Navigating IHC Assay Validation: A Comprehensive Guide to CLIA Requirements and Best Practices
This article provides researchers, scientists, and drug development professionals with a current and actionable guide to Immunohistochemistry (IHC) assay validation within the Clinical Laboratory Improvement Amendments (CLIA) framework.
Navigating IHC Assay Validation: A Comprehensive Guide to CLIA Requirements and Best Practices
Abstract
This article provides researchers, scientists, and drug development professionals with a current and actionable guide to Immunohistochemistry (IHC) assay validation within the Clinical Laboratory Improvement Amendments (CLIA) framework. It covers foundational regulatory concepts, step-by-step methodological protocols for assay setup, strategies for troubleshooting and optimizing performance, and essential validation procedures for compliance. The content synthesizes the latest guidelines, including the 2024 CAP update and 2025 CLIA regulatory changes, to offer a complete resource for developing robust, reliable, and clinically actionable IHC assays.
Understanding the IHC and CLIA Regulatory Landscape: A Foundation for Validated Assays
Defining IHC Assay Validation and Verification in a Clinical Context
In clinical diagnostics and therapeutic decision-making, Immunohistochemistry (IHC) serves as a critical bridge between cellular morphology and specific protein identification. The clinical utility of any IHC assay, however, is entirely dependent on the rigorous assessment of its performance characteristics. Within a regulated clinical laboratory environment, this assessment is formalized through two distinct but related processes: validation and verification. Validation applies to laboratory-developed tests (LDTs) and entails a comprehensive establishment of performance specifications. In contrast, verification is the process of confirming the stated performance characteristics of a U.S. Food and Drug Administration (FDA)-cleared or approved assay within one's own laboratory setting [1] [2]. Adherence to these processes is mandated under the Clinical Laboratory Improvement Amendments (CLIA) of 1988, which set the federal standards for all laboratory testing in the United States [1] [3]. The College of American Pathologists (CAP) has further elaborated on these requirements through evidence-based guidelines, the most recent update of which was published in February 2024, ensuring that laboratory practices evolve to meet new challenges and incorporate the latest evidence [1] [4]. This guide objectively compares the performance requirements for different types of IHC assays within this regulatory framework, providing the experimental data and protocols essential for researchers and drug development professionals.
Regulatory Framework and Key Definitions
The foundation of clinical IHC testing is built upon a clear understanding of the regulatory landscape and its specific terminology. Compliance is not optional; it is a prerequisite for patient testing.
CLIA Requirements: CLIA regulations establish the baseline federal standards that all clinical laboratories must follow to ensure the accuracy, reliability, and timeliness of patient test results. While CLIA mandates that laboratories must validate/verify the performance characteristics of all assays before reporting patient results, it does not typically prescribe the detailed methods for doing so [1] [3].
CAP Guidelines: The College of American Pathologists provides detailed, evidence-based guidelines that laboratories use to satisfy CLIA requirements. The 2024 update to the "Principles of Analytic Validation of Immunohistochemical Assays" harmonizes and clarifies previous recommendations, offering a robust framework for laboratories [1] [4]. It is important to note that while these guidelines represent best practices, CAP-accredited laboratories must comply with the current edition of the Laboratory Accreditation Program (LAP) Checklist, which may not immediately incorporate all new guideline recommendations [1].
Key Definitions:
- Validation: The comprehensive process used by a laboratory to establish the performance characteristics of a laboratory-developed test (LDT) before it is used for patient testing. This includes defining analytical sensitivity, specificity, precision, and reportable range [2].
- Verification: The process of confirming that a previously validated or FDA-cleared/approved assay performs as expected within the laboratory's own environment. The extent of verification is generally less extensive than a full validation [5] [2].
- Analytic Validation: This focuses on proving the assay itself reliably detects the target antigen. It answers the question, "Does the test work?" This is distinct from clinical validation, which determines the test's ability to predict a clinical outcome or response to therapy.
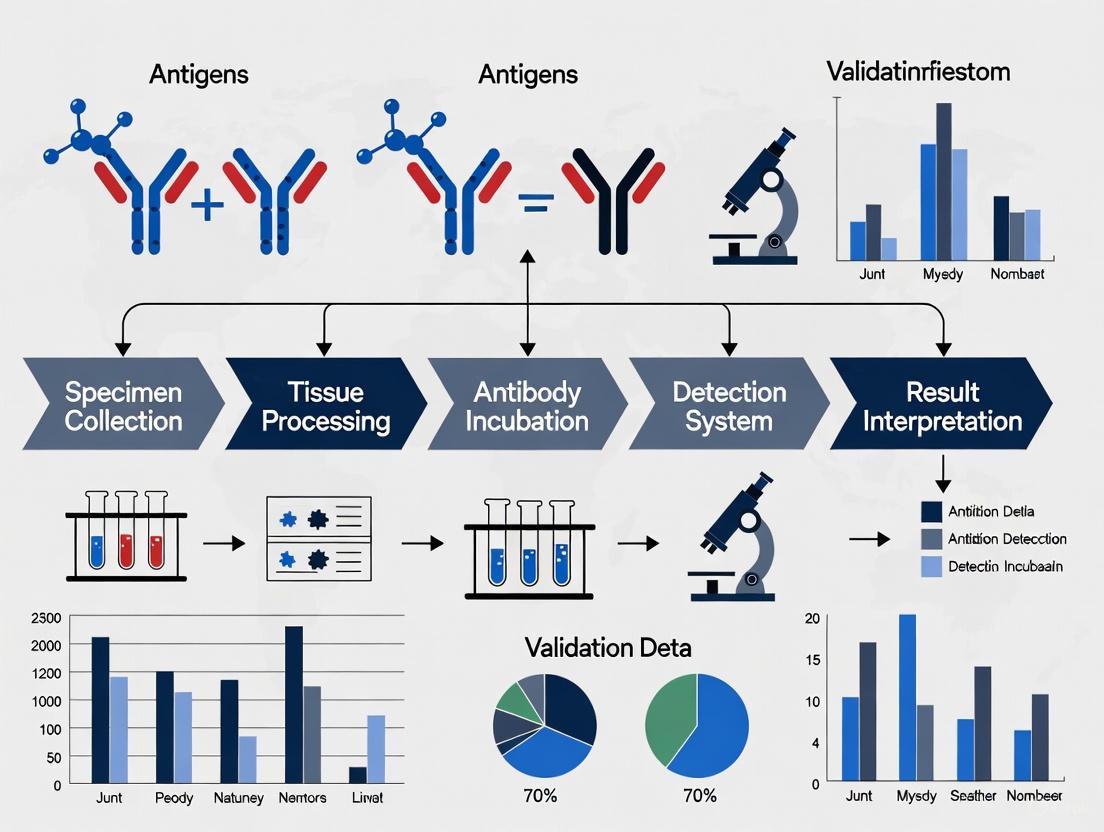
The following workflow diagram outlines the key decision points and processes for IHC assay validation and verification as per current guidelines:
Comparative Performance Data for IHC Assays
The CAP guidelines provide specific, quantitative requirements for the initial validation and verification of IHC assays. These requirements vary based on the assay type and its clinical application. The table below summarizes the key performance criteria for different assay categories.
Table 1: Summary of Analytic Validation and Verification Requirements from CAP Guidelines
| Assay Category | Minimum Case Requirements | Target Concordance | Key Considerations & Scope |
|---|---|---|---|
| Laboratory-Developated Non-Predictive Assays [2] | 10 positive and 10 negative cases | ≥90% overall concordance | Validation set should include high and low expressors and span the expected range of clinical results. |
| Laboratory-Developed Predictive Marker Assays [2] | 20 positive and 20 negative cases | ≥90% overall concordance | Applies to all predictive markers, harmonizing previous varying requirements for ER, PR, HER2. |
| FDA-Cleared/Approved Predictive Marker Assays [2] | Follow manufacturer's instructions; if none, use 20 positive and 20 negative cases | ≥90% overall concordance | Applies to unmodified FDA-approved/cleared assays. |
| Predictive Assays with Distinct Scoring Systems (e.g., PD-L1, HER2) [1] [2] | 20 positive and 20 negative cases per assay-scoring system combination | ≥90% overall concordance | Each unique antibody clone and scoring system combination must be separately validated. |
| IHC on Cytology Specimens with Alternative Fixation [1] [2] | 10 positive and 10 negative cases per fixation method | ≥90% overall concordance | Required for specimens not fixed identically to initial validation tissues (e.g., alcohol-fixed smears, cell blocks). |
A pivotal update in the 2024 guideline is the harmonization of the minimum concordance threshold to 90% for all IHC assays, including predictive markers like estrogen receptor (ER), progesterone receptor (PR), and HER2 performed on breast carcinoma, superseding previous differing thresholds [4]. Furthermore, the guideline introduces a strong recommendation for the separate validation of each unique antibody clone and scoring system combination for complex predictive markers like PD-L1 and HER2, which may employ different scoring criteria based on tumor site or type [1] [6].
Experimental Protocols for Validation Studies
Core Validation Study Design and Comparators
A fundamental component of validation is designing a study that robustly compares the new assay's performance against a reliable standard. The CAP guideline provides a list of acceptable comparators, ordered here from most to least stringent [1]:
- Cell Line Calibrators: Comparison to IHC results from cell lines with known protein quantities.
- Orthogonal Methods: Comparison with a non-immunohistochemical method (e.g., flow cytometry, fluorescent in-situ hybridization).
- External Laboratory Testing: Comparison with results from testing the same tissues in another laboratory using a validated assay.
- Prior Testing in Same Lab: Comparison with results from prior testing of the same tissues with a validated assay within the same laboratory.
- Clinical Trial Laboratory: Comparison with results from a laboratory that performed testing for a clinical trial.
- Antigen Localization: Comparison with the expected architectural and subcellular localization of the target antigen.
- Published Clinical Trials: Comparison against percent positive rates documented in published clinical trials.
- Proficiency Testing Challenges: Comparison with previously graded tissue challenges from a formal proficiency testing program.
Protocol for Validating Loss-of-Protein Expression Assays
Assays designed to detect the loss of protein expression, such as those for Succinate Dehydrogenase B (SDHB) and H3K27me3, present unique technical challenges during optimization and validation. The standard protocols optimized for detecting protein presence may not be suitable for interpreting loss of expression [7].
- Objective: To establish an IHC protocol that reliably distinguishes true loss of protein expression from weak or heterogeneous staining in tumor cells, while maintaining robust staining in internal positive control tissues.
- Methodology:
- Tissue Selection for Validation: Include known positive cases (with normal tissue serving as internal control), known negative cases (with confirmed genetic mutations leading to protein loss), and challenging cases with potential heterogeneous or "intermediate" staining patterns [7].
- Antibody Protocol Calibration: Titrate antibody dilution and antigen retrieval conditions to achieve optimal signal-to-noise ratio. The goal is a protocol that produces intense, specific staining in internal control elements (e.g., non-neoplastic cells, blood vessels) while showing definitive absence of staining in tumor cells of known negative cases. Avoid protocols that yield weak staining in controls, as this can make loss of expression in tumors difficult to distinguish [7].
- Platform Comparison: Run the validation set on different autostainer platforms if available, as staining results, particularly for heterogeneous markers, can vary significantly between instruments [7].
- Microscopic Analysis and Interpretation: Multiple pathologists should review the stained slides, focusing on the stark contrast between internal positive controls and the tumor. "Intermediate" staining patterns (weak or heterogeneous) should be noted and used to refine the diagnostic threshold [7].
- Key Experimental Controls:
- Positive Control Tissue: Tissue with known protein expression and reliable internal control elements.
- Negative Control Tissue: Tissue with a confirmed genetic alteration causing protein loss.
- Technical Control: Omission of the primary antibody to confirm absence of non-specific signal from the detection system.
Research Reagent Solutions and Materials
Successful IHC validation is contingent upon the use of well-characterized reagents and materials. The following table details essential components and their functions in the validation process.
Table 2: Essential Research Reagents and Materials for IHC Validation
| Item | Function in Validation | Critical Considerations |
|---|---|---|
| Primary Antibodies | Specifically binds to the target antigen of interest. | Clone specificity is critical. Switching clones requires full revalidation; changing vendor for the same clone requires a smaller verification [5] [2]. |
| Control Tissue Microarrays (TMAs) | Contain multiple positive and negative tissue specimens on a single slide for efficient validation. | Must include tissues with varying expression levels (high, low, negative) and should represent the intended clinical use cases [2]. |
| Antigen Retrieval Solutions | Unmask hidden epitopes altered by tissue fixation. | Changes in retrieval method (e.g., pH, buffer, heat platform) require extensive verification to ensure consistent results [5] [2]. |
| Detection System | Visualizes the antibody-antigen complex, typically using enzymatic reactions (e.g., HRP). | Changing the detection system requires verification with a sufficient number of cases to ensure performance is maintained [5]. |
| Cell Line Calibrators | Provide a standardized source of material with known antigen expression levels. | Serves as the most stringent comparator for validation study design [1]. |
| Automated Staining Platforms | Provide standardized and reproducible assay conditions. | Validation should account for platform-specific performance. Changing platforms requires verification [5] [2]. |
Navigating Verification for Modified IHC Procedures
Laboratories often need to modify existing IHC assays. The CAP guideline provides a pragmatic framework for the verification process, distinguishing between minor and major changes. The following diagram illustrates the decision-making pathway and corresponding actions for common procedural modifications.
As outlined in the pathway, the extent of verification required is proportional to the significance of the change [5] [2]:
- Minor Changes (Verification with 2 positive & 2 negative cases):
- Antibody dilution
- Antibody vendor (for the same clone)
- Incubation or retrieval times (with the same method)
- Major Changes (Verification with sufficient cases to ensure consistency):
- Fixative type
- Antigen retrieval method (e.g., change in pH, different buffer, different heat platform)
- Detection system
- Tissue processing or automated testing equipment
- Environmental conditions (e.g., laboratory relocation, water supply)
- Critical Change (Requires Full Revalidation):
- Changing the antibody clone
Within the clinical context, the rigorous processes of IHC assay validation and verification are non-negotiable prerequisites for ensuring diagnostic accuracy and patient safety. The updated 2024 CAP guidelines provide a clear, harmonized framework for laboratories, emphasizing a 90% minimum concordance for all assays, separate validation for complex predictive markers with multiple scoring systems, and specific guidance for cytology specimens and assay modifications. For researchers and drug developers, a deep understanding of these requirements is not merely about regulatory compliance; it is the foundation upon which reliable, reproducible, and clinically impactful IHC data is built. By adhering to these structured protocols and utilizing the appropriate reagents and controls, laboratories can ensure their IHC assays perform as intended, directly supporting precise therapeutic decision-making and advancing the field of personalized medicine.
Core CLIA Requirements for Laboratory-Developed Tests (LDTs) and FDA-Cleared Assays
For researchers and drug development professionals, navigating the regulatory landscape for immunohistochemistry (IHC) assays is fundamental to ensuring reliable and reproducible biomarker data. The U.S. regulatory framework primarily involves two distinct pathways: the Clinical Laboratory Improvement Amendments (CLIA) and the Food and Drug Administration (FDA) clearance or approval process [3]. CLIA establishes quality standards for all laboratory testing performed on human specimens, focusing on the analytical validity of the testing process itself, regardless of whether the test is a laboratory-developed test (LDT) or an FDA-cleared assay [8]. In contrast, the FDA regulates commercial in vitro diagnostic (IVD) products, assessing their safety and effectiveness before they are marketed [8].
Understanding the distinction between LDTs and FDA-cleared assays is critical. An LDT is a test that is developed, validated, and used within a single laboratory [8]. These tests are crucial for personalized medicine, especially for novel biomarkers where no commercial test exists. They are validated under CLIA regulations, with specific analytical performance characteristics established by the laboratory director. An FDA-cleared or approved assay is a commercial product that has undergone rigorous FDA review to demonstrate its safety and effectiveness for its intended use [3]. When a laboratory introduces such a test, it must perform a verification process to confirm the manufacturer's claims under its own CLIA-certified conditions [1] [2]. The core distinction lies in the regulatory focus: CLIA ensures the quality of the laboratory's testing process, while FDA oversight for IVDs ensures the safety and effectiveness of the commercial test product itself.
Comparative Analysis of Core CLIA Requirements
The validation and verification requirements for IHC assays under CLIA differ significantly between LDTs and FDA-cleared tests, primarily in scope, sample size, and performance benchmarks. The table below summarizes the key requirements based on the latest College of American Pathologists (CAP) guidelines.
Table: Core CLIA Validation and Verification Requirements for IHC Assays
| Requirement | Laboratory-Developed Tests (LDTs) | FDA-Cleared/Approved Assays |
|---|---|---|
| General Principle | Must undergo full analytic validation before reporting patient results [1] [2]. | Must undergo analytic verification to confirm manufacturer's stated performance [1] [2]. |
| Overall Concordance | Must achieve at least 90% overall concordance with the comparator method [2]. | Must achieve at least 90% overall concordance with the expected results [2]. |
| Non-Predictive Markers | Minimum of 10 positive and 10 negative tissue cases [2]. | Follow manufacturer's instructions; if none, minimum of 20 positive and 20 negative tissues is recommended [2]. |
| Predictive Markers | Minimum of 20 positive and 20 negative tissue cases [2]. | Follow manufacturer's instructions; if none, minimum of 20 positive and 20 negative tissues is recommended [2]. |
| Assays with Multiple Scoring Systems | Each assay-scoring system combination must be separately validated with 20 positive and 20 negative tissues [1] [2]. | Each assay-scoring system combination must be separately verified with 20 positive and 20 negative tissues [1] [2]. |
| Cytology Specimens (Alternative Fixatives) | Separate validation required; minimum of 10 positive and 10 negative cases recommended for each fixation method [1] [2]. | Not explicitly stated, but laboratories should ensure performance is verified for alternative fixatives if used. |
Key Considerations for Validation and Verification
- Validation Study Design: For LDTs, the CAP guideline outlines multiple comparator options for validation study design, listed here from most to least stringent: comparison to protein-calibrated cell lines; non-IHC methods (e.g., flow cytometry); testing in another validated lab; prior testing in the same lab; expected antigen localization; results from clinical trials; published positive rates; and formal proficiency challenges [1] [2].
- Revalidation Triggers: CLIA requires laboratories to confirm assay performance after specific changes. A full revalidation (equivalent to an initial validation) is required when the antibody clone is changed. Other changes, such as in antibody dilution, vendor (same clone), incubation times, fixative type, antigen retrieval method, detection system, or testing platform, require a sufficient number of tissues to be tested to ensure consistent performance [2].
- Personnel Qualifications: CLIA regulations set strict personnel standards for laboratory directors, technical consultants, and testing personnel. Recent updates, effective in 2025, have refined the definitions of qualified degrees and experience, generally requiring education in chemical, biological, or clinical laboratory science and experience obtained in a CLIA-compliant facility [9] [10].
Experimental Protocols for IHC Assay Validation
This section details standard experimental methodologies used to generate the validation data required for compliance with CLIA standards.
Standard Validation Protocol for a Predictive IHC LDT
The following protocol is aligned with CAP guidelines for validating a predictive, laboratory-developed IHC assay, such as HER2 or PD-L1 [2].
Objective: To establish the analytical validity of a new LDT for a predictive biomarker by determining its concordance with a validated comparator method.
Materials and Reagents:
- Tissue Selection: A minimum of 40 unique, de-identified FFPE tissue blocks (20 positive, 20 negative) that span the expected range of clinical results, including high and low expressors where appropriate [2]. Tissues must be processed with the same fixative and methods intended for clinical use.
- Primary Antibody: The antibody clone and detection system under validation.
- Comparator Method: The gold-standard method for comparison (e.g., a different validated IHC assay, FISH, or NGS) [1].
Methodology:
- Sectioning and Staining: Cut sections from all 40 FFPE blocks. Process all slides in a single batch using the fully defined LDT protocol to minimize run-to-run variation.
- Comparison Testing: Subject the same set of cases to the established comparator method, ideally within a short timeframe.
- Blinded Evaluation: A pathologist, blinded to the results of the comparator method, scores all slides from the LDT. A second pathologist should independently score a significant subset to assess inter-observer reproducibility.
- Data Analysis: Calculate the overall percent agreement, positive percent agreement, and negative percent agreement between the LDT and the comparator. The overall concordance must meet or exceed the 90% threshold to be acceptable [2].
Protocol for an Interlaboratory Concordance Study
Interlaboratory studies are critical for verifying the reproducibility of an assay, a key aspect of robust validation [3] [11].
Objective: To evaluate the consistency of IHC results for a specific biomarker across different laboratories using the same or different antibody assays.
Materials and Reagents:
- Common Tissue Set: A series of FFPE tissue samples with a range of biomarker expression levels (e.g., HER2-zero, HER2-low, HER2-positive).
- Standardized Protocols: Participating laboratories may use their established, validated protocols, including different antibody clones (e.g., A0485 vs. 4B5 for HER2) and staining platforms [11].
Methodology:
- Sample Distribution: Distribute the common tissue set to all participating laboratories.
- Independent Staining and Scoring: Each laboratory processes, stains, and scores the tissues according to their standard clinical protocols. Pathologists in each lab score the samples without knowledge of other labs' results.
- Data Consolidation and Analysis: A central team collects all scores and calculates the concordance rates between laboratories. Statistical analysis, such as Cohen's kappa for inter-rater reliability, is performed.
- Interpretation: The study can reveal assay-specific differences. For example, the cited study showed a significantly higher detection rate for HER2-low expression using the Ventana 4B5 assay compared to the Dako A0485 antibody [11].
Emerging Methodologies and AI in IHC Validation
Advanced computational approaches are revolutionizing IHC biomarker prediction and validation, offering paths to enhanced standardization.
AI-Assisted Biomarker Prediction Workflow
Artificial intelligence models, particularly those using dual-modality learning, show promise in improving the accuracy and objectivity of IHC interpretation [12].
Diagram: AI-Powered Biomarker Prediction from H&E and IHC
This workflow illustrates a dual-modality AI framework that integrates both H&E and IHC stained whole slide images to predict biomarker status with high accuracy (AUROC >0.96) [12]. The model extracts features from both image types, aggregates them, and generates a prediction that has demonstrated superior prognostic precision compared to standard biomarker assessments in some studies [12].
Experimental Protocol for AI Model Validation
Objective: To validate the performance of an AI tool in predicting a key biomarker (e.g., PD-L1) from H&E and IHC whole slide images.
Materials and Reagents:
- Dataset: A large, retrospective cohort of WSIs (H&E and matched IHC) with confirmed biomarker status determined by standard methods (e.g., PCR for MSI, IHC with CPS scoring for PD-L1) [12].
- Computational Resources: High-performance computing clusters with GPUs suitable for deep learning.
- Software: Image analysis pipelines (e.g., QuPath for tissue segmentation) and deep learning frameworks (e.g., PyTorch, TensorFlow).
Methodology:
- Data Preprocessing: Train pixel classification models to segment tissues from H&E and IHC WSIs. Extract smaller image patches from the segmented tissue regions [12].
- Model Training: Train a transformer-based model on the image patches to extract relevant features. Use a separate aggregation algorithm to combine patch-level features into a single slide-level prediction [12].
- Performance Evaluation: Evaluate the model's performance on a held-out test set of WSIs by calculating the area under the receiver operating characteristic curve (AUROC), sensitivity, and specificity. Compare the AI-predicted biomarker status against the ground-truth clinical status.
- Clinical Correlation: Assess the clinical utility of the AI prediction by analyzing outcomes such as time-on-treatment and overall survival for patients treated with targeted therapies, comparing the stratification achieved by the AI model to that of conventional IHC [12].
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagent Solutions for IHC Assay Development and Validation
| Item | Function in IHC Assay Validation |
|---|---|
| Primary Antibodies | Key reagent that binds specifically to the target antigen. Validation requires careful selection of clone, vendor, and optimal dilution [2] [11]. |
| Control Cell Lines | Cell lines with known protein expression levels used as calibrators; one of the most stringent comparators for validation [1] [2]. |
| FFPE Tissue Microarrays (TMAs) | Contain multiple tissue cores on a single slide, enabling high-throughput screening of antibody performance across many tissues during validation [12]. |
| Detection Kits | Reagent systems that generate a detectable signal from antibody-antigen binding; changing the detection system requires revalidation [2]. |
| Automated Staining Platforms | Instruments that standardize the staining process; changing platforms requires confirmation of assay performance [2] [11]. |
| Image Analysis Software | AI and digital pathology tools that provide quantitative, objective scoring of IHC staining, reducing inter-observer variability [13] [12]. |
In the field of diagnostic pathology and therapeutic development, Immunohistochemistry (IHC) assays serve as critical tools for detecting protein biomarkers in tissue samples. The accuracy and reliability of these assays are paramount, as they directly influence patient diagnosis, prognosis, and treatment decisions. Within the framework of the Clinical Laboratory Improvement Amendments (CLIA), two principal guideline systems govern the validation of IHC assays: the College of American Pathologists (CAP) "Principles of Analytic Validation of Immunohistochemical Assays" 2024 update and the Clinical and Laboratory Standards Institute (CLSI) standards, particularly ILA28. These guidelines provide complementary but distinct pathways to ensure that IHC assays perform with the precision, accuracy, and reliability required for clinical use. This guide objectively compares these foundational frameworks, examining their respective requirements, experimental approaches, and applications within the context of modern laboratory medicine and drug development.
Comparative Analysis: CAP 2024 Update vs. CLSI Standards
The CAP 2024 Guideline Update and CLSI standards represent two comprehensive but differently focused approaches to IHC assay validation. The table below summarizes their core characteristics and requirements for direct comparison.
Table 1: Core Characteristics of CAP and CLSI IHC Validation Guidelines
| Feature | CAP 2024 Guideline Update | CLSI ILA28 Standard |
|---|---|---|
| Primary Focus | Analytical validation of IHC assays for clinical use [1] | Quality assurance for the total test system, including design control and implementation [14] |
| Scope | Focused on analytical validation/verification processes | Covers the total product life cycle: discovery, design, development, verification, and validation [14] |
| Key Applications | Diagnostic, prognostic, and predictive markers; expanded guidance for cytology specimens and predictive markers with distinct scoring systems [1] | Diagnostic, prognostic, and predictive applications on formalin-fixed, paraffin-embedded material and cytological preparations [14] |
| Validation Cases (Predictive Markers) | 20 positive and 20 negative cases [15] | Not explicitly specified in search results; defers to laboratory director's judgment |
| Validation Cases (Non-predictive Markers) | 10 positive and 10 negative cases [15] | Not explicitly specified in search results; defers to laboratory director's judgment |
| Concordance Threshold | 90% for all IHC assays [1] | Not explicitly specified in search results |
| Cytology Specimen Validation | Minimum 10 positive and 10 negative cases for alternative fixatives [1] | Addresses cytological preparations but specific case numbers not detailed [14] |
| Regulatory Recognition | Informs CAP Laboratory Accreditation Program; not currently mandated in LAP checklist [1] | FDA-recognized consensus standard [14] |
Experimental Protocols for IHC Assay Validation
CAP 2024 Recommended Workflow
The CAP 2024 guideline outlines a structured process for bringing new IHC assays into clinical use, from initial feasibility assessment to ongoing maintenance [15]. This workflow encompasses pre-analytical, analytical, and post-analytical phases to ensure comprehensive validation.
Pre-Validation Investigation: Before validation begins, laboratories must conduct a thorough investigation documenting clinical utility, projected test volumes, cost-effectiveness, and resource availability. This includes literature review of clone-specific performance data from sources like NordiQC and consultation with ordering pathologists and clinicians [15].
Optimization Phase: For laboratory-developed tests (LDTs), this involves selecting an appropriate antibody clone, identifying tissues with known expression of the target antigen, and iteratively adjusting reaction conditions (dilution, incubation, pretreatment parameters) until optimal staining is achieved. FDA-cleared/approved assays typically skip this phase and are used according to manufacturer specifications [15].
Validation/Verification Execution: The validation study tests the assay against a predetermined number of known positive and negative cases. CAP recommends 20 positive and 20 negative cases for predictive markers and 10 each for non-predictive markers. For rare antigens, collaborative approaches or cell lines may be necessary [15].
