Perfusion vs. immersion: Perfusion fixation through the vascular system allows rapid fixation of organs, while immersion fixation is suitable for smaller tissue specimens [2].
Following fixation, tissues are typically embedded in paraffin (FFPE) or optimal cutting temperature (OCT) compound for sectioning, preserving anatomical relationships for microscopic examination.
Biochemical Detection Systems: Signal Generation and Amplification
Detection methodologies in immunochemistry employ biochemical principles to generate measurable signals from antibody binding events. Two primary detection modalities are employed:
- Chromogenic detection: Utilizes enzyme-conjugated antibodies (e.g., horseradish peroxidase, alkaline phosphatase) that generate colored precipitates at the antigen site [6].
- Fluorescent detection: Employs fluorophore-conjugated antibodies directly visualized through fluorescence microscopy, enabling multiplexed detection of multiple targets [2].
Three principal method architectures govern antibody application:
- Direct method: Primary antibodies are directly labeled with fluorescent dyes or enzymes, shortening experimental time but potentially reducing signal [6].
- Indirect method: Unlabeled primary antibodies are detected using labeled secondary antibodies, providing signal amplification through multiple secondary antibodies binding to each primary [6].
- Amplification method: Incorporates additional amplification steps such as biotin-avidin complexes to enhance signal detection for low-abundance targets [6].
Experimental Workflow: From Tissue to Analysis
The following diagram illustrates the comprehensive workflow for immunohistochemical analysis of formalin-fixed, paraffin-embedded (FFPE) tissues, integrating critical steps from multiple disciplines:
Sample Preparation and Fixation Protocols
Proper sample preparation preserves anatomical context while maintaining biochemical antigenicity. For FFPE tissues, the following protocol is recommended [6] [1]:
- Fixation: Immerse tissue in 10% neutral buffered formalin (approximately 4% formaldehyde) for 2-24 hours at room temperature, depending on tissue size.
- Embedding: Process fixed tissues through graded ethanol series (70%-100%), clear in xylene, and infiltrate with molten paraffin at 56-58°C.
- Sectioning: Cut paraffin blocks into 4-5 μm sections using a microtome, float in a water bath, and mount on coated glass slides.
- Baking: Dry slides at 60°C for several hours to several days to enhance tissue adhesion.
Alternative approaches include frozen section preparation, where tissues are embedded in OCT compound and sectioned using a cryostat, preserving antigenicity but potentially compromising morphological detail.
Antigen Retrieval and Epitope unmasking
A critical advancement in immunochemistry, antigen retrieval techniques reverse formaldehyde-induced cross-links that mask epitopes. Two primary approaches are employed [6] [1]:
- Heat-Induced Epitope Retrieval (HIER): Incubate slides in citrate buffer (pH 6.0) or Tris-EDTA buffer (pH 9.0) using a microwave oven, water bath, pressure cooker, or autoclave. For microwave retrieval, heat for 10 minutes twice with a 5-minute cooling interval.
- Proteolytic-Induced Epitope Retrieval (PIER): Treat sections with proteinase K (5-20 μg/mL) or pepsin (0.1-0.5%) for 5-20 minutes at room temperature.
Optimization of antigen retrieval method, pH, temperature, and duration is essential for each antibody-epitope combination, as demonstrated by the variable performance of different retrieval methods with specific antibodies [1].
Immunostaining and Detection
The core immunodetection process requires precise optimization of conditions to maximize specific signal while minimizing background [1]:
- Blocking: Incubate sections with 0.5% BSA and 5% serum from the secondary antibody host species for 30 minutes at room temperature to reduce non-specific binding.
- Primary Antibody Incubation: Apply primary antibody diluted in blocking buffer for 1-2 hours at room temperature or overnight at 4°C. Optimal concentration must be determined empirically for each antibody.
- Secondary Antibody Incubation: Incubate with enzyme-conjugated or fluorophore-labeled secondary antibody for 1 hour at room temperature.
- Signal Development:
- For chromogenic detection: Incubate with DAB substrate for 3-10 minutes, monitoring development microscopically.
- For fluorescent detection: Protect from light and proceed to mounting.
Counterstaining, Mounting, and Visualization
Final processing steps contextualize specific staining within tissue morphology [6]:
- Counterstaining: Apply Mayer's hematoxylin for 5 minutes for nuclear staining, followed by bluing in running water for 20 minutes.
- Dehydration and Clearing: Process through graded ethanol series (80%-100%) and xylene.
- Mounting: Apply coverslip using xylene-based hydrophobic mounting medium for long-term preservation.
- Visualization: Image using brightfield microscopy (chromogenic) or fluorescence microscopy with appropriate filter sets.
Quantitative Analysis in Immunochemistry
Traditional pathologist visual scoring of IHC staining has limitations in subjectivity, cost, and generation of ordinal rather than continuous data [3] [4]. Digital image analysis approaches overcome these limitations through automated quantification.
Digital Image Analysis Versus Visual Scoring
A comparative study of 215 ovarian serous carcinoma specimens stained for S100A1 demonstrated strong correlation between digital analysis and pathologist scoring [3] [4]. The table below summarizes key quantitative comparisons:
Table 1: Quantitative Comparison of IHC Staining Assessment Methods
| Assessment Metric | Correlation Type | Correlation Coefficient | Statistical Significance |
|---|---|---|---|
| Percentage of Carcinoma with S100A1 Staining (%Pos) | Spearman | 0.88 | p < 0.0001 |
| Staining Intensity × Percentage Positive (OD*%Pos) | Spearman | 0.90 | p < 0.0001 |
The study utilized Genie Histology Pattern Recognition software for tissue classification and Color Deconvolution algorithms for stain separation, demonstrating that computer-aided methods can produce data highly similar to pathologist evaluation [4].
Automated Quantitative Analysis Algorithms
Recent advances employ deep learning techniques for precise cellular and subcellular quantification. A fully automated method combining CellViT nuclear segmentation with region-growing algorithms accurately quantifies nuclear, membrane, and cytoplasmic expression patterns in whole-slide images [7]. Optical density separation techniques differentiate hematoxylin and DAB staining components, enabling precise quantification of biomarker expression.
Essential Reagents and Research Solutions
Successful immunochemistry requires optimization of multiple reagent systems. The following table outlines key solutions and their functions in the experimental workflow:
Table 2: Essential Research Reagent Solutions for Immunochemistry
| Reagent Category | Specific Examples | Function | Optimization Considerations |
|---|---|---|---|
| Fixatives | 10% Neutral Buffered Formalin, 4% Paraformaldehyde | Preserve tissue architecture and antigenicity | Duration and temperature critical; overfixation masks epitopes |
| Antigen Retrieval Buffers | Citrate Buffer (pH 6.0), Tris-EDTA Buffer (pH 9.0) | Reverse formaldehyde cross-links | pH optimal for specific epitopes; heating method affects efficiency |
| Blocking Agents | BSA, Serum, Non-fat Dry Milk | Reduce non-specific antibody binding | Match serum species to secondary antibody host |
| Detection Systems | HRP-DAB, Alkaline Phosphatase-Fast Red | Generate visible signal from antibody binding | Enzyme inactivation essential for endogenous activity |
| Counterstains | Hematoxylin, Methyl Green | Provide anatomical context | Differentiation and bluing steps affect nuclear detail |
| Mounting Media | Xylene-based, Aqueous | Preserve staining and optimize microscopy | Match refractive index to microscopy method |
Applications in Research and Drug Development
Immunochemistry serves critical functions across biomedical research and therapeutic development:
- Biomarker Validation: IHC validates genomic discoveries through direct protein visualization in histologically relevant tissue regions, overcoming limitations of homogenization-based assays [4].
- Clinical Diagnostics: IHC identifies pathogenic features including neoplasia, metastasis, infection, and inflammation, with applications in companion diagnostic development [1].
- Therapeutic Target Verification: Spatial localization of drug targets within tissue microenvironments informs target engagement strategies and candidate selection.
- Tumor Microenvironment Analysis: Multiplexed IHC characterizes immune cell infiltration, stromal interactions, and cellular heterogeneity within tumors, guiding immunotherapy development [8].
Immunochemistry represents the essential convergence of immunology's specificity, anatomy's structural context, and biochemistry's detection principles. This interdisciplinary integration enables the precise spatial localization of biomolecules within their native tissue environments, providing insights inaccessible to reductionist approaches. As the field advances with automated quantification, multiplexed detection, and computational integration, immunochemical techniques will continue to expand their vital role in basic research, translational science, and therapeutic development. The continued refinement of standardized protocols and analytical frameworks will enhance reproducibility and quantitative rigor across applications.
Immunochemistry represents a cornerstone of modern biological science and therapeutic development, fundamentally reliant on the specific interaction between antibodies and antigens. This specific binding event serves as the foundational principle for a vast array of techniques essential for disease diagnosis, biomedical research, and drug development. Antibodies, also known as immunoglobulins, are large Y-shaped glycoproteins produced by B-cells as a primary immune defense, capable of specifically recognizing and binding unique molecular patterns on pathogens called antigens [9]. The exquisite specificity of this interaction enables researchers to detect single proteins within complex biological mixtures, localize biomarkers within tissues with microscopic precision, and quantify minute concentrations of analytes critical for assessing disease states.
The significance of antibody-antigen interactions extends far beyond basic research into clinical applications. Immunoassays form the basis for diagnosing infectious diseases, autoimmune disorders, and cancers, while also monitoring therapeutic drug levels and immune responses. In drug development, these principles are harnessed for target validation, pharmacokinetic studies, and the development of biologic therapies themselves, particularly monoclonal antibodies. The kinetics and affinity of these interactions directly influence assay sensitivity and therapeutic efficacy, making their thorough understanding paramount for professionals in these fields [10]. As biological therapies and precision medicine continue to advance, the principles governing antibody-antigen reactions remain fundamentally important for innovating new detection technologies and therapeutic strategies.
Structural and Biochemical Principles
Antibody Structure and Function
The characteristic Y-shaped antibody molecule consists of four polypeptide chains: two identical heavy chains and two identical light chains, stabilized by disulfide bonds [9]. These chains organize into distinct structural and functional domains:
- Variable regions (V) located at the amino-terminal ends of both heavy and light chains form the antigen-binding site (paratope). This region contains three hypervariable complementarity-determining regions (CDRs) that create the unique molecular surface complementary to the antigen's epitope.
- Constant regions (C) form the Fragment crystallizable (Fc) region and determine the antibody's isotype, which dictates its functional properties and interactions with other immune system components [9].
The antibody structure can be divided functionally into F(ab) and Fc regions. Proteolytic cleavage with enzymes like papain separates these domains: the F(ab) region contains the antigen-binding sites, while the Fc region mediates effector functions such as complement activation and binding to Fc receptors on immune cells [9]. This structural duality enables antibodies to simultaneously recognize specific antigens while recruiting immune responses, a feature exploited in many immunoassay designs.
Antigen Characteristics and Epitope Recognition
Antigens are substances that can elicit an immune response and be specifically recognized by antibodies or T-cell receptors. Effective antigens typically possess several key characteristics:
- Molecular complexity with areas of structural stability
- Minimal molecular weight of 8,000-10,000 Da, though haptens (small molecules) can become immunogenic when conjugated to carrier proteins
- Immunogenic amino acids such as lysine, arginine, glutamic acid, aspartic acid, glutamine, and asparagine in significant proportions [9]
The specific portion of the antigen recognized by an antibody is called an epitope. Epitopes can be classified as:
- Linear epitopes: consisting of a contiguous sequence of amino acids
- Conformational epitopes: formed by spatially adjacent amino acids from different regions of the antigen brought together by protein folding
The antibody-antigen interaction occurs between the paratope of the antibody and the epitope of the antigen, maintained by non-covalent forces including van der Waals interactions, hydrogen bonds, electrostatic attractions, and hydrophobic effects [9]. The strength of this interaction is defined by affinity (the binding strength between a single paratope-epitope pair) and avidity (the overall binding strength when multiple interactions occur simultaneously, as with multivalent antibodies like IgM).
Table 1: Antibody Isotypes and Their Functions
| Isotype | Heavy Chain | Structure | Molecular Weight (kDa) | Primary Functions and Locations |
|---|---|---|---|---|
| IgA | α | Monomer - tetramer | 150-600 | Mucosal immunity; found in gut, respiratory, urogenital tracts; secreted in milk |
| IgD | δ | Monomer | 150 | B cell receptor; function not fully defined |
| IgE | ε | Monomer | 190 | Allergy response; protection against parasitic worms |
| IgG | γ | Monomer | 150 | Most abundant in serum; provides majority of antibody-based immunity |
| IgM | μ | Pentamer | 900 | First response antibody; high avidity; B cell receptor |
Antigen Processing and Presentation
For T-cell dependent immune responses, the antibody-antigen reaction is preceded by critical processing and presentation steps. The immune system employs two major pathways for presenting antigenic peptides to T-cells:
- MHC Class I Pathway: Processes endogenous antigens (intracellular proteins from viruses or self-proteins). Proteins are degraded by the proteasome, transported into the endoplasmic reticulum by TAP transporters, and loaded onto MHC-I molecules for presentation to CD8+ T-cells [11].
- MHC Class II Pathway: Processes exogenous antigens (extracellular proteins). Antigens are internalized by antigen-presenting cells, degraded in increasingly acidic endosomal compartments, and loaded onto MHC-II molecules with the assistance of the invariant chain for presentation to CD4+ T-cells [12] [11].
These pathways ensure that protein antigens are appropriately processed into peptide fragments and presented in the context of MHC molecules to initiate and shape adaptive immune responses, ultimately leading to antibody production by B-cells.
Diagram 1: Antigen Processing and Presentation Pathways. The MHC Class I pathway processes intracellular antigens for CD8+ T-cell recognition, while the MHC Class II pathway processes extracellular antigens for CD4+ T-cell recognition.
Key Experimental Techniques and Methodologies
Enzyme-Linked Immunosorbent Assay (ELISA)
The Enzyme-Linked Immunosorbent Assay (ELISA) is a plate-based technique designed for detecting and quantifying soluble substances such as peptides, proteins, antibodies, and hormones [13]. In an ELISA, the antigen is immobilized on a solid surface (typically a polystyrene microplate) and complexed with an antibody linked to a reporter enzyme. Detection is accomplished by measuring the enzyme's activity via incubation with an appropriate substrate to produce a measurable product. The key steps in a standard ELISA protocol include:
- Coating: Direct or indirect immobilization of antigens to microplate wells
- Blocking: Addition of irrelevant protein to cover all unsaturated binding sites
- Probing: Incubation with antigen-specific antibodies
- Detection: Measurement of signal generated via enzyme-substrate reaction [13]
ELISA formats vary based on experimental needs:
- Direct ELISA: Uses a labeled primary antibody for detection; faster but less sensitive
- Indirect ELISA: Uses an unlabeled primary antibody followed by a labeled secondary antibody; offers signal amplification
- Sandwich ELISA: Employs two antibodies recognizing different epitopes on the target antigen; offers high specificity and sensitivity
- Competitive ELISA: Measures antigen concentration by detecting signal interference from competing labeled and unlabeled antigens; ideal for small antigens with single epitopes [13]
Table 2: Comparison of ELISA Formats
| Format | Sensitivity | Specificity | Steps | Time | Best Applications |
|---|---|---|---|---|---|
| Direct | Moderate | High | Fewest | Shortest | High-abundance targets; quick screens |
| Indirect | High | Moderate | More | Longer | General purpose; enhanced sensitivity |
| Sandwich | Highest | Highest | Most | Longest | Complex samples; low-abundance targets |
| Competitive | High | High | Moderate | Moderate | Small molecules; haptens |
Immunohistochemistry (IHC)
Immunohistochemistry (IHC) combines histological, immunological, and biochemical techniques to detect specific antigens in tissue sections, preserving spatial and morphological context [14] [15]. This technique is indispensable in pathology for disease diagnosis, classification, and prognostic assessment, particularly in oncology. The standard IHC protocol involves:
- Tissue Collection and Fixation: Tissues are typically fixed in 10% neutral-buffered formalin to preserve cellular morphology and antigenicity.
- Tissue Processing: Embedding in paraffin wax and sectioning into thin slices (4-6 μm) using a microtome.
- Deparaffinization and Rehydration: Removal of paraffin with xylene followed by rehydration through graded alcohol solutions.
- Antigen Retrieval: Application of heat-induced epitope retrieval (HIER) or enzymatic digestion to unmask antigenic sites obscured by formalin fixation.
- Blocking: Incubation with serum or BSA to prevent non-specific antibody binding.
- Antibody Incubation: Sequential incubation with primary antibody and enzyme-conjugated secondary antibody.
- Detection: Application of chromogenic substrate (e.g., DAB for horseradish peroxidase) to produce a colored precipitate at the antigen site.
- Counterstaining and Mounting: Application of hematoxylin to visualize cell nuclei followed by coverslipping for microscopic examination [14] [15].
Recent advances in IHC include multiplex immunohistochemistry, which allows simultaneous detection of multiple targets using different fluorophores, and the integration of digital pathology with AI-based image analysis to improve accuracy and consistency of interpretation [14].
Diagram 2: IHC Experimental Workflow. Key steps in immunohistochemistry from tissue preparation through analysis, highlighting critical antigen retrieval and detection phases.
Surface Plasmon Resonance (SPR) for Kinetic Analysis
Surface Plasmon Resonance (SPR) has emerged as a powerful label-free technique for real-time analysis of biomolecular interactions, particularly valuable for determining the kinetic parameters of antibody-antigen interactions [10]. Unlike endpoint assays like ELISA, SPR provides detailed information about association (k~on~) and dissociation (k~off~) rates, from which the equilibrium dissociation constant (K~D~) can be calculated. Recent advances have dramatically improved SPR throughput; for instance, the LSA instrument from Carterra Inc. can simultaneously measure 384 interactions, enabling high-throughput screening of antibody libraries [10].
A notable application of SPR in antibody engineering involves deep mutational scanning of complementarity-determining regions (CDRs) to optimize affinity and specificity. In one study, researchers performed alanine and tyrosine scanning mutagenesis of all CDR residues in an anti-human PD-1 antibody, followed by high-throughput SPR analysis against human and mouse PD-1 [10]. This approach identified specific mutations that enhanced affinity for mouse PD-1 by over 100-fold, demonstrating the power of data-driven antibody design.
Quantitative Analysis of Antibody Kinetics
Understanding the kinetic parameters of antibody-antigen interactions is crucial for both diagnostic and therapeutic applications. Recent longitudinal studies have mapped the kinetics of binding IgA and IgG antibodies against SARS-CoV-2 spike proteins following booster vaccination, revealing important insights into the duration of protection [16].
Table 3: Antibody Kinetic Parameters and Protection Against Infection
| Parameter | IgG (Wild-Type) | IgG (Omicron BA.1) | IgA (Wild-Type) | IgA (Omicron BA.1) |
|---|---|---|---|---|
| Peak Response | Day 28 post-booster | Day 28 post-booster | Day 28 post-booster | Day 28 post-booster |
| Waning Rate | Slower for mRNA-1273 | Faster for BNT162b2 | Slower for mRNA-1273 | Faster for BNT162b2 |
| Protection Correlation | High levels at day 28 associated with reduced infection risk (HR: 0.47) | Moderate correlation | Moderate correlation | High levels at day 28 associated with reduced infection risk (HR: 0.36) |
| Duration of Protection | ~155 days to maintain 80% protection at medium incidence | Shorter duration compared to WT | ~155 days to maintain 80% protection at medium incidence | Shorter duration compared to WT |
Key findings from longitudinal antibody studies include:
- Antibody responses wane more rapidly following Pfizer/BioNTech BNT162b2 booster compared to Moderna mRNA-1273 booster [16]
- Higher antibody levels at day 28 post-booster are associated with significantly reduced infection risk
- For BA.1 IgA, a response of at least 20% is needed to sustain 80% protection over 155 days post-booster at medium COVID-19 case incidence [16]
- Mathematical modeling of antibody kinetics can predict durations of protection and inform optimal booster timing
Validation and Quality Control
Antibody Validation Strategies
The reproducibility of research findings using antibody-based techniques depends critically on rigorous antibody validation. The International Working Group for Antibody Validation (IWGAV) has established guidelines to address concerns about antibody specificity and reproducibility [17]. Key validation strategies include:
- Genetic controls: Using knockout cells or tissues to confirm specificity
- Independent-epitope strategies: Employing antibodies targeting different regions of the same antigen
- Orthogonal methods: Verifying results with different methodological approaches
- Bioinformatic validation: Comparing expression patterns with existing databases [17]
For Western blotting, knockout validation is considered the gold standard, while for IHC, proper validation requires demonstration of specific staining patterns in tissues with known expression profiles [17]. Additional considerations include:
- Batch-to-batch variation: A significant source of irreproducibility, particularly with polyclonal antibodies
- Recombinant antibodies: Offer superior consistency compared to traditional hybridoma-derived antibodies
- Application-specific validation: Antibodies must be validated for each specific experimental context [17]
Controls and Standardization
Appropriate controls are essential for ensuring the validity of immunoassay results:
- Positive controls: Validate protocol success using cell lines or tissues known to express the target
- Negative controls: Assess background staining by omitting the primary antibody
- Biological controls: Include tissues with known expression patterns
- Standard reference materials: Enable inter-laboratory comparison and standardization [14]
In IHC, standardization efforts face challenges due to variability in tissue processing, antigen retrieval methods, and detection systems. Recent initiatives promoting automated staining platforms, digital pathology, and algorithm-assisted scoring are improving reproducibility across laboratories [14].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Antibody-Based Techniques
| Reagent/Category | Function | Examples/Formats | Application Notes |
|---|---|---|---|
| Primary Antibodies | Bind specifically to target antigen | Monoclonal, polyclonal, recombinant | Specificity validation critical; consider host species for multiplexing |
| Secondary Antibodies | Bind to primary antibodies; conjugated to detection moieties | Enzyme-linked, fluorescent, biotinylated | Must be specific for host species of primary antibody |
| Detection Enzymes | Catalyze signal generation from substrates | Horseradish peroxidase, Alkaline phosphatase | HRP offers higher sensitivity but can be inhibited by azide |
| Chromogenic Substrates | Produce colored precipitate upon enzyme catalysis | DAB (brown), AEC (red), NBT/BCIP (blue-purple) | DAB is most common; produces permanent stain |
| Fluorescent Dyes | Emit light upon excitation at specific wavelengths | FITC, TRITC, Alexa Fluor series | Enable multiplexing; require fluorescence microscope |
| Blocking Reagents | Reduce non-specific binding | BSA, non-fat dry milk, animal sera | Choice affects background; optimize for each application |
| Antigen Retrieval Reagents | Unmask epitopes obscured by fixation | Citrate buffer, EDTA, enzymes | Critical for FFPE tissues; heat-induced methods most common |
| Microplates | Solid phase for assay immobilization | 96-well, 384-well; high binding capacity | Polystyrene with protein binding capacity >400 ng/cm² recommended |
| Sensor Chips | Surface for immobilization in SPR | CM5, NTA, hydrogel-based | Different surfaces optimized for various biomolecules |
The antibody-antigen reaction remains the fundamental principle underlying numerous techniques essential to biomedical research and clinical diagnostics. From the basic structural principles governing this specific interaction to advanced applications in drug development and quantitative kinetic analysis, understanding these interactions enables researchers to design more sensitive, specific, and reproducible experiments. As technology advances, particularly in high-throughput screening, multiplex detection, and computational analysis, the field continues to evolve, offering ever more powerful tools to explore biological systems and develop novel therapeutics. However, these advances must be grounded in rigorous validation and quality control practices to ensure the reliability and reproducibility of the data generated. For researchers and drug development professionals, mastering both the fundamental principles and contemporary applications of antibody-antigen interactions remains essential for driving innovation in human health and disease treatment.
The evolution of immunostaining techniques represents a cornerstone of modern biomedical science, enabling researchers and clinicians to visualize specific molecular components within cells and tissues with exceptional precision. From its origins in the early 1940s, immunofluorescence (IF) has expanded into a sophisticated family of methodologies that bridge immunology, histology, and biochemistry [18] [19]. These techniques have become indispensable tools for both fundamental research and clinical diagnostics, particularly in the classification of neoplasms, diagnosis of immunobullous disorders, and understanding of complex cellular environments [18] [20]. This review traces the technical evolution from basic immunofluorescence to contemporary multiplexed imaging and artificial intelligence-driven approaches, framing these developments within the broader context of immunochemistry principles and their applications in research and therapeutic development.
Historical Development of Immunofluorescence
The conceptual foundation for immunofluorescence was established in 1941 by Albert Hewett Coons and his colleagues, who first constructed a fluorescein-isocyanate compound to visualize pneumococcal antigens in infected tissue [18] [21] [19]. This pioneering work demonstrated that antibodies could be tagged with fluorescent markers and used as specific histological stains, creating a new paradigm for antigen localization [19].
For approximately two decades, the field progressed gradually until a significant advance came in 1964, when Beutner and Jordon utilized indirect immunofluorescence (IIF) to detect antibodies in sera from patients with pemphigus vulgaris [18] [21]. This innovation amplified detection signals and expanded the technique's diagnostic utility. Around the same period, in 1963, researchers first described granular deposits of IgG and C3 along the dermo-epidermal junction in lupus erythematosus lesions, establishing immunofluorescence as a crucial diagnostic tool for autoimmune connective tissue diseases [18].
The subsequent development of complement binding indirect immunofluorescence further enhanced sensitivity by exploiting the amplification potential of complement activation. This three-step technique generates numerous C3 molecules at antigen-antibody binding sites, enabling detection even when few IgG or IgM antibodies bind to tissue antigens [18].
Core Immunofluorescence Techniques and Principles
Fundamental Principles
Immunofluorescence techniques share a common principle: exploiting the specific binding between antibodies and antigens to localize target molecules within biological samples, with detection enabled by fluorophore tags [19]. The specific region an antibody recognizes on an antigen is called an epitope, and antibodies differ in their binding affinity for these epitopes [19]. The conjugated fluorophore absorbs light at a specific shorter wavelength and emits it at a longer wavelength, producing detectable fluorescence when examined under appropriate microscopy systems [18] [19].
Direct Immunofluorescence (DIF)
Direct immunofluorescence is a one-step histological staining procedure that identifies in vivo antibodies bound to tissue antigens [18]. In this method, a single fluorophore-conjugated antibody directly binds to the target antigen [19]. The procedure involves obtaining tissue specimens (typically via punch biopsy), snap-freezing them, cutting frozen sections (4-6μm), and overlaying the sections with FITC-conjugated antibodies specific to immunoglobulins (IgG, IgM, IgA), complement components (C3), or fibrin [18].
The key advantage of DIF lies in its procedural simplicity and reduced non-specific background signal, as fewer processing steps minimize potential errors and antibody cross-reactivity [19]. However, its limitation includes potentially reduced sensitivity due to the limited number of fluorophore-labeled antibodies that can bind to each antigen [19].
Indirect Immunofluorescence (IIF)
Indirect immunofluorescence employs two types of antibodies: an unlabeled primary antibody that binds specifically to the target epitope, and a fluorophore-tagged secondary antibody that recognizes and binds to the primary antibody [18] [19]. This technique provides significant signal amplification because multiple secondary antibodies can bind to a single primary antibody, increasing the number of fluorophore molecules per antigen [19]. This enhanced sensitivity makes IIF particularly valuable for detecting low-abundance antigens and for serological studies identifying circulating antibodies in body fluids [18].
The standard IIF protocol involves incubating substrate sections with serial dilutions of the patient's serum, followed by application of FITC-conjugated anti-IgG or other antibody conjugates of defined specificity [18]. Appropriate positive and negative control sera must be tested simultaneously to ensure result validity [18].
Table 1: Comparison of Direct and Indirect Immunofluorescence Techniques
| Parameter | Direct Immunofluorescence (DIF) | Indirect Immunofluorescence (IIF) |
|---|---|---|
| Steps | One-step procedure | Two-step procedure |
| Antibodies Used | Single fluorophore-conjugated antibody | Primary unlabeled antibody + fluorophore-conjugated secondary antibody |
| Procedure Time | Shorter | Longer |
| Sensitivity | Lower | Higher due to signal amplification |
| Specificity | High | Potentially reduced due to additional step |
| Background Signal | Lower | Potentially higher |
| Flexibility | Limited | High (different secondary antibodies can be used with same primary) |
| Common Applications | Detecting in vivo antibody deposition in tissue | Detecting circulating antibodies in serum, research applications |
Specialized Immunofluorescence Variations
Several sophisticated IF variations have been developed to address specific diagnostic and research challenges:
Salt Split Technique: This method distinguishes between subepidermal blistering conditions with similar DIF findings by incubating normal human skin in 1M NaCl for 48-72 hours to split it at the lamina lucida level. Bullous pemphigoid antibodies bind to the roof (epidermal side) and floor (dermal side) of the split skin, while epidermolysis bullosa acquisita antibodies bind solely to the dermal side [18].
Antigenic Mapping: Used to differentiate between major forms of epidermolysis bullosa, this method involves creating a mechanically induced blister and performing indirect immunofluorescence with antibodies against different antigenic components of the dermal-epidermal junction (bullous pemphigoid antigen, laminin, type 4 collagen). The cleavage plane is determined by noting which antigens are detected on the roof versus the floor of the induced blisters [18].
Complement Indirect Immunofluorescence: This three-step technique increases detection sensitivity by exploiting complement activation. First, tissue sections are incubated with heat-inactivated serum to destroy complement-fixing activity. Sections are then treated with a complement source (fresh human serum), followed by fluorescein-labeled anti-human C3 antibodies. The method detects C3 molecules generated at antigen-antibody binding sites, providing enhanced sensitivity when minimal specific antibodies are present [18].
The Emergence and Evolution of Immunohistochemistry
While immunofluorescence revolutionized antigen detection, it faced limitations in routine clinical settings due to requirements for fluorescence microscopy and specialized expertise. This prompted the development of immunohistochemistry (IHC), which utilizes enzyme-substrate reactions (e.g., horseradish peroxidase or alkaline phosphatase) rather than fluorophores for signal detection [14] [21]. IHC offers the significant advantage of being viewable with standard light microscopy without specialized equipment [14].
The critical breakthrough for IHC came with the development of antigen retrieval (AR) methods by Shi et al., which reversed the cross-linking effects of formalin fixation and paraffin embedding, making epitopes more accessible to antibody binding [20]. This advancement dramatically expanded IHC applications to archived formalin-fixed paraffin-embedded (FFPE) tissue samples, which are easily stored and widely available in clinical settings [20].
Table 2: Evolution of Key Immunostaining Milestones
| Time Period | Technological Development | Significance |
|---|---|---|
| 1941 | First immunofluorescence by Coons et al. | Enabled specific antigen visualization in tissue |
| Early 1960s | Application to autoimmune skin diseases | Established diagnostic utility for immunobullous diseases |
| 1964 | Indirect immunofluorescence by Beutner and Jordon | Signal amplification for enhanced sensitivity |
| 1970s-1980s | Monoclonal antibody development | Increased specificity and reproducibility |
| 1990s | Antigen retrieval techniques | Enabled IHC on archived FFPE tissues |
| 2000s | Automated staining systems | Improved standardization and throughput |
| 2010s | Multiplex immunofluorescence | Simultaneous detection of multiple markers |
| 2020s | AI-powered image analysis and virtual staining | Enhanced quantification and prediction capabilities |
Modern Techniques and Current Status
Multiplex Immunofluorescence (mIF)
A paradigm shift in immunostaining occurred with the development of multiplex immunofluorescence, which enables simultaneous detection of numerous markers within a single tissue section [22] [23]. This capability is particularly valuable for analyzing complex cellular environments, such as the tumor microenvironment, where understanding spatial relationships between different cell types is crucial [22]. Technologies such as Co-Detection by Indexing (CODEX), cyclic immunofluorescence (CyCIF), and multiplexed immunohistochemistry (mIHC) now permit visualization of dozens of proteins simultaneously, providing unprecedented insights into cellular interactions and functional states [22] [23].
However, mIF presents substantial challenges, particularly technical variations in staining intensities arising from differences in tissue fixation, antibody concentrations, and imaging conditions [22]. These variations necessitate robust normalization procedures to ensure accurate biological interpretations across samples and batches.
Normalization and Standardization Approaches
Recent computational advances have addressed normalization challenges in multiplex imaging. The UniFORM pipeline represents a significant innovation—a non-parametric, Python-based method for normalizing multiplex tissue imaging data at both feature and pixel levels [22]. UniFORM employs automated rigid landmark registration tailored to the distributional characteristics of MTI data, aligning biologically invariant negative populations to remove technical variation while preserving tissue-specific expression patterns in positive populations [22]. Benchmarking across multiple platforms (CyCIF, ORION, COMET) demonstrates that UniFORM consistently outperforms existing methods in mitigating batch effects while maintaining biological signal fidelity [22].
