Solving Spotty Staining: A Scientist's Guide to Troubleshooting Uneven IHC Background
This article provides a comprehensive guide for researchers and drug development professionals tackling spotty, uneven background staining in Immunohistochemistry (IHC).
Solving Spotty Staining: A Scientist's Guide to Troubleshooting Uneven IHC Background
Abstract
This article provides a comprehensive guide for researchers and drug development professionals tackling spotty, uneven background staining in Immunohistochemistry (IHC). Covering foundational principles to advanced validation techniques, it details the common causes—from inadequate deparaffinization and drying artifacts to suboptimal blocking and antibody issues. The content offers systematic troubleshooting workflows, method optimization strategies for robust protocols, and emphasizes the critical role of controls and quantitative analysis to ensure data reproducibility and reliability in preclinical and clinical research.
Understanding Spotty Staining: Identifying Causes and Impact on Data Integrity
What are the common causes of spotty and uneven background staining?
Spotty and uneven background staining in immunohistochemistry (IHC) and histology experiments can arise from numerous sources throughout the sample preparation and staining workflow. The table below summarizes the primary causes, their descriptions, and the specific artifacts they produce.
Table 1: Common Causes of Spotty and Uneven Staining
| Cause Category | Specific Cause | Description of Artifact |
|---|---|---|
| Slide Preparation | Inadequate Deparaffinization [1] | Spotty, uneven background staining. |
| Dry Tissue Sections [1] | Loss of signal; sections must remain covered in liquid. | |
| Contaminated Water Bath [2] | "Floaters" or debris on the slide, out of the tissue plane. | |
| Fixation & Tissue Processing | Over- or Under-Processed Tissue [2] | Chatter (over-processed) or "exploding" sections (under-processed). |
| Acidic Formalin [2] | Searing of tissue edges and over-drying of tissues. | |
| Delayed Fixation [3] | Loss of RNA (for ISH) and degradation of targets. | |
| Adhesive Problems | Protein-Based Adhesives [3] | Uneven staining due to pooling of reagents beneath lifting sections. |
| Inconsistent Adhesive Application [2] | Variable background staining between slides. | |
| Detection System | Endogenous Peroxidase Activity [1] | Excess, diffuse background signal when using HRP-based detection. |
| Endogenous Biotin [1] | High background in tissues like kidney and liver with biotin-based detection. | |
| Secondary Antibody Cross-Reactivity [1] | High background, especially in mouse-on-mouse staining. |
What experimental protocols can resolve these issues?
Protocol 1: Addressing Inadequate Deparaffinization and Section Adhesion
- Problem: Spotty, uneven background staining from incomplete wax removal or poor section adhesion [1].
- Solution:
- Repeat the experiment with new tissue sections.
- Use fresh xylene or other dewaxing agents to ensure complete paraffin removal [1].
- Use charged slides for superior and consistent adhesion. Avoid using protein-based adhesives (e.g., gelatin, albumin) on charged slides, as they can block the charged surface and lead to uneven staining or section lifting [3].
- Ensure sections are thoroughly dried onto the slide before staining [3].
Protocol 2: Optimizing Antigen Retrieval for Consistent Staining
- Problem: Lack of staining or uneven staining intensity due to masked epitopes.
- Solution: Antigen retrieval reverses formaldehyde-induced crosslinks. The method significantly impacts results [1].
- Preferred Method: Use a microwave oven for heating slides in antigen retrieval buffer [1].
- Alternative Method: For some targets, a pressure cooker may enhance signals beyond what a microwave achieves. Water baths are not recommended [1].
- Buffer: Always prepare a fresh 1X antigen retrieval solution daily and use the buffer specified on the antibody datasheet [1].
Protocol 3: Blocking and Detection to Minimize High Background
- Problem: High, diffuse background from endogenous enzymes, biotin, or secondary antibodies.
- Solution:
- Blocking: Incubate slides in 1X TBST with 5% normal serum from the host species of the secondary antibody for 30 minutes prior to primary antibody incubation [1].
- Peroxidase Quenching: If using an HRP-based detection system, quench slides in 3% H₂O₂ (in RODI water) for 10 minutes before the primary antibody to neutralize endogenous peroxidase activity [1].
- Biotin Block: For tissues with high endogenous biotin (e.g., kidney, liver), use a polymer-based detection system instead of avidin-biotin complex (ABC). Alternatively, perform a biotin block after the standard blocking step [1].
- Secondary Antibody Control: Always include a control slide incubated with only the secondary antibody to identify non-specific binding and cross-reactivity, particularly in mouse-on-mouse studies [1].
Troubleshooting Pathway for Spotty Staining
How can I prevent uneven staining during sample collection and fixation?
Proper sample handling before and during fixation is critical for preventing artifacts that lead to uneven staining.
- Prompt Fixation: Immerse samples in fixative immediately after collection. Delayed fixation, especially for RNA in situ hybridization (ISH), encourages degradation by endogenous RNases, leading to weak or variable staining [3].
- Avoid Drying Artifacts: Do not use gauze or other porous materials to handle small biopsies, as these can wick moisture from the tissue, causing drying artifacts and uneven staining. Use non-porous instruments or saline to transfer tissue [2].
- Use Fresh, Buffered Formalin: Old or improperly stored formalin can become acidic, causing "searing" of tissue edges and over-drying. This creates a barrier that prevents even reagent penetration [2].
- Consistent Fixation Conditions: Use known and consistent fixation conditions (type, pH, time, temperature). Inconsistent fixation is a major source of variability, making troubleshooting difficult [3].
What are the best practices for using controls to interpret staining artifacts?
Appropriate controls are non-negotiable for determining if staining is specific or an artifact.
- Positive Control: A tissue or cell pellet known to express the target. This confirms that the entire staining protocol, from antibody to detection, is working correctly. A lack of staining in the test sample but positive staining in the control indicates a problem with the test sample itself (e.g., absence of antigen, improper fixation) [1].
- Negative Control (No Primary Antibody): A slide from the same test sample processed without the primary antibody but with all other reagents. This controls for non-specific signal from the detection system or secondary antibody cross-reactivity. Staining in this control indicates high background that needs to be blocked [1].
- Biological Negative Control: A tissue known not to express the target. This helps confirm the specificity of the antibody.
- For ISH: Use a known positive tissue and a negative control with a non-specific probe to validate every run [3].
Essential Controls for Stain Validation
What key reagent solutions are essential for preventing staining artifacts?
The choice of reagents is fundamental to achieving clean, reproducible results. The table below details key solutions and their functions.
Table 2: Research Reagent Solutions for Optimal Staining
| Reagent Category | Specific Product/Type | Function in Preventing Artifacts |
|---|---|---|
| Antigen Retrieval Buffers | Citrate Buffer, EDTA, Tris-EDTA [1] | Reverses cross-links from formalin fixation to unmask hidden epitopes, preventing false negatives. |
| Antibody Diluent | SignalStain Antibody Diluent / Optimized Diluent [1] | Maintains antibody stability and prevents non-specific binding, reducing high background. |
| Detection System | Polymer-based (e.g., SignalStain Boost) [1] | Provides high sensitivity and avoids endogenous biotin, reducing background in sensitive tissues. |
| Blocking Solution | 1X TBST with 5% Normal Goat Serum [1] | Occupies non-specific binding sites on tissue to minimize background staining. |
| Wash Buffer | 1X TBST (Tris-Buffered Saline with Tween) [1] | Removes unbound antibody and reagents; adequate washing is critical for low background. |
| Mounting Medium | Xylene-compatible or specific substitute [2] | Preserves staining and allows for clear microscopy. Must be compatible with clearing agents. |
How does the detection system choice influence background staining?
The detection system is a major determinant of sensitivity and background.
- Polymer-Based Systems: These are more sensitive than traditional avidin/biotin-based (ABC) systems and are recommended. They consist of multiple secondary antibody and enzyme molecules linked to a polymer backbone, providing significant signal amplification without the use of biotin, thereby eliminating background from endogenous biotin [1].
- Biotin-Based Systems (ABC): These systems can produce high background in tissues with high endogenous levels of biotin, such as liver and kidney. If you must use them, a biotin-blocking step may be necessary [1].
- Directly HRP-Conjugated Primaries: These generally do not provide sufficient signal amplification for most IHC applications and are not commonly used [1].
Table 3: Comparison of Detection Systems
| System Type | Sensitivity | Risk of Endogenous Biotin Background | Recommended Use |
|---|---|---|---|
| Polymer-Based | High | Low | General use, especially for biotin-rich tissues. |
| Biotin-Based (ABC) | High | High | Use with biotin block if endogenous biotin is present. |
| Directly Conjugated | Low | None | Limited to high-abundance targets. |
Frequently Asked Questions
What are the immediate signs that my staining issue is caused by deparaffinization? The most immediate signs are spotty or uneven background staining across the tissue section [4]. This is distinct from high, uniform background and often appears as a random pattern of darker and lighter areas.
Can inadequate deparaffinization affect my positive staining signal? Yes. Incomplete removal of paraffin prevents antibodies from accessing the target epitopes, which can lead to weak or a complete lack of specific staining, even if the protocol is otherwise correct [5].
My deparaffinization solution is not expired. What else could be wrong? Using a ready-to-use solution as if it needed dilution, or vice versa, is a common error [5]. Always verify the correct preparation of all solutions. Also, ensure the heating elements on automated machines are functioning correctly to reach the paraffin's melting point [5].
My slides were stored for a long time. Could this be a factor? Yes. Slides for IHC may lose signal over time in storage [4]. For best results, use freshly cut sections. If slides must be stored, keep them at 4°C and avoid baking them before storage [4].
Besides deparaffinization, what other slide preparation issues can cause problems? Using the wrong type of slide is a critical error. For formalin-fixed, paraffin-embedded (FFPE) tissues, ensure you are using positively charged slides to prevent tissue loss during stringent processing steps. Using a regular slide will result in the tissue detaching [5].
Troubleshooting Guide: Spotty/Uneven Background Staining
| Problem Cause | Symptoms | Solution |
|---|---|---|
| Inadequate Deparaffinization | Spotty, uneven background; weak or absent specific staining [4] [5]. | Repeat with new tissue sections and fresh xylene [4]. Verify solution preparation and oven/heat pad temperature [5]. |
| Improper Blocking | Dark dots randomly scattered across the blot (also applicable to IHC membranes) [6]. | Ensure the blocking agent (e.g., BSA, milk) is completely dissolved before use. Filter buffers through a 0.2 µm filter if needed [6]. |
| Antibody Aggregation | Dark spots or patches on the blot or membrane [6]. | Use a fresh aliquot of antibody. If not possible, filter the antibody solution through a 0.2 µm filter to remove aggregates [6]. |
| Air Bubbles | Uneven white spots or patches where transfer or antibody binding did not occur [6]. | Carefully remove all air bubbles when assembling the transfer sandwich or during antibody incubation. Ensure gentle agitation during incubations [6]. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| Fresh Xylene | Effectively dissolves and removes paraffin wax from tissue sections to expose antigens [4]. |
| SignalStain Antibody Diluent | An optimized buffer to dilute the primary antibody, which can be critical for achieving a strong, specific signal with low background [4]. |
| SignalStain Boost IHC Detection Reagent (HRP, Polymer) | A highly sensitive, polymer-based detection system that provides superior signal amplification compared to older biotin-based systems [4]. |
| TBST Buffer with 5% Normal Goat Serum | Used for washing and blocking to reduce non-specific background staining [4]. |
| 3% H₂O₂ in RODI Water | Quenches endogenous peroxidase activity in tissues, preventing false-positive signals when using HRP-based detection [4]. |
| Ponceau S Stain | A reversible stain used to quickly assess the quality and evenness of protein transfer onto a membrane in Western blotting [6]. |
Experimental Protocol: Correct Deparaffinization and Slide Preparation
A robust deparaffinization and rehydration protocol is fundamental for high-quality IHC results. The following workflow details the critical steps to prevent spotty staining.
Detailed Methodology
- Slide Baking: Bake slides at 60°C for 30-60 minutes. This ensures the tissue is firmly adhered to the slide. A key detail is to confirm the tissue is completely dry and no water is trapped under the section, as this can cause tissue loss during subsequent steps [5].
- Deparaffinization: Immerse slides in a first bath of fresh xylene for the time specified in your protocol (e.g., 5-10 minutes). Transfer the slides to a second bath of fresh xylene for an equal duration. Using old or overused xylene is a primary cause of inadequate deparaffinization and subsequent spotty staining [4] [5].
- Rehydration: Hydrate the tissue through a series of graded ethanol washes to prepare it for an aqueous environment.
- 100% Ethanol (2 changes)
- 95% Ethanol (1 change)
- 70% Ethanol (1 change)
- Rinse: Rinse the slides gently in distilled or deionized water.
- Antigen Retrieval: Proceed with the appropriate antigen retrieval method. For most targets, a microwave oven is the preferred and recommended method, as a water bath often yields suboptimal results. For some difficult targets, a pressure cooker may provide enhanced signal [4].
Troubleshooting Guides
How does tissue fixation contribute to spotty, uneven background staining?
Inadequate fixation is a primary cause of uneven staining. When tissue is not fixed properly or promptly, several issues can arise that lead to background staining problems.
- Incomplete Fixation: If the fixative does not fully penetrate the tissue, the inner regions remain under-fixed. This can cause variable staining intensity across the tissue section, with well-fixed edges staining differently than under-fixed centers. The internal proteins are not stabilized, leading to diffusion and non-specific binding of dyes during staining [7].
- Delay in Fixation: Placing tissues in carrying media (like saline) for extended periods before fixation can initiate tissue degradation through autolysis and bacterial decomposition [7]. This degradation releases cellular contents that can bind stains non-specifically, creating a spotty, uneven background.
- Use of Acidic Formalin: Formalin that has been stored improperly, such as in direct sunlight, can become acidic. Acidic formalin causes a "searing" or "burned" appearance on the tissue's outer edge. This altered protein layer acts as a barrier, preventing uniform reagent infiltration during staining and leading to uneven results [2].
What embedding and sectioning errors lead to uneven staining?
The processes of embedding and sectioning are critical for producing a uniform surface for staining. Errors here directly cause physical artifacts that result in spotty and uneven staining.
- Improper Sectioning Technique: Sections that are cut at an angle, too thick, or too thin will not stain uniformly. Angled or thick sections prevent dyes from penetrating evenly, while thin sections may tear or have missing parts, leading to a blotchy appearance [8]. "Chatter" (a ripple effect in the section) caused by over-processed, brittle tissue also creates an uneven surface for dye application [2].
- Floaters and Contamination: "Floaters" are small tissue fragments that contaminate the slide during sectioning or from a dirty water bath. When these foreign tissues are present on your slide, they will pick up stain, creating dark spots and a distracting, uneven background [2].
- Tissue Processing Mismatch: Placing small, delicate biopsies on an overnight processing protocol designed for larger tissues will cause over-dehydration. This makes the tissue hard and brittle, leading to excessive cracking and poor sectioning. These cracks and fissures trap stain, creating dark lines and an irregular staining pattern [2].
How can water quality and reagent contamination cause a pink hazy background?
Carryover contamination of reagents, particularly water into alcohols and xylenes, is a common culprit behind a specific type of background staining: a diffuse pink haze.
