Solving Autofluorescence in Immunofluorescence: A Researcher's Guide to Enhanced Signal Detection
Autofluorescence presents a significant barrier to achieving reliable, high-sensitivity results in immunofluorescence (IF) microscopy, particularly in human tissue and disease research.
Solving Autofluorescence in Immunofluorescence: A Researcher's Guide to Enhanced Signal Detection
Abstract
Autofluorescence presents a significant barrier to achieving reliable, high-sensitivity results in immunofluorescence (IF) microscopy, particularly in human tissue and disease research. This article provides a comprehensive guide for researchers and drug development professionals on overcoming this challenge. It covers the foundational science behind autofluorescence, explores both established and cutting-edge methodological solutions—including high-speed Fluorescence Lifetime Imaging Microscopy (FLIM) and chemical quenching—and offers a practical troubleshooting framework for assay optimization. Finally, it validates these approaches through comparative analysis with gold-standard techniques and discusses their impact on advancing precision medicine and multiplexed spatial biology.
Understanding Autofluorescence: Sources, Impact, and Identification in Biological Samples
Autofluorescence is the background fluorescence emitted naturally by biological structures or sample preparation components, which can severely compromise the detection and quantification of specific immunofluorescence signals [1] [2]. This inherent emission of light by endogenous molecular components is a widespread phenomenon in cells and tissues, arising from sources such as metabolic cofactors, structural proteins, and pigments [1]. For researchers and drug development professionals, effectively managing autofluorescence is not merely an optimization step but a fundamental requirement for obtaining reliable, interpretable data, especially when working with endogenously tagged proteins, low-abundance targets, or complex tissue samples where signal-to-noise ratio is critical [3]. This guide provides a comprehensive framework for understanding, troubleshooting, and resolving autofluorescence challenges in immunofluorescence research.
What is Autofluorescence and Why Does It Matter?
Autofluorescence originates from endogenous fluorophores—biological molecules with intrinsic fluorescent properties. Much like engineered fluorophores, these molecules contain polycyclic hydrocarbons with delocalized electrons that absorb incoming photons and emit light at a lower energy and longer wavelength [1]. However, unlike the specific signals from antibody-conjugated dyes, autofluorescence is an unavoidable background inherent to the biological sample itself.
The primary significance of autofluorescence lies in its capacity to obscure specific immunofluorescence signals, leading to:
- Reduced Signal-to-Noise Ratio: Autofluorescence elevates the background "noise," making it difficult to distinguish weak but genuine "signals" [4].
- Impaired Quantification: Accurate measurement of protein expression levels or localization becomes challenging when specific signal is contaminated with variable background [3].
- False Positives: In multiplexed experiments, autofluorescence can be mistakenly interpreted as a positive signal, leading to incorrect conclusions [5].
The table below summarizes the most common endogenous sources of autofluorescence encountered in biological research:
Table 1: Common Endogenous Sources of Autofluorescence
| Source | Localization | Excitation/Emission (approx.) | Notes |
|---|---|---|---|
| NAD(P)H [1] | Cytoplasm | ~340 nm / ~450 nm | Metabolic cofactor; only the reduced form (NAD(P)H) fluoresces. |
| Flavins (FAD) [1] | Mitochondria | ~380-490 nm / ~520-560 nm | Metabolic coenzyme; only the oxidized form (FAD) fluoresces. |
| Collagen [1] [2] | Extracellular Matrix | ~270 nm / ~390 nm | Key structural protein; abundant in connective tissues. |
| Elastin [1] | Extracellular Matrix | ~350-450 nm / ~420-520 nm | Structural protein often found with collagen. |
| Lipofuscin [1] | Lysosomes (various cells) | ~345-490 nm / ~460-670 nm | "Age pigment"; accumulates over time in long-lived cells. |
| Tryptophan [1] | Most proteins | ~280 nm / ~350 nm | Amino acid found in most folded proteins. |
| Melanin [1] | Skin, hair, eyes | ~340-400 nm / ~360-560 nm | Natural pigment; photoprotective. |
Troubleshooting Guide: FAQs on Autofluorescence
How can I determine if autofluorescence is a problem in my experiment?
The most straightforward method is to run an unlabeled control [5] [4]. Process your sample identically through the entire immunofluorescence protocol, but omit the primary and secondary antibodies. Any signal detected in this control under your standard imaging settings can be attributed to autofluorescence or other non-specific background, providing a baseline for troubleshooting.
My immunofluorescence signal is weak or absent despite confirmed antibody specificity. Could autofluorescence be the cause?
While autofluorescence typically manifests as a high background, it can sometimes mask a weak specific signal, making it appear absent. The causes and recommendations for weak signal are summarized in the table below:
Table 2: Troubleshooting Weak or No Signal
| Possible Cause | Recommendations |
|---|---|
| Signal Masking [6] | Use signal amplification (e.g., TSA) [7] or pair with a brighter, red-shifted fluorophore [5]. |
| Inadequate Fixation [6] | Follow validated protocols; use fresh 4% formaldehyde for phospho-specific antibodies to inhibit phosphatases. |
| Target Protein Not Induced/Low Expression [6] | Confirm protein expression by Western blot; use positive controls; optimize treatment conditions. |
| Incorrect Antibody Dilution [6] | Titrate antibodies and consult the manufacturer's datasheet for recommended dilutions. |
| Sample Degradation [6] | Use freshly prepared slides and image immediately after mounting. Store samples in the dark. |
The background in my images is overwhelmingly high. What are the primary strategies to reduce it?
High background is a classic symptom of autofluorescence. The solutions can be categorized as follows:
Table 3: Troubleshooting High Background
| Possible Cause | Recommendations |
|---|---|
| Sample Autofluorescence [6] [8] | Use red/far-red fluorophores [5]; employ chemical quenching (e.g., Vector TrueVIEW Kit, Sudan Black B, sodium borohydride) [5] [4]; or employ photobleaching prior to staining [4]. |
| Fixative-Induced Fluorescence [1] [5] | Avoid glutaraldehyde; use fresh formaldehyde; treat aldehyde-fixed samples with sodium borohydride (e.g., 0.1% in PBS) to reduce fluorescent cross-links [5] [8]. |
| Insufficient Blocking or Washing [6] [8] | Increase blocking incubation time; consider different blocking agents (e.g., normal serum, BSA); ensure thorough washing between steps. |
| Antibody Concentration Too High [6] [8] | Titrate both primary and secondary antibodies to find the optimal signal-to-background ratio. |
| Non-biological Sources [1] [4] | Use phenol red-free media for live imaging; image with glass-bottom dishes; ensure paper labels are not in the light path. |
Experimental Protocols for Autofluorescence Management
Protocol 1: Chemical Quenching with Sodium Borohydride
This protocol is effective for reducing autofluorescence caused by aldehyde-based fixatives [5] [8].
- After fixation and subsequent PBS washes, prepare a fresh solution of 0.1% sodium borohydride (NaBH4) in PBS.
- Caution: The solution will fizz as hydrogen gas is released. Prepare in a fume hood and allow it to settle before use.
- Incubate the sample with the NaBH4 solution for 10-30 minutes.
- Wash the sample thoroughly 3-4 times with PBS before proceeding with standard immunofluorescence staining protocols.
Protocol 2: Spectral Separation and Fluorophore Selection
This is a preventive strategy to minimize spectral overlap with autofluorescence.
- Identify Autofluorescence Profile: Use a spectral detector on your microscope to lambda scan an unstained control sample. Identify the peak excitation and emission wavelengths of the background [4].
- Select Optimal Fluorophores: Choose fluorescent dyes whose emission spectra are far from the major autofluorescence peaks. Since autofluorescence is most intense in the blue-green spectrum (350-550 nm), selecting far-red dyes (e.g., Cy5, Alexa Fluor 647, Cy7) is highly advantageous [1] [5] [4].
- Titrate Antibodies: Perform a dilution series of your fluorophore-conjugated antibodies to find the concentration that yields the best signal-to-background ratio, not just the strongest signal [4].
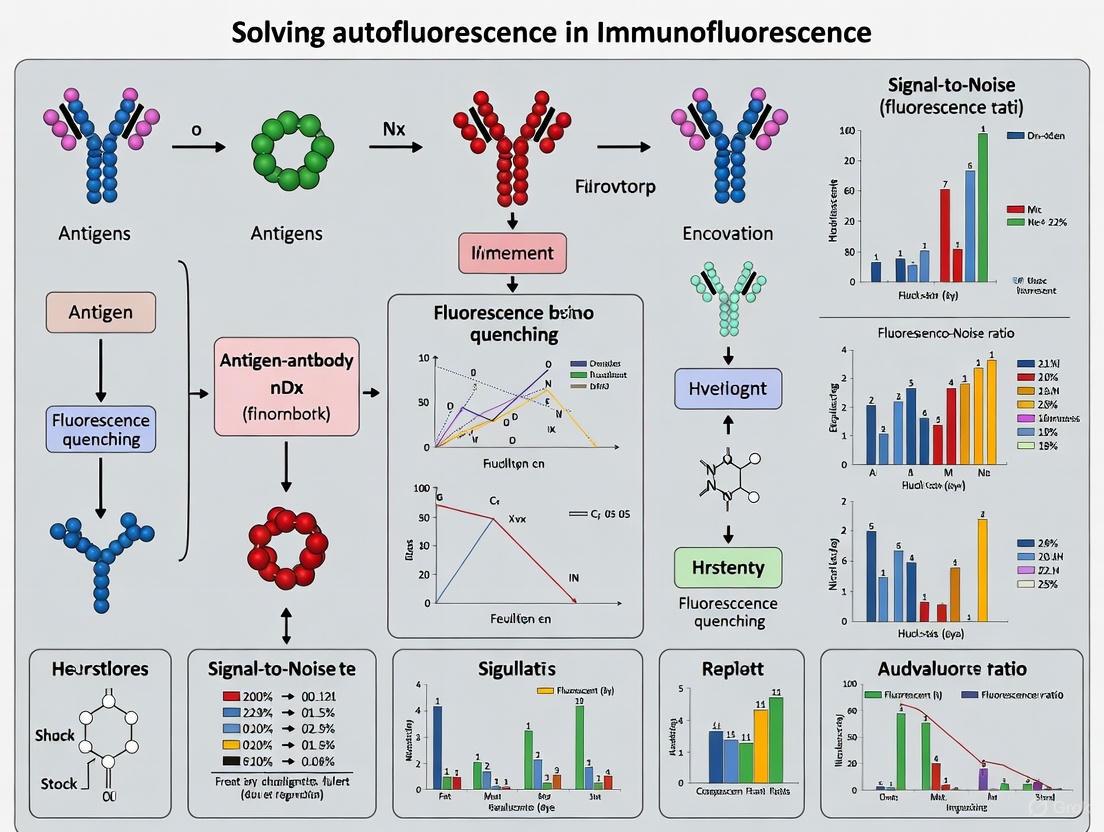
The following diagram illustrates the decision-making workflow for addressing autofluorescence:
The Scientist's Toolkit: Key Reagent Solutions
The table below lists essential reagents and tools for managing autofluorescence, as compiled from the referenced sources.
Table 4: Research Reagent Solutions for Autofluorescence Management
| Item / Reagent | Function / Explanation | Reference |
|---|---|---|
| Sodium Borohydride (NaBH4) | Reduces aldehyde groups from fixatives that cause background fluorescence. | [5] [8] |
| Sudan Black B | Chemical quencher that suppresses a broad range of autofluorescence signals. | [9] [5] |
| Vector TrueVIEW Kit | Commercial kit designed to bind and quench autofluorescent elements in tissues. | [5] |
| Phenol Red-Free Media | Eliminates background fluorescence from the pH indicator in cell culture media during live imaging. | [1] [4] |
| Glass-Bottom Dishes | Non-fluorescent imaging vessels that prevent background from plastic cultureware. | [1] [4] |
| ProLong Gold Antifade Mountant | Mounting medium that contains antifade agents to reduce signal photobleaching. | [6] |
| Far-Red Fluorophores (e.g., Cy5, Alexa Fluor 647) | Bright dyes emitting >620 nm, spectrally distant from common autofluorescence in blue-green range. | [1] [5] [4] |
| TSA (Tyramide Signal Amplification) | Enzyme-mediated system that significantly amplifies weak signals, helping overcome background. | [7] |
Advanced and Future Directions
For persistent autofluorescence that cannot be resolved with basic methods, advanced techniques offer powerful solutions.
Fluorescence Lifetime Imaging Microscopy (FLIM) leverages the distinct nanosecond-scale decay rates (lifetimes) of fluorophores. Since autofluorescence and specific immunofluorescence signals often have different lifetimes, even with spectral overlap, FLIM can digitally separate them [9] [4]. Phasor analysis, a graphical approach to FLIM data, allows for clear visualization and separation of these lifetime components, enabling precise quantification of the specific immunofluorescence signal fraction [9]. Furthermore, computational tools like the SAIBR (Spectral Autofluorescence Image Correction By Regression) plugin for FIJI provide a platform-independent method for spectral autofluorescence correction, which is particularly useful for quantifying weakly expressed proteins at endogenous levels [3].
Autofluorescence (AF), the background fluorescence emitted naturally by biological structures, presents a significant challenge in immunofluorescence (IF) microscopy [5]. This signal, originating from sources other than the specific antibody-fluorophore interaction, can obscure target detection, complicate image interpretation, and reduce the signal-to-noise ratio, particularly for low-abundance targets [10] [11]. This interference is primarily caused by endogenous fluorophores—molecules inherent to cells and tissues that possess fluorescent properties [12] [1]. Understanding and managing the autofluorescence from four key endogenous fluorophores—Collagen, NADH, Lipofuscin, and Elastin—is crucial for improving the reliability and interpretability of immunofluorescence data in research and diagnostic applications [10] [12]. This guide provides a structured, practical framework for researchers to identify, troubleshoot, and overcome these common autofluorescence challenges.
Fluorophore Profiles: Identification and Spectral Characteristics
The first step in troubleshooting is recognizing the source of autofluorescence. The table below summarizes the key characteristics of the four major endogenous fluorophores.
Table 1: Spectral and Biological Profiles of Common Endogenous Fluorophores
| Fluorophore | Biological Role & Location | Excitation/Emission Peaks (approx.) | Key Features & Troubleshooting Notes |
|---|---|---|---|
| Collagen | Extracellular matrix structural protein; ubiquitous in tissues [12] [1]. | Exc: 330-340 nm / Em: 400-410 nm [12] (Also reported: Exc: 270 nm / Em: 390 nm [1]) | Emits in the blue region [11] [13]. A major source of background in many tissues. |
| NAD(P)H | Metabolic coenzyme; found in cytoplasm and mitochondria [12] [1]. | Exc: 330-380 nm / Em: 440-462 nm [12] (Also reported: Exc: 340 nm / Em: 450 nm [1]) | Emits in the blue/green region [11] [13]. Signal increases in metabolically active cells (e.g., liver) [11]. Only the reduced form (NAD(P)H) fluoresces [1]. |
| Lipofuscin | Granular, lipophilic "wear-and-tear" pigment; accumulates in lysosomes with age in neurons, heart, skeletal muscle [10] [11] [1]. | Exc: 345-490 nm / Em: 460-670 nm [1] (Broadest emission, strongest at ~500-695 nm [11] [13]) | A particularly problematic, broad-spectrum fluorophore that interferes with many common dyes [10] [14]. Its granular appearance can be mistaken for specific staining [11]. |
| Elastin | Extracellular matrix protein providing elasticity; often interspersed with collagen around vasculature and in skin [1]. | Exc: 350-450 nm / Em: 420-520 nm [1] | Emits in the blue-green region. Like collagen, it is a major source of background in connective tissues and skin [1]. |
The following workflow diagram outlines a systematic strategy for diagnosing and resolving autofluorescence based on the fluorophores involved:
Frequently Asked Questions (FAQ) & Troubleshooting
Q1: How can I confirm that the signal I'm seeing is autofluorescence? The most straightforward method is to run an unlabeled control [5]. Process your sample identically to your stained samples, but omit the primary and secondary antibody reagents. Any fluorescence detected in this control can be attributed to autofluorescence from the sample itself or other assay components, providing a baseline for troubleshooting [5] [13].
Q2: My tissue has high levels of lipofuscin (e.g., aged or neuronal tissue). What is the most effective way to reduce its interference? Lipofuscin is notoriously difficult due to its broad emission spectrum. Two highly effective methods are:
- Chemical Quenching: Staining tissue sections with Sudan Black B (SBB) is a common and effective method to quench lipofuscin autofluorescence [10] [11] [13]. SBB is a lipophilic dye that binds to the lipid-rich components of lipofuscin, masking its fluorescence.
- Photobleaching: A robust pre-staining protocol using high-intensity white LED light can near-totally reduce lipofuscin autofluorescence without negatively impacting subsequent multiplex fluorescence detection [14]. This is a simple, scalable, and cost-effective solution.
Q3: I am working with a tissue rich in collagen and elastin (e.g., skin, heart). How can I improve my signal-to-noise ratio? For structural proteins like collagen and elastin that emit in the blue-green spectrum, the best strategy is often to avoid the problem spectrally.
- Switch Fluorophores: Choose reporter dyes that emit in the red or far-red region (e.g., CoraLite 594, CoraLite 647, Alexa Fluor 647) [11] [5] [1]. This places your signal of interest in a spectral window with much lower background interference.
- Use Bright Fluorophores: Selecting brighter fluorophores like PE or APC can help the specific signal overcome the background [5].
Q4: Aldehyde fixation has caused high background in my samples. Can I fix this? Yes, aldehyde fixatives like formalin and glutaraldehyde create fluorescent Schiff bases. You can:
- Prevent It: Use alternative fixatives like chilled (-20°C) ethanol where possible, or opt for paraformaldehyde over glutaraldehyde, fixing for the minimum time required [11] [5] [13].
- Treat It: Treatment with sodium borohydride (NaBH₄) can reduce the fluorescent cross-links formed by aldehydes [9] [11]. However, its effects can be variable, and it is not always well-recommended [11] [13].
Q5: Are there advanced imaging techniques that can digitally separate autofluorescence? Yes, technological solutions are becoming more accessible.
- Fluorescence Lifetime Imaging Microscopy (FLIM): This powerful technique leverages the distinct fluorescence lifetime decay profiles of fluorophores to differentiate specific immunofluorescence signals from autofluorescence, even if their emission spectra overlap [9]. Recent advances in high-speed, GPU-accelerated FLIM are making this a more practical option for routine imaging [9].
- Spectral Unmixing: Hyperspectral imaging can record the full emission spectrum for each pixel, and computational algorithms can then "unmix" the signal based on the unique spectral signature of the target fluorophore and the autofluorescence [1].
Experimental Protocols for Autofluorescence Reduction
Chemical Quenching with Sudan Black B
This protocol is primarily effective for reducing lipofuscin autofluorescence [10] [11] [13].
- Reagent Preparation: Prepare a 0.1% to 1% (w/v) solution of Sudan Black B in 70% ethanol. The solution can be gently warmed and filtered to ensure it is fully dissolved.
- Sample Processing: After completing the standard immunofluorescence staining procedure (including antibody incubations and final washes), but prior to mounting, incubate the tissue sections with the Sudan Black B solution.
- Incubation: Incubate for 10-30 minutes at room temperature, protected from light.
- Washing: Rinse the sections thoroughly with 70% ethanol to remove excess dye, followed by several washes with PBS or your preferred buffer.
- Mounting: Proceed with mounting the slides with an aqueous mounting medium.
White Light Photobleaching for Lipofuscin Reduction
This is a physical method to reduce lipofuscin autofluorescence prior to staining [14].
- Sample Preparation: Deparaffinize and rehydrate formalin-fixed paraffin-embedded (FFPE) tissue sections following standard histological protocols.
- Photobleaching: Place the slides under a high-intensity, broad-spectrum white LED light source. Ensure the light uniformly illuminates the sample.
- Exposure: Expose the samples for 20-30 minutes. The required duration may need optimization for different tissues and light source intensities.
- Staining: After photobleaching, proceed with your standard immunofluorescence staining protocol.
- Advantage: This method is simple, low-cost, and does not involve chemicals that might affect antigenicity or require extensive washing [14].
Fluorophore Selection and Spectral Imaging Workflow
This protocol outlines a strategic approach to avoid autofluorescence by experimental design and advanced analysis.
- Control Imaging: First, image an unstained tissue section to create a reference map of autofluorescence across all detection channels you plan to use [5].
- Strategic Fluorophore Selection: Based on the autofluorescence profile, select bright fluorophores whose emission spectra are in "quiet" windows, typically the red and far-red (e.g., 620-750 nm) [5] [1]. See "The Scientist's Toolkit" below for options.
- Image Acquisition & Processing:
- Conventional Microscopy: Use the unstained control to set your background threshold and exposure settings to avoid saturation by autofluorescence.
- FLIM/Spectral Imaging: If available, use Fluorescence Lifetime Imaging Microscopy (FLIM) to separate signals based on lifetime differences [9] or use spectral unmixing to mathematically separate the signals during image processing [1].
The following diagram illustrates the principle of the FLIM-based separation method, a advanced digital approach to this problem:
The Scientist's Toolkit: Key Reagents and Technologies
Table 2: Essential Reagents and Tools for Managing Autofluorescence
| Tool/Reagent | Function | Primary Use Case / Target |
|---|---|---|
| Sudan Black B | Lipophilic dye that quenches fluorescence by binding to lipid-rich structures [10] [11]. | Highly effective against lipofuscin autofluorescence. |
| Sodium Borohydride (NaBH₄) | Reducing agent that breaks fluorescent Schiff bases formed by aldehyde fixation [9] [11]. | Reduces background from aldehyde-based fixation. |
| Copper Sulfate (CuSO₄) | Chemical treatment that can reduce autofluorescence from various sources [10] [5]. | Used against lipofuscin and potentially other sources like heme [10] [13]. |
| TrueVIEW Kit (Vector Labs) | Commercial autofluorescence quenching kit. | Broad-spectrum reduction of autofluorescence from aldehyde fixation, RBCs, collagen/elastin [5] [13]. |
| White LED Photobleaching | Physical method using light to quench fluorescent molecules prior to staining [14]. | Highly effective for lipofuscin in human nervous system tissue [14]. |
| Far-Red Fluorophores (e.g., CoralLite 647, Alexa Fluor 647, Cy7) | Reporter dyes whose emission is spectrally distant from most autofluorescence [11] [1] [15]. | General strategy to avoid interference from collagen, NADH, and elastin (which emit in blue-green). |
| Quantum Dots (Qdots) | Nanocrystals with very large Stokes shifts, allowing excitation and emission in spectral windows with low autofluorescence [15]. | Effective for tissues with very high background (e.g., human retina); can avoid all common AF [15]. |
| FLIM (Fluorescence Lifetime Imaging Microscopy) | Advanced imaging modality that separates signals based on fluorescence decay time, not just color [9]. | Digital method to distinguish specific IF from AF regardless of spectral overlap [9]. |
{#key-takeaways}
| Source | Cause of Autofluorescence | Primary Solution |
|---|---|---|
| Aldehyde Fixatives (e.g., Formaldehyde, Glutaraldehyde) | Form reactive Schiff's bases with amine groups [16] [17] | Use non-aldehyde fixatives (e.g., ice-cold methanol, acetone) or treat with sodium borohydride (NaBH4) [18] [19] [16]. |
| Plasticware (e.g., culture flasks, microplates) | Inherent property of the plastic material [16] [20] | Switch to glass-bottomed vessels or specialized, non-fluorescent polymer labware [16] [20]. |
| Culture Media | Supplements like Fetal Bovine Serum (FBS) and Phenol Red [16] | Use media without phenol red and avoid serum supplements for live-cell imaging [16]. Use specialized low-autofluorescence mounting media [21]. |
Experimental Protocols for Troubleshooting
Protocol 1: Quenching Aldehyde-Induced Autofluorescence with Sodium Borohydride
Aldehyde fixatives create fluorescent Schiff's bases; this protocol reduces them to non-fluorescent salts [16] [17].