Artificial Intelligence and Virtual Staining
The integration of artificial intelligence represents the current frontier in immunostaining technology. ROSIE (RObust in Silico Immunofluorescence from H&E images) is a deep-learning framework that computationally imputes the expression and localization of dozens of proteins from standard H&E images [23]. Trained on a massive dataset of over 1,300 tissue samples co-stained with H&E and CODEX (spanning over 16 million cells), ROSIE can predict 50 different biomarkers from H&E input alone [23]. This approach demonstrates particular utility in identifying immune cell subtypes like B cells and T cells that are not readily discernible with H&E staining alone, offering a powerful tool for enhancing standard histopathological practice without additional costly staining procedures [23].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Their Functions
| Reagent/Material | Function | Technical Notes |
|---|---|---|
| Primary Antibodies | Bind specifically to target antigens | Monoclonal (higher specificity) or polyclonal (higher sensitivity); require optimization of dilution [20] |
| Secondary Antibodies | Bind to primary antibodies; conjugated with fluorophores or enzymes | Enable signal amplification; must match host species of primary antibody [19] |
| Fluorophores | Emit light at specific wavelengths when excited | FITC, TRITC, Alexa Fluor series; choice depends on microscope filters and experimental design [18] [19] |
| Enzymatic Labels | Catalyze color-producing reactions | Horseradish peroxidase (HRP) or alkaline phosphatase (AP); used with chromogens like DAB [21] [20] |
| Fixatives | Preserve cellular structure and prevent degradation | Paraformaldehyde (PFA), methanol; choice affects epitope preservation [21] [20] |
| Antigen Retrieval Buffers | Reverse cross-linking from fixation | Citrate-based, EDTA, or commercial solutions; critical for FFPE tissues [20] |
| Blocking Reagents | Reduce non-specific antibody binding | BSA, normal serum, or commercial blockers; minimize background staining [21] [20] |
| Mounting Media | Preserve samples for microscopy | May include anti-fading agents for fluorescence; choice affects signal preservation [18] |
Experimental Protocols
Standard Direct Immunofluorescence Protocol
For detecting in vivo antibody deposition in skin diseases [18]:
- Sample Collection: Obtain perilesional skin via 3-5 mm punch biopsy or surgical biopsy.
- Preservation: Snap-freeze specimen immediately in liquid nitrogen or cold solid carbon dioxide. If delay occurs, keep in cold saline. Alternatively, use Michel's medium for transport at ambient temperature.
- Sectioning: Cut frozen 4-6μm sections using a cryostat and place on glass slides. Air-dry for 15 minutes.
- Staining: Rinse in phosphate-buffered saline (PBS), pH 7.2. Overlay slides in a moist chamber with FITC conjugates having specificities for anti-IgG, anti-IgM, anti-IgA, anti-C3, and anti-fibrin (testing each reagent on separate slides).
- Visualization: Rinse in PBS, mount in buffered glycerin, and examine under a fluorescence microscope.
Immunohistochemistry Protocol for FFPE Tissues
For detecting specific antigens in formalin-fixed paraffin-embedded tissues [20]:
- Slide Preparation: Section FFPE blocks at 4-7μm thickness, mount on adhesion-treated slides, and dry at 60°C for at least 2 hours (preferably overnight).
- Deparaffinization and Rehydration:
- Immerse slides in 3 changes of xylene (10 minutes each)
- Dip in graded alcohols sequentially (100%, 100%, 80%, to 70%)
- Immerse in deionized water
- Antigen Retrieval:
- Place slides in retrieval buffer (e.g., 10mM citrate)
- Heat using microwave oven (100°C for 5-10 minutes) or pressure cooker
- Cool slides for 15 minutes
- Blocking:
- Inhibit endogenous peroxidase with 3% hydrogen peroxide (5 minutes)
- Apply blocking reagent to decrease nonspecific background staining (e.g., Background Sniper)
- Antibody Incubation:
- Apply optimized concentration of primary antibody for appropriate duration
- Rinse and apply labeled secondary antibody (if using indirect method)
- Detection:
- Apply enzyme substrate (e.g., DAB for peroxidase)
- Counterstain with hematoxylin
- Dehydrate, clear, and mount for light microscopy
Visualization of Technique Evolution and Relationships
The journey from Coons' initial fluorescent antibody conjugates to contemporary multiplexed imaging and AI-powered virtual staining reflects a remarkable technological evolution in immunostaining. Throughout this progression, the fundamental principle has remained constant: exploiting the specific binding between antibodies and antigens to visualize molecular components within biological samples. What has evolved dramatically is the sensitivity, multiplexing capability, quantitative precision, and accessibility of these techniques. Current research focuses not only on developing new fluorophores and detection methods but also on computational approaches that extract unprecedented information from existing staining methods or even predict immunofluorescence patterns from standard H&E stains. As these technologies continue to advance, they will further bridge the gap between morphological observation and molecular characterization, enhancing both fundamental biological understanding and clinical diagnostic capabilities in anatomic pathology, drug development, and personalized medicine.
In the field of immunochemistry, antibodies are indispensable tools for detecting, quantifying, and localizing specific antigens within biological samples. These reagents form the foundation of numerous diagnostic and research applications, from basic science to drug development. Antibodies are broadly classified into two categories based on their origin and specificity: polyclonal antibodies (pAbs), a heterogeneous mixture produced by multiple B-cell clones, and monoclonal antibodies (mAbs), a homogeneous population derived from a single B-cell clone [24] [25]. The strategic selection between these antibody types, along with appropriate labeling strategies, is critical for experimental success, influencing outcomes in techniques such as immunohistochemistry (IHC), immunofluorescence (IF), western blotting, and flow cytometry.
Immunohistochemistry, the most common immunostaining technique, perfectly exemplifies the importance of antibody choice. IHC amalgamates principles from histology, immunology, and biochemistry to precisely localize target antigens within tissue samples, offering a unique advantage over other molecular biology techniques by preserving spatial and morphological context [14]. This technical guide provides an in-depth comparison of monoclonal and polyclonal antibodies, details their production and labeling methodologies, and outlines their applications within modern research and therapeutic contexts, providing scientists with the knowledge to make informed reagent decisions.
Fundamental Differences Between Monoclonal and Polyclonal Antibodies
The core distinction between monoclonal and polyclonal antibodies lies in their specificity and heterogeneity. Polyclonal antibodies are produced by multiple different B cell lineages within an immunized host animal. They recognize a wide array of epitopes—distinct molecular regions—on a single target antigen. This results in a diverse mixture of antibody molecules with varying paratopes and affinities for the antigen [24] [25]. In contrast, monoclonal antibodies originate from a single, immortalized B cell clone. Consequently, every mAb molecule is identical, exhibiting uniform structure and unparalleled specificity for a single, unique epitope on an antigen [24] [25].
This fundamental difference drives their respective strengths and weaknesses, making each type suitable for different experimental scenarios. The following table summarizes the key characteristics and comparative advantages of each antibody type.
Table 1: Key Characteristics of Monoclonal vs. Polyclonal Antibodies
| Characteristic | Monoclonal Antibodies (mAbs) | Polyclonal Antibodies (pAbs) |
|---|---|---|
| Origin | Single B cell clone [24] [25] | Multiple B cell clones [24] [25] |
| Epitope Specificity | Single, defined epitope [24] [25] | Multiple, different epitopes [24] |
| Specificity & Cross-Reactivity | High specificity; low cross-reactivity [24] | Broader specificity; increased potential for cross-reactivity [24] |
| Homogeneity & Batch Variability | Homogeneous population; minimal lot-to-lot variability [24] | Heterogeneous population; significant batch variability [24] |
| Typical Production Time | ~6 months (complex process) [24] | ~3 months (straightforward process) [24] |
| Development Cost | High [24] [25] | Low to moderate [24] [25] |
| Best Uses | Detecting specific antigens or single protein family members; assays requiring high consistency (e.g., flow cytometry, IF, diagnostics, therapeutics) [24] [25] | Detecting low-abundance targets, denatured proteins, or multiple isoforms; capturing antigen (e.g., immunoprecipitation); western blotting [24] |
Antibody Production Methodologies
Monoclonal Antibody Production via Hybridoma Technology
The production of monoclonal antibodies is a more complex and protracted process, with the classic method being hybridoma technology. The workflow begins with the immunization of a host animal, typically a mouse or rabbit, with the target antigen to elicit an immune response [24]. Once a sufficient immune response is mounted, B-cells are isolated from the animal's spleen. These B-cells are then fused with immortalized myeloma cells (cancerous B-cells) to create hybrid cells known as hybridomas [24]. This fusion step is critical, as it confers the B-cell's ability to produce a specific antibody with the myeloma cell's capacity for indefinite division.
The resulting pool of hybridomas is subsequently diluted and screened in a process called limiting dilution cloning to isolate single cells producing the antibody of desired specificity. Each selected hybridoma clone is then propagated, creating a stable and renewable source of genetically identical monoclonal antibodies [24]. These antibodies are secreted into the culture supernatant, from which they can be harvested and purified. For large-scale production, hybridomas can be injected into the peritoneal cavity of a mouse to produce antibody-rich ascites fluid [24].
Diagram 1: Monoclonal Antibody Production Workflow
Recombinant Monoclonal Antibodies
An advanced and increasingly prevalent method for mAb production bypasses hybridomas altogether, leveraging recombinant DNA technology. This involves cloning the genes encoding the variable regions of the antibody from B-cells and expressing them in controlled host systems, such as mammalian or microbial cells [24] [26]. Recombinant mAbs offer significant advantages, including superior batch-to-batch consistency, defined amino acid sequences, the potential for animal-free production, and the ability to be engineered for enhanced properties like humanization or altered effector functions [24] [27].
Polyclonal Antibody Production
The production of polyclonal antibodies is a more direct process. A host animal—such as a rabbit, goat, or sheep—is immunized with the target antigen following a scheduled protocol over several weeks [24] [25]. This triggers a natural immune response, activating multiple B-cell clones that each produce antibodies against different epitopes of the antigen. After the immunization period, the polyclonal antibodies are harvested by drawing blood and purifying the IgG fraction from the serum [24]. While faster and less expensive than mAb production, this method results in a heterogeneous antibody mixture with inherent batch-to-batch variability, as a new animal must be immunized for each production run [24].
Antibody Labeling Techniques and Kits
For detection in most experimental applications, antibodies must be conjugated to detectable labels, such as enzymes, fluorescent dyes, or other markers. The choice of labeling strategy profoundly impacts the sensitivity, specificity, and signal-to-noise ratio of an assay.
Conventional Labeling Methods
Traditional antibody labeling kits often rely on amine-reactive chemistry. These kits use reactive dyes that covalently bind to free lysine residues (primary amines) on the antibody molecule [28]. While effective, this is a non-site-specific method. Since antibodies contain multiple lysines, this can result in heterogeneous labeling, with dyes potentially attaching to the antigen-binding site (paratope) and impairing antibody affinity [28]. Examples of such kits include the Alexa Fluor Antibody Labeling Kits and Zip Rapid Antibody Labeling Kits, which offer protocols ranging from 15 to 60 minutes [28].
Site-Specific Labeling Methods
To overcome the limitations of conventional chemistry, advanced site-specific labeling methods have been developed. A prominent example is the SiteClick Antibody Labeling Kit [28]. This technology targets the carbohydrate groups located on the Fc region of the antibody heavy chain, well away from the antigen-binding sites. It uses a copper-free click chemistry reaction to attach labels specifically to this site [28]. This approach ensures uniform labeling, preserves antigen-binding affinity, and produces highly consistent conjugates. The trade-off is a longer protocol time, typically 6 to 18 hours, but it yields superior reagents for sensitive applications [28].
Table 2: Comparison of Common Antibody Labeling Kit Types
| Kit Type / Characteristic | Zenon (Affinity) | Zip Rapid (Amine-Reactive) | SiteClick (Site-Specific) |
|---|---|---|---|
| Label Target/Method | Fc portion of IgG / Antibody affinity [28] | Free lysines / Covalent amine-reactive chemistry [28] | Carbohydrates on IgG heavy chain / Click chemistry [28] |
| Protocol Time | ~5 minutes [28] | ~15 minutes [28] | 6-18 hours [28] |
| Site-Specific? | No [28] | No [28] | Yes [28] |
| Conjugate Storage | Not recommended (>24 hr) [28] | Yes [28] | Yes [28] |
| Requires Purification? | No [28] | No [28] | Yes (included) [28] |
| Optimal Applications | Rapid screening, IF, FC [28] | IF, FC, WB, HCA [28] | Highly sensitive IF, FC, HCA requiring minimal background [28] |
Applications in Research and Therapeutics
Research Applications: A Guide to Selection
The choice between monoclonal and polyclonal antibodies is dictated by the specific requirements of the experimental application.
- Immunohistochemistry (IHC): Both antibody types are widely used. Polyclonals are often preferred for detecting low-abundance targets due to their signal amplification from multiple epitope binding. Monoclonals are favored when high specificity is needed to distinguish between closely related protein isoforms, offering lower background staining [24] [14]. Rigorous validation using positive and negative controls is essential for reliable IHC results [14] [29].
- Western Blotting: Polyclonal antibodies are excellent for detecting denatured proteins, as they can bind multiple linear epitopes exposed upon protein denaturation. Monoclonals are ideal for confirming the identity of a specific band or when probing for post-translational modifications like phosphorylation [24].
- Flow Cytometry / Immunofluorescence (IF): Monoclonal antibodies are generally the gold standard. Their singular specificity results in clean staining with low background, which is crucial for accurately quantifying protein expression levels. The use of polyclonals in flow cytometry can lead to incorrect quantification due to signal amplification [24].
- Immunoprecipitation (IP): Polyclonal antibodies are superior for "pulling down" a target protein from a complex solution because their ability to bind multiple epitopes increases the efficiency of antigen capture [24].
Therapeutic and Diagnostic Applications
Monoclonal antibodies have revolutionized medicine, forming the backbone of precision medicine by targeting specific disease mechanisms.
- Oncology: mAbs like trastuzumab (targeting HER2) and pembrolizumab (a PD-1 immune checkpoint inhibitor) have transformed cancer treatment. Antibody-Drug Conjugates (ADCs), such as trastuzumab emtansine, combine the targeting ability of a mAb with the cell-killing power of a cytotoxic drug, delivering the payload directly to cancer cells [26] [30].
- Bispecific Antibodies: These engineered mAbs can engage two different targets simultaneously. For example, some bispecifics physically bridge T-cells with cancer cells to induce a targeted immune attack, creating novel therapeutic mechanisms [26].
- Autoimmune & Infectious Diseases: mAbs like adalimumab are used to modulate immune responses in rheumatoid arthritis, while others like sipavibart provide passive immunity against pathogens such as SARS-CoV-2 for immunocompromised individuals [30].
- Neurological Disorders: mAbs like aducanumab and lecanemab target amyloid-beta plaques in Alzheimer's disease, representing a promising approach to slowing disease progression [30].
The Scientist's Toolkit: Essential Reagent Solutions
Successful immunochemistry experiments rely on a suite of core reagents and solutions beyond just the primary antibody.
Table 3: Essential Reagents for Immunochemistry Workflows
| Reagent / Solution | Function / Purpose |
|---|---|
| Primary Antibodies (mAb/pAb) | The key reagent that provides specificity by binding the target antigen [24]. |
| Labeled Secondary Antibodies | Enable detection by binding to the primary antibody and carrying a label (enzyme, fluorophore) [14]. |
| Blocking Buffers | Contain irrelevant proteins (e.g., BSA) to adsorb to non-specific sites, minimizing background staining [14] [29]. |
| Antigen Retrieval Solutions | Critical for IHC on FFPE tissues; reverse formaldehyde-induced cross-links to unmask hidden epitopes (e.g., Heat-Induced Epitope Retrieval) [14] [29]. |
| Fixatives | Preserve tissue architecture and prevent antigen degradation (e.g., formalin) [14] [29]. |
| Chromogenic Substrates | Enzymes (HRP, AP) on antibodies convert these substrates into an insoluble, colored precipitate for visualization [14]. |
| Detection Kits (e.g., Polymer-Based) | Multi-component systems that significantly amplify the detection signal, enhancing sensitivity [14] [29]. |
| Mounting Media | Preserve the stained sample under a coverslip for microscopy; may contain antifade agents for fluorescence [14]. |
The field of antibody technology is dynamic, with several key trends shaping its future. There is a marked shift from traditional monospecific mAbs toward more complex bispecific antibodies and antibody-drug conjugates (ADCs), which now constitute a significant portion of new approvals [26]. Concurrently, nanobodies—small, stable antibody fragments derived from camelids—are gaining traction for their superior tissue penetration and unique epitope recognition [26]. Underpinning all these advancements is the transformative role of Artificial Intelligence (AI) and Machine Learning, which are revolutionizing antibody discovery and engineering by predicting structures, optimizing properties, and generating novel candidates de novo, thereby dramatically reducing development timelines and costs [26] [30].
In conclusion, understanding the fundamental distinctions between monoclonal and polyclonal antibodies, along with their appropriate labeling strategies, is a cornerstone of experimental design in immunochemistry. Monoclonal antibodies offer unparalleled specificity and consistency, making them ideal for targeted therapies and quantitative assays. Polyclonal antibodies provide robust signal amplification and versatility, suited for antigen capture and detection of denatured targets. The ongoing innovation in antibody formats, production methods, and conjugation technologies promises to further empower researchers and clinicians, continuing to drive progress in biomedical science and personalized medicine.
Immunodetection methods form the cornerstone of modern biomedical research and diagnostic development. Among these, direct and indirect detection strategies represent two fundamental approaches, each with distinct advantages and limitations in sensitivity, simplicity, and application suitability. This technical review provides a comprehensive comparison of these methodologies, examining their underlying principles, procedural workflows, and performance characteristics. Within the framework of immunochemistry principles, we analyze how researchers and drug development professionals can strategically select between these methods based on experimental requirements, focusing specifically on their differential signal amplification capabilities and operational complexity. The article incorporates detailed experimental protocols, quantitative performance data, and practical implementation guidelines to facilitate optimal method selection for various research scenarios.
Immunodetection methodologies leverage the specific binding between antibodies and antigens to identify and quantify biological molecules of interest. These techniques have become indispensable tools in research laboratories, clinical diagnostics, and drug development pipelines. The fundamental distinction between direct and indirect detection approaches lies in the configuration of the detection system, particularly in how the signal-generating moiety is incorporated into the assay architecture [31] [32]. Direct detection methods utilize primary antibodies that are directly conjugated to a detection label (enzyme, fluorophore, etc.), while indirect methods employ an unlabeled primary antibody followed by a labeled secondary antibody that recognizes the primary antibody [33] [34].
The choice between these approaches significantly impacts multiple experimental parameters, including sensitivity, specificity, time requirements, and cost-effectiveness. Understanding the core principles and mechanistic differences between these methods is essential for optimizing experimental design in immunochemistry applications [35]. This review systematically examines both methodologies, providing a technical foundation for researchers to make informed decisions based on their specific project requirements, whether for basic research, assay development, or diagnostic applications.
Fundamental Principles and Methodologies
Core Principles of Direct Detection
Direct detection methods operate on a straightforward principle: a single incubation step with a primary antibody that is directly conjugated to a detection molecule [33]. This configuration creates a direct physical link between the antigen-binding site and the signal-generating moiety, resulting in a simplified experimental workflow. In this approach, the labeled primary antibody binds specifically to the target antigen, and the resulting complex can be immediately visualized or quantified without additional binding steps [34].
The conceptual simplicity of direct detection translates into several practical advantages. The method involves fewer procedural steps, reducing total hands-on time and potential sources of error [33]. With only one antibody required, there is minimal risk of cross-reactivity with non-target proteins, leading to reduced background signal in many applications [35]. Additionally, the streamlined protocol makes direct detection particularly suitable for multiplexing experiments, where multiple targets are detected simultaneously using different conjugated primary antibodies with distinct labels [33].
Core Principles of Indirect Detection
Indirect detection employs a two-tiered antibody system consisting of an unlabeled primary antibody that specifically binds the target antigen, followed by a labeled secondary antibody that recognizes the constant region of the primary antibody [35] [34]. This layered approach introduces a signal amplification mechanism absent in direct detection, as multiple secondary antibodies can bind to a single primary antibody, dramatically increasing the signal output [33].
The signal amplification inherent in indirect detection significantly enhances sensitivity, making it particularly advantageous for detecting low-abundance targets [34]. This methodology also offers greater flexibility and cost-effectiveness, as a single conjugated secondary antibody can be used with various primary antibodies from the same host species [33]. This universality reduces the need for multiple labeled primary antibodies, expanding experimental possibilities without proportionally increasing reagent costs [32]. The indirect approach does, however, introduce additional complexity to the experimental workflow and requires careful optimization to minimize non-specific binding [34].
Figure 1: Comparative Workflows of Direct and Indirect Detection Methods. Direct detection requires fewer steps with only primary antibody incubation, while indirect detection involves sequential primary and secondary antibody incubations with additional wash steps, providing signal amplification but increased complexity.
Comparative Analysis: Sensitivity and Simplicity
The strategic selection between direct and indirect detection methods requires careful consideration of their relative performance characteristics, particularly regarding sensitivity and operational simplicity. The table below summarizes the core advantages and disadvantages of each approach across multiple experimental parameters:
Table 1: Comprehensive Comparison of Direct and Indirect Detection Methods
| Parameter | Direct Detection | Indirect Detection |
|---|---|---|
| Sensitivity | Lower (limited signal amplification) | Higher (significant signal amplification via multiple secondary antibodies) [33] [34] |
| Simplicity | Higher (fewer steps, shorter protocols) [33] | Lower (additional incubation and wash steps required) [33] |
| Time Requirements | Shorter (single incubation step) [33] | Longer (multiple incubation steps) [33] [34] |
| Cost Considerations | Higher (conjugated primary antibodies more expensive) [33] | Lower (inexpensive secondary antibodies work with multiple primaries) [33] |
| Flexibility | Lower (each target requires specific conjugated primary) [34] | Higher (same secondary antibody works with multiple primaries from same host) [33] |
| Background Signal | Generally lower (fewer non-specific binding opportunities) [33] | Potentially higher (risk of secondary antibody cross-reactivity) [33] [34] |
| Multiplexing Capability | Simplified (minimal species cross-reactivity concerns) [33] | Complex (requires primary antibodies from different species) [33] |
| Antigen Conservation | Better (fewer processing steps) | Reduced (extended processing may affect antigen integrity) |
| Optimization Requirements | Lower (fewer variables to optimize) | Higher (both primary and secondary antibodies require optimization) |
The sensitivity advantage of indirect detection stems from its inherent signal amplification mechanism. Each primary antibody provides multiple epitopes for secondary antibody binding, with each secondary antibody typically carrying several reporter enzymes or fluorophores [35]. This multi-layer amplification can increase signal intensity by an order of magnitude or more compared to direct methods, making indirect detection particularly valuable when working with low-abundance targets or when maximal detection sensitivity is required [34].
Conversely, direct detection offers significant advantages in procedural simplicity and time efficiency. The single incubation step reduces total experimental time and minimizes potential error introduction [33]. The absence of secondary antibodies eliminates concerns about species cross-reactivity, which is particularly beneficial in multiplexing experiments where multiple protein targets are simultaneously detected using different conjugated primary antibodies [35]. This streamlined approach also typically yields lower background signal since fewer reagents are employed, reducing opportunities for non-specific binding [33].
Experimental Protocols and Methodologies
Detailed Protocol for Direct ELISA
The direct ELISA format provides a straightforward approach for antigen detection and quantification. The following protocol outlines the key steps for implementing this methodology:
Plate Coating: Dilute the antigen of interest in carbonate-bicarbonate buffer (50 mM, pH 9.6) to an appropriate concentration. Add 100 μL/well to a 96-well microtiter plate and incubate overnight at 4°C [31].
Blocking: Remove the coating solution and wash the plate three times with PBS-T (phosphate-buffered saline with 0.05% Tween-20). Add 200 μL/well of blocking buffer (typically 1-5% BSA or non-fat dry milk in PBS) and incubate for 1-2 hours at room temperature [31].
Primary Antibody Incubation: Prepare the enzyme-conjugated primary antibody in blocking buffer at the predetermined optimal dilution. Add 100 μL/well to the plate after washing three times with PBS-T. Incubate for 1-2 hours at room temperature [31] [34].
Signal Detection: Wash the plate three times with PBS-T. Add 100 μL/well of appropriate enzyme substrate. For horseradish peroxidase (HRP), use TMB substrate, which produces a blue color that turns yellow after stopping with acid. For alkaline phosphatase (AP), use pNPP substrate, which produces a yellow color [31].
Signal Measurement: Stop the reaction at the optimal time point (typically 15-30 minutes) by adding stop solution (e.g., 1M H₂SO₄ for TMB). Measure the absorbance at the appropriate wavelength (450 nm for TMB, 405 nm for pNPP) using a microplate reader [31].
Detailed Protocol for Indirect Immunofluorescence
Indirect immunofluorescence leverages the signal amplification properties of the indirect method for enhanced sensitivity in cellular localization studies:
Sample Preparation: Culture cells on sterile glass coverslips or use tissue cryosections. Fix samples with 4% paraformaldehyde in PBS for 15 minutes at room temperature. Permeabilize with 0.1% Triton X-100 in PBS for 10 minutes if intracellular targets are being detected [35].
Blocking: Incubate samples with blocking buffer (typically 1-5% BSA in PBS with 0.05% Tween-20) for 30-60 minutes at room temperature to reduce non-specific binding [35].
Primary Antibody Incubation: Dilute the unlabeled primary antibody in blocking buffer to the appropriate concentration. Apply to samples and incubate in a humidified chamber for 1-2 hours at room temperature or overnight at 4°C for enhanced specificity [35].
Secondary Antibody Incubation: Wash samples three times with PBS-T (5 minutes per wash). Apply fluorophore-conjugated secondary antibody (e.g., Alexa Fluor 488, Cy3) diluted in blocking buffer. Incubate for 45-60 minutes at room temperature in the dark [35].
Nuclear Counterstaining and Mounting: Wash samples three times with PBS-T. Optional: incubate with DAPI (1 μg/mL) for 5 minutes to stain nuclei. Wash with PBS and mount coverslips onto glass slides using antifade mounting medium [35].
Imaging and Analysis: Visualize using a fluorescence microscope with appropriate filter sets. Capture images using consistent exposure settings across experimental conditions for quantitative comparisons [35].
Detection Labels and Reagent Systems
The selection of appropriate detection labels is critical for optimizing both direct and indirect detection methodologies. Different labels offer distinct advantages depending on the specific application requirements and detection instrumentation available:
Table 2: Common Detection Labels and Their Applications
| Label Type | Examples | Primary Applications | Key Characteristics |
|---|---|---|---|
| Enzymatic | Horseradish Peroxidase (HRP), Alkaline Phosphatase (AP) | ELISA, Western Blot, Immunohistochemistry [31] [33] | Signal amplification through enzyme-substrate reaction, colorimetric or chemiluminescent detection [31] |
| Fluorescent | FITC, Alexa Fluor series, Cy dyes [35] | Immunofluorescence, Flow Cytometry, Fluorescent Western Blot [35] [33] | Direct signal detection, multiplexing capability, requires specific excitation/emission filters [35] |
| Biotin | Biotinylated antibodies | ELISA, Western Blot, Immunohistochemistry [33] | Secondary amplification with enzyme-streptavidin conjugates, extremely high sensitivity |
| Luminescent | Luciferase, Acridinium esters | High-sensitivity ELISA, Automated immunoassay systems [32] | Very high sensitivity, broad dynamic range, specialized instrumentation required |
Fluorescent labels warrant particular attention due to their versatility across multiple platforms. Traditional fluorophores like FITC provide cost-effective detection but are prone to photobleaching [35]. Newer synthetic dyes such as the Alexa Fluor series offer enhanced photostability and brighter fluorescence, making them preferable for quantitative applications and long-term imaging studies [35]. The Cy dye family (Cy3, Cy5, Cy7) provides strong brightness and excellent spectral separation, facilitating multiplex experiments [35].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of direct and indirect detection methodologies requires access to high-quality specialized reagents. The following table outlines essential components for establishing these techniques in the research laboratory:
Table 3: Essential Reagents for Immunodetection Methods
| Reagent Category | Specific Examples | Function and Application Notes |
|---|---|---|
| Solid Phase Matrices | 96-well microplates, glass slides | Provide surface for antigen or antibody immobilization [31] |
| Detection Enzymes | Horseradish Peroxidase, Alkaline Phosphatase | Catalyze substrate conversion to detectable signals [31] |
| Enzyme Substrates | TMB, pNPP, BCIP/NBT | Converted by detection enzymes to colored, fluorescent, or luminescent products [31] |
| Blocking Agents | BSA, non-fat dry milk, casein | Reduce non-specific binding to improve signal-to-noise ratio [31] |
| Wash Buffers | PBS-T, TBS-T | Remove unbound reagents while maintaining protein stability and binding [31] |
| Fluorophores | Alexa Fluor 488, Cy3, FITC | Enable fluorescent detection for microscopy and flow cytometry [35] [33] |
| Secondary Antibodies | Goat anti-mouse IgG, Donkey anti-rabbit IgG | Species-specific antibodies for indirect detection [35] |
| Mounting Media | Antifade reagents with DAPI | Preserve samples for microscopy and provide nuclear counterstain [35] |
Applications in Research and Diagnostic Contexts
The strategic selection between direct and indirect detection methods varies significantly across different research and diagnostic applications, with each approach offering distinct advantages in specific contexts.
In diagnostic microbiology, direct detection methods are often preferred for rapid pathogen identification. The simplified workflow and reduced assay time facilitate quicker turnaround, while the minimized cross-reactivity enhances test specificity [31]. These characteristics make direct methods particularly valuable in clinical settings where speed and reliability are paramount. The application of direct fluorescent antibody labeling for detecting bacteria or viruses exemplifies this approach, providing specific identification with minimal processing time [35].
In contrast, research applications requiring maximal sensitivity often employ indirect detection methods. The signal amplification inherent in indirect systems enables detection of low-abundance targets that might otherwise remain undetectable [34]. This enhanced sensitivity is particularly crucial in biomarker discovery, analysis of limited samples, and detection of weakly expressed proteins. Additionally, the cost-effectiveness of indirect methods benefits research laboratories screening multiple targets, as a single conjugated secondary antibody can be used with numerous primary antibodies [33].
Quantitative immunohistochemistry represents a specialized application where detection method selection significantly impacts data quality. Studies comparing different detection approaches have demonstrated that enzyme-based methods with appropriate substrates (e.g., Vector Red for alkaline phosphatase) provide excellent linearity and quantification capabilities [36]. The enhanced sensitivity of indirect detection is particularly valuable when staining low-abundance biomarkers, while the simplified direct approach may suffice for highly expressed targets [37].
Advanced multiplexing applications present unique challenges that influence detection method selection. Direct detection's minimal species cross-reactivity simplifies experimental design when simultaneously detecting multiple targets [33]. However, the limited availability of directly conjugated primary antibodies can constrain panel development. Indirect methods offer greater flexibility in antibody selection but require careful planning to avoid cross-reactivity between secondary antibodies [35]. Recent advancements in mass cytometry and oligonucleotide-labeled antibodies have expanded multiplexing capabilities beyond traditional fluorescence-based detection [33].
Figure 2: Application-Based Selection Guide for Detection Methods. The choice between direct and indirect detection should be guided by specific application requirements, with direct methods favoring speed and simplicity and indirect methods providing enhanced sensitivity and cost-efficiency for appropriate applications.
The comparative analysis of direct and indirect detection methods reveals a consistent trade-off between sensitivity and simplicity that researchers must navigate based on their specific experimental requirements. Direct detection methods offer streamlined workflows, reduced background signal, and simplified multiplexing capabilities, making them ideal for applications involving high-abundance targets, rapid diagnostics, and situations where species cross-reactivity presents significant concerns [33] [34]. Conversely, indirect detection methods provide substantial signal amplification, enhanced sensitivity for low-abundance targets, and greater cost-effectiveness through reagent flexibility [33] [34].
The strategic selection between these approaches should be guided by careful consideration of multiple factors, including target abundance, required detection sensitivity, available experimental time, and resource constraints. As immunoassay technologies continue to evolve, with emerging platforms including digital ELISA and advanced multiplexing systems, the fundamental principles governing direct and indirect detection remain relevant [32]. Understanding these core methodologies provides researchers and drug development professionals with a solid foundation for selecting, optimizing, and implementing immunodetection strategies across diverse applications, from basic research to clinical diagnostic development.
Step-by-Step Protocols and Diverse Applications in Research and Diagnostics
In the study of disease mechanisms and the development of new therapeutics, the integrity of research data is fundamentally rooted in the quality of the starting biological samples. For researchers and drug development professionals, the pre-analytical phase—encompassing tissue collection, fixation, and embedding—represents a critical juncture that dictates the success of downstream applications, particularly in immunochemistry. The choices made during these initial steps directly influence the preservation of tissue morphology, the accessibility of antigenic epitopes, and the integrity of nucleic acids and labile proteins.
Two principal methodologies dominate tissue preservation for pathological and research purposes: Formalin-Fixed Paraffin-Embedding (FFPE) and cryopreservation (Frozen Sections). The FFPE process involves stabilizing tissue with formalin followed by embedding in a solid paraffin wax block, a method that has served as the historical gold standard for pathological archives [38]. In contrast, frozen section methodology relies on the rapid cooling of tissue to ultra-low temperatures to suspend biological activity and preserve biomolecules in a near-native state [39]. Within the context of a broader thesis on immunochemistry principles, understanding the technical nuances, advantages, and limitations of these two pathways is not merely procedural but foundational to ensuring that the resulting data accurately reflects the in vivo biological reality.
FFPE Tissue Preparation: A Standardized Workflow for Morphological Preservation
The creation of FFPE tissue blocks is a multi-stage process designed to permanently stabilize tissue architecture for long-term storage and sectioning.
Key Steps in FFPE Processing
The transformation of fresh tissue into a stable FFPE block follows a sequential protocol that must be meticulously executed to optimize sample quality [40]:
- Tissue Collection: Fresh tissue is obtained via biopsy or resection. Careful handling is essential to prevent mechanical damage or autolysis, which can compromise morphology and antigenicity. The interval between resection and fixation (cold ischemia time) should be minimized [14].