Analysis and Acceptance Criteria: Results are analyzed for overall concordance, with a target threshold of 90% for all IHC assays. Discordant results are scrutinized to identify potential issues with assay sensitivity or specificity [1].
CLSI's Total Test System Approach
CLSI guideline ILA28 emphasizes a comprehensive "total test system" approach, ensuring quality across all phases of the assay lifecycle from design to implementation [14]. The standard provides guidelines for developing validated IHC assays with attention to pre-examination, examination, and post-examination processes to ensure clinical applicability.
Technical Challenges and Special Considerations
Validation of Assays for Loss of Protein Expression
IHC assays designed to detect loss of protein expression, such as Succinate Dehydrogenase subunit B (SDHB) and H3K27me3, present unique validation challenges. These require different optimization strategies compared to assays detecting protein overexpression [7].
- SDHB Validation Challenges: Antibody protocols must produce strong staining in internal controls to effectively distinguish true loss of expression in tumor cells. Suboptimal protocols can result in staining patterns in mutated tumors that are difficult to distinguish from retained expression [7].
- H3K27me3 Heterogeneous Staining: Some tumors, including malignant peripheral nerve sheath tumors (MPNST), show heterogeneous staining, with results potentially varying between different autostainer platforms. This heterogeneity complicates protocol calibration and diagnostic interpretation [7].
- Tissue Selection for Validation: The choice of validation tissues is particularly critical for these assays. Establishing an optimal balance between analytical sensitivity and specificity during protocol optimization is essential for reliable performance [7].
Specimen-Specific Validation Requirements
The CAP 2024 update provides specific guidance for validating IHC assays on cytology specimens fixed in alternative fixatives, recognizing the variable sensitivity of IHC on such specimens compared to formalin-fixed, paraffin-embedded (FFPE) tissues. Laboratories must perform separate validations with a minimum of 10 positive and 10 negative cases for each alternative fixative type used [1].
Platform and Personnel Variability
The CAP guideline recommends that validation plans address potential variability from instruments and personnel. A robust strategy might include running validation sets on different instruments over several days, with each run performed by different laboratory personnel to ensure consistency across operational conditions [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful IHC assay validation relies on a comprehensive toolkit of reagents and materials. The table below details essential components and their functions in the validation process.
Table 2: Essential Research Reagent Solutions for IHC Assay Validation
| Reagent/Material | Function in Validation | Application Notes |
|---|---|---|
| Primary Antibodies | Specifically binds to target antigen for detection | Clone selection critical; consult NordiQC assessments and CAP proficiency testing data for performance characteristics [15] |
| Control Tissue Arrays | Contain multiple tissue types with known antigen expression on a single slide | Enable efficient validation with reduced reagent use; ideal for including range of expression levels [15] |
| Cell Line Calibrators | Contain known amounts of target protein | Serve as stringent comparators for validation study design; particularly valuable for rare antigens [1] |
| Antigen Retrieval Reagents | Unmask hidden epitopes altered by tissue fixation | Optimization of retrieval conditions (pH, time, method) is often necessary for LDTs [15] |
| Detection Systems | Amplify and visualize antibody-antigen interactions | Selection affects assay sensitivity and background; must be compatible with primary antibody [14] |
| Reference Standards | Provide predetermined expected results for comparison | Can include orthogonal testing methods (e.g., FISH, molecular), results from another laboratory, or published clinical trial data [1] |
Regulatory Pathways and Compliance Framework
CLIA Compliance and Beyond
While CLIA provides federal standards for all laboratory testing, it does not specify detailed methodologies for satisfying performance requirements for IHC assays [3]. Laboratories therefore rely on CAP and CLSI guidelines to demonstrate CLIA compliance. However, manufacturers seeking commercial approval for in vitro diagnostic (IVD) tests must follow more rigorous pathways through the FDA, which often requires studies exceeding basic CLIA requirements [3].
Comparison of US and EU Regulatory Requirements
The regulatory landscape for IHC assays differs significantly between the United States and European Union, affecting validation strategy for globally marketed products.
US Regulatory Pathway: In the United States, companion diagnostics (CDx) may be classified as either Class II or Class III devices, with approval processes involving Premarket Approval (PMA) submissions to the FDA. The FDA favors a modular PMA process with timelines of approximately 12-24 months, requiring compliance with 21 CFR Part 820 and Bioresearch Monitoring (BIMO) audits [3].
EU Regulatory Pathway: Under the In Vitro Diagnostic Regulation (IVDR), companion diagnostics are uniformly classified as Class C devices. The approval process involves submission of a technical dossier to a notified body, with typical timelines of 12-18 months for CE marking, and requires quality management system audits against ISO 13485 [3].
The CAP 2024 Guideline Update and CLSI ILA28 standard provide robust, complementary frameworks for IHC assay validation within CLIA requirements. The CAP guidelines offer specific, evidence-based recommendations for analytical validation with defined case numbers and concordance thresholds, particularly valuable for clinical laboratories implementing both predictive and non-predictive IHC assays. Meanwhile, CLSI standards provide comprehensive guidance covering the entire assay lifecycle, with emphasis on total quality management systems. For researchers and drug development professionals, understanding both frameworks is essential for developing clinically reliable assays. The CAP guidelines serve as an immediate resource for validation protocols, while CLSI standards provide the foundation for quality systems supporting regulatory submissions. Together, these guidelines ensure that IHC assays meet the rigorous standards required for both diagnostic use and therapeutic development in an evolving precision medicine landscape.
The Clinical Laboratory Improvement Amendments (CLIA) regulations underwent their first major update in over three decades, with significant changes to personnel qualifications taking full effect in 2025 [16] [17]. These revisions establish more precise standards for laboratory directors and staff performing moderate- and high-complexity testing, directly impacting how laboratories approach immunohistochemistry (IHC) assay validation and daily operations. For researchers, scientists, and drug development professionals, understanding these updated requirements is essential for maintaining compliance while advancing diagnostic and therapeutic development.
The updated rules reflect a concerted effort to balance addressing healthcare workforce shortages with ensuring patient safety and test reliability [16]. Key modifications include refined educational requirements, new experience mandates, and expanded pathways for certain roles, all while eliminating previous equivalency provisions that allowed for greater interpretation [9] [18]. This guide provides a detailed comparison of the updated standards, offering clarity on qualification pathways for laboratory directors and staff within the context of modern laboratory practice and IHC validation requirements.
Updated Qualification Pathways for Laboratory Directors
Laboratory directors bear ultimate responsibility for all test operations, and the 2025 CLIA rules substantially redefine the qualification pathways for these critical roles [9] [16]. The updates create distinct requirements based on testing complexity and degree type, with an increased emphasis on documented specialized training and specific scientific disciplines.
Comparative Analysis of Director Qualifications
Table: CLIA 2025 Laboratory Director Qualification Pathways
| Position & Complexity | Degree Requirement | Key Experience Requirements | New Training Mandates | Grandfathering Provision |
|---|---|---|---|---|
| High-Complexity Lab Director (Non-Physician) | Doctoral degree (PhD) in chemical, biological, or medical laboratory science [16] | 2 years of laboratory training/experience AND 2 years of experience directing/supervising high-complexity testing [16] | 20 continuing education (CE) hours in laboratory practice covering director responsibilities [16] | Yes, for individuals continuously employed in role since 12/28/2024 [18] |
| Moderate-Complexity Lab Director (Master's Degree) | Master's degree in chemical, biological, clinical, or medical laboratory science [9] | 1 year of laboratory training/experience AND 1 year of supervisory experience in nonwaived testing [16] | 20 CE hours covering director responsibilities [16] | Yes, for individuals continuously employed in role since 12/28/2024 [9] |
| Moderate-Complexity Lab Director (Bachelor's Degree) | Bachelor's degree in chemical, biological, or medical laboratory science [9] | 2 years of laboratory training/experience AND 2 years of supervisory experience in nonwaived testing [16] | 20 CE hours covering director responsibilities [16] | Yes, for individuals continuously employed in role since 12/28/2024 [9] |
Key Changes and Enforcement Discretion
A significant change requires non-physician directors of high-complexity laboratories to hold board certification from an HHS-approved board, such as the American Board of Bioanalysis (ABB) or American Board of Clinical Chemistry (ABCC) [18]. The previously available pathway using "equivalent qualifications" has been eliminated [9] [18].
While the new rules formally mandate 20 CE credit hours in laboratory director responsibilities for most pathways, the Centers for Medicare & Medicaid Services (CMS) has announced it will not currently enforce this CE requirement through a temporary enforcement discretion [18]. This provides a transition period for current personnel, though future compliance is likely expected.
The updated regulations also specify that physical science degrees no longer automatically qualify individuals for director positions or other roles requiring a science degree [16]. CMS now recognizes only degrees in biological sciences, chemical sciences, or clinical/medical laboratory technology [9] [17].
Revised Requirements for Technical Consultants, Supervisors, and Testing Personnel
The updated CLIA regulations extend beyond director roles, significantly modifying qualifications for technical consultants, supervisors, and testing personnel [9] [16]. These changes create new pathways for some roles while restricting others, with important implications for laboratory staffing and workflow management.
Technical Consultants and Supervisors
Technical consultants (for moderate-complexity testing) and technical supervisors (for high-complexity testing) now have more structured qualification pathways. A notable expansion allows individuals with an associate degree in medical laboratory technology plus four years of lab training or experience in nonwaived testing to qualify as technical consultants for moderate-complexity testing [9] [16]. This change helps address workforce shortages while maintaining quality standards.
For high-complexity technical supervisors, the updated rules remove previous qualification mechanisms such as certification by the American Society of Cytology, requiring instead that candidates meet more standardized educational and experience benchmarks [9].
Testing Personnel and Military Training
The updated rules provide clearer equivalency standards for testing personnel with bachelor's degrees, specifying that 120 semester hours from an accredited institution can substitute for a degree if they include specific coursework in medical laboratory science, biology, and chemistry [9].
A significant permanent pathway now exists for military-trained laboratory technicians with the medical laboratory specialist occupational specialty to qualify as testing personnel for moderate- and high-complexity testing [16]. This formal recognition of military training helps create a pipeline for veterans to enter civilian laboratory roles.
Nursing Professionals and High-Complexity Testing
After receiving substantial feedback, CMS reversed its initial proposal that would have allowed individuals with a Bachelor of Science in Nursing (BSN) to perform high-complexity testing without additional training [16] [17]. The final rule requires nurses to complete additional training in biological/chemical sciences and clinical lab science equivalent to an associate degree in laboratory science before performing high-complexity testing [16].
Practical Implications for IHC Assay Validation and Laboratory Workflow
The updated personnel qualifications directly impact how laboratories approach IHC assay validation and daily operations. Understanding the practical implications of these changes is crucial for maintaining compliance while ensuring efficient laboratory workflow and reliable test results.
Integration with IHC Validation Guidelines
The 2025 CLIA personnel requirements complement recent updates to IHC validation standards, particularly the College of American Pathologists (CAP) "Principles of Analytic Validation of Immunohistochemical Assays" guideline update released in early 2024 [1]. Laboratory directors overseeing IHC validation must now ensure that:
- Personnel involved in validation processes meet updated educational and training requirements [9] [16]
- Each assay-scoring system combination (e.g., HER2, PD-L1) is separately validated/verified [1]
- Validations for IHC performed on cytology specimens with alternative fixatives include at least 10 positive and 10 negative cases [1]
The harmonized 90% concordance requirement for all predictive marker IHC assays in the updated CAP guidelines aligns with the CLIA emphasis on standardized quality measures [1].
Modified Assay Verification Protocols
For laboratories modifying existing IHC procedures, the personnel changes coincide with simplified verification protocols for specific changes. When switching antibodies from different vendors while using the same clone, CAP guidelines recommend verification with only 2 known positive and 2 known negative cases rather than full re-validation [5]. This efficient protocol can be implemented by qualified technical staff under the supervision of appropriately credentialed directors.
Table: IHC Assay Modification Requirements Under CAP Guidelines
| Type of Modification | Verification Requirement | Personnel Oversight |
|---|---|---|
| Minor Changes: Antibody dilution, vendor (same clone), incubation/retrieval times (same method) [5] | Confirm performance with 2 known positive and 2 known negative cases [5] | Technical supervisor with updated CLIA qualifications [9] |
| Major Changes: Fixative type, antigen retrieval method, detection system, testing equipment [5] | Comprehensive validation with sufficient cases to ensure consistent performance [5] | Laboratory director meeting updated 2025 CLIA standards [16] |
Implementation Workflow and Compliance Strategy
The following diagram illustrates the logical workflow for implementing the 2025 CLIA personnel requirements in the context of IHC assay validation:
Essential Research Reagent Solutions for IHC Validation
Implementing proper IHC assay validation under the updated CLIA framework requires specific reagent systems and materials. The following solutions represent core components necessary for developing compliant IHC assays.
Table: Essential Research Reagent Solutions for IHC Validation
| Reagent Solution | Primary Function in IHC Validation | Regulatory Compliance Consideration |
|---|---|---|
| Validated Primary Antibodies | Target antigen detection with defined specificity and sensitivity [5] | Must demonstrate 90% concordance for predictive markers; clone-specific verification simplifies process [1] [5] |
| Antigen Retrieval Buffers | Expose epitopes masked by formalin fixation [5] | Changes in retrieval method (pH, buffer) require more extensive verification [5] |
| Detection Systems | Amplify signal with minimal background noise [5] | Switching detection systems necessitates comprehensive re-validation [5] |
| Control Cell Lines | Provide known antigen expression levels for calibration [1] | Serves as stringent comparator for validation study design [1] |
| Reference Standards | Establish expected staining patterns and intensity [1] | Enables comparison against published clinical trial data [1] |
The 2025 CLIA personnel updates represent the most significant regulatory change in decades for laboratory operations, establishing more rigorous and specific qualification pathways for directors and staff. For professionals involved in IHC assay validation and drug development, these changes necessitate careful review of current personnel credentials, strategic planning for staffing needs, and integration with updated analytical validation guidelines from organizations like CAP.
While the new requirements create certain challenges for laboratories, particularly regarding board certification for high-complexity PhD directors and the elimination of physical science degrees as automatic qualifications, they also provide clearer pathways for military-trained personnel and technical consultants. The concurrent updates to IHC validation guidelines offer opportunities to streamline certain verification processes, especially when implementing minor methodological changes.
Successful navigation of this new landscape requires a proactive approach to compliance, including documentation of grandfathering status where applicable, strategic pursuit of board certifications, and development of comprehensive training programs that address both technical competencies and regulatory requirements. By integrating these updated personnel standards with robust analytical validation protocols, laboratories can maintain compliance while advancing the development of reliable diagnostic and therapeutic tools.
For researchers and drug development professionals navigating the complex landscape of In Vitro Diagnostic (IVD) development, understanding how regulatory bodies classify device risk is fundamental to clinical trial planning and regulatory strategy. The U.S. Food and Drug Administration (FDA) classifies investigational IVDs used in clinical studies as either Significant Risk (SR) or Nonsignificant Risk (NSR), a determination that directly dictates the pathway for regulatory compliance [19] [20].
This classification is critical because it determines whether a manufacturer must obtain an Investigational Device Exemption (IDE) from the FDA before initiating clinical studies [21] [19]. SR device studies require an approved IDE application, subjecting them to full FDA oversight and more stringent regulatory requirements. In contrast, NSR device studies are subject to "abbreviated" IDE requirements and rely primarily on institutional review board (IRB) oversight [19]. This risk assessment is uniquely tied to the device's potential to harm research participants, focusing primarily on the sampling procedures required and the potential consequences of erroneous results [19].
Regulatory Framework and Key Definitions
The regulatory framework for IVDs is established under the Federal Food, Drug, and Cosmetic Act, with IVDs defined as reagents, instruments, and systems intended for the diagnosis of disease or other conditions using specimens taken from the human body [21]. Like other medical devices, IVDs are subject to premarket and postmarket controls, and the FDA classifies them into Class I, II, or III based on the level of regulatory control needed to assure safety and effectiveness [21].
For clinical investigations, the key definitions guiding risk assessment are:
- Significant Risk (SR): A clinical investigation is deemed SR when it involves an investigational medical device that presents a potential for serious risk to the health, safety, or welfare of a participant [19]. SR determinations require an IDE submission to the FDA.
- Nonsignificant Risk (NSR): An investigational device that does not carry this potential for serious risk is classified as NSR [19]. NSR studies are subject to abbreviated IDE requirements.
The intended use and indications for use are primary drivers of the risk classification [20]. If an incorrect test result could lead to patient harm—such as a false negative causing a subject to miss a critical treatment—the IRB or FDA may consider the device SR, even if the sampling procedure itself is minimal risk [20].
Table 1: Key Regulatory Definitions for IVD Risk Assessment
| Term | Definition | Regulatory Consequence |
|---|---|---|
| Significant Risk (SR) | Presents potential for serious risk to health, safety, or welfare of a participant [19] | Requires an approved Investigational Device Exemption (IDE) from FDA [19] |
| Nonsignificant Risk (NSR) | Does not carry potential for serious risk [19] | Subject to abbreviated IDE requirements; primary oversight by IRB [19] |
| Investigational Device Exemption (IDE) | Allows an investigational device to be used in a clinical study to collect safety and/or effectiveness data [21] | Permits device shipment for research without full compliance with commercial distribution requirements [21] |
Core Components of IVD Risk Assessment
Evaluation of Sampling Procedures
The first critical component in risk assessment involves analyzing the sampling procedures required to obtain specimens for the investigational IVD. If these procedures are performed solely for research purposes and present significant risk, the entire study is typically classified as SR [19].
Table 2: Risk Classification of Common IVD Sampling Procedures
| Typically Significant Risk (SR) Procedures | Typically Nonsignificant Risk (NSR) Procedures |
|---|---|
| Biopsy of a major organ [19] | Blood obtained via finger stick or simple venipuncture [19] |
| Sampling requiring general anesthesia [19] | Saliva collection and buccal swabs [19] |
| Placement of a blood access line into an artery or large vein [19] | Use of existing specimens (archival tissue, biorepository samples) [19] |
| Procedures that prolong standard of care surgery [19] | Use of otherwise-discarded remnant tissue from standard procedures [19] |
| Skin punch biopsies [19] |
It is crucial to note that patient population characteristics—including health status, comorbidities, and medications—can elevate the risk of typically NSR procedures, necessitating careful study-specific evaluation [19].
Impact of Invalid Test Results
When research does not involve SR sampling procedures, the assessment shifts to the potential harm from inaccurate test results. All investigational IVD clinical trials must consider the impact of returning results on participants' clinical care outside the trial [19].
- False Positive Results: May lead to misdiagnosis, unnecessary treatments, unneeded confirmatory testing, and psychological trauma if a participant erroneously believes they have a serious disease [19] [22].
- False Negative Results: Might cause participants to forego or delay needed treatment, with potentially serious health implications [19] [22].
The method of result return also affects risk. IVDs intended for home use may present greater risk than lab-based tests because lay users interpret results without professional training [19]. Furthermore, using investigational IVDs for treatment decisions in therapeutic product trials substantially increases their risk profile [3].
Special Considerations for Therapeutic Product Trials
Clinical trials investigating therapeutic products present additional risk considerations when they utilize investigational IVDs for participant selection, treatment arm assignment, safety monitoring, or outcome prediction [19]. In these contexts, the safety profile of the therapeutic agent itself becomes a significant factor in the risk determination, as its safety and effectiveness have not been fully established [19].
Key protection considerations include:
- Foregoing Established Treatments: Will IVD results lead participants to forego or delay treatments known to be effective? Risk increases when established treatments are available outside the clinical trial [19].
- Exposure to Safety Risks: Will IVD use expose participants to safety risks from the investigational therapeutic that exceed those of standard care? As potential side effects increase in severity, so does the impact of invalid results [19].
- Biomarker-Therapeutic Relationship: Is there a well-established link between the biomarker detected by the IVD and the investigational therapeutic? Using an IVD with unestablished clinical validity to enroll participants increases overall risk [19].
For companion diagnostics specifically, regulatory strategy must account for their classification as Class II or III devices in the U.S., requiring either Premarket Approval (PMA) or 510(k) clearance [3].
Risk Determination Protocols and Regulatory Pathways
The Risk Determination Process
Sponsors and sponsor-investigators have several pathways for obtaining formal risk determinations:
- Sponsor's Initial Assessment: The sponsor performs an initial risk determination based on the potential for harm to subjects, including risks associated with device use [19] [20].
- IRB Review and Determination: IRBs serve as FDA surrogates in device risk determinations. They review the sponsor's assessment and can agree or reclassify the study [19] [20]. If an IRB reclassifies an NSR study as SR, the sponsor must notify the FDA within five working days and submit an IDE application [20].
- FDA Q-Submission Process: The traditional way to obtain a formal device risk determination is through the Q-Submission process [19]. For therapeutic product trials conducted under an IND, sponsors can also contact their FDA program officer for help determining if an investigational IVD is SR [19].
- Dual 510(k) and CLIA Waiver Pathway: For certain devices, manufacturers may pursue a dual submission containing both a 510(k) and CLIA Waiver by Application, with the FDA providing substantive interaction within 90 days [23].
Study Risk Determination for IVDs in Therapeutic Trials
When an IVD assay is used for prospective stratification or clinical decision-making in therapeutic trials, a Study Risk Determination (SRD) is necessary to evaluate if an IDE is required [3]. Manufacturers can submit an SRD Q-submission to the FDA for an official determination, have the IRB assess risk as an FDA surrogate, include the assessment in a pre-IND briefing book, or simply assume significant risk and submit an IDE [3].
Table 3: Methodological Approaches to IVD Risk Determination
| Methodology | Description | Application Context |
|---|---|---|
| Risk Analysis | Identification of potential sources of error for the device [23] | Required for CLIA Waiver by Application; fundamental to all IVD risk assessment |
| Risk Evaluation & Control | Description of implemented mitigation measures and validation studies for failure alerts and fail-safe mechanisms [23] | Critical for demonstrating risk control in SRD submissions and IDE applications |
| Flex Studies | Demonstration of test system insensitivity to environmental and usage variations under stress conditions [23] | Particularly important for waived tests and point-of-care devices |
| Clinical Performance Studies | Studies designed to demonstrate insignificant risk of erroneous results in hands of intended users [23] | Required for all IVDs; design varies based on intended use and complexity |
Table 4: Key Research Reagent Solutions and Regulatory Resources
| Resource | Function/Purpose | Application in IVD Risk Assessment |
|---|---|---|
| Q-Submission Program | Formal process for obtaining FDA feedback on regulatory questions [21] [3] | Obtain formal device risk determination from FDA prior to study initiation [19] |
| Pre-Submission Meeting | Forum for sponsor and FDA to discuss proposed study designs [21] [23] | Align on appropriate designs for analytical validation studies and risk assessment [3] |
| ISO 20916:2019 | International standard for clinical performance studies using human specimens [22] [20] | Guidance on planning/conducting IVD clinical performance studies, including interventional designs [20] |
| CLIA Waiver Decision Summaries | Publicly available FDA reviews of successful waiver applications [24] | Understand evidence needed to demonstrate simple, low-risk device characteristics [24] |
| 21 CFR 812 | Investigational Device Exemption regulations [19] [20] | Defines boundaries for researching investigational devices in interstate commerce [20] |
Determining significant versus nonsignificant risk for IVDs is a critical, study-specific process that demands careful evaluation of sampling procedures and potential consequences of erroneous results. The regulatory pathway—and ultimately the timeline to market—depends heavily on this initial risk classification. As IVD technologies evolve and play increasingly prominent roles in therapeutic development, particularly in personalized medicine approaches, understanding these risk assessment principles becomes ever more essential for researchers, scientists, and drug development professionals. By systematically addressing both procedural risks and result impact concerns, and by engaging early with regulatory bodies through the available mechanisms, sponsors can navigate this complex landscape more efficiently while maintaining focus on patient safety.
Executing IHC Assay Validation: A Step-by-Step Protocol from Optimization to Go-Live
Within the rigorous framework of Clinical Laboratory Improvement Amendments (CLIA) research, the pre-validation investigation represents a critical, strategic phase that precedes formal analytical validation. This stage determines an assay's potential for success by systematically evaluating its foundational requirements: clinical utility, market demand, and necessary resources. For researchers and drug development professionals, a robust pre-validation assessment de-risks the subsequent, resource-intensive analytical validation process, which is mandated by CLIA regulations for any test used in patient diagnosis, treatment, or prevention [1] [3]. The 2024 update to the College of American Pathologists (CAP) guidelines emphasizes that while laboratories are not legally bound to follow these specific recommendations, adopting them is a best practice that significantly enhances the quality and safety of clinically important immunohistochemistry (IHC) assays [1]. This guide objectively compares methodologies for conducting this essential preliminary investigation, providing a data-driven foundation for project planning and go/no-go decisions in assay development.
Quantifying Clinical Utility: Methodologies and Comparative Data
Clinical utility is defined as a test's ability to influence clinical decision-making and improve patient outcomes or healthcare efficiency [25]. Establishing this utility is a prerequisite for securing coverage and reimbursement from payers [26]. The following section compares the primary methodologies used to generate evidence of clinical utility.
Comparative Analysis of Clinical Utility Assessment Methods
Table 1: Comparison of Methods for Assessing Clinical Utility
| Method | Key Feature | Best Use Case | Relative Cost & Timeline | Key Strength | Primary Limitation |
|---|---|---|---|---|---|
| Randomized Controlled Trial (RCT) with Virtual Patients [26] | Randomizes physicians to control/intervention arms; uses virtual patient vignettes. | Demonstrating change in physician behavior and diagnostic/treatment planning. | Lower cost; Shorter timeline (months). | Cost-effective; Measures proximal behavioral change. | Does not directly measure long-term patient outcomes. |
| Traditional Patient-Level RCT [25] [26] | The gold standard; randomizes patients to testing strategies. | Providing the highest level of evidence for regulatory and payer submissions. | Very high cost; Long timeline (years). | Directly measures impact on patient outcomes. | Prohibitively expensive and slow for many diagnostic companies. |
| Systematic Review [25] | Summarizes and pools data from existing published studies. | Early-stage assessment of a test's potential and known drawbacks. | Low cost; Variable timeline. | Comprehensive use of existing evidence. | Limited by the quality and scope of existing literature. |
| Decision Analysis [25] | Uses mathematical models to compare outcomes of different diagnostic strategies. | Informing trial design and estimating value when clinical data is sparse. | Moderate cost; Short timeline. | Models optimal use in clinical practice. | Relies on assumptions which may not hold true. |
| Expert Opinion [25] | Leverages the experience and knowledge of healthcare providers. | Gathering preliminary, real-world insights on test applicability. | Low cost; Short timeline. | Provides practical, clinical context. | Subjective and not considered high-level evidence. |
Experimental Protocol: Virtual Patient Randomized Controlled Trial
The virtual patient RCT is an emerging and efficient method for generating high-quality evidence of clinical utility. The detailed protocol, as implemented in multiple diagnostic studies, is as follows [26]:
- Physician Recruitment and Randomization: A nationally representative sample of board-certified physicians is recruited. Eligible physicians must have no prior experience with the new test. Participants are formally consented and then randomized into a control arm and one or more intervention arms.
- Baseline Assessment (Round 1): All physicians, in both control and intervention arms, care for an initial set of three virtual patient vignettes, known as Clinical Performance and Value (CPV) vignettes. These vignettes are developed by clinical experts to represent the intended use population and contain explicit, evidence-based scoring criteria (typically 40-66 criteria per case) across domains of care: history, physical exam, workup, and diagnosis plus treatment (DxTx).
- Intervention: In the interval between assessment rounds, physicians in the intervention arm receive educational materials about the new diagnostic test. In some study designs, a second intervention arm may be added that not only receives education but is also automatically provided with the test results for their patients in the second round.
- Post-Intervention Assessment (Round 2): All physicians care for a second set of three virtual patients. Intervention physicians have the option (or are required) to order the new test.
- Analysis: The primary outcomes are the changes in overall CPV score and, more specifically, the DxTx domain score between Rounds 1 and 2. A difference-in-difference analysis using multivariate linear regression is employed to compare the improvement in the intervention arm(s) versus the control arm. The study is typically powered to detect a clinically meaningful 3-5% change in CPV scores.