- Water Contamination in Alcohols and Xylenes: During the staining process, water can be carried over from rinsing steps into the dehydrating alcohols. If these alcohols are not changed regularly, their water content increases. This water is then transferred to the xylene clearing agents [2].
- Eosin Seeping: Excess water in the xylene causes the eosin stain (which is pink) to seep from the tissue. This presents as a generalized pink haze over the entire slide, obscuring cellular details [2].
- Poor Water Quality: The pH and mineral content of tap water used in staining procedures can be variable. A basic pH tap water can raise the pH of slightly acidic hematoxylin, making it less effective and potentially contributing to an overall blotchy and suboptimal nuclear stain [2].
How do adhesives and slides contribute to background staining?
The method used to adhere the tissue section to the glass slide can be a direct source of background staining.
- Albumin and Protein Adhesives: Historically, laboratories used albumin or other protein-based adhesives. These adhesives can bind dye molecules, leading to significant background staining across the entire slide, which is especially problematic for immunohistochemistry [2].
- Inconsistent Use of Adhesives: When technologists manually add different amounts of adhesive to a water bath, it leads to slide-to-slide variability, with some slides having heavy background stain from excess adhesive [2].
- Solution: Using positively charged slides is the recommended practice. They provide consistent adhesion without the use of additional glues, thereby eliminating the background staining associated with protein adhesives [2].
What is the impact of frozen tissue section handling on staining uniformity?
Frozen sections are particularly prone to uneven staining if handled incorrectly, often due to the need for speed in intraoperative diagnoses.
- Insufficient Fixation and Rinsing: The most common error is rushing the fixation and rinsing steps prior to staining. The water-soluble media used to support frozen tissues during sectioning must be completely removed, similar to how paraffin is removed from routine samples. If not thoroughly rinsed, this media prevents even dye infiltration, resulting in patchy, uneven staining [2].
- Tissue Drying During Collection: If samples are collected using gauze or other porous materials, water can be wicked away from the tissue, causing drying artifacts. This desiccation leads to dark, irregular staining patterns. This is common with small biopsies [2].
Frequently Asked Questions (FAQs)
What is the best carrying media if formalin is not immediately available?
According to a comparative study evaluating sectioning ability, staining intensity, and microscopic details, Normal Saline (0.9% NaCl) is the preferred carrying media for temporary tissue storage until a proper fixative is available. The study found that tissues held in normal saline showed the least crumbling during sectioning and maintained acceptable nuclear and cytoplasmic staining for up to 18 hours, outperforming other media like honey, local anesthetic, and hydrogen peroxide [7].
Can fixation time affect my ability to section tissue properly?
Yes, fixation time is critical. Under-fixation (inadequate time in formalin) results in tissues that are soft and poorly infiltrated, leading to "exploding" sections or tearing during microtomy. Conversely, over-fixation (prolonged formalin exposure) causes tissues to become overly dehydrated, hard, and brittle. This results in sections with excessive "chatter" or cracking, making them difficult to flatten and stain evenly [2] [8].
My eosin stain has a pink haze over everything. What is the most likely cause?
A diffuse pink haze is most commonly caused by water contamination in your xylene clearing agents. This happens when water is carried over from previous staining steps (like eosin or alcohol baths) into the xylene. The excess water in the xylene causes the eosin stain to seep from the tissue. The solution is to replace your alcohols and xylenes with fresh reagents, especially if they have been used for a high volume of slides [2].
How can I prevent "soap bubble" artifacts in the nuclei?
Nuclear bubbling, which looks like soap bubbles, is caused by protein coagulation and is often a result of poorly fixed samples exposed to high heat. To prevent this [2]:
- Ensure rapid and adequate fixation to stabilize nuclear proteins.
- Avoid using high temperatures (e.g., 70°C) to dry slides after sectioning.
- Lower the oven temperature or allow slides to air dry partially before placing them in the oven.
Why should I avoid using adhesives with charged slides?
Using protein adhesives (like albumin) in combination with positively charged slides is counterproductive. The properties of the adhesive and the charged slide cancel each other out. The adhesive negates the positive charges on the slide, effectively turning it back into a plain, uncharged glass slide, which increases the risk of tissue loss without providing any benefit [2].
Experimental Protocols & Data
Table 1: Impact of Carrying Media on Tissue Quality Over Time
This table summarizes quantitative data from a study that assessed the sectioning ability and staining quality of tissues held in different carrying media for various time intervals before standard formalin fixation [7].
| Time Interval | Normal Saline | 10% Honey | Local Anesthetic | 2% Hydrogen Peroxide |
|---|---|---|---|---|
| 6 Hours | Good sectioning; Good staining | Good sectioning; Good staining | Good sectioning; Good staining | Significant crumbling; Poor staining |
| 12 Hours | Good sectioning; Good staining | Significant crumbling | Significant crumbling | Not Acceptable |
| 18 Hours | Good sectioning; Acceptable staining | Not Acceptable | Not Acceptable | Not Acceptable |
| 24-30 Hours | Not Acceptable | Not Acceptable | Not Acceptable | Not Acceptable |
Key Finding: Normal Saline is the most effective holding media, preserving tissue integrity and staining quality for up to 18 hours, while Hydrogen Peroxide is unsuitable [7].
Table 2: Troubleshooting Guide for Tissue Processing Artifacts
This table links common processing errors to their observable effects and provides direct solutions.
| Processing Error | Observed Artifact | Recommended Solution |
|---|---|---|
| Delay in Fixation | Autolysis, poor nuclear detail, uneven staining [7] | Immerse tissue in fixative immediately after collection; use Normal Saline as a short-term holding media [2] [7] |
| Over-Processing | Tissue chatter, cracking, hard to cut [2] | Use processing protocols tailored to tissue size; avoid placing small biopsies on long overnight protocols [2] |
| Under-Processing | "Exploding" sections, tearing [2] | Ensure adequate processing time for large samples; use processed paraffin for embedding [2] [9] |
| Water in Xylene | Pink haze over eosin stain [2] | Change dehydrating alcohols and clearing xylenes regularly to prevent water carryover [2] |
| Dirty Water Bath | Floaters on slide [2] | Maintain a clean water bath; use filtered or distilled water; clean instruments regularly [2] |
Protocol 1: Optimized Fixation and Embedding for Zebrafish
This protocol, adapted from a study on creating a high-quality reference atlas, minimizes tissue discontinuity, a common sectioning error [9].
- Fixation: Immerse tissue in 10% Neutral Buffered Formalin at 21°C for 24 hours.
- Decalcification: For juveniles and adults, decalcify with 0.35 M EDTA.
- Processing and Embedding: Process formalin-fixed tissues and embed them in plasticized forms of paraffin wax to improve cohesion.
- Sectioning: To prevent tissue loss and fragmentation, periodically hydrate the block surface in ice water between sets of sections.
- Staining: Refine standard H&E staining protocols for optimal results on processed tissues [9].
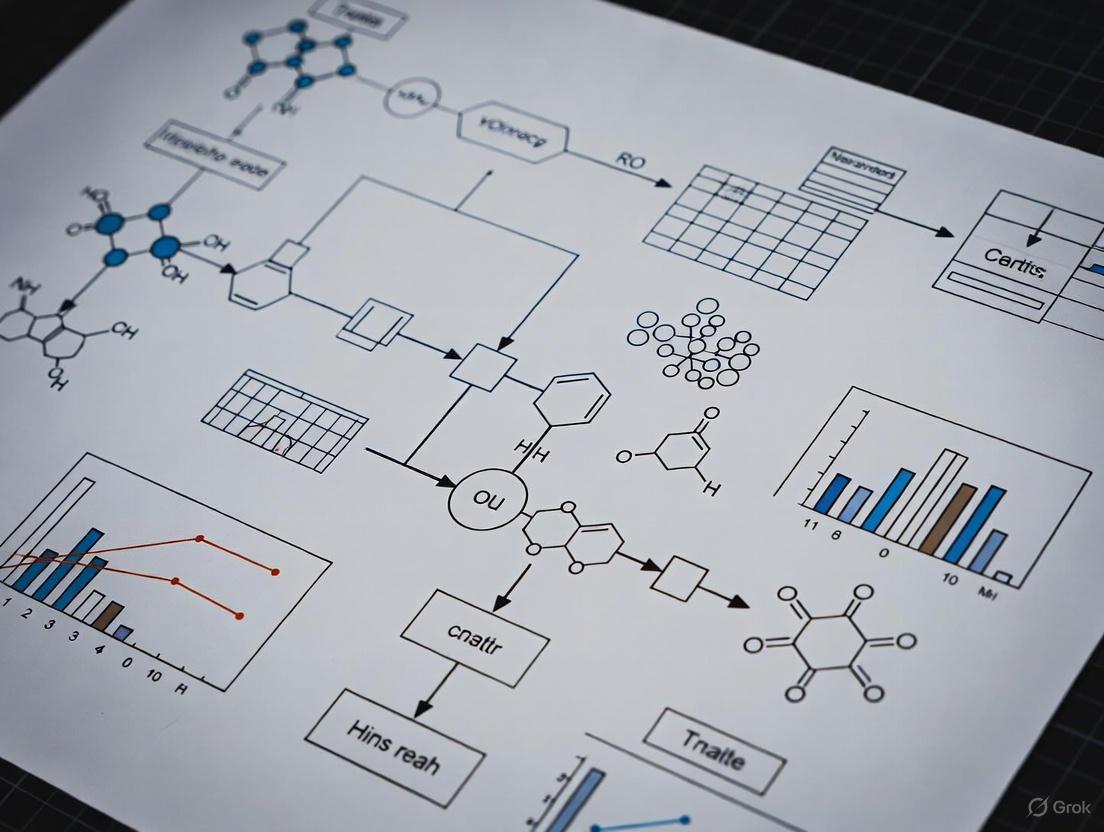
Workflow Diagrams
Diagram 1: Tissue Processing Workflow and Error Propagation. This diagram illustrates the standard H&E staining workflow (blue) and maps common processing errors (red) at each stage that lead to spotty, uneven background staining.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Preventing Processing and Staining Artifacts
| Item | Function & Rationale |
|---|---|
| 10% Neutral Buffered Formalin | The universal fixative for routine histology. The buffering prevents acidity, which causes tissue searing and over-drying, preserving good nuclear detail [2] [9]. |
| Normal Saline (0.9% NaCl) | The preferred isotonic carrying media for temporary tissue storage when fixative is not immediately available. Prevents tissue desiccation and preserves morphology better than alternatives like honey or anesthetics [7]. |
| Positively Charged Slides | Provide consistent adhesion for tissue sections without the need for protein adhesives like albumin, thereby eliminating a significant source of background staining [2]. |
| Deionized (DI) Water | Used for rinsing and preparing solutions. Removes variability in pH and mineral content found in tap water, which can affect hematoxylin staining and dye life [2]. |
| Plasticized Paraffin Wax | Used for embedding. Provides better tissue support and cohesion than standard paraffin, minimizing tissue discontinuity and fragmentation during sectioning [9]. |
| Fresh Xylene & Alcohols | Regular replacement of dehydrating alcohols and clearing agents is critical. Prevents water contamination, which is a primary cause of eosin seepage and a pink hazy background [2]. |
Impact of Non-Specific Binding and Hydrophobic Interactions on Background
Core Concepts: Understanding the Problem
What are the primary causes of spotty, uneven background staining? Spotty and uneven background staining in immunohistochemistry (IHC) and other immunoassays primarily stems from non-specific binding and hydrophobic interactions between antibodies or detection reagents and non-target components in the tissue or on the membrane. The major causes include [10] [11] [12]:
- Insufficient Blocking: Failure to adequately block endogenous enzymes (peroxidases, phosphatases), biotin, or reactive sites on tissues.
- Hydrophobic Interactions: Antibodies non-specifically sticking to proteins and lipids in the tissue due to exposed hydrophobic patches on their surface [13] [12].
- Antibody-Related Issues: Using a primary or secondary antibody concentration that is too high, leading to non-specific binding to off-target epitopes [10] [12].
- Suboptimal Sample Preparation: Issues such as inadequate deparaffinization of tissue sections, tissue drying during the protocol, or over-fixation can create artifacts and increase background [11] [12].
- Cross-Reactivity: The secondary antibody exhibiting affinity for non-target antigens or endogenous immunoglobulins in the sample [10] [11].
What is the molecular basis for non-specific antibody binding? Non-specific binding is governed by the physicochemical properties of the antibody's surface. Research has shown that [13]:
- Surface Patches: Groupings of amino acids with similar properties on the antibody surface are key drivers. The size and nature of hydrophobic patches and charged patches correlate directly with the propensity for nonspecific interactions.
- Trade-off: Nonspecific binding affinity is a trade-off between the area of hydrophobic patches and the total area of charged patches on the antibody's surface.
- Macroscopic Manifestations: These molecular-scale nonspecific interactions can manifest macroscopically as issues like high background staining, high solution viscosity, and even phase separation of antibody solutions under certain conditions [13].
Troubleshooting FAQs & Guides
FAQ: My IHC experiment has high, spotty background. What are the first steps to fix this? Start by addressing the most common causes. First, ensure your tissue sections never dried out during staining, as this causes irreversible non-specific binding [12]. Re-perform deparaffinization with fresh xylene if the background is spotty and uneven [11]. Then, systematically optimize your antibody concentrations; a primary antibody concentration that is too high is a very frequent cause of background [12].
FAQ: I have already blocked with serum, but background remains high. What else can I do? Serum blocking may not be sufficient to address all interactions. Consider these advanced steps [10] [12]:
- Block Hydrophobic Interactions: Add a gentle detergent like Tween-20 (0.05%) to your antibody diluent and wash buffers to minimize hydrophobic binding.
- Block Endogenous Biotin: If using a biotin-based detection system, use a commercial avidin/biotin blocking kit, especially for tissues like liver and kidney with high endogenous biotin [11].
- Increase Ionic Strength: Add NaCl to your antibody diluent to a final concentration of 0.15 M to 0.6 M to reduce ionic interactions. The optimal concentration must be determined empirically [10].
- Re-evaluate Blocking Necessity: Some studies suggest that for routinely fixed paraffin-embedded samples, traditional protein blocking steps may be unnecessary, as fixation renders endogenous Fc receptors inactive [14]. Testing your protocol without a blocking step could provide insight.
FAQ: How can I confirm if the secondary antibody is causing the background? Run a control slide where you omit the primary antibody. If the high background persists after applying only the secondary antibody and the detection system, then the secondary antibody is the source of the problem [11]. If this occurs, try reducing the concentration of the secondary antibody or switching to a different one [10] [15].