- Fixation: The tissue is immersed in a fixative, most commonly 10% Neutral Buffered Formalin [14] [41]. Formalin works by forming covalent methylene bridges between proteins, effectively cross-linking them and hardening the tissue. Fixation times typically range from 6 to 24 hours, depending on tissue size, to ensure complete penetration [40]. Under-fixation can lead to poor morphological preservation, while over-fixation can excessively mask antigenic sites, making subsequent antibody binding difficult [14].
- Dehydration: Following fixation, the water within the tissue must be removed. This is achieved by immersing the tissue through a series of ethanol solutions of increasing concentration (e.g., 70%, 90%, 100%) [40].
- Clearing: A clearing agent, such as xylene, is used to displace the ethanol. This step is crucial because ethanol is not miscible with paraffin wax. Xylene renders the tissue transparent, indicating successful clearing [40].
- Infiltration and Embedding: The cleared tissue is infiltrated with molten paraffin wax (around 60°C) under vacuum to ensure complete penetration. The tissue is then positioned in a mold, covered with fresh wax, and cooled to form a solid block [38] [40].
- Sectioning: The solidified FFPE block is thinly sectioned (typically 4–6 μm thick) using a microtome. The resulting ribbons of paraffin-containing tissue are floated on a water bath and mounted on glass slides for subsequent staining and analysis [42].
Consequences of Formalin Fixation on Biomolecules
While excellent for preserving structure, formalin fixation introduces significant chemical modifications to biomolecules, which poses challenges for downstream analysis [43].
- Proteins: Formaldehyde leads to protein denaturation and the formation of protein-protein cross-links. This can alter or obscure antibody-binding sites (epitopes), often necessitating an antigen retrieval step during immunostaining to reverse these cross-links [38] [41].
- Nucleic Acids: Formalin fixation accelerates DNA and RNA fragmentation [38]. It also induces chemical alterations such as cytosine deamination (leading to C>T/G>A artifacts in sequencing) and the formation of apurinic/apyrimidinic (AP) sites, which can compromise the accuracy of genetic analysis like PCR and Next-Generation Sequencing (NGS) [43].
The following diagram illustrates the complete FFPE tissue processing workflow and the major biomolecule alterations caused by formalin fixation.
Frozen Tissue Preparation: Preserving Native Molecular State
The frozen tissue pathway prioritizes the preservation of biomolecules in their native, biologically active state through rapid physical stabilization by freezing.
Key Steps in Frozen Tissue Processing
The protocol for frozen tissue preparation is generally faster than FFPE but requires immediate processing and continuous temperature control [41] [42]:
- Tissue Collection and Immediate Processing: Immediately after resection, the tissue must be processed to prevent degradation. RNA and proteins are particularly susceptible to rapid degradation at room temperature [38] [39].
- Stabilization (Optional Fixation): Tissues can be processed as either "fresh frozen" or "fixed frozen." For fresh frozen, the tissue is frozen without prior chemical fixation. For fixed frozen, tissue may be briefly immersed in a fixative like acetone or ethanol before freezing, or fixed after sectioning [41] [44].
- Snap-Freezing and Embedding: To preserve morphology and avoid ice crystal formation, the tissue is "snap-frozen". This is optimally done by immersing the specimen in a cold cryoprotective medium like O.C.T. (Optimal Cutting Temperature compound) and then submerging it in a pre-cooled slurry of isopentane in liquid nitrogen [41]. Slow freezing leads to the formation of large ice crystals that disrupt cellular membranes and compromise tissue architecture.
- Storage: Frozen tissue blocks are stored at -80°C or lower to maintain stability. Long-term storage in liquid nitrogen is also an option [38].
- Sectioning: Sections are cut using a cryostat, which is a microtome housed in a freezing chamber (typically -20°C). The sections are then mounted on slides and may be fixed briefly with cold acetone or ethanol before staining [41] [42].
Advantages for Molecular and Functional Studies
The frozen tissue method excels in preserving molecules for functional and molecular analyses:
- Proteins: Proteins are preserved in their native, non-denatured state, maintaining their biological activity and authentic antibody-binding epitopes. This often eliminates the need for antigen retrieval and provides more reliable results for immunohistochemistry (IHC), western blot, and mass spectrometry [38] [39].
- Nucleic Acids: DNA and RNA are preserved with high integrity and minimal chemical modifications, making frozen tissue the preferred source for high-quality genomic, transcriptomic, and next-generation sequencing applications [38] [39].
The workflow for frozen tissue processing, highlighting the critical snap-freezing step, is summarized below.
Comparative Analysis: FFPE vs. Frozen Sections
Selecting the appropriate tissue preservation method requires a balanced consideration of research objectives, logistical constraints, and the required quality of downstream data. The table below provides a direct comparison of FFPE and Frozen tissues across key parameters.
Table 1: Comprehensive comparison of FFPE and Frozen tissue sections
| Parameter | FFPE Sections | Frozen Sections |
|---|---|---|
| Tissue Morphology | Excellent preservation of cellular and tissue architecture [38] [41] | Moderate to good; can be compromised by freezing artifacts (ice crystals) [41] [42] |
| Biomolecule Integrity | Proteins: Denatured and cross-linked [38].Nucleic Acids: Fragmented and chemically modified [43] | Proteins: Native state, functionally active [38] [39].Nucleic Acids: High integrity, minimal alterations [38] [39] |
| Long-term Storage | Years to decades at room temperature; cost-effective and space-efficient [38] [42] | Years at -80°C or in liquid nitrogen; requires reliable equipment, vulnerable to power failures [38] [42] |
| Immunochemistry (IHC/IF) | Requires antigen retrieval to unmask epitopes [14] [41]. Well-established for diagnostic markers. | Often no antigen retrieval needed; superior for many research antibodies, especially phosphorylation-specific antibodies [41] |
| Downstream Applications | Ideal for routine histology, diagnostic IHC, and retrospective studies [38] [44] | Essential for RNA/DNA sequencing, mass spectrometry, western blot, enzyme histochemistry [38] [39] [44] |
| Cost & Logistics | Low ongoing storage costs; easy to transport [38] [39] | High equipment and maintenance costs; complex and expensive shipping [38] |
| Processing Time | Laborious and time-consuming (days) [38] [40] | Rapid (minutes to hours) [42] |
Essential Research Reagent Solutions
The execution of tissue processing and subsequent immunochemistry relies on a suite of critical reagents and materials. The following table details key components and their functions in the pre-analytical workflow.
Table 2: Key reagents and materials for tissue processing and analysis
| Reagent/Material | Function | Application Context |
|---|---|---|
| 10% Neutral Buffered Formalin | Chemical fixative that cross-links proteins to preserve tissue morphology and prevent decay [14] [41] | Primary fixation for FFPE tissues |
| Paraffin Wax | Embedding medium that infiltrates tissue to provide structural support for thin-sectioning with a microtome [38] [40] | FFPE tissue block formation |
| O.C.T. Compound | Water-soluble embedding medium that supports tissue during cryostat sectioning and helps minimize freezing artifacts [41] | Frozen tissue embedding |
| Primary Antibodies | Bind specifically to target antigens (proteins) of interest within the tissue sample [14] [45] | Detection of specific biomarkers in IHC and IF |
| Enzyme-Conjugated Secondary Antibodies | Bind to primary antibodies and catalyze a colorimetric reaction (e.g., with HRP/DAB) for visualization under a light microscope [14] [15] | Chromogenic detection in IHC |
| Antigen Retrieval Solutions | Chemical or heat-based treatment to break methylene bridges and reverse formalin-induced cross-linking, unmasking epitopes [14] [42] | Essential pre-treatment for most IHC on FFPE tissue |
| Liquid Nitrogen & Isopentane | Ultra-cold cooling media for rapid snap-freezing of tissues to preserve biomolecular integrity and minimize ice crystal damage [41] | Preparation of high-quality frozen tissues |
The choice between FFPE and frozen tissue methodologies is not a matter of identifying a superior technique, but rather of selecting the most appropriate tool for a specific research question within the framework of immunochemistry. The decision matrix is clear: FFPE is unparalleled for long-term biobanking, morphological studies, and large-scale retrospective analyses where architectural detail is paramount. Conversely, frozen tissue is indispensable for probing the native state of biomolecules, enabling advanced genomic, proteomic, and functional analyses that require high-integrity DNA, RNA, and proteins.
Future developments in biomedical research are poised to further bridge the gap between these two methods. Advances in antigen retrieval techniques and DNA repair enzymes are continuously improving the utility of FFPE samples for molecular analyses [43]. Simultaneously, the integration of digital pathology and artificial intelligence (AI) is enhancing the quantitative analysis of IHC results from both sample types, reducing subjectivity and improving reproducibility [14]. Furthermore, the refinement of multiplex immunohistochemistry and immunofluorescence allows for the simultaneous detection of multiple targets on a single section, maximizing the information gained from precious samples [14] [45]. For the researcher, a thorough understanding of these critical pre-analytical steps ensures that the foundational material of their study is optimally prepared, thereby validating all subsequent data and conclusions in the pursuit of scientific and therapeutic breakthroughs.
The analysis of formalin-fixed, paraffin-embedded (FFPE) tissues represents the gold standard in pathological diagnosis and translational research, providing exceptional morphological preservation. However, formalin fixation creates methylene bridges that cross-link proteins, thereby masking antigenic epitopes and significantly diminishing immunohistochemistry (IHC) sensitivity [46] [47]. Antigen retrieval (AR) stands as a pivotal technical milestone that effectively reverses this cross-linking, enabling successful immunohistochemical staining on FFPE tissues and unlocking the vast potential of archival tissue collections for research and diagnostic purposes [46]. The development of AR techniques has effectively divided IHC for FFPE tissues into two distinct eras: pre-AR and post-AR, marking it as a fundamental breakthrough in morphological sciences [46]. This guide provides an in-depth examination of both heat-induced and enzymatic antigen retrieval methods, offering researchers and drug development professionals the technical knowledge required to optimize IHC outcomes through scientifically sound retrieval protocols.
The Science of Formalin Fixation and Epitope Masking
Formalin fixation preserves tissue architecture through a series of chemical reactions that initially form hydroxymethyl groups on proteins, which subsequently react over hours to days to establish stable methylene bridges (protein cross-links) [47]. These cross-links alter protein biochemistry and sterically hinder antibody access to epitopes, dramatically reducing immunoreactivity [48] [49]. Research investigating clinically relevant antibodies has revealed that those effective on FFPE tissues predominantly target linear epitopes—contiguous stretches of amino acids in the native protein [47]. The loss of immunoreactivity after formalin fixation appears to result primarily from steric hindrance caused by cross-linked proteins rather than irreversible destruction of the primary epitope structure [47]. This fundamental understanding explains why antigen retrieval methods, which disrupt these cross-links, can successfully restore immunoreactivity even after harsh fixation procedures.
The following diagram illustrates the molecular mechanism of formalin fixation and antigen retrieval:
Antigen Retrieval Methodologies
Heat-Induced Epitope Retrieval (HIER)
Heat-Induced Epitope Retrieval (HIER) represents the most widely adopted antigen retrieval approach, utilizing elevated temperatures to break formalin-induced cross-links [48] [50]. The technique involves heating tissue sections in specific buffer solutions, typically at temperatures ranging from 95°C to 120°C, using various heating devices including microwaves, pressure cookers, steamers, or water baths [48] [50]. The mechanism of HIER primarily involves protein denaturation and the breakdown of methylene bridges through thermal energy, effectively unmasking epitopes and restoring antibody accessibility [50]. The efficacy of HIER depends critically on multiple interdependent parameters: temperature, heating duration, heating method, and particularly the pH and composition of the retrieval buffer [48] [49].
Proteolytic-Induced Epitope Retrieval (PIER)
Proteolytic-Induced Epitope Retrieval (PIER) employs proteolytic enzymes such as trypsin, pepsin, proteinase K, or ficin to digest proteins surrounding the epitopes [50]. This method represents a gentler approach compared to HIER and may be preferable for certain delicate epitopes or fragile tissues [50]. The enzymatic treatment selectively breaks down specific protein structures, thereby exposing masked epitopes without requiring high temperatures [50]. However, PIER demands precise optimization of enzyme concentration, incubation temperature, and incubation time to achieve effective retrieval while avoiding excessive proteolysis that could damage both the antigen of interest and tissue morphology [50]. The success rate for restoring immunoreactivity with PIER is generally lower than with HIER, limiting its broad application [50].
Comparative Analysis of HIER and PIER Methods
Table 1: Comparison of Heat-Induced and Proteolytic Antigen Retrieval Methods
| Parameter | Heat-Induced Epitope Retrieval (HIER) | Proteolytic-Induced Epitope Retrieval (PIER) |
|---|---|---|
| Mechanism | Thermal energy breaks cross-links | Enzymatic digestion of surrounding proteins |
| Typical Applications | Broad range of antigens, especially nuclear proteins | Fragile tissues, specific challenging epitopes |
| Advantages | Broader efficacy for most antibodies, better morphology preservation | Less thermally disruptive, suitable for heat-sensitive targets |
| Disadvantages | Potential tissue damage from overheating, inadequate retrieval with suboptimal heating | Lower success rate, potential for destroying antigens and morphology |
| Critical Optimization Parameters | Buffer pH, temperature, heating duration, heating method | Enzyme concentration, incubation time, temperature |
Technical Implementation and Optimization
Buffer Selection for HIER
The pH and chemical composition of the retrieval buffer significantly influence HIER efficacy. Different antibodies demonstrate variable staining patterns in response to buffer pH, generally categorized as stable type (pH-insensitive), V type (effective at high and low pH but not intermediate), increasing type (improving with higher pH), and decreasing type (weakening with higher pH) [50]. Commonly used buffers include:
- Citrate-based buffers (pH ~6.0): Effectively preserve tissue morphology and work well for many cytoplasmic antigens [49] [50].
- EDTA-based buffers (pH ~8.0-9.0): Often provide superior results for nuclear antigens and over-fixed tissues, typically generating stronger staining intensity for most antibodies [49] [50].
- Tris-EDTA buffers (pH ~9.0): Particularly effective for challenging nuclear antigens [48] [50].
Table 2: Antigen Retrieval Buffer Selection Guide
| Buffer Type | Typical pH Range | Best Applications | Considerations |
|---|---|---|---|
| Citrate | 6.0 | Cytoplasmic antigens, general use | Excellent morphology preservation |
| EDTA | 8.0-9.0 | Nuclear antigens, over-fixed tissues | Higher staining intensity for most antibodies |
| Tris-EDTA | 9.0 | Challenging nuclear antigens | May increase section loss; requires charged slides |
| Glycine-HCl | 3.0-5.0 | Specific V-type pattern antigens | Limited general application |
Standard HIER Protocol Using Microwave Method
The following protocol provides a robust starting point for HIER optimization using microwave heating [50]:
Deparaffinization and Rehydration:
- Incubate slides in xylene or substitute (3 × 5 minutes)
- Transfer through graded ethanols: 100% (2 × 5 minutes), 90% (5 minutes), 70% (5 minutes)
- Rinse in distilled water (5 minutes)
Antigen Retrieval Solution Preparation:
- Prepare appropriate retrieval buffer (e.g., 1-10 mM citrate, EDTA, or Tris-EDTA)
- Pre-heat buffer in microwave-safe container using microwave until boiling
Heat-Induced Retrieval:
- Immerse slides in pre-heated antigen retrieval buffer
- Microwave at 95-100°C for 8-20 minutes (optimize according to antibody requirements)
- Maintain slides at sub-boiling temperature for additional 4-10 minutes
- Cool slides to room temperature in retrieval solution (approximately 20-30 minutes)
Post-Retrieval Processing:
- Rinse slides in phosphate-buffered saline (PBS) or Tris-buffered saline (TBS)
- Proceed with standard immunohistochemistry staining protocol
Alternative heating devices including pressure cookers, steamers, or water baths may achieve similar results with potentially more uniform heating [50] [51]. Pressure cookers are particularly effective for consistent temperature maintenance at approximately 120°C, while water baths provide precise temperature control at 95-98°C [51].
Standard PIER Protocol Using Trypsin
For antigens requiring enzymatic retrieval, the following protocol using trypsin provides a methodological foundation [50]:
Section Preparation:
- Deparaffinize and rehydrate slides as described in HIER protocol
- Rinse in distilled water
Enzyme Solution Preparation:
- Prepare 0.1% trypsin solution in appropriate buffer (calcium chloride in distilled water, pH 7.8)
- Preheat solution to 37°C
Enzymatic Retrieval:
- Pipette enzyme solution onto tissue sections
- Incubate in humidified chamber at 37°C for 10-30 minutes
- Optimal incubation time requires empirical determination for each antibody
Termination and Washing:
- Transfer slides to container with tap water to stop enzymatic reaction
- Rinse under running water for 3 minutes
- Proceed with standard immunohistochemistry staining
Advanced Applications and Future Directions
Antigen retrieval principles have expanded beyond conventional IHC to diverse applications including immunoelectron microscopy, in situ hybridization, TUNEL apoptosis assays, and flow cytometry [46]. Furthermore, AR-based methods now facilitate extraction of nucleic acids and proteins from FFPE tissues, enabling genomic and proteomic analysis of archival specimens [46]. The emerging field of quantitative IHC (qIHC) employs novel amplification systems that permit precise protein quantification directly in FFPE tissue through dot counting, providing superior detection limits compared to traditional IHC or even ELISA methods [52]. This quantitative approach, combined with AR principles, promises to advance personalized medicine through more accurate biomarker identification and measurement [46] [52].
The following workflow summarizes the strategic approach to antigen retrieval optimization:
The Scientist's Toolkit: Essential Reagents for Antigen Retrieval
Table 3: Key Research Reagent Solutions for Antigen Retrieval
| Reagent/Category | Function/Purpose | Examples/Types |
|---|---|---|
| Retrieval Buffers | Create appropriate chemical environment for epitope unmasking | Citrate (pH 6.0), EDTA (pH 8.0-9.0), Tris-EDTA (pH 9.0) |
| Heating Devices | Provide controlled thermal energy for HIER | Microwave, pressure cooker, steamer, water bath |
| Proteolytic Enzymes | Digest proteins surrounding epitopes for PIER | Trypsin, pepsin, proteinase K, ficin |
| Slide Coating | Ensure tissue adhesion during high-temperature processing | Charged slides, poly-L-lysine, APTS |
| Blocking Reagents | Reduce nonspecific background staining | Normal serum, protein blocks, biotin blocks |
| Detection Systems | Visualize antibody-antigen interactions | Polymer-based systems, avidin-biotin complexes |
Mastering antigen retrieval techniques is indispensable for modern immunohistochemistry on FFPE tissues. HIER generally represents the preferred initial approach due to its broad efficacy and minimal morphological disruption, while PIER provides a valuable alternative for specific challenging epitopes. Methodical optimization of retrieval conditions—including buffer pH, heating parameters, or enzyme concentrations—is essential for achieving robust, reproducible staining results. As IHC continues to evolve toward quantitative applications and expanded use of archival tissues in biomarker discovery, precisely controlled antigen retrieval will remain fundamental to extracting meaningful biological information from FFPE specimens, thereby advancing both diagnostic pathology and translational research initiatives.
Immunohistochemistry (IHC) is a cornerstone technique that combines the principles of immunology, histology, and biochemistry to detect specific antigens within tissue sections using labeled antibodies [14]. Its unique advantage over other protein detection methods lies in its ability to provide precise spatial localization of target antigens within the architectural context of tissue, making it indispensable for both research and clinical diagnostics [14] [45]. The fundamental principle of IHC relies on the highly specific binding of antibodies to their target antigens, which are then visualized through various detection systems [53] [14]. This protocol will focus on the critical post-sectioning stages of IHC for formalin-fixed, paraffin-embedded (FFPE) tissues, which preserve tissue morphology exceptionally well but require specific steps to overcome the protein cross-linking introduced by formalin fixation [53] [54].
Core Protocol Workflow
The following diagram illustrates the complete workflow for standard IHC processing of FFPE tissue sections, from deparaffinization through to visualization:
Materials and Reagents
Research Reagent Solutions
The following table details essential reagents required for executing the standard IHC protocol:
Table 1: Essential Reagents for IHC Protocol
| Reagent Category | Specific Examples | Function & Purpose |
|---|---|---|
| Deparaffinization Agents | Xylene, Xylene substitutes [53] [55] | Dissolves and removes paraffin wax from tissue sections |
| Rehydration Solvents | Ethanol series (100%, 95%, 85%, 75%, 50%) [53] [55] | Gradually hydrates tissue to prepare for aqueous-based solutions |
| Antigen Retrieval Buffers | Sodium Citrate (pH 6.0), Tris-EDTA (pH 9.0), EDTA (pH 8.0) [55] [54] | Breaks protein cross-links formed during fixation to expose epitopes |
| Blocking Solutions | Normal Serum (e.g., Goat), BSA (3-5%), Commercial Protein Blockers [54] [45] | Reduces non-specific antibody binding to minimize background |
| Endogenous Enzyme Blockers | Hydrogen Peroxide (H₂O₂), Peroxidase Suppressor [55] [54] | Quenches activity of endogenous enzymes that could react with chromogen |
| Primary Antibodies | Monoclonal or Polyclonal antibodies specific to target antigen [14] [29] | Binds specifically to the protein/epitope of interest |
| Detection Systems | Polymer-based systems, Avidin-Biotin Complex (ABC) [29] | Amplifies signal and enables visualization of antibody binding |
| Chromogen Substrates | DAB (3,3'-Diaminobenzidine), AEC, BCIP/NBT [55] | Produces a colored precipitate at the site of antigen-antibody complex |
| Counterstains | Hematoxylin, Nuclear Fast Red, DAPI [55] | Provides contrasting stain for tissue structures/nuclei |
| Mounting Media | Aqueous (for fluorescence), Organic (for chromogenic) [55] | Preserves stain and enables high-resolution microscopy |
Detailed Methodologies
Deparaffinization and Rehydration
Before immunostaining can begin, the paraffin wax used for embedding must be completely removed and tissues must be rehydrated to allow aqueous-based reagents to penetrate [53] [55]. Incomplete deparaffinization is a common source of staining failure and high background.
- Procedure:
- Incubate slides in xylene or a less hazardous alternative for 10-15 minutes [53].
- Transfer to a second fresh xylene bath for another 10-15 minutes [53].
- Rehydrate tissues through a graded series of ethanol baths to gradually introduce water:
- Rinse slides thoroughly in distilled or deionized water three times [53]. > Critical Note: From this step onward, do not allow the slides to dry out, as this causes irreversible protein denaturation and results in high, non-specific background staining [53].
Antigen Retrieval
Formalin fixation creates methylene bridges that cross-link proteins and mask epitopes, significantly reducing antibody binding. Antigen retrieval reverses this process and is essential for most FFPE IHC [53] [54].
Heat-Induced Epitope Retrieval (HIER) is the most common and generally recommended method [54].
- Buffers: 10 mM Sodium Citrate (pH 6.0) or Tris-EDTA (pH 9.0) [55] [54].
- Protocol: Place slides in pre-heated retrieval buffer and heat using a microwave, pressure cooker, or steamer. Maintain at 95-98°C for 15-20 minutes [55] [54].
- Cooling: After heating, cool the slides in the buffer at room temperature for 20-30 minutes before proceeding [55].
Protease-Induced Epitope Retrieval (PIER) is an enzymatic alternative used for specific targets.
Blocking and Antibody Incubation
This phase prepares the tissue for specific antibody binding while suppressing non-specific signals.
Endogenous Enzyme Blocking: If using an HRP-based detection system, incubate slides with 0.3-3% hydrogen peroxide in buffer for 15 minutes to quench endogenous peroxidase activity [55] [54]. For alkaline phosphatase (AP) systems, use an AP blocker.
Protein Blocking: Incubate tissues with a protein block for 30-60 minutes at room temperature to occupy non-specific binding sites [54]. Common blockers include 3-5% BSA, normal serum from the host species of the secondary antibody, or commercial protein blocking solutions [54] [45].
Primary Antibody Incubation:
- Dilute the antibody to the optimized concentration in an antibody diluent or blocking buffer.
- Apply to tissues and incubate in a humidified chamber to prevent evaporation.
- Incubation is typically performed overnight at 4°C for maximum specificity and signal, though shorter incubations (1-2 hours) at room temperature can be sufficient for some antibodies [55] [54].
Washing Steps: After primary incubation, wash slides three times for 5-10 minutes each with a wash buffer (e.g., PBS or TBS with a mild detergent like 0.025% Triton X-100) to remove unbound antibody [55] [45].
Detection System Application:
- For indirect methods, incubate with the appropriate secondary antibody (e.g., HRP- or AP-conjugated) for 1-2 hours at room temperature [55].
- Modern polymer-based systems, where multiple secondary antibodies and enzymes are linked to a polymer backbone, offer superior sensitivity and are now widely used [29].
- Wash thoroughly three times for 5-10 minutes after secondary antibody application [55].
Detection, Counterstaining, and Mounting
The final stages render the antibody-antigen complex visible and preserve the sample.
Chromogenic Detection:
- For HRP enzymes, incubate with DAB substrate for approximately 10 minutes, monitoring color development under a microscope [55]. DAB produces a brown, alcohol-insoluble precipitate.
- Stop the reaction by transferring slides to water.
Counterstaining:
Dehydration, Clearing, and Mounting:
- For DAB and other organic-solvent compatible chromogens, dehydrate tissues through a reverse ethanol series (50%, 75%, 95%, 100%) and clear in xylene [55].
- Mount under a coverslip using a permanent, organic mounting medium [55].
- For fluorescent signals, mount with an aqueous, anti-fade mounting medium to preserve fluorescence and prevent photobleaching [55] [45].
Quality Control and Troubleshooting
Robust IHC requires rigorous quality control. This includes running positive control tissues known to express the target antigen and negative controls (e.g., omission of the primary antibody or use of an isotype control) with every batch to validate staining specificity and assess background [14] [29].
Table 2: Common IHC Challenges and Optimization Strategies
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| High Background | Incomplete blocking, slides dried during processing, antibody concentration too high, insufficient washing [14] [45] | Optimize blocking serum and duration; ensure slides remain wet; titrate antibody; increase wash times/volume [45]. |
| Weak or No Signal | Over-fixation, insufficient antigen retrieval, low antibody titer or degraded antibody, incorrect retrieval buffer pH [53] [54] | Extend HIER time or try PIER; perform antibody titration; check antibody expiry; test different retrieval buffers (pH 6.0 vs 9.0) [54]. |
| Non-Specific Staining | Cross-reactivity of antibodies, over-digestion with protease [45] | Use highly validated antibodies; include appropriate negative controls; optimize PIER time and concentration [54] [45]. |
| Patchy/Uneven Staining | Inadequate coverage of tissue during antibody incubation, bubbles on tissue section [29] | Ensure sufficient volume of reagent covers entire tissue; use a humidified chamber to prevent evaporation. |
Concluding Remarks
Mastering the core steps of IHC—from effective deparaffinization and antigen retrieval to precise antibody incubation and stringent washing—is fundamental to generating reliable, high-quality data. As the field advances, techniques are becoming more standardized and quantitative, with growing integration of digital pathology and artificial intelligence for analysis [14] [56]. Furthermore, multiplex immunohistochemistry/immunofluorescence (mIHC/IF) is emerging as a powerful extension, allowing simultaneous visualization of multiple markers on a single tissue section to characterize complex cellular interactions and the tumor microenvironment [56]. Adherence to the detailed protocols and quality control measures outlined in this guide provides a solid foundation for both current research applications and future technological implementations.
Immunohistochemistry (IHC) is an indispensable technique that combines immunological, biochemical, and histological principles to detect specific antigens within tissue sections. Its unique advantage lies in its ability to provide spatial context for protein expression, which is not possible with techniques like western blotting or ELISA [14]. The visualization of antibody-antigen binding is achieved primarily through chromogenic or fluorescent detection systems, each with distinct characteristics and applications. The choice between these systems significantly impacts the sensitivity, resolution, multiplexing capability, and ultimate interpretation of experimental results [57] [58]. This technical guide provides an in-depth examination of both chromogenic (focusing on the widely used 3,3'-Diaminobenzidine or DAB) and fluorescent detection techniques, with particular emphasis on the critical role of counterstaining for morphological context.
Core Principles of IHC Detection
Direct vs. Indirect Detection
The fundamental detection methodologies in IHC are direct and indirect detection, which differ in their configuration and resultant signal amplification.
Direct Detection: In this method, the label—either an enzyme for chromogenic detection or a fluorophore for fluorescent detection—is conjugated directly to the primary antibody that binds the target antigen [59]. This approach involves fewer processing steps, reducing potential background and making it suitable for multi-labeling experiments. However, it offers relatively low signal amplification, making it best suited for detecting highly abundant antigens [59].
Indirect Detection: This more common method uses an unlabeled primary antibody, which is then detected by a labeled secondary antibody raised against the species of the primary antibody [58] [60]. The key advantage is significant signal amplification, as multiple secondary antibodies can bind to a single primary antibody [57] [58]. This makes indirect detection the preferred method for antigens with low to medium expression levels, though it may require additional optimization to manage background noise [59].
Table 1: Comparison of Direct and Indirect Detection Methods
| Feature | Direct Detection | Indirect Detection |
|---|---|---|
| Complexity | Fewer steps; simpler protocol [57] | More steps; requires secondary antibody [58] |
| Signal Amplification | Low; limited by primary antibody labeling [59] | High; multiple secondary antibodies bind per primary [57] [58] |
| Sensitivity | Suitable for highly expressed antigens [59] | Enhanced sensitivity for low-abundance targets [58] |
| Background | Generally lower | Potentially higher, requires optimization [59] |
| Multiplexing Potential | Good; minimizes species cross-reactivity [59] | Possible with careful host species selection [58] |
Signal Amplification Systems
For enhanced sensitivity, especially when using indirect detection, advanced signal amplification systems are often employed.
Avidin-Biotin Complex (ABC): This method utilizes a biotin-conjugated secondary antibody that links the primary antibody to an avidin-biotin-peroxidase complex [58]. The high affinity between avidin (which has four biotin-binding sites) and biotin allows for the formation of large complexes containing multiple copies of the reporter enzyme (e.g., HRP). This high enzyme-to-antibody ratio greatly increases sensitivity compared to methods where the enzyme is directly conjugated to the secondary antibody [58].
Labeled Streptavidin-Biotin (LSAB): Similar to the ABC method, the LSAB method uses a biotin-conjugated secondary antibody. However, it is linked to a streptavidin-peroxidase complex directly. The advantage of this approach is a smaller complex size compared to ABC, which facilitates better tissue penetration and can further enhance sensitivity [58].
Polymer-Based Methods: These systems feature multiple secondary antibodies and enzyme molecules (HRP or AP) linked to a polymer backbone. This design eliminates the need for a biotinylation step and offers the highest level of sensitivity and signal amplification among the common methods. It also reduces the number of procedural steps and avoids potential background from endogenous biotin [58].
The following diagram illustrates the key components and mechanisms of these detection systems.
Chromogenic Detection
The DAB Chromogen System
Chromogenic detection is one of the most established methods in IHC. It relies on enzymes conjugated to antibodies converting soluble substrates into insoluble, colored precipitates at the site of antigen expression [58]. The most common enzymatic labels are Horseradish Peroxidase (HRP) and Alkaline Phosphatase (AP) [59].
DAB is the most popular chromogen used with HRP. When HRP is present, it catalyzes the oxidation of DAB in the presence of hydrogen peroxide, resulting in a brown, alcohol- and xylene-insoluble precipitate at the antigen site [58]. DAB is favored for its longevity, resistance to fading when exposed to light, and compatibility with permanent mounting media, allowing slides to be stored for years [57] [58].
Multiplex Chromogenic IHC Protocol
Multiplexing with chromogenic detection allows for the visualization of multiple antigens on a single tissue section. The following protocol, adapted from a published method that can stain up to five consecutive antibodies per slide, details this process [61].
Before You Begin:
- Tissue Preparation: Fix tissues in 10% neutral buffered formalin (NBF) or 4% PFA for 12-24 hours at 4°C. The fixative volume should be 5-10 times the tissue volume. Post-fixation, process tissues through a graded ethanol series (70% to 100%), clear in xylene, and embed in paraffin wax. Cut sections at 4-5 μm thickness for optimal antibody penetration [61].
- Slide Storage: Air-dry mounted sections for 14-15 hours and then bake at 60°C for 1 hour. Use slides within 3 months to preserve antigenicity [61].
Staining Procedure (for the first antigen, e.g., CD206):
- Deparaffinization and Rehydration: Deparaffinize slides in xylene and rehydrate through a graded ethanol series to distilled water [61] [60].
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER) using a citrate-based unmasking solution (pH 6.0) in a pressure cooker or microwave to break protein cross-links formed during fixation [61] [60].
- Endogenous Peroxidase Blocking: Incubate slides with a 2% hydrogen peroxide solution in ethanol to quench endogenous peroxidase activity, reducing false-positive signals [61].
- Protein Blocking: Apply a protein block (e.g., BSA, normal serum, or commercial protein-free block) for 30 minutes to prevent non-specific antibody binding [60].
- Primary Antibody Incubation: Apply the first primary antibody (e.g., CD206, diluted in a suitable buffer like Emerald antibody diluent) and incubate. Optimal concentration and incubation time (e.g., overnight at 4°C or 1 hour at room temperature) should be determined by titration [61] [57].
- Polymer Detection: Incubate with an HRP-labeled polymer reagent (e.g., ImmPress anti-Rabbit) for 30 minutes. This step detects the bound primary antibody [61].
- Chromogen Development: Apply DAB chromogen substrate. Monitor the development of the brown precipitate under a microscope to avoid over-staining [61].
- Counterstaining (Initial): Lightly counterstain with hematoxylin to visualize nuclei. Differentiate in acid alcohol and blue in a suitable buffer [61].