The workflow for this experimental design is standardized and can be visualized as follows:
Navigating the Validation and Regulatory Landscape
A successful pre-validation investigation must align with the regulatory pathway the assay will ultimately follow. The requirements for a laboratory-developed test under CLIA differ from those for a commercially distributed in vitro diagnostic (IVD) kit [3].
Comparative Analysis of Validation Tiers and Regulatory Pathways
Table 2: Comparison of Validation Tiers and Regulatory Pathways for IHC Assays
| Aspect | CLIA Laboratory-Developed Test [1] [3] | FDA-Cleared IVD Kit (US) [3] | CE-Marked IVD (EU) [3] |
|---|---|---|---|
| Governing Body | CMS & CAP (for accredited labs) | FDA (Center for Devices and Radiological Health) | Notified Body (under IVDR) |
| Primary Focus | Analytical validity within a single lab. | Analytical and clinical validity for broad, commercial use. | Analytical and clinical validity under EU risk classification. |
| Key Validation Guidance | CAP "Principles of Analytic Validation" (e.g., 90% concordance for predictive markers) [1]. | CLSI guidelines; Pre-submission meetings with FDA recommended. | IVDR; ISO 13485 (QMS); ISO 14971 (Risk Management). |
| Typical Sample Size for Initial Validation | Varies; e.g., 10 positive & 10 negative for alternative fixatives [1]. | Defined by CLSI guidelines; typically larger, multi-site studies. | Defined by IVDR and harmonized standards; similar to FDA. |
| Modification Process ("Verification") | Simplified verification for same antibody clone (e.g., 2 positive & 2 negative cases) [5]. | Often requires a new submission or supplemental data. | Requires technical documentation and assessment by Notified Body. |
| Risk Assessment for Clinical Trials | SRD (Study Risk Determination) or IRB assessment [3]. | IDE (Investigational Device Exemption) often required for significant risk. | Annex XIV submission to national competent authority [3]. |
The Pre-Validation Workflow: From Concept to Viability Assessment
Integrating the assessments of clinical utility, demand, and resources into a single, coherent pre-validation investigation is crucial. The following workflow provides a logical pathway for researchers to systematically evaluate an IHC assay's potential before committing to formal validation.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are critical for conducting robust IHC pre-validation and validation studies. Their consistent quality is foundational to generating reliable data.
Table 3: Key Research Reagent Solutions for IHC Assay Development
| Reagent / Material | Critical Function | Pre-Validation & Validation Considerations |
|---|---|---|
| Primary Antibodies | Binds specifically to the target antigen of interest. | Clone specificity is paramount. Switching vendors for the same clone requires verification (e.g., 2 positive & 2 negative cases) [5]. |
| Antigen Retrieval Buffers | Unmasks hidden epitopes altered by tissue fixation. | pH, buffer composition, and retrieval method (e.g., heat platform) are critical variables. Changing the method requires extensive verification [5]. |
| Detection Systems | Visualizes the antibody-antigen binding. | Sensitivity and signal-to-noise ratio must be optimized and consistent. Changing the detection system triggers a full verification [5]. |
| Control Tissue Sections | Serves as positive and negative controls for assay performance. | Must include tissues with varying expression levels and known negatives. Sourcing a sufficient number of well-characterized controls is a major challenge [1] [5]. |
| Cell Lines | Used as calibrators or internal controls. | Cell lines with known protein expression levels provide a stringent comparator for validation study design [1]. |
A comprehensive pre-validation investigation is an indispensable strategic exercise in IHC assay development. By objectively comparing and implementing modern methodologies like virtual patient RCTs to assess clinical utility, and by clearly understanding the resource commitments for different regulatory pathways, researchers and drug developers can make data-driven decisions. This rigorous approach ensures that only the most promising assays, with a high probability of clinical adoption and commercial success, advance into the costly and formal analytical validation phase required by CLIA and other regulatory bodies.
Immunohistochemistry (IHC) serves as a cornerstone technique in both research and diagnostic laboratories, playing a vital role in identifying biomarkers within tissue samples [3]. The reliability of IHC data, however, is critically dependent on the selection and validation of primary antibodies, with studies indicating that approximately 49% of commercially available antibodies fail validation procedures [27]. This high failure rate has significant scientific and financial implications, contributing to an estimated $800 million wasted annually on poorly performing antibodies and approximately $350 million lost in biomedical research due to irreproducible results [27]. Within clinical laboratories operating under Clinical Laboratory Improvement Amendments (CLIA) regulations, demonstrating analytic validity for IHC assays is not merely best practice but a fundamental requirement for accreditation and patient testing [1] [28].
The College of American Pathologists (CAP) emphasizes that validation ensures an IHC assay is reliable and reproducible for biomarker detection in clinical settings [1] [3]. The level of validation required correlates directly with the assay's intended purpose, with tests informing patient treatment decisions necessitating more robust validation than those designed for research purposes alone [3]. This guide provides a comprehensive framework for antibody and clone selection, leveraging established quality resources and vendor data to meet the exacting standards required for CLIA-compliant IHC assay validation.
Proficiency Testing and External Quality Assessment
External quality assessment (EQA) programs provide invaluable, real-world data on antibody performance across multiple laboratories and testing conditions. NordiQC (Nordic Immunohistochemical Quality Control) represents a premier EQA resource that aims to "promote the quality of immunohistochemistry and expand its clinical use by arranging schemes for immunohistochemical proficiency testing" [29]. Through its proficiency testing schemes, NordiQC provides participants with performance feedback and publishes recommended protocols, tissue controls, and technical parameter descriptions that laboratories can consult when selecting and validating antibodies [29]. The organization maintains strict independence from commercial interests, ensuring unbiased evaluation data [29].
Antibody Search Engines and Comparison Tools
Several specialized search engines facilitate the initial identification of available antibody clones targeting specific antigens:
- Biocompare, SelectScience, and NCBI antibody search portals allow researchers to find and compare antibodies from multiple vendors simultaneously, saving valuable time compared to visiting individual vendor websites [27].
- BD Biosciences' Clone Comparison Tool enables systematic comparison of antibody clones against the same antigen, presenting scientific details, qualified applications, and available formats in an easy-to-read table format [30].
- Human Cell Differentiation Molecules (HCDM) database provides information on clones characterized through international workshops, detailing which antibodies have been independently tested for specific CD markers [31].
Vendor-Supplied Validation Data
Reputable antibody vendors provide varying levels of validation data, though the completeness and quality of this information must be critically evaluated. When assessing vendor data, laboratories should look for:
- Complete, uncropped western blot images with specified protein loading amounts [27]
- Validation using multiple biologically relevant sample types or tissues [27]
- Demonstration of performance under fixation conditions matching the laboratory's intended use [1]
- Clear specification of the antibody clone and species reactivity [30] [27]
- Data generated using appropriate positive and negative controls [27]
Experimental Design for Antibody Clone Comparison
Establishing Comparison Criteria
When comparing antibody clones for the same target, laboratories should establish standardized evaluation criteria prior to testing. The following table outlines essential parameters for systematic clone comparison:
Table 1: Key Parameters for Antibody Clone Comparison
| Parameter | Assessment Method | Optimal Result |
|---|---|---|
| Specificity | Western blot with relevant cell lysates; IHC with knockout/knockdown controls | Single band at expected molecular weight; absence of staining in negative controls |
| Sensitivity | Titration series on known positive samples with expected antigen expression levels | Detect antigen at biologically relevant concentrations with minimal background |
| Optimal Dilution | Chessboard titration using a range of antibody concentrations | Highest dilution providing strong specific signal with minimal background |
| Inter-lot Variability | Parallel testing of different manufacturing lots | Consistent performance across lots |
| Platform Compatibility | Testing on different automated IHC platforms | Robust performance across platforms with minimal protocol adjustments |
| Fixation Compatibility | Testing on tissues fixed with different fixatives and fixation times | Consistent performance with intended fixation protocol |
Stepwise Validation Protocol
The CAP guidelines outline a structured approach for analytic validation of IHC assays [1] [28]. The following workflow provides a detailed protocol for comparing antibody clones during assay validation:
Figure 1: Systematic workflow for comparing antibody clones during IHC assay validation. The process begins with clear definition of assay requirements and proceeds through iterative testing phases to identify the optimal reagent.
Define Intended Use and Validation Requirements: Clearly establish whether the assay will be used for predictive, prognostic, or diagnostic purposes, as this determines the stringency of validation needed [3]. For predictive markers, the 2024 CAP guideline update harmonizes concordance requirements to 90% for all IHC assays [1].
Identify Available Clones and Resources: Utilize search engines and comparison tools to identify all commercially available clones against the target antigen [30] [27]. Consult NordiQC and published literature for performance data on specific clones.
Acquire Candidate Clones and Materials: Select 2-3 top candidate clones based on available data. Purchase sufficient quantities of each clone from vendors who provide comprehensive technical support [27].
Perform Specificity Testing:
- Test each clone on cell lines or tissues with known expression of the target antigen, along with appropriate negative controls [27].
- For well-characterized targets, use siRNA knockdown or CRISPR knockout controls to confirm specificity [27].
- Pre-absorb antibodies with blocking peptides where available to demonstrate epitope specificity.
Determine Sensitivity and Optimal Dilution:
- Perform chessboard titrations with each clone across a range of concentrations (e.g., 1:50 to 1:2000) using known positive tissues [27].
- Identify the optimal working dilution as the highest dilution that provides strong specific signal with minimal background.
- Compare sensitivity by testing serial dilutions on tissues with low antigen expression levels.
Assess Concordance with Reference Methods:
Evaluate Platform and Fixation Compatibility:
Select Optimal Clone and Document Results: Choose the clone demonstrating the best combination of specificity, sensitivity, and reliability. Comprehensively document all validation data for regulatory compliance [1] [28].
Regulatory Considerations for CLIA Compliance
Validation Requirements for Different Assay Types
CLIA regulations apply broadly to all laboratory tests but do not specify how to satisfy each performance study requirement [3]. The CAP guidelines provide evidence-based recommendations for meeting CLIA standards through proper validation design. The following table summarizes key validation requirements:
Table 2: CLIA Validation Requirements for IHC Assays Based on CAP Guidelines
| Assay Type | Minimum Case Requirements | Concordance Standards | Special Considerations |
|---|---|---|---|
| Predictive Markers (ER, PR, HER2, PD-L1) | Sufficient to establish 90% concordance | ≥90% with reference method | Each scoring system combination requires separate validation [1] |
| Non-predictive Markers | Laboratory-defined based on intended use | Laboratory-defined based on intended use | Comparator may include expected staining pattern or literature rates [1] |
| Cytology Specimens (alternative fixatives) | 10 positive and 10 negative cases | Comparable to FFPE performance | Required when fixatives differ from original validation [1] |
| FDA-cleared/Approved Assays | Manufacturer specifications | Manufacturer specifications | Explicit verification required per manufacturer claims [1] |
Documentation and Quality Management
Laboratories must maintain comprehensive documentation of all validation procedures and results. Survey data demonstrates significant improvement in validation practices following dissemination of CAP guidelines, with 99% of laboratories now validating their predictive marker assays compared to 74.9% in 2010 [28]. A well-designed validation plan should evaluate both inter-instrument and inter-day variability by running validation sets on different instruments over multiple days using different personnel [1].
Essential Research Reagent Solutions
The following reagents and resources are essential for conducting thorough antibody validation studies:
Table 3: Essential Research Reagent Solutions for Antibody Validation
| Reagent/Resource | Function in Validation | Selection Criteria |
|---|---|---|
| Positive Control Tissues | Verify antibody sensitivity and establish expected staining patterns | Tissues with known antigen expression levels; available from commercial biorepositories |
| Negative Control Tissues | Demonstrate antibody specificity and establish background levels | Tissues known to lack target antigen; isogenic knockout controls ideal |
| Reference Antibodies | Serve as comparator for new clones | Well-characterized clones with published validation data |
| Cell Line Microarrays | Provide standardized substrate for initial clone screening | Include lines with varying expression levels of target antigen |
| Tissue Microarrays | Enable high-throughput screening on multiple tissue types | Contain both normal and pathological tissues from multiple cases |
| Blocking Peptides | Confirm antibody specificity through competitive inhibition | Should contain the exact epitope recognized by the antibody |
| Automated IHC Platform | Standardize staining conditions across comparisons | Compatible with laboratory workflow and throughput requirements |
Systematic antibody and clone selection represents a foundational element in developing robust, CLIA-compliant IHC assays. By leveraging quality assessment resources like NordiQC, utilizing comparison tools for clone identification, and implementing structured validation protocols, laboratories can significantly improve assay reliability and reproducibility. The harmonized validation requirements outlined in the 2024 CAP guideline update provide clear benchmarks for demonstrating analytic validity, particularly for predictive markers requiring 90% concordance with reference methods [1]. As the field continues to evolve with new biomarkers and technologies, maintaining rigorous selection and validation practices remains essential for generating clinically actionable data in both diagnostic and research settings.
For researchers and drug development professionals, the analytical validation of immunohistochemistry (IHC) assays represents a critical gateway for translating biomarkers into clinical practice. Within Clinical Laboratory Improvement Amendments (CLIA)-certified laboratories, validation requires precise determination of appropriate positive and negative cases in a validation cohort to ensure analytical accuracy, precision, and reliability. The fundamental challenge lies in selecting a cohort size and composition that statistically guarantees assay performance while satisfying regulatory requirements for companion diagnostics and clinical tests. Historically, guidelines from professional organizations like the College of American Pathologists (CAP) have provided framework recommendations, yet emerging quantitative technologies now demand more rigorous, fit-for-purpose validation approaches that blend traditional IHC standards with principles from quantitative ligand-binding assays [32].
The determination of positive and negative case numbers is not arbitrary; it stems from statistical considerations of diagnostic power, concordance targets, and the intended clinical application of the assay. For subjective, pathologist-read IHC assays, validation has traditionally followed case number recommendations based on achieving specific concordance levels. However, with the advent of quantitative immunohistochemistry (qIHC) platforms and computational pathology approaches, the validation paradigm is shifting toward more rigorous analytical standards that require demonstration of quantitative performance across the assay's dynamic range [33]. This evolution reflects the growing importance of tumor infiltrating lymphocyte (TIL) biomarkers and low-abundance protein quantification for immunotherapy and antibody-drug conjugate response prediction [34] [32].
Current Standards and Methodologies
Regulatory Requirements and Traditional Guidelines
CLIA establishes quality standards for laboratory testing, with updated 2025 proficiency testing acceptance limits reflecting increasingly stringent requirements for analytical performance [35]. Within this regulatory framework, validation cohort design follows two primary pathways depending on assay type and application:
- Predictive Biomarker Assays: Require 40-case validation with 20 positive and 20 negative cases, providing sufficient statistical power for 90% concordance targets [32]
- Non-Predictive Assays: Require 20 specimens (10 positive, 10 negative) to establish baseline performance characteristics [32]
These guidelines, initially published by Fitzgibbons et al. and adopted by CAP, form the foundation for CLIA laboratory inspections and validation protocols. The underlying statistical principle ensures that with 20 positive and 20 negative cases, a 90% observed concordance has a 95% confidence interval of approximately 77-97%, providing reasonable certainty about assay performance [32].
Emerging Quantitative Methodologies
Traditional IHC validation approaches are increasingly supplemented by quantitative methodologies that combine IHC with ligand-binding assay principles:
- High-Sensitivity HER2 (HS-HER2) Assays: Employ continuous, objective measurement scales (attomoles/mm²) rather than categorical scores, requiring validation across the analytical measurement range rather than binary classification [32]
- Quantitative IHC (qIHC): Utilizes amplification systems generating countable dots corresponding to individual protein molecules, requiring precision, linearity, and sensitivity assessments [33]
- Image Analysis Platforms: Provide quantitative scores for biomarker expression (e.g., percent positive cells or positive cells/mm²), requiring correlation with pathologist visual assessment [34]
These quantitative approaches necessitate expanded validation cohorts that include samples spanning the entire dynamic range of expression rather than simple positive/negative dichotomies.
Table 1: Validation Cohort Requirements by Assay Type and Application
| Assay Type | Total Cases | Positive Cases | Negative Cases | Key Considerations | Regulatory Reference |
|---|---|---|---|---|---|
| Predictive IHC | 40 | 20 | 20 | Must demonstrate 90% concordance | CAP/CLIA [32] |
| Non-Predictive IHC | 20 | 10 | 10 | Sufficient for baseline validation | CAP/CLIA [32] |
| Quantitative IHC | 40+ | Range of expressions | Range of expressions | Must span reportable range | Fit-for-purpose [33] |
| AI-Assisted Assays | 240+ | Minimum 30% | Minimum 30% | Based on statistical power calculations | CLIA [36] |
Experimental Protocols for Validation Cohort Construction
Traditional IHC Validation Protocol
For conventional IHC assays, the validation workflow follows a structured approach:
- Sample Selection: Identify archival formalin-fixed, paraffin-embedded (FFPE) tissue specimens with known biomarker status based on reference methods [32]
- Staining and Analysis: Perform IHC staining using standardized protocols (e.g., HercepTest for HER2) on an automated stainer [33]
- Pathologist Assessment: Employ multiple blinded pathologists to score specimens according to established criteria (e.g., HER2 0, 1+, 2+, 3+)
- Concordance Calculation: Compare results to reference method to determine positive/negative agreement
- Precision Evaluation: Assess inter-observer and intra-observer variability using subset of cases
This traditional approach served as the foundation for the 20/20 and 10/10 case validation models and remains relevant for subjective, pathologist-read assays [32].
Quantitative IHC Validation Protocol
For quantitative assays, validation incorporates additional analytical parameters:
- Calibration Standards: Create cell line microarrays with target protein concentrations determined by mass spectrometry to serve as quantitative references [32]
- Precision Studies: Evaluate repeatability and reproducibility across multiple operators, instruments, and days with coefficient of variation targets <10% [32] [33]
- Linearity and Dynamic Range: Demonstrate proportional response across the reportable range using serial dilutions or samples with varying expression levels
- Sensitivity Determination: Establish limit of detection (LOD) and limit of quantification (LOQ) using dilutional studies [33]
- Method Comparison: Evaluate correlation between quantitative measurements and traditional pathologist scores using regression analysis [34]
This expanded protocol requires approximately 40 cases but with expression levels spanning the analytical measurement range rather than simple positive/negative classification [32] [33].
Diagram 1: Validation cohort design workflow comparing traditional and quantitative approaches
Advanced Computational and AI-Assisted Validation
For artificial intelligence (AI)-assisted and computational pathology platforms, validation requirements expand further:
- Enhanced Sample Sizes: Method comparison studies may require 240+ samples based on statistical power calculations for both binary classification and quantitative correlation [36]
- Statistical Considerations: Sample size calculations based on minimum tolerable accuracy (e.g., 97.5%), alpha error (5%), and beta error (20% representing 80% power) [36]
- Precision Studies: Comprehensive evaluation across multiple operators, instruments, and days with specific acceptance criteria for repeatability and within-laboratory precision [36]
- Drift Detection: Implementation of continuous monitoring systems to detect changes in input data distribution or model performance over time [36]
This rigorous approach demonstrated 97.5% concordance with manual analysis in validated DNN-assisted flow cytometry applications [36].
Comparative Experimental Data and Case Studies
Traditional vs. Quantitative Validation Outcomes
Comparative studies demonstrate significant performance differences between traditional and quantitative validation approaches:
- Inter-observer Variability: Traditional HER2 IHC assessment shows 26-85% concordance between pathologists for distinguishing IHC 0 from IHC 1+ cases [32]
- Quantitative Improvement: qIHC methods demonstrate coefficients of variation <10% with lower limits of detection than both traditional IHC and ELISA methods [33]
- Dynamic Range: HS-HER2 assays identify 71% of IHC 0 cases as having measurable HER2 expression above the limit of quantification, revealing previously undetectable biomarker levels [32]
These findings highlight how quantitative approaches uncover limitations in traditional binary classification systems, particularly for low-abundance biomarkers.
Table 2: Performance Comparison of Validation Approaches for HER2 Assessment
| Performance Parameter | Traditional IHC | Quantitative IHC (qIHC) | High-Sensitivity HER2 |
|---|---|---|---|
| Inter-observer Concordance | 26-85% (IHC 0 vs 1+) [32] | Not applicable | >90% [32] |
| Coefficient of Variation | Not typically measured | <10% [33] | <10% [32] |
| Dynamic Range | 0-3+ (categorical) | 4+ orders of magnitude [33] | Continuous (attomoles/mm²) [32] |
| Limit of Detection | Subjective visual threshold | Superior to IHC and ELISA [33] | 94% cases above LOD [32] |
| Cases with Measurable HER2 | IHC 1+, 2+, 3+ only | Not reported | 71% of IHC 0 cases [32] |
Impact on Clinical Decision-Making
The rigor of validation cohort design directly impacts clinical utility:
- Therapeutic Selection: DESTINY-Breast06 trial showed IHC 2+ cases had significantly better response to T-DXd than IHC 1+ (hazard ratios 0.43 vs 0.74), emphasizing need for precise classification [32]
- Outcome Prediction: Quantitative assessment of tumor infiltrating lymphocytes (CD3, CD8, FOXP3) enables more accurate prognosis and immunotherapy response prediction [34]
- Treatment Eligibility: Up to 6% of cases fall below limit of detection with more sensitive assays, potentially affecting patient eligibility for targeted therapies [32]
These clinical implications underscore the critical importance of appropriate validation cohort design that matches the intended use of the assay.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for Validation Studies
| Reagent/Platform | Function in Validation | Application Example |
|---|---|---|
| FFPE Cell Line Pellet Arrays | Calibration standards with known protein concentration | HER2 quantification in attomoles/mm² [32] |
| iCARD qIHC Amplification System | Signal amplification for protein quantification | Dot counting for precise protein measurement [33] |
| Automated IHC Stainers | Standardized staining protocols | HercepTest implementation [33] |
| Quantitative Image Analysis Software | Objective measurement of biomarker expression | Scoring % positive cells or cells/mm² [34] |
| Deep Neural Network Platforms | Automated analysis of complex patterns | CLL MRD detection in flow cytometry [36] |
| CMA Calibration Standards | Quantitative reference for protein measurement | HER2 assay calibration [32] |
Diagram 2: Quantitative IHC workflow using amplification and dot counting for precise protein measurement
The determination of positive and negative case numbers in validation cohorts has evolved from simple fixed-number approaches to sophisticated, statistically-powered designs that reflect assay technology and clinical application. The traditional 20/20 case model for predictive biomarkers remains relevant for subjective IHC assays, but emerging quantitative technologies demand more comprehensive validation spanning analytical measurement ranges with 40+ cases. The most advanced computational approaches may require 240+ samples to establish both qualitative and quantitative performance with sufficient statistical power [36].
Future directions in validation cohort design include:
- Hybrid Validation Models: Combining traditional IHC case number recommendations with ligand-binding assay precision requirements [32]
- Continuous Monitoring: Implementing post-deployment performance tracking to detect data drift in AI-assisted platforms [36]
- Standardized Reference Materials: Developing universally accepted calibration standards for quantitative protein measurement in FFPE tissue [33]
- Fit-for-Purpose Approaches: Tailoring validation strategies to specific clinical contexts, from high-abundance predictive biomarkers to low-abundance response predictors
As IHC assays continue to evolve toward quantitative, objective measurement, the principles for determining validation cohort size and composition will increasingly emphasize statistical power, analytical precision, and demonstration of clinical utility across the full dynamic range of biomarker expression.
In the rigorous world of immunohistochemistry (IHC) assay validation, the choice of an appropriate comparator is not merely a technical step—it is a foundational decision that determines the accuracy, reliability, and regulatory acceptance of your assay. For researchers and drug development professionals navigating Clinical Laboratory Improvement Amendments (CLIA) requirements, selecting the right comparator directly impacts whether an assay is deemed valid for clinical decision-making. The 2024 CAP guideline update reaffirms that proper analytical validation ensures accuracy and reduces variation in IHC laboratory practices, with comparator selection serving as the cornerstone of this process [1]. A well-chosen comparator provides the evidence base needed to demonstrate that your IHC assay performs consistently and delivers clinically actionable results, thereby fulfilling both scientific and regulatory imperatives.
The Critical Role of Comparators in IHC Validation
A comparator in IHC validation serves as a reference point against which the performance of a new or modified assay is measured. This choice directly influences the validation of the assay's analytical performance characteristics, which is a fundamental requirement under CLIA regulations before any patient results can be issued [1] [3].
The College of American Pathologists (CAP) outlines that a comparator provides the basis for determining the performance characteristics of a new assay, especially since most IHC assays lack a perfect gold standard [1]. Confounding by indication poses a significant threat to validity when comparators are poorly matched, particularly in observational studies where treatment isn't randomized [37]. The principles of comparator selection extend beyond IHC to broader comparative effectiveness research, where choosing a clinically meaningful alternative within the same indication is considered the least biased approach [38].
The consequences of poor comparator selection include:
- Introduction of systematic bias that compromises assay reliability [37]
- Inaccurate concordance rates failing to meet the updated 90% minimum concordance requirement for predictive markers [1]
- Regulatory non-compliance risking citations from accrediting agencies [1]
- Compromised patient safety if clinical decisions are based on unvalidated assays [3]
Comparator Options for IHC Assays: Strategies and Applications
CAP guidelines provide a hierarchy of comparator options, ordered here from most to least stringent [1]:
Table 1: Comparator Options for IHC Assay Validation
| Comparator Type | Description | Best Use Cases | Strength of Evidence |
|---|---|---|---|
| Protein Calibrators | Cell lines with known protein quantities | Quantitative IHC, assay standardization | Highest |
| Non-IHC Method | Flow cytometry, FISH, other molecular methods | Predictive markers, confirmatory testing | High |
| External Laboratory | Testing same tissues in another lab with validated assay | Method transfer, verification | Medium-High |
| Prior Testing | Comparison with previously validated results in same lab | Assay modifications, reagent changes | Medium |
| Clinical Trial Lab | Comparison with laboratory used in clinical trials | Companion diagnostic development | Medium-High |
| Antigen Localization | Comparison with expected architectural patterns | Screening assays, initial validation | Medium |
| Published Rates | Comparison with percent positive in clinical literature | Rare targets, limited tissue availability | Low-Medium |
| Proficiency Testing | Formal graded challenges | Ongoing validation, quality control | Varies |
The selection among these options depends on the intended use of the assay, with predictive markers (e.g., PD-L1, HER2) requiring more stringent comparators than screening assays. The CAP guideline emphasizes that "laboratories should separately validate/verify each assay-scoring system combination" for predictive markers with distinct scoring systems [1].
Special Considerations for Different IHC Applications
Predictive IHC Markers
For predictive markers like PD-L1 and HER2, the 2024 CAP guideline update has harmonized validation requirements across all predictive markers, setting a uniform 90% concordance threshold for both positive and negative agreement [1]. This represents a significant standardization from previous guidelines which had variable requirements for different markers.
Cytology Specimens
For IHC performed on cytology specimens that use alternative fixatives different from formalin-fixed, paraffin-embedded (FFPE) tissues used in initial validation, the updated guidelines now require separate validations with a minimum of 10 positive and 10 negative cases [1]. This conditional recommendation addresses the variable sensitivity observed with different fixatives and imposes additional validation burdens that laboratories must incorporate into their planning.
Companion Diagnostic Development
When developing IHC assays as companion diagnostics, regulatory strategy must align with validation design. The FDA favors a modular pre-market approval (PMA) process, with each module reviewed independently [3]. Comparators for these high-stakes assays must be selected with an understanding that they will undergo intense regulatory scrutiny, including potential Bioresearch Monitoring (BIMO) audits [3].
Experimental Design for Concordance Studies
Sample Size Considerations
The CAP guidelines provide specific sample size requirements for different validation scenarios [1]:
Table 2: Sample Size Requirements for IHC Assay Validation
| Validation Scenario | Minimum Positive Cases | Minimum Negative Cases | Total Minimum Cases |
|---|---|---|---|
| General IHC Validation | Not specified | Not specified | 20-60 |
| Alternative Fixatives | 10 | 10 | 20 |
| Predictive Markers | Sufficient to demonstrate 90% concordance | Sufficient to demonstrate 90% concordance | Laboratory determined |
Statistical Approaches for Concordance Analysis
Proper statistical analysis moves beyond simple correlation coefficients, which the literature clearly identifies as "unsuitable indicator[s] of the degree of agreement" [39]. Instead, researchers should employ:
- Bland-Altman diagrams to visualize differences between measurements and identify systematic bias [39]
- Cohen's kappa for categorical agreement assessment, particularly for nominal or ordinal ratings [39]
- Concordance correlation coefficients that measure agreement rather than mere correlation
The Bland-Altman plot is particularly valuable as it displays the limits of agreement (±1.96 standard deviations of the differences between methods), allowing researchers to assess whether the magnitude of disagreement is clinically acceptable [39].