Quantitative Data & Experimental Comparisons
Table 1: Summary of Key Blocking Reagents and Their Applications
| Reagent | Primary Function | Example Usage/Concentration | Key Consideration |
|---|---|---|---|
| Normal Serum [10] | Blocking; theorized to block Fc receptors. | 2-10% (v/v) in diluent. | Source should be same as secondary antibody species; necessity debated [14]. |
| BSA / Non-Fat Dry Milk [15] | Blocking; thought to block hydrophobic/ionic interactions. | 3-5% (w/v) in buffer. | May contain bovine IgG that can cross-react with some secondary antibodies [14]. |
| Detergents (Tween-20) [12] | Reduce hydrophobic interactions. | 0.05% - 0.1% (v/v) in wash/block buffer. | Reduces surface tension, minimizes non-specific sticking. |
| H₂O₂ (3%) [10] [11] | Quench endogenous peroxidases. | 10-15 min incubation before primary antibody. | Critical for HRP-based detection systems. |
| Avidin/Biotin Block [10] [11] | Block endogenous biotin. | Commercial kit, used according to manufacturer instructions. | Essential for biotin-rich tissues when using biotin-streptavidin detection. |
| NaCl (High Salt) [10] | Reduce ionic interactions. | 0.15 M - 0.6 M in antibody diluent. | Concentration must be optimized empirically. |
Table 2: Systematic Troubleshooting Guide for Spotty/Uneven Background
| Problem Indicator | Potential Root Cause | Recommended Corrective Experiment |
|---|---|---|
| High, diffuse background across entire tissue | Primary antibody concentration too high [12]. | Perform a primary antibody titration; test a series of dilutions. |
| Spotty, uneven background | Inadequate deparaffinization [11]; Tissue drying [12]. | Repeat with new sections and fresh xylene; ensure slides remain wet. |
| Background in negative control (no primary) | Secondary antibody cross-reactivity or over-concentration [10] [15]. | Omit primary control; titrate secondary antibody to find optimal concentration. |
| High background in biotin-rich tissues | Endogenous biotin not blocked [10] [11]. | Incorporate an avidin/biotin blocking step prior to primary antibody incubation. |
| Persistent background after standard blocking | Hydrophobic/ionic interactions dominating [13] [12]. | Add Tween-20 (0.05%) to buffers and/or increase ionic strength with NaCl [10]. |
Detailed Experimental Protocols
Protocol 1: Titrating Primary Antibody to Reduce Background This protocol is used to identify the optimal concentration of primary antibody that provides a strong specific signal with minimal background [12].
- Prepare serial dilutions of your primary antibody. Start with the manufacturer's recommended dilution and prepare several dilutions above and below it (e.g., 1:50, 1:100, 1:200, 1:500).
- Apply each dilution to adjacent tissue sections from the same block, ensuring all other steps in the IHC protocol are identical.
- Process all slides simultaneously using the same detection system and development time.
- Evaluate under a microscope. The optimal dilution yields strong, specific staining in expected locations with a clean, low-background counterstain.
Protocol 2: Testing for Secondary Antibody Specificity This control experiment confirms whether the secondary antibody is contributing to background staining [11].
- For every experiment, include a negative control slide.
- On this control slide, omit the primary antibody. Instead, apply only the antibody diluent (the buffer the primary is normally diluted in).
- Continue with the rest of the protocol as normal, including incubation with the secondary antibody and the detection system.
- Interpretation: Any staining observed on this control slide is due to non-specific binding of the secondary antibody or other detection reagents. If significant background is present, further optimization of the secondary antibody concentration or blocking steps is required.
Protocol 3: Comprehensive Blocking for Hydrophobic and Ionic Interactions This protocol combines multiple strategies to address stubborn background [10] [12].
- Deparaffinize and rehydrate tissue sections using fresh xylene and graded ethanols.
- Perform antigen retrieval as required for your target.
- Block endogenous peroxidases with 3% H₂O₂ for 10-15 minutes.
- Prepare a high-stringency blocking/diluent buffer containing:
- 1X PBS or TBS
- 5% normal serum from the secondary antibody host species
- 0.05% - 0.1% Tween-20
- (Optional) 0.15 M - 0.6 M NaCl
- Block the tissue with this buffer for 30-60 minutes at room temperature.
- Dilute the primary and secondary antibodies in the same high-stringency buffer.
- Perform all washes with buffer containing 0.05% - 0.1% Tween-20.
Visualizations & Workflows
Diagram 1: Background Staining Troubleshooting
Diagram 2: Effects of Nonspecific Binding
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Mitigating Non-Specific Background
| Reagent / Material | Function / Rationale | Specific Examples / Notes |
|---|---|---|
| Tween-20 | Non-ionic detergent that reduces hydrophobic interactions by lowering surface tension in buffers [12]. | Add at 0.05% - 0.1% to blocking, antibody dilution, and wash buffers. |
| NaCl (Sodium Chloride) | High salt concentration shields electrostatic/ionic interactions between charged residues on antibodies and non-target tissue components [10]. | Use at 0.15 M - 0.6 M in antibody diluent; requires empirical optimization. |
| Polymer-Based Detection Kits | Replaces avidin-biotin (ABC) systems to avoid background from endogenous biotin; often provides higher sensitivity [11]. | SignalStain Boost IHC Detection Reagents; reduces background in biotin-rich tissues. |
| Azide-Free Buffers | Sodium azide is an inhibitor of Horseradish Peroxidase (HRP); its absence is critical for maintaining enzyme activity in HRP-based detection [10]. | Ensure no azide is present in buffers used with HRP-conjugated antibodies. |
| Advanced Verification Antibodies | Antibodies subjected to additional specificity tests to ensure high confidence and lower propensity for non-specific binding [10]. | Look for antibodies with "Advanced Verification" badges; check product data galleries. |
| Zwitterionic Buffers/Polymers | Provides strong hydration layers and charge balance, resisting non-specific protein adsorption via hydration lubrication mechanism [16]. | Used in surface coatings and diluents for antifouling properties. |
How Drying Artifacts and Contamination Cause Patchy Staining
Patchy, uneven, or spotty background staining is a common yet frustrating problem in histological and immunohistochemical (IHC) techniques. This artifact can obscure critical cellular details, compromise experimental data, and lead to misinterpretation of biological structures. The root causes often trace back to two main culprits: drying artifacts and various forms of contamination. Understanding how these factors interfere with staining uniformity is the first step toward achieving consistent, publication-quality results. This guide provides a systematic approach to troubleshooting these issues, ensuring that researchers can identify and rectify the underlying problems in their staining workflows.
Troubleshooting Guide: Common Causes and Solutions
The following table summarizes the frequent causes of patchy staining related to drying and contamination, along with their recommended solutions.
| Cause of Artifact | Specific Problem | Recommended Solution | Supporting Controls/Evidence |
|---|---|---|---|
| Drying Artifacts | Partial drying of sections during reagent application [17] | Process slides in smaller batches to ensure reagents fully cover the section without drying [17]. | Use a positive control tissue processed in the same way [17]. |
| Incomplete Processing | Incomplete removal of paraffin (dewaxing) [17] | Use fresh xylene or other dewaxing reagents for deparaffinization [18] [17]. | |
| Fixation Issues | Improper or uneven fixation, particularly in immersion-fixed specimens [17] | Ensure tissue blocks are of appropriate size/thickness and are fixed for an optimal duration [17]. | |
| Contamination | Air bubbles trapped during steps causing uneven reagent dispersion [17] | Carefully roll out or remove bubbles when assembling steps like transfer sandwiches; ensure reagents evenly cover the sample [17]. | Use a negative control (e.g., non-immune IgG) to check for nonspecific binding [17]. |
| Carryover Contamination | Water carryover into alcohols or xylenes, leading to a pink haze or uneven eosin staining [2] | Change reagents regularly; ensure slides are adequately drained between steps [2]. | |
| Endogenous Activity | Endogenous peroxidase or biotin activity, especially in tissues like kidney and liver [18] | For HRP-based systems: quench with 3% H2O2 for 10 min. For biotin systems: use a biotin block or switch to a polymer-based detection system [18]. | Include a control slide without the primary antibody to check for secondary antibody background [18]. |
| Adhesive Residue | Use of protein-based adhesives in water baths causing background staining [2] | Switch to charged slides and minimize the use of water bath adhesives [2]. |
Experimental Protocols for Diagnosis and Resolution
Protocol 1: Validating Staining Specificity with Controls
Purpose: To determine whether patchy staining is due to a specific antibody-antigen reaction or non-specific background using positive and negative controls [17].
Positive Control Selection and Use:
- Select a control tissue (e.g., tonsil) known to express a moderate to high level of your target antigen [17].
- It is critical that the positive control is processed (fixed, embedded, and sectioned) in the exact same way as your experimental samples [17].
- Run the positive control in parallel with your experimental stain using the identical protocol.
- Interpretation: If the positive control stains correctly but the experimental sample does not, the issue is likely specific to the experimental sample (e.g., antigen expression level, unique fixation). If the positive control also shows patchy or absent staining, the problem lies within the staining protocol or reagents [17].
Negative Control Selection and Use:
- Substitute the primary antibody with a non-immune IgG from the same species, isotype, and concentration [18] [17].
- Alternatively, use an irrelevant antibody that does not recognize any antigen in your experimental specimen (e.g., an antibody against keratin for CNS tissue) [17].
- Interpretation: The presence of staining in this negative control indicates non-specific binding of the detection system or the primary antibody isotype. An absence of staining confirms the specificity of your experimental results [17].
Protocol 2: Optimizing Antigen Retrieval for Uniformity
Purpose: To resolve patchy staining caused by inconsistent or inadequate antigen retrieval, a common source of variability [18] [17].
- Method Selection: For IHC, heat-induced epitope retrieval (HIER) using a microwave oven or pressure cooker is generally preferred over a water bath, as it provides more uniform and robust signal retrieval [18].
- Buffer Preparation: Always prepare a fresh 1X antigen retrieval solution daily. Use the buffer specified on the antibody's datasheet (e.g., citrate or EDTA-based) [18].
- Standardization:
- Carefully control and document the pH, temperature, and duration of retrieval [17].
- Ensure the retrieval container is not overloaded, allowing for even heat distribution.
- After retrieval, allow the slides to cool naturally to room temperature before proceeding to the next step.
Protocol 3: Ensuring Complete and Uniform Deparaffinization
Purpose: To eliminate spotty, uneven background caused by residual paraffin, which blocks reagent access [18] [17].
- Reagent Freshness: Use fresh xylene (or xylene substitute) for dewaxing. Do not use reagents that have been used for an excessive number of slides [18] [17].
- Protocol:
Visualizing the Troubleshooting Workflow
The following diagram outlines a logical, step-by-step process for diagnosing and resolving patchy staining issues.
The Scientist's Toolkit: Essential Research Reagent Solutions
A reliable staining process depends on high-quality, fresh reagents. The following table details key solutions and their functions in preventing patchy staining.
| Reagent / Material | Primary Function | Role in Preventing Patchy Staining |
|---|---|---|
| Fresh Xylene / Clearing Agent | To completely remove paraffin wax from tissue sections [18] [19]. | Prevents spotty, uneven background caused by residual wax that blocks dye and reagent access [18] [17]. |
| Appropriate Antibody Diluent | To dilute the primary antibody to the correct concentration while maintaining stability [18]. | Using the manufacturer-recommended diluent prevents non-specific binding and aggregation, which can cause high, uneven background [18]. |
| SignalStain Boost IHC Detection Reagent (HRP, #8114) | A polymer-based detection system for enhanced sensitivity [18]. | More sensitive than avidin-biotin systems; avoids background from endogenous biotin in tissues like liver and kidney [18]. |
| Buffered Neutral Formalin | A standardized fixative for tissue preservation [20]. | Prevents the formation of acid-formalin pigment (brown-black granules) and searing of tissue edges, which can create artifacts [20] [2]. |
| Charged Slides | Microscopy slides with a positive surface charge [2]. | Provide consistent tissue adhesion, minimizing the need for protein adhesives that can cause background staining [2]. |
| 3% Hydrogen Peroxide (H₂O₂) | A quenching agent for endogenous enzymes [18]. | Eliminates background signal from endogenous peroxidase activity when using HRP-based detection systems [18]. |
| Blocking Serum (e.g., Normal Goat Serum #5425) | A protein solution used to occupy non-specific binding sites [18]. | Reduces high background by preventing non-specific binding of the primary or secondary antibody to the tissue [18]. |
| Fresh Ethanol/Dehydrating Alcohols | To remove water from stained sections before clearing with xylene [19]. | Prevents water carryover into clearing agents, which can cause a pink haze and uneven staining, particularly of eosin [2]. |
Frequently Asked Questions (FAQs)
Q1: My positive control stains perfectly, but my experimental tissue is patchy. What does this mean? This typically indicates that your staining protocol and reagents are functioning correctly. The issue is specific to the experimental tissue sample itself. The most likely causes are improper or uneven fixation, or the tissue may have partially dried out during dissection or processing before fixation [17].
Q2: I see a pink haze over my entire slide. What is the cause, and how can I fix it? A pink haze is often a sign of water contamination in your xylene or xylene substitute, which causes the eosin to seep [2]. To fix this, replace all your dehydration alcohols and clearing xylenes with fresh reagents. Ensure slides are adequately drained between steps to minimize carryover [2].
Q3: How can I definitively tell if my background staining is non-specific? The most reliable method is to run a rigorous negative control. Replace your primary antibody with a non-immune IgG from the same species and at the same concentration. If this control slide shows the same patchy background pattern, then the signal is non-specific and you need to optimize your blocking, antibody concentration, or washing steps [18] [17].
Q4: What is the simplest first step if my staining suddenly becomes patchy? Before changing complex protocol steps, check the simplest factors first. Ensure all your core reagents—especially dewaxing agents, alcohols, and buffers—are fresh and have not expired [17]. Contamination or degradation of these basic solutions is a very common cause of new staining problems.
Assessing the Consequences for Data Interpretation and Reproducibility
Frequently Asked Questions (FAQs)
Q: My negative control shows uneven, spotty background staining. What does this mean and what should I investigate first? A: Spotty staining in your negative control strongly indicates a non-specific staining or a slide preparation issue, not a true positive signal. Your first step should be to check your slide preparation, particularly the deparaffinization step. Inadequate deparaffinization is a known cause of spotty, uneven background staining [21]. Repeat the experiment with new tissue sections and fresh xylene to resolve this [21].
Q: I am using a polymer-based detection system, but my slides still have high, uneven background. What could be the cause? A: High background with a polymer-based system often points to an issue with antibody dilution or inadequate washing. First, confirm you are using the antibody diluent recommended on the product datasheet, as the wrong diluent can cause high background [21]. Second, ensure you are performing adequate washing by washing slides three times for five minutes with an appropriate buffer like TBST after both primary and secondary antibody incubations [21].
Q: What are the critical positive and negative controls I should run to validate my staining results? A: You should use appropriate controls with every run. This includes a known positive tissue control to confirm the antibody and procedure are working, and a negative control using a non-specific probe to identify non-specific binding [3]. For phospho-specific antibodies or those against rarely expressed proteins, employing a high-expressing positive control, such as paraffin-embedded cell pellets, is essential [21].
Q: How can the antigen retrieval method affect my staining results and reproducibility? A: The antigen retrieval method is critical for exposing the target antigen. Using a suboptimal method or inconsistent conditions can lead to weak, negative, or variable staining. A microwave oven is generally recommended for antigen retrieval over a water bath, as it provides superior results for many targets [21]. For maximum reproducibility, always follow the product-specific protocol, which includes the optimal antigen retrieval buffer and method, and prepare fresh 1X retrieval solutions daily [21].
Q: Why is my staining weak or negative even though I confirmed my antibody is valid for IHC? A: Weak or negative staining can result from several factors. First, ensure your slides are freshly cut, as signal can be lost over time in storage [21]. Second, verify your antigen retrieval technique and buffer. Finally, confirm you are using a sensitive, polymer-based detection reagent (not a standard avidin/biotin system) and that it has not expired [21].