Stripping and Reprobing (for subsequent antigens, e.g., PD-L1):
- Signal Stripping: To remove the primary-secondary antibody complexes from the first round, incubate the slide in a stripping buffer (e.g., 0.5 M Tris, 9% NaCl, 0.1% Tween 20, pH 8.4) at an elevated temperature (e.g., on a hot plate). This is a critical step to prevent cross-talk between markers [61].
- Validation of Stripping: Confirm the complete removal of the first signal by visualizing the slide under a microscope. The brown DAB precipitate should no longer be visible [61].
- Reprobing: Repeat steps 2-8 for the second primary antibody (e.g., PD-L1), omitting the initial deparaffinization and rehydration. A Fab fragment secondary antibody blocking step may be included before applying the second primary antibody to minimize cross-reactivity [61].
Finalization:
- Mounting: After all staining cycles are complete, dehydrate the tissue through a graded ethanol series, clear in xylene, and mount with a permanent mounting medium like DPX [61].
The entire workflow for a multiplex chromogenic IHC experiment is summarized below.
Fluorescent Detection
Principles of Immunofluorescence (IF)
Fluorescent detection relies on fluorophores—molecules that absorb light at a specific wavelength (excitation) and emit light at a longer, lower-energy wavelength (emission) [57]. Fluorophores can be conjugated directly to a primary antibody (direct IF) or, more commonly, to a secondary antibody that recognizes the primary (indirect IF) [60]. The indirect method is widely preferred due to its superior signal amplification, as multiple secondary antibodies can bind to a single primary antibody [57] [60].
Key Considerations for Immunofluorescence
- Fluorophore Selection: The choice of fluorophore is critical. Factors to consider include the available light sources and filters on your microscope, the fluorophore's extinction coefficient and quantum yield (brightness), and its susceptibility to photobleaching [60]. Common fluorophores include DyLight dyes, Alexa Fluor dyes, FITC, and TRITC [57] [60].
- Multiplexing: The narrow emission spectra of fluorophores enable the simultaneous detection of multiple antigens (multiplexing) [58]. For successful multiplex IF, select fluorophores with minimal spectral overlap. Primary antibodies should be raised in different host species to prevent cross-reactivity, and species-specific secondary antibodies should be used [57] [58].
- Signal Amplification: Similar to chromogenic IHC, sensitivity in fluorescent IHC can be enhanced using methods like the fluorophore-labeled Streptavidin-Biotin complex. In this approach, a biotinylated secondary antibody is used, which is then detected by fluorophore-conjugated streptavidin. Each streptavidin molecule can bind multiple biotin molecules, and each streptavidin can be conjugated to several fluorophores, resulting in significant signal amplification [57] [60].
- Photobleaching and Mounting: Fluorophores are susceptible to photobleaching (fading upon prolonged light exposure). To mitigate this, minimize light exposure during and after staining, and use an anti-fade mounting medium to preserve fluorescence. While properly mounted slides can retain signal for weeks or months, chromogenic stains offer superior long-term stability, often lasting for years [57] [60].
Counterstaining in IHC
The Role of Counterstains
Counterstains are dyes applied after the primary IHC staining to colorize cellular components not targeted by the antibody [62]. Most cells are colorless, so a counterstain provides essential morphological context and architectural contrast, allowing the specific antibody signal to be pinpointed within the tissue [63] [62]. The choice of counterstain depends on the detection method (chromogenic vs. fluorescent) and the desired color contrast.
Common Counterstains and Applications
Table 2: Common Counterstains for Chromogenic and Fluorescent IHC
| Counterstain | Type | Target | Resulting Color | Key Applications and Notes |
|---|---|---|---|---|
| Hematoxylin | Chemical | Nuclear histones (proteins) [63] [62] | Blue to Violet [63] | The standard nuclear counterstain for brown DAB. Provides excellent contrast [62]. |
| Nuclear Fast Red | Chemical | Nucleic Acids [63] [62] | Red [63] | Fast (5 min) nuclear stain. Ideal for contrasting with brown or green signals [63] [62]. |
| Methyl Green | Chemical | Nucleic Acids [63] [62] | Green [63] | Fast (5 min) nuclear stain. Contrasts well with red or brown signals [63] [62]. |
| Eosin | Chemical | Cytoplasmic proteins [63] [62] | Pink to Red [63] | Cytoplasmic & ECM stain. Useful when the target antigen is nuclear [63] [62]. |
| DAPI | Fluorescent | Double-stranded DNA [63] [62] | Blue [63] | Gold standard for fluorescence. Minimal cytoplasmic staining [62]. |
| Hoechst | Fluorescent | DNA [63] [62] | Blue [63] | Similar to DAPI. A common nuclear counterstain for multiplex IF [63]. |
| Propidium Iodide | Fluorescent | DNA/RNA [63] [62] | Red [63] | Requires RNase treatment to avoid RNA staining. Useful if blue channel is occupied [62]. |
Selecting a Counterstain Based on Antigen Location
The cellular location of the target antigen should guide the choice of counterstain [62]:
- Nuclear Antigens: If the target protein is in the nucleus (e.g., a transcription factor), a heavy nuclear stain like hematoxylin could mask the signal. In this case, a cytoplasmic stain like Eosin is recommended, as it will stain the surrounding cytoplasm pink, providing context without obscuring the nuclear target [62].
- Cytoplasmic/Membrane Antigens: For antigens located in the cytoplasm or on the cell membrane, a nuclear counterstain is ideal. Hematoxylin (blue) is the standard choice, but Nuclear Fast Red (red) or Methyl Green (green) can be used for alternative color schemes [62].
- Multiplex Fluorescence: In multi-color IF experiments, select a nuclear stain whose emission color (e.g., DAPI/Hoechst for blue) does not overlap with the fluorophores used for antibody detection (e.g., Alexa Fluor 488 for green, Alexa Fluor 594 for red) [62].
Comparison, Analysis, and Quantification
Direct Comparison of Chromogenic and Fluorescent Detection
The choice between chromogenic and fluorescent detection hinges on the experimental goals, as each method offers distinct advantages and limitations [57] [58].
Table 3: Comprehensive Comparison of Chromogenic and Fluorescent Detection
| Parameter | Chromogenic Detection (e.g., DAB) | Fluorescent Detection |
|---|---|---|
| Signal Generation | Enzyme (HRP/AP) converts soluble substrate to insoluble colored precipitate [58] | Fluorophore emits light upon excitation by specific wavelength [57] |
| Sensitivity | High. Signal amplification via ABC, LSAB, or polymer methods increases sensitivity [58] | Variable. Generally lower than amplified chromogenic methods, but can be enhanced with biotin-streptavidin [58] |
| Spatial Resolution | Lower. Enzyme precipitate can diffuse, causing "fuzziness" [57] | Higher. Excellent for high-resolution and confocal microscopy; precise protein localization [57] |
| Multiplexing | Challenging. Limited by chromogen color overlap; best for antigens in distinct compartments [58] | Excellent. Many fluorophores with narrow emission spectra allow for multi-target co-localization [57] [58] |
| Signal Stability | Excellent. DAB is permanent; slides can be stored for years [57] [58] | Limited. Susceptible to photobleaching; requires anti-fade mountant [57] [58] |
| Microscopy | Standard brightfield microscope [14] | Requires more expensive fluorescence/confocal microscope [57] |
| Quantification | Semi-quantitative; enzymatic reaction has a narrow dynamic range [58] | True quantitative. Linear dynamic range suitable for high-throughput automated analysis [57] [58] |
| Protocol Steps | More steps, including substrate addition [57] | Fewer steps; no substrate addition required [57] |
Image Analysis and Quantification
Accurate analysis is crucial for translating IHC staining into robust, reproducible data.
- Chromogenic IHC Analysis: Analysis typically involves a semi-quantitative assessment that considers the staining intensity (negative, weak, moderate, strong) and the percentage of positive cells [14]. This approach, while common, is subjective and prone to inter-observer variability [14]. Digital pathology and automated image analysis can reduce this subjectivity. A key first step is the digital separation of the DAB signal from the hematoxylin counterstain. Advanced algorithms, such as color deconvolution, can isolate these signals, allowing for pixel-based quantification of the DAB-positive area [64].
- Fluorescent IHC Analysis: Fluorescence detection is inherently more suited for quantification due to its linear dynamic range and the ability to measure fluorescence intensity directly [57]. This makes it ideal for high-content screening and automated microscopy platforms. Analysis involves measuring the intensity of the fluorescence signal within a defined region of interest, which can be correlated with protein expression levels [57].
The Scientist's Toolkit: Essential Reagents and Materials
Successful IHC requires a suite of reliable reagents and instruments. The following table lists key solutions and tools used in modern IHC workflows, as featured in the protocols and discussions above.
Table 4: Essential Research Reagent Solutions for IHC
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Primary Antibodies | Bind specifically to the target antigen of interest. | Monoclonal (specific) or polyclonal (sensitive); require validation for IHC [14]. |
| Detection Systems | Visualize the bound primary antibody. | HRP- or AP-based polymer systems, ABC kits, fluorescently-labeled secondary antibodies [58]. |
| Chromogens | Form a colored precipitate at the antigen site upon enzyme action. | DAB (brown), AEC (red) [58]. |
| Fluorophores | Emit light upon excitation for fluorescent detection. | Alexa Fluor dyes, DyLight dyes, FITC, TRITC [57] [60]. |
| Antigen Retrieval Reagents | Reverse formaldehyde cross-links to unmask epitopes. | Citrate buffer (pH 6.0), Tris-EDTA buffer (pH 9.0) [61] [60]. |
| Blocking Reagents | Reduce non-specific background staining. | Normal serum, BSA, or commercial protein-free blocking buffers [60]. |
| Counterstains | Provide morphological context. | Hematoxylin (chromogenic), DAPI/Hoechst (fluorescent) [63] [62]. |
| Mounting Media | Preserve the stain and optimize microscopy. | Aqueous for fluorescence (with anti-fade agents), permanent (e.g., DPX) for chromogenic [61] [57]. |
| Automated Staining Instrument | Standardize and automate the staining procedure. | Platforms from vendors like Agilent, Roche, and Leica [29]. |
| Digital Slide Scanner | Digitize whole slides for analysis and archiving. | Brightfield and fluorescence scanners (e.g., Hamamatsu NanoZoomer) [61]. |
| Image Analysis Software | Quantify staining intensity and area. | Open-source (QuPath, ImageJ/FIJI) and commercial solutions [61] [64]. |
Both chromogenic and fluorescent detection techniques are powerful tools for visualizing protein expression in situ. The decision to use DAB-based chromogenic detection or immunofluorescence is not a matter of one being superior to the other, but rather which is most appropriate for the specific research question. Chromogenic IHC, with its permanent record, high sensitivity, and compatibility with brightfield microscopy, remains a cornerstone for clinical diagnostics and single-marker studies. In contrast, fluorescent IHC offers superior capabilities for multiplexing, high-resolution co-localization, and quantitative analysis, making it ideal for advanced research applications. A thorough understanding of the principles, protocols, and tools underlying both techniques—including the strategic use of counterstains—enables researchers to design robust experiments, generate reliable data, and push the boundaries of discovery in biomedical science.
This whitepaper explores the pivotal role of immunochemistry in advancing diagnostic and research capabilities across three critical disease domains: cancer, infectious diseases, and neurodegenerative disorders. Within the framework of immunochemistry principles, we examine cutting-edge techniques including immunohistochemistry (IHC), companion diagnostics, seed amplification assays (SAAs), and their integration with artificial intelligence (AI) and digital pathology. The content provides detailed technical protocols, analyzes key signaling pathways, and presents quantitative data comparisons to serve researchers, scientists, and drug development professionals. Emerging trends such as AI-driven image analysis, circulating tumor DNA (ctDNA) monitoring, and multiplexed immunohistochemistry are highlighted as transformative forces in precision medicine.
Immunochemistry harnesses the specific binding between antibodies and antigens to detect, localize, and quantify target molecules within biological samples. Its core principle lies in the precise molecular recognition that allows for the visualization of protein expression within its native morphological context [14]. Immunohistochemistry (IHC), the most common immunostaining technique, combines histological, immunological, and biochemical principles to detect specific antigens in tissue sections using enzyme-labeled or fluorescent-tagged antibodies [14] [15].
The fundamental procedure involves multiple critical steps: tissue fixation and processing, antigen retrieval to unmask epitopes, antibody incubation for specific binding, and detection via chromogenic or fluorescent methods [14] [15]. Two primary methods are employed: the direct method, where a labeled primary antibody binds directly to the antigen, and the more sensitive indirect method, which uses a labeled secondary antibody that amplifies the signal [14]. The technique's unique advantage over methods like Western blot or ELISA is its ability to precisely localize target proteins within intact tissue architecture without requiring protein digestion [14].
Immunochemistry in Cancer Diagnostics
Technical Applications and Workflow
IHC is indispensable in oncologic pathology for tumor diagnosis, classification, prognostic assessment, and predicting response to targeted therapies. It enables the identification of tissue of origin for metastatic cancers and the detection of predictive biomarkers that guide therapeutic decisions [14] [15]. For example, HER2/neu status in breast cancer determines eligibility for trastuzumab therapy, while markers like TTF-1 and Napsin A help distinguish primary lung adenocarcinoma from metastatic lesions [15] [65].
The standard IHC workflow for cancer diagnostics involves formalin-fixed, paraffin-embedded (FFPE) tissue sections that undergo deparaffinization, rehydration, and antigen retrieval using heat-induced epitope retrieval (HIER) methods [14] [15]. Following blocking of endogenous peroxidases, sections are incubated with primary antibodies specific to the target antigen (e.g., HER2, Ki-67, PD-L1), followed by enzyme-conjugated secondary antibodies and chromogenic substrates like 3,3'-Diaminobenzidine (DAB) to produce a visible reaction product [15]. Counterstaining with hematoxylin provides nuclear detail, allowing for pathological evaluation under light microscopy [14].
Key Signaling Pathways and Biomarkers
Cancer biomarkers detectable via IHC often represent critical nodes in oncogenic signaling pathways. The HER2 signaling pathway illustrates this principle: upon ligand binding and dimerization, HER2 activates downstream effectors including the MAPK pathway promoting cell proliferation, and the PI3K/Akt pathway enhancing cell survival and growth [65]. In breast cancer, HER2 overexpression drives tumor aggressiveness, making it a crucial therapeutic target [65].
Other significant biomarkers include mismatch repair (MMR) proteins (MLH1, MSH2, MSH6, PMS2) for identifying microsatellite instability-high tumors, and PD-L1 for assessing eligibility for immune checkpoint inhibitors [66]. Emerging biomarkers like c-MET protein overexpression in 35-72% of non-small cell lung cancers (NSCLC) and FGFR2b expression in 20-30% of gastric cancers represent new frontiers in companion diagnostics [67].
Diagram 1: HER2 oncogenic signaling pathway in breast cancer.
Research Reagent Solutions
Table 1: Essential Research Reagents for Cancer Immunochemistry
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Primary Antibodies | HER2/neu, Ki-67, p53, PD-L1, TTF-1, CK7, CK20 | Detect specific tumor-associated antigens for diagnosis and classification |
| Detection Systems | Horseradish peroxidase (HRP), Alkaline phosphatase (AP), DAB chromogen | Visualize antibody-antigen binding through colorimetric or fluorescent signals |
| Tissue Processing Reagents | 10% Neutral buffered formalin, Xylene, Ethanol grades, Paraffin | Preserve tissue morphology and prepare sections for staining |
| Antigen Retrieval Solutions | Citrate buffer (pH 6.0), EDTA buffer (pH 8.0) | Unmask epitopes obscured by formalin fixation through heat-induced methods |
| Blocking Reagents | Normal serum, Bovine serum albumin (BSA), Hydrogen peroxide | Reduce non-specific background staining and block endogenous enzyme activity |
Current Advances and Future Perspectives
The field of cancer immunochemistry is evolving rapidly through integration with digital pathology and artificial intelligence (AI). AI algorithms can now assist in interpreting complex staining patterns, potentially improving scoring objectivity and diagnostic accuracy [67] [14]. The transition from traditional microscopy to digital image analysis is accelerating, facilitated by recent FDA clearances for digital pathology systems [67].
Companion diagnostics (CDx) represent another growing area, with over 60 FDA-approved tests in hematology and oncology as of early 2025 [67]. Emerging trends include CDx that can only be evaluated digitally because the staining patterns are imperceptible to the human eye [67]. The convergence of companion diagnostics with digital pathology is expected to drive improvements in biomarker development and performance through AI-based technology [67].
Additional advances include multiplex immunohistochemistry, which allows simultaneous detection of multiple targets using different fluorophores, enabling comprehensive analysis of the tumor microenvironment [15]. Spatial transcriptomics and single-cell sequencing are further enhancing our understanding of tumor heterogeneity and therapy resistance mechanisms [66].
Immunochemistry in Infectious Disease Research
Technical Applications and Workflow
In infectious disease pathology, IHC provides a powerful tool for detecting and localizing pathogens within tissues, particularly when cultures cannot be obtained or the infectious agent is slow-growing or fastidious [14]. The technique can identify a broad spectrum of pathogens including viruses (e.g., cytomegalovirus), bacteria (e.g., Mycobacterium tuberculosis), and fungi (e.g., Histoplasma capsulatum) within the context of host tissue response [15].
The IHC protocol for infectious agents follows similar principles to cancer diagnostics but requires careful selection of antibodies targeting pathogen-specific antigens. Tissue handling and fixation remain critical to preserve both microbial antigens and host tissue architecture [14]. Key applications include identifying the etiology of unexplained infections, characterizing novel emerging pathogens, and understanding host-pathogen interactions through localization studies [68].
Research Reagent Solutions
Table 2: Essential Research Reagents for Infectious Disease Immunochemistry
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Pathogen-Specific Antibodies | Viral proteins (CMV, HPV), Bacterial antigens, Fungal elements | Detect and localize specific infectious agents in tissue sections |
| Signal Amplification Systems | Polymer-based detection, Tyramide signal amplification (TSA) | Enhance sensitivity for detecting low-abundance microbial antigens |
| Tissue Preservation Reagents | Formalin, Paraformaldehyde, Optimal cutting temperature (OCT) compound | Maintain structural integrity of both host tissue and pathogen elements |
| Counterstains | Hematoxylin, DAPI | Provide contrast for visualizing tissue architecture and nuclear details |
| Control Materials | Known positive infected tissues, Non-infected tissues | Validate staining specificity and assay performance |
Current Research Focus and International Initiatives
Recent research highlighted at the 2025 Infectious Diseases Research Symposium reflects diverse applications of immunochemical techniques, including studies on "Duration and Quantification of Histoplasma capsulatum Antigenuria During Treatment" and "New diagnostic tests to detect parasite proteins in the blood of people with heavy Loa loa infections" [68]. The detection of pathogen-specific antigens remains a cornerstone of infectious disease diagnostics.
International collaborative efforts such as the U.S.-Japan Cooperative Medical Sciences Program are promoting early-stage investigator research in infectious diseases and immunology, with 2025 funding focusing on projects related to nutrition and metabolism in infectious diseases [69]. These initiatives highlight the global commitment to advancing diagnostic capabilities for emerging infectious threats.
Immunochemistry in Neurodegenerative Disorder Research
Technical Applications and Workflow
In neurodegenerative disease research, IHC enables the detection and characterization of pathological protein aggregates that define various disorders. Key applications include identifying tau protein in Alzheimer's disease, α-synuclein (α-Syn) in Lewy body diseases, and transactive response DNA binding protein 43 (TDP-43) in frontotemporal lobar degeneration and amyotrophic lateral sclerosis [70] [15].
The standard protocol involves obtaining central or peripheral nervous tissue specimens, fixation in formalin or paraformaldehyde, and sectioning using a microtome or cryostat. For α-Syn detection, antigen retrieval using formic acid pretreatment enhances the exposure of epitopes [70]. Incubation with phosphorylation-specific α-Syn antibodies (e.g., clone 4D6) followed by standard detection methods allows visualization of Lewy bodies, Lewy neurites, and glial cytoplasmic inclusions [70].
Alpha-Synuclein Pathogenesis and Detection
Alpha-synuclein (α-Syn) is a 14 kDa presynaptic protein that undergoes misfolding and aggregation in Parkinson's disease and related synucleinopathies [70]. In its pathological form, α-Syn transitions from a natively unfolded state to β-sheet-rich amyloid fibrils that accumulate as intracellular inclusions [70]. The protein contains three domains: N-terminal region (residues 1-60), central hydrophobic non-amyloid component domain (residues 61-95), and acidic C-terminal domain (residues 95-140) [70].
The pathological process follows a seeding/nucleation mechanism where misfolded α-Syn acts as a template for converting normal protein, enabling prion-like spread through neural networks [70]. This propagation follows a characteristic pattern described by Braak staging, beginning in peripheral autonomic and olfactory regions before progressing through brainstem, limbic system, and ultimately neocortical areas [70].
Diagram 2: Alpha-synuclein aggregation pathway in Parkinson's disease.
Advanced Detection Methodologies: RT-QuIC
While traditional IHC remains valuable for post-mortem confirmation, seed amplification assays (SAAs) have emerged as sensitive antemortem diagnostic tools. Real-time quaking-induced conversion (RT-QuIC) represents a particularly promising SAA that detects minute quantities of misfolded α-Syn in cerebrospinal fluid, blood, skin, or other tissues [70].
The RT-QuIC protocol involves incubating the biological sample with recombinant α-Syn substrate in a plate reader system with periodic shaking. If pathological α-Syn seeds are present, they template the conversion of the substrate to amyloid fibrils, which can be detected using fluorescent dyes like thioflavin T that bind to β-sheet structures [70]. This method demonstrates high sensitivity (approximately 90%) and specificity (82-100%) for detecting α-synucleinopathies, enabling diagnosis at early disease stages [70].
Research Reagent Solutions
Table 3: Essential Research Reagents for Neurodegenerative Disease Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Phospho-Specific Antibodies | Anti-phospho-α-synuclein, Anti-phospho-tau, Anti-TDP-43 | Detect pathological protein aggregates characteristic of specific neurodegenerative diseases |
| Amyloid Detection Dyes | Thioflavin T, Thioflavin S | Bind β-sheet structures in amyloid fibrils for fluorescence-based detection |
| Recombinant Proteins | Recombinant α-synuclein monomer | Serve as substrate in seed amplification assays like RT-QuIC |
| Tissue Processing Reagents | Phosphate-buffered formalin, Sucrose solutions, Optimal cutting temperature (OCT) compound | Preserve neural tissue architecture for sectioning and staining |
| Signal Development Reagents | DAB, Vector NovaRED, Fluorescent-conjugated secondary antibodies | Visualize antibody binding in tissue sections or assay platforms |
Comparative Analysis of Technical Approaches
Table 4: Quantitative Comparison of Immunochemical Detection Methods
| Parameter | Traditional IHC | Fluorescent IHC | Digital Pathology with AI | RT-QuIC SAA |
|---|---|---|---|---|
| Sensitivity | Moderate | High | High (algorithm-dependent) | Very High (~90% for α-Syn) |
| Specificity | High (antibody-dependent) | High (antibody-dependent) | High (algorithm-dependent) | High (82-100%) |
| Morphological Context | Preserved | Preserved | Preserved | Not applicable |
| Multiplexing Capability | Limited (sequential staining) | High (multiple fluorophores) | High | Limited |
| Throughput | Moderate | Moderate | High | Moderate to High |
| Quantification Potential | Semi-quantitative (subjective) | Semi-quantitative to quantitative | Quantitative | Quantitative kinetic parameters |
| Primary Applications | Diagnostic pathology, Biomarker localization | Research, Multiplex analysis, Subcellular localization | High-throughput analysis, Pattern recognition | Early detection, Biomarker validation |
Future Perspectives in Immunochemistry
The future of immunochemistry is marked by several convergent technological trends. Artificial intelligence integration will increasingly assist in pattern recognition, reduce scoring subjectivity, and automate routine tasks in pathology [67]. Digital pathology platforms will transition from interpretation tools to analytical systems capable of extracting novel biomarkers from existing stainings [67] [66].
In cancer diagnostics, companion diagnostics will increasingly intersect with digital pathology, with some future CDx potentially being exclusively evaluated through digital image analysis because the staining patterns are undetectable by human eye [67]. The continued evolution of multiplexed immunohistochemistry will enable more comprehensive single-cell expression analysis within tissue architecture [14].
For neurodegenerative diseases, refinement of seed amplification assays like RT-QuIC will focus on establishing standardized, reproducible protocols for worldwide diagnostic use [70]. These advances will collectively enhance our ability to detect diseases at earlier stages, monitor treatment responses more precisely, and develop more effective targeted therapies across the spectrum of human disease.
Immunochemical techniques continue to evolve as cornerstone methodologies in biomedical research and clinical diagnostics. From foundational IHC to cutting-edge applications in digital pathology and seed amplification assays, these tools provide unprecedented insights into disease mechanisms while enabling precise diagnosis and personalized treatment approaches. As technology advances, the integration of immunochemistry with artificial intelligence, multiplexed analysis, and novel detection platforms will further expand its applications across cancer, infectious diseases, and neurodegenerative disorders. For researchers and drug development professionals, understanding these techniques, their appropriate applications, and their future trajectories is essential for driving the next wave of diagnostic and therapeutic innovations.
The Role of Immunochemistry in Drug Development and Biomarker Discovery
Immunochemistry (IHC) is an indispensable technique in modern biomedical research and development. By leveraging antibody-epitope interactions to detect and visualize specific proteins within tissue samples, IHC provides critical insights that drive innovation in drug development and biomarker discovery. Its unique ability to provide spatial context in a physiologically relevant tissue environment makes it superior to many other protein analysis techniques for diagnostic and research applications. This whitepaper details the technical applications, methodologies, and emerging trends of immunochemistry, framing them within core principles of the technique to illustrate its vital role in advancing precision medicine.
Immunochemistry in the Drug Development Pipeline
Immunochemistry techniques are deeply integrated throughout the entire drug development continuum, from initial discovery to clinical trials and companion diagnostics. The global pharmaceutical industry's pipeline is increasingly dominated by modalities that rely heavily on immunochemical characterization, with new modalities now accounting for $197 billion, or 60% of the total projected pipeline value [71].
Key Therapeutic Areas and Modalities
- Biopharmaceutical Characterization: Immunochemistry is fundamental for characterizing biological drugs, especially monoclonal antibodies (mAbs). It is used to verify purity, potency, and stability during manufacturing, and to monitor immune responses in clinical trials [72]. The mAbs clinical pipeline remains the largest among new modalities, showing 7% growth in clinical-stage products and 9% growth in pipeline value in the past year [71].
- Therapeutic Antibodies and Beyond: Beyond standard mAbs, more complex formats like Antibody-Drug Conjugates (ADCs) and Bispecific Antibodies (BsAbs) require sophisticated IHC for target validation and pharmacodynamic studies. ADCs have seen a 40% growth in expected pipeline value during the past year, while BsAbs have experienced a 50% increase in forecasted pipeline revenue [71].
- Cell and Gene Therapies: IHC is crucial for monitoring the tissue localization and persistence of cell therapies like CAR-T cells. While CAR-T pipelines continue growing rapidly, other emerging cell therapies face challenges including clinical delays and high manufacturing costs [71].
Table 1: Quantitative Impact of Key Modalities Reliant on Immunochemistry Analysis
| Modality | Pipeline Value Growth (Past Year) | 5-Year CAGR | Key Applications of IHC |
|---|---|---|---|
| mAbs | 9% | Information Missing | Target validation, biodistribution studies |
| ADCs | 40% | 22% | Target expression profiling, patient stratification |
| BsAbs | 50% | Information Missing | Mechanism of action studies, biomarker co-localization |
| CAR-T | Information Missing | Information Missing | Tracking cell persistence and tumor infiltration |
Clinical Translation and Personalized Medicine
Immunochemistry enables personalized medicine by identifying patient-specific biomarkers that guide targeted therapy decisions [72]. For example, testing for HER2 in breast cancer using IHC determines eligibility for HER2-targeted treatments. This approach improves treatment efficacy while reducing adverse effects. Pharmaceutical companies increasingly use immunochemical assays to stratify patients in clinical trials, significantly increasing the likelihood of successful outcomes [72].
Advanced Applications in Biomarker Discovery
The evolving role of biomarkers in translational research demands increasingly sophisticated immunochemistry approaches. Cancer biomarkers provide insights into cancer presence, progression, recurrence potential, and likely therapeutic outcomes [73].
Spatial Biology and Tumor Microenvironment Analysis
Spatial biology techniques represent one of the most significant advances in IHC-based biomarker discovery [73]. Unlike traditional approaches that homogenize tissues, spatial transcriptomics and multiplex IHC allow researchers to study gene and protein expression in situ without altering spatial relationships between cells [73].
Critical Insights from Spatial Analysis:
- Distribution patterns of biomarkers within specific tumor regions often have greater prognostic value than mere presence/absence
- Cell-to-cell interaction distances can serve as functional biomarkers for immunotherapy response
- Different tumor microenvironments express distinct biomarkers relevant to various aspects of disease progression
- The physical organization of immune cells within tumors predicts response to immunotherapies
Integrated Multi-Omics Approaches
Combining IHC with genomic, epigenomic, and proteomic data provides a holistic approach to biomarker discovery [73]. Multi-omics can reveal novel insights into the molecular basis of diseases and drug responses, identifying new biomarkers and therapeutic targets that would be missed with single-platform analyses.
Exemplar Case: An integrated multi-omic approach played a central role in identifying the functional role of two genes, TRAF7 and KLF4, which are frequently mutated in meningioma [73].
Artificial Intelligence-Enhanced Analytics
Artificial intelligence (AI) and machine learning represent transformative advancements for analyzing complex data generated by modern IHC platforms [73]. These technologies can pinpoint subtle biomarker patterns in high-dimensional multi-omic and imaging datasets that conventional methods miss.
AI Applications in IHC:
- Predictive models that forecast patient responses, recurrence risk, and survival likelihood
- Automated image analysis algorithms that exceed human capabilities for consistency and throughput
- Natural language processing (NLP) to extract insights from clinical records and identify biomarker-patient outcome relationships
- AI-powered biosensors that detect circulating tumor cells and predict treatment responses
Technical Framework: Experimental Protocols and Methodologies
Core IHC Workflow
The following diagram illustrates the generalized IHC protocol, highlighting critical decision points and potential optimization requirements at each stage:
Case Study: Quantitative IHC Analysis of PAUF in Pancreatic Cancer
A 2025 study investigated Pancreatic Adenocarcinoma Upregulated Factor (PAUF) as a prognostic biomarker in Pancreatic Ductal Adenocarcinoma (PDAC) using rigorous IHC methodology [74]. The experimental protocol provides an exemplar for robust biomarker validation.
Experimental Protocol:
Sample Preparation:
- Surgical specimens from 93 patients with PDAC
- Tissues fixed in 40 g/L formaldehyde and processed into paraffin blocks
- Sectioning at 4-5μm thickness
- Deparaffinization in xylene and rehydration through graded ethanol series
Antigen Retrieval:
- Tissue slides immersed in 10 mmol/L sodium citrate buffer (pH 6.0)
- Microwave heating for 10 minutes
- Cooling at room temperature for 30 minutes
Immunostaining:
- Endogenous peroxidase blocking with 0.88 mol/L hydrogen peroxide in methanol (10 minutes)
- Blocking with 100 g/L normal animal serum (30 minutes)
- Primary antibody incubation: Rabbit-derived polyclonal antibody against recombinant human PAUF (12 μg/mL concentration, 4°C overnight)
- Detection: Peroxidase-based chromogenic detection system (EnVision+ HRP) with 3,3'-diaminobenzidine development (10 minutes)
- Counterstaining with hematoxylin
Quantitative Analysis:
- Digital slide scanning using Pannoramic 250 Flash II scanner
- Assessment of staining intensity (0: no staining, 1+: weak, 2+: moderate to strong)
- Evaluation of percentage of positively labeled tumor regions (0-100%)
- Dichotomization at 5% cutoff for statistical analysis (PAUF-low: 0 or 1%-4% staining; PAUF-high: 1+ or 2+ and >5% staining)
Statistical Validation:
- Association with clinicopathological characteristics
- Kaplan-Meier survival analysis with log-rank Mantel-Cox test
- Multivariate Cox regression for independent prognostic factor identification
Table 2: Key Research Reagent Solutions for IHC Biomarker Studies
| Reagent/Category | Specific Examples | Function & Importance |
|---|---|---|
| Fixatives | Formalin, Paraformaldehyde (PFA), Ethanol | Preserves tissue integrity and antigenicity; critical for morphology preservation [2] |
| Antigen Retrieval Buffers | Sodium citrate buffer (pH 6.0) | Reverses formaldehyde-induced cross-linking; essential for antibody access to epitopes [74] |
| Primary Antibodies | Rabbit polyclonal anti-PAUF (PBP1510) | Specifically binds target protein; determines assay specificity [74] |
| Detection Systems | EnVision+ HRP, DAB chromogen | Amplifies signal and enables visualization; critical for sensitivity [74] |
| Blocking Agents | Normal animal serum (10%) | Reduces non-specific background staining; improves signal-to-noise ratio [2] |
| Counterstains | Hematoxylin, DAPI | Provides morphological context; nuclear localization reference [74] |
Automated Quantitative Analysis
Advanced computational methods are revolutionizing IHC quantification. Recent developments include deep learning techniques and image processing algorithms for automated quantitative analysis of nuclear, membrane, and cytoplasmic expressions in whole-slide images [7].