- Reagents: Sodium borohydride (NaBH4), Phosphate-Buffered Saline (PBS) [17].
- Procedure:
- Prepare Solution: Dissolve NaBH4 in PBS to a final concentration of 1 mg/mL [17]. Keep the solution ice-cold.
- Incubate: After fixing and washing your samples, incubate them in the fresh, ice-cold NaBH4 solution.
- Duration: A typical incubation is 5-10 minutes, but optimization may be required for your specific tissue [19] [22].
- Wash: Wash the samples thoroughly with PBS before proceeding with your staining protocol [19].
Protocol 2: Preparing Low-Autofluorescence Culture Media for Live-Cell Imaging
This protocol adapts standard practices for minimizing media-based interference [16] [20].
- Reagents: Your standard culture medium, Phenol Red-free medium, Fetal Bovine Serum (FBS).
- Procedure:
- Select Medium: Use a phenol red-free version of your culture medium [16].
- Eliminate Serum: For the duration of the imaging experiment, use media without FBS or other serum supplements [16].
- Equilibrate Media: Before imaging, allow all media to reach the experimental temperature (e.g., 37°C) to prevent convective currents and bubble formation that can disturb microscopy [20].
Troubleshooting Guide: Exogenous Autofluorescence
High Background Signal
| Question | Answer |
|---|---|
| My tissue sections show high background after aldehyde fixation. What can I do? | This is likely due to fluorescent Schiff's bases. Treat fixed samples with a sodium borohydride solution (see Protocol 1) or use a commercial autofluorescence quenching kit [16] [17] [22]. |
| My cell culture plasticware is fluorescent. How do I fix this? | Standard plastic labware is often autofluorescent. For imaging, use vessels with a glass bottom or those specifically marketed as having low-autofluorescence polymer coverslips [16] [20]. |
| The culture media itself is creating background noise during live imaging. | Avoid phenol red and serum. Use phenol red-free media and image in media without FBS [16]. Always equilibrate media to the imaging temperature beforehand [20]. |
| My mounting medium is contributing to background. | Standard mounting media can be autofluorescent. Switch to a commercial mounting medium specifically formulated for low autofluorescence [21]. |
Weak or No Specific Signal
| Question | Answer |
|---|---|
| After using a strong fixative, my signal is weak. Could background and fixation be linked? | Yes. Overfixation with aldehydes can both mask your epitope (reducing signal) and increase autofluorescence (increasing background). Reduce fixation time, or perform an antigen retrieval step post-fixation to unmask the epitope [18] [21]. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Example/Best Practice |
|---|---|---|
| Sodium Borohydride (NaBH4) | Quenches autofluorescence induced by aldehyde fixatives [17]. | Use at 1 mg/mL in PBS, ice-cold [17]. |
| Low-Autofluorescence Vessels | Provides a substrate with minimal inherent fluorescence for imaging [20]. | Use ibidi µ-Slides with polymer or glass coverslip bottoms, or similar products [20] [21]. |
| Phenol Red-Free Media | Eliminates fluorescence from the pH indicator in standard culture media [16]. | Essential for live-cell fluorescence imaging. |
| TrueVIEW Autofluorescence Quenching Kit | Commercial kit designed to reduce various forms of autofluorescence in fixed tissues [22]. | Incubation times can be optimized (e.g., 2-5 minutes) for different tissues [22]. |
| Low-Fluorescence Mounting Medium | Preserves sample and minimizes background during imaging without introducing its own signal [21]. | Use a product like ibidi Mounting Medium [21]. |
| Methanol or Acetone | Non-aldehyde, precipitating fixatives that do not create fluorescent Schiff's bases [18] [22]. | An alternative to aldehydes if epitope integrity and activity are maintained [18]. |
Experimental Workflow and Chemical Pathways
Autofluorescence Quenching Workflow
Aldehyde Fixative Reaction Pathway
Autofluorescence (AF) is the background fluorescence emitted naturally by biological samples and certain reagents, which does not result from specific fluorescent staining [16]. This phenomenon presents a significant and costly challenge in immunofluorescence research and diagnostic applications. The presence of autofluorescence can severely hinder the detection of specific fluorescence signals, leading to increased background noise, reduced assay sensitivity, and potential false positives or negatives in data interpretation [9] [16].
In the context of drug discovery and diagnostics, where accurate quantification and qualification of biological targets are paramount, autofluorescence interferes with the clear visualization of specific immunofluorescent labeling, making it difficult to discern critical biological information [23]. This interference is particularly problematic for low-abundance targets, where the specific signal may be completely masked by background autofluorescence, potentially leading to incorrect conclusions and costly missteps in the research and development pipeline.
The following diagram illustrates the core problem and the primary solution pathways for overcoming autofluorescence in research and diagnostics:
To effectively troubleshoot autofluorescence issues, researchers must first understand the common sources contributing to background signal. The interfering fluorescence can originate from both endogenous biological components and common laboratory reagents.
Many intrinsic biomolecules exhibit natural fluorescence properties, with varying excitation and emission profiles that can overlap with commonly used fluorescent dyes [12] [1]. The table below summarizes the key endogenous fluorophores and their spectral characteristics:
Table 1: Common Biological Sources of Autofluorescence
| Source | Excitation/Emission Range | Biological Location | Research Impact |
|---|---|---|---|
| NAD(P)H [1] | Exc: ~340 nm; Em: ~450 nm [1] | Cytoplasm, mitochondria [1] | Interferes with blue-emitting fluorophores; indicates metabolic activity |
| Flavins (FAD) [1] | Exc: 380-490 nm; Em: 520-560 nm [1] | Mitochondria [1] | Masks green-emitting dyes (e.g., FITC, Alexa Fluor 488); indicates redox state |
| Collagen [1] | Exc: ~270 nm; Em: ~390 nm [1] | Extracellular matrix [23] [16] | Prominent in connective tissues; most visible in green wavelengths [23] |
| Lipofuscin [23] [16] | Exc: 345-490 nm; Em: 460-670 nm [1] | Lysosomes of post-mitotic cells [16] | Broad spectrum interferes multiple channels; accumulates with aging [23] |
| Elastin [16] [1] | Exc: 350-450 nm; Em: 420-520 nm [1] | Blood vessels, skin, ECM [16] [1] | Affects blue to green emission range; common in vascular tissues |
| Tryptophan [1] | Exc: ~280 nm; Em: ~350 nm [1] | Most proteins [1] | Ubiquitous in protein structures; UV excitation |
Beyond biological components, several laboratory reagents and consumables contribute significantly to autofluorescence:
Table 2: Technical Sources of Autofluorescence
| Source | Common Examples | Alternative Solutions |
|---|---|---|
| Aldehyde Fixatives [16] | Formaldehyde, paraformaldehyde, glutaraldehyde | Use ice-cold methanol fixation [16] or treat with sodium borohydride [16] |
| Plastic Ware [16] | Culture flasks, microplates | Use glass-bottomed or nonfluorescent polymer containers [16] |
| Media Components [16] | Phenol red, fetal bovine serum | Use phenol red-free media for live-cell imaging [16] |
| Paper Labels [1] | Slides, container labels | Keep labels away from imaging areas or use non-fluorescent alternatives |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q: How can I quickly determine if my sample has problematic autofluorescence? [16]
A: Prepare an unstained control sample and process it identically to your experimental samples. Image this control using all your available filter sets and acquisition settings. Any signal detected represents autofluorescence that will contribute to background in your experimental samples [16].
Q: My specific signal is weak and overwhelmed by background. What are my options?
A: Several strategies can help:
- Switch to fluorophores in the near-infrared range (e.g., Cy7, Alexa Fluor 750) which are farther from common autofluorescence peaks [16] [1]
- Use chemical quenching with Sudan Black B or similar agents [23] [16]
- Consider fluorescence lifetime imaging microscopy (FLIM) to distinguish based on fluorescence decay characteristics rather than just intensity [9] [16]
- Optimize your fixation method - coagulating fixatives like acetone:methanol may reduce autofluorescence compared to aldehydes [23]
Q: What is the most advanced method for autofluorescence removal?
A: High-speed fluorescence lifetime imaging microscopy (FLIM) combined with phasor analysis represents a cutting-edge digital approach [9]. This method leverages the distinct lifetime-spectrum profiles of fluorophores to differentiate specific immunofluorescence signals from autofluorescence without chemical treatments that can affect signal integrity [9]. Recent implementations using GPU acceleration have addressed previous throughput limitations [9].
Q: How does autofluorescence directly impact drug discovery costs?
A: Autofluorescence increases research costs through:
- Extended optimization time for assay development
- Need for additional controls and validation experiments
- Potential for false leads based on inaccurate data
- Requirement for more sophisticated (and expensive) instrumentation
- Delays in project timelines due to troubleshooting and validation
Step-by-Step Troubleshooting Guide
Problem: High Background Autofluorescence
Possible Causes and Solutions:
Biological tissue with inherent fluorophores
Aldehyde-induced fluorescence
Non-optimal filter sets
- Solution: Choose filter sets that minimize overlap with autofluorescence spectra
- Solution: Use narrow bandpass filters to exclude broader autofluorescence emissions
Problem: Weak or No Specific Signal
Possible Causes and Solutions:
Autofluorescence masking specific signal
Fixation method compromising epitopes
- Solution: Test alternative fixatives (e.g., isopropanol, acetone, methanol, or 1:1 acetone methanol) [23]
- Solution: Optimize fixation time and temperature
Research Reagent Solutions
The following table summarizes key reagents and materials used to combat autofluorescence in research settings:
Table 3: Essential Research Reagents for Autofluorescence Management
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Sudan Black B [23] [16] | Chemical quencher that masks lipofuscin and eosinophilic autofluorescence [23] | Prepare as 0.3% in 70% ethanol; incubate 10 min post-fixation [23] |
| Sodium Borohydride [16] | Reduces fluorescent Schiff's bases formed by aldehyde fixation [16] | Use fresh 0.1% solution in PBS; 10-30 min treatment post-fixation [16] |
| Non-aldehyde Fixatives [23] [16] | Coagulating fixatives (methanol, acetone) that avoid aldehyde-induced fluorescence | Acetone:methanol (1:1) fixative demonstrated lower mean fluorescence intensities [23] |
| Near-Infrared Fluorophores [16] [1] | Dyes with excitation/emission >700 nm avoid common autofluorescence spectra | Examples: Cy7, Alexa Fluor 750; minimize spectral overlap with biological fluorophores [1] |
| Low Autofluorescence Optical Fibers [25] | Specialized fibers that reduce background in photometry applications | Do not require repeated bleaching unlike conventional fibers [25] |
| Ethyl Cinnamate (ECi) [26] | Non-hazardous optical clearing agent for tissue imaging | Less toxic alternative to BABB; suitable for clinical translation [26] |
Advanced Methodologies and Protocols
High-Speed FLIM with Phasor Analysis
Fluorescence lifetime imaging microscopy (FLIM) represents a powerful approach for autofluorescence separation that doesn't rely on chemical treatments. Recent advances in high-speed FLIM using GPU acceleration have made this technique more accessible for routine imaging [9].
Experimental Workflow:
Sample Preparation: Prepare tissue sections as usual for immunofluorescence, including fixation and antibody labeling with an appropriate fluorophore [9].
Reference Measurement: Acquire FLIM data from:
- Unstained tissue to create an autofluorescence reference phasor
- Fluorophore in solution to create an immunofluorescence reference phasor [9]
Data Acquisition: Image stained samples using a high-speed FLIM system with pulsed laser excitation and time-resolved detection [9].
Phasor Analysis: Transform fluorescence lifetime decays into phasor coordinates (G and S) using Fourier-like transformations [9].
Signal Separation: Calculate the fractional contribution of specific immunofluorescence using the geometrical relationship in phasor space:
- Fraction of IF = da / (da + d_i)
- Where d_a = distance to autofluorescence reference
- Where d_i = distance to immunofluorescence reference [9]
The following diagram illustrates this advanced workflow for autofluorescence separation:
Chemical Quenching Protocol
For laboratories without access to advanced instrumentation, chemical quenching remains a valuable and effective approach:
Sudan Black B Staining Protocol: [23]
Solution Preparation: Prepare 0.3% Sudan Black B in 70% ethanol. Stir in the dark for 2 hours to ensure complete dissolution [23].
Tissue Processing:
- Cut frozen tissue sections (6 µm) and adhere to microscope slides
- Air-dry overnight at room temperature
- Fix with appropriate fixative (e.g., 1:1 acetone methanol at -20°C for 5 minutes)
- Rehydrate with 0.05 M Tris buffer for 10 minutes [23]
Quenching Step:
- Incubate tissue sections with 100 µL of Sudan Black B solution
- Maintain at room temperature for 10 minutes in a humidified chamber
- Rinse with 70% ethanol to remove excess stain
- Wash for 5 minutes in 0.05 M Tris buffer with 0.2% Tween-20 and 0.9% NaCl [23]
Mounting and Imaging:
- Mount slides with anti-fade mounting medium such as ProLong Gold
- Image using standard fluorescence microscopy techniques [23]
Economic Impact and Future Directions
The economic implications of autofluorescence in drug discovery and diagnostics are substantial. Inefficient troubleshooting of autofluorescence issues leads to extended project timelines, wasted reagents, and potential misinterpretation of data that can direct research down unproductive paths. The implementation of robust autofluorescence management strategies, whether through chemical, optical, or computational approaches, represents a valuable investment in research quality and efficiency.
Emerging technologies like high-speed FLIM [9] and machine learning-enhanced tissue characterization [26] show particular promise for transforming autofluorescence from a nuisance to a source of additional biological information. These approaches not only suppress unwanted background but can also extract metabolic and structural information from the autofluorescence signals themselves, potentially creating new diagnostic parameters from previously problematic background signals [26].
As these technologies continue to develop and become more accessible, the research community can anticipate improved reliability in immunofluorescence assays, accelerated drug discovery pipelines, and enhanced diagnostic capabilities—ultimately reducing the economic burden currently imposed by autofluorescence in biomedical research and development.
Why is evaluating autofluorescence in unstained controls critical?
Autofluorescence is the non-specific, background fluorescence emitted by biological samples or reagents themselves, independent of your fluorescent labels [27]. Evaluating this in unstained controls is a critical first step because it allows you to measure this background level directly. Without this baseline, you cannot distinguish true positive signal from background, which can lead to false positives or mask weak but specific signals, compromising your entire dataset [28].
A properly evaluated unstained control serves as a foundational tool for troubleshooting high background and validating that the signals in your stained samples are specific [28].
Methods for Evaluation and Analysis
The optimal method for evaluating your unstained control depends on your instrumentation. The core principle is to process the unstained sample identically to your stained samples and analyze its fluorescence profile.
Flow Cytometry: Spectral and Conventional
For spectral flow cytometry, several software-driven methods exist to extract the autofluorescence signature from your unstained control [29]:
| Method | Ease of Use | Accuracy | Reproducibility | Best Use Case |
|---|---|---|---|---|
| FSC/SSC Gating | High | Low to Moderate [29] | Low to Moderate [29] | Homogeneous populations (e.g., lymphocytes) [29] |
| Treating AF as a Fluorophore | Moderate | High [29] | High [29] | Isolating intense, distinct AF (e.g., in macrophages) [29] |
| AF Explorer Tools | Low (Complex) | Very High (if used carefully) [29] | Variable [29] | Complex tissues with multiple cell types (e.g., lung, skin) [29] |
For conventional flow cytometry, the process involves comparing the fluorescence intensity of your unstained control to your stained sample in each channel. A significant shift in the stained sample indicates a specific signal over the autofluorescence background.
Fluorescence Microscopy
In microscopy, simply image your unstained control using the same exposure times, light intensity, and filter sets you plan to use for your stained samples. Look for any signal emanating from the tissue or cells themselves. This signal often has a characteristic appearance and may be uniform across the sample or associated with specific structures like mitochondria or lipofuscin granules.
Troubleshooting Common Scenarios
Problem: Weak or No Specific Signal
Potential Cause: Overwhelming autofluorescence is masking your specific signal. Solutions:
- Choose brighter fluorophores: Use fluorophores that are brighter than the autofluorescence background, typically in the far-red and near-infrared spectrum where tissue autofluorescence is lower [27].
- Use signal amplification: Consider methods like tyramide signal amplification (TSA) to enhance your specific signal above background levels [19].
Problem: High Background
Potential Cause: Sample autofluorescence is the primary contributor to background. Solutions:
- Validate with unstained control: Always include an unstained sample to establish the level of autofluorescence [28].
- Use chemical quenching: Aldehyde fixatives can induce autofluorescence. This can be reduced by treating fixed cells or tissues with a solution of sodium borohydride (e.g., 1% NaBH4 in PBS) [19].
- Check reagent age: Old fixatives, especially formaldehyde, can autofluoresce. Prepare fresh dilutions or use fresh, high-quality EM-grade glutaraldehyde from ampules [28].
- Image in a different channel: For low-abundance targets, image them using a longer-wavelength channel (e.g., far-red) where autofluorescence is generally lower [28].
Problem: Poor Data Quality in Spectral Flow Cytometry
Potential Cause: Incorrect autofluorescence extraction is distorting the unmixing of your panel's fluorophores. Solutions:
- Use the right AF extraction method: Don't rely solely on the default FSC/SSC gating for complex samples. Use the AF Explorer tool or treat AF as a fluorophore for more accurate results [29].
- Check similarity thresholds: When using AF Explorer tools, set a reasonable similarity threshold (e.g., 0.9) for vetting AF signatures; an overly strict threshold (e.g., 0.98) can lead to poor unmixing [29].
- Inspect extracted spectra: If your software allows, look at the normalized autofluorescence spectrum being extracted. This helps in panel design to avoid fluorophores whose spectra overlap heavily with the AF signature [29].
Experimental Workflow for Evaluation
The following workflow outlines the key steps for using an unstained control to diagnose and mitigate autofluorescence.
Research Reagent Solutions
This table lists key reagents mentioned in this guide that can help you manage autofluorescence.
| Item | Function | Example/Note |
|---|---|---|
| Sodium Borohydride (NaBH4) | Quenches autofluorescence induced by aldehyde-based fixation [19]. | Use a 1% solution in PBS; optimize treatment time [19]. |
| Anti-fade Mounting Medium | Reduces photobleaching during microscopy; helps preserve signal [28]. | e.g., ProLong Gold Antifade Reagent [28]. |
| EM-grade Glutaraldehyde | High-quality fixative that autofluoresces less if used fresh [28]. | Prepare fresh dilutions from ampules [28]. |
| Normal Serum | Blocking agent to reduce non-specific antibody binding and background [28]. | Use serum from the same species as the secondary antibody [28]. |
| Signal Amplification Kits | Enhance specific signal above background (e.g., TSA kits) [19]. | Useful for detecting low-abundance targets [19]. |
By systematically evaluating autofluorescence using your unstained controls and applying these troubleshooting strategies, you can significantly improve the quality and reliability of your immunofluorescence data.
Advanced Techniques for Autofluorescence Suppression: From Chemical Quenching to FLIM
Autofluorescence, the background fluorescence emitted naturally by tissues and biomaterials, presents a significant challenge in immunofluorescence research. It can obscure specific signals, leading to inaccurate data interpretation. Chemical quenching is a prevalent method to suppress this autofluorescence. This guide details the protocols for two primary chemical quenchers, Sudan Black B (SBB) and Sodium Borohydride (NaBH4), providing troubleshooting and FAQs to support researchers in obtaining clear and reliable imaging results.
Researcher's Toolkit: Essential Reagents and Materials
The following table summarizes the key reagents used for autofluorescence suppression, their primary functions, and important considerations for their use.
| Research Reagent | Primary Function in Autofluorescence Suppression | Key Considerations & Applications |
|---|---|---|
| Sudan Black B (SBB) | A lipophilic dye that quenches autofluorescence by absorbing scattered light and smoothing material surfaces to reduce light refraction [30]. It is particularly effective against lipofuscin and polymer scaffold autofluorescence [31] [32]. | - Concentration: Typically used at 0.1% - 0.3% in 70% ethanol [33] [31].- Application: Can be used as a pre-culture treatment for scaffolds or post-fixation for tissues [30] [31].- Caveat: Fluoresces in the far-red channel; consider this in multiplex panels [32]. |
| Sodium Borohydride (NaBH4) | A reducing agent that minimizes autofluorescence induced by aldehyde-based fixatives (e.g., formalin, glutaraldehyde) by reducing reactive Schiff bases [34] [32]. | - Concentration: Common concentrations range from 0.1% to 1% in aqueous solution [34].- Handling: Decomposes in water to produce hydrogen gas; solutions must be prepared fresh and reactions vented to prevent pressurization [34].- Efficacy: Reported to have variable effects across different sample types [32]. |
| TrueVIEW Autofluorescence Quenching Kit | A commercial reagent used to reduce autofluorescence from multiple causes, including aldehyde fixation and endogenous pigments [32]. | - Follow the manufacturer's protocol for specific tissue types and fixation methods. |
Detailed Experimental Protocols
Sudan Black B (SBB) Quenching Protocol
SBB is highly effective for quenching autofluorescence from lipids (lipofuscin) and various polymer scaffolds. The protocol can be adapted for either pre-culture treatment of scaffolds or post-fixation treatment of tissues.
SBB Solution Preparation
- Prepare a 0.1% - 0.3% (w/v) solution of Sudan Black B in 70% ethanol [33] [31].
- Dissolve completely by stirring or vortexing. The solution can be stored at room temperature, protected from light.
Application Workflow: Pre-culture vs. Post-fixation
Key Protocol Details
- Pre-culture Treatment for Live-Cell Imaging: This method is ideal for polymer scaffolds like polycaprolactone (PCL) or silk fibroin. Treating the scaffold with 0.3% SBB before cell seeding effectively suppresses autofluorescence for up to 28 days without significantly affecting cell viability, proliferation, or differentiation [31].
- Post-fixation Treatment for Tissues: After standard immunofluorescence staining (fixation, permeabilization, and antibody labeling), incubate the sample with 0.1% SBB in 70% ethanol for 20-30 minutes. This is followed by thorough washing before mounting [33] [30]. This method preserves specific fluorescent signals while reducing background.
Sodium Borohydride (NaBH4) Quenching Protocol
Sodium borohydride is used specifically to reduce autofluorescence caused by aldehyde-based fixatives.
NaBH4 Solution Preparation
- Prepare a fresh 1% (w/v) solution of Sodium Borohydride (NaBH4) in phosphate-buffered saline (PBS). Do not use Tris-based buffers as they can react with NaBH4 [34].
- The solution will begin bubbling upon dissolution due to the release of hydrogen gas. Prepare it immediately before use and keep it on ice.
Aldehyde-Induced Autofluorescence Quenching Workflow
Key Protocol Details
- Treatment: After aldehyde fixation and PBS washing, incubate the sample with the freshly prepared 1% NaBH4 solution. Treatment times are typically short (2-10 minutes) as prolonged exposure can damage tissue morphology [34] [32].
- Quenching and Washing: The reaction is quenched by washing the sample several times with PBS. Bubbling will occur during washes due to residual NaBH4.
- Safety Note: As NaBH4 decomposes in aqueous solutions to produce hydrogen gas, reactions must be vented to prevent pressurization of vessels [34].
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: Which quencher should I use for my specific autofluorescence problem?
- For aldehyde-fixed tissues: Start with Sodium Borohydride (NaBH4) to target the Schiff bases formed during fixation [32].
- For lipofuscin, lipids, or polymer scaffolds (e.g., PCL, silk): Sudan Black B (SBB) is the superior choice [30] [31] [32].
- For complex or mixed-source autofluorescence: Consider a combination of treatments or the use of commercial kits like TrueVIEW [32].
Q2: I am performing live-cell imaging in a 3D scaffold. Can I use these quenchers?