Workflow for Comparator Selection and Validation
The following diagram illustrates the systematic process for selecting and validating an appropriate comparator for IHC assays:
Essential Research Reagents and Materials
Successful IHC validation requires carefully selected reagents and materials that ensure reproducibility and compliance. The following table outlines key solutions and their functions in comparator studies:
Table 3: Essential Research Reagent Solutions for IHC Comparator Studies
| Reagent/Material | Function in Validation | Critical Quality Metrics |
|---|---|---|
| Well-Characterized Cell Lines | Serve as protein calibrators with known antigen expression | Documented expression levels, stability data |
| Control Tissue Microarrays | Provide positive/negative controls for multiple markers | Tissue preservation quality, antigen integrity |
| Reference Primary Antibodies | Establish benchmark for specific antigen detection | Specificity, sensitivity, lot-to-lot consistency |
| Detection Systems | Amplify signal while minimizing background | Signal-to-noise ratio, linearity, reproducibility |
| Automated Staining Platforms | Standardize technical variables across comparisons | Run-to-run precision, temperature uniformity |
| Image Analysis Software | Enable quantitative assessment and minimize rater bias | Algorithm accuracy, precision, reproducibility |
Regulatory and Compliance Considerations
Under CLIA regulations, laboratories must validate the performance characteristics of all assays before issuing patient results, but CLIA does not specify how to satisfy each performance study [3]. The CAP guidelines fill this gap by providing specific recommendations, though laboratories should note that "some recommendations may not align with the 2023 Laboratory Accreditation Program (LAP) Checklist" [1].
For global development, manufacturers must plan parallel validation strategies that meet both U.S. CLIA standards and EU In Vitro Diagnostic Regulation (IVDR) requirements [3]. This often involves designing studies that comply with both CLSI guidelines and ISO standards, particularly ISO 13485 for quality management systems [3].
The risk classification of an IHC assay determines the regulatory pathway. When an assay is used for "prospective stratification or clinical decision-making," manufacturers must perform a study risk determination to evaluate if an investigational device exemption (IDE) is required [3].
Choosing the right comparator for IHC assay concordance is both a scientific and strategic imperative that extends beyond mere regulatory compliance. The updated CAP guidelines provide a structured framework for comparator selection, emphasizing methodical validation approaches tailored to the assay's intended use and clinical context. As the field evolves with new biomarkers and technologies, the principles of rigorous comparator selection—rooted in evidence-based methodology and clear documentation—will continue to underpin reliable IHC testing. For researchers and drug development professionals, mastering these principles ensures that IHC assays not only meet CLIA requirements but also deliver the precision medicine community's ultimate goal: accurate, actionable data that advances patient care.
Immunohistochemistry (IHC) stands as a cornerstone technique in diagnostic pathology and therapeutic decision-making, particularly in oncology. The analytical validation of these assays ensures their reliability in detecting specific biomarkers that guide critical treatment decisions. Within this framework, establishing performance thresholds is not merely an academic exercise but a fundamental requirement for clinical implementation. The 90% overall concordance threshold has emerged as a widely adopted standard for demonstrating adequate assay performance before clinical use [1] [6]. This comparison guide examines the evidence base, application protocols, and strategic implementation of this critical benchmark across different IHC validation scenarios, providing researchers and drug development professionals with a structured approach to analytical validation.
Establishing the 90% Concordance Benchmark
Evidence Base and Guideline Evolution
The 90% overall concordance standard represents a harmonization of validation requirements across various biomarker types. The 2024 update to the College of American Pathologists (CAP) "Principles of Analytic Validation of Immunohistochemical Assays" specifically affirmed this threshold for all IHC assays, including predictive markers like HER2, ER, PR, and PD-L1 [1] [6]. This update replaced previous recommendations that had suggested varying concordance requirements for different biomarkers, creating a unified standard that simplifies validation design while ensuring analytical rigor.
Survey data demonstrates significant improvement in laboratory compliance with validation requirements following the dissemination of evidence-based guidelines. Between 2010 and 2015, the percentage of laboratories that validated their most recently introduced predictive marker assay increased from 74.9% to 99% [28]. This substantial improvement highlights the positive impact of standardized validation thresholds on laboratory practice.
Comparative Concordance Requirements Across Validation Types
Table 1: Concordance Requirements for Different IHC Validation Scenarios
| Validation Scenario | Minimum Case Requirements | Concordance Threshold | Key Considerations |
|---|---|---|---|
| Predictive Markers (Initial validation) | 20 positive and 20 negative cases [15] | 90% overall concordance [1] | Includes biomarkers with therapeutic implications |
| Non-Predictive Markers (Initial validation) | 10 positive and 10 negative cases [15] | 90% overall concordance [1] | Diagnostic and prognostic markers without direct therapeutic implications |
| Cytology Specimens (Alternative fixatives) | 10 positive and 10 negative cases [1] | 90% overall concordance [1] | Required when fixatives differ from original FFPE validation |
| Modified FDA-Cleared Assays (Verification) | 2 known positive and 2 known negative cases [5] | Comparable performance to existing assay | Applies to changes in antibody vendor (same clone), dilution, or incubation times |
| Laboratory-Developed Tests (LDTs) | 20 positive and 20 negative cases for predictive markers [15] | 90% overall concordance [1] | Required for non-FDA-approved assays |
Experimental Protocols for Concordance Assessment
Core Validation Methodology
The fundamental approach to establishing concordance involves a structured comparison between the new IHC assay and predetermined expected results. The CAP guidelines outline a hierarchy of comparators, presented below from most to least stringent [1]:
- Cell line calibrators with known protein quantities
- Non-immunohistochemical methods (e.g., flow cytometry, FISH)
- Testing in another laboratory using a validated assay
- Prior testing of the same tissues with a validated assay in the same laboratory
- Archival results from clinical trial laboratories
- Expected architectural and subcellular localization of the antigen
- Published positive rates from clinical trials
- Formal proficiency testing challenges
The validation process typically follows three key phases [15]:
- Optimization: Selecting appropriate antibody clones and establishing optimal staining protocols through iterative testing
- Validation/Verification: Testing the predetermined number of known positive and negative cases to establish performance characteristics
- Ongoing Monitoring: Implementing quality control procedures, lot-to-lot comparisons, and proficiency testing to ensure sustained performance
Specialized Validation Protocols
For predictive markers with distinct scoring systems (e.g., PD-L1, HER2 in different tumor sites), the updated CAP guidelines stipulate that laboratories must separately validate each assay-scoring system combination [1]. This requirement acknowledges that the same antibody may perform differently when applied with different scoring criteria across tumor types.
For cytology specimens fixed differently from standard formalin-fixed, paraffin-embedded (FFPE) tissues, separate validation is necessary due to variable sensitivity observed with alternative fixatives [1]. The literature has demonstrated significant staining variations in cytology specimens, justifying this additional validation requirement despite the added burden to laboratories.
Analysis of Discordant Results and Troubleshooting
When validation studies fail to achieve the 90% concordance threshold, systematic investigation is required. The pattern of discordance provides crucial diagnostic information about assay performance [15]:
- False negatives with concordant negatives: Suggests inadequate assay sensitivity
- False positives with concordant positives: Indicates specificity problems
- Discordance in both cohorts: Suggests fundamental issues with assay design or validation case selection
For algorithm-based IHC assessment, recent advances in artificial intelligence have demonstrated potential for maintaining concordance standards. A 2024 study developing deep learning-based IHC biomarker prediction models reported AUCs ranging from 0.90 to 0.96, with accuracies between 83.04% and 90.81% across five different biomarkers [40]. The consistency rates between AI-generated IHC and conventional IHC were high for Desmin, Pan-CK, and P40 (96.67-100%) though more moderate for P53 (70.00%) [40].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for IHC Validation Studies
| Reagent/Material | Function in Validation | Application Notes |
|---|---|---|
| FFPE Tissue Sections | Primary validation material | Should represent spectrum of expression levels [15] |
| Cytology Specimens | Alternative fixation validation | Required when lab offers IHC on non-FFPE specimens [1] |
| Cell Line Calibrators | Stringent comparator | Contain known protein quantities for quantitative assessment [1] |
| Multi-tissue Blocks | Efficient validation | Enables testing multiple tissues while conserving reagents [15] |
| Reference Standards | Concordance comparator | Previously validated assays or established methodologies [1] |
| Automated Stainers | Platform consistency | Must be validated for each platform used in laboratory [15] |
Regulatory Considerations and Strategic Implementation
Compliance Framework
The 90% concordance threshold operates within a broader regulatory context that varies by jurisdiction. In the United States, CLIA regulations establish the foundation for laboratory testing requirements, while CAP guidelines provide specific implementation details [3]. The FDA recognizes distinct pathways for IHC assays, with different evidence requirements for 510(k) clearance versus Premarket Approval (PMA) [41].
Internationally, significant differences exist between regulatory frameworks. The European Union's In Vitro Diagnostic Regulation (IVDR) classifies companion diagnostics uniformly as Class C devices, while the US system may classify them as Class II or III [3]. For global assay development, parallel validation strategies that address both CLIA and IVDR requirements can streamline regulatory approval across jurisdictions.
Strategic Implementation Recommendations
Successful implementation of the 90% concordance threshold requires both technical and strategic considerations:
- Validation Design: Include a range of expression levels in validation cohorts, not just strongly positive and negative cases [15]
- Rare Antigens: For low-frequency antigens, consider collaborative approaches with other laboratories or use of cell lines when sufficient positive cases are unavailable [15]
- Documentation: Maintain thorough records of validation procedures, results, and director approval, as lack of documentation may result in citations by accrediting agencies [1]
- Ongoing Verification: Implement regular lot-to-lot comparison and proficiency testing to ensure maintained concordance after initial validation [15]
The 90% overall concordance threshold represents an evidence-based standard for IHC assay validation that has demonstrated significant improvement in laboratory practices since its formal adoption. While this benchmark provides a clear target for analytical performance, its implementation requires careful consideration of assay type, specimen characteristics, and regulatory context. The continued evolution of IHC technologies, including digital pathology and AI-assisted interpretation, may refine these standards further, but the fundamental requirement for demonstrated analytical validity remains constant. By applying the structured approaches outlined in this guide, researchers and drug development professionals can ensure their IHC assays meet the rigorous standards required for both diagnostic accuracy and therapeutic decision-making.
Finalizing an immunohistochemistry (IHC) assay for clinical use represents the critical transition from development to diagnostic implementation. This phase demands rigorous documentation, formal director approval, and systematic clinical integration to meet regulatory requirements and ensure patient safety. Under the Clinical Laboratory Improvement Amendments (CLIA), laboratories must establish and demonstrate the analytical validity of their tests before reporting patient results [3] [2]. This process applies to both laboratory-developed tests (LDTs), which require full validation, and FDA-cleared/approved assays, which require verification [15]. The complexity of this finalization process has evolved significantly, with evidence-based guidelines from the College of American Pathologists (CAP) substantially improving laboratory validation practices and compliance [28]. This guide compares the requirements for different assay types and provides the experimental frameworks necessary for successful implementation.
Regulatory Requirements: Documentation and Approval Standards
Adherence to established regulatory and accreditation standards is fundamental to assay finalization. The following table summarizes the core documentation and approval requirements across different regulatory frameworks.
Table 1: Documentation and Approval Requirements for IHC Assay Finalization
| Component | CLIA Requirements | CAP Guidelines (2024 Update) | FDA Considerations |
|---|---|---|---|
| Director Approval | Mandated before clinical use; Laboratory Director ultimately responsible for test validity [42]. | Affirmation of validation/verification and approval for clinical use required [15] [2]. | For IVDs, Director ensures compliance with approved labeling; for LDTs, ensures robust validation. |
| Validation Documentation | Must establish and document performance specifications for accuracy, precision, and reportable range [3] [42]. | Detailed records of validation design, cases, results, and concordance calculations required [1] [2]. | More stringent requirements for Premarket Approval (PMA); exceeds CLIA standards [3]. |
| Test Complexity | Standards apply broadly based on test type, not complexity level [42]. | Adherence to specific validation protocols for predictive vs. non-predictive markers required [2]. | Risk classification (Class II/III in US, Class C in EU) influences submission data requirements [3]. |
| Proficiency Testing (PT) | Ongoing participation required; must meet CLIA acceptance criteria [35]. | Enroll in PT or alternative assessments; monitor for trends indicating assay "drift" [15]. | PT success is a key component of ongoing quality assurance for maintaining approval. |
The following workflow outlines the key decision points and procedural steps from validation to clinical implementation, integrating the requirements detailed in Table 1.
Experimental Protocols for Validation and Verification
The nature and extent of analytical validation are determined by the assay type and its intended clinical use. The following experimental protocols are based on the 2024 CAP Guideline update [1] [2].
Core Validation Protocol for Laboratory-Developed Tests (LDTs)
For LDTs and modified FDA-approved assays, a full validation is required. The experimental design must confirm the assay's performance characteristics before clinical use [2].
Step 1: Case Selection and Cohort Building
- Predictive Markers (e.g., PD-L1, HER2): A minimum of 20 known positive and 20 known negative cases is required. The positive cohort should include a range of expression levels (high and low expressors) to adequately challenge the assay's dynamic range [2].
- Non-Predictive Markers: A minimum of 10 known positive and 10 known negative cases is required [2].
- Rare Antigens: If the recommended minimum number of cases is not feasible, the Laboratory Director must document a scientifically sound rationale for using fewer cases [15] [2].
- Tissue Quality: Validation tissues must be processed using the same fixative (e.g., 10% NBF), processing methods, and specimen types (e.g., FFPE) as future clinical cases [43] [2].
Step 2: Establishing a Comparator Method A robust comparator is essential for determining concordance. CAP guidelines list several acceptable methods, ordered here from most to least stringent [1]:
- Comparison to IHC results from protein-calibrated cell lines.
- Comparison with a non-IHC method (e.g., flow cytometry, FISH).
- Comparison with results from a validated assay in another laboratory.
- Comparison with prior validated test results on the same tissues in the same lab.
- Comparison with expected antigen localization patterns or published positive rates.
Step 3: Staining, Interpretation, and Concordance Calculation
- Execute the optimized IHC protocol on all validation cases [44].
- Interpret slides blinded to the expected results, if possible.
- Calculate the overall concordance between the new assay and the comparator. The CAP guideline requires a minimum of 90% overall concordance for the assay to be considered validated [1] [6] [2].
- Investigate any discordant results to determine if the issue is with sensitivity (false negatives) or specificity (false positives) [15].
Verification Protocol for Unmodified FDA-Cleared/Approved Assays
For unmodified FDA-cleared/approved assays, the process is one of verification, confirming the assay performs as specified in the manufacturer's instructions [15].
- Primary Protocol: Follow the specific verification instructions provided in the manufacturer's package insert.
- Secondary Protocol: If the package insert lacks specific instructions, the laboratory should default to the more rigorous validation standard, typically using a minimum of 20 positive and 20 negative cases for predictive markers [2].
- Documentation: The Laboratory Director must review and approve the verification data, confirming the assay's performance meets the manufacturer's claims before clinical implementation.
Performance Data Comparison: Validation Benchmarks
The following table synthesizes key quantitative requirements from current guidelines, providing a clear reference for establishing validation performance benchmarks.
Table 2: Analytical Validation Performance Benchmarks and Requirements
| Validation Parameter | Predictive Markers (e.g., HER2, PD-L1) | Non-Predictive Markers | Cytology Specimens (Alternative Fixative) |
|---|---|---|---|
| Minimum Case Number | 20 positive, 20 negative [2] | 10 positive, 10 negative [2] | 10 positive, 10 negative (recommended) [2] |
| Overall Concordance | ≥ 90% [1] [2] | ≥ 90% [1] [2] | ≥ 90% [1] |
| Revalidation Trigger | Change in antibody clone, detection system, or antigen retrieval method [2] | Change in antibody clone, detection system, or antigen retrieval method [2] | Required for each new fixation method [1] |
| Post-Implementation Monitoring | Track positive/negative rates; review all PT results [15] | Monitor for staining quality and expected morphological patterns [15] | Monitor for staining quality and expected morphological patterns [15] |
Survey data demonstrates the positive impact of standardized guidelines. Following the dissemination of the 2014 CAP guideline, the percentage of laboratories that validated their most recently introduced predictive marker assay jumped from 74.9% in 2010 to 99% in 2015. Furthermore, the number of laboratories with written validation procedures for predictive markers increased significantly from 45.9% to 73.8% in the same period [28].
The Scientist's Toolkit: Essential Reagents and Materials
A successful IHC clinical implementation relies on a foundation of consistent, high-quality reagents and materials.
Table 3: Essential Research Reagent Solutions for IHC Validation
| Reagent/Material | Critical Function | Implementation Considerations |
|---|---|---|
| Primary Antibodies | Specific epitope binding for target detection. | Select clones with well-documented performance (e.g., via NordiQC). For FDA-approved assays, do not modify [15]. |
| Detection System | Amplifies signal for visualization. | Adhere to manufacturer's protocol. Changes require partial or full revalidation [2]. |
| Antigen Retrieval Buffers | Unmasks epitopes cross-linked by fixation. | pH (e.g., Citrate pH 6.0, EDTA pH 8.0) must be optimized and consistent [43] [44]. |
| Control Tissues | Monitors assay performance daily. | Should include known positive, weak positive, and negative tissues. On-slide controls are preferred [15]. |
| Cell Lines / Tissue Microarrays | Provides standardized material for validation. | Crucial for validating rare antigens and for building multi-tissue validation blocks [1] [15]. |
Troubleshooting and Quality Assurance
A systematic approach to troubleshooting is vital for maintaining assay performance post-implementation. The following pathway guides the investigation of common post-validation issues.
- Investigating Discordance: If validation yields unexpected results (e.g., <90% concordance), the IHC Medical Director must lead an investigation. Causes can include problems with assay sensitivity (false negatives), specificity (false positives), or issues with the validation cohort itself [15].
- Managing Reagent and Process Changes: Assay consistency is paramount. A new antibody lot requires testing with at least 1 known positive and 1 known negative tissue. Changes in antibody dilution, vendor (same clone), or incubation times require 2 positive and 2 negative tissues. A change in antibody clone, detection system, or antigen retrieval method necessitates a full revalidation [2].
- Ongoing Quality Assurance: Enroll in proficiency testing (PT) programs and carefully review all reports. Track positive and negative rates for predictive markers and compare them to established benchmarks. Encourage feedback from pathologists to identify cases where results differ from expectations [15].
IHC Assay Maintenance and Troubleshooting: Ensuring Ongoing Accuracy and Performance
Strategies for Verifying a Modified IHC Procedure or Antibody Switch
For researchers and drug development professionals, navigating the regulatory requirements for immunohistochemistry (IHC) assay changes represents a critical component of laboratory quality systems. Verification of modified IHC procedures ensures reliable, reproducible results while maintaining compliance with regulatory standards. The Clinical Laboratory Improvement Amendments (CLIA) establish the federal framework for all laboratory testing, mandating that laboratories establish and verify the performance characteristics of their assays [3]. Within this context, the College of American Pathologists (CAP) provides specific, evidence-based guidelines that laboratories often adopt to satisfy CLIA requirements through more detailed recommendations [5].
A fundamental distinction in regulatory terminology guides the extent of testing required: verification confirms that a modified procedure performs equivalently to an established validated assay, while validation establishes the performance characteristics of a completely new assay [5]. This distinction is crucial for efficiently allocating laboratory resources. When implementing procedural modifications, such as switching antibody vendors or changing incubation times, following structured verification protocols ensures analytical reliability while minimizing unnecessary repetition of extensive validation studies. This guide examines the specific strategies, experimental data, and regulatory considerations for verifying modified IHC procedures, providing a framework for researchers operating within CLIA-regulated environments.
Regulatory Framework and Verification Tiers
CLIA Requirements and CAP Guidelines
CLIA regulations provide the foundational requirements for laboratory testing but do not specify detailed procedures for IHC verification [5] [3]. The CAP guidelines operationalize these requirements by offering tiered recommendations based on the type and extent of the procedural modification. Laboratories accredited by CAP must comply with these standards, while non-accredited laboratories can use them as recognized best practices for satisfying CLIA's more general requirements [5]. The 2024 CAP guideline update harmonizes validation requirements across predictive markers and provides new guidance for cytology specimens and assays with distinct scoring systems [1].
A critical concept in the regulatory framework is the classification of assay risk based on intended use. IHC assays used for patient treatment decisions, such as predictive biomarkers, require more extensive validation and verification than those used for non-predictive purposes [3]. This risk-based approach directly influences verification strategies, with higher-risk modifications necessitating more rigorous assessment. Understanding this framework enables researchers to design appropriate verification protocols that satisfy both regulatory requirements and analytical quality standards.
Categorization of Procedural Modifications
The CAP guidelines classify procedural modifications into distinct tiers based on their potential impact on assay performance [5] [2]. The table below outlines these categories and their corresponding verification requirements:
Table: CAP Verification Requirements for IHC Procedure Modifications
| Modification Category | Examples of Changes | Minimum Verification Cases | Key Regulatory Reference |
|---|---|---|---|
| Minor Changes | Antibody dilution, antibody vendor (same clone), incubation or retrieval times (same method) | 2 known positive + 2 known negative cases | [5] [2] |
| Major Changes | Fixative type, antigen retrieval method (change in pH, different buffer, different heat platform), detection system, tissue processing equipment, automated testing platform, environmental conditions | "Sufficient number" of tissues to ensure consistent expected results (director determined) | [5] [2] |
| Critical Changes | Antibody clone change | Full revalidation (equivalent to initial analytic validation) | [2] |
| New Lot Verification | New antibody lot for existing validated assay | 1 known positive + 1 known negative tissue (control tissue with known positive and negative cells suffices) | [2] |
This tiered approach allows laboratories to match the verification intensity to the potential risk of the modification. Minor changes, such as switching to the same antibody clone from a different vendor, require only limited verification, while critical changes, such as altering the antibody clone itself, trigger full revalidation [2]. This risk-based framework ensures efficient resource allocation while maintaining assay quality and regulatory compliance.
Experimental Design for Verification Studies
Specimen Selection and Study Design
Appropriate specimen selection forms the foundation of reliable verification studies. For initial analytic validation of non-predictive laboratory-developed tests, CAP guidelines recommend testing a minimum of 10 positive and 10 negative tissues [2]. For predictive markers, this requirement increases to 20 positive and 20 negative tissues [1] [2]. The validation set should include both high and low expressors where appropriate and span the expected range of clinical results for markers reported using semiquantitative or numerical scoring systems [2].
For verification of modified procedures, the specimen requirements are reduced but must still represent biologically relevant challenges. The selected cases should demonstrate that the modified procedure maintains expected staining patterns across different expression levels. When verifying assays with distinct scoring systems—such as HER2 or PD-L1, which employ different criteria based on tumor site or type—laboratories must separately verify each assay-scoring system combination [1]. This ensures that the modification does not adversely affect the application of clinically relevant scoring criteria.
Comparative Analysis and Acceptance Criteria
The core methodology for verification studies involves comparative analysis between the established and modified procedures. For antibody vendor switches using the same clone, this entails testing the same set of specimens with both the existing and new antibodies under their respective optimal conditions [5]. The results are then compared to ensure the modified procedure produces equivalent or superior staining patterns, intensity, and specificity.
The CAP guideline recommends achieving at least 90% overall concordance between the modified assay and the comparator for initial validation [2]. This concordance threshold applies universally across all IHC assays in the updated guideline, harmonizing what were previously variable requirements for different markers [1]. The assessment should evaluate multiple parameters including staining intensity, cellular distribution patterns, and background staining. This comprehensive approach ensures that modifications do not adversely affect critical assay characteristics that could impact clinical or research interpretations.
Figure: IHC Procedure Modification Verification Workflow
Quantitative Comparison of Verification Strategies
Verification Requirements Across Modification Types
The extent of verification testing varies significantly based on the nature of the procedural change. The table below summarizes the key differences in verification scope and documentation requirements:
Table: Comparative Verification Requirements for IHC Modifications
| Verification Parameter | Minor Changes(Same clone vendor switch) | Major Changes(Detection system change) | Critical Changes(Antibody clone change) |
|---|---|---|---|
| Minimum Case Numbers | 2 positive + 2 negative | Director determined based on complexity | Full revalidation (e.g., 10-40 per initial validation) |
| Comparative Analysis | Side-by-side staining comparison | Extended comparison across expression range | Comprehensive performance characterization |
| Concordance Threshold | ≥90% overall concordance | ≥90% overall concordance | ≥90% overall concordance |
| Documentation Level | Modified procedure verification form | Extended validation report | Complete validation package |
| Director Approval | Required before implementation | Required before implementation | Required before implementation |
| Regulatory Basis | CAP Anatomic Pathology Checklist | CAP Analytic Validation Guidelines | CLIA requirements + CAP Guidelines |
For minor changes, the verification process focuses on confirming that the modification does not alter the essential staining characteristics of the assay [5]. The limited case number (2 positive + 2 negative) reflects the lower risk associated with these changes when the critical reagent (antibody clone) remains unchanged. For major changes, the laboratory director determines the appropriate number of cases based on the complexity of the modification and the clinical or research implications of inaccurate results [2]. This flexibility allows for risk-based resource allocation while ensuring thorough verification of potentially impactful modifications.
Experimental Data Supporting Verification Approaches
Research studies provide quantitative data supporting the verification strategies outlined in regulatory guidelines. One study comparing semi-automated quantification methods with traditional manual counting demonstrated strong correlation between methods (r = 0.9602, p < 0.0001 for collagen type II; r = 0.9044, p = 0.0001 for N-cadherin) with no significant differences (p = 0.783, p = 0.386) [45]. This level of agreement exceeds the 90% concordance threshold recommended by CAP guidelines and supports the use of standardized quantification approaches in verification protocols.
Additionally, studies implementing semi-automated analysis methods have shown improved inter-rater reliability, with intraclass correlation coefficients (ICC) for single raters reaching 0.853 [45]. This enhanced reproducibility is particularly valuable in verification studies, where objective assessment of staining patterns is essential for determining equivalence between established and modified procedures. The integration of these quantitative approaches strengthens the verification process and provides robust data for regulatory compliance.
Special Considerations and Emerging Technologies
Unique Verification Scenarios
Certain laboratory scenarios require specialized verification approaches beyond the standard protocols. For IHC performed on cytologic specimens that are not fixed in the same manner as the tissues used for initial validation, separate validations are required for each new analyte and corresponding fixation method [1] [2]. A minimum of 10 positive and 10 negative cases is recommended for each validation, with increased numbers for predictive markers [2]. Similarly, for decalcified tissues, the laboratory director must determine the sufficient number of tissues to ensure consistent expected results [2].
For predictive immunohistochemical assays with distinct scoring schemes (e.g., HER2, PD-L1), laboratories must separately verify each assay-scoring system combination with a minimum of 20 positive and 20 negative tissues [1] [2]. This requirement acknowledges that scoring system specificity can be as critical as the staining itself for proper clinical interpretation. The verification set should include challenges based on the intended clinical use of the assay, particularly around critical clinical decision points such as the cutoff for HER2 positivity in breast cancer [46].
Advanced and Automated Analysis Methods
Emerging technologies are transforming IHC verification methodologies. Digital image analysis and deep learning algorithms are increasingly applied to IHC quantification, reducing subjectivity and improving reproducibility [45] [47]. These automated systems can precisely identify and quantify nuclear, membrane, and cytoplasmic expressions in whole-slide images, providing objective data for comparative verification studies [47].