Technical Approach:
- Optical density separation to differentiate hematoxylin and DAB staining components
- CellViT nuclear segmentation algorithm for precise nuclei identification
- Region growing algorithm for membrane and cytoplasmic delineation
- Experimental validation demonstrating excellent accuracy and recall compared to traditional manual interpretation [7]
Emerging Technologies and Future Directions
The future of immunochemistry in drug development and biomarker discovery is being shaped by several converging technological innovations that enhance precision, throughput, and clinical relevance.
Integrated Technology Platforms
Advanced Disease Models:
- Organoids: Recapitulate complex architectures and functions of human tissues; excellent for functional biomarker screening and target validation [73]
- Humanized Systems: Mimic human tumor-immune interactions; particularly valuable for immunotherapy response and resistance studies [73]
When combined with multi-omic technologies and spatial biology, these models significantly enhance the predictive accuracy of biomarker studies, bridging the gap between bench research and clinical application [73].
Digital Pathology and Automation
The integration of IHC with digital pathology platforms enables:
- High-throughput quantitative analysis across entire tissue sections
- Artificial intelligence-driven pattern recognition beyond human capability
- Standardized assessment eliminating inter-observer variability
- Advanced multiplexing capabilities for analyzing complex biomarker networks
Regulatory and Commercial Landscape
The immunochemistry ecosystem includes leading players such as Abbott, Roche, Thermo Fisher Scientific, Bio-Rad, and Agilent Technologies, who offer comprehensive product portfolios from reagents to automated analyzers [72]. The field is supported by collaborations between academia, industry, and regulatory bodies that foster innovation and standardization.
By 2025, immunochemistry will become more integrated with digital health tools, AI-driven data analysis, and automation, enabling faster, more accurate diagnostics and personalized treatments [72]. The adoption of multiplex and digital immunochemistry platforms will expand, providing comprehensive insights from minimal sample volumes.
Immunochemistry remains a cornerstone technology in drug development and biomarker discovery, with evolving methodologies and applications that continuously expand its utility. The integration of spatial biology, multi-omics approaches, artificial intelligence, and automated quantification platforms represents the next frontier in IHC innovation. As personalized medicine advances, the role of immunochemistry in validating therapeutic targets, stratifying patient populations, and guiding treatment decisions will only intensify. The continued refinement of IHC protocols and analytical methods ensures this established technique will maintain its critical position in the biomedical research arsenal for the foreseeable future.
Identifying and Resolving Common Immunochemistry Challenges for Optimal Staining
Weak or absent staining presents a significant challenge in immunohistochemistry (IHC), potentially compromising experimental validity and diagnostic accuracy. This issue fundamentally stems from the failure of the antibody to bind effectively to its target antigen, with the root causes primarily categorized into two domains: inadequate antigen retrieval and compromised antibody potency [75] [14]. Within the broader context of immunochemistry principles, resolving these issues is essential for generating specific, reproducible, and biologically relevant data. This guide provides a systematic framework for researchers and drug development professionals to diagnose and remediate these common technical failures, ensuring the reliability of IHC outcomes in research and preclinical studies.
Core Principles and the Staining Problem
The Fundamental IHC Workflow and Failure Points
The standard IHC protocol is a multi-stage process where failure at any step can lead to suboptimal results. The visualization of a target antigen relies on a cascade of molecular interactions, beginning with effective epitope exposure and culminating in chromogenic or fluorescent signal detection [14]. The most common points of failure leading to weak or no signal occur early in this workflow, specifically during tissue preparation (antigen retrieval) and primary antibody binding [75] [76].
The Critical Role of Antigen Retrieval
Formalin fixation, while essential for preserving tissue morphology, introduces methylene bridges between proteins, leading to epitope masking [77] [78]. This cross-linking alters the three-dimensional conformation of protein epitopes, rendering them inaccessible to primary antibodies. Antigen retrieval is the deliberate process of reversing these cross-links to restore antibody binding capacity [77]. Without this step, even a highly specific and potent antibody will fail to bind its target, resulting in false-negative staining.
Systematic Diagnosis of Staining Failure
A methodical approach is required to isolate the root cause of staining failure. The following diagnostic workflow guides users through the critical decision points.
Diagnostic Workflow
Primary Causes and Initial Solutions
Table 1: Quick-Reference Guide to Common Causes and Immediate Solutions
| Category | Specific Cause | Immediate Remedial Action |
|---|---|---|
| Antigen Retrieval | Insufficient epitope unmasking (under-retrieval) [75] [77] | Increase heating time; switch to higher pH buffer (e.g., Tris-EDTA, pH 9.0) [79]. |
| Formalin over-fixation [75] | Increase duration/intensity of antigen retrieval step [75]. | |
| Antibody Potency | Incorrect antibody concentration [75] | Perform a titration experiment (e.g., test 1:50, 1:100, 1:200 dilutions) [75]. |
| Antibody degradation or denaturation [76] | Run a positive control; aliquot antibodies to avoid freeze-thaw cycles; ensure proper storage [76]. | |
| Antibody not validated for IHC or specific sample type (e.g., FFPE) [75] | Confirm antibody is application-validated; use a monoclonal antibody validated for IHC [75] [80]. | |
| Protocol & Reagents | Inactive detection system (secondary antibody or enzyme-substrate) [75] [76] | Test detection system separately; ensure substrates are fresh and not incompatible with buffers (e.g., no azide with HRP) [76] [80]. |
| Tissue drying during incubation [75] | Always use a humidity chamber for long incubation steps [75]. |
Solving Antigen Retrieval Issues
Antigen Retrieval Methods
Two primary methods are employed to unmask epitopes:
- Heat-Induced Epitope Retrieval (HIER): The most widely used method, HIER uses high temperature (95-120°C) in a specific buffer to break the formalin-induced cross-links [77] [79]. Heating apparatuses include water baths, microwave ovens, and pressure cookers, each requiring specific time optimization [77].
- Protease-Induced Epitope Retrieval (PIER): This chemical method uses proteolytic enzymes (e.g., trypsin, proteinase K, pepsin) to cleave proteins and expose epitopes [77]. It operates at 37°C but carries a higher risk of tissue damage and epitope destruction if over-digested [77].
Optimization Protocol for HIER
A systematic approach is required to optimize HIER. The following protocol provides a step-by-step guide.
Table 2: Experimental Matrix for Optimizing HIER Conditions
| Retrieval Buffer | Typical pH Range | Common Incubation Time & Temperature | Best For |
|---|---|---|---|
| Sodium Citrate | 6.0 [79] [76] | 15-20 min at 95-100°C [79] | A wide range of nuclear and cytoplasmic antigens [77]. |
| Tris-EDTA | 8.0 - 9.9 [77] | 10-30 min at 95-100°C [77] | Often superior for challenging or phosphorylated antigens [77] [78]. |
| Enzymatic (PIER) | Varies (e.g., Trypsin pH 7.8) [77] | 10-20 min at 37°C [77] | A secondary option if HIER fails; requires careful optimization to avoid tissue damage [77]. |
Troubleshooting Antigen Retrieval
- Problem: Weak staining due to under-retrieval.
- Problem: High background due to over-retrieval.
- Problem: Tissue detachment or damage.
- Solution: Use adhesive slides. Allow the retrieval solution to cool gradually to room temperature before handling slides [79].
Addressing Antibody Potency Problems
Establishing Antibody Specificity and Activity
A high-quality antibody is the foundation of successful IHC. To confirm an antibody is suitable and active, several validation steps are necessary, as outlined in the workflow below.
Antibody Titration and Validation Protocol
- Preparation: Create a series of primary antibody dilutions (e.g., 1:50, 1:100, 1:200, 1:500) in an appropriate antibody diluent [75].
- Application: Apply each dilution to consecutive tissue sections from the same positive control block.
- Incubation and Detection: Follow your standard IHC protocol for incubation, detection, and visualization.
- Analysis: Examine the slides to identify the dilution that provides the strongest specific signal with the cleanest background (lowest non-specific binding). This is the optimal concentration.
Advanced Antibody Validation Techniques
For critical applications, especially in drug development, more rigorous validation is recommended:
- Knockout/Knockdown Validation: The most specific control. Staining should be absent in tissues or cell lines where the target gene has been genetically ablated [77].
- Blocking Peptide Assay: Pre-incubate the primary antibody with a saturating amount of the immunizing peptide. A significant reduction or loss of staining confirms specificity [77]. Some manufacturers offer matched antigen-antibody pairs for this purpose [77].
- Orthogonal Validation: Correlate IHC results with another technique, such as Western blot or mRNA in situ hybridization, to confirm the pattern of expression [14].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for IHC Troubleshooting
| Reagent / Material | Critical Function | Application Notes |
|---|---|---|
| Citrate-Based Unmasking Solution (pH ~6.0) | Low-pH retrieval buffer for HIER [78]. | A standard starting point for many antigens [79]. |
| Tris-EDTA Buffer (pH ~9.0) | High-pH retrieval buffer for HIER [78]. | Often more effective for difficult targets; requires empirical testing [77]. |
| Proteinase K / Trypsin | Proteolytic enzyme for PIER [77]. | Use if HIER fails; monitor incubation closely to prevent tissue damage [77]. |
| Normal Serum | Blocking agent to reduce non-specific binding [75] [76]. | Should be from the same species as the secondary antibody host [76]. |
| Peroxidase Suppressor (e.g., 3% H₂O₂) | Quenches endogenous peroxidase activity to lower background [75] [80]. | Essential for HRP-based detection systems [76]. |
| Avidin/Biotin Blocking Kit | Blocks endogenous biotin to reduce background [75] [76]. | Critical for biotin-streptavidin based detection systems [76]. |
| IHC-Validated Primary Antibodies | Ensures antibody specificity and performance in IHC applications [75]. | Always check the datasheet for validation data in IHC and the specific sample type (FFPE/frozen) [75]. |
| Adhesive Microscope Slides | Prevents tissue detachment during rigorous HIER protocols [75]. | Crucial for maintaining tissue integrity, especially with long retrieval times [75]. |
Diagnosing and resolving weak or absent IHC staining demands a structured, evidence-based approach centered on the two most critical variables: antigen retrieval and antibody potency. Success is achieved not by arbitrary adjustments but by systematically optimizing retrieval conditions and rigorously validating antibody reagents. By adhering to the protocols and principles outlined in this guide—employing systematic HIER optimization, performing comprehensive antibody titrations, and implementing robust controls—researchers can transform failed experiments into robust, reliable, and reproducible data. This rigor is paramount for advancing both basic research and the development of novel antibody-based therapeutics.
Immunohistochemistry (IHC) is an indispensable auxiliary method for pathologists and researchers, enabling specific visualization of target molecule distributions within the context of intact tissue architecture [81]. However, the technique's effectiveness is frequently compromised by high background staining, which obscures specific signals and complicates interpretation. This non-specific staining arises from multiple sources, primarily through two mechanisms: non-specific antibody binding to tissue components and interference from endogenous molecules capable of reacting with detection systems [82] [83]. Proper blocking procedures are therefore not merely optional refinements but essential prerequisites for obtaining publishable, reliable data.
The fundamental challenge in IHC lies in distinguishing specific antigen-antibody binding from non-specific interactions governed by the same physicochemical forces [83]. While hydrophobic interactions, ionic forces, and hydrogen bonding facilitate desired epitope-antibody recognition, these same forces can promote undesirable background staining when antibodies interact non-specifically with tissue elements [83]. Additionally, tissues contain endogenous enzymes (peroxidases, phosphatases) and molecules (biotin) that react with detection systems, generating false-positive signals [84] [85]. This technical guide provides comprehensive methodologies for identifying sources of high background and implementing effective blocking strategies to enhance signal-to-noise ratio for optimal IHC results.
Understanding and Blocking Endogenous Enzymes
Chromogenic detection systems in IHC typically employ enzymes such as horseradish peroxidase (HRP) or alkaline phosphatase (AP) conjugated to secondary antibodies. However, many tissues contain endogenous versions of these enzymes that remain active after fixation and can react with substrates to produce widespread background staining [85] [76].
Endogenous Peroxidases
Identification and Sources: Endogenous peroxidases are particularly abundant in tissues containing red blood cells (e.g., vascular tissue), kidney, and liver [85] [82]. Their presence can be confirmed by incubating a rehydrated tissue section with substrate alone (e.g., DAB); colored precipitate formation indicates endogenous peroxidase activity [84].
Blocking Protocols:
- Hydrogen Peroxide Method: Incubate tissue sections with 0.3%-3% hydrogen peroxide in methanol or phosphate-buffered saline (PBS) for 10-15 minutes at room temperature [84] [85] [81]. Methanol is preferred for peroxidase-rich tissues as aqueous solutions may damage tissue architecture [82].
- Commercial Blockers: Ready-to-use peroxidase suppressing solutions (e.g., Thermo Fisher Peroxidase Suppressor) are available and specifically formulated for IHC applications [84] [76].
Endogenous Alkaline Phosphatase
Identification and Sources: Endogenous AP is prevalent in intestine, kidney, lymphoid tissue, osteoblasts, and placenta, with generally higher activity in frozen tissues [85]. Testing involves incubation with BCIP/NBT substrate solution; blue precipitate indicates endogenous AP activity [84] [85].
Blocking Protocols:
- Levamisole Inhibition: Add levamisole hydrochloride to the AP substrate solution at a final concentration of 1-10 mM to inhibit endogenous AP activity [84] [85] [81]. Note that the intestinal form of AP is levamisole-resistant.
- Acetic Acid Blocking: For levamisole-resistant intestinal AP, 1% acetic acid can be effective [83].
- Universal Blockers: Reagents like BLOXALL Endogenous Blocking Solution can inactivate both peroxidase and alkaline phosphatase through a single 10-minute incubation [82].
Table 1: Summary of Endogenous Enzyme Blocking Methods
| Enzyme Type | Common Tissue Sources | Detection Method | Blocking Reagent | Concentration | Incubation Time |
|---|---|---|---|---|---|
| Peroxidase (HRP) | Kidney, liver, red blood cells | DAB substrate conversion | Hydrogen Peroxide | 0.3%-3% | 10-15 minutes |
| Alkaline Phosphatase (AP) | Intestine, kidney, lymphoid tissue, placenta | BCIP/NBT substrate conversion | Levamisole | 1-10 mM | Added to substrate |
| Both Enzymes | Various | Combined substrate conversion | Commercial Blocker (e.g., BLOXALL) | Ready-to-use | 10 minutes |
Strategies for Blocking Non-Specific Antibody Binding
Non-specific antibody binding represents another major source of background staining in IHC. This occurs through several mechanisms, including interactions with endogenous Fc receptors, hydrophobic interactions, and ionic interactions [82] [83].
Protein Blocking Methods
Protein blocking agents physically occupy non-specific binding sites before antibody incubation, preventing non-specific antibody attachment [82] [86].
Normal Serum Blocking:
- Mechanism: Normal serum from healthy animals contains antibodies that bind non-specifically to Fc receptors, blocking primary antibodies from interacting [82]. The serum should originate from the species in which the secondary antibody was raised [85] [82].
- Protocol: Incubate sections with 5%-10% normal serum for 30 minutes to 1 hour at room temperature [87] [81]. For multiple staining with secondary antibodies from different species, blocking sera from all relevant species may be necessary [85].
Protein-Based Blockers:
- Bovine Serum Albumin (BSA): Use at concentrations of 0.1%-5% in buffers to block hydrophobic binding sites [86] [76].
- Non-Fat Dry Milk: Effective for blocking hydrophobic interactions but contains biotin and is inappropriate for avidin-biotin detection systems [81] [76].
- Animal-Free Synthetic Blockers: Commercial mixes of synthetic peptides (e.g., Animal-Free Blocker) avoid potential cross-reactivity with animal-derived antibodies [82].
Addressing Specific Binding Interactions
Hydrophobic Interactions: Neutral amino acid side chains create hydrophobic sites that promote non-specific binding [83]. Reduction strategies include:
- Adding non-ionic detergents (0.1%-0.5% Triton X-100 or Tween-20) to blocking and antibody solutions [86] [83].
- Using protein blocks (BSA, serum) that physically occupy hydrophobic sites [83].
Ionic Interactions: Net charge differences between antibodies and tissues can cause non-specific attraction [83]. Solutions include:
- Increasing ionic strength of antibody diluent with NaCl (0.15-0.6 M) to reduce ionic interactions [76].
- Note that this approach may impair monoclonal antibody binding more than polyclonal antibodies due to single epitope specificity [83].
Fc Receptor Interactions: Despite being widely cited as a major concern, recent evidence suggests Fc receptors may not retain binding capability after standard aldehyde fixation [88]. One study found no difference in background staining between samples processed with or without protein blocking steps in routinely fixed tissues [88]. However, for frozen sections, smears, and lightly fixed tissues, Fc receptor-mediated background remains a consideration [81].
Table 2: Protein Blocking Methods and Applications
| Blocking Method | Mechanism of Action | Recommended Use | Advantages | Limitations |
|---|---|---|---|---|
| Normal Serum | Binds Fc receptors and non-specific sites | Matched to secondary antibody species | Effective for Fc receptor blocking | Multiple sera needed for multiple staining |
| Bovine Serum Albumin (BSA) | Blocks hydrophobic sites | General purpose blocking | Widely available, inexpensive | Potential bovine IgG contamination |
| Non-Fat Dry Milk | Blocks hydrophobic sites | Non-biotin detection systems | Inexpensive, effective | Contains biotin, unsuitable for ABC methods |
| Synthetic Peptide Mixes | Blocks various non-specific sites | All applications, especially animal-free workflows | No cross-reactivity, consistent | Typically more expensive |
Special Considerations and Advanced Scenarios
Endogenous Biotin Blocking
Biotin is a vitamin and coenzyme abundant in tissues such as liver, kidney, heart, brain, and mammary gland [84] [85]. In avidin-biotin complex (ABC) detection systems, endogenous biotin causes significant background, particularly in frozen sections [84].
Blocking Protocol:
- Coat sample with excess unlabeled streptavidin (or avidin) to bind endogenous biotin [89] [84].
- Add excess free biotin to saturate all remaining biotin-binding sites on the streptavidin molecules [89] [84].
- Proceed with standard IHC protocol.
Alternative Approaches:
- Use streptavidin or NeutrAvidin instead of avidin, as these are not glycosylated and won't bind to tissue lectins [84] [76].
- Consider polymer-based detection methods for tissues with high endogenous biotin content, as these systems don't rely on biotin-streptavidin chemistry [85].
Mouse-on-Mouse Staining
Using mouse primary antibodies on mouse tissues presents special challenges because anti-mouse secondary antibodies will bind to endogenous mouse immunoglobulins throughout the tissue [85].
Solutions:
- Use F(ab) or F(ab')₂ fragments of primary antibodies to eliminate Fc-mediated binding [85] [81].
- Employ pre-adsorbed secondary antibodies specifically validated for mouse-on-mouse staining [89].
- Consider using conjugated primary antibodies to eliminate the need for secondary detection, though this reduces signal amplification [89].
Autofluorescence Reduction
For fluorescent detection, tissue autofluorescence can mimic specific signal, particularly in formalin-fixed paraffin-embedded sections [85] [76].
Reduction Strategies:
- Treat samples with sodium borohydride (1 mg/mL) or glycine/lysine to reduce aldehyde-induced fluorescence [85].
- Use fluorescent dyes that quench autofluorescence, such as pontamine sky blue, Sudan black, or trypan blue [85] [76].
- Select fluorophores in red or infrared wavelengths (e.g., Alexa Fluor 647, 680) to avoid overlap with common autofluorescence spectra [85] [76].
Experimental Protocols and Workflows
Comprehensive IHC Blocking Workflow
The following diagram illustrates a systematic approach to troubleshooting and blocking high background staining in IHC:
Systematic Troubleshooting for High Background
Standardized Protocol for Comprehensive Blocking
Materials:
- Hydrogen peroxide (0.3%-3%)
- Levamisole solution (1-10 mM)
- Normal serum or protein blocking solution
- Avidin/biotin blocking solutions (if using biotin detection)
- PBS or TBS washing buffers
Procedure:
- Deparaffinization and Rehydration: Process slides through xylene and ethanol series to water [89] [81].
- Antigen Retrieval: Perform heat-induced or enzymatic epitope retrieval as required for your target [81].
- Endogenous Peroxidase Blocking (for HRP systems): Incubate with 0.3% H₂O₂ in methanol or PBS for 10-15 minutes at room temperature [84] [81].
- Wash: Rinse 2-3 times with PBS or TBS [81].
- Endogenous Biotin Blocking (for ABC systems): Apply avidin solution for 15 minutes, wash, then apply biotin solution for 15 minutes [85] [82].
- Wash: Rinse 2-3 times with buffer [81].
- Protein Blocking: Apply 5%-10% normal serum or protein blocking solution for 30-60 minutes at room temperature [87] [81].
- Proceed with primary antibody incubation without washing out blocking solution.
Research Reagent Solutions
Table 3: Essential Reagents for Blocking in IHC
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Enzyme Blockers | Hydrogen Peroxide (0.3-3%) | Quenches endogenous peroxidase activity | Use methanol base for peroxidase-rich tissues |
| Enzyme Blockers | Levamisole (1-10 mM) | Inhibits endogenous alkaline phosphatase | Add directly to substrate solution |
| Universal Enzyme Blockers | BLOXALL Solution | Blocks both peroxidase and phosphatase | 10-minute incubation, ready-to-use |
| Protein Blockers | Normal Serum (species-matched) | Blocks Fc receptors and non-specific sites | Use serum from secondary antibody species |
| Protein Blockers | Bovine Serum Albumin (1-5%) | Blocks hydrophobic interactions | Often used with 0.1% Triton X-100 |
| Protein Blockers | Animal-Free Synthetic Blockers | Blocks non-specific binding | Avoids cross-reactivity with animal tissues |
| Biotin Blockers | Avidin/Biotin Blocking Kits | Sequentially blocks endogenous biotin | Essential for ABC systems in high-biotin tissues |
| Detergents | Triton X-100, Tween-20 (0.1-0.5%) | Reduces hydrophobic interactions | Add to blocking and antibody solutions |
Effective blocking of endogenous enzymes and non-specific binding sites is fundamental to successful immunohistochemistry. While standard protocols provide a solid foundation, optimal blocking strategies must be empirically determined for each antibody-tissue combination, particularly considering fixation methods and detection systems. A systematic approach to troubleshooting background staining—beginning with careful controls and proceeding through targeted blocking protocols—enables researchers to achieve the high signal-to-noise ratio essential for accurate data interpretation. As IHC methodologies continue to evolve, with increasing emphasis on multiplexing and quantification, robust blocking procedures remain the cornerstone of reliable histopathological analysis and biomarker research.
Addressing Autofluorescence in Fluorescent IHC and Tissue Artifacts
Autofluorescence is a pervasive challenge in fluorescent immunohistochemistry (IHC) and related techniques, where naturally occurring substances within biological samples emit light upon excitation, interfering with specific antibody-derived signals. This non-specific background fluorescence can significantly reduce assay sensitivity, obscure detection of low-abundance analytes, and potentially lead to misinterpretation of experimental results [90]. The issue is particularly pronounced in the green spectrum channel, where it can mask signals from commonly used fluorophores such as Alexa Fluor 488 and fluorescein isothiocyanate (FITC), as well as green fluorescent protein (GFP) tags used as reporters for gene expression [90].
The impact of autofluorescence extends across multiple fluorescence-based applications, including IHC, immunocytochemistry (ICC), and flow cytometry, where it increases background noise and can completely obscure specific signals when severe [90]. Effectively managing this interference is therefore essential for obtaining reliable, reproducible data in both research and diagnostic settings. This technical guide examines the sources of autofluorescence, provides detailed strategies for its identification and mitigation, and explores advanced computational approaches for artifact management, all within the framework of core immunochemistry principles.
Autofluorescence in biological samples originates from two primary categories: endogenous biomolecules and exogenous substances introduced during sample processing. Understanding these sources is fundamental to developing effective countermeasures.
Numerous intrinsic biological molecules exhibit natural fluorescence properties. The table below summarizes the key endogenous autofluorescent compounds, their locations, and primary characteristics [90]:
Table 1: Key Endogenous Autofluorescence Sources
| Compound | Location/Tissue | Fluorescence Characteristics | Biological Role |
|---|---|---|---|
| Lipofuscin | Lysosomes of post-mitotic cells (e.g., neurons, myocytes) | Broad spectrum; accumulates with age [90] | Pigmented byproduct of intracellular catabolism |
| Collagen & Elastin | Extracellular matrix (blood vessels, skin, lungs) | Green spectrum [90] [91] | Structural proteins providing tissue support and elasticity |
| NAD(P)H & FAD | Mitochondria and cytoplasm | Metabolic oscillations; indicator of cellular metabolism [92] | Key coenzymes in cellular energy production |
| Heme | Red blood cells (hemoglobin) | Iron-protoporphyrin complex [90] | Oxygen transport and cytochrome functions |
| Melanin | Skin, hair, iris | Protective pigment against UV light [90] | UV protection and reactive oxygen species scavenging |
| Aromatic Amino Acids (Tryptophan, Tyrosine) | Ubiquitous in proteins | Tryptophan and tyrosine correlate with tissue structural changes [91] | Protein structure components |
Lipofuscin deserves particular attention in human tissue studies, especially in neurological research. This autofluorescent pigment accumulates progressively in the lysosomes and cytosol of post-mitotic cells such as neurons and myocytes over time [90]. In highly impacted tissues like Alzheimer's disease brain or dorsal root ganglion, lipofuscin can occupy up to 80% of the visible neuronal cytoplasm, affecting approximately 45% of neurons in a typical section, creating significant interference across wavelengths used for common fluorophores [93].
Autofluorescence also arises from laboratory reagents and materials used in sample preparation and processing:
- Aldehyde fixatives including formaldehyde, paraformaldehyde, and glutaraldehyde can induce autofluorescence by reacting with amine groups to form fluorescent Schiff's bases [90].
- Plastic microplates and cell culture flasks often exhibit inherent fluorescence, making glass-bottomed or non-fluorescent polymer containers preferable for fluorescence imaging [90].
- Media supplements such as Fetal Bovine Serum (FBS) and Phenol Red can contribute to background fluorescence and should be avoided in live-cell imaging studies [90].
Detection and Evaluation of Autofluorescence
Establishing Experimental Controls
Proper detection begins with implementing appropriate controls. Researchers should always include an unstained control sample (processed identically to test samples but omitting fluorescently-labeled reagents) to assess the level and spectral characteristics of inherent autofluorescence [90]. This control is essential for distinguishing specific signal from background and determining whether protocol optimization is necessary before proceeding with full experiments.
Advanced Detection Methodologies
Beyond simple observation, several advanced technologies facilitate more sophisticated autofluorescence assessment:
- Spectral flow cytometry allows for detailed characterization of autofluorescence signatures across multiple detection channels, enabling better separation from specific signals [90].
- Fluorescence lifetime imaging microscopy (FLIM) discriminates between fluorophores based on their fluorescence decay characteristics rather than just spectral properties, allowing separation of autofluorescence from immunofluorescence even when their emission spectra overlap [90] [92].
- Machine learning approaches utilizing convolutional autoencoders (CAEs) can automatically detect artifact-laden images by training on artifact-free images and identifying discrepancies in new images [94]. These systems have demonstrated 95.5% accuracy in classifying artifacts across different datasets and can detect previously unseen artifact types [94].
The following workflow diagram illustrates the process for detecting and addressing autofluorescence in IHC experiments:
Diagram 1: Autofluorescence Assessment Workflow
Strategies for Managing and Reducing Autofluorescence
Sample Preparation and Treatment Methods
Several physical and chemical treatments can effectively reduce autofluorescence in tissue samples:
- Sodium Borohydride Treatment: Aldehyde-induced autofluorescence from Schiff's base formation can be mitigated by treating fixed samples with sodium borohydride, which reduces amine-aldehyde compounds into non-fluorescent salts [90].
- White Light Photobleaching: A recent innovative approach uses high-intensity white LED light to nearly eliminate lipofuscin autofluorescence in human tissue, including highly impacted Alzheimer's brain tissue. This simple, cost-effective protocol performed before staining significantly increases signal-to-noise ratio without adverse effects on target signal or tissue integrity [93].
- Chemical Quenching: Incubating samples with 5% H₂O₂ or treating with Sudan black B can effectively reduce autofluorescence from various sources [90].
- Alternative Fixation Methods: Replacing aldehyde fixatives with organic solvents such as ice-cold methanol can prevent the formation of fluorescent Schiff's bases altogether [90].
Spectral and Fluorophore Selection Strategies
Strategic experimental design can minimize interference from autofluorescence:
- Near-Infrared Fluorophores: Selecting fluorophores that emit in the near-infrared (NIR) range, where tissue autofluorescence is significantly reduced, can dramatically improve signal-to-background ratios [90].
- Spectral Separation: Choosing fluorophores whose emission spectra are distinct from observed autofluorescence patterns helps avoid spectral overlap [90].
- Anti-GFP Antibody Conjugates: When using GFP tags, employing antibody conjugates that shift detection away from the green channel can circumvent interference in this problematic spectral region [90].
Instrumentation and Detection Approaches
Advanced instrumentation provides additional solutions:
- Spectral Unmixing: Spectral flow cytometry or imaging systems can mathematically separate autofluorescence signatures from specific signals based on their full spectral profiles rather than single emission peaks [95].
- Fluorescence Lifetime Imaging (FLIM): This technique separates signals based on fluorescence decay rates rather than just spectral characteristics, enabling discrimination between autofluorescence and specific labels even with overlapping emission spectra [90].
- Photobleaching Protocols: Controlled exposure to high-intensity light prior to antibody incubation can reduce autofluorescence by photobleaching endogenous fluorophores [90].
Table 2: Autofluorescence Mitigation Techniques Comparison
| Method | Mechanism | Best For | Limitations |
|---|---|---|---|
| White Light Photobleaching [93] | Photochemical reduction of fluorophores | Human nervous system tissue, aged tissue, lipofuscin | Requires optimization of exposure time |
| Sodium Borohydride Treatment [90] | Chemical reduction of Schiff's bases | Aldehyde-fixed tissues | May affect some epitopes |
| Sudan Black B Incubation [90] | Chemical quenching | Broad-spectrum autofluorescence | May require concentration optimization |
| Spectral Unmixing [95] | Computational separation | Complex samples with multiple fluorophores | Requires specialized equipment/software |
| NIR Fluorophores [90] | Spectral avoidance | All applications, especially deep tissue | Limited fluorophore choices in NIR range |
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Autofluorescence Management
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Sodium Borohydride | Reduces fluorescent Schiff's bases formed by aldehyde fixation | Use on aldehyde-fixed tissues; prepare fresh solutions [90] |
| Sudan Black B | Chemical quencher of broad-spectrum autofluorescence | Particularly effective for lipofuscin; requires concentration optimization [90] |
| Hydrogen Peroxide (5%) | Oxidizes and reduces autofluorescence | Can be used overnight incubation; may affect some epitopes [90] |
| Methanol (Ice-cold) | Alternative fixative avoiding aldehyde artifacts | Prevents formation of Schiff's bases; may not preserve all antigens equally [90] |
| Glass-bottomed Culture Dishes | Reduce container autofluorescence | Replace fluorescent plasticware for imaging [90] |
| Phenol Red-free Media | Eliminates medium-derived background | Essential for live-cell imaging [90] |
| Autofluorescence Explorer Software | Spectral unmixing of AF signatures | Available on spectral cytometers (Aurora, ID7000) [95] |
Integration with Broader Immunochemistry Principles
Effective management of autofluorescence must be integrated with core immunochemistry principles throughout the experimental workflow. Tissue handling and fixation processes significantly impact both antigen preservation and autofluorescence. Inadequate fixation or processing can create tissue artifacts that exacerbate autofluorescence issues [14]. Similarly, proper epitope retrieval techniques must balance the need for antigen exposure with potential induction of autofluorescence [29].
Quality control measures fundamental to immunochemistry are equally critical for autofluorescence management. Appropriate use of positive controls (tissues known to express the target antigen) and negative controls (omitting primary antibody) are essential for validating staining patterns and distinguishing specific signal from background [14] [29]. The increasing integration of digital pathology and artificial intelligence with IHC holds promise for automated detection of artifacts and improved standardization of autofluorescence assessment [14].
The relationship between autofluorescence and tissue pathology is an emerging area of interest. A 2025 study demonstrated that specific autofluorescence signatures, particularly from tryptophan and elastin, correlate strongly with atherosclerotic pathology in human aorta, predicting 58% of the variance in intima thickness [91]. This suggests that autofluorescence, rather than being merely a nuisance, may potentially provide valuable diagnostic information when properly characterized.
Autofluorescence remains a significant challenge in fluorescent IHC, but a systematic approach combining appropriate sample preparation, strategic fluorophore selection, and advanced detection methodologies can effectively mitigate its impacts. The researcher's comprehensive strategy should begin with proper assessment using unstained controls, implement relevant mitigation techniques based on the specific autofluorescence sources present, and employ appropriate instrumentation and computational tools when available.
Future developments in autofluorescence management will likely include more sophisticated computational approaches for artifact detection and removal, expanded fluorophore options in spectral regions with minimal background, and improved chemical treatments that more specifically target autofluorescent compounds without affecting antigen integrity. Furthermore, the growing recognition that autofluorescence signatures themselves may contain biologically and clinically relevant information opens new research avenues where this traditionally problematic phenomenon can be transformed into a valuable diagnostic tool.
The efficacy of immunochemical techniques—including flow cytometry, immunohistochemistry (IHC), and enzyme-linked immunosorbent assay (ELISA)—is fundamentally dependent on two critical optimization processes: the titration of antibody concentrations to maximize specificity and the strategic selection of an appropriate detection system to achieve the desired sensitivity. This guide provides a detailed framework for researchers to systematically optimize these parameters, thereby ensuring the generation of reproducible, high-quality data in both research and diagnostic applications. Adherence to the protocols and principles outlined herein is essential for the accurate interpretation of immunochemical assays.