Troubleshooting Guide: Spotty & Uneven Background Staining
This guide helps you diagnose and fix the specific problem of spotty or uneven background staining.
Table: Troubleshooting Spotty and Uneven Background Staining
| Problem Area | Possible Cause | Recommended Solution | Consequence for Data Interpretation |
|---|---|---|---|
| Slide Preparation | Inadequate deparaffinization [21] | Repeat experiment with new tissue sections and fresh xylene [21]. | Spotty background can obscure true signal and be misinterpreted as specific staining, leading to false positives. |
| Section Adhesion | Use of protein-based adhesives on charged slides [3] | Avoid protein-based section adhesives (glue, starch, gelatin) in the flotation bath for charged slides [3]. | Pooling of reagents beneath lifting sections creates uneven staining, compromising reproducibility and quantitative analysis. |
| Detection System | Use of biotin-based system on tissues with high endogenous biotin (e.g., kidney, liver) [21] | Switch to a polymer-based detection system or perform a biotin block [21]. | High, non-specific background can mask a true weak signal (false negative) or be mistaken for a true positive (false positive). |
| Antibody Incubation | Evaporation of probe or reagents during long incubation times [3] | Use good quality equipment to prevent reagents from drying out, especially at the edges of the section [3]. | Drying causes heavy, non-specific staining at section edges, rendering the entire slide uninterpretable and wasting resources. |
| Washing Steps | Non-standardized washing techniques between users or runs [3] | Implement standardized washing steps (duration, volume, and form of agitation) for all users [3]. | Variable staining intensity between experiments destroys reproducibility and makes it impossible to compare results across studies. |
Experimental Protocol: Resolving Spotty Background from Inadequate Deparaffinization
Objective: To obtain a clean, uniform background in IHC staining by ensuring complete removal of paraffin from tissue sections.
Principle: Paraffin wax, used for embedding tissues, is immiscible with aqueous staining reagents. Incomplete removal creates a physical barrier, leading to spotty staining and high, uneven background.
Materials:
- Freshly cut formalin-fixed, paraffin-embedded (FFPE) tissue sections on charged slides [21].
- Fresh xylene [21].
- Ethanol series (100%, 95%, 70%).
- Deionized water.
- Phosphate-buffered saline (PBS) or TBST buffer [21].
Methodology:
- Deparaffinization: Immerse slides in a first bath of fresh xylene for 5-10 minutes.
- Clear Residual Wax: Transfer slides to a second bath of fresh xylene for another 5-10 minutes.
- Rehydration: Hydrate the tissue sections through a series of graded ethanols:
- 100% Ethanol: 5 minutes
- 100% Ethanol: 5 minutes
- 95% Ethanol: 5 minutes
- 70% Ethanol: 5 minutes
- Rinse: Rinse slides gently in deionized water.
- Buffer Rinse: Transfer slides to PBS or TBST buffer until ready to proceed with antigen retrieval and immunostaining.
- Antigen Retrieval: Perform heat-induced epitope retrieval using a microwave oven and the appropriate buffer as per your antibody's datasheet [21].
Experimental Workflow: Systematic IHC Staining
This diagram outlines the core workflow for a robust IHC experiment, highlighting critical steps that impact background staining and reproducibility.
Research Reagent Solutions
Table: Essential Reagents for Troubleshooting IHC Background
| Reagent / Solution | Function | Troubleshooting Application |
|---|---|---|
| Fresh Xylene [21] | Organic solvent for complete removal of paraffin wax from tissue sections. | Solving spotty, uneven background caused by inadequate deparaffinization. |
| SignalStain Antibody Diluent [21] | Optimized solution for diluting primary antibodies. | Prevents high background; superior to generic diluents like TBST/5% NGS for many antibodies. |
| SignalStain Boost IHC Detection Reagent (HRP, Polymer) [21] | A sensitive, polymer-based detection system that does not rely on avidin-biotin chemistry. | Reduces background in tissues with high endogenous biotin (e.g., liver, kidney); enhances sensitivity. |
| TBST Buffer with 5% Normal Goat Serum [21] | Washing and blocking solution. | Used for adequate blocking (30 min) and rigorous washing (3x5 min) to ensure low background. |
| 3% H₂O₂ in RODI Water [21] | Quenching solution for endogenous peroxidase activity. | Reduces high background when using HRP-based detection systems. |
Building a Robust IHC Protocol: Prevention Through Best Practices
Troubleshooting Guide: Resolving Spotty and Uneven Background Staining
This guide addresses the common causes of and solutions for spotty, uneven background staining in immunohistochemistry (IHC) and immunofluorescence (IF) experiments, a critical challenge in histological research.
Table 1: Troubleshooting Spotty and Uneven Background Staining
| Problem Manifestation | Potential Cause | Recommended Solution | Key References |
|---|---|---|---|
| Spotty, uneven staining across the section | Incomplete deparaffinization [22] [23] | Use fresh xylene or other dewaxing solvents for complete paraffin removal. [22] | [22] [23] |
| Heavy, non-specific staining at section edges; uneven staining | Evaporation of reagents during incubation, causing drying of the section. [3] | Use a good quality, sealed humidification chamber during all incubation steps to prevent drying. [3] | [3] |
| Variable background staining between runs; uneven staining | Inconsistent washing techniques by different operators. [3] | Standardize washing steps (duration, volume, agitation) for all users. [3] | [3] |
| Pooling of reagents beneath lifting sections; uneven staining | Poor section adhesion, often from using protein-based adhesives on charged slides. [3] | Use charged slides and avoid protein-based section adhesives (glue, starch, gelatin) in the flotation bath. [3] | [3] |
| High general background | Antibody concentration is too high. [24] [25] | Titrate both primary and secondary antibodies to find the optimal concentration that minimizes background. [24] [25] | [24] [25] |
| High background in tissues with endogenous biotin (e.g., liver, kidney) | Non-specific binding from a biotin-based detection system. [22] [25] | Use a polymer-based detection system instead. [22] Alternatively, perform an avidin/biotin block after the normal blocking procedure. [25] | [22] [25] |
| High background in species-on-species staining (e.g., mouse antibody on mouse tissue) | Secondary antibody binding to endogenous immunoglobulins in the tissue. [22] [25] | Use a species-specific blocking reagent, such as a Mouse-on-Mouse (M.O.M.) kit. [25] Alternatively, use a polymer-based system with anti-mouse reagents that are specifically validated for mouse tissue. [22] | [22] [25] |
Frequently Asked Questions (FAQs)
How does fixation lead to spotty background staining?
Uneven or suboptimal fixation is a primary cause. Under-fixation, often due to a large tissue-to-fixative ratio or short fixation time, fails to preserve the tissue uniformly, typically leaving the center of the specimen under-fixed. This can result in aberrant, uneven staining and high background in the poorly fixed areas [25]. Over-fixation can mask antigen targets and increase tissue autofluorescence, which contributes to background noise [25] [23]. Consistent fixation conditions (type, pH, time, temperature) are crucial for reproducible results [3].
What controls can help me identify the source of background staining?
Implementing the correct controls is essential for systematic troubleshooting [3] [25]:
- Secondary Antibody Deletion Control: Omit the primary antibody. Significant staining indicates non-specific binding from the secondary antibody or detection system [25].
- Detection System Deletion Control: Omit both primary and secondary antibodies. Staining here points to non-specific binding of the detection reagents, such as binding to endogenous biotin [25].
- Endogenous Enzyme Control: Incubate the tissue with only the chromogen/substrate. Development of color indicates activity from endogenous peroxidases or phosphatases that needs to be blocked [25].
Besides fixation and antibodies, what else can cause high, uniform background?
Other common sources include:
- Endogenous Enzymes: Tissues like liver, spleen, and kidney have high levels of endogenous peroxidases. Block with 3% H~2~O~2~ for 10 minutes prior to primary antibody incubation [22] [23].
- Autofluorescence: Tissue components (e.g., collagen, elastin, lipofuscins) and aldehyde fixatives can autofluoresce [25] [26]. Use autofluorescence quenchers like TrueVIEW or Sudan Black B [25] [26], or switch to a far-red fluorescent dye where autofluorescence is lower [26].
- Insufficient Blocking: Ensure adequate blocking with 5% normal serum from the host species of the secondary antibody or other commercial blocking agents for 30 minutes to prevent non-specific antibody binding [22] [23].
Experimental Protocols for Optimization
Protocol 1: Fixation and Antigen Retrieval Optimization
This protocol helps determine the optimal sample preparation for a new antibody or tissue type [27].
Table 2: Fixation and Unmasking Optimization Scheme
| Sample | Fixation Method | Antigen Retrieval (Unmasking) | Staining | Control Purpose |
|---|---|---|---|---|
| #1 | Organic Solvent (e.g., -20°C Acetone) | None | Normal | Positive control for organic solvent |
| #2 | Organic Solvent | None | No Primary Antibody | Negative control for organic solvent |
| #3 | Cross-linking (e.g., 4% PFA) | None | Normal | Positive control for cross-linking |
| #4 | Cross-linking | None | No Primary Antibody | Negative control for cross-linking |
| #5 | Cross-linking | Heat-Induced (Tris-EDTA, pH 9) | Normal | Tests cross-linking + HIER |
| #6 | Cross-linking | Heat-Induced (Tris-EDTA, pH 9) | No Primary Antibody | Negative for cross-linking + HIER |
| #7 | Cross-linking | Enzymatic (e.g., Proteinase K) | Normal | Tests cross-linking + PIER |
| #8 | Cross-linking | Enzymatic (e.g., Proteinase K) | No Primary Antibody | Negative for cross-linking + PIER |
Procedure:
- Tissue Preparation: Use a standardized, relevant tissue sample for troubleshooting [27].
- Fixation: Follow the methods in Table 2. For cross-linking, use 3-4% paraformaldehyde for 5-10 minutes (cells) or up to 30 minutes (tissue blocks). For organic solvents, use cold acetone or methanol for 5-10 minutes [27].
- Antigen Retrieval:
- Heat-Induced Epitope Retrieval (HIER): Submerge slides in 10 mM Tris Base, 1 mM EDTA, 0.05% Tween 20, pH 9.0 for 10-40 minutes at 95-100°C. Let cool for 20 minutes before proceeding [27]. A microwave oven is often preferred over a water bath [22].
- Proteolytic-Induced Epitope Retrieval (PIER): Submerge slides in a 20 µg/mL solution of Proteinase K in TE buffer, pH 8.0 for 10-20 minutes at 37°C [27].
- Staining and Analysis: Complete your standard IHC/IF protocol. Analyze results for the combination that provides the strongest specific signal with the lowest background and best tissue morphology [27].
Protocol 2: Antibody Titration for Optimal Signal-to-Noise
This protocol finds the antibody concentration that maximizes specific signal while minimizing background [24] [25].
- Prepare Slides: Prepare multiple sections of your target tissue with optimal fixation and antigen retrieval.
- Create Dilutions: Prepare a dilution series of your primary antibody (e.g., 0.1, 0.5, 1, 2, 5 µg/mL) in the recommended diluent.
- Apply Antibodies: Apply each dilution to a separate section and incubate according to your standard protocol (often overnight at 4°C).
- Complete Staining: Complete the rest of your IHC/IF protocol with all other conditions held constant.
- Evaluate: Under the microscope, identify the dilution that yields strong, specific staining with the cleanest background. This is your optimal concentration.
Visual Workflow for Troubleshooting
The following diagram outlines a logical decision-making process for diagnosing the root causes of spotty and uneven background staining.
Troubleshooting Spotty and Uneven Staining
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Preventing Background Staining
| Reagent / Solution | Function | Example Use Case |
|---|---|---|
| Charged Slides | Provides a surface that promotes strong section adhesion, preventing lifting and reagent pooling. [3] | Essential for all ISH and recommended for IHC/IF to ensure flat, evenly stained sections. [3] |
| SignalStain Antibody Diluent | An optimized buffer for diluting primary antibodies to enhance specific binding and reduce non-specific background. [22] | Used as the recommended diluent for many antibodies to achieve superior signal-to-noise compared to TBST/NGS. [22] |
| Polymer-Based Detection Reagents | Highly sensitive detection systems that avoid the use of biotin, eliminating background from endogenous biotin. [22] | Critical for staining tissues with high endogenous biotin (e.g., liver, kidney) and for mouse-on-mouse staining. [22] |
| M.O.M. (Mouse on Mouse) Blocking Reagent | Blocks endogenous immunoglobulins in mouse tissue to prevent non-specific binding of mouse primary and secondary antibodies. [25] | Essential when using a mouse primary antibody on mouse tissue to reduce high background. [25] |
| TrueVIEW Autofluorescence Quencher | A chemical solution that reduces non-specific fluorescence from aldehyde fixation and intrinsic tissue elements. [25] | Applied after staining but before mounting to quench autofluorescence, improving signal clarity in IF. [25] |
| BLOXALL Endogenous Blocking Solution | Blocks endogenous peroxidase and alkaline phosphatase activity simultaneously. [25] | Used before detection to prevent false-positive signals from endogenous enzymes in tissues like liver and spleen. [25] |
FAQs on Antigen Retrieval for Troubleshooting Spotty, Uneven Background Staining
What is the primary cause of spotty, uneven background staining, and how is it related to antigen retrieval?
Spotty, uneven background staining often stems from inadequate deparaffinization of tissue sections prior to immunohistochemistry (IHC) [28]. If paraffin is not completely removed, it can trap reagents and chromogen, leading to uneven, distracting background patterns under the microscope [29]. Furthermore, inconsistent or suboptimal antigen retrieval can exacerbate this issue by causing uneven epitope exposure across the tissue section.
How does the choice of buffer pH affect heat-induced epitope retrieval (HIER) efficiency?
The efficiency of HIER is highly dependent on the pH of the retrieval buffer, which should be selected based on the isoelectric point (pI) of the target antigen [30]. A fundamental principle is that antigens with an acidic pI generally require a basic pH buffer for efficient retrieval, while antigens with an alkaline pI require an acidic pH buffer [30]. This is because the electrostatic charge of the antigens significantly contributes to the HIER process, helping to restore antibody binding capability.
What are the immediate steps to take when spotty background appears?
When spotty background staining occurs, the first critical step is to repeat the experiment with new tissue sections and use fresh xylene or xylene substitutes to ensure complete deparaffinization [28] [29]. You should also verify that your deparaffinization and rehydration reagents are not saturated and have been changed regularly based on usage, as depleted reagents lose their potency [29].
Optimizing Antigen Retrieval Buffer Selection
Selecting the correct antigen retrieval buffer is a critical parameter for successful IHC, as it directly influences the unmasking of epitopes cross-linked during formalin fixation.
Common Antigen Retrieval Buffers and Their Applications
The table below summarizes the three most commonly used buffers for HIER.
| Buffer Type | Typical Composition | Optimal pH Range | Recommended For |
|---|---|---|---|
| Sodium Citrate | 10 mM Sodium citrate, 0.05% Tween 20 [31] | 6.0 [31] [29] | A widely used general-purpose buffer [31]. |
| Tris-EDTA | 10 mM Tris base, 1 mM EDTA, 0.05% Tween 20 [31] | 8.0 - 9.0 [31] [29] | A high-pH buffer often used for more challenging targets [31] [32]. |
| EDTA | 1 mM EDTA [31] | 8.0 [31] | Another high-pH buffer alternative [31]. |
A Strategic Framework for Buffer Optimization
In the absence of a manufacturer's recommendation, use this strategic approach to select a buffer:
- Start with a Neutral Buffer: Begin optimization using a neutral buffer like PBS (pH 7.2–7.6) [32].