- Yes. Pre-culture treatment of your scaffold with SBB is specifically designed for this purpose. It quenches scaffold autofluorescence before cells are introduced, allowing for clear live-cell imaging without cytotoxic effects during the culture period [31].
Q3: SBB treatment weakened my specific immunofluorescence signal. What went wrong?
- This can happen with post-fixation SBB treatment, as it may slightly reduce the intensity of some fluorescent tags. To mitigate this:
- Ensure you are using the correct concentration (0.1% for post-fixation).
- Avoid over-incubating with SBB.
- Consider using brighter fluorophores or increasing antibody concentrations slightly.
Q4: My NaBH4 solution is bubbling vigorously. Is this normal?
- Yes, this is expected. NaBH4 reacts with water to produce hydrogen gas. This is why you must use fresh solutions, vent reaction containers, and not be alarmed by bubbling during the treatment or subsequent washes [34].
Troubleshooting Common Problems
The table below outlines common issues, their potential causes, and recommended solutions.
| Problem | Possible Cause | Solution |
|---|---|---|
| High background after SBB treatment | Insufficient washing after SBB application, leaving residual dye. | Increase the number and volume of washes (using 70% ethanol followed by PBS). |
| Loss of cell viability on SBB-treated scaffolds | SBB concentration used for pre-treatment is too high. | Titrate the SBB concentration. 0.3% is generally safe, but test lower concentrations like 0.1% for sensitive cell types [31]. |
| Poor autofluorescence reduction with NaBH4 | Solution was not prepared fresh and has degraded. NaBH4 is not effective for the type of autofluorescence in your sample. | Always prepare a fresh NaBH4 solution immediately before use. If the problem persists, your autofluorescence may not be aldehyde-induced; switch to SBB. |
| Tissue morphology appears damaged after NaBH4 | Treatment time was too long. | Reduce the incubation time with NaBH4 to 2-5 minutes. Aldehyde-induced autofluorescence is reduced quickly [32]. |
To ensure success in suppressing autofluorescence, adhere to the following best practices:
- Know Your Source: Identify the primary source of autofluorescence in your sample (e.g., fixative, lipofuscin, scaffold material) to select the appropriate quencher.
- Run Controls: Always include unstained controls and controls without the primary antibody to accurately assess the level and nature of autofluorescence.
- Consider Fluorophore Choice: If autofluorescence is strong in the green spectrum, using far-red fluorophores (e.g., CoraLite 647) can improve signal distinction [32].
- Fixation: Where possible, use paraformaldehyde instead of glutaraldehyde and fix for the minimum time required to reduce aldehyde-induced autofluorescence at the source [32].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: What is the primary benefit of using high-intensity white LED light for photobleaching? The primary benefit is the effective and near-total reduction of tissue autofluorescence, particularly from age-pigments like lipofuscin, which can overwhelm specific fluorescence signals in human tissue. This method is a simple, cost-effective protocol that significantly increases the signal-to-noise ratio without adversely affecting the target immunofluorescence signal or tissue integrity [14].
Q2: My tissue autofluorescence returns after deparaffinization and antigen retrieval. Is this normal? Yes, this is a known and quantitatively documented phenomenon. Even after successful initial photobleaching, the deparaffinization (DP) and antigen retrieval (AR) processes can significantly increase autofluorescence levels again. The protocol can be repeated post-DP/AR to suppress this newly induced autofluorescence [35].
Q3: How long does the white LED photobleaching process typically take? Protocol duration can vary. Some systems using high-power LEDs with cooling can achieve significant autofluorescence reduction in about 60 minutes [36]. Other methods may require longer exposure, but the use of a bleaching solution containing reagents like hydrogen peroxide can accelerate the process, reducing the required exposure time to just a few hours [35].
Q4: Can this method be used on highly autofluorescent tissue, like Alzheimer's disease brain samples? Yes. Research has demonstrated that this method is effective even in highly impacted pathological tissue such as Alzheimer's disease brain, which contains high levels of autofluorescent interference from lipofuscin [14].
Q5: Does intense LED illumination damage the tissue or the target epitopes? When properly configured, studies indicate no significant damage. One system employing filtered photobleaching to block damaging UV and IR wavelengths demonstrated that even after 20 rounds of photobleaching, tissue integrity was maintained and antibody binding was not impaired [37]. Proper cooling of the sample during extended illumination is also crucial to prevent heat-related damage [36].
Troubleshooting Common Problems
| Problem | Possible Cause | Solution |
|---|---|---|
| High background after DP/AR | DP/AR procedures chemically induce new autofluorescence. | Re-apply photobleaching after the DP/AR steps for a further 2-24 hours [35]. |
| Incomplete autofluorescence removal | Insufficient illumination time or low light power. | Increase exposure duration and ensure LEDs are high-power. Consider using an accelerating bleaching solution (e.g., with H₂O₂) [35]. |
| Sample overheating during bleaching | High-power LEDs generating excessive heat. | Use a system with a cooling mechanism, such as cooling fans or submerging slides in PBS in a cooled container [36]. |
| Low signal-to-noise in specific channels | Autofluorescence persists in certain emission ranges. | Photobleaching efficacy varies by wavelength; it is often most significant in the 450 nm and 520 nm channels. For other channels, consider combining with other techniques [35]. |
| Photobleaching of the specific IF signal | Excessive exposure or harsh conditions. | Use filtered photobleaching systems that remove damaging UV/IR light and optimize exposure time to target autofluorescence while preserving IF signals [37]. |
Experimental Protocols & Data
Standardized Photobleaching Protocol
This protocol summarizes the method of using high-intensity white LED light to reduce autofluorescence in formalin-fixed paraffin-embedded (FFPE) tissue sections prior to immunofluorescence staining [14] [35].
- Sectioning: Cut FFPE tissue sections to a thickness of 5 μm and mount on slides.
- Pre-bleaching Setup:
- Prepare a bleaching solution (optional accelerator): 4.5% (wt/vol) H₂O₂ and 20 mM NaOH in 1x PBS [35].
- Submerge the tissue slides in the solution within a petri dish or transparent container.
- Photobleaching:
- Illuminate slides using a high-power, full-spectrum white LED array. The setup should contain high-power LEDs (e.g., 30W per LED) [36].
- Duration: Expose slides to light for a duration between 1 to 24 hours, depending on the setup and tissue type. The use of an accelerating solution can reduce this time to 1-3 hours.
- Cooling: Ensure the setup includes cooling fans or is otherwise configured to prevent sample heating, which can damage tissue [36].
- Post-bleaching Processing:
- After illumination, rinse slides thoroughly with distilled water or PBS.
- Proceed with standard deparaffinization, antigen retrieval, and immunofluorescence staining protocols.
Note: For tissues that remain autofluorescent after DP/AR, a second, shorter round of photobleaching (2-24 hours) can be performed after these steps [35].
Quantitative Efficacy Data
The following table summarizes quantitative findings on the efficacy of LED photobleaching from published research:
| Tissue Type | LED Type / Power | Exposure Time | Key Efficacy Finding | Source |
|---|---|---|---|---|
| Human DRG & Alzheimer's Brain | High-intensity white LED | Not Specified | Near-total reduction of lipofuscin autofluorescence; no adverse effects on tissue integrity or target signal. | [14] |
| FFPE Human Tonsil | Multiwavelength LED Array | 24 hours | Consistent AF reduction across all emission channels; most significant reduction at 450 nm & 520 nm excitation. | [35] |
| Mouse Brain Sections | High-power Blue (475 nm) / Cool White LED (30W/LED) | 60 minutes | Autofluorescence from lipofuscin-like granules completely eliminated; required evaporative cooling. | [36] |
| FFPE Human Tissues (Various) | LED with H₂O₂ accelerator | 1-3 hours | Significant AF reduction achieved in a much shorter timeframe compared to overnight methods. | [35] |
Workflow Visualization
The diagram below illustrates the key decision points in the autofluorescence troubleshooting workflow using high-intensity LED photobleaching.
The Scientist's Toolkit
Research Reagent Solutions
The table below lists key materials and reagents used in the high-intensity LED photobleaching method for suppressing autofluorescence.
| Item | Function & Application | Key Notes |
|---|---|---|
| High-Power White LED Array | Provides intense, full-spectrum light to chemically bleach autofluorescent compounds like lipofuscin. | Systems with high-power LEDs (e.g., 30W per LED) and integrated cooling are most effective [14] [36]. |
| Accelerating Bleaching Solution (H₂O₂/NaOH) | A chemical assist that speeds up the photobleaching process, reducing exposure time from ~24h to 1-3h. | Typically contains 4.5% H₂O₂ and 20 mM NaOH in PBS [35]. |
| Active Cooling System | Prevents heat damage to tissue epitopes during extended high-power illumination. | Can include cooling fans or submerging slides in PBS to dissipate heat [36]. |
| Filtered Photobleaching System | A safer bleaching method that blocks damaging UV and IR wavelengths, preserving tissue and epitopes. | Enables multiple rounds of bleaching and staining without significant tissue degradation [37]. |
Core Concept: Why Far-Red and NIR Fluorophores Are the Solution
What is the fundamental advantage of using far-red and near-infrared (NIR) fluorophores to combat autofluorescence?
Autofluorescence is the background fluorescence inherent to biological samples that is not from your specific fluorescent stain. It presents a major challenge in techniques like immunohistochemistry (IHC) and immunocytochemistry (ICC) by reducing assay sensitivity and obscuring the detection of low-abundance targets [16]. This unwanted signal arises from many common endogenous sample components, including:
- Extracellular matrix proteins like collagen and elastin [16] [38].
- Metabolic coenzymes such as riboflavin, NADH, and flavins [16] [39].
- Cellular pigments including lipofuscin (which accumulates over time in post-mitotic cells), heme groups in red blood cells, and melanin [16] [40].
Critically, the spectral profile of this autofluorescence is predominantly in the blue to green spectrum, typically with emission maxima between 350-550 nm [16] [38] [41]. Far-red and NIR fluorophores, which have emission wavelengths starting around 650 nm and extending beyond 700 nm, emit light in a spectral region largely free from this background noise [42] [39] [41]. By shifting your detection to these longer wavelengths, you place your specific signal in a much cleaner channel, dramatically improving the signal-to-noise ratio [42].
Table 1: Comparison of Common Far-Red and NIR Fluorophores
| Fluorophore | Excitation Peak (nm) | Emission Peak (nm) | Key Characteristics |
|---|---|---|---|
| Alexa Fluor 647 | ~650 | ~668 | Bright, photostable; spectrally similar to Cy5 [43] [38] |
| Cy5 | ~649 | ~670 | Common cyanine dye; high extinction coefficient [43] [44] |
| CellTrace Far Red | 648 | 658 | Excitable with a 640 nm laser [43] |
| Alexa Fluor 700 | ~696 | ~719 | Part of the NIR Alexa Fluor dye family [42] |
| Cy7 | 750 | 773 | NIR cyanine dye; useful for deep tissue imaging [44] |
| DyLight 755 | ~754 | ~776 | NIR dye with emission above the visible spectrum [42] |
| APC/Fire 810 | N/A | ~810 | Tandem dye from BioLegend; emission in the NIR range [42] |
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: My negative control still shows background in the far-red channel. What could be causing this?
While autofluorescence is strongest in the green channel, it can sometimes have a broad tail into the red spectrum. Here are the primary culprits and solutions:
- Cause: Aldehyde Fixation. Formaldehyde and especially glutaraldehyde can generate fluorescent Schiff bases upon reaction with amines, creating a broad-spectrum background [40] [45].
- Solution: Use fresh, high-quality paraformaldehyde instead of glutaraldehyde, and keep fixation times to the minimum required for your sample [46] [40] [38]. After fixation, you can treat samples with a reducing agent like sodium borohydride (e.g., 0.1% in PBS) to reduce these fluorescent complexes [16] [40] [38].
- Cause: Lipofuscin. This "wear-and-tear" pigment fluoresces across a very broad range, including the far-red [16] [40].
- Cause: Red Blood Cells. The heme group in red blood cells has a porphyrin ring structure that autofluoresces [40].
FAQ 2: I am designing a multiplex panel. How should I assign my far-red fluorophore?
Strategic panel design is key to successful multiplexing. Follow these guidelines:
- Priority Assignment: Assign your brightest far-red or NIR fluorophores (e.g., Alexa Fluor 647, Cy5) to detect the lowest-abundance targets [42] [41]. This leverages the high signal-to-noise ratio of these channels to maximize your chance of detecting weak signals.
- Spectral Spillover: Be aware of spectral overlap. Fluorophores like Cy5 and Alexa Fluor 700, while both in the far-red, have distinct emission spectra. Use your instrument's spectral unmixing capabilities or choose filters carefully to minimize "spillover" of a strong signal into an adjacent detector [41] [45].
- Laser Availability: Ensure your imaging system or flow cytometer is equipped with lasers suitable for exciting your chosen far-red dyes. A 640 nm or 647 nm laser is standard for exciting dyes like Alexa Fluor 647 and Cy5, while true NIR dyes like Cy7 require longer-wavelength lasers (e.g., 750 nm) [43] [44].
FAQ 3: My far-red signal is weak or absent. How can I improve it?
A weak signal in any channel requires systematic troubleshooting.
- Verify Instrument Configuration: This is the first check. Ensure you are using the correct laser for excitation and that your emission filter is correctly matched to your fluorophore. For example, CellTrace Far Red is optimally excited by a 640 nm laser and detected with a 660/20 nm bandpass filter [43].
- Check Antibody Concentration and Incubation: The primary antibody may be too dilute. Titrate your antibody to find the optimal concentration and follow validated incubation protocols. For many antibodies, incubation at 4°C overnight provides optimal results [46].
- Confirm Sample Integrity: Protein antigenicity can be lost over time. Use freshly prepared slides or plates. Over-fixation can also mask epitopes; if suspected, optimize fixation time or perform antigen retrieval [46] [45].
- Consider Signal Amplification: For very low-abundance targets, even a bright fluorophore may not be sufficient. Consider using a signal amplification method, such as tyramide signal amplification (TSA), to boost your detection sensitivity [46].
The following workflow diagram summarizes the key decision points and actions for addressing autofluorescence using far-red and NIR fluorophores.
Research Reagent Solutions for Autofluorescence Troubleshooting
Table 2: Essential Reagents for Implementing Spectral Solutions
| Reagent / Material | Function / Purpose | Example Usage in Protocol |
|---|---|---|
| Far-Red/NIR Conjugated Antibodies | Primary or secondary antibodies conjugated to dyes (e.g., Alexa Fluor 647, Cy5) to shift detection away from autofluorescence. | Use according to datasheet recommendation for dilution; incubate in the dark [46] [38]. |
| Sodium Borohydride | Reducing agent that quenches autofluorescence caused by aldehyde-based fixatives. | Prepare a 0.1% solution in PBS; treat fixed samples for a short period (e.g., 10-30 mins) [16] [40]. |
| Sudan Black B | Lipophilic dye that quenches the broad-spectrum autofluorescence of lipofuscin. | Use a 0.1-0.3% solution in 70% ethanol; incubate before antibody staining [16] [40]. |
| Phenol Red-Free Media | Cell culture medium without phenol red, a source of background fluorescence for live-cell imaging. | Use for washing and imaging live cells to reduce background [16] [38]. |
| ProLong Gold Antifade Mountant | Anti-fade mounting medium that preserves fluorophore signal and reduces photobleaching. | Mount samples with this reagent and store slides in the dark before imaging [46]. |
| Glass-Bottomed Culture Dishes | Non-fluorescent imaging vessels that avoid the autofluorescence inherent to standard plastic [16]. | Use for live-cell or fixed-cell imaging instead of standard polystyrene plates or flasks [16] [38]. |
Core Principles of FLIM-FRET
What is the fundamental principle that allows FLIM-FRET to overcome autofluorescence limitations?
Fluorescence Lifetime Imaging Microscopy (FLIM) measures the average time a fluorophore remains in an excited state before emitting a photon, a property independent of fluorophore concentration and excitation light intensity [47] [48]. When combined with Förster Resonance Energy Transfer (FRET)—a non-radiative energy transfer process between fluorophores in close proximity (1-10 nm)—this technique can distinguish specific signals from background autofluorescence based on lifetime differences rather than intensity alone [49] [50]. Since autofluorescence often exhibits distinct, usually shorter, lifetime characteristics compared to targeted probes, FLIM-FRET provides a robust environment-insensitive method for isolating specific molecular interaction signals in complex biological environments like immunofluorescence studies [47] [51].
How does FLIM-FRET provide superior quantification for protein interactions compared to intensity-based methods?
In intensity-based FRET measurements, the apparent FRET efficiency (Eapp) conflates the intrinsic FRET efficiency (E) and the fraction of donor molecules undergoing FRET (fD), making it impossible to resolve these parameters separately [52]. FLIM-FRET directly measures the donor's fluorescence lifetime, which shortens upon FRET, allowing calculation of the intrinsic FRET efficiency (E) through the equation E = 1 - (τDA/τD), where τDA is the donor lifetime in the presence of acceptor and τD is the donor lifetime in the absence of acceptor [53] [54]. This lifetime-based measurement is independent of fluorophore concentration, excitation path length, and donor-acceptor stoichiometry, providing more reliable quantification of molecular interactions [52] [48].
Essential Research Reagent Solutions
Table 1: Key Reagents and Their Functions in FLIM-FRET Experiments
| Reagent Category | Specific Examples | Function in FLIM-FRET |
|---|---|---|
| Genetically Encoded Donors | CFP, Cerulean, GFP [52] [54] | Protein labeling; provides lifetime signal that shortens during FRET [50] |
| Genetically Encoded Acceptors | YFP, Venus [52] [54] | Energy acceptor from donor; enables distance measurement via FRET efficiency [50] |
| Synthetic Dye Pairs | Alexa Fluor 546/Alexa Fluor 647 [51] | Reduced autofluorescence; improved quantum yield for higher signal-to-noise [55] |
| FLIM-Based Biosensors | ERK FRET-FLIM biosensor [48] | Reporters for metabolic state, cellular microenvironment, and signaling activity [48] |
| Environmental Sensors | pH-, viscosity-, ion-sensitive dyes [47] [48] | Probing local microenvironmental conditions within cellular compartments [47] |
Troubleshooting Common Experimental Challenges
Table 2: Troubleshooting Guide for High-Speed FLIM-FRET Experiments
| Problem | Potential Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Low Signal-to-Noise Ratio | Low photon counts, high autofluorescence, photobleaching [55] | - Increase laser power within sample tolerance- Use brighter fluorophores (e.g., quantum dots)- Apply pixel-by-pixel autofluorescence correction [51] | - Use red-shifted dye pairs (e.g., Alexa Fluor 546/647) [51]- Optimize expression levels |
| Inaccurate FRET Efficiency | Non-interacting donor fraction, improper lifetime calculation [53] | - Use double-exponential decay analysis- Apply amplitude-weighted lifetime (τₘ) for calculations [53] | - Include donor-only controls in every experiment- Verify single-exponential donor decay in controls |
| Slow Acquisition Speed | Traditional TCSPC limitations, insufficient photon budget [52] | - Implement fast-gated CCD cameras or multifocal multiphoton systems [52]- Use phasor analysis for rapid processing [48] | - Utilize integrated systems like STELLARIS 8 FALCON for video-rate FLIM [48] |
| Spatially Varying Autofluorescence | Tissue heterogeneity, uneven dye penetration [51] | - Apply pixel-by-pixel autofluorescence correction algorithms- Use four-channel detection with auxiliary AF measurement [51] | - Incorporate cell-free calibration standards for spillover factors [51] |
| Multi-Exponential Decay Complexity | Multiple donor populations, environmental heterogeneity [53] | - Implement minimal fraction analysis (mfD) for dynamic studies [52]- Use phasor analysis for complex decay separation [48] | - Characterize donor behavior in controlled environments first |
Advanced Methodologies & Protocols
Protocol: Pixel-by-Pixel Autofluorescence Correction for Quantitative FRET
This protocol, adapted from Szabó et al. 2023, enables accurate FRET efficiency determination in samples with spatially varying autofluorescence [51]:
Four-Channel Image Acquisition:
- Collect images using four distinct detection channels:
- I₀: Autofluorescence channel (blue-shifted relative to donor)
- I₁: Donor channel (donor excitation/emission)
- I₂: FRET channel (donor excitation, acceptor emission)
- I₃: Acceptor channel (acceptor excitation/emission)
- Collect images using four distinct detection channels:
Background Subtraction:
- Measure instrument background on non-fluorescent slides
- Subtract background values from each corresponding channel
Spectral Spillover Factor Determination:
- Calculate spillover factors using donor-only and acceptor-only samples:
- S₁ = I₂ᴰ/I₁ᴰ (Donor spillinto FRET channel)
- S₂ = I₂ᴬ/I₃ᴬ (Acceptor spillinto FRET channel)
- B₁ = I₁ᴺˡ/I₀ᴺˡ (Autofluorescence in donor channel)
- Calculate spillover factors using donor-only and acceptor-only samples:
Pixel-by-Pixel Correction:
- Apply correction matrix to solve for true donor intensity (Iᴰ), acceptor intensity (Iᴬ), autofluorescence (AF), and FRET efficiency (E) using the equations:
- I₁ = AF·B₁ + Iᴰ(1-E) + Iᴬ·S₄ + Iᴰ·E·α·S₄/S₂
- I₂ = AF·B₂ + Iᴰ(1-E)·S₁ + Iᴬ·S₂ + Iᴰ·E·α
- Apply correction matrix to solve for true donor intensity (Iᴰ), acceptor intensity (Iᴬ), autofluorescence (AF), and FRET efficiency (E) using the equations:
FRET Efficiency Calculation:
- Compute corrected FRET efficiency values using the established relationships between quenched donor lifetime and energy transfer efficiency
Protocol: Double-Exponential Analysis for Accurate FRET Efficiency
This protocol addresses the common mistake of using single-exponential approximations when non-interacting donor fractions are present [53]:
Data Acquisition:
- Acquire time-domain FLIM data using TCSPC with sufficient photons for double-exponential fitting (>1000 photons/pixel recommended)
Decay Model Selection:
- Fit fluorescence decay to double-exponential model:
- I(t) = α₁exp(-t/τ₁) + α₂exp(-t/τ₂)
- where τ₁ is the FRETing donor lifetime, τ₂ is the non-FRETing donor lifetime
- Fit fluorescence decay to double-exponential model:
Lifetime Calculation:
- Calculate amplitude-weighted lifetime:
- τₘ = (α₁τ₁ + α₂τ₂)/(α₁ + α₂)
- Avoid intensity-weighted lifetime (τᵢ = (α₁τ₁² + α₂τ₂²)/(α₁τ₁ + α₂τ₂)) for FRET efficiency calculations
- Calculate amplitude-weighted lifetime:
FRET Efficiency Determination:
- Compute accurate FRET efficiency using:
- E = 1 - (τₘ/τ_D)
- where τ_D is the donor lifetime in absence of acceptor (typically equals τ₂)
- Compute accurate FRET efficiency using:
Frequently Asked Questions (FAQs)
Q: What is the minimum photon count required for reliable FLIM-FRET analysis? A: For single-exponential fitting, several hundred photons per pixel may suffice, but for double-exponential analysis needed in FRET systems with non-interacting fractions, >1000 photons/pixel is recommended. For fast acquisitions with limited photons, the minimal fraction of interacting donor (mfD) approach can provide quantitative information even with limited statistics [52].
Q: How can I distinguish true FRET from environmental effects on donor lifetime? A: Always include proper controls: (1) donor-only samples to establish baseline lifetime (τD), (2) acceptor-only samples to assess spectral bleed-through, and (3) unlabeled samples to characterize autofluorescence. Environmental effects typically cause uniform lifetime shifts across the sample, while FRET produces spatially distinct patterns corresponding to expected interaction sites [53] [54].