Open-source software platforms like QuPath enable semi-automated cell counting and classification, significantly reducing inter-rater variability [45]. One study demonstrated that semi-automated quantification achieved strong correlation with manual counting while minimizing subjective interpretation and regional bias [45]. These tools are particularly valuable for verification studies, as they provide standardized, quantitative endpoints for comparing established and modified procedures. As these technologies mature, they are likely to become integral components of robust verification protocols, potentially satisfying regulatory requirements for objectivity and standardization.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table: Key Research Reagent Solutions for IHC Verification Studies
| Reagent/Solution | Function in Verification | Application Notes |
|---|---|---|
| Positive Control Tissues | Verify staining performance and intensity; ensure modified procedure detects target | Should represent range of expression levels; tissue microarray formats efficient for verification |
| Negative Control Tissues | Confirm specificity; assess background staining | Critical for determining signal-to-noise ratio in modified procedure |
| Cell Line Calibrators | Provide standardized protein expression reference | Useful as comparators when natural tissues with known protein amounts are unavailable |
| Antigen Retrieval Buffers | Unmask epitopes altered by fixation | pH and buffer composition changes require major change verification |
| Detection Systems | Amplify signal while minimizing background | Changes require sufficient verification cases to ensure consistent performance |
| Primary Antibodies | Specifically bind target antigen | Clone changes require full revalidation; same clone vendor switches need limited verification |
This toolkit represents the essential reagents required for comprehensive IHC verification studies. The selection of appropriate positive and negative control tissues is particularly critical, as these materials form the basis for comparative analysis between established and modified procedures [5] [2]. For laboratories maintaining multiple IHC assays, developing well-characterized tissue microarrays containing both positive and negative controls for multiple targets can streamline the verification process for routine modifications.
Verification of modified IHC procedures requires a systematic, tiered approach based on the type and potential impact of the change. By implementing the strategies outlined—categorizing modifications appropriately, following structured experimental protocols, applying quantitative acceptance criteria, and leveraging emerging technologies—laboratories can ensure robust verification that satisfies regulatory requirements while maintaining assay quality. The framework presented enables efficient resource allocation through risk-based verification intensity, with more extensive testing reserved for changes with greater potential impact on assay performance. As IHC technologies continue to evolve, incorporating standardized quantitative methods and automated analysis platforms will further enhance the objectivity and reproducibility of verification protocols, ultimately supporting the generation of reliable research and clinical data.
Immunohistochemistry (IHC) serves as a cornerstone technique in diagnostic pathology and research, providing critical insights into cellular and molecular processes by detecting specific antigens within tissue samples [48] [49]. The reliability of IHC results is paramount for accurate diagnosis, prognosis, and treatment decisions, particularly in areas such as breast cancer biomarker testing like HER2 [50]. However, this reliability is heavily dependent on pre-analytical variables—the processes that tissue specimens undergo before actual staining and analysis. Factors related to tissue fixation, decalcification, and the handling of cytology specimens significantly impact antigen preservation and, consequently, the accuracy and interpretability of IHC results [50] [49]. Within the framework of Clinical Laboratory Improvement Amendments (CLIA) requirements for assay validation, understanding and controlling these variables is not merely a recommendation but a fundamental necessity for ensuring that IHC assays are both reliable and reproducible in clinical settings [3] [1]. This guide objectively compares the performance of IHC assays across different pre-analytical conditions, providing structured data and methodologies essential for researchers and drug development professionals to navigate validation requirements effectively.
The Impact of Fixation on IHC Assay Performance
Fixation Parameters and Their Effects
Tissue fixation is the critical first step in stabilizing cellular structures and antigens. The type of fixative, fixation time, and ischemic intervals collectively determine the quality of subsequent IHC analysis.
Table 1: Comparative Analysis of Fixation Variables and IHC Performance
| Pre-Analytical Variable | Optimal Condition | Suboptimal Condition | Impact on IHC Results | Supporting Data |
|---|---|---|---|---|
| Cold Ischemic Time | As short as possible; ideally <1 hour [50] | Prolonged (>1 hour) | HER2 protein degradation; score reduction (e.g., 2+ to 1+/0); poor ISH hybridization [50] | One- or two-step HER2 IHC score reduction observed [50] |
| Fixation Time | 6-72 hours in 10% NBF [50] | Under-fixation (<6h); Over-fixation (>72h) | Under-fixation: poor morphology, antigen loss; Over-fixation: epitope masking, reduced sensitivity [50] [49] | Standard per ASCO-CAP guidelines [50] |
| Fixative Type | 10% Neutral Buffered Formalin (NBF) | Non-standard fixatives | Variable antigen sensitivity, altered staining intensity [1] [49] | Requires separate validation for alternative fixatives [1] |
Experimental Protocols for Evaluating Fixation
To systematically evaluate the impact of fixation, the following experimental methodology is recommended:
- Sample Preparation and Variable Application: Select uniform tissue samples (e.g., breast carcinoma known to express HER2). Subject them to controlled cold ischemic times (e.g., 0.5, 1, 2, 4 hours) followed by fixation in 10% NBF for varying durations (e.g., 4, 8, 24, 96 hours) [50].
- IHC Staining and Interpretation: Process all samples identically using a standardized IHC protocol for the target antigen (e.g., HER2). This includes automated staining platforms and polymer-based detection systems to minimize analytical variation [48] [50].
- Morphological Correlation: Examine Hematoxylin and Eosin (H&E) stained sections from all test conditions. Key indicators of ischemic damage include cytoplasmic vacuoles, nuclear pyknosis, karyorrhexis, or karyolysis, particularly in the center of tissue fragments [50].
- Data Analysis: Compare IHC staining intensity, percentage of positive cells, and cellular distribution across the different pre-analytical conditions. A reduction in staining score (e.g., from 2+ to 1+) coupled with morphological changes confirms a negative impact [50].
Diagram 1: Fixation variable impact on IHC results.
Decalcification and Specialized Processing
Comparative Effects of Decalcification Methods
Decalcification is essential for processing bony specimens but poses a significant risk to antigen integrity. The choice of method and protocol directly influences IHC validity.
Table 2: Decalcification Methods and Antigen Preservation
| Decalcification Method | Principle | Impact on Antigenicity | Recommendations for IHC |
|---|---|---|---|
| Weak Acids (e.g., Formic Acid) | Slow chelation of calcium ions; better tissue preservation [48] [49] | Moderate antigen damage; some epitopes remain detectable | Preferred for IHC; may require protocol optimization (e.g., extended AR) |
| Strong Acids (e.g., Nitric, Hydrochloric) | Rapid dissolution of mineral content | Severe antigen damage; many epitopes destroyed or masked | Generally avoided for IHC-critical specimens |
| Chelating Agents (EDTA) | Slow, gentle chelation without acidic damage [49] | Minimal antigen damage; best preservation of protein structure | Gold standard for IHC; requires longer processing time |
Validation Protocol for Decalcified Specimens
Validating IHC assays on decalcified tissues is a key part of a laboratory's quality assurance. The 2024 CAP guidelines emphasize that any change in pre-analytical processing, including decalcification, requires verification of assay performance [1]. The recommended protocol involves:
- Parallel Testing: Identify a case with involved bone and concurrent soft tissue metastasis or a non-decalcified primary tumor. The soft tissue segment serves as the optimal, non-decalcified control [50].
- Controlled Decalcification: Subject the portion requiring decalcification to the laboratory's standard EDTA-based protocol. Avoid strong acids to maximize antigen survival [49].
- IHC Staining and Comparison: Perform IHC for the target antigens on both the decalcified and control tissues using an identical, optimized protocol. Pay particular attention to antigen retrieval, which may need to be enhanced for decalcified specimens [48] [1].
- Concordance Analysis: Evaluate the staining concordance between the two samples. A minimum of 10 positive and 10 negative cases is recommended for validation studies when moving to a new pre-analytical condition [1]. Acceptable performance is typically defined as ≥90% concordance with the control tissue [1].
Cytology Specimens in IHC Assays
Performance Comparison: Cytology vs. Histology
Cytology specimens, such as fine-needle aspirates (FNAs) and effusions, are increasingly used for IHC, but their variable fixation presents unique challenges.
Table 3: Cytology vs. Histology Specimens for IHC
| Characteristic | Formalin-Fixed Paraffin-Embedded (FFPE) Histology | Cytology Specimens (e.g., Cell Blocks) | Implication for IHC Validation |
|---|---|---|---|
| Fixation | Standardized 10% NBF [50] | Variable (e.g., alcohol-based, spray fixatives) [1] | Requires separate validation for each fixative type [1] |
| Tissue Architecture | Preserved | Lost (individual cells or small clusters) | Scoring systems may differ; internal controls are crucial |
| Validation Sample Size | Established per lab protocol | Minimum 10 positive and 10 negative cases for alternative fixatives [1] | Increased validation burden for cytology |
| Concordance Requirement | ≥90% with comparator method [1] | ≥90% with FFPE or other gold standard [1] | Performance standard remains high |
Experimental Workflow for Cytology Validation
The 2024 CAP guideline update provides explicit recommendations for validating IHC on cytology specimens fixed differently from the tissues used in the initial validation [1]. The following workflow ensures rigorous assessment:
- Sample Selection and Preparation: Collect a minimum of 20 well-characterized cytology samples (10 positive, 10 negative for the target antigen) prepared as cell blocks using the laboratory's standard cytology fixative [1].
- Reference Standard Comparison: Compare IHC results on the cytology samples against a validated reference standard. This can be IHC on FFPE tissue from the same patient, results from a different validated method (e.g., flow cytometry), or expected staining based on clinical or molecular data [1].
- Staining Optimization: Titrate antibody concentrations and optimize antigen retrieval methods specifically for the cytology specimens. This is crucial because fixation differences can significantly alter antigen accessibility [48] [1].
- Blinded Interpretation: Have pathologists evaluate the cytology IHC stains in a blinded fashion against the reference standard. Calculate the concordance rate, aiming for at least 90% for both positive and negative agreement to meet validation standards [1].
Diagram 2: Cytology specimen IHC validation workflow.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful management of pre-analytical variables requires specific reagents and materials. The following table details essential components for robust IHC validation studies.
Table 4: Essential Research Reagents and Materials for IHC Pre-Analytical Validation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| 10% Neutral Buffered Formalin (NBF) | Standard chemical fixative that cross-links proteins to preserve tissue morphology [50] [49] | The benchmark fixative; fixation time must be controlled (6-72 hours) [50]. |
| EDTA-Based Decalcification Solution | Gently chelates calcium ions from bone with minimal damage to protein epitopes [49] | Preferred over strong acids for IHC; requires longer processing time but superior antigen preservation. |
| Antigen Retrieval Buffers (e.g., Citrate, EDTA, Tris-EDTA) | Reverses formalin-induced cross-links, making epitopes accessible to antibodies [48] [49] | Heat-induced epitope retrieval (HIER) is standard; buffer pH and heating method (microwave, pressure cooker) must be optimized for each antibody and tissue type. |
| Primary Antibodies (Monoclonal/Polyclonal) | Bind specifically to the target antigen of interest [48] [49] | Monoclonal antibodies offer higher specificity; must be carefully titrated using known positive and negative tissues to establish optimal dilution. |
| Polymer-Based Detection Systems | Signal amplification system where multiple enzyme and antibody molecules are conjugated to a polymer backbone [48] [49] | Provides high sensitivity and low background compared to older avidin-biotin systems; reduces staining time. |
| Chromogens (e.g., DAB, NovaRed) | Enzymatic substrates that produce a colored precipitate at the antigen site [48] | DAB (brown) is most common; choice may be influenced by laboratory preference, counterstain, and need for permanent staining. |
| Blocking Reagents (e.g., Normal Serum, Protein Block) | Reduce non-specific background staining by occupying reactive sites on the tissue [48] [49] | Critical for clean results; can be normal serum from the species of the secondary antibody or commercial universal blocking agents. |
The journey of a tissue specimen from the patient to the microscope slide is fraught with variables that can fundamentally alter the outcome of an IHC assay. As demonstrated through comparative data and standardized protocols, factors such as prolonged cold ischemia, deviation from optimal formalin fixation, harsh decalcification, and the use of variably fixed cytology specimens pose significant risks to antigen integrity and, consequently, the reliability of diagnostic and research results. Adherence to the updated CAP guidelines and a rigorous, evidence-based validation strategy are not optional but imperative for CLIA compliance [1]. This involves establishing and documenting specific protocols for each pre-analytical step, conducting parallel validation studies when conditions change (e.g., using a new fixative or processing a new specimen type), and maintaining a robust quality management system. By systematically addressing these pre-analytical challenges with the methodologies and reagents outlined, laboratories can ensure the delivery of accurate, reproducible, and clinically actionable IHC data, thereby upholding the highest standards of patient care and scientific inquiry.
In the rigorous field of diagnostic assay development, discordant results—where different tests yield conflicting answers for the same sample—present a significant challenge for researchers and clinicians. These discrepancies often serve as critical indicators of underlying issues with a test's diagnostic sensitivity and specificity, two foundational pillars of assay performance [51] [52]. Sensitivity defines a test's ability to correctly identify individuals with a disease (true positives), while specificity measures its capacity to correctly identify those without the disease (true negatives) [51] [53]. Within the framework of IHC assay validation and compliance with the Clinical Laboratory Improvement Amendments (CLIA), a deep understanding of these metrics is not merely academic; it is a regulatory and practical necessity for ensuring patient safety and the reliability of data supporting drug development [3]. This guide objectively compares diagnostic test performance by examining experimental data, validation protocols, and the analytical tools essential for resolving diagnostic discordance.
Defining Diagnostic Performance Metrics
The interpretation of any diagnostic test, including Immunohistochemistry (IHC) assays, relies on a core set of statistical measures. These metrics are derived from a 2x2 contingency table that cross-references test results with known disease status [51] [53].
- Sensitivity: The proportion of truly diseased individuals who test positive. A highly sensitive test is optimal for "ruling out" a disease when the result is negative and is crucial for screening [52].
- Specificity: The proportion of truly healthy individuals who test negative. A highly specific test is optimal for "ruling in" a disease when the result is positive and is used for confirmation [52].
- Positive Predictive Value (PPV): The probability that a subject with a positive test result actually has the disease. This value is heavily influenced by disease prevalence [51] [53].
- Negative Predictive Value (NPV): The probability that a subject with a negative test result is truly free of the disease. Like PPV, it varies with disease prevalence [51] [53].
- Likelihood Ratios: These ratios, which are not prevalence-dependent, quantify how much a given test result will raise or lower the pretest probability of disease. A Positive Likelihood Ratio (LR+) greater than 10 is considered a strong indicator to rule in disease, while a Negative Likelihood Ratio (LR-) less than 0.1 is excellent for ruling it out [53].
The inverse relationship between sensitivity and specificity is a fundamental concept. Adjusting a test's cutoff value to improve sensitivity often compromises specificity, and vice versa [52]. This trade-off must be carefully managed based on the test's intended clinical use.
Case Studies in Diagnostic Discordance
Discordant results often arise when tests of differing sensitivities and specificities are applied to the same clinical question. The following case studies provide concrete examples and quantitative data.
Case Study 1: Fourth-Generation HIV Testing in a Field Setting
A 2025 study evaluated the point-of-care performance of the Determine HIV Early Detect (a fourth-generation antigen/antibody test) in rural Eswatini, revealing a significant disparity with earlier laboratory-based evaluations [54].
- Experimental Protocol: The study nested a diagnostic accuracy evaluation within a larger STI burden study. HTS counsellors performed the index test (Determine HIV Early Detect) on finger-prick blood in parallel with the national serial RDT algorithm. The reference standard was an HIV viral load (VL) test performed on plasma using the Xpert platform in a central laboratory. Acute HIV Infection (AHI) was defined by a negative/discordant RDT result combined with a VL >10,000 copies/mL, or two consecutive detectable VL measurements [54].
- Results and Interpretation: The performance data, summarized in the table below, highlights a critical finding: the test's sensitivity for detecting Acute HIV Infection was markedly low in a real-world field setting compared to its established performance for chronic infection. This underscores how test performance can vary dramatically between controlled laboratory environments and routine point-of-care use, potentially due to factors like sample collection and operator technique [54].
Table 1: Performance of Determine HIV Early Detect in a Field Setting (N=1163) [54]
| Condition | Sensitivity (%) | 95% CI | Specificity (%) | 95% CI |
|---|---|---|---|---|
| Overall HIV Infection | 83.7 | 70.3–92.7 | 99.8 | 99.4–100 |
| Acute HIV Infection (AHI) | 20.0 | 2.5–55.6 | 99.8 | 99.4–100 |
Case Study 2: Discordant SARS-CoV-2 Testing
During the COVID-19 pandemic, a common scenario involved an initial positive Rapid Antigen Test (RAT) followed by a negative confirmatory Nucleic Acid Amplification Test (NAAT), such as RT-PCR [55].
- Experimental Protocol: Researchers developed a statistical model to interpret these discordant results. The model incorporated key variables: RAT sensitivity (84.6% for BinaxNOW) and specificity, NAAT false-negative rates (which vary by time since exposure), and estimated community prevalence of SARS-CoV-2. The output was the probability that the initial positive RAT was a false positive [55].
- Results and Interpretation: The model demonstrated that the predictive value of a discordant result is highly dependent on disease prevalence. For example, when community prevalence was low (below 200 weekly cases per 100,000), the probability that a positive RAT was a false positive after a negative same-day NAAT was 89.6%. This probability changed if the NAAT was administered several days later. This case study powerfully illustrates how pre-test probability, driven by prevalence, is crucial for interpreting individual test results and that a single positive RAT in a low-prevalence setting requires confirmation with a more specific test [55].
Case Study 3: Automated vs. Laboratory-Develop PCR Tests
A 2022 study directly compared the diagnostic performance of the fully automated Roche Cobas 6800 system against a laboratory-developed test (LDT) based on ICMR protocols for detecting SARS-CoV-2 [56].
- Experimental Protocol: The study employed two approaches. First, a validation method where 188 samples previously tested by LDT were re-tested on the Cobas 6800. Second, a head-to-head evaluation of 1631 samples tested on both platforms simultaneously. A quantitative algorithm was used to resolve inconclusive results, considering symptoms, contact history, and additional testing [56].
- Results and Interpretation: The initial validation showed 88% overall agreement, but 20 samples were discordant (all Cobas positive/LDT negative). The head-to-head evaluation showed much higher agreement (99%), suggesting that sample handling or timing may influence results. The discordant samples were characterized by very low viral loads, highlighting the impact of a test's Limit of Detection (LoD) on its clinical sensitivity, especially in recovering patients or during early/very late infection stages [56].
Table 2: Comparison of SARS-CoV-2 Testing Platforms [56]
| Testing Approach | Overall Agreement | Kappa Statistic (κ) | Positive Agreement | Key Findings |
|---|---|---|---|---|
| Validation (n=180) | 88% | 0.76 (Substantial) | 100% | 20 discordant samples (Cobas+/LDT-) |
| Head-to-Head (n=1566) | 99% | 0.98 (Almost Perfect) | 100% | 3 discordant samples with high Ct values |
IHC Assay Validation and CLIA Requirements
For IHC assays used in clinical trials and patient care, rigorous validation is mandated to ensure results are accurate, reproducible, and reliable. The College of American Pathologists (CAP) provides evidence-based guidelines for this process, which laboratories use to satisfy CLIA requirements [1] [2].
CLIA establishes the federal standards for all U.S. facilities testing human specimens, but it does not prescribe how to satisfy each performance study [3]. The 2024 CAP guideline update offers detailed, actionable recommendations for the analytic validation of IHC assays [1] [2]:
- Laboratory-Developed Tests (LDTs): Must be fully validated. For non-predictive assays, a minimum of 10 positive and 10 negative cases is required. For predictive markers (e.g., PD-L1, HER2), a minimum of 20 positive and 20 negative cases is required [2].
- FDA-Cleared/Approved Assays: Must undergo verification. If manufacturer instructions are lacking, a minimum of 20 positive and 20 negative cases should be used for predictive markers [2].
- Concordance Threshold: Laboratories must achieve at least 90% overall concordance between the new assay and the comparator method during initial validation/verification [2].
- Assay Specifics: Separate validation is required for different scoring systems, specimen types (e.g., cytology vs. surgical pathology), and fixatives. Any change in antibody clone necessitates a full revalidation [1] [2].
The following workflow diagram illustrates the core principles and decision points in the IHC assay validation process as defined by CAP guidelines and CLIA standards.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully validating an IHC assay and troubleshooting discordant results requires a suite of high-quality reagents and materials. The following table details key components essential for robust assay development and performance assessment.
Table 3: Essential Research Reagent Solutions for IHC Assay Validation
| Reagent/Material | Critical Function | Validation Consideration |
|---|---|---|
| Primary Antibody | Binds specifically to the target antigen of interest. The clone, host, and concentration are critical. | A change in antibody clone necessitates a full revalidation. Lot-to-lot variation must be checked with control tissues [2]. |
| Control Tissues | Tissue specimens with known positive and negative status for the target antigen. | Used to establish assay performance during validation and in every run for quality control. Must represent a range of expression levels [2]. |
| Detection System | A kit that typically includes secondary antibodies, enzyme conjugates (e.g., HRP), and chromogens (e.g., DAB) to visualize antibody binding. | Changing the detection system requires confirmation of assay performance with a sufficient number of positive and negative tissues [2]. |
| Antigen Retrieval Reagents | Buffers (e.g., citrate, EDTA) and methods (heat, enzyme) used to unmask epitopes altered by tissue fixation. | A change in the antigen retrieval method (buffer, pH, or platform) requires confirmation of performance with multiple tissues [2]. |
| Cell Lines with Known Protein Expression | Cultured cells containing calibrated amounts of the target protein. | Can serve as a highly stringent comparator for initial analytic validation, acting as a "calibrator" [1] [2]. |
Discordant diagnostic results are not merely contradictions to be resolved; they are opportunities to deepen our understanding of assay performance under the critical lenses of sensitivity, specificity, and clinical context. As demonstrated, a test's performance is not an immutable property but is influenced by the population tested, disease prevalence, sample type, and operational setting. For researchers and drug developers operating within the strict confines of CLIA and CAP guidelines, a rigorous, data-driven approach to validation is non-negotiable. By systematically applying the principles of diagnostic accuracy, utilizing appropriate statistical models, and adhering to structured validation workflows, scientists can ensure that IHC and other diagnostic assays deliver the reliable, reproducible data necessary to drive accurate patient diagnosis and successful therapeutic development.
Managing Rare Analytes and Low-Frequency Antigens with Limited Tissue
Immunohistochemistry (IHC) validation is a critical process ensuring that assays are reliable, accurate, and reproducible for clinical diagnostics and research. The College of American Pathologists (CAP) has established comprehensive guidelines outlining evidence-based practices for analytic validation of IHC assays [1]. For laboratories worldwide, a significant challenge emerges when applying these principles to rare analytes and low-frequency antigens—biomarkers with scarce expression in the population or associated with rare diseases [57].
The fundamental requirement for validation is a cohort of known positive and negative tissue cases. CAP guidelines typically recommend using a minimum of 20 positive and 20 negative cases for predictive marker assays and 10 positive and 10 negative cases for non-predictive assays [15]. For rare antigens, procuring these numbers is often technologically daunting and sometimes practically impossible. This creates a compliance gap, as the Clinical Laboratory Improvement Amendments (CLIA) require laboratories to validate the performance characteristics of all assays before reporting patient results [1]. This guide compares practical strategies and solutions for overcoming these validation hurdles, providing a structured framework for researchers and laboratory directors.
Quantifying the Challenge: The Landscape of Rare Antigens
The difficulty of validation is directly proportional to the rarity of the antigen and the associated disease incidence. For some markers, a laboratory might need to screen hundreds or even thousands of archival cases to find a sufficient number of positive samples.
Table 1: Validation Case Requirements and Challenges for Selected Rare Antigens
| Antigen / Marker | Disease Context | Frequency / Incidence | Validation Challenge |
|---|---|---|---|
| ALK | Anaplastic Large Cell Lymphoma (ALCL) | 2-3% of all lymphomas (adults); only 50-60% are ALK+ [57] | Finding a single positive case is challenging; protocols differ from ALK+ lung cancer. |
| MSH2 | Lynch Syndrome (Colorectal Cancer) | ~2% of colorectal carcinomas [57] | Requires screening ~1,000 cancers to find 20 MSH2-deleted cases. |
| INI-1 | Malignant Rhabdoid Tumor | ~0.19 per million for renal tumors [57] | Extremely low incidence makes accruing positive cases nearly impossible through routine practice. |
| Myo-D1 / Myogenin | Rhabdomyosarcoma | 4.5 cases/million children/adolescents per year [57] | Pediatric rarity makes tissue procurement difficult. |
| PD-L1 | Non-Small Cell Lung Cancer (NSCLC) | Varies by cutoff (e.g., 24% of cases >5% tumor cell positivity) [57] | A limited number of "positive" cases meet specific clinical trial percent-positive cutoffs. |
The CAP acknowledges this constraint, stating that for low-incidence antigens, the laboratory medical director ultimately determines the extent of validation required, provided a scientifically supported justification is documented [57] [15].
Comparison of Practical Validation Strategies
When standard tissue cohorts are unattainable, laboratories must employ alternative strategies. The following table compares the most common and practical approaches, detailing their implementation and limitations.
Table 2: Comparison of Practical Solutions for Validating Rare Antigens
| Strategy | Description | Key Implementation Steps | Advantages | Limitations / Considerations |
|---|---|---|---|---|
| Internal Biorepository Mining | Retrospective & prospective searches of Laboratory Information System (LIS) for archival material [57]. | 1. Query LIS for historical cases and diagnoses.2. Retrieve blocks/slides from pathology archives.3. Use as validation set or to supplement other methods. | Uses in-house resources; tissues have known pre-analytical conditions. | Success depends on archive breadth and organization. May still yield insufficient numbers for very rare targets. |
| Tissue Microarrays (TMAs) & Multi-Tissue Blocks | Purchased from commercial vendors or constructed in-house by combining multiple small tissue cores into a single block [57]. | 1. Source TMAs with required rare tissues.2. Construct multi-tissue blocks with available positive cases.3. Validate using the multi-core block slide. | Extremely valuable; maximizes data from scarce tissue; reduces reagent use and cost [57] [58]. | Homemade TMA construction requires expertise. Staining intensity may vary from whole sections [58]. |
| Cell Line Controls | Using cell lines with known protein expression levels as positive controls and validation materials [1] [58]. | 1. Identify cell lines expressing the target antigen.2. Create FFPE cell pellets.3. Use pellets in validation slides. | Provides a consistent and renewable source of positive material [58]. | Cells lack the complex tissue architecture and microenvironment of real patient samples. |
| External Quality Assessment (EQA) & Collaboration | Participation in EQA programs or collaborating with other laboratories to share cases and data [57]. | 1. Enroll in EQA programs (e.g., NordiQC).2. Partner with reference or academic labs.3. Share archival material or validation data. | Provides interlaboratory comparison and educational feedback. | EQA may provide insufficient case numbers; collaboration agreements can be complex. |
| Literature-Based Correlation | Conducting a thorough literature search and correlating the staining patterns of the new test with expected results from published clinical trials and studies [57]. | 1. Perform systematic literature review.2. Correlate observed staining with expected patterns and localization.3. Document justification. | Practical when no other materials are available. | Considered the least stringent comparator; should be combined with other methods where possible [1]. |
These strategies are not mutually exclusive and are most powerful when used in combination. A robust validation plan for a rare antigen might use a TMA supplemented with a few key archival cases and qualified cell line pellets, with results benchmarked against published literature.
Experimental Protocols for Validating Rare Antigens
Protocol 1: Validation Using Tissue Microarrays (TMAs)
TMAs are a high-throughput tool essential for validating rare biomarkers. The protocol below outlines their use in a validation study.
Methodology:
- TMA Sourcing or Construction: Procure a commercial TMA containing the rare tissue of interest or construct one in-house. For construction, use a tissue microarrayer to core archival FFPE donor blocks and array them into a recipient paraffin block [57] [58].
- Sectioning and Staining: Cut sections from the TMA block at a standard thickness (4-7 μm). Follow a standard IHC protocol: deparaffinization, rehydration, antigen retrieval using Heat-Induced Epitope Retrieval (HIER), application of primary and labeled secondary antibodies, and chromogenic detection [48] [58].