The Critical Role of Antibody Titration
Antibody titration is not merely a recommendation but a fundamental prerequisite for any rigorous immunochemical experiment. Using antibodies at non-optimized, vendor-suggested concentrations often leads to excessive background noise from off-target binding or insufficient signal from the target antigen [96]. The objective of titration is to identify the antibody concentration that yields the optimal staining index (SI) or signal-to-noise ratio, which maximizes assay sensitivity while conserving reagents and reducing non-specific binding [96].
Quantitative Method for Antibody Titration in Flow Cytometry
The following protocol is designed for titrating antibodies for flow cytometry applications and can be adapted for other techniques.
Materials:
- Cells of interest (with a known positive population for the target antigen)
- Antibody to be titrated
- Staining buffer (e.g., FACS buffer)
- Flow cytometer
Procedure:
- Prepare a Dilution Series: Create a series of doubling dilutions of the antibody in staining buffer. A typical series might include eight dilutions, starting from the vendor's recommended concentration down to a 1:512 dilution.
- Stain Cells: Aliquot a fixed number of cells (e.g., 1 x 10^6) into separate tubes. Stain each pellet with the different antibody dilutions using a consistent staining volume and protocol (including incubation time and temperature) [96].
- Acquire and Analyze Data: Run the samples on a flow cytometer. For each dilution, identify the median fluorescence intensity (MFI) of the positive population (MedPOS) and the negative population (MedNEG). Also, record the value at the 84th percentile of the negative population (84%NEG) [96].
- Calculate the Staining Index (SI): For each antibody dilution, compute the SI using the formula: ( \text{SI} = \frac{\text{Med}{\text{POS}} - \text{Med}{\text{NEG}}}{2 \times (\text{84\%}{\text{NEG}} - \text{Med}{\text{NEG}})} ) [96].
- Plot and Determine Optimal Concentration: Graph the SI against the antibody concentration. The optimal concentration is at the plateau of the titration curve, where the SI is highest and most stable. Using a higher concentration wastes reagent and increases background, while a lower concentration reduces specific signal [96].
Table 1: Example Data from an Antibody Titration Experiment
| Antibody Dilution | MedPOS (MFI) | MedNEG (MFI) | 84%NEG (MFI) | Staining Index (SI) |
|---|---|---|---|---|
| 1:50 | 45,200 | 980 | 1,150 | 26.0 |
| 1:100 | 42,500 | 650 | 780 | 53.7 |
| 1:200 | 38,100 | 520 | 620 | 60.3 |
| 1:400 | 28,400 | 480 | 570 | 49.1 |
| 1:800 | 15,000 | 450 | 530 | 27.4 |
Checkerboard Titration for ELISA Optimization
For ELISA, particularly sandwich formats, a checkerboard titration is used to simultaneously optimize the concentration of both the capture antibody and the detection antibody [97].
Procedure:
- Prepare Dilutions: Prepare a series of dilutions for the capture antibody (e.g., down the columns of a microtiter plate) and a series for the detection antibody (e.g., across the rows).
- Coat and Block: Coat the plate with the capture antibody dilutions, then block.
- Add Antigen: Add a constant, known concentration of antigen to all wells.
- Detect: Apply the different detection antibody dilutions, followed by the enzyme conjugate and substrate, following standard ELISA protocol.
- Analyze: The optimal pair of concentrations is identified by the well that produces the strongest specific signal with the lowest background, providing the best working conditions for the assay [97].
Selecting the Right Detection System
The choice of detection system is a strategic compromise between sensitivity, specificity, multiplexing capability, and the nature of the sample. Systems range from simple direct detection to complex signal amplification methods.
Classification and Comparison of Detection Systems
Table 2: Key Characteristics of Immunohistochemistry Detection Systems
| Detection System | Principle | Sensitivity | Key Advantages | Key Limitations | Best Suited For |
|---|---|---|---|---|---|
| Direct Method | Primary antibody is directly conjugated to an enzyme (HRP) or fluorophore [98] [99]. | Low | Fast; minimal non-specific background; avoids secondary antibody issues [98]. | Low sensitivity; requires conjugation for every primary antibody [98]. | Highly expressed antigens; multiplex immunofluorescence [98]. |
| Indirect Method | Unlabeled primary antibody is detected by a labeled secondary antibody [98] [99]. | Moderate | Higher sensitivity than direct; signal amplification; flexible and cost-effective [98]. | Risk of cross-reactivity; may require additional blocking steps [98]. | Routine IHC/IF; a wide range of applications. |
| Enzyme-Antienzyme Complexes (e.g., PAP, APAAP) | A tertiary complex (e.g., peroxidase-antiperoxidase) is linked via a secondary "bridge" antibody [98]. | High (100-1000x over indirect) [98] | Very high sensitivity; avoids chemical conjugation of primary antibody [98]. | Multi-step, time-consuming; may be less effective on FFPE tissue with some mAbs [98]. | Detecting low-abundance antigens; research on frozen sections [98]. |
| Polymer-Based Systems | Multiple enzymes and secondary antibodies are conjugated to a polymer backbone [99]. | Very High | High sensitivity and specificity; rapid; low background; no endogenous biotin interference [99]. | Typically more expensive than older methods. | Most modern IHC applications, especially on FFPE tissue; preferred for clinical diagnostics [99]. |
| Tyramide Signal Amplification (TSA) | Enzyme (HRP) activates tyramide, depositing numerous labeled molecules near the antigen site [98]. | Extremely High | Exceptional sensitivity for very low-abundance targets [98]. | Can easily produce high background if not optimized; requires careful titration [98]. | Detecting minimally expressed markers; challenging FFPE targets. |
Diagram 1: Detection System Selection Logic
Integrated Workflow for Assay Optimization
A systematic approach combining antibody validation, titration, and detection system selection is crucial for robust assay development. The following workflow integrates these elements.
Diagram 2: Assay Optimization Workflow
Essential Blocking Strategies
Blocking is a critical step to minimize non-specific binding and background signal. The strategy must be tailored to the technique:
- Flow Cytometry: Use sera from the host species of your primary antibodies (e.g., rat and mouse serum for a panel of rat and mouse antibodies) to block Fc receptors. For panels containing polymer-based dyes (e.g., Brilliant Violet), a Brilliant Stain Buffer is essential to prevent dye-dye interactions [100].
- IHC/Immunofluorescence: Use normal serum from the species of the secondary antibody or a commercial protein block to reduce non-specific binding of the secondary antibody. Blocking endogenous peroxidase (for HRP-based systems) or alkaline phosphatase activity with hydrogen peroxide or levamisole, respectively, is also mandatory [20] [99].
The Imperative of Experimental Controls
No optimized assay is complete without proper controls [99]:
- Positive Control: A tissue or cell sample known to express the target antigen validates that the entire staining protocol is working correctly.
- Negative Control: Includes an isotype control (for flow cytometry) or omission of the primary antibody (for IHC). This is essential for distinguishing specific signal from background noise [20] [99].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Immunochemistry Optimization
| Reagent / Solution | Function / Purpose | Example Use Case |
|---|---|---|
| Normal Sera | Blocks Fc receptors and non-specific binding sites on cells/tissues. | Preparing blocking solution for flow cytometry [100] or IHC [20]. |
| Brilliant Stain Buffer | Prevents fluorophore-fluorophore interactions between polymer dyes. | Essential for multicolor flow cytometry panels containing "Brilliant" dyes (e.g., BV421, BV605) [100]. |
| Tandem Stabilizer | Prevents the degradation of tandem fluorophores (e.g., PE-Cy7, APC-Cy7). | Added to antibody cocktails and storage buffers to maintain signal integrity [100]. |
| CellBlox | A blocking reagent designed to prevent non-specific binding for specific dye families (e.g., NovaFluors). | Used in flow cytometry panels containing NovaFluor dyes [100]. |
| Protein Block | A generic protein solution (e.g., BSA, non-fat milk) to coat non-specific binding sites. | Reducing background staining in IHC and ELISA [20] [101]. |
| Enzyme Blockers | Inhibits endogenous enzyme activity (e.g., peroxidase, phosphatase). | Hydrogen peroxide block for IHC with HRP detection [20] [99]. |
| Antigen Retrieval Buffers | Reverses formaldehyde-induced cross-links to expose hidden epitopes. | Heat-Induced Epitope Retrieval (HIER) for IHC on FFPE tissue [20]. |
| Chromogens | Enzyme substrates that produce an insoluble, colored precipitate. | DAB (brown) or AP/RED (red) for visualizing target antigen in IHC [20] [99]. |
The meticulous optimization of antibody concentrations and the informed selection of detection systems are non-negotiable pillars of reliable immunochemistry. By systematically applying titration protocols to determine the optimal staining index and by strategically choosing a detection system based on a clear understanding of the required sensitivity and sample characteristics, researchers can significantly enhance the quality, reproducibility, and interpretability of their data. This guide provides a foundational framework for these processes, empowering scientists to build robust and validated immunochemical assays for both research and clinical applications.
In the scientific method, experimental controls serve as critical reference points that anchor new findings to established knowledge, providing an objective, systematic framework for interpreting data [102]. They are fundamental to scientific rigor, eliminating alternate explanations for experimental results and helping to validate both the performance of the experimental setup and the reliability of its outcomes [103]. Without controls, experiments lack this rigor and may lead to misleading conclusions, rendering them essentially worthless from a scientific standpoint [102]. In disciplines like immunochemistry, where techniques such as Immunohistochemistry (IHC), Western Blot (WB), and Enzyme-Linked Immunosorbent Assay (ELISA) are pivotal, the use of appropriate controls is a standard practice. These controls are indispensable for confirming the validity of results, minimizing the effects of variables other than the independent variable, and controlling for uncontrolled bias and systematic error [103] [104].
Controls primarily fall into two categories: positive controls and negative controls. A positive control is designed to produce an expected result, thereby verifying that the experimental protocol, reagents, and equipment are functioning correctly. Conversely, a negative control is characterized by the absence of a key reagent or treatment necessary for a positive outcome. It is not expected to produce the result and thus serves as a "baseline," helping to identify non-specific signals or false-positive reactions [103]. The strategic implementation of both control types is essential for demonstrating the sensitivity and specificity of any diagnostic test [104].
The Critical Role of Controls in Scientific Discovery
Interpreting Experimental Outcomes Through Controls
The validity of results from a treatment group is critically assessed by examining the outcomes of both positive and negative controls run concurrently. The interplay between these controls allows researchers to determine whether observed effects are true or artifacts. The table below outlines how to interpret experimental results based on control outcomes.
Table 1: Interpretation of Experimental Results Based on Control Group Outcomes
| Positive Control | Negative Control | Treatment Group | Outcome Interpretation |
|---|---|---|---|
| + | + | - | False-positive present. Potential causes: use of inappropriately high antibody concentration, non-specific antibody-antigen binding, or interfering buffer components [103]. |
| - | + | - | False-negative indicated. The experimental protocol requires optimization [103]. |
| + | - | - | The procedure is working and optimized. The negative result from the treatment is valid (true negative), indicating the treatment had no effect [103]. |
| + | - | + | The procedure is working and optimized. The positive result is valid (true positive), confirming the treatment produced an effect [103]. |
| + | + | + | The positive result may be due to false-positive or non-specific signal. A confounding variable is likely involved, meaning the positive results are not solely due to the treatment [103]. |
When Controls Fail: Catalyzing Paradigm Shifts
While controls are typically expected to behave predictably, their failure can sometimes signal a flaw in established knowledge rather than the experiment itself. History shows that investigating failed controls has led to groundbreaking discoveries.
The Discovery of Catalytic RNA: In the late 1970s, Tom Cech's team observed that splicing of Tetrahymena rRNA occurred even in a negative control reaction lacking nuclear extract [102]. Instead of dismissing the result, they pursued it and proved the RNA was splicing itself, independent of proteins. Simultaneously, Sydney Altman's group found that the RNA component of RNase P was catalytically active on its own in their negative controls [102]. These failed negative controls led to the once-heretical conclusion that RNA can act as an enzyme, a discovery that earned them the 1989 Nobel Prize in Chemistry and gave rise to the "RNA world" hypothesis [102].
Uncovering a Universal Oxygen-Sensing Mechanism: Peter Ratcliffe's group, while studying the regulation of the erythropoietin (EPO) gene, encountered a failed negative control. They found that a reporter gene linked to the EPO enhancer exhibited oxygen-sensitive activity even in cell lines not producing EPO, where the oxygen-sensing system was presumed absent [102]. This indicated that the oxygen-sensing mechanism was universal. This discovery unraveled the pathway involving HIF-1 (hypoxia-inducible factor 1) and earned Ratcliffe, Gregg Semenza, and William Kaelin the 2019 Nobel Prize in Physiology or Medicine [102].
These examples underscore that while controls are essential for validating expected results, a rigorous investigation of their unexpected failure can open entirely new fields of research.
Implementing Controls in Key Immunochemistry Techniques
Controls for Immunohistochemistry (IHC)
Running appropriate controls in IHC is critical for confirming the validity of the observed staining pattern and ensuring accurate interpretation. The selection of controls should be based on "fit-for-use" principles to ensure specificity and avoid non-specific signals [103] [104].
Table 2: Established Controls for Immunohistochemistry (IHC)
| Type of Control | Specific Control | Description | Purpose |
|---|---|---|---|
| Tissue Controls | Positive Tissue Control | Tissue section known to express the target protein [103]. | Confirms the staining protocol is successful and provides expected sensitivity/specificity. Validates that negative results are accurate [103]. |
| Negative Tissue Control | Tissue section known not to express the target protein [103]. | Checks for non-specific signal and false-positive results [103]. | |
| Reagent Controls | No Primary Antibody Control | Tissue section incubated with antibody diluent alone, followed by secondary antibody and detection reagents [103]. | Ensures staining is not produced by the detection system or non-specific binding of the secondary antibody [103]. |
| Isotype Control | Tissue section incubated with a non-immune antibody of the same isotype and concentration as the primary antibody [103]. | Ensures observed staining is not caused by non-specific interactions of the antibody with the tissue. Primarily for monoclonal antibodies [103]. | |
| Absorption Control | Tissue section incubated with primary antibody that has been pre-absorbed (blocked) with its purified immunogen [103]. | Demonstrates staining specificity. Little to no staining is expected, confirming the primary antibody binds specifically to the target antigen [103]. |
The following workflow outlines the logical decision process for establishing IHC controls:
Controls for Western Blot (WB)
Western Blot analysis requires multiple control types to support the specificity of the analysis and enable accurate protein quantification.
Table 3: Established Controls for Western Blot (WB)
| Type of Control | Description | Purpose |
|---|---|---|
| Positive Control Lysate | Lysate from a cell line or tissue known to express the target protein. Common examples: cells overexpressing the target, proven positive cell lines, or purified recombinant protein [103]. | Demonstrates the staining protocol is successful and provides the expected sensitivity. Confirms that negative results in test samples are accurate [103]. |
| Negative Control Lysate | Lysate from a knockout/knockdown cell line or tissue known not to express the target protein [103]. | Checks for non-specific binding and false-positive results [103]. |
| Loading Control | Antibodies to housekeeping proteins (e.g., GAPDH, Actin, Tubulin) that are constitutively expressed at relatively constant levels [103]. | Confirms equal protein loading and efficient transfer across all lanes. Validates that observed differences in target protein are real and not due to loading errors [103]. |
| No Primary Antibody Control | A strip of the membrane is incubated without the primary antibody (only with antibody dilution buffer), but with the secondary antibody [103]. | Checks for non-specific binding (false positives) caused by the secondary antibody [103]. |
Table 4: Commonly Used Loading Controls for Western Blot
| Sample Type | Protein | Molecular Weight (kDa) |
|---|---|---|
| Whole-cell / Cytoplasmic | β/α-Actin | 43 [103] |
| GAPDH | 30-40 [103] | |
| β/α-Tubulin | 55 [103] | |
| Nuclear | Lamin B1 | 66 [103] |
| Histone H3 | 18 [103] | |
| Mitochondrial | VDAC1/Porin | 31 [103] |
| HSP60 | 60 [103] |
Controls for ELISA
To verify that an ELISA is performing accurately, several control samples are used to monitor different aspects of the assay.
Table 5: Established Controls for ELISA
| Type of Control | Description | Purpose |
|---|---|---|
| Positive Control | An endogenous sample known to contain the target protein, or a purified protein/peptide containing the immunogen sequence [103]. | Verifies the assay protocol is successful and provides the expected level of sensitivity/specificity. Confirms that negative results are accurate [103]. |
| Negative Control | Lysate from a source known not to express the target protein. Common examples: Zero blank & chromogen blank [103]. | Checks for non-specific signal and false-positive results. Helps identify the cause of high background [103]. |
| Standard Control | Contains a known, precise concentration of the target protein [103]. | Necessary for quantification. Used to generate a standard curve. An R² value >0.99 for the trend line indicates a good curve and adequate antibody binding [103]. |
| Spike Control | A known amount of the standard diluted into serum from the species being tested [103]. | Tests for matrix effects that could interfere with the assay. Demonstrates the target protein is recoverable; an acceptable recovery is typically 80–120% [103]. |
The Researcher's Toolkit: Essential Reagent Solutions
The selection and validation of high-quality reagents, particularly antibodies, is as critical as the experimental design itself. Using inappropriate reagents is a common source of problematic results. The following table details key research reagent solutions used in immunochemistry experiments.
Table 6: Key Research Reagent Solutions for Immunochemistry
| Reagent / Material | Function / Purpose | Key Considerations |
|---|---|---|
| Primary Antibody | Binds specifically to the target protein (antigen) of interest [103]. | Critical to select a high-quality antibody validated for the specific application (IHC, WB, ELISA). Source, clonality, host species, and concentration must be optimized [103]. |
| Secondary Antibody | Binds to the primary antibody and is conjugated to a detection molecule (e.g., enzyme, fluorophore) [103]. | Must be raised against the host species of the primary antibody. Conjugate type determines detection method (e.g., HRP for chemiluminescence, fluorophores for fluorescence) [103]. |
| Positive Control Lysate/Lysate | A characterized sample known to express the target protein, used to confirm assay functionality [103]. | Can be from overexpressing cell lines, tissues with proven expression, or purified recombinant protein. Should be matched to the species and sample type being tested [103]. |
| Negative Control Lysate | A characterized sample known not to express the target protein, used to check for non-specificity [103]. | Ideal sources are knockout or knockdown cell lines. Essential for establishing assay specificity and identifying false positives [103]. |
| Loading Control Antibody | An antibody against a ubiquitously expressed housekeeping protein for Western Blot normalization [103]. | Target should have a substantially different molecular weight than the protein of interest to avoid overlapping bands. Must be highly expressed in the sample type [103]. |
| Isotype Control | A non-immune immunoglobulin that matches the primary antibody's isotype, host species, and conjugation [103]. | Used primarily in IHC/IF to control for non-specific Fc receptor binding or background staining caused by the antibody itself [103]. |
| Detection Reagents | Substrates (e.g., chromogenic, chemiluminescent) that generate a measurable signal from the enzyme conjugate [103]. | Choice depends on application (microscopy vs. imaging) and required sensitivity. Must be fresh and prepared correctly for optimal performance [103]. |
| Blocking Solution | A solution of protein (e.g., BSA, serum) used to occupy non-specific binding sites on the tissue or membrane [103]. | Reduces background staining. The protein used should not interfere with the antibodies (e.g., use normal serum from the secondary antibody host species) [103]. |
A general workflow for implementing controls in a protein detection experiment, applicable across techniques, can be visualized as follows:
The consistent and thoughtful implementation of positive and negative controls is a non-negotiable component of rigorous scientific research, particularly in immunochemistry. Controls are not merely a procedural formality but are fundamental to validating experimental findings, optimizing protocols, troubleshooting problems, and ultimately, drawing accurate and reliable conclusions. As demonstrated, the strategic use of technique-specific controls—ranging from tissue and reagent controls in IHC to loading and lysate controls in WB—provides the necessary evidence for the sensitivity and specificity of an assay. Furthermore, while controls are designed to confirm expectations, the scientific community must remain open to the profound discoveries that can emerge when these controls fail unexpectedly. By adhering to the principles and methodologies outlined in this guide, researchers and drug development professionals can ensure the integrity of their work, uphold the highest standards of quality, and contribute robust, trustworthy data to the advancement of science and medicine.
Ensuring Reliability: Validation Standards and Comparative Analysis of Immunoassays
Assay validation is a fundamental process in scientific research and clinical diagnostics, providing objective evidence that an analytical method fulfills the requirements for its intended use. This process is particularly critical in immunochemistry, where techniques such as immunohistochemistry (IHC), enzyme-linked immunosorbent assay (ELISA), and immunofluorescence rely on precise antigen-antibody interactions to generate reliable data [14] [105]. Validation ensures that the results generated are not only scientifically sound but also reproducible across different laboratories and under varying conditions [106].
The core principle of assay validation establishes that the process is not a one-time event but rather a continuous, incremental process that requires constant vigilance and maintenance [106]. As defined by regulatory agencies, validation confirms through documented investigation that the performance characteristics of a method are suitable for its intended analytical application [107]. In practical terms, this means that a properly validated assay should consistently deliver accurate results that correctly classify samples according to the true biological status of the subject, whether for diagnostic purposes, drug development, or basic research [106].
For researchers in immunochemistry, validation is foundational to generating meaningful results. Techniques like IHC combine principles from histology, immunology, and biochemistry to detect specific antigens within tissue samples, providing invaluable information about protein localization and expression levels [14] [15]. However, without proper validation, even the most technically sophisticated assays can produce misleading results due to non-specific staining, cross-reactivity, or inadequate sensitivity [14] [45]. Therefore, understanding and implementing the core principles of specificity, sensitivity, and reproducibility is essential for any researcher working with immunochemical methods.
Core Principles of Assay Validation
Specificity
Specificity refers to the ability of an assay to exclusively detect and measure the target analyte in the presence of other components that may be expected to be present in the sample matrix [107] [108]. In immunochemical methods, this principle is demonstrated by the specific binding of an antibody to its target antigen without cross-reacting with other molecules [14] [45].
For immunohistochemistry and related techniques, specificity ensures that the observed staining pattern truly represents the distribution of the target antigen rather than non-specific background or cross-reactivity with similar epitopes [14]. Challenges to specificity in immunochemistry include non-specific antibody binding, endogenous enzyme activity, and autofluorescence in fluorescent-based detection methods [45]. These can be addressed through careful antibody selection, appropriate blocking steps, optimization of washing protocols, and using controls to identify and minimize interfering factors [14] [45].
Sensitivity
Sensitivity defines the lowest concentration of an analyte that an assay can reliably detect (limit of detection, LOD) and quantify (limit of quantitation, LOQ) [107] [108]. The LOD is typically defined as the lowest concentration that can be detected but not necessarily quantified, usually with a signal-to-noise ratio of 3:1, while the LOQ represents the lowest concentration that can be quantified with acceptable precision and accuracy, typically with a signal-to-noise ratio of 10:1 [107].
In immunochemistry, sensitivity is influenced by multiple factors including antibody affinity, efficiency of antigen retrieval (particularly in formalin-fixed, paraffin-embedded tissues), signal amplification methods, and detection system efficiency [14] [15]. The indirect detection method, which uses a labeled secondary antibody that binds to the primary antibody, generally provides higher sensitivity than direct methods due to signal amplification through multiple secondary antibodies binding to each primary antibody [45].
Reproducibility
Reproducibility encompasses the closeness of agreement between test results when the same method is applied repeatedly to multiple samplings of homogeneous samples under stipulated conditions [105] [107]. This principle is typically evaluated at three levels: repeatability (intra-assay precision), intermediate precision (inter-assay precision), and reproducibility (inter-laboratory precision) [107].
For immunochemical techniques, reproducibility can be affected by variations in tissue processing, fixation times, antibody lots, incubation conditions, and analyst technique [14] [15]. Maintaining reproducibility requires careful standardization of protocols and environmental conditions, as well as rigorous quality control measures including the consistent use of positive and negative controls [14].
Table 1: Key Validation Parameters and Their Definitions
| Parameter | Definition | Importance in Immunochemistry |
|---|---|---|
| Specificity | Ability to measure analyte accurately in presence of interfering components | Ensures staining represents true antigen distribution rather than cross-reactivity or non-specific binding |
| Sensitivity | Lowest concentration of analyte that can be reliably detected/quantified | Determines ability to detect low-abundance antigens; critical for biomarkers with low expression levels |
| Precision | Closeness of agreement between independent test results | Ensures consistent results across different experiments, operators, and laboratories |
| Accuracy | Closeness of measured value to true concentration | Validates that staining intensity correlates with actual antigen concentration |
| Robustness | Capacity to remain unaffected by small variations in method parameters | Assesses method reliability despite minor changes in protocol conditions |
Experimental Protocols for Validation
Establishing Specificity
For immunochemical methods, specificity is demonstrated through a series of controlled experiments that confirm the antibody binds exclusively to its intended target:
- Absorption Test: Pre-absorb the primary antibody with an excess of the purified target antigen prior to application on tissue sections. The result should show complete or significant loss of staining, demonstrating that the observed signal is specific to the target antigen [14].
- Negative Controls: Omit the primary antibody or replace it with an isotype-matched irrelevant antibody at the same concentration. Any remaining staining indicates non-specific binding of secondary antibodies or endogenous activity that needs to be addressed through blocking [14] [15].
- Cross-reactivity Testing: Evaluate the assay against a panel of related antigens or tissues known to express similar epitopes to demonstrate minimal cross-reactivity [108].
- Genetic Controls: When possible, use knockout tissues or cell lines lacking the target antigen to confirm absence of staining [14].
- Multi-site Validation: Use antibodies that recognize different epitopes on the same target antigen to confirm consistent staining patterns [14].
For immunohistochemistry, proper antigen retrieval methods must be optimized and standardized, as both insufficient and excessive retrieval can alter antibody specificity [14] [15]. Enzymatic retrieval (e.g., proteinase K) or heat-induced epitope retrieval (HIER) should be carefully calibrated for each antibody-antigen pair [15].
Determining Sensitivity
The sensitivity of immunochemical assays is determined through systematic dilution experiments:
- Limit of Detection (LOD): Prepare serial dilutions of a known antigen standard in the appropriate matrix. The LOD is typically defined as the lowest concentration that produces a signal statistically significantly different from the negative control (usually with 95% confidence). For quantitative assays, this is often determined using the formula: LOD = 3.3 × (SD of the blank response/slope of the calibration curve) [107] [108].
- Limit of Quantification (LOQ): Similarly determined using serial dilutions, the LOQ is the lowest concentration that can be quantified with acceptable precision (typically ≤20% CV) and accuracy (typically 80-120% of the theoretical value). The formula is often: LOQ = 10 × (SD of the blank response/slope of the calibration curve) [107] [108].
- Titration Curve: For semi-quantitative IHC, perform antibody titrations to identify the optimal dilution that provides the strongest specific signal with minimal background. The sensitivity endpoint is the highest dilution that still produces detectable specific staining [14] [15].
- Signal-to-Noise Optimization: Compare the specific staining intensity to background staining across different antigen concentrations. The optimal conditions provide the highest signal-to-noise ratio across the dynamic range of the assay [108].
Assessing Reproducibility
Reproducibility testing evaluates consistency across different experimental conditions:
- Repeatability (Intra-assay Precision): Analyze the same sample multiple times within the same assay run (e.g., multiple wells on the same ELISA plate or multiple sections from the same block in IHC). Calculate the coefficient of variation (CV) among replicates, which should generally be <15% for quantitative assays [107] [108].
- Intermediate Precision (Inter-assay Precision): Analyze the same samples across different assay runs performed on different days, by different analysts, or using different reagent lots. The CV for intermediate precision should generally be <20% [107] [108].
- Reproducibility (Inter-laboratory Precision): For methods intended for multi-center use, conduct studies across different laboratories using the same protocol and samples. This represents the strictest measure of precision [105] [107].
- Sample Preparation Consistency: For IHC, test how variations in fixation time, processing conditions, and section thickness affect staining results to establish acceptable ranges for these pre-analytical variables [14] [15].
Table 2: Experimental Design for Precision Studies
| Precision Type | Experimental Approach | Acceptance Criteria | Application in Immunochemistry |
|---|---|---|---|
| Repeatability | Multiple replicates of the same sample within one assay run | CV < 15% | Multiple wells in same ELISA plate; adjacent tissue sections stained simultaneously |
| Intermediate Precision | Same samples analyzed in different runs (different days, analysts, equipment) | CV < 20% | Staining performed on different days with different reagent lots by different technologists |
| Reproducibility | Collaborative study across multiple laboratories | CV < 25% | Multi-center validation of a new IHC marker or diagnostic antibody |
Validation Workflows and Quality Control
The validation process follows a logical sequence from initial optimization through final implementation. The following workflow diagrams illustrate the key stages in assay validation and the essential quality control components.
Diagram 1: Assay Validation Workflow - This diagram illustrates the sequential stages of assay validation from defining intended use through to implementation with quality control measures.
Diagram 2: Quality Control Framework - This diagram shows the essential components of a quality control system for immunochemical assays, spanning pre-analytical, analytical, and post-analytical phases.
The Scientist's Toolkit: Essential Research Reagents
Successful assay validation in immunochemistry requires careful selection and standardization of reagents. The following table outlines essential materials and their functions in validation experiments.
Table 3: Essential Research Reagents for Immunochemistry Validation
| Reagent Category | Specific Examples | Function in Validation | Optimization Considerations |
|---|---|---|---|
| Primary Antibodies | Monoclonal, polyclonal, recombinant | Bind specifically to target antigen | Titrate for optimal signal-to-noise; validate specificity using knockout controls |
| Secondary Antibodies | HRP-conjugated, AP-conjugated, fluorescently-labeled | Detect primary antibody binding | Ensure species specificity; optimize concentration to minimize background |
| Detection Systems | DAB, AEC, fluorescent substrates | Visualize antigen-antibody complexes | Match substrate sensitivity to antigen abundance; compare different systems |
| Blocking Reagents | BSA, normal serum, commercial blockers | Reduce non-specific binding | Test different blockers and concentrations for optimal specific signal |
| Antigen Retrieval | Citrate buffer, EDTA, proteinase K | Unmask epitopes in fixed tissues | Optimize method (HIER vs. enzymatic), time, and temperature for each target |
| Mounting Media | Aqueous, organic, anti-fade | Preserve staining and enable visualization | Select based on detection method (brightfield vs. fluorescence) |
| Control Materials | Cell lines, tissue microarrays, purified antigens | Validate assay performance | Ensure controls represent relevant expression levels and staining patterns |
Regulatory and Standardization Frameworks
Assay validation in regulated environments must adhere to guidelines established by authorities such as the U.S. Food and Drug Administration (FDA), European Medicines Agency (EMA), and International Conference on Harmonisation (ICH) [105] [109] [108]. These guidelines provide frameworks for validating analytical methods used in pharmaceutical development, clinical diagnostics, and biomedical research.
According to these regulatory standards, full validation is required for novel in-house developed methods, while partial validation may suffice when implementing commercially developed assays in a new laboratory setting [105]. The extent of validation should always be commensurate with the intended use of the assay, with diagnostic applications typically requiring more rigorous validation than research applications [105].
For immunochemistry methods, adherence to Good Laboratory Practice (GLP) principles is essential for generating reliable data. This includes maintaining detailed records of validation procedures, establishing acceptance criteria prior to validation experiments, documenting all deviations from protocols, and implementing change control procedures for validated methods [105] [108]. Proper documentation should demonstrate that the method consistently performs as intended and meets all predefined acceptance criteria for critical validation parameters.
Standardization initiatives, such as those developed by the BIOMARKAPD project for neurodegenerative disease biomarkers, aim to harmonize validation procedures across laboratories to ensure comparable results [105]. These efforts include developing standard operating procedures (SOPs) for validation parameters and establishing reference measurement procedures and certified reference materials [105].
The principles of assay validation—specificity, sensitivity, and reproducibility—form the foundation of reliable immunochemical methods in both research and clinical applications. Establishing these parameters through systematic experimentation ensures that assays generate accurate, meaningful data that can be trusted for scientific conclusions and diagnostic decisions. As immunochemical techniques continue to evolve with advancements in multiplexing, digital pathology, and artificial intelligence, the fundamental importance of rigorous validation remains constant. By adhering to established validation frameworks and maintaining continuous quality assessment, researchers can confidently employ these powerful techniques to advance scientific knowledge and improve patient care.
Immunohistochemistry (IHC) combines histological, immunological, and biochemical methods to detect specific antigens within tissue sections, providing critical diagnostic, prognostic, and predictive information in anatomic pathology and research [14]. This powerful technique allows for the localization of specific proteins within the context of preserved tissue morphology, making it indispensable for tumor classification, identification of infectious agents, and assessment of therapeutic biomarkers [15]. However, the multistep nature of IHC—encompassing tissue collection, fixation, processing, staining, and interpretation—introduces multiple potential variables that can compromise result accuracy and reproducibility [14]. Quality control (QC) and quality assurance (QA) protocols are therefore essential to ensure that IHC results are reliable, consistent, and clinically actionable.
Without rigorous QC measures, common errors such as non-specific staining, high background, weak signals, and tissue artifacts can substantially affect the accuracy and biological interpretation of IHC results [14]. The College of American Pathologists (CAP) establishes evidence-based guidelines and protocols that place emphasis on the pathologist's role in ensuring accurate diagnoses and optimal patient care [110]. This technical guide examines the comprehensive QC framework for IHC, encompassing guidelines from professional organizations such as CAP, detailed methodologies for implementation, and emerging trends that are shaping the future of quality assurance in immunohistochemistry.