- Systematic pH Testing: If signal intensity is weak or absent, create a testing matrix to evaluate different combinations of buffer pH and incubation times [32] [33]. Compare the results against a control slide that did not undergo HIER [33].
- Apply the pI Principle: For targeted optimization, use the relationship between the antigen's isoelectric point (pI) and buffer pH: select a basic buffer for acidic pI antigens and an acidic buffer for basic pI antigens [30].
Heat-Induced Epitope Retrieval (HIER) Methods and Protocols
HIER uses heat to break the methylene cross-links formed during formalin fixation, thereby restoring the antigenicity of the tissue [31]. The following are standard HIER methods.
Pressure Cooker Method
The pressure cooker method is highly effective due to the high temperatures achievable (around 120°C), which allow for shorter retrieval times [31] [29].
Detailed Protocol:
- Add the appropriate antigen retrieval buffer to the pressure cooker and begin heating on a hot plate [31].
- While the buffer is heating, deparaffinize and rehydrate the tissue sections [31].
- Once the buffer is boiling, carefully transfer the slides into it [31].
- Secure the lid and allow the cooker to reach full pressure. Once reached, start timing for 3 minutes [31].
- After 3 minutes, turn off the heat, place the cooker in a sink, and run cold water over it to release pressure and cool the slides [31].
- Once depressurized, open the lid and run cold water over the slides for 10 minutes to cool them completely and allow the antigenic sites to re-form [31].
- Proceed with the rest of your IHC staining protocol [31].
Microwave Method
While a scientific microwave is preferred, a domestic microwave can be used with caution, though uneven heating ("hot and cold spots") can be a problem [31].
Detailed Protocol:
- Deparaffinize and rehydrate the tissue sections [31].
- Place the slides in a microwave-safe vessel filled with enough antigen retrieval buffer to cover them by several centimeters [31].
- Place the vessel in the microwave. If using a domestic microwave, heat on full power until the solution boils, then continue boiling for 20 minutes [31]. For a scientific microwave, program it to maintain 98°C for 20 minutes [31].
- Critical: Monitor the buffer level closely to prevent the slides from drying out, adding more buffer if necessary [31].
- After 20 minutes, remove the vessel and run cold tap water into it for 10 minutes to cool the slides [31].
- Continue with the IHC staining protocol [31].
Steamer Method
This method maintains a temperature of 95–100°C without the vigorous boiling of the microwave, which can be gentler on tissues [31].
Detailed Protocol:
- Deparaffinize and rehydrate the tissue sections and preheat a vegetable steamer [31].
- Separately, pre-heat the antigen retrieval buffer to boiling in a flask [31].
- Place a container with a slide rack into the steamer. Carefully add the hot buffer to the container, followed by the rack of slides [31].
- Close the steamer lid and maintain the temperature for 20 minutes [31].
- After 20 minutes, remove the vessel and run cold tap water into it for 10 minutes [31].
- Proceed with the IHC staining [31].
Decision Workflow for Antigen Retrieval Optimization
The following diagram illustrates a logical workflow for diagnosing and resolving spotty background staining through antigen retrieval optimization.
Research Reagent Solutions for HIER
This table details key reagents and materials essential for performing and optimizing HIER protocols.
| Reagent / Material | Function / Purpose | Examples & Notes |
|---|---|---|
| Retrieval Buffers | Breaks formalin-induced cross-links to unmask epitopes; pH choice is critical for success [31] [30]. | Sodium Citrate (pH 6.0), Tris-EDTA (pH 9.0), EDTA (pH 8.0) [31]. Universal kits are also available [31]. |
| HIER Equipment | Applies consistent, controlled heat to tissue sections for epitope retrieval. | Pressure Cooker (short time, ~120°C) [31] [29], Scientific Microwave (consistent 98°C) [31], Vegetable Steamer (gentle, 95-100°C) [31]. |
| Blocking Solutions | Reduces non-specific binding of antibodies to tissue, minimizing background [10] [34]. | Normal serum (from secondary antibody species), BSA, or commercial protein blocks [10] [34] [28]. |
| Endogenous Enzyme Blockers | Quenches activity of native tissue enzymes that can react with chromogen, causing background [10] [34]. | 3% H₂O₂ (for peroxidases) [10] [28], Levamisole (for alkaline phosphatase) [10] [34], BLOXALL (blocks both) [34]. |
| Detection System | Amplifies the primary antibody signal for visualization. | Polymer-based systems (high sensitivity, low background) are often preferred over avidin-biotin systems, which can bind endogenous biotin [34] [28]. |
Effective Blocking Strategies for Peroxidases, Biotin, and Non-Specific Sites
A technical support guide to diagnosing and eliminating the common culprits of spotty, uneven background staining in your experiments.
FAQ: Addressing Common Blocking Challenges
This section answers frequently asked questions to help you troubleshoot the root causes of spotty and uneven background staining.
1. How do I know which endogenous component is causing my background staining?
Running the appropriate negative control tissue is the most reliable way to diagnose the problem. A negative tissue control uses a sample known to lack your target antigen. If you see staining in this control, it indicates background staining that requires blocking. Furthermore, you can test for specific interferents:
- For endogenous peroxidase: Incubate a deparaffinized and rehydrated tissue section with only the DAB substrate. Any brown precipitate indicates endogenous peroxidase activity [35].
- For endogenous biotin: Incubate your tissue section with streptavidin-HRP followed by DAB. A brown deposit signals the presence of problematic endogenous biotin [35].
2. My background is still high after blocking. What should I check?
If you have confirmed your blocking steps are correct, consider these common pitfalls:
- Primary antibody concentration is too high: This is a leading cause of non-specific binding. Perform a titration experiment to find the optimal dilution that maximizes signal and minimizes background [12].
- Insufficient washing: Inadequate washing after antibody incubations can leave unbound reagents that contribute to a high, even background. Ensure you are washing slides 3 times for 5 minutes with an appropriate buffer like TBST [36].
- Tissue sections dried out: Allowing tissue sections to dry at any point during the staining procedure causes irreversible, non-specific antibody binding and can create edge artifacts. Always keep sections covered with liquid and use a humidity chamber for long incubations [12].
3. I am using a biotin-based detection system. Are there alternatives to avoid endogenous biotin blocking?
Yes. A highly effective strategy is to switch to a polymer-based detection system. These systems do not rely on the avidin-biotin complex and are therefore unaffected by endogenous biotin, eliminating the need for a separate biotin-blocking step. They also offer enhanced sensitivity [36].
Troubleshooting Guide: Blocking for a Clean Background
Systematically address spotty and uneven staining by consulting the following guide.
| Problem Observed | Potential Cause | Recommended Solution |
|---|---|---|
| Spotty, uneven background | Inadequate deparaffinization [36] [12] | Repeat the experiment with new tissue sections and fresh xylene. |
| Inconsistent reagent coverage during incubation [12] | Use a humidified chamber and ensure liquid fully covers the tissue section. | |
| High general background | Endogenous peroxidase activity (in liver, kidney, spleen) [37] [38] [35] | Quench with 3% H2O2 (in methanol or water) for 10-15 minutes before primary antibody incubation [37] [36] [35]. |
| Endogenous biotin activity (in liver, kidney, brain, lung) [37] [38] [35] | Use an avidin/biotin blocking kit or switch to a polymer-based detection system [37] [36] [35]. | |
| Non-specific antibody binding to proteins or Fc receptors [38] [35] | Block with normal serum (from the secondary antibody species) or a protein block (BSA) for 30 minutes [36] [38]. | |
| No staining on target | Over-blocking | Titrate blocking reagents; excessive blocking can mask the target antigen. |
| Blocking serum species is incorrect | If using normal serum, ensure it matches the species of the secondary antibody, not the primary [38]. |
Experimental Protocols: Standardized Blocking Methods
Follow these detailed, step-by-step protocols to effectively suppress the most common sources of background staining.
Protocol 1: Blocking Endogenous Peroxidase Activity
This protocol is crucial when using HRP-based detection systems, especially with tissues high in red blood cells like liver, kidney, and spleen [37] [38] [35].
Preparation: After completing deparaffinization and rehydration of your tissue sections, prepare a peroxidase blocking solution. This is typically 3% hydrogen peroxide (H2O2) in distilled water or methanol [37] [36].
- Note: Methanol is often preferred as it helps preserve tissue morphology. If 3% H2O2 damages epitopes, a concentration as low as 0.3% can be tested [37].
Incubation: Submerge the slides in the peroxidase blocking solution and incubate for 10-15 minutes at room temperature [37] [36].
Washing: Thoroughly wash the slides twice with buffer (e.g., PBS or TBS) before proceeding with the rest of your staining protocol [37] [35].
Protocol 2: Blocking Endogenous Biotin
This two-step sequential block is essential when using ABC or LSAB detection methods on tissues like liver, kidney, and heart [37] [38] [35].
Apply Avidin/Streptavidin: Following your normal blocking procedure, incubate the sample with an excess of free, unlabeled avidin or streptavidin. This will bind to all endogenous biotin sites. Streptavidin is generally preferred over avidin because it is non-glycosylated, which avoids lectin binding and lower background [37].
Apply Biotin: Without washing, add an excess of free biotin. This will saturate all the remaining biotin-binding sites on the avidin/streptavidin molecules added in the first step [37].
Result: The end result is that all endogenous biotin is occupied and the detection streptavidin has nothing to bind to except the biotinylated secondary antibody. Proceed with your primary and secondary antibody incubations.
Protocol 3: Blocking Non-Specific Protein Binding
This step prevents antibodies from sticking to hydrophobic sites, Fc receptors, and other non-target proteins on the tissue [38] [35].
Prepare Blocking Solution: Common blocking solutions include:
- Normal Serum: Use 5% normal serum from the same species as the secondary antibody, diluted in TBST or TBS [36] [38].
- Protein Solutions: 1-5% Bovine Serum Albumin (BSA) in buffer is also effective [38] [35].
- Critical Note: If you are using a biotin-based detection system, avoid blocking with non-fat dry milk, as it contains biotin and will cause severe background [38].
Incubation: Apply the blocking solution to cover the entire tissue section. Incubate for 30 minutes at room temperature in a humidified chamber to prevent evaporation [36].
Tip: Do not rinse after this step. Simply tap off the excess blocking serum and apply the primary antibody directly.
The Scientist's Toolkit: Research Reagent Solutions
A curated list of essential reagents for effective blocking, with their specific functions.
| Reagent | Function/Purpose | Key Consideration |
|---|---|---|
| Hydrogen Peroxide (H₂O₂) | Quenches endogenous peroxidase activity to prevent non-specific chromogen deposition [37] [36] [35]. | Typically used at 3% concentration; can be reduced to 0.3% for sensitive epitopes [37]. |
| Levamisole | Inhibits endogenous alkaline phosphatase activity when using AP-based detection [37] [38]. | Ineffective against intestinal alkaline phosphatase; use acetic acid for those isozymes [38]. |
| Avidin/Biotin Blocking Kit | Sequentially blocks endogenous biotin to prevent binding of streptavidin-based detection reagents [37] [35]. | Essential for tissues like liver and kidney; can be circumvented by using polymer-based detection [37] [36]. |
| Normal Serum | Blocks non-specific hydrophobic and charge interactions; reduces binding to Fc receptors [38] [35]. | The species must match the host of the secondary antibody (e.g., goat serum for anti-goat secondary) [38]. |
| Bovine Serum Albumin (BSA) | A general protein block that reduces non-specific antibody binding to tissue proteins [38] [35]. | Ensure it is biotin-free if you plan to use a biotin-streptavidin detection system [38]. |
Experimental Workflow for Blocking
The following diagram outlines the logical decision-making process and sequential steps for implementing an effective blocking strategy to resolve spotty, uneven background staining.
Diagram Title: Diagnostic and Blocking Workflow for IHC Background.
Antibody Dilution and Diluent Selection for Clean Signal-to-Noise
Frequently Asked Questions (FAQs)
General Principles
1. What is signal-to-noise ratio and why is it critical in immunoassays? The signal-to-noise ratio (S/N) is a quantitative measure obtained by dividing the specific signal from your target by the background noise. A high S/N ratio is essential for assay sensitivity and reliability, as it ensures that the specific signal is easily distinguishable from non-specific background, which is particularly crucial for accurate trace analysis [39].
2. Are manufacturer-recommended antibody dilutions guaranteed to work? No, recommended dilutions are suggestions based on the manufacturer's experimental conditions and should be considered a starting point for your own optimization. Your optimal dilution may differ due to variations in sample type, experimental conditions, buffers, and detection systems [40].
3. Why might a previously working antibody suddenly stop producing good results? Antibodies, particularly in diluted solutions, are less stable and can lose reactivity over time. This occurs due to protein adsorption to container walls and aggregation, which is more impactful at low concentrations. For consistent results, prepare fresh working dilutions as needed and avoid reusing frozen diluted antibodies [41].
Diluent Selection
4. How does assay diluent affect my experiment? Assay diluents are crucial for equalizing differences between sample matrices (e.g., serum, plasma) and the calibrator diluent used for the standard curve. The right diluent formulation minimizes matrix effects, reduces non-specific binding, and is key to achieving a high signal-to-noise ratio in immunoassays like ELISA [42].
5. How can I quickly find the best assay diluent for my ELISA? You can run a parallel comparison using an Assay Diluent Optimization Pack, which typically contains different formulations (e.g., General, IgM-Reducing, Neptune). Test these diluents on the same coated plate with spiked samples to determine which one gives the most accurate recovery of the spike concentration [42].
Troubleshooting
6. My immunofluorescence has a high background. What should I check? High background often stems from insufficient blocking, excessive antibody concentration, sample autofluorescence, or insufficient washing. Ensure your sample remains hydrated, use validated blocking reagents, confirm your antibody dilutions, and increase washing stringency. For autofluorescence, use an unstained control and consider longer wavelength fluorophores [43].
7. I see no signal in my western blot. What are the common causes? Common causes include insufficient protein loaded, incomplete transfer during western blotting, SDS not being thoroughly washed out before staining, or the primary antibody being too dilute. Always load a positive control and confirm protein concentration and transfer efficiency [44].
Troubleshooting Guides
Weak or No Signal
| Possible Cause | Recommendations |
|---|---|
| Incorrect antibody dilution | Perform a titration experiment. Test a range of dilutions (e.g., 1:200, 1:500, 1:1000, 1:2000) around the manufacturer's suggestion to find the optimal concentration for your system [45] [40]. |
| Insufficient incubation time/temperature | For many antibodies, especially those from Cell Signaling Technology, optimal signal is achieved with overnight incubation at 4°C. Shorter incubations, even at higher temperatures, may yield significantly lower signal [45]. |
| Inadequate fixation or permeabilization | Consult the antibody datasheet for the recommended protocol. Ensure immediate and thorough fixation after treatment, and use the correct permeabilization method to allow antibody access to the target [43]. |
| Low expression of target protein | Confirm target expression by Western blot or other methods. For low-abundance targets, consider using signal amplification techniques or pairing the antibody with a brighter fluorophore [43]. |
| Loss of antigenicity | Use freshly prepared slides or plates. Samples stored for too long can lose the ability to bind the antibody effectively [43]. |
Diagram 1: Troubleshooting workflow for weak or no signal.