- Microscopic Evaluation and Scoring: Examine the entire TMA section under a microscope. Score each core individually for the presence, intensity, and subcellular localization of staining.
- Data Correlation and Analysis: Compare the IHC staining results from the TMA with the expected results for each core, as defined by the gold standard (e.g., known diagnosis, molecular data, or results from a validated assay in another lab). Calculate the concordance rate.
Protocol 2: Validation Using Cell Line Pellets
Cell lines provide a standardized and renewable biological control material, which is crucial for rare antigens.
Methodology:
- Cell Line Culture and Pellet Formation: Culture cell lines known to express (positive) and not express (negative) the target antigen. Harvest the cells, wash, and centrifuge to form a tight pellet.
- Fixation and Processing: Fix the cell pellet in 10% neutral buffered formalin for a standardized time (e.g., 6-24 hours). Process the fixed pellet through graded alcohols and xylene, then embed it in paraffin (FFPE) to create a cell block [58].
- IHC Staining and Interpretation: Section the FFPE cell block and subject it to the same IHC protocol as patient tissues. Interpret the staining under a microscope. The positive control cell line should show the expected staining pattern, while the negative control should show no specific staining.
- Integration into Validation: Cell line pellets can be included on validation slides as internal controls or used as a primary component of the validation set when patient tissues are utterly unavailable [1].
The following workflow diagram illustrates the decision-making process for selecting and implementing these strategies to build a compliant validation study.
The Scientist's Toolkit: Key Reagents and Materials
Successful validation of rare antigens relies on a suite of key reagents and materials. The following table details these essential components and their functions in the validation process.
Table 3: Key Research Reagent Solutions for Rare Antigen Validation
| Item / Reagent | Function in Validation | Application Notes |
|---|---|---|
| Primary Antibodies (Monoclonal) | Bind specifically to a single epitope on the target antigen. | Offer greater batch-to-batch consistency; preferred for standardized assays [58]. |
| Primary Antibodies (Polyclonal) | Bind to multiple epitopes on the target antigen. | Can be more sensitive for hard-to-detect targets but may have more nonspecific background [48] [58]. |
| Tissue Microarray (TMA) | Allows simultaneous validation of an antibody on dozens of tissue samples on a single slide. | Invaluable for maximizing data from rare tissues; available commercially or custom-made [57] [58]. |
| Cell Lines (with known expression) | Provide a renewable and standardized source of positive and negative control material. | Essential for rare antigens; FFPE pellets can be used for validation and as run controls [1] [58]. |
| Antigen Retrieval Buffer (e.g., Citrate, EDTA) | Reverses formaldehyde-induced cross-links, unmasking epitopes for antibody binding. | Critical for FFPE tissues; the pH and method (HIER) must be optimized for each antibody [48]. |
| Polymer-Based Detection System | Visualizes the antigen-antibody interaction with high sensitivity and low background. | Uses enzyme-labeled polymers; largely replaces older avidin-biotin systems to reduce endogenous biotin background [48]. |
| Multi-Tissue Block (Homemade) | A cost-effective alternative to TMAs, created by embedding multiple small tissue fragments in a single block. | Offers great utility for clinical IHC laboratories when commercial TMAs are unavailable [57]. |
Validating IHC assays for rare analytes and low-frequency antigens demands a strategic and often combinatorial approach. While the CAP guidelines set the ideal standard, they provide the flexibility for laboratory directors to design and document scientifically sound validation studies that overcome tissue scarcity. By leveraging solutions such as TMAs, cell lines, and inter-laboratory collaboration, and by clearly documenting the rationale for the chosen approach, researchers can ensure regulatory compliance and, most importantly, deliver reliable, high-quality test results that ultimately benefit patient care.
Within the framework of Clinical Laboratory Improvement Amendments (CLIA) requirements, robust and ongoing quality control (QC) is not optional but a fundamental mandate for any laboratory reporting patient results. For immunohistochemistry (IHC) assays, which play a critical role in diagnosis, predictive marker assessment, and therapeutic decisions, a comprehensive QC program ensures the analytical validity of test results over time. This program is a dynamic process that extends far beyond initial assay validation, actively monitoring performance through three core, interconnected activities: proficiency testing, lot-to-lot comparisons, and vigilant monitoring for assay drift. Adherence to evidence-based guidelines, such as those from the College of American Pathologists (CAP), provides a structured path to meeting and exceeding CLIA standards, thereby ensuring the accuracy, reliability, and clinical safety of IHC testing [1] [2].
Proficiency Testing
Purpose and CLIA Requirements
Proficiency Testing (PT), also known as external quality assessment (EQA), is a cornerstone of CLIA compliance. Its primary purpose is to provide an objective, external evaluation of a laboratory's testing performance by comparing its results with a consensus of other laboratories or a reference method. PT acts as a crucial safeguard, validating that the laboratory's entire testing process—from pre-analytical to analytical and post-analytical phases—is functioning correctly. Under CLIA regulations, successful participation in approved PT programs is mandatory for certified laboratories. Failure to achieve satisfactory performance can trigger sanctions and requires immediate corrective action.
Recommended Practices and Experimental Protocols
The CAP guidelines, which serve as a de facto standard for laboratory accreditation, strongly emphasize the role of PT. Laboratories should enroll in formal, graded PT programs where available for their specific tests [1]. For assays where commercial PT is not available, laboratories must establish an alternative performance assessment system. This typically involves periodic split-sample comparison with another reference laboratory.
A recommended protocol for this alternative assessment is as follows:
- Frequency: Testing should be performed at least twice per year.
- Sample Selection: Use well-characterized clinical specimens or previously validated tissue cell line blocks.
- Methodology: Select a minimum of 5-10 samples encompassing the assay's reportable range (e.g., negative, weak positive, strong positive). Split each sample, testing one portion in-house and sending the other to a reference laboratory that uses a validated/verified method.
- Data Analysis: Calculate the concordance between the two sets of results. The CAP guideline update has harmonized the required concordance for all IHC assays to at least 90% [1] [2].
- Documentation: Meticulously document all procedures, results, and corrective actions taken for any discrepancies. This documentation is essential for inspection readiness.
Table 1: Core Components of a Proficiency Testing Plan
| Component | Description | Frequency | Acceptance Criterion |
|---|---|---|---|
| Formal PT | Enrollment in a CAP-approved or equivalent graded program | As per program schedule (e.g., 3x/year) | Satisfactory grade from PT provider |
| Alternative Assessment | Split-sample comparison with a reference lab | At least twice per year | ≥90% overall concordance [1] |
| Internal Challenges | Use of archived, previously characterized tissues | With each PT event or new reagent lot | Consistency with expected results |
Lot-to-Lot Comparisons
Purpose and Regulatory Guidance
Antibodies and detection kits are biological reagents subject to inherent variability between manufacturing lots. A lot-to-lot verification is a critical QC procedure designed to ensure that a new reagent lot performs equivalently to the validated lot currently in use, thereby preventing unforeseen changes in assay sensitivity or specificity. The CAP guideline provides clear, actionable statements on the requirements for this process, framing it as an essential part of assay revalidation [2].
Experimental Protocol for Lot-to-Lot Verification
The scope of testing required depends on the nature of the change. The protocol below outlines the minimum verification standard when placing a new antibody lot into clinical service for an existing, validated assay.
- Objective: To confirm that a new lot of primary antibody produces staining results equivalent to the current lot.
- Sample Selection: The CAP guideline states that laboratories should test at least 1 known positive and 1 known negative tissue [2]. A control tissue containing both positive and negative internal cells (e.g., tonsil for many lymphocytes) can satisfy this requirement.
- Staining Procedure: The new and old antibody lots should be used to stain serial sections from the selected tissue blocks. All other variables (detection system, staining platform, incubation times) must remain identical.
- Evaluation: Staining should be evaluated for key parameters:
- Specificity: Staining is present only in the expected cell types and subcellular localization.
- Intensity: The staining intensity of the positive cells is equivalent.
- Background: There is no significant increase in non-specific background staining.
- Documentation: The laboratory director or designee must review and approve the comparison results before the new lot is released for clinical use.
It is critical to note that a more extensive revalidation is required if the change involves the antibody clone, vendor, dilution, or detection system. For such significant changes, the CAP guideline recommends a full revalidation equivalent to the initial analytic validation [2].
The following workflow visualizes the decision process for reagent and assay changes:
Monitoring for Assay Drift
Understanding Assay Drift
Assay drift refers to the gradual, often insidious change in an assay's performance characteristics over time, leading to a deviation from its original, validated state. Unlike sudden failures, drift is a slow degradation that can be difficult to detect without systematic monitoring. It can manifest as a change in sensitivity (calibration drift), leading to consistently weaker or stronger staining, or an increase in background noise. Drift can be caused by subtle factors like reagent degradation (even within the same lot), gradual wear and tear on instrumentation, changes in environmental conditions, or shifts in water purity [59]. In the context of computational models used with quantitative IHC, "calibration drift" can also occur when the relationship between the staining result and the clinical outcome changes over time due to population shifts [60].
Strategies and Detection Protocols
Monitoring for drift requires a proactive, data-driven approach. While CLIA does not prescribe a specific method, it mandates that laboratories ensure ongoing test accuracy. The following protocol outlines a robust method for detecting potential drift.
- Objective: To proactively identify gradual changes in assay sensitivity and specificity.
- Core Tool: Longitudinal Control Tracking: Implement a system to track and trend the results of daily positive and negative controls. This includes both qualitative assessment (e.g., staining intensity scores) and, if applicable, quantitative data (e.g., H-scores, percentage of positive cells).
- Protocol:
- Establish a Baseline: Using a stable control material (e.g., a multi-tissue block or cell line), establish a baseline mean and acceptable range for staining intensity during the assay's validated state.
- Monitor with Controls: Include this control material in every run or at a defined regular frequency (e.g., weekly).
- Statistical Analysis: Plot the results on a control chart (e.g., a Levey-Jennings chart). Apply Westgard rules or similar statistical process control rules to identify trends, shifts, or increased variation that may indicate the onset of drift.
- Proactive Challenges: Periodically (e.g., quarterly), test a panel of archived specimens with known, well-characterized staining patterns. Comparing current results to the historical data for these specimens can reveal drift that may not yet be apparent in daily controls.
- Documentation and Action: Any trends or shifts triggering a rule violation must be investigated. Root causes may include a deteriorating reagent lot, a change in antigen retrieval solution pH, or instrument performance issues. All investigations and corrective actions must be documented.
Table 2: Comparison of Ongoing QC Activities
| Activity | Primary Goal | Key Regulatory Driver | Minimum Recommended Frequency | Core Experimental Design |
|---|---|---|---|---|
| Proficiency Testing | External verification of accuracy | CLIA Mandate | Twice yearly | Split-sample comparison with reference lab (≥5 samples) |
| Lot-to-Lot Comparison | Ensure consistency after reagent change | CAP Guideline [2] | With every new lot | Staining comparison with old lot (1 positive, 1 negative) |
| Assay Drift Monitoring | Detect gradual performance degradation | CLIA & CAP Requirements | Continuous (via controls) & Periodic | Longitudinal tracking of control values on statistical charts |
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of these QC strategies relies on a set of essential materials. The following table details key research reagent solutions and their functions in ongoing QC.
Table 3: Essential Materials for IHC Quality Control
| Material / Solution | Function in QC Protocols |
|---|---|
| Characterized Tissue Microarray (TMA) | Serves as a multi-tissue control for daily runs, lot-to-lot comparisons, and proficiency testing. Contains cores of known positive and negative tissues for multiple markers. |
| Cell Line Blocks | Provide a consistent, renewable source of standardized material with known antigen expression levels, ideal for monitoring calibration drift. |
| Stable Control Slides | Pre-stained or ready-to-stain slides used for daily monitoring of assay consistency and detection of major deviations. |
| Polymer-Based Detection System | A modern, high-sensitivity detection method that reduces background from endogenous biotin, a common variable in QC [61]. |
| Reference Laboratory Service | An accredited partner laboratory for split-sample testing, which is the foundation of alternative proficiency testing. |
| Statistical Process Control Software | Tools for creating control charts, tracking trends, and applying statistical rules to objective data for early detection of assay drift. |
A rigorous, multi-layered approach to ongoing quality control is the bedrock of reliable IHC testing in a CLIA-regulated environment. By systematically implementing proficiency testing, lot-to-lot comparisons, and assay drift monitoring, laboratories can create a safety net that ensures the long-term analytical validity of their assays. These activities are not isolated tasks but are deeply interconnected, forming a comprehensive quality management system. Adherence to updated evidence-based guidelines, such as the 2024 CAP guideline, provides a clear and effective roadmap for meeting regulatory requirements. Ultimately, this diligent commitment to QC directly translates to improved patient care by ensuring that diagnostic, prognostic, and predictive IHC results remain accurate, reproducible, and clinically trustworthy over time.
Advanced Validation and Global Compliance: From Predictive Markers to Commercialization
Validating Predictive Biomarkers with Distinct Scoring Systems (e.g., PD-L1, HER2)
Immunohistochemistry (IHC) serves as a cornerstone technique in diagnostic pathology and drug development, enabling the visualization of specific protein biomarkers within tissue architectures [62] [63]. The validation of predictive biomarkers, such as PD-L1 and HER2, is critically important as their expression levels directly inform patient selection for targeted therapies [63]. Unlike simple positive/negative assays, these biomarkers often employ distinct scoring systems that vary by tumor type, clinical context, and even the specific therapeutic drug involved [1] [64]. This complexity necessitates rigorous analytical validation to ensure that the assay reliably and reproducibly categorizes patients.
The Clinical Laboratory Improvement Amendments (CLIA) establish federal standards for all U.S. facilities testing human specimens for health assessment, diagnosis, or treatment [3]. For laboratories, CLIA validation forms the foundational requirement, though the pathway does not specify precisely how to satisfy each performance study [3]. The College of American Pathologists (CAP) provides more specific guidance, with its 2024 guideline update affirming and expanding principles to ensure accuracy and reduce variation in IHC laboratory practices [1]. This guide objectively compares the validation approaches and scoring complexities for PD-L1 and HER2, two biomarkers with distinct and critical roles in modern oncology.
Comparative Analysis of Scoring Systems
PD-L1 Scoring Systems
PD-L1 expression assessment is complicated by the existence of multiple FDA-approved assays, each with potentially different scoring algorithms that consider different cell types [64]. The scoring method directly impacts the reported positivity rate and, consequently, patient identification.
Table 1: Comparison of PD-L1 Scoring Methods in Breast Cancer Using the 22C3 Assay
| Scoring Method | Cell Population Assessed | Positive Rate in Entire Cohort (n=496) | Positive Rate in TNBC Subset | Key Clinical Correlation |
|---|---|---|---|---|
| Tumor Cell (TC) Score | Membranous staining on viable invasive tumor cells | 10% | 16% | Shows trend for worse survival in some subgroups [64] |
| Immune Cell (IC) Score | Proportion of tumor-infiltrating immune cells staining for PD-L1 | 16% | 31% | Most consistently associated with worse overall survival, especially in patients with neoadjuvant chemotherapy [64] |
| Combined Positive Score (CPS) | Combination of PD-L1 staining on tumor cells, lymphocytes, and macrophages | 20% | 35% | Most sensitive method to identify PD-L1-positive breast cancer [64] |
The choice of scoring method is not merely academic; it has real-world implications. Research indicates that the IC score demonstrates the most consistent prognostic value, being significantly associated with worse overall survival in patients receiving neoadjuvant chemotherapy [64]. Furthermore, in HER2-positive breast cancer, PD-L1 positivity (on cancer cells) is significantly correlated with higher levels of tumor-infiltrating lymphocytes (TILs) and a dramatically improved pathological complete response (pCR) rate to neoadjuvant chemotherapy combined with trastuzumab (86.4% in PD-L1-positive vs. 61.5% in PD-L2-negative patients) [65].
HER2 Scoring Systems
The HER2 scoring paradigm has evolved from a binary (positive/negative) system to a more nuanced continuum, particularly with the emergence of the "HER2-low" category, defined as IHC 1+ or IHC 2+ with negative in situ hybridization (ISH) [66]. This category accounts for a substantial proportion—approximately 40%—of all breast cancers [66].
Table 2: Comparison of HER2 Expression Categories in Breast Cancer
| HER2 Category | IHC Result | ISH Result | Prevalence | Response to Traditional Anti-HER2 Therapy | Response to Novel ADCs (e.g., Trastuzumab Deruxtecan) |
|---|---|---|---|---|---|
| HER2-negative | IHC 0 | Not applicable | ~60% of breast cancers [66] | No | No |
| HER2-low | IHC 1+ | Negative | ~40% of breast cancers [66] | No | Yes [66] |
| HER2-positive | IHC 2+ | Positive | ~15-20% of breast cancers | Yes | Yes |
| IHC 3+ | Not required (Positive) |
Critical differences in biology and treatment response exist between these categories. Studies show that patients with HER2-0 breast cancer have higher pCR rates after neoadjuvant chemotherapy compared to those with HER2-low tumors (30.1% vs. 18.1%, p < 0.0001) [66]. However, the development of novel antibody-drug conjugates (ADCs) has improved outcomes for the HER2-low population, expanding the applicability of HER2-targeted drugs [66].
Validation Requirements and Regulatory Frameworks
CLIA and CAP Guidelines
Validating IHC assays for biomarkers with multiple scoring systems introduces unique challenges. The 2024 CAP guideline update provides critical, evidence-based recommendations for this process [1]. A cornerstone principle is that laboratories must separately validate and verify each unique assay-scoring system combination used in clinical practice [1]. For example, if a laboratory uses one PD-L1 antibody but applies both the CPS and IC scoring algorithms for different clinical indications, each algorithm must undergo independent validation.
The updated CAP guidelines have also harmonized the validation requirements for all predictive IHC markers, setting a uniform 90% concordance requirement for all IHC assays, a standardization that applies to HER2, ER, PR, and PD-L1 alike [1]. Furthermore, the guidelines address validation on cytology specimens, which may use different fixatives. They stipulate that when using alternative fixatives, a separate validation with a minimum of 10 positive and 10 negative cases is required to account for variable sensitivity [1].
Advanced Regulatory Strategy
For assay commercialization, particularly for companion diagnostics (CDx), CLIA validation is only the first step. Regulatory pathways for in vitro diagnostics (IVDs) in the U.S. and European Union (EU) are distinct and require strategic planning.
Table 3: Comparison of US and EU Regulatory Pathways for IHC Assays
| Aspect | United States (FDA) | European Union (IVDR) |
|---|---|---|
| Regulatory Authority | Food and Drug Administration (FDA) | Notified Body |
| CDx Classification | Class II or Class III | Uniformly Class C |
| Key Submission Type | Pre-market Approval (PMA), de novo | Technical Dossier under Annex XIV |
| Quality System | 21 CFR Part 820 (transitioning to include ISO 13485) | ISO 13485 |
| Approval Timeline | 12-24 months | 12-18 months for CE marking |
| Clinical Trial Requirement | SRD Q-submission or IDE often required | Annex XIV submission to national competent authority |
A critical step in the U.S. pathway is the Study Risk Determination (SRD). When an assay is used for prospective patient stratification or clinical decision-making, an SRD must be performed to evaluate if an Investigational Device Exemption (IDE) is required [3]. This risk assessment can be submitted to the FDA via a Q-submission, or determined by an Institutional Review Board (IRB) [3]. For global development, manufacturers are advised to build comprehensive validation packages from the outset that simultaneously satisfy both CLIA/CLSI standards and EU IVDR requirements under ISO 13485, thus streamlining the process [3].
Experimental Protocols for Validation
IHC Staining Procedure
A robust and reproducible IHC protocol is the foundation of any validated assay. The following steps outline the core procedure, with attention to critical variables that impact assay performance [62] [63].
- Sample Preparation: Tissue samples are fixed, typically in formalin, and embedded in paraffin (FFPE) to preserve morphology [63]. Sections are cut to a thickness of 4-5 µm and mounted on charged slides to ensure adhesion [62].
- Deparaffinization and Rehydration: Slides are treated with xylene to remove paraffin, followed by a series of ethanol washes of decreasing concentration to rehydrate the tissue [63].
- Antigen Retrieval: This critical step reverses formaldehyde-induced cross-links to expose epitopes. Heat-Induced Epitope Retrieval (HIER) using a citrate or EDTA-based buffer in a microwave, pressure cooker, or steamer is most common [63]. The method must be optimized for each antibody [62].
- Blocking: Endogenous enzymes (e.g., peroxidase) are blocked to prevent false-positive signals [62]. A protein block (e.g., serum or BSA) is applied to reduce non-specific antibody binding [63].
- Antibody Application:
- Primary Antibody: A monoclonal or polyclonal antibody specific to the target (e.g., PD-L1 clone 22C3 or HER2 clone 4B5) is applied at an optimized concentration and incubation time [62] [64]. Monoclonal antibodies are preferred for superior specificity [62].
- Secondary Antibody & Detection: An enzyme-labeled (e.g., HRP) secondary antibody is applied, followed by a chromogen substrate like DAB (brown) or Fast Red (red) [62] [63]. Polymer-based detection systems can offer enhanced sensitivity [63].
- Counterstaining and Mounting: A counterstain, typically hematoxylin (blue), is applied to visualize cell nuclei and tissue architecture [67]. The stained sections are then permanently mounted under a coverslip for microscopic evaluation [63].
Validation Study Design
The CAP guideline outlines several acceptable comparators for validation study design, listed here from most to least stringent [1]:
- Comparison to IHC results from cell lines with known protein amounts ("calibrators").
- Comparison with a non-IHC method (e.g., flow cytometry, FISH).
- Comparison with results from another laboratory using a validated assay.
- Comparison with prior testing of the same tissues in the same laboratory.
- Comparison with expected architectural and subcellular localization of the antigen.
For initial verification of an unmodified FDA-approved/cleared assay, the CAP guideline provides explicit requirements to streamline the process [1]. The validation must account for pre-analytical variables; laboratories are advised to run the validation set on different instruments over several days and with different personnel to incorporate real-world variability [1].
The Scientist's Toolkit
Successful validation and application of predictive IHC assays rely on a suite of essential reagents and tools.
Table 4: Essential Research Reagent Solutions for IHC Validation
| Reagent / Tool | Function | Key Considerations |
|---|---|---|
| Primary Antibodies | Specifically binds to the target antigen (e.g., PD-L1, HER2) | Select based on clone specificity (e.g., 22C3 for PD-L1); prefer monoclonal for reproducibility; verify with specification sheets [62] [64]. |
| Detection System | Visualizes the antigen-antibody complex via enzymatic reaction | Polymer-based systems offer enhanced sensitivity; choose HRP or AP enzymes matched to chromogen [62] [63]. |
| Chromogens | Produces an insoluble colored precipitate at the antigen site | DAB (brown) is most common and permanent; AEC (red) provides contrast; select for compatibility with counterstain [62] [63]. |
| Counterstains | Provides contrast by staining non-target structures (e.g., nuclei) | Hematoxylin (blue) is standard; Nuclear Fast Red (red) or Methyl Green (green) are alternatives for color contrast [67]. |
| Control Cell Lines & Tissues | Serves as positive and negative controls for assay performance | Use cell lines with known antigen expression or well-characterized tissue controls; essential for run validation [1] [62]. |
| Antigen Retrieval Buffers | Unmasks epitopes obscured by tissue fixation | Citrate (pH 6.0) and EDTA/TRIS (pH 9.0) are common; optimal pH and buffer must be determined for each antibody [62] [63]. |
Visualizing Workflows and Relationships
Biomarker Validation and Regulatory Pathway
PD-L1 Scoring Methodologies
The validation of predictive biomarkers like PD-L1 and HER2, with their distinct and sometimes multiple scoring systems, represents a significant complexity in modern diagnostic pathology. A successful validation strategy must be multi-faceted, encompassing robust analytical techniques, strict adherence to updated CAP guidelines requiring separate validation of each scoring algorithm, and a forward-looking regulatory plan for global commercialization. As the field evolves with the recognition of new categories like HER2-low and the refinement of immune cell scoring for PD-L1, the principles of rigorous validation, including the use of proper controls and a thorough understanding of the clinical context, remain paramount for ensuring accurate patient stratification and the success of targeted therapies.
Harmonizing Validation Requirements for All Predictive Markers to 90% Concordance
In the field of diagnostic pathology, immunohistochemistry (IHC) serves as a critical tool for detecting predictive biomarkers that guide therapeutic decisions, particularly in oncology. The analytical validation of these assays ensures their reliability, accuracy, and clinical utility. Historically, validation requirements varied significantly between different predictive markers, creating a complex regulatory environment for laboratories. The 2024 update to the "Principles of Analytic Validation of Immunohistochemical Assays" by the College of American Pathologists (CAP) has introduced a significant harmonization by establishing a uniform 90% concordance requirement for all predictive IHC assays, replacing previous variable standards that existed for markers such as ER, PR, and HER2 [1]. This change represents a paradigm shift in laboratory medicine, streamlining validation processes while maintaining rigorous quality standards essential for clinical decision-making.
The harmonization to 90% concordance across all predictive markers addresses the growing complexity of IHC testing in modern pathology practice, which now includes challenging assays like PD-L1 and HER2 with distinct scoring systems that vary by tumor site and clinical indication [1]. This guideline update, developed through a systematic review of the medical literature, provides a standardized framework that helps reduce variation in IHC laboratory practices while ensuring analytical accuracy. For researchers and drug development professionals, understanding these updated requirements is essential for developing robust biomarker assays that meet regulatory standards across multiple jurisdictions, facilitating more efficient translational research and diagnostic commercialization.
Comparative Analysis of Validation Standards
Evolution of Concordance Requirements
The transition to harmonized validation standards represents a significant milestone in standardizing IHC practices. The table below compares key aspects of validation requirements before and after the 2024 guideline update:
Table 1: Comparison of IHC Validation Requirements Before and After Harmonization
| Validation Aspect | Pre-2024 Requirements | 2024 Harmonized Requirements |
|---|---|---|
| Concordance Threshold for Predictive Markers | Variable requirements for different markers (e.g., ER, PR, HER2) | Uniform 90% concordance for all predictive markers [1] |
| Validation Cases for Predictive Markers | 20 positive and 20 negative cases [15] | 20 positive and 20 negative cases maintained [15] |
| Validation Cases for Non-Predictive Markers | 10 positive and 10 negative cases [15] | 10 positive and 10 negative cases maintained [15] |
| Assay-Scoring System Validation | Not explicitly addressed | Separate validation required for each assay-scoring system combination [1] |
| Cytology Specimen Validation | Limited specific guidance | Minimum 10 positive and 10 negative cases for alternative fixatives [1] |
Implementation Framework for Harmonized Standards
The harmonized validation requirements provide laboratories with a clear framework for assay implementation while addressing previously unmet needs. A critical advancement in the updated guideline is the explicit requirement for laboratories to separately validate each assay-scoring system combination, particularly relevant for predictive markers like PD-L1 and HER2 that employ different scoring systems based on tumor site and type [1]. This specificity ensures that validation accurately reflects clinical use conditions, especially important for companion diagnostics used in therapeutic decision-making.
For cytology specimens, the updated guideline introduces specific validation requirements recognizing the analytical differences between traditional formalin-fixed, paraffin-embedded tissues and alternative fixatives commonly used in cytology laboratories [1]. The guideline mandates separate validations with a minimum of 10 positive and 10 negative cases for IHC performed on specimens fixed in alternative fixatives, addressing the variable sensitivity observed with these preparation methods [1]. This represents a conditional recommendation acknowledging the added burden to laboratories while ensuring assay reliability across specimen types.