CAP Guidelines and Quality Measures for IHC
Cancer Protocol Templates and Reporting Standards
The CAP Cancer Protocols provide detailed guidelines for collecting essential data elements for complete reporting of malignant tumors, incorporating the latest standards from the World Health Organization Classification of Tumors and the American Joint Committee on Cancer Staging Manual [111]. These protocols are regularly updated to reflect advances in cancer reporting, with recent revisions impacting IHC quality assurance. Laboratories and hospitals rely on these synoptic reporting templates to comply with requirements for organizations like the American College of Surgeons Commission on Cancer and the CAP Laboratory Accreditation Program [111].
Recent updates to CAP Biomarker Reporting Protocols demonstrate the evolving nature of IHC quality standards. For gynecologic biomarkers, CAP now requires additional validation steps; HER2 In Situ Hybridization Testing Status must be reported for equivocal (score 2+) protein overexpression in HER2 status for trastuzumab use, and MLH1 Promoter Methylation Analysis Status is required when reporting loss of nuclear expression of MLH1 and PMS2 in immunohistochemistry interpretation for mismatch repair proteins [111]. Similarly, the General IHC Quantitative Biomarkers protocol has been enhanced with optional cold ischemic time, fixative, and fixation time reporting, acknowledging the impact of pre-analytical variables on IHC quality [111].
Pathology Quality Measures and MIPS Reporting
CAP establishes specific quality measures for pathologists participating in the Merit-based Incentive Payment System (MIPS), providing a structured framework for evaluating performance in key areas of immunohistochemistry and pathology reporting [112]. These measures include both MIPS clinical quality measures and CAP-developed qualified clinical data registry measures available exclusively through the Pathologists Quality Registry.
Table 1: Selected CAP Quality Measures Relevant to IHC and Pathology Reporting
| Measure Number | Measure Name | Reporting Method | 2025 Updates |
|---|---|---|---|
| QPP 249 | Barrett Esophagus Pathology Reporting | Registry and Claims | Specimen site other than anatomic location of esophagus now a Denominator Exception |
| QPP 250 | Radical Prostatectomy Pathology Reporting | Registry and Claims | - |
| QPP 395 | Lung Cancer Reporting (Biopsy/Cytology Specimens) | Registry and Claims | - |
| QPP 396 | Lung Cancer Reporting (Resection Specimens) | Registry and Claims | - |
| QPP 491 | Mismatch Repair or Microsatellite Instability Biomarker Testing Status | Registry Specifications | Historical benchmark established in 2025 |
| CAP 34 | Molecular Assessment Biomarkers Non-Small Cell Lung Cancer | Pathologists Quality Registry | Denominator statement amended to include cytology specimens |
| CAP 42 | Barrett's Esophagus Complete Analysis with Appropriate Consultation | Pathologists Quality Registry | Denominator expanded to all cases of Barrett's Esophagus |
These measures reflect CAP's focus on standardizing reporting for specific cancer types and biomarker assessments where IHC plays a crucial diagnostic role. For instance, QPP 491 addresses mismatch repair (MMR) or microsatellite instability (MSI) biomarker testing status in colorectal carcinoma, endometrial, gastroesophageal, or small bowel carcinoma—contexts where IHC is frequently employed for initial screening [112]. The ongoing refinement of these measures, such as the 2025 expansion of CAP 42 to all Barrett's Esophagus cases, demonstrates CAP's commitment to evolving quality standards based on emerging evidence and clinical needs [112].
Comprehensive Quality Control Framework for IHC
Pre-Analytical Controls
The foundation of reliable IHC begins with rigorous pre-analytical controls. Tissue handling and fixation are crucial steps in preserving cellular integrity and preventing degradation during sample processing [14]. Chemical fixation, most commonly with 10% neutral-buffered formalin, stabilizes cells and tissues while preserving morphological detail for diagnosis and specialized testing [14]. Adequate sample size and fixative volume are essential for effective fixation, ensuring thorough penetration of the fixative. Under-fixation may result in poor tissue preservation, while over-fixation can mask antigens, leading to false-negative results [15].
Antigen retrieval represents another critical pre-analytical step, as formalin fixation can mask antigenic sites through protein cross-linking. Heat-induced epitope retrieval using microwave or pressure cooker methods has largely superseded enzymatic digestion as the preferred approach for most antigens [14]. The selection of appropriate retrieval buffer (e.g., citrate, EDTA, or Tris-EDTA) and optimization of heating time and temperature require systematic validation for each antibody and tissue type.
Analytical Controls and Validation
During the analytical phase, controls are essential for verifying staining specificity and assay performance. Positive controls, consisting of tissues or cells known to express the target antigen, validate staining patterns and intensity while confirming protocol and reagent functionality [14]. Negative controls, in which the primary antibody is omitted or replaced with an isotype-matched non-immune immunoglobulin, assess background staining levels and identify non-specific binding [14]. Utilizing both control types confirms the specificity and sensitivity of the IHC assay.
Table 2: Essential Research Reagent Solutions for IHC Quality Control
| Reagent Category | Specific Examples | Function in QC Process |
|---|---|---|
| Primary Antibodies | Monoclonal and polyclonal antibodies | Bind specifically to target antigens; require thorough validation for specificity |
| Detection Systems | HRP- or AP-conjugated secondary antibodies | Amplify signal and enable visualization; impact sensitivity and background |
| Chromogenic Substrates | DAB (3,3'-diaminobenzidine), AEC | Produce colored precipitate at antigen site; different substrates offer varying sensitivity and stability |
| Counterstains | Hematoxylin, methyl green | Provide nuclear contrast; must not interfere with chromogen visualization |
| Blocking Reagents | Normal serum, BSA, casein | Reduce non-specific background staining by blocking endogenous proteins |
| Antigen Retrieval Solutions | Citrate buffer, EDTA, Tris-EDTA | Unmask epitopes obscured by formalin fixation; critical for consistent staining |
| Fixatives | 10% neutral-buffered formalin, zinc fixatives | Preserve tissue architecture and antigenicity; impact downstream staining quality |
The CAP guidelines emphasize that antibody validation must demonstrate that "an antibody consistently and specifically detects the intended target antigen with appropriate sensitivity and specificity" [113]. This includes characterizing cross-reactivity with similar epitopes and verifying staining patterns across a range of normal and pathological tissues. For predictive biomarkers, such as HER2 or PD-L1, additional validation against clinical outcomes is necessary to establish therapeutic relevance [111].
Post-Analytical Controls and Interpretation
Following staining, standardized interpretation and reporting protocols are essential for minimizing inter-observer variability. Analysis of immunostains in IHC must consider spatial arrangement, percentage of positively stained cells, staining intensity, and established thresholds [14]. The adoption of semi-quantitative scoring systems, such as the Allred score for hormone receptors or the HER2 scoring system, has improved consistency in interpretation, though some subjectivity remains [14].
The integration of digital pathology and artificial intelligence represents a transformative development in post-analytical QC. Digital pathology platforms allow for the scanning and analysis of entire tissue slides, enabling high-throughput image acquisition [14]. AI algorithms can then assist in automated interpretation of complex staining patterns, providing more objective and reproducible quantification of biomarker expression [14]. This approach is particularly valuable for multiplex IHC, where manual analysis of multiple markers becomes prohibitively time-consuming and subjective.
Advanced Techniques and Emerging Directions in IHC QC
Quality Control for Multiplex Immunohistochemistry
Multiplex IHC and immunofluorescence represent advanced applications that enable simultaneous detection of multiple markers within a single tissue section, allowing researchers to define complex immunophenotypes, quantify immune cell subsets, and assess spatial relationships [56]. However, these techniques introduce additional QC challenges, including the need for rigorous validation of each antibody in the multiplex panel, verification that detection systems do not cross-react, and confirmation that staining cycles do not compromise tissue integrity or antigenicity.
The Society for Immunotherapy of Cancer has convened a task force of pathologists and laboratory leaders to develop best practice guidelines for quantitative image analysis of mIHC/IF output and data management considerations [56]. Their recommendations cover image acquisition, color deconvolution and spectral unmixing, tissue and cell segmentation, phenotyping, and algorithm verification. Additional QC measures such as batch-to-batch correction and quality control for assembled images are also addressed [56].
For image acquisition in multiplex IHC, the appropriate per-pixel resolution depends on the specific research question and technology used. Whole slide imaging, although more demanding in terms of time and computation, provides advantages when marker or tissue heterogeneity is high or when complex cell populations are being assessed across multiple large regions [56]. This approach reduces potential region of interest selection bias, which will benefit standardization across studies and institutions as these technologies move toward clinical use.
Regulatory Perspectives and FDA Guidelines
The Food and Drug Administration provides comprehensive guidance for submission of immunohistochemistry applications, outlining the necessary documentation for premarket review [113]. This guidance serves as the special control for class II immunohistochemistry in vitro diagnostic devices under 21 CFR § 864.1860, providing the types and amounts of valid scientific evidence needed to support performance claims for IHC devices [113].
FDA recommendations emphasize comprehensive antibody characterization, including validation and verification of immune reactivity with panels of normal tissues and well-characterized clinical specimens [113]. For class II IHCs with claims for quantitative results for prediction or prognosis of clinically significant outcomes, the FDA requires more extensive validation, including comparison to widely-accepted reference methods and resolution of any discrepancies [113]. These regulatory standards align with and reinforce the QC protocols advocated by CAP and other professional organizations.
IHC Quality Control Workflow
Quality control in immunohistochemistry represents a multifaceted process requiring diligence across pre-analytical, analytical, and post-analytical phases. The guidelines established by the College of American Pathologists, complemented by recommendations from organizations such as the Society for Immunotherapy of Cancer and regulatory frameworks from the FDA, provide a comprehensive structure for ensuring IHC reliability and reproducibility. As IHC technologies evolve, particularly with the advent of multiplex staining and digital pathology, QC protocols must similarly advance to address new challenges and opportunities. By adhering to established guidelines while embracing innovative approaches to quality assurance, laboratories can ensure that IHC remains a robust and trustworthy technique for diagnostic pathology and research applications.
Immunochemical techniques are foundational tools in biomedical research and clinical diagnostics, enabling the specific detection and quantification of target molecules. This whitepaper provides a comparative analysis of two principal methodologies: Immunohistochemistry (IHC), which provides spatial context within a tissue, and immunoassays, such as the Enzyme-Linked Immunosorbent Assay (ELISA) and Radioimmunoassay (RIA), which offer quantitative data from sample solutions. The core principle unifying these techniques is the high-specificity binding between an antibody and its target antigen, but their applications, data output, and technical requirements differ significantly [14] [15]. Understanding the strengths and limitations of each method is crucial for selecting the appropriate technique in drug development and basic research, particularly as the field moves toward greater automation and multiplexing [14] [114].
Immunohistochemistry (IHC)
IHC is a powerful technique that combines histological, immunological, and biochemical methods to detect specific antigens (proteins) directly within tissue sections. Its unique advantage is the preservation of morphological detail, allowing researchers to visualize the distribution and localization of biomarkers within the context of intact tissue architecture and specific cell types [14] [15]. The technique can be performed via direct or indirect methods, with the latter being more common due to signal amplification [14].
- Sample Type: Tissue sections, typically formalin-fixed and paraffin-embedded (FFPE) or frozen [15].
- Detection: Visualization is achieved via chromogenic or fluorescent methods. Chromogenic detection (e.g., using enzymes like Horseradish Peroxidase (HRP) with DAB substrate) produces a colored precipitate visible under a standard light microscope. Fluorescent detection (increasingly termed immunohistofluorescence) uses fluorophore-conjugated antibodies and requires a fluorescence microscope [2] [115].
- Key Output: Semi-quantitative data on protein expression, including subcellular localization, abundance, and distribution in complex tissue environments [2] [14].
Immunoassay Methods: ELISA and RIA
Immunoassays are quantitative techniques used to measure the concentration of an analyte—such as a peptide, protein, antibody, or hormone—in a liquid sample (e.g., serum, urine, or cell lysate) [116] [117]. The assays are typically performed in multi-well plates, allowing for high-throughput analysis.
- Enzyme-Linked Immunosorbent Assay (ELISA): ELISA uses an enzyme-linked antibody as the detection label. The most common format is the sandwich ELISA, which is prized for its high sensitivity and specificity. It involves capturing the target antigen between a solid-phase capture antibody and an enzyme-conjugated detection antibody. The enzyme then converts a substrate into a colored, fluorescent, or luminescent product that can be measured with a plate reader [116].
- Radioimmunoassay (RIA): RIA was one of the first immunoassay techniques developed. It uses a radioactive isotope (most commonly Iodine-125, I-125) as a tracer. In the classic competitive RIA, radiolabeled and unlabeled antigens compete for a limited number of antibody-binding sites. The radioactive signal is inversely proportional to the concentration of the target antigen in the sample [117] [118].
Table 1: Fundamental Characteristics of IHC, ELISA, and RIA
| Feature | Immunohistochemistry (IHC) | ELISA | RIA |
|---|---|---|---|
| Core Principle | Antibody-antigen binding on tissue sections | Antibody-antigen binding on a plate surface | Competition between labeled/unlabeled antigen for antibody binding |
| Sample Type | Tissue sections (FFPE/frozen) | Soluble samples (serum, lysates) | Soluble samples (serum, lysates) |
| Key Output | Protein localization & semi-quantification | Quantitative concentration data | Quantitative concentration data |
| Data Nature | Spatial, contextual, semi-quantitative | Fully quantitative | Fully quantitative |
| Detection Modality | Chromogenic (DAB) or Fluorescent | Colorimetric, Fluorescent, Chemiluminescent | Radioactive decay (Gamma rays) |
| Readout Instrument | Light or Fluorescence Microscope | Spectrophotometer (Plate Reader) | Gamma Counter |
Performance and Analytical Comparison
The choice between IHC, ELISA, and RIA is often dictated by the required analytical performance, including sensitivity, specificity, and throughput.
- Sensitivity and Specificity: RIA and modern chemiluminescence immunoassays are generally considered the most sensitive techniques for detecting low analyte concentrations [117] [114]. A foundational study comparing methods for detecting cytomegalovirus IgG antibody found that RIA and ELISA were "comparable in sensitivity and specificity," and both were "10 to 100 times more sensitive" than older techniques like complement-fixation [119]. ELISA, particularly the sandwich format, offers high specificity due to the requirement for two antibodies to bind the target simultaneously [116]. IHC's sensitivity and specificity are highly dependent on antibody validation and protocol optimization but are sufficient for most diagnostic and research applications in tissue [14].
- Throughput and Automation: ELISA and other plate-based immunoassays are inherently suited for high-throughput analysis and full automation, processing dozens to hundreds of samples simultaneously [116] [114]. RIA can also process many samples but is limited by the handling of radioactive materials. IHC is a lower-throughput, more labor-intensive technique, though automation of staining platforms has improved its reproducibility and efficiency in clinical settings [14].
- Quantitative Capability: ELISA and RIA are designed to be fully quantitative, providing precise concentration measurements against a standard curve. IHC, in contrast, provides semi-quantitative data. Results are often scored based on staining intensity and the percentage of positive cells, which can introduce subjectivity, though digital pathology and AI are improving quantification [14] [15].
Table 2: Performance and Practical Comparison of IHC, ELISA, and RIA
| Parameter | Immunohistochemistry (IHC) | ELISA | RIA |
|---|---|---|---|
| Sensitivity | Medium [2] | High [119] [117] | Very High [119] [117] |
| Specificity | Medium (depends on antibody) [2] | High (especially sandwich) [116] | High [119] [118] |
| Quantification | Semi-quantitative | Fully Quantitative | Fully Quantitative |
| Multiplexing Capability | Up to 4+ targets with fluorescence [2] | Limited (typically single-plex) [2] | Limited (typically single-plex) |
| Throughput | Low to Medium | High | High |
| Automation Potential | Medium (automated stainers) | High (fully automated systems) | Medium |
| Major Limitation | Subjective interpretation, antigen masking | Hook effect at high [Ag] | Radioactive hazards & disposal |
Detailed Experimental Protocols
Protocol: Immunohistochemistry (IHC) for FFPE Tissues
The following protocol outlines the key steps for indirect chromogenic IHC on formalin-fixed, paraffin-embedded (FFPE) tissue sections [2] [14] [15].
Tissue Fixation and Sectioning:
- Fixation: Immerse tissue in 10% neutral-buffered formalin for 18-24 hours at room temperature to preserve morphology and antigenicity.
- Processing & Embedding: Dehydrate the fixed tissue through a series of graded alcohols and xylene, then embed in paraffin wax.
- Sectioning: Cut thin sections (4-6 μm) using a microtome and mount them on glass slides.
Deparaffinization and Rehydration:
- Immerse slides in xylene (or substitute) to remove paraffin, followed by rehydration through a descending series of alcohols (100%, 95%, 70%) to water.
Antigen Retrieval:
- To unmask epitopes cross-linked by formalin fixation, perform Heat-Induced Epitope Retrieval (HIER). Incubate slides in a target-specific retrieval buffer (e.g., citrate, pH 6.0 or EDTA, pH 9.0) and heat in a pressure cooker or water bath.
Blocking and Antibody Incubation:
- Blocking: Apply a protein block (e.g., serum, BSA) to cover non-specific binding sites and quench endogenous peroxidase activity if using an HRP-based system.
- Primary Antibody: Incubate sections with the specific primary antibody, diluted in buffer, for a defined period (30 minutes to several hours) in a humidity chamber.
- Secondary Antibody: Apply an enzyme-conjugated (e.g., HRP) secondary antibody that is specific to the host species of the primary antibody.
Detection and Visualization:
- Incubate slides with a chromogenic substrate, such as 3,3'-Diaminobenzidine (DAB), which produces a brown precipitate upon reaction with HRP.
Counterstaining and Mounting:
- Counterstain: Apply hematoxylin to stain cell nuclei blue.
- Mounting: Dehydrate through an ascending alcohol series, clear in xylene, and mount under a coverslip with a permanent mounting medium for microscopic examination.
Protocol: Sandwich ELISA for Protein Detection
The sandwich ELISA is the preferred format for sensitive and specific quantification of proteins [116].
Plate Coating:
- Dilute the capture antibody in a coating buffer (e.g., carbonate-bicarbonate buffer, pH 9.4). Add the solution to a 96-well polystyrene microplate and incubate overnight at 4°C. A typical concentration is 2-10 μg/mL.
Washing and Blocking:
- Discard the coating solution and wash the plate 2-3 times with a wash buffer (e.g., PBS containing 0.05% Tween 20).
- Add a blocking buffer (e.g., 1-5% BSA or non-fat dry milk in PBS) to all wells to cover any remaining protein-binding sites. Incubate for 1-2 hours at room temperature.
Sample and Standard Incubation:
- Wash the plate. Add diluted samples and a dilution series of the standard (protein of known concentration) to the wells. Incubate for 1-2 hours to allow the antigen to be captured.
Detection Antibody Incubation:
- Wash the plate to remove unbound antigen. Add the detection antibody (an antibody recognizing a different epitope on the target antigen), which is conjugated to an enzyme (e.g., HRP). Incubate for 1-2 hours.
Signal Development and Measurement:
- Wash the plate thoroughly. Add a substrate solution suitable for the enzyme (e.g., TMB for HRP). Incubate in the dark for a defined period until color develops.
- Stop the reaction by adding a stop solution (e.g., sulfuric acid for TMB).
- Measure the absorbance of the solution in each well immediately using a plate reader at the appropriate wavelength (e.g., 450 nm for TMB).
The Scientist's Toolkit: Essential Research Reagents
Successful execution of immunochemical techniques relies on a suite of critical reagents and materials.
Table 3: Essential Reagents for Immunochemistry
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Primary Antibodies | Specifically bind to the target antigen. | Monoclonal (high specificity) vs. Polyclonal (high sensitivity); requires rigorous validation [14]. |
| Labeled Secondary Antibodies | Bind to primary antibodies; conjugated to enzymes (HRP, AP) or fluorophores for detection. | Must be raised against the host species of the primary antibody; cross-adsorbed to minimize cross-reactivity [116]. |
| Formalin (10% NBF) | Cross-linking fixative for tissues; preserves morphology for IHC. | Over-fixation can mask epitopes, making antigen retrieval a critical step [2] [14]. |
| Chromogenic Substrates (DAB, TMB) | Enzymatic conversion produces a visible, colored precipitate. | DAB for IHC (brown, alcohol-insoluble); TMB for ELISA (blue, turns yellow when stopped). |
| Paraffin Wax | Embedding medium for fixed tissues; provides support for thin-sectioning. | Enables long-term storage of tissue blocks and preserves morphology [15]. |
| Microtome | Instrument to cut thin, consistent tissue sections from FFPE blocks. | Essential for preparing high-quality samples for IHC [15]. |
| Blocking Buffer (BSA, Serum) | Prevents non-specific binding of antibodies to the sample or plate surface. | Reduces background signal, improving the signal-to-noise ratio [116] [14]. |
| 96- or 384-Well Plates | Solid phase for immobilizing antigens or antibodies in ELISA. | High-binding polystyrene plates are standard; choice of color (clear/white) depends on detection method [116]. |
Applications in Research and Drug Development
The application of IHC and immunoassays is dictated by the research question.
IHC Applications:
- Cancer Diagnosis and Classification: Identifying tumor origin and subtypes using specific markers (e.g., cytokeratins, TTF-1) [14] [15].
- Predictive and Prognostic Biomarker Analysis: Detecting expression of therapeutic targets (e.g., HER2 in breast cancer) and proliferation markers (e.g., Ki-67) to guide treatment and assess prognosis [14] [15].
- Infectious Disease and Neuropathology: Localizing pathogens within tissues and identifying protein aggregates in neurodegenerative diseases (e.g., beta-amyloid in Alzheimer's) [14].
ELISA/RIA Applications:
- Biomarker Quantification in Bodily Fluids: Measuring hormone levels, cytokine panels, and therapeutic drug concentrations in serum or plasma [117].
- Serological Testing: Detecting and quantifying specific antibodies against pathogens, such as in SARS-CoV-2 serology [117] or cytomegalovirus [119].
- Quality Control in Biopharmaceutical Production: Quantifying the concentration of recombinant proteins and detecting host cell proteins during drug development.
Current Status and Future Perspectives
The field of immunochemistry is evolving rapidly, driven by demands for greater precision, throughput, and information density.
- Digital Pathology and AI: The integration of whole-slide imaging for IHC and artificial intelligence for analysis is reducing subjective interpretation and enabling the discovery of novel, complex morphological biomarkers [14].
- Automation and Standardization: Fully automated immunoassay systems (like CLIA) and IHC stainers are becoming the standard in clinical labs, enhancing reproducibility and enabling large-scale screening programs, as seen in recent type 1 diabetes initiatives [114].
- Multiplexing and Mass Spectrometry: Techniques like multiplex IHC/IF and imaging mass cytometry allow for the simultaneous detection of dozens of markers on a single tissue section, providing a systems-level view of the tissue microenvironment [14].
- Assay Harmonization: Despite advancements, a key challenge remains the lack of harmonization between different assay platforms and laboratories, leading to inter-assay variability. Ongoing efforts focus on standardizing protocols, antibodies, and reporting criteria to ensure data reliability and comparability [114].
IHC, ELISA, and RIA each occupy a critical and complementary niche in the researcher's toolkit. The selection of the appropriate technique is not a matter of which is superior, but which is most fit-for-purpose. IHC is unparalleled for visualizing target expression within the morphological context of tissue. In contrast, ELISA and RIA provide robust, quantitative data from solution-based samples, with RIA offering exceptional sensitivity and ELISA providing a safer, more versatile, and automatable platform. For drug development professionals and scientists, a comprehensive understanding of the principles, performance metrics, and applications of these techniques is fundamental to designing rigorous experiments, validating biomarkers, and making informed decisions that bridge basic research and clinical application.
Antibodies are indispensable tools in clinical diagnostics and therapeutic development, serving as critical reagents for detecting, quantifying, and characterizing protein biomarkers in patient samples. In clinical contexts, antibody-based tests directly influence patient management decisions, particularly in oncology where assessment of biomarkers such as estrogen receptor α (ER-α) and human epidermal growth factor receptor 2 (HER2) determines treatment courses with profound therapeutic and economic implications [120]. The validation of these antibodies transcends routine research reagent verification, becoming a fundamental requirement for ensuring diagnostic accuracy, prognostic reliability, and therapeutic predictability.
The process of antibody validation demonstrates that an antibody is specific, selective, and reproducible for its intended clinical use context [120]. Without rigorous validation, antibodies may produce unreliable results, contributing to what has been termed the 'reproducibility crisis' in biomedical research [121]. Concerns about antibody specificity are substantial, with studies indicating that more than 50% of commercial antibodies fail one or more performance tests, potentially compromising countless research findings and clinical applications [122]. The College of American Pathologists (CAP) has established evolving guidelines to address these challenges, with recent 2024 updates reflecting advances in validation methodologies for complex biomarker applications [123].
Core Principles of Antibody Validation
Defining Validation Performance Characteristics
Antibody validation for clinical biomarker development requires demonstration of three essential performance characteristics: specificity, selectivity, and reproducibility. Specificity refers to the antibody's ability to bind exclusively to its intended target antigen amidst complex biological matrices. Selectivity denotes the capacity to recognize the target under specific assay conditions, while reproducibility ensures consistent performance across different reagent lots, operators, instruments, and time [120]. These characteristics must be established within the context of the antibody's intended clinical application, as performance varies significantly across different experimental platforms.
The clinical implications of inadequate validation are profound. Non-specific antibodies have led to erroneous scientific conclusions, as demonstrated by studies where antibodies against G protein-coupled receptors produced positive staining in knockout mice lacking the target receptors [120]. Similarly, different lots of the same monoclonal antibody have shown completely divergent staining patterns—one nuclear and another membranous/cytoplasmic—highlighting critical reproducibility concerns in clinical assay development [120].
Regulatory and Guidelines Framework
The validation of antibodies for clinical use exists within a robust regulatory framework designed to ensure patient safety and assay reliability. The FDA defines validation as "the process of demonstrating, through the use of specific laboratory investigations, that the performance characteristics of an analytical method are suitable for its intended analytical use" [120]. The College of American Pathologists (CAP) has further refined this concept for immunohistochemical assays through regularly updated guidelines, with the most recent 2024 update addressing emerging challenges in clinical biomarker development [123].
Key updates in the 2024 CAP guidelines include harmonized validation requirements for all predictive markers with a standardized 90% concordance threshold, detailed guidance for validating assays with distinct scoring systems (such as PD-L1 and HER2), and specific recommendations for IHC assays performed on cytology specimens with alternative fixatives [123]. These evidence-based recommendations, while not always immediately incorporated into accreditation checklists, represent the current standard of care for ensuring quality and safety in clinically important assays.
Strategic Validation Approaches and Methodologies
The Five Pillars of Antibody Validation
A comprehensive framework for antibody validation has been codified in the "five pillars" strategy, which provides a multi-faceted approach to establishing antibody specificity and reliability [124]. This systematic methodology addresses validation through complementary techniques that collectively provide robust evidence of antibody performance.
Genetic Strategies (Knockout/Knockdown): This approach involves creating cellular models in which the gene encoding the target protein is completely inactivated (knockout) or its expression significantly reduced (knockdown). The absence or reduction of target protein expression allows researchers to confirm antibody specificity by demonstrating loss or diminution of signal in modified compared to wild-type cells [124] [121]. This method is particularly valuable for distinguishing specific from non-specific binding and is considered a gold standard in validation [121].
Orthogonal Antibody Comparison: This pillar utilizes multiple antibodies recognizing different epitopes on the same target protein. When these independent antibodies produce concordant staining patterns, confidence in specificity increases significantly [124]. This approach is especially useful when knockout models are unavailable, though it requires access to multiple well-characterized antibodies against the same target.
Immunoprecipitation with Mass Spectrometry (IP/MS): This powerful technique combines the target isolation capabilities of immunoprecipitation with the identification power of mass spectrometry. The antibody pulls down the target protein from complex mixtures, and co-precipitated proteins are identified by MS, providing direct evidence of specificity while revealing potential off-target interactions [124].
Biological and Orthogonal Validation: This pillar incorporates biological context into validation by comparing antibody results with established knowledge about protein behavior, such as subcellular localization, expression patterns in known positive and negative tissues, or predictable responses to biological stimuli [124]. Orthogonal validation uses non-antibody-based methods to measure the same target, with consistency between methods strengthening validation evidence.
Recombinant Protein Expression: This approach involves expressing the recombinant target protein in heterologous systems to serve as a positive control. Detection of the recombinant protein at the expected molecular weight provides confirmation of antibody specificity, though this method may not recapitulate native protein modifications or interactions [124].
Application-Specific Validation Considerations
Antibody performance varies significantly across different applications due to fundamental differences in antigen presentation and detection methodologies. Consequently, validation must be performed separately for each intended use [121]. The table below summarizes key validation considerations for major application categories:
Table 1: Application-Specific Antibody Validation Requirements
| Application | Antigen State | Key Validation Parameters | Common Pitfalls |
|---|---|---|---|
| Western Blotting | Denatured, linear epitopes | Single band at expected molecular weight [121] | Non-specific bands, proteolytic cleavage [120] |
| Immunohistochemistry (IHC) | Cross-linked, fixed tissue | Appropriate cellular localization, expected tissue distribution [125] [121] | Over-fixation masking epitopes, non-specific background [120] |
| Immunofluorescence (IF) | Native or fixed structures | Subcellular localization concordance with known markers [121] | Autofluorescence, antibody cross-reactivity [120] |
| Immunoprecipitation (IP) | Native conformation | Efficient target capture, minimal non-specific binding [121] | Protein complexes masking epitopes, weak interactions [124] |
| ELISA | Native solution state | Target specificity in native conformation, minimal cross-reactivity [121] | Epitope masking in complex fluids, matrix effects [121] |
Advanced Technical Protocols
Knockout Validation Protocol
Genetic validation using knockout models represents the most stringent approach for establishing antibody specificity. The following protocol outlines a standardized method for knockout-based validation:
Cell Line Selection and Engineering: Select appropriate cell lines expressing the target protein using RNA expression databases (e.g., DepMap "Expression" database). Establish threshold expression levels (e.g., 2.5 log2(TPM+1)) for candidate selection [122]. Generate isogenic knockout lines using CRISPR-Cas9 technology, prioritizing common cell backgrounds with short doubling times and high CRISPR efficiency [122].
Validation of Knockout Lines: Confirm successful gene editing through genomic sequencing and demonstrate complete absence of target protein using multiple orthogonal methods. Verify that knockout lines maintain viability and appropriate morphology for experimental applications.
Parallel Testing: Test antibodies in parallel on parental and knockout cell lines across all intended applications. For Western blot, use lysates from both cell lines. For immunohistochemistry, create cell pellets from both lines processed identically to clinical specimens [122] [121].
Result Interpretation: Specific antibodies will show complete absence of signal in knockout samples while maintaining appropriate signals in parental lines. Any residual signal in knockout samples indicates non-specific binding and requires further investigation or antibody rejection [121].
The following diagram illustrates the knockout validation workflow:
Orthogonal Validation with Mass Spectrometry
For antibodies intended for immunoprecipitation or native-state applications, IP/MS provides unparalleled specificity assessment:
Sample Preparation: Prepare cell lysates under non-denaturing conditions to preserve protein structure and interactions. Include appropriate controls (beads only, isotype control) to identify non-specific binding.
Immunoprecipitation: Incubate antibody with protein A/G beads, then add to cell lysate. Include knockout cell lysates as negative controls. Wash beads thoroughly to remove non-specifically bound proteins [124].
Protein Elution and Digestion: Elute bound proteins using mild denaturing conditions. Digest proteins with trypsin or similar protease to generate peptides for mass spectrometry analysis.
Mass Spectrometry Analysis: Analyze peptides using LC-MS/MS. Search resulting spectra against appropriate protein databases to identify all proteins present in the immunoprecipitate.
Data Interpretation: Specific antibodies will yield primarily the target protein with few interacting partners. Non-specific antibodies will pull down multiple unrelated proteins, indicating inadequate specificity for reliable use [124].
Validation for Specific Clinical Applications
Immunohistochemistry in Clinical Biomarkers
IHC presents unique validation challenges due to the complex effects of tissue fixation and processing on antigen preservation and accessibility. Formalin fixation creates methylene bridges between proteins that can mask epitopes, while variable fixation times and processing protocols introduce significant pre-analytical variables that must be controlled [120]. The 2024 CAP guidelines provide specific recommendations for IHC assay validation:
Predictive Markers with Distinct Scoring Systems: For biomarkers such as HER2 and PD-L1 that employ different scoring systems based on tumor type or site, laboratories must separately validate each assay-scoring system combination [123].
Cytology Specimens: IHC assays performed on cytology specimens fixed in alternative fixatives require separate validation from FFPE tissues, with a minimum of 10 positive and 10 negative cases [123].
Concordance Standards: The updated guidelines harmonize concordance requirements for all predictive IHC assays to 90%, eliminating previous variations between different biomarker types [123].
IHC validation should incorporate multiple control strategies, including known positive and negative tissues, cell line pellets with characterized expression levels, and biological controls such as tissues with inherent expression patterns [125]. The use of blocking peptides provides additional specificity confirmation by competing for antibody binding sites [125].
Quantitative Biomarker Assays
For antibodies used in quantitative clinical assays, additional validation parameters must be established:
Linearity and Range: Demonstrate that the assay produces results directly proportional to analyte concentration across the clinically relevant range.
Limit of Detection and Quantification: Establish the lowest concentration that can be reliably detected and quantified.
Precision and Reproducibility: Assess intra-assay, inter-assay, and inter-laboratory variability to establish performance consistency.