High or Spotty Background
| Possible Cause | Recommendations |
|---|---|
| Antibody concentration too high | Over-concentrated antibody is a common cause of background. Titrate to find a dilution that minimizes background while preserving specific signal. A high S/N is the goal [45]. |
| Insufficient blocking | Use normal serum from the same species as the secondary antibody or a charge-based blocker. Ensure adequate blocking time and concentration [43]. |
| Sample autofluorescence | Use an unstained control to check levels. Replace old formaldehyde stocks, and for low-abundance targets, choose longer wavelength channels to reduce interference [43]. |
| Insufficient washing | Increase wash volume, duration, and frequency. Thorough washing removes excess fixative, unbound antibodies, and loosely bound non-specific interactions [43]. |
| Non-specific antibody binding | Include appropriate controls like isotype controls or secondary-only controls. If available, compare results using knockout cells to identify non-specific binding [43]. |
Optimization Experimental Protocols
Protocol 1: Antibody Titration for Optimal Signal-to-Noise
Purpose: To empirically determine the ideal primary antibody dilution for your specific experimental system that maximizes specific signal while minimizing background [45] [40].
Methodology:
- Prepare a dilution series: Create a range of primary antibody dilutions. For a recommended 1:1000 dilution, test 1:200, 1:500, 1:1000, 1:2000, and 1:4000 [40].
- Include essential controls: Process positive control samples (known target expression) and negative controls (no or low expression) in parallel for each dilution [45].
- Apply to samples: Treat your test samples with each antibody dilution following your standard protocol (e.g., incubation overnight at 4°C).
- Quantify and calculate: Image the results and quantify the Mean Fluorescence Intensity (MFI) for both positive (MFI+) and negative (MFI-) controls. Calculate the Signal-to-Noise ratio for each dilution using the formula: S/N = MFI(+) ÷ MFI(-) [45].
- Analyze results: The optimal dilution is the one that yields the highest S/N ratio, not necessarily the strongest absolute signal.
The table below illustrates a sample data set from such a titration.
| c Antibody Dilution | MFI(+) (Positive Cells) | MFI(-) (Negative Cells) | Signal-to-Noise (S/N) |
|---|---|---|---|
| 1:200 | 850 | 180 | 4.7 |
| 1:500 | 720 | 95 | 7.6 |
| 1:1000 | 550 | 50 | 11.0 |
| 1:2000 | 350 | 35 | 10.0 |
| 1:4000 | 200 | 25 | 8.0 |
Table 1: Example data from an antibody titration experiment. The 1:1000 dilution provides the optimal S/N ratio and should be selected for future experiments [45].
Protocol 2: Spike-and-Recovery Experiment for ELISA Validation
Purpose: To assess whether the sample matrix (e.g., serum, plasma) affects the accuracy of detecting the analyte compared to the standard diluent, and to validate your diluent choice [46].
Methodology:
- Prepare spikes: Add a known amount of purified analyte (the "spike") into both the standard diluent and the natural sample matrix.
- Run the assay: Measure the response of the spiked samples against a standard curve using your ELISA protocol.
- Calculate recovery: For each spike level, calculate the percentage recovery using the formula:
- Recovery % = (Observed concentration in sample matrix / Observed concentration in standard diluent) × 100
- Interpret results: Ideally, recovery should be close to 100%. Consistent under- or over-recovery indicates matrix interference.
The table below shows how results from a spike-and-recovery experiment can be summarized.
| c Sample (n) | Spike Level | Expected (from diluent) | Observed (from matrix) | Recovery % |
|---|---|---|---|---|
| Urine (9) | Low (15 pg/mL) | 17.0 pg/mL | 14.7 pg/mL | 86.3% |
| Urine (9) | Medium (40 pg/mL) | 44.1 pg/mL | 37.8 pg/mL | 85.8% |
| Urine (9) | High (80 pg/mL) | 81.6 pg/mL | 69.0 pg/mL | 84.6% |
Table 2: Example summary of spike-and-recovery results for a human urine sample assay [46].
Diagram 2: Experimental workflow for a spike-and-recovery assay.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| General Assay Diluent | A standard diluent containing mammalian proteins, used to match the matrix of common biological samples like serum and plasma, helping to equalize the standard curve and sample wells [42]. |
| IgM-Reducing Assay Diluent | Specifically formulated to reduce interfering IgM, which can cause non-specific binding and high background in assays [42]. |
| Neptune Assay Diluent | Contains non-mammalian proteins, ideal for samples that may have high levels of endogenous immunoglobulins or when working with mammalian-derived detection systems where non-mammalian proteins reduce interference [42]. |
| Antigen-Down Assay Diluent | Optimized for "antigen-down" ELISA formats where the antigen is immobilized on the plate. It helps minimize non-specific binding of the detecting antibody [42]. |
| Anti-fade Mounting Medium | Preserves fluorescence signal during imaging by reducing photobleaching of fluorophores when exposed to light. Essential for maintaining signal intensity in immunofluorescence [43]. |
| Signal Amplification Kits | Used to enhance the detection signal for targets with low abundance, thereby improving the sensitivity of the assay and helping to distinguish weak specific signals from noise [43]. |
Precision in Washes, Incubation Times, and Reagent Application
Frequently Asked Questions (FAQs)
Q: What are the primary causes of uneven or patchy staining? A: The most common causes are inconsistent reagent coverage during incubation, tissue folding, incomplete section adhesion to the slide, and variable fixation conditions across the tissue sample [3] [12]. Ensuring reagents fully cover the section and standardizing fixation times are crucial first steps.
Q: How can I reduce high, uneven background staining? A: High background is frequently due to a primary antibody concentration that is too high, insufficient blocking of endogenous enzymes, or incomplete washing steps [12] [47]. A titration experiment for your primary antibody, combined with thorough washing and the use of appropriate blocking sera, can significantly improve specificity [12].
Q: My washes are standardized, but results are still variable between users. Why? A: Standardized washing involves more than just duration. Consistency in the volume of wash buffer used and the form of agitation (e.g., gentle rocking vs. vigorous shaking) is critical. Variable results between different operators are often traced back to different washing techniques [3].
Q: Can the drying of reagents cause staining artifacts? A: Yes. Allowing the probe or antibody solution to dry onto the tissue section during long incubation times is a common problem that causes heavy, non-specific staining, particularly at the edges of the section [3]. Using a well-sealed humidity chamber is essential to prevent this.
Troubleshooting Guide: Spotty and Uneven Background Staining
| Problem Category | Specific Issue | Recommended Solution | Key Quantitative Considerations |
|---|---|---|---|
| Reagent Application | Uneven or patchy staining | Use a humidified chamber; ensure liquid fully covers the tissue section without bubbles [3] [12]. | N/A |
| Reagents drying on sections | Ensure sealed humidity chamber; optimize incubation times to prevent evaporation [3]. | N/A | |
| Incubation | Primary antibody concentration | Perform a titration experiment to find optimal concentration [12]. | Test a range (e.g., 1:50, 1:100, 1:200) starting from datasheet recommendation [12]. |
| Chromogen over-development | Monitor color development under a microscope and stop reaction promptly [12]. | Development time can vary from seconds to minutes; requires real-time monitoring. | |
| Washes | Variable results between runs or users | Standardize all aspects of washing: duration, volume, and agitation method [3]. | Use a large, consistent volume (e.g., copious copious rinsing) with gentle agitation [47]. |
| Incomplete wax removal | Ensure thorough dewaxing with fresh, high-quality solvents prior to hydration [3]. | N/A | |
| Tissue & Section Quality | Tissue folding or poor adhesion | Use charged slides for IHC/ISH; check sections before staining [3] [12]. | N/A |
| Variable fixation | Standardize fixation conditions (time, temperature, pH) for all samples [3]. | Formalin fixation times should be consistent; over-fixation can mask epitopes [12]. |
Experimental Protocols for Precision
Protocol 1: Precision Verification for Washes This protocol is designed to establish a consistent washing technique that minimizes variability.
- Materials: Wash buffer (e.g., PBS with 0.05% Tween-20), staining dishes, timer.
- Method: Following any incubation step (e.g., after primary antibody), perform the wash as follows:
- Gently agitate the slide to dislodge the reagent.
- Immerse the slide in a copious and consistent volume of wash buffer (e.g., 200 mL per slide).
- Agitate continuously using a standardized platform shaker set to low speed (e.g., 50-60 rpm).
- Duration: Perform three washes, each for 5 minutes.
- Key Consideration: Ensure all technicians in the lab follow the same volume, agitation, and duration protocol [3].
Protocol 2: Antibody Titration for Optimal Incubation This protocol finds the ideal primary antibody concentration to maximize signal while minimizing background.
- Materials: Primary antibody, antibody diluent, positive control tissue.
- Method:
- Prepare a series of primary antibody dilutions (e.g., 1:50, 1:100, 1:200, 1:500) in diluent.
- Apply each dilution to adjacent serial sections of the positive control tissue.
- Incubate for a fixed, standardized time (e.g., 60 minutes at room temperature or overnight at 4°C).
- Complete the rest of the IHC protocol identically for all slides.
- Evaluate under a microscope. The optimal dilution provides the strongest specific signal with the cleanest background [12].
Experimental Workflow for Troubleshooting Uneven Staining
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function | Application Note |
|---|---|---|
| Charged Slides | Provides a positively charged surface to enhance tissue section adhesion, preventing lift-off during rigorous washes [3]. | Essential for ISH and automated IHC protocols to prevent uneven staining due to pooling [3]. |
| Blocking Sera | Reduces non-specific binding of antibodies by saturating reactive sites on the tissue section [12] [47]. | Should be normal serum from the same species as the secondary antibody. |
| Antibody Diluent | A buffer solution used to reconstitute and dilute antibodies. Often contains proteins and detergents to enhance stability and reduce background [12]. | Using a diluent with 0.05% Tween-20 can minimize hydrophobic interactions that cause background [12]. |
| Enzyme Block | Inactivates endogenous enzymes (e.g., peroxidases or phosphatases) present in tissues that could react with the chromogen, creating false-positive signal [12]. | A 3% H₂O₂ solution is commonly used to block endogenous peroxidases in HRP-based detection [12]. |
| Automated Stainer | A robotic system that performs all staining steps (dewaxing, reagent application, washing) according to a programmed protocol [47]. | Eliminates operator-to-operator variability and ensures precise, consistent incubation times and reagent application [47]. |
In the field of protein detection via immunohistochemistry (IHC) and western blotting, the choice of detection system is critical. Researchers often face the challenge of selecting between polymer-based and biotin-based (avidin-biotin) methods. This technical guide focuses on troubleshooting a common problem in both systems: spotty, uneven background staining. Understanding the principles, advantages, and limitations of each system is the first step in diagnosing and resolving these issues to achieve clean, reproducible results for drug development and diagnostic applications.
Core Concepts at a Glance
The table below summarizes the fundamental principles and characteristics of biotin-based and polymer-based detection systems.
Table 1: Comparison of Core Detection System Concepts
| Feature | Biotin-Based Systems | Polymer-Based Systems |
|---|---|---|
| Core Principle | Uses a biotinylated secondary antibody followed by an enzyme-conjugated streptavidin/avidin complex. [48] [49] | Uses a secondary antibody directly conjugated to a polymer backbone carrying numerous enzyme molecules. [50] [49] |
| Typical Steps | 3-step: Primary Ab → Biotinylated Secondary Ab → Enzyme-Streptavidin. [48] | 2-step: Primary Ab → Enzyme-Polymer Conjugated Secondary Ab. [49] |
| Key Component | Biotin, Streptavidin | Dextran polymer chain |
| Endogenous Interference | Endogenous biotin can cause significant background. [48] | No endogenous biotin interference. [49] |
The following diagram illustrates the basic structural difference between the two detection methodologies, which is the root cause of their different performance characteristics.
Quantitative Performance Data
The selection of a detection system often involves a trade-off between sensitivity and the potential for background. The following table compiles key performance metrics from experimental comparisons.
Table 2: Quantitative Performance Comparison of Detection Systems
| Detection System | Reported Sensitivity Increase (vs. Traditional HRP) | Key Advantages | Key Disadvantages / Background Issues |
|---|---|---|---|
| Streptavidin-PolyHRP | Up to 110-fold increase. [48] | Highest sensitivity for low-abundance targets. [48] | High endogenous biotin interference requires modified blocking. [48] |
| Streptavidin-HRP | Relatively small (e.g., ~2-fold). [48] | Well-established protocol. | High background after harsh antigen retrieval. [50] [49] |
| Polymer-Based (e.g., ImmPRESS) | Similar or higher intensity than EnVision+ in 16/18 antigens. [50] | Lower cost (e.g., 25% less than EnVision+). [50] No endogenous biotin issues. [49] | Can produce abundant background with certain antigens (e.g., calretinin). [50] |
| Polymer-Based (e.g., EnVision+) | Established high sensitivity polymer system. [50] | Reliable, commercially available. | Background can vary by antigen. [50] |
| Traditional HRP-secondary Ab | Baseline (No amplification). | Simple, low-cost. | Lower sensitivity, can require more primary antibody. [48] |
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Why is my background staining high and uneven with biotin-based systems?
Answer: The most common cause is interference from endogenous biotin present in the tissue itself. [48] [49] This is especially prevalent in tissues like liver, kidney, and brain.
- Solution: Implement a modified blocking procedure. [48]
- Prior to adding the primary antibody, block the tissue section with a solution containing free streptavidin (e.g., 50–100 µg/mL) for 20 minutes to bind endogenous biotin sites. [48]
- Without washing, add a solution containing free biotin (e.g., 50–100 µg/mL) for 20 minutes to block the binding sites on the streptavidin. [48]
- Proceed with your standard protocol (primary antibody, etc.). This two-step blocking strategy effectively neutralizes endogenous biotin.
FAQ 2: My polymer-based system is showing high background. What should I check?
Answer: Background in polymer-based systems is typically due to non-specific antibody binding or suboptimal protocol conditions. [50] [51]
- Solution:
- Optimize antibody concentrations: High concentrations of primary or secondary antibody are a primary cause of non-specific binding and background. [51] [52] Perform an antibody titration to find the optimal dilution.
- Re-evaluate your blocking buffer: Ensure you are using a compatible blocking agent. For example, when detecting phosphoproteins, avoid milk or casein and use BSA in Tris-buffered saline instead. [51]
- Increase wash stringency: Ensure sufficient wash buffer volume, agitation, and wash duration (e.g., 3 x 5 minutes) with a buffer containing 0.05% Tween 20. [51] [52]
FAQ 3: When should I choose a polymer-based system over a biotin-based one?
Answer: The choice depends on your specific experimental needs and tissue type. Use this decision flow to guide your selection:
FAQ 4: My signal is weak, even for abundant targets. How can I improve it?
Answer: Weak signal can be caused by several factors across different systems. [51]
- For all systems: Check transfer efficiency (for western blots) by staining the gel post-transfer or the membrane with reversible protein stain. Ensure antibodies have not lost activity and that antigen is not degraded. [51]
- For biotin-based systems: Ensure the streptavidin-enzyme conjugate is fresh and active. The incubation time or concentration may need optimization.