Q: What are the advantages of phasor analysis over traditional fitting for FLIM-FRET? A: Phasor analysis provides a graphical, fit-free approach to FLIM data analysis that is particularly valuable for rapid screening and complex multi-exponential decays. It enables straightforward separation of different lifetime populations and direct visualization of FRET efficiency changes, making it ideal for high-speed applications [48].
Q: Can FLIM-FRET be applied to clinical samples for immunotherapy response prediction? A: Yes, recent research has demonstrated FLIM-FRET's potential for quantifying PD-1/PD-L1 interactions in tumor samples, providing superior predictive value for immune checkpoint inhibitor response compared to traditional immunohistochemistry. This approach directly measures interaction rather than mere co-expression [49].
Q: What fluorophore pairs are most suitable for high-speed FLIM-FRET in autofluorescent samples? A: Red-shifted pairs like Alexa Fluor 546/Alexa Fluor 647 are preferred due to reduced autofluorescence in longer wavelengths. For genetic encoding, CyPet-YFP or mCherry-miRFP670 pairs offer improved separation from cellular autofluorescence [51] [55].
FAQs: Addressing Common Autofluorescence Challenges
1. What are the primary causes of autofluorescence in immunofluorescence samples? Autofluorescence stems from two main sources: endogenous biomolecules and fixation artifacts. Key endogenous fluorophores include lipofuscin (accumulates with age in lysosomes), collagen (structural protein emitting in blue region 300-450 nm), NADH (metabolic enzyme emitting around 450 nm), and heme groups in red blood cells [56] [57] [5]. Fixation-induced autofluorescence occurs when aldehyde fixatives like formalin or paraformaldehyde form Schiff bases through reactions with amine groups [56] [57].
2. How can I modify fixation protocols to minimize autofluorescence? To reduce fixation-induced autofluorescence: use paraformaldehyde instead of glutaraldehyde (glutaraldehyde > paraformaldehyde > formaldehyde in autofluorescence intensity), fix for the minimum time required to preserve tissue structure, and consider alternative fixatives like chilled (-20°C) ethanol or methanol, particularly for cell surface markers [56] [57] [5]. Aldehyde fixatives create protein cross-links that preserve tissue but generate broad-spectrum autofluorescence across blue, green, and red spectral ranges [57].
3. Which pre-staining treatments effectively reduce autofluorescence? Several chemical treatments can be applied to samples before antibody staining: Sudan Black B effectively reduces lipofuscin autofluorescence (though it fluoresces in far-red channel), sodium borohydride (with mixed results) decreases formalin-induced autofluorescence, and copper sulfate or ammonium chloride at low pH can reduce red blood cell autofluorescence [56] [58] [57]. Photobleaching with broad-spectrum white LED light before staining also effectively reduces various autofluorescence sources without affecting specific probe fluorescence [58].
4. How does fluorophore selection help overcome autofluorescence issues? Since autofluorescence often occurs in blue to green spectra (350-550 nm), selecting fluorophores emitting in red to far-red regions (620-750 nm) such as CoraLite594 or CoraLite647 helps distinguish specific signal from background [56] [57] [5]. Brighter fluorophores like phycoerythrin (PE) or allophycocyanin (APC) can also improve signal-to-background ratio against autofluorescence [5].
Table 1: Spectral properties of common autofluorescent compounds to inform fluorophore selection
| Autofluorescence Source | Emission Spectrum Range | Tissues/Conditions Where Prominent |
|---|---|---|
| Collagen | 300-450 nm (blue) | Ubiquitous structural protein [56] [57] |
| NADH | ~450 nm (blue-green) | Metabolically active tissues (liver) [56] [57] |
| Lipofuscin | 500-695 nm (broad spectrum) | Aging tissues, particularly brain, cardiac muscle, neurons [56] [58] |
| Formalin Fixation | Blue, green, and red spectrum | Aldehyde-fixed tissues, increases with heating/dehydration [56] [57] |
| Red Blood Cells (Heme) | Broad spectrum | Tissues with residual blood [56] [5] |
Comparative Analysis of Autofluorescence Reduction Methods
Table 2: Performance characteristics of different autofluorescence reduction techniques
| Method | Mechanism | Effect on Specific Signal | Limitations | Best For |
|---|---|---|---|---|
| Chemical Quenchers | Chemical binding to autofluorescent sources | May decrease specific signal [9] | Variable effectiveness; may require optimization [56] | Lipofuscin (Sudan Black B) [56] [57] |
| Photobleaching | Broad-spectrum light degrades fluorophores | Minimal effect [58] | Requires 24-48 hours pretreatment [58] | Postmitotic tissues, aged samples [58] |
| FLIM | Distinguishes signals by fluorescence lifetime differences | Preserves specific signal [9] | Requires specialized instrumentation [9] [59] | Research settings with appropriate equipment [9] |
| Spectral Unmixing | Digital separation based on spectral signatures | Preserves specific signal | Requires specialized systems [58] | Multiplexed experiments |
| Fixation Optimization | Minimizes Schiff base formation | Preserves specific signal | Limited effectiveness alone [56] [57] | All sample types as preventive measure |
Detailed Experimental Protocols
Protocol 1: Photobleaching with White LED Arrays
This protocol effectively reduces various autofluorescence sources, particularly lipofuscin in aged tissues [58].
Materials Needed:
- White phosphor LED desk lamp (with diffusers/opaque plastic removed)
- 100 mm × 100 mm transparent square petri dish (slide chamber)
- Tris-buffered saline (TBS: 150 mM NaCl, 50 mM Tris-Cl, pH 7.4)
- Sodium azide (10% stock solution)
- Reflective dome (aluminum foil-lined box)
- Scaffold to elevate slide chamber
Procedure:
- Construct photobleaching apparatus:
- Prepare azide-TBS solution (0.05% sodium azide in TBS) to prevent microbial growth
- Build scaffold to elevate slide chamber 5-10 cm above LED array
- Remove any diffusers from LED lamp to maximize light intensity
- Create reflective dome cover with aluminum foil-lined box
Photobleaching treatment:
- Pour 50 mL azide-TBS into slide chamber
- Submerge tissue sections mounted on glass slides in solution
- Cover apparatus with reflective dome
- Turn on LED lamp and incubate for 48 hours at 4°C
- For thicker tissues or high lipofuscin content, increase duration to 72 hours
Proceed with standard immunofluorescence:
- After photobleaching, perform antigen retrieval if needed
- Continue with standard blocking, antibody incubation, and washing steps
- Note: Photobleaching pretreatment does not affect specific antibody signal intensity [58]
Protocol 2: Chemical Treatment with Sudan Black B
This method specifically targets lipofuscin autofluorescence, which accumulates in aged tissues and has broad emission spectrum [56] [57].
Materials Needed:
- Sudan Black B working solution (0.1-0.3% in 70% ethanol)
- Phosphate-buffered saline (PBS)
- 70% ethanol
Procedure:
- Prepare Sudan Black B solution:
- Make saturated solution in 70% ethanol (approximately 0.3%)
- Filter through filter paper before use
- Prepare fresh for each experiment
Staining procedure:
- After rehydration and washing steps, incubate sections with Sudan Black B solution for 10-30 minutes
- Rinse thoroughly with 70% ethanol until no more color leaches out
- Wash extensively with PBS to remove residual ethanol
- Proceed with standard immunofluorescence protocol
Important considerations:
- Sudan Black B fluoresces in far-red channel—avoid using with far-red fluorophores [56]
- Optimal concentration and incubation time should be determined empirically for each tissue type
- Works by binding lipophilic compartments where lipofuscin accumulates
Protocol 3: Sodium Borohydride Treatment for Aldehyde-Induced Autofluorescence
This method reduces autofluorescence caused by Schiff base formation during aldehyde fixation [56] [57].
Materials Needed:
- Sodium borohydride (NaBH4) freshly prepared
- Phosphate-buffered saline (PBS), pH 7.4
- Containers for slide incubation
Procedure:
- Prepare sodium borohydride solution:
- Make 0.1% NaBH4 in PBS (1 mg/mL)
- Prepare fresh immediately before use as solution degrades rapidly
Treatment procedure:
- After deparaffinization and rehydration (for FFPE sections) or directly after fixation
- Incubate sections in NaBH4 solution for 30-60 minutes
- Rinse thoroughly with PBS (3 × 5 minutes)
- Proceed with standard immunofluorescence protocol
Important considerations:
Experimental Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential reagents for autofluorescence reduction and their applications
| Reagent | Function | Application Notes |
|---|---|---|
| Sudan Black B | Lipophilic dye that binds and quenches lipofuscin autofluorescence | Avoid with far-red fluorophores; use after fixation before antibody incubation [56] [57] |
| Sodium Borohydride | Reduces Schiff bases formed by aldehyde fixation | Fresh preparation critical; variable efficacy across tissues [56] [57] |
| TrueVIEW Kit | Commercial autofluorescence quenching kit | Effective for multiple autofluorescence sources; follows manufacturer protocol [5] |
| Copper Sulfate | Reduces red blood cell autofluorescence | Use with ammonium chloride at low pH [56] |
| Sodium Azide | Prevents microbial growth during extended photobleaching | Use in photobleaching buffer during LED treatment [58] |
| Eriochrome Black T | Alternative to Sudan Black B for lipofuscin and formalin autofluorescence | Similar application to Sudan Black B [57] |
| ProLong Gold Antifade | Mounting medium that reduces signal fading | Helps preserve specific signal during imaging [60] |
Advanced Technique: Fluorescence Lifetime Imaging Microscopy (FLIM)
For laboratories with specialized equipment, FLIM represents a powerful digital approach to autofluorescence separation that doesn't require chemical treatments [9] [59]. This technique leverages differences in fluorescence decay kinetics between specific immunofluorescence signals and autofluorescence.
Principle: FLIM uses the distinct lifetime-spectrum profiles of fluorophores as a unique fingerprint, separating signals in the lifetime-spectral domains [9]. The phasor analysis approach transforms fluorescence lifetime decays into coordinates that can be plotted to map lifetime clusters and distributions.
Implementation: High-speed FLIM systems with GPU acceleration can now perform this analysis in real-time, addressing previous limitations of slow data acquisition [9]. The fraction of specific immunofluorescence signal at each pixel is calculated based on geometrical relationships in phasor space between the sample pixel and reference phasors for both autofluorescence and specific fluorophore.
Advantages: Preserves specific signal integrity, requires no chemical modifications to samples, and provides quantitative separation of signals based on intrinsic photophysical properties [9].
Troubleshooting Autofluorescence: A Step-by-Step Protocol for Clearer Images
What is Autofluorescence and Why is it a Problem?
Autofluorescence is the background fluorescence emitted naturally by biological structures or sample preparation materials, independent of any fluorescent labels used in your experiment [61]. This inherent "glow" can obscure specific signals, reduce your signal-to-noise ratio, and lead to false-positive results or mask the detection of low-abundance targets [1] [62] [5].
The interference is particularly problematic in techniques like immunofluorescence and flow cytometry, where accurate signal detection is paramount [62]. For instance, in flow cytometry, autofluorescence can compromise the accurate definition of cellular phenotypes and hinder the resolution of dim signals [62].
FAQ: Common Questions on Autofluorescence
Q: What are the most common biological sources of autofluorescence? A: Numerous endogenous molecules contribute. Key sources include metabolic cofactors like NAD(P)H and flavins (FAD), structural proteins like collagen and elastin in the extracellular matrix, and pigments such as lipofuscin (which accumulates with age) and melanin [1] [61]. The table in the following section provides their specific spectral profiles.
Q: My sample was fine, but the background is high after fixation. What happened? A: This is a classic sign of fixative-induced autofluorescence. Aldehyde-based fixatives like formalin and glutaraldehyde react with proteins to form fluorescent Schiff bases [63] [5]. Glutaraldehyde is particularly problematic, but paraformaldehyde can also cause this issue [63].
Q: How can I quickly check if autofluorescence is affecting my experiment? A: Always run an unlabeled control. Process your sample identically to your experimental groups but omit the primary and secondary fluorescent antibodies. Imaging this control will reveal the level and pattern of background autofluorescence inherent to your sample [4] [5].
A Step-by-Step Diagnostic Workflow
Follow this systematic workflow to identify the source of autofluorescence in your samples. The diagram below outlines the logical process for pinpointing the cause.
Step 1: Initial Assessment with Unlabeled Controls
As highlighted in the FAQ, begin by preparing and imaging an unstained control. This is your baseline for identifying the presence and spatial distribution of autofluorescence [4]. When imaging, use the same channel settings (exposure time, laser power, gain) as you would for your experimental samples.
Step 2: Analyze the Signal Pattern and Color
The pattern and color of the signal in your control sample are key diagnostic clues.
- Signal in Specific Cellular or Tissue Structures: Points to a biological source. For example, a punctate pattern in cultured cells might indicate lipofuscin in lysosomes, while a fibrous network in tissues could be collagen [1].
- Uniform Signal Across the Sample: Often indicates fixative-induced autofluorescence from aldehyde-based fixatives [63].
- Signal Localized to the Plate or Well: Suggests the background is from the imaging dish or culture media (e.g., phenol red) [4].
Step 3: Identify the Source
Compare the emission color of your autofluorescence to the known spectra of common sources. The table below lists the excitation and emission peaks of major endogenous fluorophores to aid in this identification.
| Autofluorescence Source | Typical Excitation (nm) | Typical Emission (nm) | Common Location |
|---|---|---|---|
| NAD(P)H [1] [61] | ~340 | ~450 | Cytoplasm |
| Flavins (FAD) [1] [61] | ~380-490 | ~520-560 | Mitochondria |
| Collagen [1] [61] | ~270-370 | ~305-450 | Extracellular Matrix |
| Elastin [1] | ~350-450 | ~420-520 | Extracellular Matrix |
| Lipofuscin [1] [61] | ~410-490 | ~500-695 | Lysosomes (various cells) |
| Tryptophan [1] [61] | ~280 | ~300-350 | Most Proteins |
| Melanin [1] [61] | ~340-400 | ~360-560 | Skin, Hair, Eyes |
The Scientist's Toolkit: Research Reagent Solutions
Having identified the likely source, the next step is to apply a solution. This toolkit lists common reagents used to mitigate autofluorescence.
| Reagent | Primary Function | Common Application |
|---|---|---|
| Sodium Borohydride [63] [17] | Reduces fluorescent Schiff bases formed by aldehyde fixatives. | Treating aldehyde-fixed samples before staining. |
| Sudan Black B [63] | Lipophilic dye that quenches fluorescence from lipids and lipofuscin. | Incubating tissue sections or cells before staining. |
| TrueVIEW Kit [63] [5] | Commercial reagent that binds and quenches various autofluorescent elements. | Quenching autofluorescence in problematic tissues like kidney or spleen. |
| Copper Sulfate [63] | Treatment to reduce autofluorescence from heme groups and other pigments. | Immersing tissue sections in an aqueous solution. |
| Phenol Red-Free Medium [4] | Culture medium without the fluorescent pH indicator phenol red. | Live-cell imaging to reduce background from the medium. |
Detailed Experimental Protocols for Mitigation
Protocol 1: Reducing Aldehyde-Induced Autofluorescence with Sodium Borohydride
This protocol is effective for samples fixed with formaldehyde or glutaraldehyde [63] [17].
- After fixation and washing, prepare a fresh 0.1% to 1% (w/v) solution of sodium borohydride (NaBH4) in phosphate-buffered saline (PBS). Note: Prepare this solution immediately before use as it degrades rapidly. Bubbles will form.
- Incubate your samples in this solution for 30 minutes at 4°C.
- Wash the samples thoroughly with PBS (3 x 5 minutes) to remove all residues.
- Proceed with your standard immunofluorescence staining protocol.
Protocol 2: Quenching Lipofuscin and Lipid-Based Autofluorescence with Sudan Black B
This method is ideal for reducing autofluorescence from aged tissues, neurons, and liver samples [63].
- After completing your immunofluorescence staining and final wash, prepare a 0.1% to 0.3% (w/v) solution of Sudan Black B in 70% ethanol.
- Filter the solution to remove any undissolved particles.
- Incubate the stained samples in the Sudan Black B solution for 10-20 minutes at room temperature.
- Rinse the samples extensively with PBS to remove the dye.
- Mount the samples and proceed with imaging. Note: Sudan Black B can fluoresce in the far-red channel, so account for this in multiplex experiments [63].
Strategic and Technical Solutions
Beyond chemical treatments, several strategic choices can prevent autofluorescence.
- Choose Far-Red Fluorophores: Autofluorescence is most intense in the blue-green spectrum. Using dyes like Alexa Fluor 647, Coralite 647, or other far-red fluorophores can dramatically improve your signal-to-noise ratio [4] [63] [5].
- Optimize Fixation: Use the mildest fixation possible. Prefer fresh paraformaldehyde over glutaraldehyde, and fix for the minimum time required [63]. Consider ethanol or methanol fixation for cells [63] [5].
- Use Spectral Imaging and Unmixing: If your microscope is equipped, use a spectral detector to unmix the specific signal of your fluorophore from the overlapping autofluorescence background [4] [51].
- Employ Fluorescence Lifetime Imaging (FLIM): Autofluorescence and your fluorophore often have different fluorescence decay rates (lifetimes). FLIM can differentiate between them, even if their emission spectra overlap [4].
The following diagram summarizes the strategic solution pathways available after identifying the problem.
Frequently Asked Questions (FAQs)
1. Why is the signal-to-noise ratio critical in immunofluorescence, and what are its main components? A high signal-to-noise ratio is essential for obtaining clear, specific, and quantifiable data. The "signal" is the specific fluorescence from your antibody-bound fluorophore, while "noise" includes non-specific background staining and autofluorescence from the sample itself, which can obscure the target signal [5] [16].
2. How does antibody titration improve my immunofluorescence results? Using an incorrect antibody concentration is a primary cause of both weak signal and high background [64] [65]. Titration—testing a range of antibody concentrations—helps identify the optimal dilution that maximizes specific binding to your target (signal) while minimizing non-specific binding to other structures (noise) [17].
3. What is autofluorescence, and how can fluorophore selection help manage it? Autofluorescence is background fluorescence emitted by endogenous sample components like collagen, elastin, lipofuscin, and red blood cells, often in the green spectrum (350–550 nm) [5] [16]. Selecting fluorophores that emit in the red to far-red or near-infrared wavelengths (620–750 nm) moves your detection away from this noisy region, significantly improving contrast [5] [17].
4. Besides titration and dye choice, what are other effective ways to reduce background? Several strategies are effective:
- Thorough Blocking and Washing: Insufficient blocking or washing can leave behind non-specifically bound antibodies, increasing background [64] [65]. Ensure these steps are optimized.
- Use of Quenchers: Chemical agents like Sudan Black B, Trypan blue, or copper sulfate can be applied to tissues to quench autofluorescence [17] [16].
- Sample Preparation: Fixing samples with fresh aldehydes or alternatives like ice-cold methanol, and removing red blood cells via perfusion or lysis, can reduce inherent autofluorescence [5] [16].
Troubleshooting Guides
Problem: Weak or No Specific Signal
| Possible Cause | Recommendations |
|---|---|
| Incorrect antibody dilution | Consult the product datasheet for the recommended dilution and perform a titration experiment to find the optimal concentration for your specific sample [64] [65]. |
| Insufficient incubation time | Primary antibody incubation according to a rigorously tested protocol provides consistent, reliable results. Many antibodies are validated for optimal results when incubated at 4°C overnight [64]. |
| Inadequate permeabilization | If your target is intracellular, ensure cells are properly permeabilized. Methanol/acetone fixation permeabilizes; if using formaldehyde, add a permeabilization step with 0.2% Triton X-100 [65]. |
| Epitope damage from over-fixation | Reduce fixation duration or change the fixative. Perform antigen retrieval to unmask the epitope [65] [21]. |
| Low expression of target protein | Run a positive control. Modify your detection approach; consider signal amplification methods or pair your primary antibody with a brighter fluorophore [64] [65]. |
Problem: High Background Staining
| Possible Cause | Recommendations |
|---|---|
| Antibody concentration too high | A primary or secondary antibody that is too concentrated is a common cause of high background. Titrate antibodies to find a concentration that minimizes noise while retaining strong specific signal [64] [65]. |
| Sample autofluorescence | Run an unstained control to check levels. Use fluorophores emitting in the red/far-red spectrum. Consider chemical quenching (e.g., Sudan Black B) or treatment with sodium borohydride for aldehyde-fixed samples [64] [5] [17]. |
| Insufficient blocking | Increase the blocking incubation period and/or concentration. Use normal serum from the same species as the secondary antibody or a charge-based blocker [64] [65]. |
| Cross-reactivity of secondary antibody | Always include a secondary-only control (no primary antibody). If staining is observed, ensure your secondary antibody is matched to the host species of the primary and consider trying a different lot or source [64] [17]. |
| Insufficient washing | Non-specifically bound antibodies can be removed through proper washing. Ensure washing steps are thorough; increase volume, duration, or number of washes, and include a mild detergent like Tween-20 [64] [65]. |
Experimental Protocols
Protocol 1: Checkerboard Antibody Titration for Optimal Signal-to-Noise
Purpose: To systematically determine the optimal concentrations of both primary and secondary antibodies that yield the strongest specific signal with the lowest background.
Materials:
- Primary antibody
- Fluorophore-conjugated secondary antibody
- Fixed cell or tissue samples
- Blocking buffer (e.g., PBS with 1-5% BSA or serum)
- Wash buffer (e.g., PBS with 0.05% Tween-20)
- Mounting medium with antifade agent [64]
Method:
- Prepare Sample Matrix: Seed or section your samples into a multi-well plate or onto multi-well slides to ensure identical processing.
- Blocking: Block all samples with an appropriate blocking buffer for 1 hour at room temperature.
- Primary Antibody Dilution: Prepare a series of dilutions for your primary antibody (e.g., 1:50, 1:100, 1:200, 1:500) in blocking buffer. Apply each dilution to a separate sample. Include a control with no primary antibody (blocking buffer only).
- Incubation and Wash: Incubate according to your protocol (often 4°C overnight [64]), then wash thoroughly 3-5 times with wash buffer.
- Secondary Antibody Dilution: Prepare a series of dilutions for your secondary antibody (e.g., 1:200, 1:500, 1:1000). Apply these in a checkerboard pattern against the primary antibody dilutions.
- Incubation and Wash: Incubate for 1-2 hours at room temperature (protected from light), followed by thorough washing.
- Mount and Image: Mount samples using an antifade mounting medium [64]. Image all samples using identical microscope settings (exposure time, gain, laser power). Do not adjust settings to "make a dim signal brighter," as this will invalidate quantitative comparisons.
Analysis: Identify the combination of primary and secondary antibody dilutions that produces a bright, specific signal with the cleanest background. The no-primary control will reveal any non-specific binding from the secondary antibody.
Protocol 2: Systematic Evaluation and Reduction of Autofluorescence
Purpose: To identify the source and level of autofluorescence in a sample and apply a quenching method to suppress it.
Materials:
- Untreated (unstained) control sample
- Sodium borohydride (NaBH₄)
- Sudan Black B solution (or similar quenching agent)
- Phosphate Buffered Saline (PBS)
Method:
- Identify Autofluorescence:
- Chemical Quenching (Example with Sodium Borohydride for Aldehyde Fixation):
- After fixation and washing, prepare a fresh solution of sodium borohydride (1 mg/mL) in ice-cold PBS [17].
- Incubate the sample in this solution for 10-30 minutes.
- Wash the sample thoroughly with PBS before proceeding to blocking and immunostaining.
- Chemical Quenching (Example with Sudan Black B):
- After completing all immunostaining and final washes, incubate the sample with a Sudan Black B solution (concentration typically 0.1-0.3% in 70% ethanol) for 5-30 minutes [16].
- Rinse the sample thoroughly with PBS or the recommended buffer to remove excess dye.
- Mount and image the sample promptly.
Analysis: Compare the intensity in the unstained control channels before and after quenching. Successful treatment will significantly reduce the background signal in the unstained control, thereby improving the signal-to-noise ratio in your stained samples.