Experimental Validation Methodologies
Core Validation Protocol Design
Implementing the harmonized 90% concordance requirement necessitates rigorous experimental approaches. The validation process for IHC assays involves multiple critical stages, each with specific methodological considerations:
Table 2: Key Stages in IHC Assay Validation and Verification
| Validation Stage | Key Activities | Methodological Considerations |
|---|---|---|
| Pre-Validation Investigation | Clinical utility assessment, literature review, resource evaluation | Review primary literature, NordiQC assessments, CAP proficiency testing data; confirm antibody clone, dilution, and protocol parameters [15] |
| Optimization | Protocol establishment, staining pattern confirmation | Select appropriate tissue for optimization; follow manufacturer protocol; adjust conditions iteratively until optimal staining achieved [15] |
| Validation/Verification | Performance confirmation, concordance assessment | Stain predetermined number of known positive/negative cases; include expression level range; compare to validated method [15] |
| Analysis | Concordance calculation, discrepancy investigation | Calculate overall concordance; scrutinize discordant results; assess sensitivity/specificity based on error patterns [15] |
| Ongoing Monitoring | Quality assurance, proficiency testing | Track positive/negative rates; compare with benchmarks; perform lot-to-lot comparisons; enroll in proficiency testing [15] |
For the core validation study comparing a new assay against a comparator method, the CAP guideline provides a hierarchy of acceptable comparators, listed here from most to least stringent: comparison to IHC results from cell lines with known protein amounts ("calibrators"); comparison with non-immunohistochemical methods like flow cytometry or FISH; comparison with results from another laboratory using a validated assay; comparison with prior testing of the same tissues in the same laboratory; comparison with testing from a clinical trial laboratory; comparison with expected architectural and subcellular localization; comparison against percent positive rates in published clinical trials; and comparison with formal proficiency testing challenges [1].
Specialized Methodologies for Predictive Markers
Predictive biomarkers requiring specialized scoring systems demand particular attention in validation study design. For example, ALK IHC validation in non-small cell lung cancer demonstrates how antibody clone selection significantly impacts assay performance. The D5F3 and 5A4 clones show superior performance (75.9-100% sensitivity and 95.0-100% specificity) compared to the ALK1 clone (44.4-90% sensitivity and 67.6-97.8% specificity) [68]. This highlights the importance of antibody selection in meeting the 90% concordance threshold.
The following diagram illustrates the complete validation workflow for IHC assays, incorporating both initial validation and ongoing monitoring requirements:
IHC Assay Validation Workflow: This diagram outlines the comprehensive process for validating immunohistochemistry assays, from initial investigation through ongoing quality monitoring, incorporating the harmonized 90% concordance requirement.
Research Reagent Solutions for IHC Validation
Successful implementation of the harmonized validation standards requires access to appropriate research reagents and materials. The following table details essential components for IHC assay validation:
Table 3: Essential Research Reagents for IHC Assay Validation
| Reagent Category | Specific Examples | Function in Validation |
|---|---|---|
| Validated Antibody Clones | D5F3, 5A4 for ALK; multiple clones for PD-L1 [68] | Detect target antigens with established performance characteristics; clone selection critical for sensitivity/specificity |
| Control Tissues | FFPE cell lines with known antigen expression; multi-tissue blocks [1] [15] | Provide known positive and negative controls for validation studies; ensure consistent assay performance |
| Antigen Retrieval Systems | pH-specific buffers; enzymatic retrieval solutions | Expose target epitopes masked by formalin fixation; critical for assay sensitivity |
| Detection Systems | Polymer-based detection; chromogens | Amplify signal while minimizing background; impact assay sensitivity and specificity |
| Platform-Specific Reagents | Autostainer reagents; buffer solutions | Ensure consistency across testing platforms; maintain assay reproducibility |
| Reference Materials | Commercial control slides; proficiency testing materials | Provide external standardization; verify ongoing assay performance |
The selection of appropriate antibody clones deserves particular emphasis, as clone performance significantly impacts the ability to achieve the 90% concordance threshold. For example, in ALK IHC validation, the D5F3 and 5A4 clones demonstrate significantly better performance characteristics (sensitivity 75.9-100%, specificity 95.0-100%) compared to the ALK1 clone (sensitivity 44.4-90%, specificity 67.6-97.8%) [68]. Similar considerations apply to PD-L1 IHC, where different clones may demonstrate varying performance across tumor types. Utilizing external quality assessment data from organizations like NordiQC and CAP proficiency testing programs provides valuable clone-specific performance data to guide selection [15].
Regulatory and Commercialization Pathways
Navigating Multi-Jurisdictional Requirements
The harmonized 90% concordance standard exists within a complex regulatory framework that varies significantly across jurisdictions. In the United States, IHC assays may follow different pathways depending on their intended use and modification status. Laboratory-developed tests (LDTs) and modified FDA-cleared/approved tests require full validation, while unmodified FDA-cleared/approved assays typically require verification [15]. The U.S. FDA classifies IHC reagents and kits as class II devices under 21 CFR 864.1860, with special controls outlined in the guidance for submission of IHC applications [41].
For global commercialization, understanding the differences between U.S. and European Union requirements is essential. The EU framework centers around the medical purpose of the assay and risk assessment based on intended use, with companion diagnostics uniformly classified as Class C devices under the In Vitro Diagnostic Regulation (IVDR) [3]. This contrasts with the U.S. system where companion diagnostics may be classified as either Class II or Class III devices [3]. These regulatory differences necessitate careful planning for parallel validation strategies that satisfy both CLIA standards and international requirements under ISO 13485 and good clinical laboratory practice guidelines [3].
Strategic Implementation for Drug Development
For researchers and drug development professionals, the harmonized validation standards create both opportunities and challenges. The standardized 90% concordance requirement streamlines assay development across multiple biomarker programs, potentially reducing development timelines. However, the requirement for separate validation of each assay-scoring system combination adds complexity for biomarkers like PD-L1 that have multiple clinical interpretations based on tumor type and therapeutic context [1].
Commercialization of companion diagnostics requires careful regulatory planning, with the FDA favoring a modular pre-market approval process for companion diagnostics, with each module reviewed independently [3]. The overall timeline for review is approximately 12 to 24 months in the U.S., while the EU process follows a different timeline with an estimated 12 to 18 months required for CE marking under IVDR [3]. Understanding these timelines is crucial for coordinating diagnostic and therapeutic development, particularly for targeted therapies where diagnostic availability is essential for treatment decisions.
The harmonization of validation requirements for all predictive IHC markers to 90% concordance represents significant progress in standardizing laboratory practices while maintaining rigorous quality standards. This harmonization, coupled with specific guidance for complex assays with multiple scoring systems and alternative specimen types, provides a robust framework for developing reliable predictive biomarker assays. For researchers and drug development professionals, understanding these requirements is essential for successful translational research and diagnostic commercialization. As the field continues to evolve with new biomarkers and technologies, these harmonized standards provide a foundation for ensuring assay reliability across laboratories and platforms, ultimately supporting more precise and effective patient care.
For researchers and drug development professionals working with immunohistochemistry (IHC) assays, navigating the regulatory landscape is crucial for successful clinical implementation and commercialization. The Clinical Laboratory Improvement Amendments (CLIA) and the Food and Drug Administration's Premarket Approval (PMA) represent two distinct regulatory pathways with fundamentally different data package requirements [69] [3]. CLIA establishes quality standards for laboratory testing processes, focusing on analytical validation to ensure tests produce reliable and reproducible results within a single laboratory [69] [70]. In contrast, PMA is the FDA's most stringent review process for Class III medical devices, which includes high-risk tests. This pathway requires a comprehensive scientific and regulatory review to evaluate the safety and effectiveness of the device, demanding extensive clinical data to provide reasonable assurance of its safety and effectiveness for its intended use [71] [72]. Understanding the differences in data requirements, experimental protocols, and strategic implications is essential for planning the development and validation of IHC assays.
Core Concept Comparison: CLIA vs. PMA
The following table outlines the fundamental distinctions between these two regulatory frameworks.
Table 1: Fundamental Differences Between CLIA Validation and Premarket Approval (PMA)
| Aspect | CLIA Validation | PMA (Premarket Approval) |
|---|---|---|
| Governing Authority | Centers for Medicare & Medicaid Services (CMS) [69] | U.S. Food and Drug Administration (FDA) [71] |
| Primary Focus | Laboratory quality standards and analytical test performance [69] [70] | Device safety and effectiveness for its intended use [71] |
| Regulatory Scope | Regulates the laboratory's testing process [69] | Regulates the medical device (test) itself [71] |
| Intended Use | Often for specialized, rare, or in-house tests (LDTs) [69] | For commercial distribution of Class III devices [71] |
| Evidence Standard | Analytical validity (accuracy, precision, reportable range) [70] [3] | Valid scientific evidence of safety & effectiveness, including clinical utility [71] [72] |
| Key Outcome | CLIA certification for the laboratory to perform the test [69] | FDA approval for the device to be marketed in the U.S. [71] |
Data Package Requirements: A Detailed Breakdown
The data packages for CLIA and PMA differ significantly in depth, breadth, and the nature of the required evidence.
CLIA Validation Data Requirements
CLIA validation focuses on establishing the analytical performance of the test. The data package demonstrates that the test meets specific performance standards before patient results are reported [70]. The key components are derived from method validation experiments.
Table 2: Core Data Requirements for CLIA Validation of a Non-Waived Test
| Performance Characteristic | Experimental Protocol & Minimum Data Points | Acceptance Criteria |
|---|---|---|
| Precision (Random Error) | Replication experiment: A minimum of 20 replicate determinations on at least two levels of control materials [70]. | Observed imprecision (e.g., standard deviation, coefficient of variation) is judged against allowable limits based on medical requirements [70]. |
| Accuracy (Systematic Error) | Comparison of methods experiment: A minimum of 40 patient specimens analyzed by both the new method and an established comparison method [70]. | The observed inaccuracy (bias) is compared to a defined quality standard, such as CLIA proficiency testing criteria [70]. |
| Reportable Range | Linearity experiment: A minimum of 5 specimens with known or assigned values, analyzed in triplicate [70]. | Demonstrates the range of analyte values over which the test provides accurate and precise results [70]. |
| Analytical Sensitivity/Specificity | Interference and recovery experiments; detection limit experiments. Testing of common interferents (e.g., lipemia, hemolysis). For detection limit, a "blank" and a "spiked" specimen are each analyzed 20 times [70] [3]. | Verifies the test's ability to correctly detect the target analyte and resist interference from other substances [70] [3]. |
| Reference Range Verification | Transference of the manufacturer's reference range or establishment of a laboratory-specific range, verifying appropriateness for the patient population [70]. | The reference interval (normal range) is confirmed to be suitable for the laboratory's patient population [70]. |
PMA Data Requirements
A PMA application is a comprehensive scientific and regulatory submission that must provide valid scientific evidence for the safety and effectiveness of the device [71] [72]. The data requirements are extensive and multi-faceted.
Table 3: Core Data Requirements for a Premarket Approval (PMA) Application
| Data Module | Required Content & Studies | Regulatory Standards |
|---|---|---|
| Non-Clinical Studies | Microbiology, toxicology, immunology, biocompatibility, stress, wear, and shelf life testing [72]. Data must demonstrate analytical validity, often exceeding CLIA-level rigor and scope [3]. | Must be conducted in compliance with Good Laboratory Practice (GLP) regulations, 21 CFR Part 58 [72]. |
| Clinical Investigations | Study protocols, safety and effectiveness data, adverse reactions, device failures, patient information, statistical analyses, and copies of individual subject report forms for subjects who died or did not complete the study [72]. | Investigations must comply with regulations for Institutional Review Board (IRB) approval (21 CFR 56), Informed Consent (21 CFR 50), and Investigational Device Exemptions (IDEs, 21 CFR 812) [72]. |
| Manufacturing Information | A complete description of the methods, facilities, and controls used in manufacturing, processing, packing, and storage [72]. | Must adhere to the Quality System Regulation (QSR), 21 CFR Part 820, which outlines good manufacturing practices [3] [72]. |
| Labeling | Copies of all proposed labeling, including instructions for use [72]. | Labeling must be adequate for the device's intended use and must not be false or misleading [72]. |
| Bibliography | A compilation of all published reports concerning the safety or effectiveness of the device [72]. | Must include both supportive and adverse reports known to the applicant [72]. |
Figure 1: Decision workflow for CLIA validation versus PMA pathway, highlighting different data packages and outcomes.
Experimental Protocols for Key Studies
Protocol for a CLIA Comparison of Methods Experiment
This experiment is critical for estimating the inaccuracy or systematic error of a new method (test method) compared to an established one (comparison method) [70].
- Objective: To estimate the systematic error (bias) of the test method.
- Specimen Requirements: A minimum of 40 patient specimens should be analyzed. The specimens should cover the entire reportable range of the test and reflect the laboratory's patient population [70].
- Procedure: Each patient specimen is analyzed by both the test method and the comparison method. The testing should be performed within a time frame that ensures the stability of the specimens (typically within 2-4 hours). The order of analysis should be randomized to avoid systematic bias.
- Data Analysis: Results are plotted using a scatter plot or a difference plot (Bland-Altman). Statistical analyses, such as linear regression and calculation of the mean difference (bias), are performed.
- Acceptance Criteria: The observed bias and its confidence interval are compared against predefined quality specifications, such as the CLIA proficiency testing allowable total error limits or biologic variation-based goals [70].
Protocol for a PMA Clinical Investigation
A PMA clinical investigation is designed to demonstrate the clinical validity and utility of the device.
- Objective: To provide valid scientific evidence that the device is safe and effective for its intended use in the target population [71] [72].
- Study Design: Typically a multi-center, prospective study. The protocol must be approved by an Institutional Review Board (IRB) and, for significant risk devices, an Investigational Device Exemption (IDE) must be in place [72].
- Subject Selection: Clearly defined inclusion and exclusion criteria, study population demographics, and sample size justification based on statistical power calculations.
- Procedure: The device is used according to its intended use and instructions for use. Outcomes are measured against a reference standard or clinically relevant endpoints.
- Data Collected: Safety and effectiveness data, all adverse reactions and complications, device failures, patient discontinuation information, and tabulations of data from all individual subject reporting forms [72].
- Statistical Analysis: Comprehensive statistical analysis of the primary and secondary endpoints to establish safety and effectiveness.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for developing and validating IHC assays, particularly in a regulated environment.
Table 4: Key Research Reagent Solutions for IHC Assay Validation
| Reagent/Material | Critical Function in Validation | Considerations for CLIA/PMA |
|---|---|---|
| Primary Antibodies | Specifically bind to the target biomarker (antigen). The core reagent determining test specificity. | For PMA, must be fully characterized (source, clone, specificity) and manufactured under controlled conditions. ASRs require user validation [73]. |
| Control Cell Lines/Tissues | Provide known positive and negative samples for establishing test performance (sensitivity, specificity) [73]. | Well-characterized controls are essential for both CLIA and PMA. For PMA, their provenance and stability data are critical. |
| Detection Systems | Amplify the primary antibody signal for visualization (e.g., polymer-based enzymatic detection). | The sensitivity and dynamic range of the detection system must be validated as part of the analytical sensitivity experiments [70]. |
| Antigen Retrieval Solutions | Unmask hidden epitopes in formalin-fixed, paraffin-embedded (FFPE) tissue sections. | The consistency and composition of these solutions can affect staining reproducibility and must be controlled. |
| Analyte-Specific Reagents (ASRs) | Antibodies or probes used in LDTs. Regulated by FDA but the test's performance is established by the lab [73]. | For CLIA LDTs, the laboratory assumes responsibility for the full validation of the test using the ASR [69] [73]. |
Strategic Implications for Drug Development Professionals
The choice between CLIA and PMA pathways has profound strategic implications.
- Timeline and Cost: The CLIA pathway offers a faster and less costly route to implementation, primarily involving analytical validation. The PMA pathway is a lengthy and expensive process, often taking 12-24 months for FDA review and requiring extensive clinical trials and manufacturing controls [3].
- Flexibility vs. Standardization: CLIA offers flexibility to customize and rapidly adapt tests for specific patient populations or emerging needs, such as during outbreaks [69]. PMA leads to a standardized product with consistent performance across multiple sites, facilitating broader commercial adoption [69].
- Regulatory Jurisdiction: For global development, note that the European Union has a different framework under the In Vitro Diagnostic Regulation (IVDR), where companion diagnostics are uniformly Class C. A global validation strategy must be planned to meet both U.S. (CLIA/PMA) and EU (IVDR) requirements in parallel [3].
- Risk-Based Decisions: The appropriate pathway is determined by the test's intended use. Tests for rare conditions, prospective patient stratification in clinical trials, or those used as investigational tools are often suited for the CLIA/LDT pathway. Tests intended as companion diagnostics or for widespread commercial sale to guide high-risk therapeutic decisions will require a PMA [69] [3].
Navigating the divergent regulatory pathways for In Vitro Diagnostic (IVD) devices in the United States (US) and European Union (EU) is a critical step for successful global market access. For Class C devices under the EU's In Vitro Diagnostic Regulation (IVDR)—a category that includes companion diagnostics (CDx) and high-risk tests like many cancer assays—understanding the distinct requirements of the US Food and Drug Administration (FDA) is essential [3]. Both regulatory systems are founded on a risk-based classification principle, but their approaches to demonstrating safety and performance differ significantly in procedure, oversight, and documentation [74] [75]. This guide provides a structured comparison to help researchers, scientists, and drug development professionals build an efficient and compliant global regulatory strategy for their IVD products, with a specific focus on the context of IHC assay validation.
Classification and Regulatory Authorities
The first major difference lies in the structure of the regulatory systems and how devices are classified. The US FDA and the EU IVDR use different classification models and are overseen by distinct authorities, which directly impacts the strategy for market entry.
The US FDA regulates IVDs as medical devices under the Code of Federal Regulations (CFR), including 21 CFR Part 809 for labeling [75]. The FDA's classification system has three categories: Class I (low risk), Class II (moderate risk), and Class III (high risk). Most Class C IVDs under IVDR would typically correspond to Class II or Class III devices under the FDA, potentially requiring a 510(k) or Premarket Approval (PMA) [3]. In contrast, the EU's IVDR features a four-class system: Class A (lowest risk), B, C, and D (highest risk) [75]. Classification rules are detailed in IVDR Annex VIII and are based on the device's intended purpose and the associated risk to patients and public health [75]. A key difference is that under the previous EU Directive (IVDD), only about 10-20% of IVDs required notified body intervention; under the IVDR, this figure has risen dramatically to approximately 80-90%, encompassing most Class C devices [74] [76].
The regulatory authorities involved also differ. In the US, the FDA serves as the central regulatory authority for premarket review and oversight [3]. In the EU, compliance is assessed by Notified Bodies, which are independent organizations designated by EU member states to conduct conformity assessments [74]. For companion diagnostics, the EU process also requires consultation with a competent authority or the European Medicines Agency (EMA) [3].
Table 1: Regulatory Frameworks and Classification
| Feature | US FDA | EU IVDR (Class C) |
|---|---|---|
| Governing Regulation | 21 CFR Parts 807, 820, 809, etc. [74] | Regulation (EU) 2017/746 (IVDR) [75] |
| Regulatory Authority | Food and Drug Administration (FDA) [3] | Notified Bodies (NBs) [74] |
| Risk Classification | Class I, II, III [75] | Class A, B, C, D [75] |
| Typical CDx Classification | Class II or III [3] | Class C [3] |
| Premarket Review Body | FDA Center for Devices and Radiological Health (CDRH) & Center for Drug Evaluation and Research (CDER) for CDx [76] | Notified Body, with consultation from a competent authority or EMA for CDx [3] |
Premarket Submission Pathways and Evidence Requirements
The journey to market approval involves different submission pathways and evidence requirements. The core of the EU's evidence is the Performance Evaluation (PE), while the US FDA focuses on premarket submission packages such as 510(k) or PMA.
For the EU IVDR, demonstrating conformity for a Class C device requires the creation and assessment of extensive technical documentation [74]. The cornerstone of this documentation is the Performance Evaluation Report (PER), which is the culmination of a continuous process that integrates three key pillars: scientific validity, analytical performance, and clinical performance [75]. This ongoing process is detailed in IVDR Annex XIII and requires regular updates throughout the device's lifecycle [74] [75]. The clinical evidence must be robust and specific, often requiring a Clinical Performance Study (CPS). It is important to note that applications for these studies must be submitted to the competent authority and ethics committee in each EU country where the study will run, which can add complexity to trial set-up [76].
In the US, the regulatory pathway depends on the device's classification. A 510(k) premarket notification is required if the device can be demonstrated to be substantially equivalent to a legally marketed predicate device [74] [75]. For higher-risk devices without a predicate, a De Novo classification may be pursued. For the highest-risk Class III devices, a Premarket Approval (PMA) is necessary, which typically requires clinical evidence demonstrating safety and effectiveness [74] [3]. The FDA's scrutiny of clinical data is rigorous, particularly for companion diagnostics, which are often reviewed under a modular PMA process [3].
Table 2: Premarket Submission and Evidence
| Requirement | US FDA | EU IVDR (Class C) |
|---|---|---|
| Core Evidence Concept | Premarket Submission (e.g., 510(k), PMA) [74] | Performance Evaluation (PE) & Report (PER) [75] |
| Clinical Evidence Basis | Clinical data from trials; reliance on predicate devices for 510(k) [74] | Clinical data & performance studies, following MEDDEV 2.7/1 Rev. 4 and IVDR Annex XIII [74] |
| Evidence Timeline | Focused on premarket review [74] | Continuous process throughout the device lifecycle [74] |
| Key Reporting Document | Premarket Submission Document (e.g., PMA Application) | Performance Evaluation Report (PER) [75] |
| Clinical Study Application | Investigational Device Exemption (IDE) for significant risk studies [3] | Annex XIV submission to national competent authorities & ethics committees [76] [3] |
Quality Management and Post-Market Surveillance
A robust Quality Management System (QMS) and vigilant post-market surveillance (PMS) are mandatory in both jurisdictions, yet the specific standards and reporting structures differ.
The QMS requirements are converging but are not yet identical. In the US, the FDA's Quality System Regulation (QSR) under 21 CFR Part 820 is the standard, which emphasizes process-based controls [74] [3]. It is important to note that the FDA is moving toward greater harmonization with international standards through the upcoming Quality Management System Regulation (QMSR), which will align more closely with ISO 13485 [74]. In the EU, certification to ISO 13485:2016 is mandatory and serves as a cornerstone of the QMS for device manufacturers [74]. Both regions also require the application of a risk management process, with the EU explicitly aligning with ISO 14971:2019 [74].
Post-market surveillance is an area of significant divergence. The EU IVDR imposes more structured and continuous post-market obligations than its US counterpart. Under IVDR, all manufacturers must implement a post-market surveillance system [75]. For Class C devices, this includes the submission of Periodic Safety Update Reports (PSURs), which summarize the results and conclusions of post-market data and specify any corrective actions [74] [75]. In the US, post-market controls are primarily focused on adverse event reporting under the Medical Device Reporting (MDR) regulation (21 CFR 803) [74] [75]. While the FDA also monitors the market, the EU's requirement for periodic, structured reports like the PSUR represents a more proactive and systematic approach to ongoing device monitoring [74].
Table 3: Quality and Post-Market Requirements
| Requirement | US FDA | EU IVDR (Class C) |
|---|---|---|
| QMS Standard | 21 CFR Part 820 (QSR), moving to ISO 13485 alignment via QMSR [74] | ISO 13485:2016 (mandatory) [74] |
| Risk Management | Required per 21 CFR 820.30, 820.100 [74] | Required per ISO 14971:2019 [74] |
| Post-Market Surveillance | Medical Device Reporting (MDR) for adverse events [74] | Structured PMS plan; Periodic Safety Update Report (PSUR) required [74] [75] |
| Vigilance Reporting | Reported to FDA [74] | Reported via EUDAMED database [74] |
| Unique Device Identification (UDI) | Required, stored in FDA's GUDID [74] | Required, stored in EUDAMED [74] |
Experimental Protocols for IHC Assay Validation
For IHC assays, particularly those intended as Class C IVDs or CDx, validation must be designed to meet the analytical performance requirements of both regulatory bodies. The following protocols are based on guidelines from the College of American Pathologists (CAP) and common standards recognized by both the FDA and EU Notified Bodies.
Analytical Validation for IHC Assays
Purpose: To establish and document the analytical performance characteristics of an IHC assay, ensuring it is reliable, reproducible, and fit for its intended clinical purpose [1] [3].
Methodology:
- Assay Definition: Precisely define the assay's intended use, including the target antigen, specimen types (e.g., FFPE tissues, cytology specimens), and scoring system [1].
- Sample Selection: Procure a sufficient number of well-characterized tissue specimens that represent the entire range of expected antigen expression (negative, weak, moderate, strong). The CAP guideline recommends a minimum of 10 positive and 10 negative cases for initial validation, though larger sample sizes may be needed for more complex assays [1].
- Comparator Selection: Choose an appropriate comparator method. CAP lists several options, ordered from most to least stringent [1]:
- Comparison to IHC results from cell lines with known protein levels ("calibrators").
- Comparison with a non-IHC method (e.g., flow cytometry, FISH).
- Comparison with results from testing the same tissues in another laboratory using a validated assay.
- Comparison with prior testing of the same tissues with a validated assay in the same laboratory.
- Precision/Reproducibility Testing:
- Intra-run Precision: Run the validation set of samples multiple times in the same batch by the same technologist.
- Inter-run Precision: Run the validation set over several days, using different reagent lots and different technologists.
- Inter-site Precision (for IVD kits): If the assay is intended for use as a kit across multiple laboratories, a multi-site reproducibility study is required [3].
- Accuracy and Concordance: Demonstrate a high level of concordance between the new assay and the chosen comparator method. The updated CAP guideline harmonizes the concordance requirement for predictive markers to ≥90% [1].
- Staining and Scoring: Perform IHC staining according to the established protocol. Scoring should be performed by qualified pathologists, ideally in a blinded manner.
- Data Analysis: Calculate performance metrics including positive/negative percent agreement, sensitivity, specificity, and the Cohen's kappa coefficient for inter-observer agreement.
Clinical Cutoff Validation (For CDx and Predictive Markers)
Purpose: To validate the clinical cutoff that will be used to determine patient stratification or treatment decisions [3].
Methodology:
- Retrospective Cohort Identification: Identify a retrospective cohort of patient samples with known clinical outcomes. The cohort must be well-annotated and representative of the intended-use population.
- IHC Testing and Scoring: Test all samples in the cohort using the fully analytically validated IHC assay. Pathologists should score the samples without knowledge of the clinical outcomes.
- Correlation with Clinical Endpoints: Correlate the IHC scores with relevant clinical endpoints, such as objective response rate (ORR) or progression-free survival (PFS), from the therapeutic clinical trial data.
- Statistical Analysis for Cutpoint Selection: Use pre-specified statistical methods (e.g., Receiver Operating Characteristic (ROC) analysis, MaxSelect method) to determine the assay cutoff that best discriminates between responders and non-responders to the therapy.
- Prospective Validation: The selected cutpoint should be prospectively validated in an independent patient cohort, often within the context of a pivotal Phase 2 or 3 clinical trial [3].
Workflow and Strategic Planning Diagrams
US FDA and EU IVDR Submission Workflow
Integrated Global Validation Strategy
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for conducting robust IHC assay validation studies that will meet regulatory scrutiny.
Table 4: Essential Research Reagent Solutions for IHC Validation
| Item | Function in Validation |
|---|---|
| Well-Characterized Tissue Microarray (TMA) | Serves as a standardized platform for staining optimization and intra-/inter-run precision testing. Contains multiple tissue types and known expression levels of the target antigen [1]. |
| Cell Line Controls (with known antigen expression) | Act as calibrators or internal controls for lot-to-lay consistency and analytical sensitivity. Cell lines with known negative, low, and high expression are critical [1]. |
| Primary Antibodies (and isotype controls) | The core reagent for specific antigen detection. Must be thoroughly characterized for specificity and optimal dilution. Isotype controls are essential for demonstrating staining specificity [1]. |
| Detection Kit with Chromogen | Amplifies the primary antibody signal for visualization. Performance (sensitivity, background) must be validated as part of the assay system. Different lots should be tested during validation [1]. |
| Antigen Retrieval Solutions | Used to unmask epitopes in FFPE tissue sections. The pH and method (heat-induced, enzyme-induced) are critical variables that must be standardized and controlled [1]. |
| Reference Standards | Well-defined control materials (e.g., commercially available validated control slides) used to demonstrate that the entire IHC system is performing within established parameters across multiple runs [1]. |
Transition Timelines and Action Plan
A critical consideration for the EU market is the IVDR transition timeline. While the IVDR became applicable in May 2022, transitional provisions have been extended for existing devices. For Class C devices that were self-declared under the previous IVDD, the deadline to place them on the market under the old certificate is now December 31, 2028, provided certain conditions are met [77] [78]. These conditions are stringent and require proactive planning:
- Quality Management System: Implement an IVDR-compliant QMS (based on ISO 13485) by May 26, 2025 [77] [78].