- For polymer-based systems: The polymer-enzyme conjugate can be inactivated by sodium azide. Never use sodium azide in buffers with HRP-conjugated antibodies. [51]
Detailed Experimental Protocols
Protocol 1: Modified 3-Step Immunoblotting with Streptavidin-PolyHRP
This protocol is designed to maximize sensitivity while controlling for endogenous biotin interference. [48]
Key Research Reagent Solutions:
- Biotinylated Secondary Antibody: e.g., Goat anti-mouse IgG (KPL #16-18-06) or Goat anti-rabbit (KPL #16-15-06). [48]
- Streptavidin-PolyHRP: e.g., Streptavidin-PolyHRP20 (Fitzgerald #65R-S107) or Streptavidin-PolyHRP80 (Fitzgerald #65R-S105). [48]
- Modified Blocking Solution: 3% non-fat milk in TBST, supplemented with free streptavidin and biotin for the initial block. [48]
Methodology:
- Electrophoresis and Transfer: Resolve proteins by SDS-PAGE and transfer to a nitrocellulose membrane using standard protocols. [48]
- Blocking (Critical Step for Background): Block the membrane with 3% non-fat milk in TBST for 1 hour at room temperature (RT). Do not use milk if using an avidin-biotin system for IHC, as milk contains biotin. [51]
- Primary Antibody Incubation: Incubate the blot with the primary antibody diluted in 1% non-fat milk in TBST overnight at 4°C. [48]
- Wash: Wash the blot three times with TBST for 5 minutes each. [48]
- Biotinylated Secondary Antibody: Incubate with the corresponding biotinylated secondary antibody (e.g., 1:10,000 dilution in 1% non-fat milk in TBST) for 1 hour at RT with gentle shaking. [48]
- Wash: Wash the blot three times with TBST for 5 minutes each. [48]
- Streptavidin-PolyHRP Detection: Incubate with Streptavidin-PolyHRP (e.g., 1:400 dilution) for 1 hour at RT with gentle shaking. [48]
- Final Wash and Develop: Perform a final wash (3 x 5 minutes with TBST) and develop using an enhanced chemiluminescence (ECL) reagent. [48]
Protocol 2: Standard 2-Step Immunoblotting with Polymer-Based Detection
This protocol highlights a simpler workflow that avoids endogenous biotin issues. [48] [49]
Key Research Reagent Solutions:
- Polymer-HRP Conjugated Secondary Antibody: e.g., Goat anti-rabbit PolyHRP (Thermo Scientific #32260). [48]
Methodology:
- Electrophoresis and Transfer: Resolve and transfer proteins as in Protocol 1. [48]
- Blocking: Block the membrane with a compatible blocking buffer (e.g., 3% BSA in TBST for phosphoproteins) for 1 hour at RT. [51]
- Primary Antibody Incubation: Incubate with the primary antibody diluted in blocking buffer overnight at 4°C. [48]
- Wash: Wash the blot three times with TBST for 5 minutes each. [48]
- Polymer-Based Secondary Antibody: Incubate with the PolyHRP-conjugated secondary antibody (e.g., 1:10,000 dilution in blocking buffer) for 1 hour at RT. [48]
- Final Wash and Develop: Wash the blot (3 x 5 minutes with TBST) and develop using ECL. [48]
The Scientist's Toolkit: Essential Reagents
Table 3: Key Research Reagent Solutions and Their Functions
| Reagent / Kit | Function / Application | Example Product / Source |
|---|---|---|
| Streptavidin-PolyHRP | High-sensitivity detection conjugate for use with biotinylated secondary antibodies. Contains multiple HRP enzymes for signal amplification. [48] | Streptavidin-PolyHRP20 (Fitzgerald #65R-S107). [48] |
| Polymer-HRP Secondary Antibody | Directly conjugated secondary antibody for simplified 2-step protocols. Avoids endogenous biotin interference. [48] [49] | Goat anti-rabbit PolyHRP (Thermo Scientific #32260). [48] |
| Free Streptavidin & Biotin | Used together for sequential blocking to neutralize endogenous biotin in tissues or samples, critical for reducing background in biotin-based systems. [48] | Streptavidin (Thermo Scientific #21122); Biotin (Arcos Organics #230090010). [48] |
| Compatible Blocking Buffers | Protein-based solutions (BSA, non-fat milk) used to cover non-specific binding sites on the membrane. Choice is critical to prevent background. [51] | StartingBlock or SuperBlock Buffers (Thermo Scientific); 3% BSA in TBST. [51] |
| High-Sensitivity Chemiluminescent Substrate | A stable, long-lasting ECL reagent is essential for capturing the strong but potentially rapid signal from amplified systems like PolyHRP. [52] | Radiance ECL (Azure Biosystems); SuperSignal West Femto (Thermo Fisher). [51] [52] |
Systematic Troubleshooting: From High Background to Pristine Staining
Step-by-Step Diagnostic Guide for Spotty Background Issues
What causes spotty, uneven background staining in IHC?
Spotty or uneven background staining in Immunohistochemistry (IHC) is a common issue that can obscure your results. This problem typically stems from inconsistencies during sample preparation, the presence of endogenous tissue components, or suboptimal antibody binding conditions [53] [10]. Accurately diagnosing the cause is the first step toward achieving a clean, interpretable stain.
Primary Causes and Corrective Actions
The table below summarizes the most frequent causes of spotty background staining and the specific steps you can take to resolve them.
| Root Cause | Specific Problem | Recommended Corrective Action |
|---|---|---|
| Sample Preparation [53] [23] | Inadequate deparaffinization | Repeat the experiment with new tissue sections and fresh xylene to ensure all paraffin wax is completely removed [53]. |
| Tissue damage during sectioning or handling | Prepare thinner sections and handle samples carefully to avoid physical damage that causes diffuse staining [10]. | |
| Endogenous Tissue Activity [53] [10] | Endogenous peroxidases | Quench slides in a 3% H₂O₂ solution (in methanol or water) for 10 minutes before primary antibody incubation [53] [10]. |
| Endogenous biotin (esp. in liver, kidney) | Use a polymer-based detection system (e.g., SignalStain Boost) instead of biotin-based systems. Alternatively, perform a biotin block using a commercial avidin/biotin blocking solution [53] [10]. | |
| Antibody & Detection Issues [53] [10] | Primary antibody concentration too high | Titrate the primary antibody to find the optimal dilution that minimizes nonspecific binding [10]. |
| Non-specific secondary antibody binding | Increase the concentration of normal serum (from the secondary antibody host species) in the blocking buffer to as high as 10%. Always run a no-primary-antibody control to check for secondary antibody background [53] [10]. | |
| Use of biotin-based systems in sensitive tissues | Switch to a polymer-based or biotin-free detection system to avoid interference with endogenous biotin [53] [23]. | |
| Insufficient Blocking or Washing [53] | Inadequate blocking of non-specific sites | Ensure adequate blocking with a suitable buffer (e.g., 1X TBST with 5% Normal Goat Serum for 30 minutes) prior to primary antibody incubation [53]. |
| Incomplete washing | Perform adequate washes after primary and secondary antibody incubations: three washes for 5 minutes each with TBST [53]. |
Step-by-Step Diagnostic Protocol
Follow this logical workflow to systematically identify the source of your spotty background staining.
Diagnostic Workflow Explained:
Run a No-Primary-Antibody Control: Incubate a test section with everything except the primary antibody (replace it with antibody diluent) [10]. This is your most important control.
- If background persists, the issue lies with the detection system, secondary antibody, or endogenous tissue activity. Proceed to block endogenous enzymes and biotin, and ensure your secondary antibody is appropriately diluted and does not cross-react [53] [10].
- If background is absent, the problem is likely related to the primary antibody, sample preparation, or antigen retrieval. Move to the next step.
Inspect Sample Preparation: Spotty staining can be a direct result of incomplete deparaffinization. If this is suspected, cut new tissue sections and use fresh xylene to ensure all wax is removed [53].
Validate with a Positive Control: Use a tissue known to express your target. If the staining is clean on the control tissue but spotty on your experimental tissue, the issue may be unique to the experimental tissue (e.g., poor fixation). If the control also shows spotty background, the problem is systemic to your protocol, likely related to the primary antibody concentration or antigen retrieval [53] [23].
Optimize Antigen Retrieval: Inconsistent or insufficient antigen retrieval is a major cause of uneven staining. For Heat-Induced Epitope Retrieval (HIER), a microwave oven is generally recommended over a water bath. Ensure you are using the correct buffer (e.g., citrate pH 6.0 or Tris-EDTA pH 9.0) as specified on the antibody datasheet, and that the solution is fresh [53] [23].
The Scientist's Toolkit: Key Research Reagent Solutions
Having the right reagents is crucial for preventing and troubleshooting background issues. The table below lists essential solutions.
| Reagent / Solution | Primary Function in Troubleshooting Spotty Background |
|---|---|
| Fresh Xylene [53] | Completely dissolves and removes paraffin wax from FFPE sections; outdated or impure xylene is a primary cause of spotty staining. |
| Hydrogen Peroxide (3%) [53] [10] | Quenches endogenous peroxidase activity present in most tissues, preventing false-positive signals with HRP-based detection. |
| Avidin/Biotin Blocking Solution [10] | Blocks endogenous biotin found at high levels in tissues like liver and kidney, preventing nonspecific binding in biotin-streptavidin detection systems. |
| Normal Serum [53] [10] | Used in blocking buffers to bind to non-specific sites and Fc receptors, reducing nonspecific binding of the secondary antibody. Should be from the same species as the secondary antibody. |
| Polymer-Based Detection Reagents [53] [23] | A biotin-free detection method that offers high sensitivity and eliminates background from endogenous biotin, providing a cleaner alternative to ABC methods. |
| SignalStain Antibody Diluent [53] | An optimized diluent that helps maintain antibody stability and can reduce nonspecific ionic interactions, leading to lower background. |
| TBST (Tris-Buffered Saline with Tween-20) [53] | A standard washing buffer; its mild detergent action helps remove unbound antibodies and reagents during washes, which is critical for achieving low background. |
Optimizing Deparaffinization and Blocking Steps for Even Staining
Troubleshooting Guide: Spotty, Uneven Background Staining
This guide addresses the common causes of spotty, uneven background staining in Immunohistochemistry (IHC) and provides targeted solutions for researchers.
- Problem: Incomplete removal of paraffin wax creates a physical barrier, leading to uneven reagent penetration, spotty background, and weak or absent specific signal [54] [23].
Solution: Ensure thorough deparaffinization by using fresh xylene or a suitable substitute. Repeat the process with new tissue sections if issues arise [54].
Problem: Endogenous enzymes (peroxidases, phosphatases) or biotin in the tissue can react with the detection system, generating a high, diffuse, non-specific background [54] [23].
Solution: Implement appropriate blocking steps prior to primary antibody incubation. The required blocks depend on your detection system and tissue type [54] [23].
Problem: Inadequate washing between steps can leave unbound antibodies or reagents on the slide, contributing to high, uneven background across the entire tissue section [54].
Solution: Perform thorough washes, typically three changes of a buffered solution like TBST, for 5 minutes each after primary and secondary antibody incubations [54].
Problem: A secondary antibody may bind to endogenous immunoglobulins within the tissue, particularly when working with tissue from the same species in which the secondary was raised (e.g., mouse-on-mouse staining) [54].
- Solution: Always include a no-primary-antibody control to identify this issue. Use species-specific polymer-based detection systems or validated kits designed to minimize this cross-reactivity [54].
The table below summarizes the reagents needed to resolve these issues.
| Reagent Type | Specific Examples | Function |
|---|---|---|
| Deparaffinization Agent | Fresh Xylene [54] | Dissolves and removes paraffin wax from FFPE tissue sections to allow aqueous-based reagents to penetrate. |
| Peroxidase Block | 3% H₂O₂ in RODI water [54] | Quenches endogenous peroxidase activity to prevent high background with HRP-based detection systems. |
| Biotin Block | Avidin/Biotin blocking kits [23] | Saturates endogenous biotin in tissues (e.g., liver, kidney) to prevent non-specific binding in biotin-based detection. |
| Protein Block | Normal Goat Serum in TBST [54] | Reduces non-specific background staining by blocking reactive sites on the tissue and slide. |
| Wash Buffer | 1X TBST [54] | Removes unbound antibodies and reagents during the staining procedure to minimize background. |
Frequently Asked Questions (FAQs)
Q1: My positive control stains well, but my test slides show high background. What should I do first? First, run a "no-primary-antibody" control on your test tissue. If background persists, the issue is likely related to your detection system or inadequate blocking. If the background is absent, the problem may be with the concentration or specificity of your primary antibody [54].
Q2: Are some tissues more prone to high background staining? Yes. Tissues with high endogenous biotin (e.g., liver and kidney) are notorious for causing high background when using biotin-streptavidin detection systems. For these tissues, switching to a polymer-based detection system is highly recommended [54] [23].
Q3: My staining is weak and the background is spotty. Could this be one single issue? Yes. Inadequate deparaffinization is a classic cause of both weak specific signal and spotty, uneven background. The residual wax prevents antibodies from reaching their target and causes reagents to pool unevenly. Always ensure deparaffinization is complete by using fresh solvents [54].
Experimental Workflow for Optimal Deparaffinization and Blocking
The following diagram outlines a standardized protocol to prevent spotty and uneven staining.
Signal and Background Optimization
Different detection systems offer varying levels of sensitivity and are prone to different background issues. The table below compares common methods to help you select the right one.
| Detection Method | Relative Sensitivity | Common Background Issues | Optimal Use Case |
|---|---|---|---|
| Standard Indirect (HRP) | Medium | High background if endogenous peroxidase is not fully blocked. | Routine detection of moderately abundant targets. |
| Avidin-Biotin Complex (ABC) | High | High background in tissues with endogenous biotin (e.g., liver, kidney) [23]. | High-sensitivity detection; avoid with biotin-rich tissues. |
| Labeled Streptavidin-Biotin (LSAB) | High | Reduced non-specific binding compared to ABC [23]. | A robust and highly sensitive alternative to ABC. |
| Polymer-Based | High [54] | Low background; not affected by endogenous biotin [54]. | Preferred for sensitive detection and tissues with high endogenous biotin. |
| Tyramide Signal Amplification | Very High | Potential for over-amplification and high background if not optimized [23]. | Detecting low-abundance targets; requires careful titration. |
Antibody Titration and Cross-Reactivity Solutions
Frequently Asked Questions
What are the primary causes of spotty, uneven background staining in IHC? Inadequate deparaffinization is a common cause, which can be resolved by repeating the experiment with new tissue sections and fresh xylene. Additionally, high background can stem from endogenous peroxidase activity (when using HRP-based detection) or endogenous biotin, particularly in tissues like kidney and liver [55].
How can cross-reactivity lead to non-specific staining and how is it avoided? Cross-reactivity occurs when an antibody binds to an off-target antigen, often due to the antibody's lack of specificity. A study cited that, out of 11,000 affinity-purified antibodies, approximately 95% showed binding to non-target proteins. To minimize this, carefully select highly specific monoclonal antibodies for critical steps and ensure thorough blocking [56].
Why is antibody titration critical, and what are the consequences of skipping it? Using an antibody at a non-optimal concentration is a major cause of high background or weak staining. Overtitration leads to high background, while undertitration results in weak or no signal. Antibodies sold by mass require titration to determine the ideal concentration for your specific cell type and application, which optimizes the signal-to-noise ratio [57].