Visual Workflows and Pathways
Signal-to-Noise Optimization Strategy
Autofluorescence Mitigation Decision Tree
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Benefit |
|---|---|
| Anti-fade Mounting Medium (e.g., ProLong Gold) | Presves fluorescence signal during imaging and storage by reducing photobleaching caused by exposure to light [64]. |
| Serum from Secondary Host | Used for blocking to prevent non-specific binding of the secondary antibody, effectively reducing background [64] [21]. |
| Chemical Quenchers (e.g., Sudan Black B, Trypan Blue) | Applied to samples to suppress autofluorescence from endogenous biomolecules or fixatives, improving signal clarity [17] [16]. |
| Bright, Photostable Fluorophores (e.g., Alexa Fluor dyes) | Provide strong signal, allowing for lower antibody concentrations and reduced background. Dyes in the red/far-red spectrum avoid common autofluorescence channels [5] [17]. |
| Sodium Borohydride (NaBH₄) | Specifically reduces autofluorescence caused by aldehyde-based fixatives (e.g., formaldehyde, glutaraldehyde) by neutralizing Schiff's bases [5] [16]. |
| Triton X-100 or Saponin | Detergents used for permeabilizing cell membranes after aldehyde fixation, allowing antibodies to access intracellular targets [65]. |
Immunofluorescence (IF) is a powerful tool for visualizing protein expression and tissue architecture. However, its effectiveness is often compromised by tissue-specific challenges, with autofluorescence being a primary obstacle. Autofluorescence describes background fluorescence not attributed to specific antibody-fluorophore interactions, and it can severely obscure target signals, especially for low-abundance proteins [66]. This technical support guide outlines tailored protocols and troubleshooting strategies for obtaining clear and reliable results from liver, brain, and aged tissues, which are notoriously prone to high autofluorescence.
Tissue-Specific Challenges and Solutions
Different tissues present unique obstacles for immunofluorescence. The table below summarizes the primary challenges and tailored solutions for liver, brain, and aged tissues.
Table 1: Tissue-Specific Autofluorescence Challenges and Solutions
| Tissue Type | Primary Sources of Autofluorescence | Recommended Solutions |
|---|---|---|
| Liver | Lipofuscin, vitamin A, lipid droplets [67] | - Use of Sudan Black B (1% in 70% ethanol) to quench background [67] [66].- Employ thick vibratome sections (100-200 µm) for 3D structural analysis [67].- Choose far-red fluorophores (e.g., Alexa Fluor 647) to avoid background in the blue/green spectrum [66]. |
| Brain | Lipofuscin (accumulates with age), neurotransmitters, myelin [66] | - Sudan Black B treatment is highly effective against lipofuscin [66].- For aldehyde-induced fluorescence, consider sodium borohydride treatment (with variable results) [66].- Perfuse with PBS prior to fixation to remove red blood cells [66]. |
| Aged Tissues | Widespread accumulation of lipofuscin, a granular pigment that fluoresces across multiple wavelengths (500-695 nm) [66] | - Sudan Black B is the most effective method for reducing lipofuscin autofluorescence [66].- Use commercial autofluorescence quenching reagents like TrueVIEW [66].- Optimize fixation time; longer fixation can increase autofluorescence [66]. |
Experimental Protocols
Optimized Protocol for Liver Tissue
This protocol is specifically designed to overcome the high autofluorescence and complex 3D architecture of the liver [67].
1. Tissue Preparation and Sectioning
- Fixation: Fix fresh liver tissues in 4% Paraformaldehyde (PFA) for 48 hours at 4°C to preserve structure and protein epitopes [67].
- Washing: Rinse fixed tissues three times with Tris-buffered saline (TBS) or PBS to remove residual PFA [67].
- Sectioning: For 3D architectural analysis, cut 100-200 µm thick sections using a vibratome. This thickness allows for the visualization of entire hepatocytes (20-30 µm in diameter) and branching sinusoidal networks [67].
- Optional Agarose Embedding for Vibratome: Embed the liver lobe in 4% agarose in TBS/PBS. Once set, trim the block and section [67].
2. Autofluorescence Quenching
- After sectioning, treat tissues with a 1% solution of Sudan Black B in 70% ethanol for an appropriate time (e.g., 10-30 minutes) to quench signals from lipids and lipofuscin [67] [66].
- Note: Sudan Black B fluoresces in the far-red channel; consider this when designing multiplex panels [66].
3. Antigen Retrieval
- Choose an antigen retrieval method and buffer based on the primary antibody's requirements. Common options include:
- Citrate Buffer (pH 6.0)
- Tris-EDTA Buffer (pH 9.0) [67]
- Heat slides in the chosen buffer at 95°C for 12-20 minutes using a water bath, microwave, or pressure cooker, then allow to cool slowly to room temperature [68] [67].
4. Immunostaining
- Blocking: Incubate sections in a blocking solution, such as 4% Bovine Serum Albumin (BSA) in TBS, for 1 hour at room temperature [67].
- Primary Antibody Incubation: Incubate with appropriately titrated primary antibody diluted in blocking solution at 4°C overnight for optimal signal and low background [67] [69].
- Washing: Wash sections with IF wash buffer (e.g., TBS with 0.01% Triton X-100, 0.025% Tween 20, 0.05% BSA) [67].
- Secondary Antibody Incubation: Incubate with fluorophore-conjugated secondary antibodies (e.g., diluted 1:500 in blocking solution) for 1-2 hours at room temperature, protected from light [67].
- Nuclear Staining: Incubate with DAPI (e.g., 1:1000 dilution) for 5-10 minutes [67].
5. Mounting and Imaging
- Mount sections using an anti-fade mounting medium such as Mowiol, Vectashield, or ProLong Gold [67].
- Image using a confocal microscope capable of optical sectioning to fully leverage the 3D information in thick sections [67].
Optimized Liver Immunofluorescence Workflow
General Best Practices for Brain and Aged Tissues
While the liver protocol provides a foundation, the following adjustments are critical for brain and aged tissues.
- Fixation: For all tissues, fix for the minimum time required with 4% PFA instead of glutaraldehyde to reduce aldehyde-induced autofluorescence. Over-fixation can increase background [66].
- Autofluorescence Quenching: For brain and aged tissues rich in lipofuscin, incorporate a Sudan Black B quenching step as described in the liver protocol. This is the most effective method for these tissues [66].
- Washing: After fixation and between all antibody incubation steps, perform thorough washes (3-4 times, 5-10 minutes each) with PBS or a specialized immunostaining wash buffer to remove unbound reagents and reduce background [68] [70].
- Antibody Titration: Always titrate your primary and secondary antibodies using positive and negative control samples. The optimal dilution provides the highest signal-to-noise ratio, not just the strongest signal [69] [71].
- Control Experiments: Always include controls to distinguish specific signal from background:
The Scientist's Toolkit: Key Reagents and Materials
The following table lists essential reagents for implementing the protocols described above, particularly for challenging tissues.
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function / Application | Specific Examples / Notes |
|---|---|---|
| Sudan Black B [67] [66] | Quenches autofluorescence from lipofuscin and lipids in liver, brain, and aged tissues. | Use a 1% solution in 70% ethanol. Note: it fluoresces in the far-red channel. |
| TrueVIEW [66] | Commercial reagent to reduce autofluorescence from multiple causes. | An alternative to Sudan Black B. |
| Far-Red Fluorophores (e.g., Alexa Fluor 647, CoraLite 647) [66] | Emit light in a spectrum farther from common autofluorescence (which is often in the blue/green). | Ideal for tissues with high native fluorescence like liver and aged tissues. |
| Triton X-100 [68] [67] | Detergent used for permeabilizing cell membranes to allow antibody entry. | Typically used at 0.1-0.5% concentration. |
| Bovine Serum Albumin (BSA) [67] | Protein used in blocking buffers to prevent non-specific antibody binding. | Use at 1-5% concentration. Ensure it is IgG-free to prevent background [71]. |
| Normal Serum [68] [72] | Used for blocking; should be from the same species as the secondary antibody. | |
| Sodium Borohydride [66] | Can reduce autofluorescence induced by aldehyde fixatives. | Results can be variable; not always well-recommended. |
| Anti-fade Mounting Medium (e.g., ProLong Gold, Mowiol, Vectashield) [67] [70] | Preserves fluorescence signal during storage and imaging by reducing photobleaching. | Critical for maintaining signal integrity, especially for long imaging sessions. |
Frequently Asked Questions (FAQs)
Q1: My immunofluorescence signal is weak or absent, even though I know my target is expressed. What should I check?
- Antibody Titration and Incubation: Confirm you are using the correct antibody dilution and that incubation is done at 4°C overnight for optimal results [69]. Shorter incubations at higher temperatures can yield weaker signals [69].
- Fixation and Permeabilization: Ensure fixation is sufficient (e.g., with at least 4% formaldehyde) and that the correct permeabilization agent (e.g., 0.1% Triton X-100) and method are used for your intracellular target [70] [73].
- Antigen Retrieval: For formalin-fixed tissues, epitopes are often masked. Perform an antigen retrieval step tailored to your antibody (e.g., with citrate or Tris-EDTA buffer at high temperature) [67] [72].
- Sample Age: Use freshly prepared samples, as stored samples can lose antigenicity [70].
Q2: I have high background staining across my entire tissue section. How can I reduce this?
- Identify the Source: First, run a no-primary-antibody control. If background is high, the issue is likely non-specific binding of the secondary antibody or autofluorescence [71].
- Improve Blocking and Washes: Ensure you are using an effective blocking agent (e.g., serum from the secondary host species or BSA) and increase the blocking time. Perform thorough washes between steps [70] [72] [71].
- Optimize Antibody Concentration: High background is often caused by excessively concentrated primary or secondary antibodies. Re-titrate your antibodies to find the optimal signal-to-noise ratio [69] [71].
- Quench Autofluorescence: If the background is from the tissue itself (e.g., in liver or aged tissues), incorporate a Sudan Black B quenching step into your protocol [67] [66].
Q3: How can I design a robust multi-color immunofluorescence (mIF) experiment for complex tissues?
- Check Antibody Host Species: For multiplexing, ensure your primary antibodies are raised in different host species (e.g., rabbit and mouse) to prevent cross-reactivity of secondary antibodies [72].
- Use Validated Panels: Consult published resources like Optimized Multicolor Immunofluorescence Panels (OMIPs) to leverage pre-validated antibody and fluorophore combinations [74].
- Mind Spectral Overlap: Choose fluorophores with well-separated emission spectra to minimize bleed-through. Consider using far-red fluorophores to avoid autofluorescence [66].
- Leverage Advanced Technologies: For highly multiplexed experiments (4-7 targets), consider using a commercial system based on Tyramide Signal Amplification (TSA), which allows for sequential staining and signal amplification on a single slide [75].
Q4: What are the best practices for preserving my fluorescent signals during imaging and storage?
- Prevent Photobleaching: Always store and incubate stained samples in the dark. Use an anti-fade mounting medium like ProLong Gold during slide preparation to slow signal decay [68] [70].
- Image Promptly: For the best results, image your slides immediately after mounting and sealing them [70].
Troubleshooting High Background in Immunofluorescence
Autofluorescence (AF) is the background fluorescence emitted naturally by tissues and cells, which can severely compromise the clarity and specificity of immunofluorescence (IF) experiments. This inherent fluorescence is caused by various endogenous fluorophores such as lipofuscin, collagen, elastin, and redox co-factors (FAD, FMN, NADH) [76] [77]. In intestinal tissue, for example, autofluorescent pigments are often caused by eosinophils and lipofuscin [23]. This background signal is particularly problematic when it spectrally overlaps with the fluorophores used in your experiment, making it difficult to discern specific antibody labeling from non-specific background [23] [77]. Effectively managing autofluorescence requires a integrated approach combining chemical, optical, and digital solutions.
Chemical and Reagent-Based Quenching Methods
Chemical methods work by physically blocking or quenching the autofluorescent compounds present in tissues. The following table summarizes the primary reagent-based solutions.
Table 1: Chemical Reagents for Autofluorescence Quenching
| Method | Primary Use/Target | Mechanism of Action | Key Considerations |
|---|---|---|---|
| Sudan Black B (SBB) [23] [77] | Lipofuscin, fatty pigments | Lipophilic dye that stains lipids and lipofuscin black, masking their fluorescence [23]. | Effective in healthy and diseased organs (e.g., kidney, brain, pancreas) [77]. |
| Copper Sulfate [77] | Lipofuscin, general reduction | Cu²⁺ ions receive excited electrons from fluorophores like lipofuscin via collisional contact, preventing fluorescence emission [77]. | Originally established for use in brain sections [77]. |
| TrueVIEW Autofluorescence Quenching Kit [78] | Aldehyde-induced AF, collagen, elastin, RBCs | Electrostatic binding to hydrophilic compounds to quench endogenous autofluorescence [78]. | Not effective against lipofuscin. Applied after IF staining; tissue may turn blue, which is normal [78]. |
| Sodium Borohydride [76] | Aldehyde-induced AF | Reduces free aldehyde groups from aldehyde-based fixatives (e.g., glutaraldehyde) [76]. | Prepare fresh solutions for optimal effect. |
Experimental Protocol: Combined Sudan Black B and DAB Treatment
This protocol, adapted from scientific literature, successfully masks autofluorescent pigments in frozen intestinal tissue sections [23].
- Tissue Preparation: Cut and air-dry frozen tissue sections (e.g., 6 µm) on microscope slides.
- Rehydration: Rehydrate the slides in an appropriate buffer (e.g., 0.05 M Tris buffer) for 10 minutes.
- Histochemical Staining:
- Prepare a 0.3% solution of Sudan Black B (SBB) in 70% ethanol and stir for 2 hours in the dark [23].
- Prepare 3,3’-Diaminobenzidine (DAB) according to the manufacturer's instructions.
- Incubate tissue sections with 100 µL of the DAB solution for 10 minutes at room temperature.
- Without rinsing, incubate with 100 µL of the SBB solution for 10 minutes at room temperature.
- Washing:
- Rinse slides incubated with SBB with 70% ethanol.
- Wash all slides for 5 minutes in a wash buffer (e.g., 0.05 M Tris buffer with 0.2% Tween-20 and 0.9% NaCl).
- Proceed with Immunofluorescence: Continue with the standard immunofluorescence protocol, including blocking, primary and secondary antibody incubation.
Optical and Microscope-Based Solutions
Optimizing your optical system and imaging workflow is crucial for minimizing the impact of autofluorescence.
Table 2: Optical Techniques for Autofluorescence Management
| Method | Description | Application Tip |
|---|---|---|
| Spectral Imaging & Unmixing [23] [29] | Software separates the specific fluorescent signal from the background autofluorescence based on their distinct spectral signatures. | Success depends on tissue and labeling quality. Requires a spectral microscope or imaging system [23]. |
| Filter Selection | Using narrow bandpass filters that precisely match your fluorophore's emission peaks can reduce bleed-through from broad-spectrum autofluorescence. | Avoid filter sets that capture the strong green autofluorescence from collagen and elastin if you are not using a green fluorophore [23]. |
| Longer Wavelength Fluorophores [79] [80] | Autofluorescence is often more intense in green (e.g., 500-550 nm) wavelengths. Using red and far-red dyes (e.g., Cy5, APC) can improve signal-to-noise. | Choose longer wavelength channels for low-abundance targets [79]. Phycoerythrin (PE) can outperform FITC and APC in flow cytometry for microglia due to AF interference [80]. |
| Control Samples | Imaging an unstained or no-primary-antibody control section is essential to identify and document the level and color of autofluorescence. | Use this control to set imaging parameters and for background subtraction during processing. |
Optical path for minimizing autofluorescence.
Digital and Post-Processing Methods
After image acquisition, digital tools can be used to subtract or separate the autofluorescence signal.
- Spectral Unmixing: This is a powerful digital method that can be performed after image acquisition on spectral confocal systems. It uses the unique spectral signature of both the fluorophores and the autofluorescence (obtained from control samples) to mathematically "unmix" the signals, creating a clean image with the autofluorescence removed [23] [29].
- Background Subtraction: Simple background subtraction in image analysis software can be effective if the autofluorescence is uniform. This involves measuring the intensity in an area of background (no specific staining) and subtracting that value from the entire image.
- Flow Cytometry AF Extraction: In spectral flow cytometry, several software methods exist to handle autofluorescence [29]:
- FSC/SSC Gating: The simplest method, where the software uses the median fluorescence of an unstained cell population from a scatter gate as the AF signature to subtract.
- Treating AF as a Fluorophore: Manually defining a specific AF signature from highly autofluorescent cells and adding it to the panel as a separate "fluorophore" for unmixing.
- AF Explorer Tools: Advanced tools that allow gating on multiple cell populations to extract different AF signatures for more accurate subtraction in complex samples.
The Scientist's Toolkit: Essential Reagents
Table 3: Key Research Reagents for Autofluorescence Quenching
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| Sudan Black B [23] [77] | Lipophilic dye that masks fluorescence from lipofuscin and other lipids. | Quenching AF in macrophages and microglia in brain, pancreas, and intestinal tissues. |
| TrueVIEW Quenching Kit [78] | Commercial kit to quench AF from aldehyde fixation, collagen, elastin, and RBCs. | Improving signal-to-noise in spleen, kidney, and tonsil FFPE tissue sections. |
| Vector VECTASHIELD Vibrance [78] | Antifade mounting medium. Crucial for maintaining signal-to-noise when used with the TrueVIEW kit. | Mounting samples after TrueVIEW treatment; substitution with other media may yield poor results. |
| Sodium Borohydride [76] | Reduces free aldehyde groups from fixatives that cause AF. | Treating tissues fixed with glutaraldehyde or old formaldehyde. |
| Copper Sulfate [77] | Quenches AF via collisional contact with fluorophores like lipofuscin. | Reducing AF in erythrocytes and immune cells in colonic tissues. |
| ProLong Gold Antifade Mountant [23] [79] | Antifade reagent that reduces photobleaching, preserving the specific fluorescent signal. | General mounting of IF samples to preserve signal during imaging and storage. |
Integrated Workflow and Decision Guide
The most effective strategy often combines multiple methods. The following diagram provides a step-by-step workflow for integrating chemical, optical, and digital solutions.
Integrated workflow combining chemical, optical, and digital methods.
Frequently Asked Questions (FAQs)
Q1: My tissue has high green autofluorescence, but I need to use a green fluorophore (like FITC). What should I do? Try a combination approach. First, use a chemical quencher like Sudan Black B or TrueVIEW Kit if the source is not lipofuscin. For imaging, use spectral unmixing if available. If not, ensure you have a high-quality unstained control to set your background levels accurately. As a last resort, consider switching your target to a channel with less interference using a different antibody conjugate [23] [78] [79].
Q2: When should I apply the TrueVIEW Autofluorescence Quenching Kit in my protocol? The TrueVIEW kit is designed to be applied after you have completed your entire immunofluorescence staining procedure, just before you mount the slides with the provided VECTASHIELD Vibrance mounting medium [78].
Q3: Does autofluorescence only affect immunofluorescence microscopy? No, autofluorescence is a significant concern in other fluorescence-based techniques. It can interfere with flow cytometry analysis, necessitating the use of fluorophores like PE that overcome AF interference or spectral unmixing tools [80]. It also affects live-cell imaging, where autofluorescent granules can reduce the amplitude of measured signals, such as calcium transients in microglia [80].
Q4: I treated my sample, but the signal is still weak relative to the background. What are my options? First, ensure your antibodies and staining protocol are optimized. If background persists, consider the following:
- Re-optimize antibody concentrations: High antibody concentrations can increase non-specific background [76] [79].
- Increase blocking: Use normal serum from the same species as your secondary antibody and consider extending the blocking incubation time [23] [79].
- Enhance washing: Implement more stringent or frequent washing steps between incubations to remove loosely bound antibodies [76] [79].
- Use signal amplification: If the specific signal is truly weak, a signal amplification system may help boost it above the background.
FAQs: Addressing Common Autofluorescence Challenges
What is the most common mistake in sample preparation that causes autofluorescence?
The most common mistake is the overuse of aldehyde-based fixatives, particularly glutaraldehyde, and fixing samples for longer than necessary. Aldehyde fixatives react with amines in proteins to form fluorescent Schiff bases, which emit a broad-spectrum signal that can mask specific staining [81] [82] [57]. Fixation-induced autofluorescence increases with higher concentrations and longer exposure durations.
How to Prevent It:
- Use the lowest effective concentration of paraformaldehyde instead of glutaraldehyde [82] [57].
- Titrate the fixative concentration; for example, a 0.5% PFA solution may work as well as 4% [81].
- Fix samples for the minimum amount of time required to preserve tissue architecture [83] [57].
Why is my background still high even after following a standard staining protocol?
High background can persist due to unaddressed endogenous factors in your tissue sample. Common culprits are red blood cells (RBCs), dead cells, and endogenous pigments like lipofuscin, collagen, and NADH [81] [5] [82]. The heme group in RBCs has a porphyrin ring that autofluoresces broadly, while dead cells and cellular debris bind reagents non-specifically and fluoresce more intensely than live cells [81] [5].
How to Prevent It:
- Remove RBCs: For whole blood, use an RBC lysis buffer and ensure thorough washing to remove lysed contents [81] [5]. For tissues, perfuse with PBS prior to fixation if possible [5] [83].
- Eliminate dead cells: Use low-speed centrifugation, Ficoll gradient centrifugation, or DNase I incubation to remove dead cells and debris [81]. Include a live/dead cell viability dye in your staining panel to gate out dead cells during analysis [81] [5].
- Quench endogenous pigments: Use chemical quenchers like Sudan Black B to reduce autofluorescence from lipofuscin and other sources [9] [82] [57].
I am using the right filters, but my signal is still weak. What am I doing wrong?
A weak specific signal can be overwhelmed by autofluorescence if you are using dim fluorophores that emit in the blue-green spectrum, where autofluorescence is most intense [81] [5]. Cellular components like collagen and NADPH naturally absorb and emit light in the 350-550 nm range, which overlaps with common dyes like FITC, GFP, and Pacific Blue [81].
How to Prevent It:
- Shift your panel to the red: Choose bright, photostable fluorophores that emit in the red and far-red regions (e.g., PE, APC, Alexa Fluor 594, Alexa Fluor 647) [81] [17] [5].
- Use the brightest fluorophores available: For targets expressed on autofluorescent cells (e.g., neutrophils), bright dyes like PE and APC can make the autofluorescence irrelevant by providing a strong specific signal [81].
- Validate with controls: Always include an unstained control and a secondary antibody-only control to reveal the level of autofluorescence and non-specific binding in your experiment [5] [82] [57].
What are the pitfalls of using chemical quenching agents, and how can I avoid them?
A major pitfall is that chemical quenchers can also diminish your specific immunofluorescence signal [9]. Furthermore, some agents have specific limitations; for example, Sudan Black B fluoresces in the far-red channel, which must be considered when designing multiplex panels [82]. The effectiveness of quenchers can also be variable across different tissue types [9].
How to Prevent It:
- Titrate the quenching agent: Determine the optimal concentration and incubation time that maximizes autofluorescence reduction while minimizing the loss of specific signal.
- Choose the right quencher for your sample: The table below compares common agents. Note that sodium borohydride must be prepared fresh and can release flammable hydrogen gas [84].
- Consider advanced methods: Fluorescence Lifetime Imaging Microscopy (FLIM) can digitally separate autofluorescence from specific signals based on their distinct fluorescence lifetimes without chemical treatment [9].
I need to store my stained samples. What is a common oversight that degrades my data?
A frequent mistake is staining cells and then storing them in fixative (like PFA) for extended periods [81]. The cross-linking reaction continues over time, increasing autofluorescence and potentially damaging epitopes.
How to Prevent It:
- Analyze fixed cells as soon as possible after staining [81].
- If you must fix cells for storage, analyze them within 24 hours and titrate the PFA to the lowest effective concentration [81].