Interference Testing: Evaluate potential interference from common sample components (hemoglobin, lipids, etc.) or related molecules with similar structures.
The following diagram illustrates the comprehensive validation strategy for clinical biomarker antibodies:
Implementation and Quality Assurance
Validation Documentation and Compliance
Comprehensive documentation is essential for demonstrating antibody validation for clinical applications. Validation reports should include:
- Detailed protocols for all validation experiments
- Raw data and statistical analyses supporting performance claims
- Lot-to-lot consistency data
- Stability information for both reagents and stored samples
- Operator training and qualification records
- Regular review and re-validation schedules
Laboratories must comply with Clinical Laboratory Improvement Amendments (CLIA) requirements, which mandate validation of all assay performance characteristics before reporting patient results [123]. Even for FDA-cleared assays, verification studies must demonstrate acceptable performance in the specific laboratory environment.
Troubleshooting Common Validation Issues
Antibody validation frequently encounters specific challenges that require systematic troubleshooting:
Non-specific Bands in Western Blot: Additional bands at unexpected molecular weights may indicate cross-reactivity with unrelated proteins, proteolytic cleavage products, or post-translational modifications. Optimization of blocking conditions, antibody concentration, and washing stringency may resolve these issues [120].
High Background in IHC: Excessive background staining can result from inadequate blocking, over-fixation, antibody concentration too high, or non-optimal epitope retrieval. Titration experiments and protocol optimization are essential [120].
Lot-to-Lot Variability: Significant performance differences between antibody lots necessitate careful bridging studies and may require switching to recombinant antibodies, which offer superior consistency compared to traditional monoclonals or polyclonals [122].
Inconsistent Cell Line Expression: Natural biological variation in target expression across cell lines requires careful selection of appropriate models and confirmation of expression levels in both parental and knockout lines [122].
Essential Research Reagent Solutions
The table below outlines key reagents and materials required for comprehensive antibody validation:
Table 2: Essential Research Reagents for Antibody Validation
| Reagent Category | Specific Examples | Primary Function in Validation |
|---|---|---|
| Validated Cell Lines | CRISPR-engineered KO lines, overexpression lines [122] | Specificity testing through genetic controls |
| Reference Materials | Recombinant proteins, peptide immunogens [124] | Positive controls and competition assays |
| Tissue Specimens | FFPE tissue microarrays, positive/negative tissues [125] [123] | Application-specific performance assessment |
| Detection Reagents | Validated secondary antibodies, detection kits [125] | Signal generation with minimal background |
| Assay Platforms | Western blot systems, IHC/IF platforms, MS instrumentation [122] [124] | Performance across intended applications |
| Validation Antibodies | Independent antibodies targeting same protein [124] | Orthogonal specificity confirmation |
Antibody validation for clinical biomarker development requires a systematic, evidence-based approach that addresses the unique challenges of clinical diagnostic applications. The integration of genetic strategies, orthogonal verification methods, and application-specific performance testing provides a robust framework for establishing antibody reliability. The recent updates to CAP guidelines reflect evolving standards in the field, with increased emphasis on harmonized requirements, specific scoring systems, and alternative specimen types [123].
Future directions in antibody validation point toward increased collaboration and data sharing within the research community. Large-scale validation initiatives, such as those testing hundreds of commercial antibodies against neuroscience targets, demonstrate the power of coordinated efforts to establish reagent reliability [122]. The growing preference for recombinant antibodies, which performed superiorly in large-scale studies, highlights the importance of renewable reagents with defined composition [122]. As clinical biomarker applications continue to expand, particularly in areas such as bispecific antibodies and antibody-drug conjugates [126] [127], rigorous validation practices will remain essential for translating promising discoveries into reliable clinical applications.
The path toward resolving the "reproducibility crisis" in antibody-based research depends on widespread adoption of comprehensive validation frameworks, transparent reporting of validation data, and manufacturer commitment to rigorous characterization. Through implementation of these advanced verification strategies, researchers and clinical laboratories can ensure that antibody-based biomarker tests deliver the reliability required for informed clinical decision-making.
Immunohistochemistry (IHC) stands as a cornerstone technique in biomedical research and clinical diagnostics, amalgamating principles from histology, immunology, and biochemistry to detect specific antigens within tissue samples [14]. Unlike other molecular biology techniques such as western blotting or ELISA, IHC provides the unique advantage of precisely localizing target proteins within the tissue architecture without digestion, using a standard light microscope [14]. This capability makes it indispensable for diagnosing neoplastic, infectious, and neurodegenerative diseases, as well as for assessing drug efficacy in pharmaceutical development [14] [128]. However, the power of IHC is tempered by significant technical challenges that can compromise the accuracy, reliability, and reproducibility of its results. This guide provides an in-depth examination of three core limitations—subjectivity in interpretation, antibody cross-reactivity, and standardization hurdles—and offers detailed, actionable strategies and protocols to navigate them, ensuring robust and defensible experimental outcomes.
Overcoming Subjectivity in IHC Interpretation
The interpretation of IHC staining has traditionally relied on semi-quantitative, visual assessment by pathologists or researchers. This method is inherently subjective, leading to substantial intra- and inter-observer variability that can affect diagnostic conclusions and research reproducibility [14].
Quantitative Digital Image Analysis
Adopting quantitative digital pathology is a primary strategy to mitigate subjectivity. This involves scanning IHC slides to create high-resolution whole-slide images, which are then analyzed by specialized software to quantify staining patterns objectively [14] [129].
Detailed Protocol for Quantitative IHC Analysis [129]:
- Tissue Staining and Digitization: Perform IHC according to an optimized protocol. Subsequently, scan all stained slides at 40x or 20x magnification using a high-throughput digital slide scanner (e.g., Pannoramic scan from 3DHistech).
- Region of Interest (ROI) Annotation: Using computer-assisted diagnosis applications (e.g., CaseViewer), a pathologist must manually outline the tumor areas or specific tissue regions for analysis on each digital slide.
- Automated Quantification: Import the annotated digital slides into image analysis software (e.g., QuantCenter). The software applies specific quantification modules based on the antigen's subcellular localization:
- Nuclear quant: For nuclear antigens like PCNA and p53.
- Membrane quant: For membrane-bound antigens like EGFR.
- Cell quant: For cytoplasmic or cellular antigens like VEGF.
- H-Score Calculation: The software generates an H-score for each analyzed region. The H-score is a quantitative metric calculated by the formula: H-score = Σpi(i+1), where:
pirepresents the percentage of positive cells (0-100%).irepresents the staining intensity score, typically categorized as 0 (negative), 1 (weak), 2 (intermediate), or 3 (strong).- The final H-score ranges from 0 to 300, providing a continuous variable for statistical analysis [129].
This method was successfully used to demonstrate that expressions of EGFR, PCNA, and VEGF were significantly higher in esophageal squamous carcinoma (ESCC) compared to non-ESCC patients, with the combination of biomarkers yielding an AUC of 0.86, superior to any single marker [129].
Standardized Scoring Systems and Training
While moving towards full automation, many labs still rely on manual scoring. Implementing rigorous, pre-defined scoring criteria and cross-laboratory training can improve consistency. Common systems include the semi-quantitative H-score and the Quickscore, which combine the proportion of positive cells and staining intensity [14]. Regular calibration sessions among observers using a standardized set of reference images are crucial to align scoring standards.
Table 1: Comparison of IHC Scoring Methods
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Semi-Quantitative (Manual) | Pathologist assigns score based on % positive cells and intensity (e.g., 0, 1+, 2+, 3+). | Fast, low cost, requires no specialized equipment. | Highly subjective, significant inter-observer variability. |
| H-Score | Quantitative score calculated as Σpi(i+1), ranging from 0 to 300. | Continuous variable, more granular, suitable for statistical analysis. | Requires training, still has a subjective element in manual assessment. |
| Digital Image Analysis | Computer software quantifies staining percentage and intensity from digitized slides. | Fully objective, highly reproducible, high-throughput capability. | Requires expensive equipment and software, needs pathologist for ROI annotation. |
Mitigating Antibody Cross-Reactivity
Antibody cross-reactivity occurs when an antibody binds to non-target epitopes that are structurally similar to the intended antigen, leading to false-positive results and misinterpretation of protein localization [14] [130]. Cross-reactivity is not an immutable property of an antibody but can be influenced by the assay format and conditions [130].
Rigorous Antibody Validation and Controls
Essential to valid interpretation is the use of antibodies that have been rigorously validated for IHC.
- Western Blot Correlation: The antibody should be validated using western blot analysis of proteins from the same tissue or cell type used for IHC. This confirms that the antibody recognizes a single band of the expected molecular weight, helping to rule out cross-reactivity with unrelated proteins [131].
- Genetic Validation: The most rigorous validation involves using genetically engineered controls. The antibody should produce staining in tissues or cells known to express the target antigen and show absent or significantly reduced staining in knockout models where the target gene has been deleted [131].
- Appropriate Negative Controls:
- The Isotype Control: The proper negative control is the substitution of the primary antibody with a non-specific immunoglobulin of the same species and isotype, at the same concentration [131]. This controls for non-specific binding of immunoglobulins to tissue components.
- The Omission Control (Common Misconception): Omitting the primary antibody is not a control for the specificity of the primary antibody. It only controls for nonspecific binding of the secondary antibody and should not be used alone to claim specificity [131].
Optimizing Assay Conditions to Modulate Selectivity
Research demonstrates that cross-reactivity can be modulated by changing the immunoassay format and reagent concentrations. Assays with sensitive detection systems that operate at low concentrations of antibodies and competing antigens are characterized by lower cross-reactivity and higher specificity [130].
Experimental Approach [130]:
- Shift to Lower Reagent Concentrations: Implementing assays that require lower concentrations of immunoreagents (primary/secondary antibodies, labeled antigens) can reduce cross-reactivity by up to five-fold. This is because at lower concentrations, the assay becomes more dependent on high-affinity binding, favoring the intended target over lower-affinity cross-reactants.
- Compare Assay Formats: When possible, compare results across different formats (e.g., ELISA vs. FPIA). Be aware that an antibody's cross-reactivity profile may differ between them.
- Optimize Antigen Retrieval: For IHC, the method of antigen retrieval (heat-induced vs. enzyme-induced, buffer pH) can significantly impact antibody binding affinity and specificity. Inadequate retrieval can mask the target epitope, while overly harsh retrieval may expose non-specific epitopes [6]. Optimization is required for each antibody-antigen pair.
Table 2: Key Research Reagent Solutions for IHC
| Reagent / Material | Function / Purpose | Key Considerations |
|---|---|---|
| Primary Antibodies | Binds specifically to the target antigen in the tissue. | Must be validated for IHC; monoclonal antibodies offer higher specificity, while polyclonal can offer higher sensitivity [14]. |
| Antigen Retrieval Buffers | Reverses formaldehyde-induced cross-links to expose hidden epitopes. | Citrate buffer (pH 6.0) and Tris-EDTA (pH 9.0) are common; optimal pH and method (heat vs. enzyme) are antigen-dependent [6]. |
| Blocking Serum | Reduces non-specific binding of antibodies to the tissue. | Should be from the same species as the secondary antibody (e.g., goat serum if using anti-rabbit goat secondary) [6]. |
| Endogenous Enzyme Block | Inactivates endogenous peroxidases or phosphatases to prevent false-positive signals. | 3% hydrogen peroxide is standard for HRP-based detection; insufficient inactivation causes non-specific staining [14] [6]. |
| Chromogenic Substrates (e.g., DAB) | Produces an insoluble, colored precipitate at the site of antibody binding. | DAB is common (brown); different substrates yield different colors for multiplexing; reaction time must be controlled to prevent background [6]. |
Achieving Standardization and Quality Assurance
A significant hurdle in IHC is the lack of standardization across laboratories regarding protocols, reagents, and equipment, leading to poor reproducibility of findings [14].
Implementing a Rigorous Quality Control System
A robust quality control (QC) system is vital to ensure reliable and reproducible IHC results.
- Use of Controls in Every Run:
- Positive Control: A tissue section known to express the target antigen must be included in every staining run. This validates that the entire protocol, from antigen retrieval to detection, functioned correctly [131].
- Negative Control: As described above, an isotype control should be used to confirm the absence of non-specific staining [131].
- Standardized Operating Procedures (SOPs): Develop and strictly adhere to detailed SOPs for every step of the IHC process, including tissue fixation, processing, antigen retrieval, and staining. This minimizes inter-technician and inter-batch variability.
- Reagent Validation and Lot Tracking: All antibodies and critical reagents should be validated upon receipt and before being put into use. Lot numbers and expiration dates must be meticulously tracked.
Detailed IHC Protocol for Formalin-Fixed Paraffin-Embedded (FFPE) Sections
The following detailed protocol for the indirect method on FFPE sections highlights critical steps where standardization is crucial [6].
Materials Needed: FFPE tissue sections, xylene, ethanol series, antigen retrieval buffer, hydrogen peroxide, blocking serum, primary antibody, labeled secondary antibody, chromogenic substrate, hematoxylin, and mounting medium.
Procedure [6]:
- Baking and Deparaffinization: Bake slides at 60°C for several hours to melt paraffin. Immerse slides in xylene (5 min, 3 times) followed by a graded ethanol series (100%, 95%, 70% - 5 min each) to hydrate. Conclude with a wash in distilled water and PBS.
- Antigen Retrieval: Place slides in a Coplin jar with citrate buffer (pH 6.0). Perform heat-induced epitope retrieval using an autoclave (125°C for 5 minutes) or a microwave (approx. 10 min, 2 times). Cool to room temperature.
- Endogenous Peroxidase Inactivation: Incubate slides with 3% hydrogen peroxide in PBS for 10 minutes at room temperature to quench endogenous peroxidase activity. Wash with PBS.
- Blocking: Circle the tissue section with a hydrophobic pen. Apply 500 µL of blocking buffer (e.g., 0.5% BSA, 5% serum in PBS) and incubate for 30 minutes at room temperature.
- Primary Antibody Reaction: Tap off blocking buffer and apply the optimized dilution of primary antibody in blocking buffer. Incubate for 1-2 hours at room temperature. Wash thoroughly with PBS-Tween and PBS.
- Secondary Antibody Reaction: Apply an enzyme-labeled secondary antibody (e.g., HRP-conjugated) and incubate for 1 hour at room temperature. Wash thoroughly with PBS-Tween and PBS.
- Chromogenic Development: Apply the chromogenic substrate (e.g., DAB) and monitor the development reaction closely (3-10 minutes). Stop the reaction by immersing in distilled water.
- Counterstaining and Mounting: Counterstain with Mayer's hematoxylin for 5 minutes, then rinse under running water for 20 minutes. Dehydrate through a graded ethanol series, clear in xylene, and mount with a xylene-based hydrophobic mounting medium.
The limitations of subjectivity, cross-reactivity, and lack of standardization in IHC are significant but not insurmountable. By integrating quantitative digital analysis, employing rigorous antibody validation and optimized assay conditions, and adhering to strict quality control protocols and standardized procedures, researchers and drug development professionals can significantly enhance the reliability and reproducibility of their IHC data. The future of IHC lies in the wider adoption of these practices, coupled with advancements in digital pathology and artificial intelligence, which promise to automate analysis and further reduce variability, solidifying IHC's role as an indispensable tool in both research and clinical diagnostics.
Conclusion
Immunochemistry remains an indispensable and evolving tool that provides unique insights into cellular and tissue biology by localizing specific antigens within their morphological context. Mastering its principles, methodologies, and optimization techniques is fundamental for obtaining reliable data in both research and clinical diagnostics. The future of immunochemistry is poised for transformative growth, driven by the integration of digital pathology, artificial intelligence for automated image analysis, and the development of highly multiplexed techniques for comprehensive single-cell expression profiling. These advancements will further solidify its role in personalized medicine, enhancing drug development and enabling more precise disease classification and therapy selection.
References
- 1. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOopYZC-iWJ7Yny2WKZ-HggG1_tnu2MqkkOOl5xtoSo_EQeXU2foI]
- 2. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 3. Quantitative comparison of immunohistochemical staining ... [https://pubmed.ncbi.nlm.nih.gov/22515559/]
- 4. Quantitative comparison of immunohistochemical staining ... [https://diagnosticpathology.biomedcentral.com/articles/10.1186/1746-1596-7-42]
- 5. Principles of Immunochemical Techniques [https://basicmedicalkey.com/principles-of-immunochemical-techniques/]
- 6. The principle and method of Immunohistochemistry (IH) [https://www.mblbio.com/bio/g/support/method/immunohistochemistry.html]
- 7. A fully automated quantitative analysis method based on ... [https://www.sciencedirect.com/science/article/pii/S2950261625000342]
- 8. Articles in 2025 | Nature Reviews Immunology [https://www.nature.com/nri/articles?year=2025]
- 9. Antibody basics guide [https://www.abcam.com/en-us/technical-resources/guides/antibody-basics/antibody-basics]
- 10. High-throughput analysis system of interaction kinetics for ... [https://www.nature.com/articles/s41598-023-46756-y]
- 11. Antigen Processing and Presentation by MHCs [https://www.thermofisher.com/us/en/home/life-science/antibodies/antibodies-learning-center/antibodies-resource-library/cell-signaling-pathways/antigen-processing-presentation-mhc.html]
- 12. The cell biology of antigen processing and presentation [https://pubmed.ncbi.nlm.nih.gov/1910692/]
- 13. ELISA Assay Technique | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa.html]
- 14. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467]
- 15. Immunohistochemistry (IHC): Principles, Techniques and ... [https://www.scitechnol.com/peer-review/immunohistochemistry-ihc-principles-techniques-and-applications-z1gC.php?article_id=27668]
- 16. Modeling Antibody Kinetics Post‐mRNA Booster ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12327169/]
- 17. Antibody validation for Western blot: By the user, for the user [https://pmc.ncbi.nlm.nih.gov/articles/PMC6983856/]
- 18. Techniques of immunofluorescence and their significance [https://ijdvl.com/techniques-of-immunofluorescence-and-their-significance/]
- 19. Immunofluorescence [https://en.wikipedia.org/wiki/Immunofluorescence]
- 20. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 21. Immunostaining and Immunofluorescence [https://www.stainsfile.com/theory/methods/immunostaining-immunofluorescence/]
- 22. Toward universal immunofluorescence normalization for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539234/]
- 23. ROSIE: AI generation of multiplex immunofluorescence ... [https://www.nature.com/articles/s41467-025-62346-0]
- 24. Polyclonal vs Monoclonal Antibodies | Updated 2025) [https://www.stressmarq.com/blog/polyclonal-vs-monoclonal-antibodies/?srsltid=AfmBOooom1dji4g3sE7q-CiZ4_SMuUT6T7WIVH01iDgRzK6oYffi5FYx]
- 25. Monoclonal vs. Polyclonal Antibodies [https://www.thermofisher.com/us/en/home/life-science/antibodies/primary-antibodies/monoclonal-vs-polyclonal-antibodies.html]
- 26. Key Trends Shaping Therapeutic Antibodies in 2025 and ... [https://www.diatheva.com/key-trends-shaping-therapeutic-antibodies-in-2025-and-beyond/]
- 27. Antibodies And Reagents For Cancer Research [https://vectorlabs.com/antibodies-reagents-for-cancer-research/?srsltid=AfmBOopvOY4vimuFkE77sDSKJ291a4_IzZS7YmbCkbsni5F92w8R2h6J]
- 28. Antibody Labeling Kits [https://www.thermofisher.com/us/en/home/life-science/antibodies/antibody-labeling.html]
- 29. CAP Pro Course - Immunohistochemistry Part 1 (2025 & 2026) [https://www.medialab.com/course.aspx?courseid=690324]
- 30. How are Monoclonal Antibodies shaping Medicine in 2025? [https://denovobiolabs.com/how-are-monoclonal-antibodies-shaping-medicine-in-2025/]
- 31. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 32. Types Of Immunoassay - And When To Use Them [https://www.quanterix.com/immunoassay-technologies-past-present-and-future/]
- 33. Direct vs indirect assays [https://www.abcam.com/en-us/technical-resources/guides/conjugation-guide/direct-vs-indirect-assays]
- 34. What is the Difference Between Direct and Indirect ELISA? [https://shop.surmodics.com/what-is-the-difference-between-direct-and-indirect-elisa]
- 35. Direct vs. Indirect Fluorescent Antibody Labeling [https://probes.bocsci.com/resources/direct-vs-indirect-fluorescent-antibody-labeling-which-is-right-for-your-research.html]
- 36. Comparison of Different Detection Methods in Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1850311/]
- 37. Comparative Analysis of Different Staining Techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12244912/]
- 38. FFPE vs Frozen Tissue Samples [https://www.biochain.com/blog/ffpe-vs-frozen-tissue-samples/]
- 39. FFPE vs. Frozen Tissue Samples - iProcess Global Research [https://iprocess.net/ffpe-vs-frozen-tissue-samples/]
- 40. FFPE Tissue Preparation Steps [https://www.biochain.com/blog/ffpe-tissue-preparation-steps/]
- 41. Frozen vs. Formalin-Fixed Paraffin-Embedded Tissue ... [https://www.stagebio.com/blog/frozen-vs-formalin-fixed-paraffin-embedded-tissue-sections-for-ihc]
- 42. IHC Embedding Optimization: Paraffin vs. Frozen Tissue [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-optimization/embedding?srsltid=AfmBOoqLwaPdWmMoaxNG4X3QYzvwqhZ768IbDFIthJM4D3SoiIW78-_W]
- 43. A critical spotlight on the paradigms of FFPE-DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10415133/]
- 44. Advantages and Drawbacks of Paraffin and Frozen Tissues [https://waxitinc.com/advantages-and-drawbacks-of-paraffin-and-frozen-tissues-2/]
- 45. Brief guide to immunostaining - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11699723/]
- 46. Antigen Retrieval Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC3201121/]
- 47. Molecular mechanisms of antigen retrieval - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4676902/]
- 48. A Guide to Better IHC Staining: Steps, Troubleshooting, ... [https://www.celnovte.com/solution/a-guide-to-better-ihc-staining-steps-troubleshooting-and-optimization/]
- 49. The Basic Truth: Antigen Retrieval Solutions and pH [https://biocare.net/media/white-papers/the-basic-truth-antigen-retrieval-solutions-and-ph/]
- 50. IHC Antigen Retrieval Protocol | Heat & Enzyme Methods [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-optimization/antigen-retrieval?srsltid=AfmBOoqgPGeAj-aUEISxhJv3NuW1RszX025S8ZIywF-6qw_Yg3cpOyff]
- 51. Colorimetric FFPE—High pH Antigen Retrieval [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/colorimetric-ffpe-high-ph-antigen-retrieval.html]
- 52. Article A novel quantitative immunohistochemistry method ... [https://www.sciencedirect.com/science/article/pii/S089339522201273X]
- 53. IHC-P protocols [https://www.abcam.com/en-us/technical-resources/protocols/ihc-with-samples-in-paraffin]
- 54. Immunohistochemistry-IHC | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cellular-imaging/ihc.html]
- 55. Immunohistochemistry Protocols [https://www.antibodies.com/applications/immunohistochemistry/ihc-protocol]
- 56. Society for Immunotherapy of Cancer - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11749220/]
- 57. Immunofluorescence Method for IHC Detection [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/immunofluorescence-method-ihc-detection.html]
- 58. IHC detection systems: Advantages and Disadvantages [https://www.bio-techne.com/applications/imaging/immunohistochemistry/ihc-detection]
- 59. IHC Sample Visualization [https://www.ptglab.com/support/immunohistochemistry-protocol/ihc-sample-visualization/?srsltid=AfmBOorA3EMzUT8_hSkABlGRLzg2w0OHwDr6SNltxRis9N1gUaOrCU_J]
- 60. An introduction to Performing Immunofluorescence Staining [https://pmc.ncbi.nlm.nih.gov/articles/PMC6918834/]
- 61. Multiplex chromogenic immunohistochemistry to stain and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9720345/]
- 62. Counterstains in Immunohistochemistry: Principles, ... [https://www.bosterbio.com/blog/post/counterstains-in-immunohistochemistry-principles-options-and-troubleshooting?srsltid=AfmBOorQo3ZXChnxvqo2Odt1F_FJVot06Ulu_vYnZinA30_JCArvROQv]
- 63. IHC Counterstains | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-counterstains.html]
- 64. Digital separation of diaminobenzidine-stained tissues via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354574/]
- 65. Advances in Molecular Diagnostics and Targeted ... [https://pubmed.ncbi.nlm.nih.gov/40729049/]
- 66. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 67. 2025: The future of cancer diagnostics in the pathology lab [https://diagnostics.roche.com/us/en/article-listing/2025-the-future-of-cancer-diagnostics-in-the-pathology-lab.html]
- 68. 2025 AGENDA INFECTIOUS DISEASES RESEARCH ... [https://infectiousdiseases.wustl.edu/items/2025-infectious-diseases-research-symposium-and-j-russell-little-md-lecture/]
- 69. FY 2025 Infectious Diseases and Immunology Research: U.S. ... [https://www.amed.go.jp/en/news/program/0301B_00035.html]
- 70. RT-QuIC: a highly promising diagnostic method for ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1578252/full]
- 71. Emerging New Drug Modalities in 2025 [https://www.bcg.com/publications/2025/emerging-new-drug-modalities]
- 72. Immunochemistry in the Real World: 5 Uses You'll Actually ... [https://www.linkedin.com/pulse/immunochemistry-real-world-5-uses-youll-actually-see-2025-oscgc]
- 73. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 74. Quantitative immunohistochemistry analysis of pancreatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12444338/]
- 75. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 76. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 77. Antigen Retrieval in IHC: Why It Matters and How to Get ... [https://www.atlasantibodies.com/knowledge-hub/blog/antigen-retrieval-in-ihc-why-it-matters-and-how-to-get-it-right/]
- 78. Unmasking Epitopes Using Antigen Retrieval For Formalin- ... [https://vectorlabs.com/blog/unmasking-epitopes-using-antigen-retrieval/?srsltid=AfmBOor8flyaaySzT42O9xwaGG9Bt0ISPU-qgnL9lpb-kmM8Z-z1j7Qw]
- 79. Optimizing HIER Antigen Retrieval for IHC [https://www.bosterbio.com/blog/post/protocol-for-optimizing-hier-antigen-retrieval-conditions?srsltid=AfmBOor9TehjkicsGTI8P3yOBa1fen2R18z-95TTnFgGuoKU9iWOuxwe]
- 80. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOoognM16nyc_JZPavagYoOsOpxI6xfTHB74cMw5saGdADJQIvqeV]
- 81. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 82. Getting To The Specifics: Blocking For Immunohistochemistry [https://vectorlabs.com/blog/blocking-for-immunohistochemistry/?srsltid=AfmBOorwvCA1ipk1lXRBqN1jh0VMfDkWK3dCmXXMhYzK1_-8FnrEUkNZ]
- 83. ICC/IHC Non-Specific Binding / Staining Prevention Protocol [https://www.rndsystems.com/resources/protocols/preventing-non-specific-staining]
- 84. Methods to Block Endogenous Detection [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/methods-block-endogenous-detection.html]
- 85. Blocking in IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/blocking-in-ihc]
- 86. IHC Blocking | Proteintech Group [https://www.ptglab.com/support/immunohistochemistry-protocol/ihc-blocking/?srsltid=AfmBOopnHsXkwkaHXi5Bvl751K10hupxj4aLBG6vZOLUC-s08i_dRxVO]
- 87. High background in immunohistochemistry [https://www.abcam.com/en-us/technical-resources/troubleshooting/high-background-in-immunohistochemistry]
- 88. Non-specific binding of antibodies in immunohistochemistry [https://www.nature.com/articles/srep00028]
- 89. Tips for Reducing Non-specific Staining in IHC [https://www.biossusa.com/blogs/news/tips-for-reducing-non-specific-staining-in-ihc?srsltid=AfmBOooPST78ShRbvwY3OvTbLhg3Nux17WUdQGD7_k1S0Qr9Cf4bHjz1]
- 90. Autofluorescence [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/autofluorescence/]
- 91. Tissue Autofluorescence is Correlated With Intima and ... [https://pubmed.ncbi.nlm.nih.gov/41220391/]
- 92. A Systematic Review of Immune Cell Autofluorescence - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12162169/]
- 93. Efficient removal of naturally-occurring lipofuscin ... [https://www.sciencedirect.com/science/article/pii/S1526590025005863]
- 94. Artifact detection in fluorescence microscopy using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12432141/]
- 95. Five ways to extract autofluorescence (and store it) [https://www.colibri-cytometry.com/post/five-ways-to-extract-autofluorescence-and-store-it]
- 96. Importance of Antibody Titration in Flow cytometry [https://bitesizebio.com/22374/importance-of-antibody-titration-in-flow-cytometry/]
- 97. Optimize ELISA Assays with Checkerboard Titration ... [https://www.bosterbio.com/blog/post/how-to-use-checkerboard-titration-to-optimize-your-elisa-immunoassays?srsltid=AfmBOorG2wk6H6Z7wchbawM-Lexvis9BujFniRKR6d3K4dQEOjIyemHB]
- 98. Detection Systems in Immunohistochemistry [https://www.intechopen.com/chapters/64808]
- 99. Intro to Immunohistochemistry (IHC) Staining: Steps & Best ... [https://www.leicabiosystems.com/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 100. Optimization of the Blocking and Signal Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462741/]
- 101. How to Analyze ELISA Data and Calculate Results [https://www.bosterbio.com/blog/post/how-to-analyze-elisa-data-and-calculate-results-step-by-step-guide-with-troubleshooting-tips?srsltid=AfmBOoo_aY99vLGU6QIN6ODc6JzrQXKQihL2WLC32ekQBppjHo9C1QcI]
- 102. The controls that got out of control: How failed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11811022/]
- 103. How to Design Positive and Negative Controls [https://www.bosterbio.com/how-to-design-positive-negative-controls-ihc-western-blot-elisa?srsltid=AfmBOorixl8C61LMPdc_vpT_RXYVnccRto2jP2pwvsafTuU8pX5bx2ed]
- 104. Standardization of Negative Controls in Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4206554/]
- 105. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 106. of serological Validation for diagnosis of infectious diseases assays [https://pubmed.ncbi.nlm.nih.gov/9713892/]
- 107. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 108. ELISA Assay : Best Practices, Methods, and Key Insights Validation [https://www.nebiolab.com/elisa-assay-validation-guide/]
- 109. of Bioanalytical Studies: Validation and Applications Principles [https://www.linkedin.com/pulse/validation-bioanalytical-studies-principles-yudhasena-dwi-indraprasta-ottbe]
- 110. Current CAP Guidelines [https://www.cap.org/protocols-and-guidelines/current-cap-guidelines]
- 111. Cancer Protocol Templates [https://www.cap.org/protocols-and-guidelines/cancer-reporting-tools/cancer-protocol-templates]
- 112. 2025 Pathology Quality Measures [https://www.cap.org/advocacy/quality-payment-program-for-pathologists/mips-for-pathologists/2025-pathology-quality-measures]
- 113. Guidance for Submission of Immunohistochemistry ... [https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/guidance-submission-immunohistochemistry-applications-food-and-drug-administration-final-guidance]
- 114. A Comparative Evaluation of the Chemiluminescence ... [https://www.mdpi.com/2075-4418/15/13/1695]
- 115. Immunohistochemistry vs Immunocytochemistry: Updated ... [https://www.stressmarq.com/blog/immunohistochemistry-vs-immunocytochemistry/?srsltid=AfmBOopd8fUsHE-DCZQkWt_3yawJAWLHONLoZfiU95SLM7wdRW9dyEyp]
- 116. ELISA是什么-ELISA法概述 - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa.html]
- 117. Comparison of Elisa with other commonly used Immunoassa [https://www.mybiosource.com/learn/comparison-of-elisa-with-other-commonly-used-immunoassa/]
- 118. 放射免疫分析簡介- 臺中 [https://www.vghtc.gov.tw/UnitPage/RowViewDetail?WebRowsID=eb24252d-23f2-4664-822d-4d4b7ee13a08&UnitID=8b3f6cb5-ee05-4292-b18e-eca05c112404&CompanyID=e8e0488e-54a0-44bf-b10c-d029c423f6e7&UnitDefaultTemplate=1]
- 119. Comparison of enzyme-linked immunosorbent assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC497975/]
- 120. Antibody validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3891910/]
- 121. Antibody Validation: Ensuring Quality and Reliability [https://www.sysy.com/antibody-validation]
- 122. Scaling of an antibody validation procedure enables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10312534/]
- 123. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 124. Guide to Antibody Validation Techniques [https://www.neobiotechnologies.com/resources/antibody-validation-methods/?srsltid=AfmBOooItJJB6rxXtzdmJOYZvru3nY2tN0M5kY-A7eABJlmH7uaqueRY]
- 125. Antibody Validation for Immunohistochemistry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-immunohistochemistry?srsltid=AfmBOoqHtymi-Oec0Eaz8EJ9Bzgai9K2dX5UgR7dci_Vm9LSViUAMyC1]
- 126. Antibody Engineering and Therapeutics 2025 [https://www.seromyx.com/antibody-engineering-and-therapeutics-2025]
- 127. Antibodies to watch in 2025 - PubMed [https://pubmed.ncbi.nlm.nih.gov/39711140/]
- 128. Review of immunohistochemistry techniques: Applications, ... [https://pubmed.ncbi.nlm.nih.gov/38744555/]
- 129. Quantitative immunohistochemistry (IHC) analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8339853/]
- 130. Changing Cross-Reactivity for Different Immunoassays ... [https://www.mdpi.com/2076-3417/11/14/6581]
- 131. Controls for Immunohistochemistry: The Histochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4212362/]