- Formal Application: Lodge a formal application with a Notified Body by May 26, 2026 [77] [78].
- Contract with NB: Sign a written agreement with the Notified Body by September 26, 2026 [78].
- No Significant Changes: The design and intended purpose of the device must not undergo significant changes [77].
Manufacturers are strongly advised not to delay their IVDR transition plans, as Notified Bodies face significant capacity constraints, and last-minute submissions risk delays [78].
Developing a successful global strategy for a Class C IHC assay demands a proactive and integrated approach. The key is to build a unified technical documentation base from the outset that can be tailored to meet the specific expectations of the FDA and EU Notified Bodies. This involves designing analytical and clinical studies to the highest common standard, which often means adhering to CLSI guidelines while operating under an ISO 13485-certified QMS [3].
The most efficient strategy is to plan for parallelism: conduct a single, comprehensive validation study that collects all necessary data for both jurisdictions simultaneously. By understanding the distinct requirements charted in this guide—from classification and evidence generation to post-market vigilance—teams can streamline their development efforts, mitigate regulatory risk, and accelerate the delivery of vital diagnostic tools to patients in both the US and EU markets.
Companion diagnostics (CDx) are essential tools in precision medicine, providing information that is critical for the safe and effective use of a corresponding therapeutic product. These in vitro diagnostic devices or imaging tools identify specific biomarkers to determine whether a patient is a suitable candidate for a particular targeted therapy. The development and commercialization of CDx represent a complex intersection of diagnostic and therapeutic innovation, requiring careful navigation of regulatory frameworks to ensure patient safety and clinical utility. In the United States, most companion diagnostics are classified as Class III medical devices by the Food and Drug Administration (FDA), necessitating approval through the Premarket Approval (PMA) pathway—the most rigorous regulatory standard for medical devices [3].
The PMA process requires manufacturers to provide valid scientific evidence demonstrating reasonable assurance that the device is safe and effective for its intended use. This evidence typically includes extensive analytical and clinical validation data, detailed device description, manufacturing information, and proposed labeling. For CDx developers, the regulatory landscape has evolved to include specialized approaches such as the Modular PMA, which allows for a more structured and potentially efficient review process by submitting well-delineated components of the complete application to the FDA as they are completed [79] [80]. This guide explores the intricacies of the Modular PMA process specifically for companion diagnostics, comparing it with traditional regulatory pathways and providing detailed methodological frameworks for successful commercialization.
Regulatory Framework Comparison: Traditional PMA vs. Modular PMA
The traditional PMA pathway requires submission of a complete application to the FDA at once, including all required volumes covering device description, non-clinical and clinical studies, manufacturing methods, and labeling. This approach is generally most suitable for devices that have already undergone extensive clinical testing and may have been approved in other markets with established medical device regulations [79]. The comprehensive single submission contains all elements necessary for FDA reviewers to evaluate the device's safety and effectiveness.
In contrast, the Modular PMA approach breaks down the complete application into well-delineated components that are submitted to the FDA as soon as each module is completed. This method begins with the submission of a "Shell" that outlines the plan for the entire submission, including descriptions of module contents and suggested timelines. The FDA review team works with applicants to develop a customized shell for each specific device [79] [80]. This approach is particularly beneficial for products in early stages of clinical development, as it allows for earlier FDA feedback and potentially more rapid final approval once all modules are submitted.
Table 1: Comparison of Traditional PMA and Modular PMA Pathways
| Feature | Traditional PMA | Modular PMA |
|---|---|---|
| Submission Structure | Single, comprehensive submission | Incremental module submissions |
| Ideal Use Case | Devices with completed clinical testing | Products in early clinical development |
| FDA Interaction | Feedback typically after complete submission | Ongoing feedback as modules are reviewed |
| Timeline Management | Fixed timeline after submission | Flexible pacing of module completion |
| Resource Allocation | Large resource deployment before submission | Distributed resources across development |
| Risk Management | Higher risk of major deficiencies | Early identification of potential issues |
| Regulatory Predictability | Lower until final submission | Higher through early FDA alignment |
The Modular PMA program requires that manufacturing and Bioresearch Monitoring (BIMO) information be submitted as standalone modules, rather than bundled with other disciplines. This modularization aligns with Quality Management System Regulation (QMSR) expectations and clarifies how reviewers will evaluate manufacturing and quality system content [81]. According to FDA guidance issued in January 2025, this approach allows manufacturers to receive timely feedback during the review process, potentially enabling more rapid closure when the final components are submitted [80].
Companion Diagnostic Validation Requirements and CLIA Compliance
Analytical Validation Standards for CDx
The analytical validation of companion diagnostics requires rigorous demonstration of assay performance characteristics, including accuracy, precision, sensitivity, specificity, and reproducibility. The College of American Pathologists (CAP) published updated guidelines in 2024 that affirm and expand on previous recommendations to ensure accuracy and reduce variation in immunohistochemistry (IHC) laboratory practices [1]. These guidelines include specific recommendations for validating IHC assays used as companion diagnostics, with particular attention to predictive markers with distinct scoring systems like PD-L1 and HER2.
For all IHC assays, including CDx, the updated CAP guidelines have harmonized validation requirements across different predictive markers, establishing a uniform 90% concordance requirement for all IHC assays, replacing previous variable concordance requirements for estrogen receptor, progesterone receptor, and HER2 IHC performed on breast carcinomas [1]. This standardization creates a consistent benchmark for assay performance regardless of the specific biomarker being detected.
CLIA Laboratory Requirements
While FDA approval addresses the commercial distribution of companion diagnostics, Clinical Laboratory Improvement Amendments (CLIA) regulations govern laboratory testing performance on human specimens. Laboratories developing laboratory-developed tests (LDTs) or implementing FDA-approved CDx must comply with CLIA standards, which saw significant updates in 2025 [82] [10]. These changes include:
- Stricter Proficiency Testing (PT) Criteria: Updated performance standards for various analytes, including newly regulated ones. For example, hemoglobin A1c is now a regulated analyte with a ±8% performance range set by CMS [82] [35].
- Updated Personnel Qualifications: Revised requirements for laboratory directors and staff, with certain degrees and "board eligibility only" no longer automatically qualifying individuals for specific roles [82] [10].
- Digital-Only Communication: CMS has phased out paper mailings in favor of exclusive electronic communication for critical notices [10].
- Announced Inspections: Accrediting bodies like CAP can now announce inspections up to 14 days in advance, requiring laboratories to maintain continuous inspection readiness [10].
Table 2: Key CLIA Proficiency Testing Requirements for 2025
| Category | Analyte/Test Example | 2025 CLIA Acceptance Criteria | Change from Previous Standard |
|---|---|---|---|
| Chemistry | Hemoglobin A1c | ±8% | Newly regulated analyte |
| Chemistry | Creatinine | ±0.2 mg/dL or ±10% (greater) | Improved from ±0.3 mg/dL or ±15% |
| Chemistry | HDL Cholesterol | ±20% TV or ±6 mg/dL (greater) | Improved from ±30% |
| Toxicology | Digoxin | ±15% or ±0.2 ng/mL (greater) | Newly regulated analyte |
| Endocrinology | Testosterone | ±20 ng/dL or ±30% (greater) | Newly regulated analyte |
| Hematology | Hemoglobin | ±4% | Improved from ±7% |
The relationship between FDA approval and CLIA compliance is particularly important for CDx commercialization. While FDA approval permits the device to be marketed, CLIA certification is required for laboratories to perform the testing. For CDx developers, understanding both regulatory frameworks is essential for successful implementation in clinical practice [3].
Modular PMA Process: Step-by-Step Workflow
Module Development and Submission Sequence
The Modular PMA process follows a structured sequence that allows for iterative development and review of application components. The process begins with early interaction with the FDA to establish the overall submission strategy and module definitions [79] [80].
The modular approach is particularly advantageous for companion diagnostics because it allows developers to align diagnostic development timelines with therapeutic development programs. The early feedback mechanism enables course correction throughout the development process rather than discovering significant issues only after a complete submission [79] [80]. This is especially valuable for complex CDx with novel biomarkers or technological platforms.
Manufacturing and BIMO as Standalone Modules
A critical aspect of the Modular PMA process for companion diagnostics is the requirement for manufacturing and Bioresearch Monitoring (BIMO) to be submitted as standalone modules. This separation from other disciplinary reviews provides clearer focus on quality system and manufacturing controls [81]. The manufacturing module must demonstrate compliance with Quality System Regulation (QSR) requirements, which are transitioning to the Quality Management System Regulation (QMSR) aligned with ISO 13485:2016, effective February 2, 2026 [81].
The BIMO module addresses compliance with regulations governing clinical investigations, ensuring the validity of data submitted in support of the PMA. For companion diagnostics, this includes verification that clinical studies were conducted properly and that the data generated reliably demonstrates the assay's clinical performance [81].
Experimental Design and Methodologies for CDx Validation
Analytical Validation Protocols
Robust analytical validation is foundational for companion diagnostics development. The experimental design must comprehensively characterize assay performance using appropriate clinical samples and controls. The 2024 CAP guidelines provide specific recommendations for IHC-based assays, which are commonly used as companion diagnostics [1].
For IHC assays with distinct scoring systems employed across different tumor types or clinical indications (e.g., HER2 with different scoring systems depending on tumor site), the CAP guidelines stipulate that laboratories should separately validate each assay-scoring system combination [1]. This requires discrete validation studies for each intended use scenario rather than extrapolating performance from one context to another.
Table 3: Key Experimental Parameters for IHC-Based CDx Analytical Validation
| Performance Characteristic | Experimental Methodology | Acceptance Criteria | Reference Standard |
|---|---|---|---|
| Accuracy/Concordance | Method comparison against reference standard | ≥90% positive/negative agreement | Clinical trial assay or validated reference method |
| Precision | Repeatability (within-run) and reproducibility (between-run, between-operator, between-day) | ≥95% concordance for reproducibility | Well-characterized positive and negative controls |
| Analytical Sensitivity | Limit of detection studies using cell lines or patient samples with known mutation status | Detection at established minimum input | Samples with known variant allele frequency |
| Analytical Specificity | Cross-reactivity with related antigens and interference from common specimen conditions | No significant cross-reactivity or interference | Samples with related antigens and interfering substances |
| Robustness | Deliberate variations in pre-analytical and analytical conditions | Consistent performance across variations | Samples tested under standard and modified conditions |
For CDx intended for use on cytology specimens that are not fixed identically to tissues used for initial validation, the CAP guidelines recommend separate validations with a minimum of 10 positive and 10 negative cases for each alternative fixative type [1]. This acknowledges the variable sensitivity of IHC assays performed on specimens with different fixation protocols compared with standard formalin-fixed, paraffin-embedded (FFPE) tissues.
Clinical Validation Study Designs
Clinical validation of companion diagnostics requires demonstration of the assay's ability to correctly identify patients who are likely to respond to the corresponding therapeutic product. The gold standard approach involves prospective clinical trials where patient eligibility is determined by the investigational CDx, with clinical outcomes correlated with test results.
Alternative approaches include:
- Retrospective analysis of archived specimens from previously conducted clinical trials
- Bridge studies demonstrating comparable performance to a previously validated assay
- Sample stratification based on biomarker status in umbrella or basket trial designs
For CDx targeting rare biomarkers, adaptive trial designs may be necessary to efficiently enroll sufficient numbers of biomarker-positive patients. In such cases, early engagement with the FDA is critical to ensure the proposed statistical plan and evidence generation strategy will support marketing authorization [3] [81].
Research Reagent Solutions for CDx Development
The development of robust companion diagnostics relies on carefully selected and qualified research reagents that ensure reproducibility and reliability. The following table outlines essential materials and their functions in CDx development and validation.
Table 4: Essential Research Reagents for Companion Diagnostics Development
| Reagent Category | Specific Examples | Function in CDx Development | Validation Requirements |
|---|---|---|---|
| Primary Antibodies | Monoclonal anti-HER2, anti-PD-L1 clones | Target detection and visualization | Specificity, sensitivity, cross-reactivity profiling |
| Control Materials | Cell lines with known mutation status, synthetic controls | Assay calibration and performance monitoring | Stability, commutability, characterization |
| Detection Systems | Polymer-based detection, enzyme substrates | Signal amplification and visualization | Sensitivity, dynamic range, background optimization |
| Nucleic Acid Reagents | Primers, probes, sequencing libraries | Target amplification and detection | Specificity, efficiency, inhibition resistance |
| Sample Processing Reagents | Fixatives, embedding media, extraction kits | Sample preservation and nucleic acid/protein recovery | Yield, purity, integrity preservation |
| Reference Standards | Commercial reference materials, patient-derived references | Assay qualification and comparison | Documentation of origin, characterization data |
The selection and qualification of research reagents should follow a risk-based approach, with more extensive validation required for critical reagents that significantly impact assay performance. Documentation of reagent sourcing, characterization, and quality control is essential for regulatory submissions and should be maintained throughout the product lifecycle [1] [3].
Strategic Considerations for Successful CDx Commercialization
Integrated Drug-Diagnostic Development
Successful commercialization of companion diagnostics requires careful coordination with the corresponding therapeutic development program. The regulatory strategy should be aligned with the therapeutic product's development phase, with diagnostic validation activities timed to support critical decision points in the drug development pathway [3].
Phase 1 clinical studies typically provide initial proof-of-concept for both the therapeutic and diagnostic, with data used to select a clinical cutoff for the CDx. CLIA validation is then designed around that cutoff to use the assay for patient selection in subsequent phase 2 studies [3]. This sequential approach allows for refinement of the diagnostic assay based on emerging clinical data while maintaining regulatory compliance.
Risk Assessment and Regulatory Strategy
Companion diagnostics developers must conduct a thorough risk assessment based on how the device will be used in investigational therapeutic studies. When an assay is used for prospective patient stratification or clinical decision-making, a Study Risk Determination (SRD) is necessary to evaluate whether an Investigational Device Exemption (IDE) is required [3].
Manufacturers have several options for obtaining an SRD:
- Submit an SRD Q-submission to the FDA for agency determination
- Have the institutional review board (IRB) assess risk as a surrogate for the FDA
- Include a risk assessment in the pre-Investigational New Drug (IND) briefing book
- Assume significant risk and submit an IDE directly [3]
The FDA is the ultimate arbiter of significant risk determination, and this assessment is independent of the phase of the clinical trial and IND submission status [3].
Global Commercialization Planning
For companion diagnostics intended for global markets, developers must plan parallel validation strategies to meet both U.S. and international regulatory requirements. Key differences between the U.S. and European Union frameworks include:
- Classification Differences: In the U.S., CDx may be classified as either Class II or III devices, while in the EU they are uniformly classified as Class C devices under the In Vitro Diagnostic Regulation (IVDR) [3].
- Regulatory Authorities: The FDA serves as the regulatory authority in the U.S., while in the EU, Notified Bodies perform this function [3].
- Country-Specific Requirements: In the EU, assays with a medical purpose in clinical trials require Annex XIV submissions to national competent authorities in each country where samples are collected, adding complexity due to local requirements [3].
Validation studies performed in U.S.-based laboratories can be designed to meet both CLIA and Clinical Laboratory Standards Institute (CLSI) standards while simultaneously supporting EU regulatory submissions under ISO 13485 and Good Clinical Laboratory Practice (GCLP) guidelines [3]. This integrated approach avoids duplication of effort and streamlines the global regulatory process.
The path to commercialization for companion diagnostics through the Modular PMA process represents a strategic approach to navigating complex regulatory requirements while advancing precision medicine. The modular framework offers advantages for complex CDx development programs by enabling early FDA feedback, distributed resource allocation, and potentially more efficient review timelines. Successful implementation requires robust analytical and clinical validation following established guidelines, careful planning of drug-diagnostic co-development, and strategic consideration of global regulatory requirements. As the regulatory landscape continues to evolve with updates to CLIA requirements and transition to QMSR, CDx developers must maintain vigilance in compliance while advancing innovative diagnostic approaches that enable targeted therapies for appropriate patient populations.
Conclusion
Successful IHC assay validation is a multifaceted process that requires a deep understanding of the evolving CLIA regulatory landscape, meticulous methodological execution, proactive troubleshooting, and strategic planning for global commercialization. The integration of the 2024 CAP guideline updates and the 2025 CLIA personnel rules underscores a continuous push for higher standards, precision, and reproducibility. For researchers and drug developers, mastering these elements is not merely about compliance—it is fundamental to ensuring that IHC assays yield reliable, clinically actionable data. As personalized medicine advances, the role of rigorously validated IHC assays, particularly for predictive biomarkers, will only grow in importance, directly impacting patient diagnosis, treatment selection, and therapeutic outcomes. Future directions will likely involve greater harmonization of international standards and increased reliance on sophisticated quality management systems integrated with standards like ISO 13485.
References
- 1. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 2. Principles of Analytic Validation of Immunohistochemical ... [https://www.guidelinecentral.com/guideline/24377]
- 3. Optimizing Immunohistochemistry Validation and ... [https://www.precisionformedicine.com/blog/optimizing-ihc-validation-regulatory-strategies]
- 4. CAP Updates Validation of Immunohistochemical Assays ... [https://newsroom.cap.org/latest-news/cap-updates-validation-of-immunohistochemical-assays-testing-guideline-for-precise-results--improved/s/e0a63afa-9f2e-438c-acaf-c272a4db029f]
- 5. Simplifying the Process of 'Switching' Antibodies and ... [https://biocare.net/media/white-papers/simplifying-the-process-of-switching-antibodies-and-verifying-the-performance-of-a-modified-ihc-procedure/]
- 6. CAP Updates Their 'Principles of Analytic Validation ... [https://www.bioanalysis-zone.com/cap-updates-their-guidelines-for-principles-of-analytic-validation-of-immunohistochemical-assays/]
- 7. Technical Challenges Faced in Validation of ... [https://pubmed.ncbi.nlm.nih.gov/41246894/]
- 8. Laboratory-developed tests and in vitro diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12086060/]
- 9. CMS Enacts New CLIA Regulations Effective January 2025 [https://www.bakerdonelson.com/cms-enacts-new-clia-regulations-effective-january-2025]
- 10. What 2025 CLIA Updates Mean for Labs and Compliance [https://reesscientific.com/blog/2025-clia-updates-for-labs]
- 11. Comparison of immunohistochemical HER2 low detection ... [https://pubmed.ncbi.nlm.nih.gov/40715555/]
- 12. Synergistic H&E and IHC image analysis by AI predicts ... [https://www.nature.com/articles/s43856-025-01045-9]
- 13. Immunohistochemistry Market Research 2025 [https://finance.yahoo.com/news/immunohistochemistry-market-research-2025-global-080700033.html]
- 14. ILA28 | Quality Assurance for Design Control and ... [https://clsi.org/shop/standards/ila28/]
- 15. Frequently Asked Questions from Immunohistochemistry ... [https://www.cap.org/member-resources/councils-committees/immunohistochemistry-topic-center/frequently-asked-questions-from-immunohistochemistry-laboratories]
- 16. CMS Implements First Major Updates to Lab Personnel ... [https://www.mwe.com/insights/cms-implements-first-major-updates-to-lab-personnel-requirements-in-30-years/]
- 17. CMS's CLIA Rule Now Fully in Effect [https://www.ascp.org/news/news-details/2025/01/09/cms-s-clia-rule-now-fully-in-effect?srsltid=AfmBOoogqJ0aTvvLdumGsbFPjym_3v5H440I1NL-0N0TcN6O7rQ4_N7b]
- 18. CLIA Lab Director Eligibility and Requirements (2025 ... [https://www.linkedin.com/pulse/clia-lab-director-eligibility-requirements-2025-update-hou-gm37e]
- 19. Device Risk Determinations for IVD Research [https://www.advarra.com/blog/device-risk-determinations-for-ivd-research/]
- 20. Regulatory and Development Approaches to Research for ... [https://acrpnet.org/2023/02/22/regulatory-and-development-approaches-to-research-for-in-vitro-diagnostics-vs-other-medical-devices-the-same-or-different]
- 21. Overview of IVD Regulation [https://www.fda.gov/medical-devices/ivd-regulatory-assistance/overview-ivd-regulation]
- 22. In vitro diagnostic medical device performance evaluation [https://blog.johner-institute.com/regulatory-affairs/performance-evaluation-of-in-vitro-diagnostics/]
- 23. CLIA Waiver by Application [https://www.fda.gov/medical-devices/ivd-regulatory-assistance/clia-waiver-application]
- 24. CLIA Waiver by Application Decision Summaries [https://www.fda.gov/about-fda/cdrh-transparency/clia-waiver-application-decision-summaries]
- 25. Methods for determining clinical utility [https://www.sciencedirect.com/science/article/abs/pii/S0009912023002023]
- 26. Establishing Clinical Utility for Diagnostic Tests Using a ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6787613/]
- 27. The ABCs of finding a good antibody - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5499787/]
- 28. Analytic Validation of Immunohistochemical Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938252/]
- 29. NordiQC - Immunohistochemical Quality Control [https://www.nordiqc.org/about.php]
- 30. 3 Steps for Comparing Antibody Clones with the New ... [https://www.bdbiosciences.com/en-us/learn/science-thought-leadership/blogs/BD-Clone-Comparison]
- 31. Selecting the Best Clone for Your Flow Cytometry ... [https://www.sonybiotechnology.com/blog/selecting-best-clone-flow-cytometry-experiments]
- 32. Validation and Prospective Testing of a High Sensitivity ... [https://www.sciencedirect.com/science/article/abs/pii/S0023683725001436]
- 33. A novel quantitative immunohistochemistry method for ... [https://www.nature.com/articles/modpathol2016176]
- 34. Analytical Validation of Quantitative Immunohistochemical ... [https://pubmed.ncbi.nlm.nih.gov/29863904/]
- 35. 2025 CLIA Acceptance Limits for Proficiency Testing [https://www.westgard.com/clia-a-quality/quality-requirements/2024-clia-requirements.html]
- 36. Clinical Validation and Post-Implementation Performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110696/]
- 37. The importance and implications of comparator selection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6338470/]
- 38. Comparator Selection - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK126184/]
- 39. Concordance Analysis: Part 16 of a Series on Evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3165924/]
- 40. Development and clinical validation of deep learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12211442/]
- 41. Guidance for Submission of Immunohistochemistry ... [https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/guidance-submission-immunohistochemistry-applications-food-and-drug-administration-final-guidance]
- 42. The clinical immunohistochemistry laboratory [https://pubmed.ncbi.nlm.nih.gov/20012854/]
- 43. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 44. Immunohistochemistry (IHC) [https://www.cellsignal.com/learn-and-support/overview-of-ihc?srsltid=AfmBOoqOfGacwAMCB9wpXVM0adHcrJbAXenIQBXtvXtPVodDTqdJJjV-]
- 45. Application and Validation of Semiautomatic Quantification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885164/]
- 46. HER2 IHC Testing Updates for mNSCLC [https://www.her2know.com/newsletter/her2-ihc-testing-mnsclc-jan-2025-update.html]
- 47. A fully automated quantitative analysis method based on ... [https://www.sciencedirect.com/science/article/pii/S2950261625000342]
- 48. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 49. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467]
- 50. Impact of pre-analytic variables on HER2 IHC results [https://www.her2know.com/pathology-perspectives/spotlight-series/impact-of-pre-analytic-variables-on-her2-ihc-results.html]
- 51. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 52. Diagnostic Performance - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/diagnostic-performance]
- 53. Measures of Diagnostic Accuracy: Basic Definitions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4975285/]
- 54. Low sensitivity of the fourth‐generation antigen/antibody HIV ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205210/]
- 55. Model for Interpreting Discordant SARS-CoV-2 Diagnostic ... [https://wwwnc.cdc.gov/eid/article/30/2/23-0200_article]
- 56. Comparative analysis of specificity and sensitivity between ... [https://link.springer.com/article/10.1007/s00203-022-03118-y]
- 57. Immunohistochemical Validation of Rare Tissues and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8143380/]
- 58. From Biomarker to Clinical Trial Assay [https://www.precisionformedicine.com/blog/immunohistochemistry-precision-medicine-biomarker-clinical-trial-assay]
- 59. Detect Assay Drift Over Time [https://www.brendan.com/detect-assay-drift-over-time/]
- 60. Detection of Calibration Drift in Clinical Prediction Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8627243/]
- 61. What are the different detection methods for IHC? [https://www.enzo.com/note/what-are-the-different-detection-methods-for-ihc/]
- 62. Intro to Immunohistochemistry (IHC) Staining: Steps & Best ... [https://www.leicabiosystems.com/us/knowledge-pathway/immunohistochemistry-an-overview-steps-to-better-ihc-staining/]
- 63. Immunohistochemistry staining [https://www.abcam.com/en-us/knowledge-center/immunohistochemistry/ihc-staining]
- 64. Comparison of three scoring methods using the FDA ... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-020-01303-9]
- 65. Clinicopathological values of PD-L1 expression in HER2- ... [https://www.nature.com/articles/s41598-019-52944-6]
- 66. Differences in HER2-0 and HER2-low Breast Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885850/]
- 67. Counterstains in Immunohistochemistry: Principles, ... [https://www.bosterbio.com/blog/post/counterstains-in-immunohistochemistry-principles-options-and-troubleshooting?srsltid=AfmBOopd9Bof5LUprf5YO4EToCjX0vvfGsoLhXmAQK4DansazDaJaXUv]
- 68. Immunohistochemistry for predictive biomarkers in non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5653529/]
- 69. Developed Test: FDA Laboratory . Vs Regulatory Guide CLIA [https://doseway.com/laboratory-developed-test-fda-vs-clia/]
- 70. Final 5 CLIA Rule. Part V: Method Validation Process and ... [https://www.westgard.com/clia-a-quality/clia-final-rule/cliafinalrule5.html]
- 71. Premarket Approval (PMA) [https://www.fda.gov/medical-devices/premarket-submissions-selecting-and-preparing-correct-submission/premarket-approval-pma]
- 72. PMA Application Contents [https://www.fda.gov/medical-devices/premarket-approval-pma/pma-application-contents]
- 73. Guidance for Fluorescence in Situ Hybridization Testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1867444/]
- 74. How Do You Comply with EU MDR/IVDR vs. U.S. FDA ... [https://avendium.com/2025/10/31/how-do-you-comply-with-eu-mdr-ivdr-vs-u-s-fda-regulations/]
- 75. IVDs – A Comparison of Requirements between the US and EU [https://blog.pqegroup.com/medical-device/ivds-a-comparison-of-requirements-between-the-us-and-eu]
- 76. Potential impact of IVDR on diagnostic testing in Europe [https://www.almacgroup.com/knowledge/library/potential-impact-of-ivdr-on-diagnostic-testing-in-europe-what-are-the-implications-for-the-pharmaceutical-industry/]
- 77. Transitional provisions of the IVDR [https://blog.johner-institute.com/regulatory-affairs/ivdr-transitional-periods/]
- 78. IVDR Transition Timelines Extended [https://www.bsigroup.com/en-US/insights-and-media/media-center/press-releases/2024/july/ivdr-transition-timelines-extended/]
- 79. PMA Application Methods [https://www.fda.gov/medical-devices/premarket-approval-pma/pma-application-methods]
- 80. Premarket Approval Application and Humanitarian Device ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/premarket-approval-application-and-humanitarian-device-exemption-modular-review]
- 81. FDA Formal Changes for PMA and HDE Submissions ... [https://rhizomeai.com/articles/what_formal_changes_has_the_fda_released_regarding_pma_and_h?question=What+formal+changes+has+the+FDA+released+regarding+PMA+and+HDE+submission+content+in+relation+to+the+Quality+Management+System+Regulation+%28QMSR%29%2C+such+as+draft+guidances%2C+and+where+can+these+documents+be+accessed&showSourceNumber=235&id=e25dbbc0-f227-4612-9d67-6c44549d64d0]
- 82. 2025 Changes to Point-of-Care Testing Regulatory ... [https://myadlm.org/education/point-of-care-testing-professional-certification/the-point/articles/2025/may]