- Store stained samples in an appropriate, non-fixative buffer at 4°C in the dark.
Troubleshooting Guide: Key Data and Protocols
Comparison of Common Autofluorescence Quenching Agents
The table below summarizes key quantitative data on commonly used chemical quenching agents to aid in selection and troubleshooting.
| Quenching Agent | Effective Concentration | Incubation Time | Key Applications & Pitfalls |
|---|---|---|---|
| Sudan Black B [82] [57] | 0.1% - 0.3% in 70% ethanol | 10 - 30 minutes | Effective against lipofuscin and aldehyde-induced autofluorescence. Pitfall: Can fluoresce in the far-red channel. |
| Copper Sulfate (CuSO₄) [84] | 0.01 M - 0.1 M in dH₂O | 10 - 20 minutes | Effective in plant and mammalian tissues; can reduce cell viability in live-cell applications. |
| Sodium Borohydride (NaBH₄) [17] [82] [84] | 0.1 mg/mL - 1 mg/mL in PBS | 10 - 30 minutes | Reduces aldehyde-based fluorescence. Pitfall: Variable results; must be prepared fresh; releases flammable gas. |
| Ammonium Chloride (NH₄Cl) [84] | 0.02 M - 0.2 M in dH₂O | 10 - 20 minutes | Used for reducing aldehyde fluorescence in fixed tissues. |
| TrueVIEW Autofluorescence Quenching Kit [5] | As per manufacturer's protocol | As per manufacturer's protocol | Commercial kit designed to quench autofluorescence from various sources, including non-lipofuscin compounds. |
Experimental Protocol: Quenching Autofluorescence with Sudan Black B
This protocol is adapted for formalin-fixed paraffin-embedded (FFPE) tissue sections and can be adjusted for other sample types [82] [57].
Materials Needed:
- Sudan Black B stock solution (e.g., 0.5% in 70% ethanol)
- 70% Ethanol
- Phosphate-Buffered Saline (PBS)
- Humidified chamber
- Coverslips and mounting medium
Methodology:
- Deparaffinization and Rehydration: Process FFPE sections through xylene and a graded ethanol series (100%, 95%, 70%) to water, following standard histological protocols [85].
- Staining: Complete all immunofluorescence staining steps, including application of primary and secondary antibodies.
- Quenching:
- Prepare a working solution of 0.1% Sudan Black B by diluting the stock solution in 70% ethanol.
- Apply the solution to cover the entire tissue section.
- Incubate in a humidified chamber at room temperature for 10-20 minutes.
- Washing:
- Rinse the slide several times with 70% ethanol to remove excess dye.
- Wash thoroughly with PBS (2 x 5 minutes) to remove residual ethanol.
- Mounting: Apply an appropriate anti-fade mounting medium and coverslip. Proceed with imaging.
Pitfall to Avoid: Do not over-incubate, as this can lead to over-quenching and potential loss of specific signal. Always test the concentration and timing on a control sample first.
Workflow for Systematic Autofluorescence Troubleshooting
The following diagram outlines a logical, step-by-step workflow to diagnose and address autofluorescence issues in your experiments.
The Scientist's Toolkit: Essential Reagents for Autofluorescence Management
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Bovine Serum Albumin (BSA) [81] [85] | Used as a blocking agent and protein component in staining buffers. | Can be used as an alternative to Fetal Calf Serum (FCS) to reduce background from serum autofluorescence. |
| Sodium Borohydride (NaBH₄) [17] [84] | Chemical reducing agent used to diminish autofluorescence induced by aldehyde fixatives. | Effectiveness is variable; prepare fresh solutions due to instability in water. |
| Sudan Black B [82] [57] | Lipophilic dye that quenches autofluorescence from lipids (lipofuscin) and aldehyde fixation. | Can autofluoresce in far-red channels; requires titration to avoid quenching specific signals. |
| TrueVIEW Kit [5] | Commercial autofluorescence quenching kit. | Suppresses autofluorescence from various non-lipofuscin sources; follow manufacturer's protocol. |
| Live/Dead Viability Dye [81] [5] | A dye used to distinguish and gate out dead cells during flow cytometry or microscopy analysis. | Critical for improving data quality as dead cells are highly autofluorescent and bind antibodies non-specifically. |
| Alexa Fluor 647 / CoraLite 647 [17] [82] [57] | Example of a far-red emitting fluorophore. | Emits in a spectral region with low inherent tissue autofluorescence, improving signal-to-noise ratio. |
| RBC Lysis Buffer [81] [5] | A buffer used to lyse and remove red blood cells from samples. | Essential when working with whole blood or tissues with high RBC content; requires thorough washing post-lysis. |
Advanced Methodology: FLIM for Autofluorescence Separation
Fluorescence Lifetime Imaging Microscopy (FLIM) offers a powerful digital approach to separate autofluorescence from specific immunofluorescence signals without chemical treatments. The method leverages the fact that fluorophores have distinct fluorescence lifetime "fingerprints" [9].
Workflow Overview:
- Image Acquisition: Tissues are excited with a pulsed laser, and time-resolved fluorescence decay data is collected for each pixel.
- Phasor Transformation: The fluorescence lifetime decay curves are transformed into a 2D phasor plot using Fourier-like sine and cosine transformations. This process is accelerated with GPU parallel computing for high-speed analysis [9].
- Signal Separation: On the phasor plot, the signals from the immunofluorescence fluorophore and autofluorescence form distinct clusters. The fractional contribution of the specific immunofluorescence signal in each pixel is calculated based on its geometrical relationship to the reference clusters.
- Image Generation: A new, autofluorescence-free image is generated based on the calculated immunofluorescence fraction [9].
Advantages and Pitfalls:
- Advantage: FLIM is a non-destructive method that does not risk quenching the specific signal with chemicals. It provides a robust, quantitative separation of signals [9].
- Pitfall: Traditional FLIM has been slow, but high-speed systems using analog mean delay and GPU computing are overcoming this limitation. The technique also requires specialized, often costly, instrumentation and expertise [9].
Validating and Comparing Autofluorescence Solutions: Efficacy, Costs, and Clinical Translation
For researchers navigating the challenges of immunofluorescence (IF), autofluorescence is more than a minor inconvenience; it is a significant barrier to achieving accurate, reliable data. This background signal, emanating from endogenous biomolecules within tissues, can severely hinder the detection of specific fluorescence, making interpretation and quantification challenging [9]. The core thesis of this technical support center is that overcoming autofluorescence is not merely an optimization step but a fundamental requirement for correlating immunofluorescence data with the trusted gold standard of immunohistochemistry (IHC). This guide details how advanced methods, particularly Fluorescence Lifetime Imaging Microscopy (FLIM), provide robust solutions to this problem, thereby enhancing the correlation of your IF results with IHC benchmarks.
FAQ: The Autofluorescence Problem
What is autofluorescence and why does it interfere with immunofluorescence? Autofluorescence is background fluorescence in a tissue sample that is not attributed to the specific antigen-antibody-fluorophore interaction. It arises from endogenous biomolecules such as collagen, elastin, flavins, NADH, and lipofuscin [9] [86] [38]. During sample handling, chemical cross-linkers like formalin and glutaraldehyde can also generate fluorescent products [86] [38]. This autofluorescence has a broad emission spectrum, often overlapping with the signals of common fluorophores like FITC or Alexa Fluor 488, which can mask the detection of low-abundance targets or be mistakenly identified as positive staining [86].
Why is IHC considered a gold standard for correlation? IHC is a cornerstone of clinical diagnostics and research pathology. It provides a permanent, high-resolution record of protein expression within intact tissue architecture, allowing for direct comparison between healthy and diseased states [87]. Its widespread use and long history have built a deep body of knowledge and validation, making it a benchmark against which newer, more quantitative techniques are often measured [88].
What is the fundamental difference between FLIM and intensity-based imaging? Traditional intensity-based fluorescence imaging measures the brightness of a signal, which can be influenced by factors like fluorophore concentration, excitation light power, and sample thickness. In contrast, FLIM measures the average time a fluorophore remains in its excited state before emitting a photon, known as its fluorescence lifetime [49] [9]. This lifetime is an intrinsic property of the fluorophore that is largely independent of concentration, excitation intensity, and photobleaching, making it a more robust and quantitative parameter [9] [89].
Methodologies: Benchmarking Advanced Techniques Against IHC
High-Speed FLIM with Phasor Analysis
This method leverages the distinct lifetime-spectrum profiles of fluorophores, acting as a unique fingerprint, to differentiate specific immunofluorescence signals from autofluorescence [9].
Experimental Protocol:
- Tissue Staining: Perform standard immunofluorescence staining on your tissue sample (e.g., FFPE or frozen sections) using your chosen antibody-fluorophore conjugate.
- Image Acquisition: Image the stained tissue using a high-speed FLIM system equipped with a picosecond pulsed laser. The system should be capable of time-resolved fluorescence detection. GPU acceleration is key for high throughput [9].
- Reference Measurement: Independantly measure the phasor clusters for:
- Autofluorescence (AF): From an unstained section of the same tissue.
- Immunofluorescence (IF): From the antibody-fluorophore conjugate in solution (e.g., PBS) [9].
- Phasor Transformation: The fluorescence lifetime decay data from each pixel is transformed into a 2D phasor plot (G and S coordinates) via Fourier-like transformations. This process can be done in real-time with GPU computing [9].
- Signal Unmixing: For each pixel in the tissue image, the fractional contribution of the specific immunofluorescence is calculated based on the geometric relationship between its phasor position and the reference phasors for AF and IF. The fraction of IF is given by: Fraction of IF = da / (da + d_i), where
d_ais the distance to the AF reference andd_iis the distance to the IF reference [9]. - Image Generation: Generate a new, autofluorescence-free image based on the calculated IF fraction for each pixel.
Performance Benchmarking: Research has demonstrated that this FLIM-based autofluorescence suppression method enhances the correlation of immunofluorescence images with IHC data, outperforming other methods like chemical-assisted photobleaching and hyperspectral imaging [9].
The following diagram illustrates the workflow of the FLIM phasor analysis for separating immunofluorescence from autofluorescence.
Fluorescence Lifetime Multiplexing (FLEX) for Spatial Biology
FLEX tackles the problem of spectral overlap, another major limitation of conventional IF, by using fluorescence lifetime as an additional, independent dimension for contrast.
Experimental Protocol:
- Palette Selection: Select antibodies conjugated to fluorophores that are distributed across a range of both emission wavelengths and fluorescence lifetimes. Up to three fluorophores with similar spectra but unique lifetimes can be multiplexed within a single color channel [90].
- Staining and Imaging: Simultaneously stain the tissue sample with the entire selected antibody panel in a single step. Image the stained tissue using a confocal FLIM system with multiple excitation lasers.
- Phasor Decomposition: Use phasor analysis to separate the contributions of the different fluorophores within each pixel based on their distinct lifetime signatures. A linear decomposition algorithm quantifies the individual contribution of each fluorophore [90].
- Data Output: The output is a highly multiplexed image where each biomarker is clearly resolved, overcoming the spectral limits of conventional IF and providing rich, co-localization data for spatial biology.
Performance Benchmarking: This approach allows for the rapid, simultaneous imaging of 11 or more biomarkers in a single staining and imaging cycle, far exceeding the capabilities of standard IHC or conventional multiplexed IF [90].
FLIM on H&E-Stained Sections
This innovative application uses FLIM to extract quantitative, functional information from the most ubiquitous staining method in histology.
Experimental Protocol:
- Sample Preparation: Prepare standard H&E-stained tissue sections (e.g., from HCC samples) [89].
- FLIM Acquisition: Use a time-domain FLIM system to directly measure the fluorescence lifetime of the eosin dye within the tissue section. Eosin is fluorescent and its lifetime is sensitive to the local microenvironment [89].
- Phasor Analysis: Apply the phasor approach to analyze the fluorescence lifetime data. Different tissue types (e.g., cancerous vs. peritumoral) will cluster in different regions of the phasor plot, generating pseudo-colored images that enhance pathological features [89].
- Correlation: Correlate the fluorescence lifetime values or ratios with clinical and pathological data.
Performance Benchmarking: A study on hepatocellular carcinoma (HCC) demonstrated that the fluorescence lifetime values in cancerous tissues (2000–2500 ps) significantly exceeded those in peritumoral tissues (500–1000 ps). The ratio of these lifetimes showed strong positive correlations with key liver function indicators like total bilirubin (correlation 0.79) and direct bilirubin (correlation 0.87), providing a quantitative method to augment traditional H&E diagnosis [89].
Troubleshooting Guide: Comparing Traditional vs. FLIM-Based Methods
The table below summarizes various methods for handling autofluorescence, highlighting the comparative advantages of the FLIM approach.
| Method | Principle | Key Protocol Steps | Limitations | Correlation with IHC |
|---|---|---|---|---|
| Chemical Quenchers (e.g., Sudan Black B) | Uses chemicals to suppress AF signal. | Incubate tissue with quencher (e.g., Sudan Black B) post-staining, then wash [86]. | Can decrease target fluorescence; may elevate background in specific channels [9]. | Variable; can compromise signal quality. |
| Photobleaching | Uses high-power light to degrade AF molecules. | Expose unstained sample to high-intensity light before staining [9] [90]. | Can lead to loss of specific IF signal; does not eliminate AF entirely [9]. | Moderate; non-specific signal reduction. |
| Image Subtraction | Digitally subtracts an AF image from the IF+AF image. | Capture image of AF only (no antibody), then image of IF+AF, and subtract [9]. | Requires perfect image alignment; slight misalignment causes artifacts [9]. | Can be imprecise due to artifacts. |
| Fluorophore Selection | Uses far-red dyes where AF is less pronounced. | Use fluorophores like Alexa Fluor 647 for staining [86] [38]. | Not a solution for targets requiring blue/green channels; limited by panel design. | Good for specific channels only. |
| High-Speed FLIM | Separates signals based on fluorescence lifetime. | See detailed protocol above. | Requires specialized FLIM instrumentation and expertise [9]. | High; directly enhances correlation by isolating specific signal [9]. |
Research Reagent Solutions
The following table lists key materials and reagents essential for implementing the FLIM-based methods described.
| Item | Function | Example/Note |
|---|---|---|
| Picosecond Pulsed Laser | Provides the excitation source for time-resolved fluorescence measurement. | A supercontinuum white laser allows multiple excitation wavelengths [89]. |
| High-Speed Detector & Digitizer | Precisely records the time of arrival of fluorescence photons. | Time-Correlated Single Photon Counting (TCSPC) electronics are commonly used [9] [89]. |
| GPU-Accelerated Computing | Enables real-time phasor transformation and data processing for high throughput. | Critical for making FLIM compatible with biomedical workflows [9]. |
| Lifetime-Defined Fluorophores | Antibody-fluorophore conjugates with distinct lifetimes for multiplexing. | Conjugates like Alexa647, Atto647, and Attorho14 can be distinguished by lifetime alone [90]. |
| Antigen Retrieval Buffers | Unmasks epitopes in FFPE tissues for effective antibody binding. | Citrate, Tris-EDTA, or Protease K buffers; choice requires optimization [87]. |
| Blocking Solution | Reduces non-specific antibody binding to minimize background. | Bovine Serum Albumin (BSA) or serum from the secondary antibody host [87]. |
The drive to correlate advanced immunofluorescence techniques with the gold standard of IHC is fundamentally linked to solving the problem of autofluorescence. While traditional methods offer partial solutions, they come with significant trade-offs. FLIM, particularly high-speed FLIM with phasor analysis, represents a paradigm shift. By leveraging the immutable, quantitative nature of fluorescence lifetime, it provides a robust, digital path to isolate specific signal from autofluorescence, thereby generating immunofluorescence data that truly merits a strong correlation with IHC. This empowers researchers and drug development professionals to achieve a new level of confidence in their spatial biology data.
Autofluorescence (AF) in immunofluorescence (IF) microscopy presents a significant barrier to research rigor, particularly in studies of the central nervous system and in aging tissues. It is primarily caused by endogenous fluorophores such as lipofuscin—a mixture of highly oxidized lipids, misfolded proteins, and metals that accumulates in lysosomes—as well as collagen, elastin, and flavins [91] [2]. This background signal can confound the interpretation of results, leading to false positives and inaccurate quantification of specific fluorescence signals [9] [80]. This guide provides a comparative analysis of the primary methods to overcome this challenge, framed within the context of a broader thesis on solving autofluorescence in immunofluorescence research.
FAQs: Addressing Core Challenges
1. What is the primary source of problematic autofluorescence in neurological research? The most significant source is lipofuscin, a lipopigment that accumulates with age within lysosomal compartments of cells, notably in microglia [91] [80]. These aggregates autofluoresce across the fluorescent spectrum, and their emission can be mistakenly interpreted as specific antibody-labeled signal, such as engulfed synaptic material [91].
2. I am studying microglial engulfment in young adult mice. Do I need to worry about autofluorescence? Yes. While historically associated with aging, lipofuscin-like autofluorescence (lipo-AF) can be detected within microglial lysosomes in mice as young as 7-9 weeks [91]. This signal accumulates first in microglia and appears earlier in white matter than in gray matter, making it a potential confound even in studies using young adult animals [91] [80].
3. Which method for reducing autofluorescence interference is least likely to affect my specific immunofluorescence signal? Digital methods, particularly Fluorescence Lifetime Imaging Microscopy (FLIM), are designed for this purpose. FLIM leverages the distinct fluorescence decay times of fluorophores to separate specific immunofluorescence signals from autofluorescence digitally, without chemically or physically altering the sample [9] [2]. In contrast, chemical and photonic methods affect all molecules in the sample and can sometimes diminish the desired signal [9].
4. For a cost-effective and simple pre-staining method, what can I use? Chemical quenching with Sudan Black B is a robust, low-cost protocol. A typical method involves incubating tissue sections in a 0.1% Sudan Black B solution in 70% ethanol for 20 minutes at room temperature before antibody staining, followed by thorough rinsing [92] [80]. Alternatively, high-intensity white LED light photobleaching has been demonstrated as a simple, scalable, and effective pre-staining method that preserves target signal [14].
Troubleshooting Guides
Issue 1: High Background from Lipofuscin in Aged or Neurological Tissue
- Symptoms: Punctate, granular fluorescence visible in multiple channels (e.g., 488, 561, 638 nm) that persists in unstained control samples.
- Solution A (Chemical Quenching): Apply a Sudan Black B treatment (0.1% in 70% ethanol for 20 min) during sample preparation. Note: Test on a control slide first, as excessive concentration or incubation time can slightly reduce specific signal intensity [92] [80].
- Solution B (Photonic Bleaching): Prior to immunostaining, expose the tissue section to high-intensity broad-spectrum white LED light. This method has been shown to nearly eliminate lipofuscin autofluorescence in human Alzheimer's disease brain tissue without negative impacts on subsequent multiplex assays [14].
Issue 2: Autofluorescence is Obscuring Weak Specific Signal in Flow Cytometry
- Symptoms: High background in channels like FITC and APC when analyzing immune cells like microglia, making it difficult to resolve positive populations.
- Solution: Switch fluorophore conjugates. Phycoerythrin (PE) has been shown to outperform FITC and Allophycocyanin (APC) for detecting surface protein expression in autofluorescent microglia by overcoming the inherent spectral interference of the cellular autofluorescence [80].
Issue 3: Need for Absolute Signal Fidelity Without Sample Alteration
- Symptoms: The experiment requires precise quantification of signal intensity, and any chemical or photonic treatment risks altering the antigen or fluorophore.
- Solution: Implement a digital separation technique like high-speed Fluorescence Lifetime Imaging Microscopy (FLIM). This method acquires time-resolved data and uses phasor analysis to computationally isolate the immunofluorescence signal from the autofluorescence based on their distinct lifetime "fingerprints" [9] [2].
Comparative Analysis Tables
| Method Category | Key Principle | Best For | Key Advantage | Major Limitation |
|---|---|---|---|---|
| Chemical Quenching [14] [92] [80] | Applying chemical agents (e.g., Sudan Black B) to suppress AF emission. | Fixed tissues; high-throughput labs needing a simple, low-cost solution. | Low cost and easy to implement with standard lab equipment. | Can potentially reduce specific antibody signal and is not suitable for live cells. |
| Photonic Bleaching [14] | Using high-intensity light (e.g., white LED) to photobleach AF molecules prior to imaging. | Fixed tissue sections, particularly those with very high lipofuscin burden (e.g., aged or diseased brain). | Effective and scalable; reported to have no adverse effect on target signal or tissue integrity. | Requires specialized light source; not applicable to live-cell imaging. |
| Digital Subtraction [9] | Capturing an AF-only image and subtracting it from the total signal image. | Situations where other pre-processing methods have failed or are not feasible. | Maintains sample integrity as no pre-treatment is required. | Challenging; requires perfect image alignment and can create artifacts if misaligned. |
| Fluorescence Lifetime (FLIM) [9] [2] | Separating signals based on the distinct fluorescence decay times of AF and specific labels. | Applications demanding high signal fidelity and quantification, and for multiplexed imaging. | Powerful separation without altering the sample; considered a gold-standard digital method. | Requires specialized, costly instrumentation and expertise in data acquisition/analysis. |
Table 2: Technical and Practical Considerations
| Consideration | Chemical Quenching | Photonic Bleaching | Digital Subtraction | Fluorescence Lifetime (FLIM) |
|---|---|---|---|---|
| Impact on Specific Signal | Possible reduction [9] | Minimal reported impact [14] | No impact | No physical impact; pure digital separation [9] |
| Live Cell Compatibility | No | No | Yes | Yes |
| Cost & Accessibility | Low | Medium | Low (if software is available) | High |
| Throughput | High | High | Medium | Medium-High (with new high-speed systems) [9] |
| Species Versatility | Mouse, marmoset, human [91] | Human, mouse [14] | All | Demonstrated across various tissues [9] |
Detailed Experimental Protocols
This protocol is for formalin-fixed, paraffin-embedded (FFPE) or frozen tissue sections.
- Follow standard steps for deparaffinization, rehydration, antigen retrieval, and permeabilization.
- Quenching: Prepare a 0.1% (w/v) solution of Sudan Black B in 70% ethanol. Incubate the slides in this solution for 20 minutes at room temperature, protected from light.
- Rinsing: Rinse the slides thoroughly with several changes of PBS until no more color leaches from the tissue.
- Proceed with standard blocking and antibody incubation steps as per your immunofluorescence protocol.
This is a pre-staining method.
- Sample Preparation: Following tissue sectioning and any necessary deparaffinization and rehydration, place slides in a suitable container.
- Bleaching: Expose the tissue sections to a high-intensity, broad-spectrum white LED light source for a defined period. Note: The exact duration and intensity must be optimized for your specific setup and tissue type.
- Proceed with your standard immunofluorescence staining protocol, including antigen retrieval, blocking, and antibody incubations.
This protocol outlines the conceptual workflow for a high-speed FLIM approach.
- Sample Preparation: Stain samples with fluorophore-conjugated antibodies as per a standard IF protocol. No special quenching is required.
- Lifetime Data Acquisition: Image tissues using a pulsed laser and a high-speed FLIM system capable of time-resolved detection. Acquire the fluorescence decay curve for every pixel in the image.
- Reference Measurement: Independently measure the fluorescence lifetime of the unstained tissue (autofluorescence reference) and the antibody-fluorophore conjugate in solution (immunofluorescence reference).
- Phasor Transformation: Transform the lifetime decay curves of each pixel, and the reference measurements, into the phasor domain using a Fourier-like transformation.
- Signal Unmixing: For each pixel, calculate the fractional contribution of the specific immunofluorescence signal based on the geometrical relationship between its phasor position and the reference phasors. The fraction of immunofluorescence (IF) is given by:
Fraction_IF = d_a / (d_a + d_i), whered_ais the distance to the AF reference andd_iis the distance to the IF reference in the phasor plot. - Image Generation: Generate a new, autofluorescence-free image based on the calculated IF fraction for each pixel.
Method Selection Workflow
The following diagram outlines a logical decision pathway for selecting the most appropriate autofluorescence mitigation method based on your experimental constraints and goals.
Research Reagent Solutions
Table 3: Essential Materials for Autofluorescence Management
| Item | Function/Benefit | Example Use Case |
|---|---|---|
| Sudan Black B [92] [80] | A chemical quencher that non-specifically reduces lipofuscin autofluorescence. | A cost-effective first-line treatment for fixed brain sections from aged models. |
| TrueBlack Lipofuscin Autofluorescence Quencher [80] | A commercial formulation designed specifically to quench lipofuscin signal. | Used in microglia immunofluorescence studies to improve signal-to-noise for intracellular proteins. |
| High-Intensity White LED Source [14] | A photonic tool for pre-staining reduction of autofluorescence across a broad spectrum. | Effective for human nervous system tissue, including Alzheimer's disease samples, prior to multiplexed imaging. |
| Anti-CD68 Antibody [91] | A marker for lysosomes, the primary organelles where lipofuscin accumulates. | Used as a co-stain to confirm the localization of autofluorescence within microglia. |
| Anti-IBA1 / Anti-P2RY12 Antibodies [91] [80] | Specific markers for identifying microglia in tissue sections. | Essential for contextualizing autofluorescence signals within the cell type of interest. |
| PE-conjugated Antibodies [80] | Fluorophore conjugates that are less susceptible to interference from cellular autofluorescence in flow cytometry. | Preferred over FITC and APC for detecting surface proteins on highly autofluorescent cells like microglia. |
Understanding Autofluorescence and Multiplexing
What is autofluorescence and how does it impact my multiplex immunofluorescence experiment?
Autofluorescence is background fluorescence emitted by endogenous components in biological samples, not from specific antibody-fluorophore staining. In multiplexing, this background signal occupies valuable spectral channels, reducing the number of markers you can detect simultaneously and obscuring specific signals from low-abundance targets [93] [16].
The common sources and their spectral characteristics are summarized in the table below.
| Source of Autofluorescence | Description | Typical Emission Range | Primary Tissue Locations |
|---|---|---|---|
| Lipofuscin [93] [16] | A granular, lipophilic pigment that accumulates with age. | Broad: 500-695 nm [93] | Lysosomes of post-mitotic cells (e.g., neurons, myocytes) [16]. |
| Collagen [16] | A major component of the extracellular matrix. | ~300-450 nm (Blue region) [93] | Ubiquitous in connective tissues [16]. |
| NADH [93] [16] | A key metabolic coenzyme. | ~450 nm (Blue/Green region) [93] | Metabolically active cells (e.g., liver) [93]. |
| Elastin [16] | An extracellular matrix component. | Broad, often in green channel [16] | Blood vessels, lungs, skin [16]. |
| Heme Group [93] | Found in hemoglobin in red blood cells. | Broad spectrum [93] | Blood vessels and whole blood [16]. |
| Aldehyde Fixatives [93] | Formalin, paraformaldehyde; form fluorescent Schiff bases. | Broad: Blue, Green, and Red [93] | All fixed tissues [93]. |
Troubleshooting Common Autofluorescence Issues
I am experiencing high background that is masking my specific signal in the green channel. What can I do?
This is a common issue as autofluorescence is often most prominent in the green channel [16]. You can try the following strategies:
- Choose longer-wavelength fluorophores: Shift your detection to channels with lower inherent autofluorescence. Using red and far-red fluorophores (e.g., CoraLite594, CoraLite647, or Near-Infrared conjugates) can dramatically improve your signal-to-noise ratio [93] [16].
- Employ chemical quenching: Treat your samples with autofluorescence quenchers. Sudan Black B is effective for lipofuscin and formalin-induced autofluorescence, though it can fluoresce in the far-red channel [93]. Sodium borohydride can reduce aldehyde-induced autofluorescence, though results can be variable [93] [16].
- Include proper controls: Always run an unstained control and a secondary antibody-only control to reveal the level of autofluorescence and non-specific binding in your experiment [93].
My multiplex panel has weak signal for some markers, and I suspect autofluorescence is to blame. How can I confirm this?
- Image an unstained control: Process a section of your tissue sample identically to your test samples but omit all fluorescently-labeled antibodies. Acquire an image using each of your microscope's filter sets. Any signal you see is autofluorescence, which will help you identify which spectral channels are most affected [16].
- Check your fixation method: Over-fixation with aldehydes, especially glutaraldehyde, significantly increases autofluorescence. Where possible, use paraformaldehyde instead of glutaraldehyde and fix for the minimum time required [93] [94]. For cells, consider using chilled organic solvents like ethanol as an alternative fixative [93].
Advanced Solutions for High-Plex Spatial Biology
For high-plex spatial proteomic studies, how can I overcome autofluorescence to free up spectral channels?
Conventional methods like chemical quenching are insufficient for highly multiplexed panels. Advanced instrumental and computational methods are required to disentangle specific signal from autofluorescence based on its physical properties.
- Fluorescence Lifetime Imaging Microscopy (FLIM): This powerful technique distinguishes fluorophores based on their fluorescence lifetime (how long the molecule stays in an excited state), which is independent of their emission color [9]. Autofluorescence typically has a much shorter lifetime (e.g., ~2.2 ns) than common immunofluorescence dyes (e.g., CF450 at ~3.5 ns) [9]. High-speed FLIM can separate these signals in real-time, effectively creating an "autofluorescence-free" image and freeing up the spectral channel for another marker [9].
- Spectral Imaging and Unmixing: Spectral flow cytometry or hyperspectral microscopy capture the full emission spectrum of every pixel in an image. Since the spectral "fingerprint" of autofluorescence is often distinct from that of fluorescent conjugates, computational unmixing can isolate and subtract the autofluorescence component, clearing the channel for true signal [16].
Can you provide a quantitative comparison of advanced autofluorescence suppression techniques?
The table below summarizes the key features of different methods, helping you select the right approach for your high-plex experiment.
| Method | Key Principle | Key Performance Metrics | Best Suited For |
|---|---|---|---|
| Chemical Quenching (e.g., Sudan Black B) [93] | Reduces AF via chemical reaction. | Effective for: Lipofuscin, aldehyde AF. Limitation: Can introduce fluorescence in far-red; may require optimization. | Low- to mid-plex IF where AF source is known and treatable. |
| Fluorophore Selection [93] [16] | Avoids AF by using fluorophores in spectral regions with low AF. | Effective for: Shifting signal to red/far-red. Limitation: Does not eliminate AF; limited by microscope laser/filter availability. | All multiplexing levels, as a fundamental panel design principle. |
| High-speed FLIM [9] | Separates signals based on fluorescence lifetime differences using phasor analysis. | Throughput: High (GPU-accelerated). Photon acquisition: >125 MHz. Separation: Robust across tissues/antibodies. | High-plex spatial biology requiring unambiguous signal separation without sacrificing spectral channels. |
| Spectral Unmixing [16] | Captures full spectrum and computationally separates overlapping signals. | Effectiveness: High, can resolve complex mixtures. Data Load: Generates large datasets. | High-plex workflows using spectral flow cytometers or hyperspectral imagers. |
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and tools are essential for implementing the advanced autofluorescence suppression methods discussed.
| Item | Function in Autofluorescence Suppression |
|---|---|
| Primary Antibody-Fluorophore Conjugates [95] | Off-the-shelf conjugates for specific targets, enabling panel design that avoids autofluorescence-rich spectral regions. |
| Validated Secondary Antibodies [95] | Conjugates with high signal-to-noise ratio, minimizing non-specific background that can compound autofluorescence issues. |
| PhenoCode Panels [96] | Ready-to-use, pre-optimized multiplex antibody panels compatible with platforms like the PhenoCycler-Fusion, simplifying high-plex workflow setup. |
| TrueVIEW Autofluorescence Quenching Kit [93] | A commercial reagent designed to reduce autofluorescence from multiple common causes. |
| ProLong Gold Antifade Reagent [97] | A mounting medium that reduces signal fading and can help preserve specific fluorescence signal against photobleaching. |
| Sodium Borohydride (NaBH₄) [93] | A chemical reducing agent used to quench autofluorescence induced by aldehyde-based fixatives. |
Experimental Protocol: Autofluorescence Removal via High-speed FLIM
This protocol is adapted from a recent study demonstrating robust, high-throughput autofluorescence suppression using GPU-accelerated Fluorescence Lifetime Imaging Microscopy (FLIM) [9].
Sample Preparation and Staining
- Prepare your tissue sections (fresh frozen or FFPE) according to standard protocols for immunofluorescence.
- Stain the tissue with your chosen panel of antibody-fluorophore conjugates. Include an unstained control section from the same tissue block for accurate autofluorescence reference [9].
- Mount the slides, ensuring compatibility with high-resolution microscopy.
Data Acquisition with High-speed FLIM
- Image the stained and unstained control tissues using a high-speed FLIM system equipped with a picosecond pulsed laser and time-gated detector.
- Acquire the fluorescence lifetime decay data. The high-speed system used in the referenced study, based on the analog mean delay method, is capable of photon count rates exceeding 125 MHz, enabling rapid data collection [9].
- For a 512 x 512 pixel image, the system can acquire approximately 500 photons per pixel per second, which is sufficient for reliable separation of immunofluorescence and autofluorescence [9].
Phasor Transformation and Analysis
- The fluorescence lifetime decay curves are transformed into the phasor domain using a Fourier-like transformation. This process is accelerated in real-time using GPU parallel computing, taking approximately 3 seconds for a 512 x 512 image [9].
- In the 2D phasor plot (G and S coordinates), the phasor points for pure immunofluorescence and pure autofluorescence (measured from the unstained control) will form distinct clusters. The phasor of each pixel in the stained image will lie on a line between these two reference clusters [9].
Signal Separation and Image Generation
- The fractional contribution of the specific immunofluorescence signal in each pixel is calculated using the geometrical relationship in the phasor plot: Fraction of IF = da / (da + d_i), where
d_ais the distance from the pixel's phasor to the autofluorescence reference, andd_iis the distance to the immunofluorescence reference [9]. - This calculation is performed for every pixel in the image, generating a new, quantitative image where the intensity is directly proportional to the specific antibody-derived signal, free from autofluorescence contamination [9].
FAQs and Troubleshooting Guides
Frequently Asked Questions
Q1: What are the most cost-effective methods to reduce autofluorescence for a clinical lab with high throughput needs?
Chemical quenching methods, such as treatment with Sudan Black B or copper sulfate, are generally the most cost-effective initial approach for labs with high throughput [9]. These reagents are inexpensive and can be integrated into existing protocols with minimal disruption. For labs using aldehyde fixatives, a highly cost-effective strategy is to optimize fixation by using the minimum required concentration and duration to prevent the formation of fluorescent cross-links [98] [83] [99].
Q2: Our lab is considering new imaging systems. What options provide the best balance of cost and capability for autofluorescence management?
Widefield fluorescence microscopes with LED light sources and standard filter sets represent a strong balance of cost and capability. They allow for the primary strategy of fluorophore selection to avoid autofluorescence peaks [1]. For labs planning larger investments, high-speed Fluorescence Lifetime Imaging Microscopy (FLIM) systems are emerging. While requiring a higher initial investment, they offer a powerful, non-destructive digital method for autofluorescence separation that can improve workflow efficiency and data reliability across many applications [9].
Q3: How can we quickly adapt our current IHC protocols to IF with minimal autofluorescence?
The most straightforward adaptation is to incorporate a dedicated autofluorescence quenching step using commercially available reagents like TrueBlack [100] or Sudan Black B [9] immediately after sample fixation and permeabilization. Furthermore, you can directly shift your panel to brighter fluorophores (e.g., PE, APC) and those emitting in the red to near-infrared spectrum (e.g., Alexa Fluor 568, 555) [101] [1] [100]. This avoids the green channel where autofluorescence is most intense.
Q4: What is the single most important control for diagnosing autofluorescence in a new sample type?
The most critical control is the "No Primary Antibody Control" (also known as the secondary antibody-only control) [102]. In this control, the primary antibody is omitted from the staining protocol, but all other steps, including incubation with the secondary antibody, are performed. Any fluorescence signal observed in this control is the result of autofluorescence or non-specific binding of the secondary antibody, providing a clear baseline for background signal [102].
Troubleshooting Common Workflow Issues
Problem: High background autofluorescence persists after standard quenching protocols.
- Potential Cause: The autofluorescence is endogenous and stems from dense structural proteins (collagen, elastin) or pigments (lipofuscin, heme) in the tissue itself [1] [83] [99].
- Recommendations:
- For heme: Perfuse tissues with PBS or saline before fixation to remove blood cells [83] [99]. For archived samples, treat with a solution of 5% H₂O₂ in methanol/DMSO overnight at 4°C [83].
- For structural proteins: If your target permits, switch to fluorophores excited by red or near-infrared light (e.g., >600 nm) to avoid exciting collagen and elastin [1].
- Digital solution: If available, use spectral imaging or the high-speed FLIM phasor analysis to digitally separate the specific signal from the autofluorescence post-acquisition [9].
Problem: Staining protocol is too long for an efficient clinical workflow.
- Potential Cause: Reliance on overnight primary antibody incubations and lengthy washing steps.
- Recommendations:
- Validate shorter incubations: Systematically test and validate shorter incubation times for the primary antibody at room temperature versus the typical 4°C overnight [98] [103].
- Use signal amplification: Implement tyramide signal amplification (TSA) systems. These can significantly reduce the required primary antibody concentration and incubation time while providing a strong signal, thus shortening the overall protocol duration [100].
- Process in batches: Organize workflow to stain and image batches of samples together to improve overall lab efficiency.
Problem: Inconsistent autofluorescence between similar tissue samples.
- Potential Cause: Variability in sample preparation, particularly in fixation time, temperature, or the age of the fixative [98] [83] [99].
- Recommendations:
- Standardize fixation: Strictly control fixation time based on tissue size and type, avoiding over-fixation. Use fresh formaldehyde dilutions and avoid old glutaraldehyde stocks [98] [83].
- Control temperature: Perform all staining and preparation steps at room temperature or below to prevent heat-induced autofluorescence. If working at 4°C, adjust incubation times accordingly [83] [99].
- Include a positive control for background: Always run a control sample known to have high autofluorescence (e.g., lung, liver) alongside your experimental samples to monitor batch-to-batch variation in background levels [102].
Decision Workflow for Autofluorescence Solutions
The following diagram outlines a systematic approach for clinical labs to select the most appropriate autofluorescence mitigation strategy based on their primary constraints.
Comparison of Autofluorescence Mitigation Strategies
The table below provides a comparative overview of common autofluorescence mitigation methods, focusing on key economic and workflow parameters critical for clinical laboratories.
Table 1: Economic and Workflow Comparison of Autofluorescence Solutions
| Method | Typical Cost | Implementation Speed | Technical Accessibility | Key Clinical Workflow Consideration |
|---|---|---|---|---|
| Chemical Quenching [100] [9] | Low | Fast (protocol addition) | High | Can be easily added to existing protocols; may require optimization for tissue type. |
| Fixation Optimization [98] [83] | Very Low | Fast (protocol change) | High | A fundamental, no-cost best practice that should be standardized first. |
| Fluorophore Selection [101] [1] | Medium | Fast (panel redesign) | Medium | May require purchasing new reagents but is a highly effective strategy. |
| Signal Amplification (TSA) [100] | Medium | Medium | Medium | Can shorten primary incubation times, speeding up workflow, but adds complexity. |
| High Dynamic Range (HDR) Imaging [100] | Medium (software) | Medium | Medium | A digital post-processing solution; requires compatible imaging systems and software. |
| High-Speed FLIM [9] | High | Slow (new system) | Low | Requires significant capital investment and specialist expertise, but is a powerful digital suppression tool. |
Detailed Experimental Protocols
Protocol 1: Chemical Quenching with TrueBlack for Rapid Background Suppression
This protocol is adapted from a 2024 study and is designed for efficiency, making it suitable for clinical labs needing to process PD-L1 or similar IF stains with minimal protocol extension [100].
- Sample Preparation: After deparaffinization, rehydration, and antigen retrieval, complete the primary and secondary antibody incubations as per your standard protocol.
- Quenching Solution Preparation: Dilute TrueBlack (Biotium, #23007) 1:20 in 70% ethanol or the buffer recommended by the manufacturer. Note: Prepare fresh and use immediately.
- Incubation: Cover the tissue section with 1X TrueBlack solution and incubate for 1.5 minutes at room temperature.
- Washing: Rinse the slide thoroughly with phosphate-buffered saline (PBS) to stop the reaction.
- Counterstaining and Mounting: Proceed with nuclear counterstaining (e.g., DAPI) and mount the slides with an anti-fade mounting medium [98] [100].
Protocol 2: High-Speed FLIM for Autofluorescence Separation
This protocol, based on a 2025 methodology, leverages GPU-accelerated phasor analysis for high-throughput, autofluorescence-free imaging [9]. While requiring specialized equipment, it represents a cutting-edge digital solution.
- Sample Preparation: Stain tissues following a standard IF protocol. The fluorophores used should have known and distinct fluorescence lifetimes from the tissue's autofluorescence.
- Reference Acquisition:
- Immunofluorescence (IF) Reference: Acquire a FLIM image of the antibody-fluorophore conjugate in solution (e.g., PBS).
- Autofluorescence (AF) Reference: Acquire a FLIM image from an unstained section of the same tissue type.
- Sample Imaging: Image the stained tissue using the high-speed FLIM system with a pulsed laser. The system should be capable of high photon acquisition rates (>125 MHz).
- GPU-Accelerated Phasor Analysis:
- The fluorescence lifetime decay data for each pixel is transformed in real-time into a 2D phasor plot (G, S coordinates) using Fourier-like transformations.
- The distinct phasor clusters for the pure IF and AF references are identified on the plot.
- Signal Separation:
- For each pixel in the tissue image, the phasor value is a linear combination of the IF and AF reference phasors.
- The fractional contribution of the specific immunofluorescence is calculated geometrically using the formula:
Fraction of IF = d_a / (d_a + d_i), whered_ais the distance to the AF phasor andd_iis the distance to the IF phasor [9].
- Image Generation: A new, autofluorescence-free image is generated based on the calculated IF fraction for each pixel.
Research Reagent Solutions
Table 2: Key Reagents for Autofluorescence Management in Clinical Workflows
| Reagent | Function in Autofluorescence Management | Example Use-Case | Citation |
|---|---|---|---|
| TrueBlack | Chemical quencher; suppresses lipofuscin and aldehyde-induced fluorescence. | Applied post-staining before mounting to rapidly reduce broad-spectrum background. | [100] |
| Sudan Black B | Chemical quencher; binds to and suppresses fluorescence from lipids and lipofuscin. | Incubated with tissue sections after permeabilization but before antibody staining. | [9] |
| Alexa Fluor 555/568 | Bright, photostable fluorophores emitting in the orange-red spectrum. | Used as a secondary antibody conjugate or in TSA to avoid green autofluorescence. | [1] [100] |
| Tyramide Signal Amplification (TSA) Kits | Signal amplification system; allows use of lower primary antibody concentrations. | Reduces non-specific binding and shortens incubation times, indirectly mitigating background. | [100] |
| Sodium Borohydride | Reducing agent; reduces fluorescent aldehyde adducts formed during fixation. | Treatment of aldehyde-fixed tissues to reduce fixation-induced autofluorescence. | [103] [9] |
| ProLong Gold Antifade Mountant | Anti-fade mounting medium; reduces photobleaching of true signal. | Preserves specific fluorescence signal during storage and imaging, improving signal-to-noise. | [98] |
Autofluorescence presents a significant challenge in immunofluorescence research, often severely hindering the detection of specific fluorescence signals [9]. This background noise, originating from endogenous biomolecules such as collagen, flavins, and lipofuscin, can markedly distort assay readouts, making interpretation and quantification challenging [9]. This technical support article explores recent case studies and methodologies developed to overcome this persistent issue, enabling clearer and more reliable imaging across critical biomedical research fields.
Technical Solutions for Autofluorescence Suppression
High-Speed Fluorescence Lifetime Imaging Microscopy (FLIM)
A 2025 study demonstrated a robust method for autofluorescence-free immunofluorescence using high-speed FLIM [9]. This technique leverages the distinct lifetime-spectrum profiles of fluorophores to differentiate specific immunofluorescence signals from autofluorescence.
Mechanism of Action:
- Principle: FLIM separates signals based on their fluorescence decay kinetics (lifetime) rather than just spectral emission [9].
- Phasor Analysis: Fluorescence lifetime decays are transformed into phasor plots (G and S coordinates) via Fourier-like functions, enabling clear separation of immunofluorescence and autofluorescence clusters based on their lifetime variances [9].
- Quantitative Separation: The fractional contribution of immunofluorescence in mixed signals is calculated geometrically in the phasor domain using the formula:
[ \text{Fraction of IF} = \frac{da}{da + d_i} ]
where (da) is the distance to the autofluorescence reference and (di) is the distance to the immunofluorescence reference [9].
Performance Metrics:
- The high-speed FLIM system can acquire approximately 500 photons per pixel per second, sufficient for effective signal separation [9].
- Computational processing takes approximately 3 seconds for a 512x512 image using GPU parallel computing [9].
- This method outperformed chemical-assisted photobleaching and hyperspectral imaging in correlating immunofluorescence images with immunohistochemistry data [9].
Convolutional Autoencoder for Artifact Detection
Another 2025 study proposed an automated approach for detecting various artifacts in fluorescence microscopy images using convolutional autoencoders (CAEs) [104].
Methodology:
- The CAE is trained exclusively on artifact-free images to learn essential patterns of authentic signals [104].
- Artifact-laden images are detected by computing the difference between input and output, with increased discrepancies indicating artifacts [104].
- This approach achieves 95.5% average accuracy in classifying artifacts across different datasets and can detect previously unseen artifact types [104].
Table 1: Comparison of Autofluorescence Suppression Techniques
| Technique | Mechanism | Advantages | Limitations |
|---|---|---|---|
| High-Speed FLIM [9] | Fluorescence lifetime separation via phasor analysis | Robust across tissue types; preserves signal integrity | Requires specialized instrumentation; computational complexity |
| Convolutional Autoencoder [104] | Machine learning-based artifact detection | Detects unseen artifacts; high accuracy (95.5%) | Limited to detection rather than suppression |
| Chemical Quenchers (Sudan Black B, CuSO₄, etc.) [9] | Chemical suppression of autofluorescence | Simple implementation; widely accessible | Can decrease desired fluorescence; elevated background in some channels |
| Photobleaching [9] | High-power light exposure to reduce autofluorescence | Effective for certain autofluorophores | Leads to significant immunofluorescence signal loss |
| Digital Subtraction [9] | Mathematical removal of autofluorescence image | Maintains sample integrity | Requires precise alignment; potential for artifacts |
Case Studies
Oncology Research: Tonsil Tissue Analysis with FLIM
Experimental Protocol:
- Sample Preparation: Tonsil tissue stained with PanCK antibody conjugated to CF450 fluorophore (PanCK-CF450) [9].
- Image Acquisition: Fluorescence and fluorescence lifetime images acquired using high-speed FLIM system [9].
- Reference Measurement: Autofluorescence reference obtained from unstained tonsil tissue; immunofluorescence reference from PanCK-CF450 in PBS solution [9].
- Phasor Analysis: Fluorescence lifetime decays transformed to phasor domain for separation of signal components [9].
Results:
- The fluorescence lifetime of PanCK-CF450 was approximately 3.5 ns, while autofluorescence lifetime was shorter at approximately 2.2 ns [9].
- Phasor analysis revealed a distinct linear pattern representing the mixture of immunofluorescence and autofluorescence [9].
- The extracted immunofluorescence displayed a clearer pattern of PanCK than the original immunofluorescence without phasor-based autofluorescence removal [9].
- The method showed superior correlation with immunohistochemistry data compared to conventional methods [9].
Neuroscience Application: sFIDA Technology for Protein Oligomer Quantification
Background: Surface-based fluorescence intensity distribution analysis (sFIDA) was developed to quantify various types of protein oligomers that serve as biomarkers for protein misfolding diseases, which are implicated in neurodegenerative disorders [104].
Challenge: The assay typically generates at least 100 images per sample, making manual artifact detection inefficient and creating analysis bottlenecks [104]. Artifacts from contamination or material defects can generate fluorescence signals that distort quantitative evaluation [104].
Solution Implementation:
- Convolutional autoencoder trained on artifact-free sFIDA images [104].
- Model capable of detecting various artifact types including those caused by contamination, nonspecific binding, and material defects [104].
- The method successfully identified artifact-laden images despite the diverse appearance of artifacts depending on sample matrix, antigen, and antibody used [104].
Significance: This automated approach enables reliable detection of artifact-laden images in high-throughput assays, essential for quantitative analysis of protein oligomers relevant to neurological diseases [104].
Infectious Disease Research: Open-3DSIM for Pathogen-Host Interactions
Technology Background: Open-3DSIM is an open-source three-dimensional structured illumination microscopy reconstruction platform that provides superior resolution with reduced artifacts [105].
Advancements:
- Adaptive Parameter Estimation: Uses ±1 and ±2 order frequency peaks for collaborative parameter estimation, improving accuracy under low signal-to-noise conditions [105].
- Frequency Domain Optimization: Implements notch filters to suppress hexagonal artifacts and specialized filters to suppress sidelobe and ringing artifacts [105].
- Multidimensional Imaging: Provides capabilities for 6D imaging (XYZθλT) - incorporating super-resolution, multi-color, dynamic, and polarization data [105].
Application Potential: While not specifically tested on infectious disease samples, the technology's ability to resolve fine cellular structures and dynamic processes makes it particularly valuable for studying pathogen-host interactions at the subcellular level [105].
Experimental Protocols
FLIM-Based Autofluorescence Suppression Protocol
Sample Preparation:
- Prepare tissue sections according to standard protocols for immunofluorescence [68].
- Stain with target primary antibodies followed by fluorophore-conjugated secondary antibodies [68].
- Include controls: unstained tissue for autofluorescence reference and fluorophore in solution for immunofluorescence reference [9].
Image Acquisition:
- Use a FLIM system equipped with a picosecond pulse laser and appropriate detection hardware [9].
- Acquire time-resolved fluorescence data with sufficient photon counts (≥500 photons per pixel) [9].
- Ensure proper system calibration for lifetime measurements [9].
Data Processing:
- Transform fluorescence decay curves to phasor domain using sine and cosine transformations [9].
- Identify reference clusters for autofluorescence and specific immunofluorescence in phasor plot [9].
- Calculate fractional contributions for each pixel using geometrical relationships in phasor space [9].
- Generate autofluorescence-free immunofluorescence image based on calculated fractions [9].
Artifact Detection Protocol for High-Throughput Screening
Image Preprocessing:
- Apply Gaussian blur (5×5 pixel kernel) to reduce background noise variance [104].
- Remove background using intensity threshold (mean + 5 standard deviations) [104].
- Standardize image size for processing efficiency [104].
Model Training:
- Train convolutional autoencoder exclusively on artifact-free images [104].
- Optimize model capacity to learn essential patterns of authentic signals [104].
- Validate model performance on separate test dataset [104].
Artifact Detection:
- Process new images through trained autoencoder [104].
- Compute difference between input and output images [104].
- Flag images with discrepancies exceeding threshold as artifact-laden [104].
- Exclude flagged images from quantitative analysis [104].
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions
| Reagent/Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Fixatives | 4% Paraformaldehyde, Methanol, Acetone [106] [68] | Stabilizes cell morphology; inactivates enzymes | Aldehyde-based fixatives preserve structure; organic solvents also permeabilize [106] |
| Permeabilization Agents | Triton X-100 (0.1-0.25%), Tween-20, Digitonin [106] [68] | Enables antibody access to intracellular targets | Concentration and time must be optimized; stronger detergents for nuclear targets [107] |
| Blocking Agents | BSA (2-10%), Normal Serum (species-matched) [106] [68] | Reduces nonspecific antibody binding | Use serum from secondary antibody species; avoid primary antibody host serum [108] |
| Fluorophores | Alexa Fluor series (488, 594, 647), CF dyes [68] | Fluorescent reporting | Newer dyes offer better photostability than FITC/TRITC [107] |
| Mounting Media | ProLong Gold, Anti-fade reagents [109] [68] | Preserves fluorescence; reduces photobleaching | Use anti-fade reagents especially for FITC/TRITC [109] |
| Autofluorescence Suppression | Sudan Black B, Trypan blue, CuSO₄ [9] [110] | Chemical quenching of autofluorescence | Can decrease specific fluorescence; not always effective [9] |
FAQs and Troubleshooting Guides
Weak or No Signal
Q: My immunofluorescence staining shows weak or no signal despite confirmed antigen presence. What could be causing this?
Potential Causes and Solutions:
- Fluorophore bleaching: Avoid extended light exposure during incubations and store samples in dark with anti-fade mounting media [109] [107].
- Inadequate fixation: Use freshly prepared 4% formaldehyde for most applications; optimize fixation time (typically 10-20 minutes) [109] [68].
- Incorrect antibody dilution: Follow manufacturer recommendations; consider increasing concentration for low-abundance targets [109].
- Insufficient permeabilization: For intracellular targets, use 0.1-0.25% Triton X-100 for 10-15 minutes after fixation [108] [68].
- Suboptimal incubation conditions: Primary antibody incubation at 4°C overnight often provides superior results compared to shorter room temperature incubations [109].
High Background and Autofluorescence
Q: My samples exhibit high background fluorescence that obscures specific signal. How can I reduce this?
Troubleshooting Strategies:
- Confirm autofluorescence: Use unstained controls to identify intrinsic fluorescence [109] [110].
- Chemical quenching: Test autofluorescence quenchers like Sudan Black B or CuSO₄, but be aware they may also diminish specific signal [9] [110].
- FLIM approach: Implement fluorescence lifetime imaging if available, as it effectively separates autofluorescence based on lifetime differences [9].
- Optimize antibody concentrations: Overly concentrated antibodies increase nonspecific binding; titrate to optimal dilution [109] [110].
- Improve blocking: Extend blocking time to 1 hour; use serum from secondary antibody species or charge-based blockers like Image-iT FX Signal Enhancer [109] [111].
- Fixative selection: Avoid glutaraldehyde which increases autofluorescence; use fresh formaldehyde preparations [110] [111].
Artifacts and Non-Specific Staining
Q: My images show unusual patterns and non-specific staining that don't match expected biological structures. How can I identify and address these artifacts?
Identification and Solutions:
- Microscope-related artifacts: Regularly calibrate equipment; check for focus issues, uneven illumination, or optical aberrations [104].
- Sample preparation artifacts: Ensure consistent fixation and avoid sample drying during processing [109] [108].
- Secondary antibody cross-reactivity: Include secondary-only controls; spin antibody solutions to remove aggregates [110].
- Automated detection: For high-throughput workflows, implement convolutional autoencoder approaches to identify artifact-laden images [104].
- Spectral overlap in multiplexing: Choose fluorophores with minimal emission overlap; verify filter sets are appropriate for fluorophore combinations [110] [107].
Workflow Diagrams
Diagram 1: Autofluorescence Solutions Workflow
Diagram 2: FLIM Experimental Workflow
The case studies presented demonstrate significant advancements in overcoming autofluorescence challenges across oncology, neuroscience, and infectious disease research. The integration of high-speed FLIM provides a powerful solution for robust autofluorescence separation, while convolutional autoencoders offer efficient artifact detection in high-throughput workflows. These technologies, combined with optimized experimental protocols and appropriate reagent selection, enable researchers to obtain cleaner, more reliable data for critical biomedical investigations. As these methods continue to evolve and become more accessible, they hold promise for further enhancing the precision and reproducibility of immunofluorescence research across diverse applications.
Conclusion
Solving the challenge of autofluorescence is not a one-size-fits-all endeavor but requires a strategic toolkit. Foundational knowledge of its sources enables precise problem identification. Methodologically, while chemical and photobleaching techniques offer accessible solutions, emerging technologies like high-speed FLIM represent a paradigm shift by digitally isolating signals based on lifetime, vastly improving reliability. A systematic troubleshooting approach is crucial for optimizing these techniques in specific tissue contexts. The validation of these methods against standards like IHC confirms their power to enhance diagnostic accuracy and research rigor. Looking forward, the effective suppression of autofluorescence is a critical enabler for the future of biomedical research, paving the way for robust, high-plex spatial biology, accelerating drug discovery by providing cleaner phenotypic data, and ultimately strengthening the foundation of precision medicine.
References
- 1. A Biological Breakdown of Autofluorescence: Why Your ... [https://evidentscientific.com/en/insights/a-biological-breakdown-of-autofluorescence-why-your-samples-naturally-glow]
- 2. Autofluorescence - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/autofluorescence]
- 3. SAIBR: a simple, platform-independent method for spectral ... [https://pubmed.ncbi.nlm.nih.gov/35713287/]
- 4. Learn how to Remove Autofluorescence from your ... [https://www.leica-microsystems.com/science-lab/life-science/learn-how-to-remove-autofluorescence-from-your-confocal-images/]
- 5. Tips to Minimize Autofluorescence [https://fluorofinder.com/autofluorescence/]
- 6. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOorElivN0pNG1g5bQhZcbji_tywkvaOTYzxO4LPffRc7XSQJGd3z]
- 7. 4-Plex Immunofluorescence Staining | DAPI + Four Marker ... [https://www.ihisto.io/molecular-pathology/immunofluorescence-staining-4plex]
- 8. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOorG7Cx_DPeEqoUaY8SYGTyDELSMT0DX7BA___NUqd8RP70EOB02]
- 9. A robust method for autofluorescence-free ... [https://www.nature.com/articles/s41598-025-89142-6]
- 10. : A potential pitfall Autofluorescence -based... in immunofluorescence [https://pubmed.ncbi.nlm.nih.gov/29458079/]
- 11. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOooKKv3gHoHprHvfiHOupdK6Gbz0vkFdaRctGIfnkD1XEIchciIZ]
- 12. Autofluorescence Spectroscopy and Imaging: A Tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4289852/]
- 13. IF实验中怎么去除自发荧光? [https://www.ptgcn.com/news/blog/how-can-self-generated-fluorescence-be-removed-in-an-if-experiment/]
- 14. Efficient removal of naturally-occurring lipofuscin ... [https://www.sciencedirect.com/science/article/pii/S1526590025005863]
- 15. A facile method for immunofluorescence microscopy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3066058/]
- 16. Autofluorescence [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/autofluorescence/]
- 17. IHC Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 18. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/]
- 19. ICC/IF Troubleshooting [https://www.antibodies.com/applications/immunofluorescence/immunofluorescence-troubleshooting]
- 20. Cell Culture | Sample Preparation for Imaging [https://ibidi.com/content/437-cell-preparation-for-imaging]
- 21. Troubleshooting - Immunofluorescence Assays [https://ibidi.com/content/366--troubleshooting]
- 22. How To Improve Your Immunofluorescence By Overcoming Autofluorescence | VectorLabs [https://vectorlabs.com/blog/how-to-improve-your-immunofluorescence-by-overcoming-autofluorescence/]
- 23. Autofluorescence and Nonspecific Immunofluorescent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5582670/]
- 24. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoqWQn2rivuR1m_TzhLprqVSnrygENvPfkfa-BDWhG0VMdq9DO4p]
- 25. Guide to Fiber Photometry|12 FAQs Answered [https://www.rwdstco.com/answers-to-12-frequently-asked-questions-about-fiber-photometry-experiments/]
- 26. Autofluorescence-based tissue characterization enhances ... [https://www.nature.com/articles/s41598-024-67366-2]
- 27. Technical Tips [https://www.jacksonimmuno.com/secondary-antibody-resource/category/technical-tips/]
- 28. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoq8NOPyyAdGa1RY1W36N2JLx04hlQ-NkjiaofU_TY7t2b90m299]
- 29. Five ways to extract autofluorescence (and store it) [https://www.colibri-cytometry.com/post/five-ways-to-extract-autofluorescence-and-store-it]
- 30. Sudan Black B Pretreatment to Suppress Autofluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12356128/]
- 31. Pre-culture Sudan Black B treatment suppresses ... [https://www.nature.com/articles/s41598-017-08723-2]
- 32. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOopdU78dbo4Qh7tiznV5m1_FLXl9TdJdyvJqK1wp4H1vri4DgcoD]
- 33. Sudan Black B treatment reduces autofluorescence and ... [https://pubmed.ncbi.nlm.nih.gov/20552552/]
- 34. Sodium Borohydride - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/sodium-borohydride]
- 35. Quantitative investigation of photobleaching-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11828445/]
- 36. Fluorescence quenching by high-power LEDs for highly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9479452/]
- 37. Photobleaching as a Signal Removal Tool in Multiplex ... [https://brukerspatialbiology.com/photobleaching-as-a-signal-removal-tool-in-multiplex-fluorescence-imaging/]
- 38. How to Reduce Autofluorescence [https://www.southernbiotech.com/how-to-reduce-autofluorescence/]
- 39. Seeing red (and beyond): extended red sensitivity for life science microscopy applications [https://news.jai.com/blog/extended-red-sensitivity]
- 40. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOorXROjYAhZQwG7_d2fsWZUKxXp-Mf1XasDKOvgDhtPl52jPNxnP]
- 41. Far-Red and Near Infrared Dyes [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/far-red-and-near-infrared-dyes/]
- 42. Near-Infrared Fluorophores For Fluorescence Imaging [https://fluorofinder.com/infrared-fluorophores/]
- 43. Spectrum [CellTrace Far Red] - Fluorescence [https://www.aatbio.com/fluorescence-excitation-emission-spectrum-graph-viewer/celltrace_far_red]
- 44. Near Infrared (NIR) Fluorescent Dyes [https://www.lumiprobe.com/c/nir-infrared-dyes]
- 45. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOopQ1ljSuH7qQoQL5LAgRk1wegcKzb_gYk8PZMdHEFPJRflcjl2p]
- 46. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOopbTZjmVQGzifcaP0fcVfXFRvTN66ZxJ8ljt0bAqCKPwYw6aBSA]
- 47. Fluorescence lifetime imaging microscopy: fundamentals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7219965/]
- 48. A Guide to Fluorescence Lifetime Imaging Microscopy (FLIM) [https://www.leica-microsystems.com/science-lab/life-science/a-guide-to-fluorescence-lifetime-imaging-microscopy-flim/]
- 49. Predicting immune checkpoint inhibitors response via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535979/]
- 50. A Guide to Fluorescence Lifetime Microscopy and Förster's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8274369/]
- 51. Pixel-by-pixel autofluorescence corrected FRET in ... [https://www.nature.com/articles/s41598-023-30098-w]
- 52. Quantitative FRET Analysis by Fast Acquisition Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2527249/]
- 53. A Common Mistake in Lifetime-Based FRET Measurement [https://www.becker-hickl.com/literature/application-notes/a-common-mistake-in-lifetime-based-fret-measurement/]
- 54. FLIM-FRET Microscopy | W.M. Keck Center for Cellular Imaging [https://kcci.virginia.edu/flim-fret-microscopy]
- 55. Overcoming Limitations of FRET Measurements - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5835960/]
- 56. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOooE3s9M5U3xPr27DRL5nHdZ1ReReTwxwilCZ8thY3Nsr3TDalYv]
- 57. How to Reduce Autofluorescence [https://www.labcompare.com/10-Featured-Articles/577255-How-to-Reduce-Autofluorescence/]
- 58. Simple Elimination of Background Fluorescence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5614400/]
- 59. A robust method for autofluorescence-free ... [https://pubmed.ncbi.nlm.nih.gov/39953137/]
- 60. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoq04z7A1MJsyHbvVmkb6q3Xy2ySSofhH042O4_fWdqMBuevwph6]
- 61. Autofluorescence [https://en.wikipedia.org/wiki/Autofluorescence]
- 62. Autofluorescence can interfere with flow cytometry imaging [https://www.bdbiosciences.com/en-us/learn/science-thought-leadership/blogs/Autofluorescence-imaging]
- 63. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOorUY5kDqH_7MrKWl8coVkDac7PfvGJYL5TUN0TkM8vyAY85OKWW]
- 64. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOorjsJKFBn6rtQ6pJPERCBGAstL-bUUKtHo1jG1dZzynB2W0hj00]
- 65. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOoozViHsPDDB5MRTtTx44bKirFK74x1okXObvpEaABOxi01XtiW3]
- 66. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOooWrX7In-lnifk_e8ma7HvhAzHt8hQM_WQPqk1VeHpubUXjArB7]
- 67. Optimized immunofluorescence for liver structure analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11999924/]
- 68. 免疫荧光试剂选择指南 [https://www.share-bio.com/article/381.html]
- 69. 成功的免疫荧光法:抗体稀释度和孵育条件 - CST 博客 [https://blog.cellsignal.cn/successful-immunofluorescence-antibody-dilution-and-incubation]
- 70. 免疫荧光(IF) 疑难排解指南 [https://www.cellsignal.cn/learn-and-support/troubleshooting/if-troubleshooting-guide]
- 71. 免疫荧光背景太强怎么解决 [https://www.biomart.cn/lab-web/que/316nrkago405e/322hp04go3631.html]
- 72. 古朵实验:免疫荧光染色背景色太强如何解决? - ELISA试剂盒 [http://m.fkbio-sh.com/article/show-248178.html]
- 73. 免疫荧光法(IF)方案 [https://cn.sinobiological.com/category/if-protocol]
- 74. 优化多色免疫荧光试剂盒(OMIPs) | Thermo Fisher Scientific [https://www.thermofisher.cn/cn/zh/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-74/bioprobes-74-optimized-multicolor-immunofluorescence-panels-omips.html]
- 75. 7色同步检测!新一代多重荧光免疫组化 - 诺唯赞 [https://bio.vazyme.com/news_xq/86.html]
- 76. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOoq8tSrli6-_LgrWh6RPwgD6JapvoFJ1sjHOe2Q3Q01cAuWf4E4w]
- 77. Autofluorescence: A potential pitfall in immunofluorescence ... [https://www.sciencedirect.com/science/article/abs/pii/S002217591730546X]
- 78. Vector TrueVIEW Autofluorescence Quenching Kit [https://vectorlabs.com/products/trueview-autofluorescence-quenching-kit/?srsltid=AfmBOopkc_AIOQgEufD2Xl8yd_wAn6Ce1lMcS5ggxgJ7Ix6CH_-YFUvJ]
- 79. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoryMHtG4slQrHkcsiIlES86QimN8mraR2gl7h_qXgjiKK8LbJeK]
- 80. Impacts of autofluorescence on fluorescence based ... [https://bmcneurosci.biomedcentral.com/articles/10.1186/s12868-022-00703-1]
- 81. 5 Tips To Reduce Autofluorescence [https://www.bosterbio.com/blog/post/5-tips-to-reduce-autofluorescence?srsltid=AfmBOopyn1Kdnhk2B4T42QeVBKIlyfhdjjN1KA83Au6aW6YDA6KxF9jn]
- 82. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOoqu5QG2aFK5-TXfon_7vZG17F1VFYGT4Q_Us6kJJ4JZyduNbwWp]
- 83. More Autofluorescence Troubleshooting for Tissue Imaging [https://visikol.com/blog/2022/03/22/more-autofluorescence-troubleshooting-for-tissue-imaging/]
- 84. Autofluorescence Quenching in Decellularized Plant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399283/]
- 85. Optimization, Design and Avoiding Pitfalls in Manual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6786767/]
- 86. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOoqk2nhRVtE1zbXaAmX4E2IOrI1K0rOT9of9t7QXK-nam3SFkgHm]
- 87. A beginners guide to Immunohistochemistry [https://www.ptglab.com/news/blog/a-beginners-guide-to-immunohistochemistry/?srsltid=AfmBOopmIde_NqUX-AKnMGs29GZNnsyLnF85oLmgatuO013libaRJUWE]
- 88. High-plex immunofluorescence imaging and traditional ... [https://www.nature.com/articles/s43018-023-00576-1]
- 89. Fluorescence lifetime imaging microscopy approach reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339318/]
- 90. Fluorescence Lifetime Multiplexing (FLEX) for ... [https://www.nature.com/articles/s42003-024-06702-8]
- 91. Lipofuscin-like autofluorescence within microglia and its ... [https://www.nature.com/articles/s41467-023-42809-y]
- 92. Comprehensive Immunofluorescence Protocols: IF Protocol Hub [https://ifprotocol.org/]
- 93. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOoriHbpVlarXeQ-zNsGDPEKG-6nFCVpytYSfOJOBYz3OI60hKN6_]
- 94. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOorJxDhBXRcVH7yIRsVyWTwkmPvjsTmf10Dey1FZaJ_zTM-h7k8P]
- 95. Multiplex Solutions for Spatial Biology [https://www.cellsignal.com/applications/multiplexing-and-spatial-biology?srsltid=AfmBOopsDbHA-9T_PdqnMuMOLyVQd_AsVkWuVEnGNrB6HWSa0UmuWkMA]
- 96. Spatial Biology Solutions, Multiplex Imaging [https://www.akoyabio.com/spatial-biology-solutions/]
- 97. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoqLx1NH0lvS_ka3O0dXB9nipvrUa9SyAewRuBM1b0g49oq1XZpx]
- 98. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOopWlcs4NBQgbuEosQNOxnR8I5Jquc9UR0mozpLo5gwgjlIFHNZr]
- 99. Causes of Autofluorescence [https://visikol.com/blog/2022/07/21/causes-of-autofluorescence/]
- 100. Optimizing immunofluorescence with high-dynamic-range ... [https://www.nature.com/articles/s41598-024-65187-x]
- 101. 5 Tips To Reduce Autofluorescence [https://www.bosterbio.com/blog/post/5-tips-to-reduce-autofluorescence?srsltid=AfmBOophIaA_9KVznD6n0BtVkquMTxb0pZtC0lVz_kaOo8QAfGBpyBZr]
- 102. 5 Controls for Immunofluorescence: An Easy Guide [https://bitesizebio.com/44370/controls-for-immunofluorescence-a-beginners-guide/]
- 103. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOopiN9zXSZPj_TFNoU4xWCACP_f_6fK82nmBxvG5fjsVDLLIRzVC]
- 104. Artifact detection in fluorescence microscopy using ... [https://www.nature.com/articles/s41598-025-18943-6]
- 105. 席鹏课题组提出开源三维结构光照明显微成像重建算法平台 [https://nbic.pku.edu.cn/cxcg/682e2fd9734f456b8bd1ca5e74859de6.htm]
- 106. The principle and method of Immunocytochemistry (IC) [https://www.mblbio.com/bio/g/support/method/immunocytochemistry.html]
- 107. 优化免疫荧光实验方案获取最优质细胞图像的技巧 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/protein-biology/flow-cytometry/antibody-immunofluorescent-tips-best-practices?srsltid=AfmBOophR4s0ciy6bD4I2yQ-iybfO6YIlkgsQl6nJLcdubarv5ag1xzM]
- 108. 免疫细胞化学免疫荧光(ICCIF) 手把手教学! 一看就懂噻~ | MCE [https://blog.sciencenet.cn/blog-3536222-1508235.html]
- 109. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOorQOPsrcFCiySTipW-KLym__KuFgyPhH3poNmYhycntqwMAmD0p]
- 110. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOoo5AVUj8Qp15U9Ekbh3ommvlzp4YL-LUTDg_R8RbGD2GMbNxBKX]
- 111. A Practical Guide to Immunocytochemistry [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-issues-2011/bioprobes-66-october-2011/guide-to-immunocytochemistry.html]