Troubleshooting Guide: Spotty and Uneven Background Staining
The table below summarizes the common causes and solutions for spotty, uneven background staining.
| Potential Cause | Recommended Solution | Key Experimental Considerations |
|---|---|---|
| Inadequate Deparaffinization [55] | Repeat with new tissue sections and fresh xylene. | Ensure deparaffinization is complete before hydration and staining. |
| Endogenous Peroxidase Activity [55] | Quench with 3% H2O2 in water for 10 minutes before primary antibody incubation. | Use with HRP-based detection systems. |
| Endogenous Biotin [55] | Use a polymer-based detection system instead of biotin-based systems. Alternatively, perform a biotin block after the standard blocking step. | Especially critical for kidney and liver tissues. |
| Insufficient Blocking [55] | Block with 1X TBST with 5% normal goat serum for 30 minutes. For flow cytometry, use serum from the host species of your antibodies [58]. | Ensure the blocking serum does not interfere with antibodies. |
| Secondary Antibody Cross-Reactivity [55] | Always run a no-primary-antibody control. For mouse-on-mouse staining, use anti-mouse secondary reagents specifically designed to minimize background. | This control identifies if the background is from the secondary antibody. |
| Inadequate Washing [55] | Wash slides 3 times for 5 minutes with TBST after primary and secondary antibody incubations. | Residual unbound antibody contributes significantly to background. |
Research Reagent Solutions
The following table details key reagents used to prevent high background and cross-reactivity.
| Reagent / Solution | Primary Function | Application Notes |
|---|---|---|
| Normal Serum [55] [58] | Blocks non-specific binding sites on tissues and cells. | Use serum from the same species as the secondary antibody, or from the host species of your primary antibodies for flow cytometry. |
| Fc Receptor Block [58] | Blocks Fc receptors on cells to prevent antibody binding independent of antigen specificity. | Crucial for flow cytometry of immune cells. Can be specific anti-FcR antibodies or excess immunoglobulin. |
| Polymer-Based Detection [55] | A detection system that avoids the use of biotin, eliminating background from endogenous biotin. | Recommended over avidin-biotin complexes for tissues high in endogenous biotin. |
| Brilliant Stain Buffer [57] | Prevents fluorescence dye-dye interactions between certain polymer dyes (e.g., Brilliant Violet) in flow cytometry. | Essential for panels containing multiple "Brilliant" class dyes to avoid off-spectrum signal and false positives. |
| Tandem Stabilizer [58] | Protects tandem fluorophores from degradation, which can cause erroneous signal spillover. | Should be added to staining mixtures and storage buffers for flow cytometry antibodies conjugated to tandem dyes. |
Experimental Protocol: Blocking for High-Parameter Flow Cytometry
This protocol is designed to minimize non-specific binding and cross-reactivity in flow cytometry, which can manifest as high background signal [58].
Materials:
- Mouse serum
- Rat serum
- Tandem stabilizer
- Brilliant Stain Buffer
- FACS buffer
- V-bottom 96-well plates
- Centrifuge and multichannel pipettes
Procedure:
- Prepare Blocking Solution: Create a mixture containing mouse serum, rat serum, and tandem stabilizer in FACS buffer. For a 1 mL mix, use 300 µL of mouse serum, 300 µL of rat serum, and 1 µL of tandem stabilizer, bringing the final volume to 1 mL with FACS buffer [58].
- Cell Preparation: Dispense cells into a V-bottom 96-well plate. Centrifuge at 300 × g for 5 minutes and decant the supernatant.
- Block Cells: Resuspend the cell pellet in 20 µL of the prepared blocking solution. Incubate for 15 minutes at room temperature in the dark.
- Prepare Staining Mix: While blocking, prepare the surface antibody staining master mix. It is recommended that the mix contain Brilliant Stain Buffer (up to 30% by volume) to prevent polymer dye interactions [58].
- Stain Cells: Add 100 µL of the surface staining mix directly to the cells without washing away the blocking solution. Mix gently by pipetting.
- Incubate and Wash: Incubate for 1 hour at room temperature in the dark. Wash the cells by adding 120 µL of FACS buffer, centrifuging, and decanting the supernatant. Repeat this wash with 200 µL of FACS buffer.
- Resuspend and Acquire: Resuspend the cells in FACS buffer containing a 1:1000 dilution of tandem stabilizer. Acquire data on a flow cytometer [58].
The diagram below outlines a logical workflow for troubleshooting spotty, uneven background staining, integrating solutions for both immunohistochemistry and flow cytometry.
Addressing Autofluorescence and Endogenous Activity
Frequently Asked Questions (FAQs)
What causes high background staining in my immunohistochemistry (IHC) experiment? High background, or a poor signal-to-noise ratio, can stem from several sources. Common causes include interference from endogenous enzymes (like peroxidases or phosphatases), the presence of endogenous biotin or lectins, nonspecific binding of your primary or secondary antibody, or issues with the primary antibody concentration and diluent [10] [59].
Why is there no staining in my IHC experiment? A lack of staining can be due to several factors, including loss of antibody potency from improper storage or degradation, issues with the enzyme-substrate reaction, or inhibition of the secondary antibody due to extremely high concentration [10]. Other potential causes are inadequate antigen retrieval or the tissue sections having dried out during storage or processing [59].
What is autofluorescence and why is it a problem? Autofluorescence is background fluorescence in a tissue that is not attributed to the specific staining of your target. It arises from endogenous molecules with fluorophore-like properties [60]. This background signal can mask the expression of low-abundance targets or dim dyes, making it challenging to distinguish specific staining from noise [61].
Which endogenous molecules cause autofluorescence? Several endogenous compounds contribute to autofluorescence, including:
- Lipofuscin: A granular lipophilic pigment that accumulates in lysosomes with age and fluoresces strongly across a broad spectrum (500-695 nm) [61] [62].
- Collagen and Elastin: Structural proteins with emission in the blue region (300-450 nm) [61].
- NADH and Flavins: Metabolic enzymes that emit around 450 nm [61].
- Heme groups: Found in red blood cells, their porphyrin ring structure causes broad autofluorescence [61].
How can I reduce autofluorescence from aldehyde fixation? Aldehyde fixatives like formalin and paraformaldehyde create Schiff bases that result in autofluorescence [61]. To minimize this:
- Fix samples for the minimum time required.
- Consider alternatives like chilled organic solvents (e.g., ethanol) where appropriate.
- Treat tissue sections with sodium borohydride (e.g., 1 mg/mL in PBS), though this can have variable results [10] [61].
Troubleshooting Guides
Guide 1: Addressing High Background in IHC Staining
| Problem Cause | Recommended Solution | Supporting Protocol / Notes |
|---|---|---|
| Endogenous Peroxidases | Quench with 3% H₂O₂ in methanol or water for 10-15 minutes at room temperature [10] [59]. | Use fresh H₂O₂ solutions. Commercial blocking solutions are also available [10]. |
| Endogenous Biotin | Use a polymer-based detection system instead of biotin-based systems. Alternatively, perform a biotin block using a commercial avidin/biotin blocking solution [10] [59]. | Particularly important for tissues with high endogenous biotin (e.g., liver, kidney) [59]. |
| Nonspecific Antibody Binding | Increase the concentration of normal serum from the source species of your secondary antibody in the blocking buffer (up to 10% v/v). Alternatively, reduce the concentration of the primary or biotinylated secondary antibody [10]. | Ensure adequate blocking (e.g., 30 minutes with 5% normal goat serum in TBST) [59]. |
| Primary Antibody Issues | Reduce the final concentration of the primary antibody. Add NaCl to the antibody diluent to a final concentration of 0.15-0.6 M to reduce ionic interactions [10]. | Titrate the antibody to find the optimal concentration. Always use the recommended diluent if specified [59]. |
| Inadequate Washes | Wash slides thoroughly 3 times for 5 minutes with a buffered solution like TBST after primary and secondary antibody incubations [59]. | Adequate washing is critical for achieving low background and high signal [59]. |
Guide 2: Identifying and Quenching Autofluorescence
The following workflow outlines a strategic approach to diagnosing and mitigating autofluorescence in your experiments.
Quantitative Data on Autofluorescence Quenching Reagents
The table below summarizes common reagents used to suppress autofluorescence, detailing their primary use and method of action.
| Reagent | Primary Use / Target | Mechanism of Action | Key Considerations |
|---|---|---|---|
| Sudan Black B [61] [62] | Lipofuscin, aldehyde-induced AF | Lipophilic dye that binds to and quashes AF from lipid-rich compounds [61]. | Fluoresces in the far-red channel; consider this in multiplex panels [61]. |
| Sodium Borohydride [10] [61] | Aldehyde-induced AF | Reduces Schiff bases formed during aldehyde fixation [61]. | Can have variable effectiveness; use ice-cold solution (1 mg/mL in PBS) [10] [61]. |
| TrueVIEW Autofluorescence Quenching Kit [61] | Broad-spectrum AF | Commercial reagent designed to reduce AF from multiple causes [61]. | Follow manufacturer's protocol for standardized results. |
| Copper Sulfate (CuSO₄) & Ammonium Chloride [61] | Red blood cell (RBC) AF | Treatment at low pH to reduce heme-group autofluorescence [61]. | PBS perfusion prior to fixation is a more effective preventative measure [61]. |
| Eriochrome Black T [61] | Lipofuscin, formalin-induced AF | Reduces autofluorescence similar to Sudan Black B [61]. | An alternative quenching agent. |
| Spectral Unmixing [63] [60] | All sources (in spectral cytometry) | Computational extraction of the AF signal based on its unique spectral signature [63]. | Requires a spectral flow cytometer and an unstained control to measure the AF signature [60]. |
Guide 3: Planning a Robust Fluorescence Experiment
Strategic experimental design is the best defense against issues with autofluorescence and background staining.
Essential Research Reagent Solutions
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| Polymer-based Detection Reagents | Increases sensitivity and avoids issues with endogenous biotin, common in avidin-biotin (ABC) systems [59]. | SignalStain Boost IHC Detection Reagents; provides enhanced sensitivity over biotin-based systems [59]. |
| Charged Slides | Provides superior adhesion for tissue sections, preventing lift-off that causes uneven staining and background [3]. | Essential for techniques like ISH and IHC to prevent pooling of reagents beneath lifting sections [3]. |
| Fresh Xylene / Dewaxing Agents | Complete removal of paraffin wax from FFPE sections is critical for even reagent application and staining [59]. | Incomplete dewaxing causes spotty, uneven background; always use fresh solutions [59]. |
| Validated Fluorophores | Dyes with bright, photostable emission in spectral ranges with low inherent tissue autofluorescence. | Invitrogen Alexa Fluor 647, Alexa Fluor 750; CoraLite 647 [10] [61] [60]. These far-red/NIR dyes are ideal for minimizing interference. |
| Antigen Retrieval Buffers | Reverses formaldehyde-induced cross-links, exposing epitopes for antibody binding. Critical for FFPE tissues [10] [59]. | Sodium citrate (pH 6.0) is common. The retrieval method (microwave, pressure cooker) must be optimized for each antibody [10] [59]. |
Correcting for Edge Artifacts and Inconsistent Reagent Coverage
This technical support center provides targeted troubleshooting guides and FAQs to help researchers resolve common issues of edge artifacts and uneven staining, framed within the broader context of troubleshooting spotty, uneven background staining in research.
Troubleshooting Guides at a Glance
The tables below summarize core diagnostic steps and advanced correction techniques for uneven staining and edge artifacts.
Table 1: Core Troubleshooting Guide for Spotty, Uneven Background Staining
| Potential Problem | Primary Cause | Recommended Solution |
|---|---|---|
| High, Spotty Background [64] | Inadequate deparaffinization of tissue sections. | Repeat experiment with new tissue sections using fresh xylene. [64] |
| High Background [65] | Inadequate blocking of the membrane or slide. | Optimize blocking buffer; use 1-5% BSA or casein; ensure sufficient blocking time (30-60 min). [66] [67] [64] |
| Weak or No Signal [65] | Low antibody concentration or degraded reagents. | Titrate antibodies to find optimal concentration; ensure proper storage and check expiration dates. [65] |
| Uneven Staining [64] | Inadequate washing leaving excess unbound reagents. | Wash membranes 3 times for 5-10 minutes with TBST/PBST after each incubation step. [67] [64] |
| Non-specific Staining [65] | Secondary antibody cross-reactivity. | Include a control slide without primary antibody; use species-specific, cross-absorbed secondary antibodies. [64] [65] |
Table 2: Advanced Techniques for Edge Artifact Correction
| Artifact Type | Detection Method | Correction Algorithm | Demonstrated Efficacy |
|---|---|---|---|
| Edge Artifacts in Doppler Time-of-Flight Velocity Imaging [68] | Self-adaptive gradient threshold applied to five continuous measurements. [68] | Per-pixel gradient-based identification and linear prediction for correction. [68] | 78.5% reduction in average velocity error; 62.7% reduction in RMSE. [68] |
| Boundary Artifacts in Spectral Filtering [69] | Analysis of signal distortion at data boundaries during bandpass filtering. [69] | "Rubber band filter" applying an optimal, iterative padding scheme. [69] | Effective artifact-free filtering demonstrated in spectroscopy and 2D imaging. [69] |
Frequently Asked Questions (FAQs)
What are the most critical steps to prevent uneven background in IHC or western blotting?
Thorough washing and effective blocking are paramount. After any antibody incubation, wash membranes or slides 3-6 times with a buffer like TBST containing a mild detergent (e.g., 0.05% Tween 20) to remove unbound reagents [67] [64]. Follow this with a blocking step using a protein solution (e.g., 1-5% BSA, casein, or normal serum) for 30-60 minutes to occupy any nonspecific binding sites [66] [67].
My positive control is staining well, but my experimental samples have high, uneven background. What should I do?
This indicates your protocol is sound, but your sample may be the issue. First, ensure your sample preparation is consistent. For tissues, complete deparaffinization with fresh xylene is critical [64]. For cells, check for high levels of endogenous biotin (in kidney/liver) or endogenous immunoglobulins. Switch from a biotin-based detection system to a polymer-based system and use appropriate blocking agents like Fc receptor blockers [64] [65].
What are "edge artifacts" and in which techniques are they commonly observed?
Edge artifacts are signal distortions that occur at the boundaries of data, such as the edges of an image or signal window. They are a known challenge in:
- Doppler Time-of-Flight (Do-ToF) Imaging: Caused when a pixel's signal switches between a moving object and a stationary background, creating artifacts in velocity images [68].
- Spectroscopic Data Processing: Introduced by conventional symmetric-padding bandpass filtering methods, which distort the signal at the edges [69].
How can edge artifacts be corrected computationally?
Advanced algorithms can identify and correct these artifacts. For instance, in Do-ToF imaging, a per-pixel, gradient-based method can be used. It models the measurement to acquire gradient features, then employs a self-adaptive gradient threshold to accurately identify artifacts without misidentifying sinusoidal patterns from moving objects. The identified artifact regions are then corrected via linear prediction [68].
Experimental Protocols for Correction and Optimization
Protocol 1: Standardized Western Blotting to Minimize Edge and Background Effects
This protocol is adapted from Thermo Fisher's guidelines for chemiluminescent detection [67].
Materials:
- Transfer Membrane: Nitrocellulose or PVDF.
- Buffers: Transfer buffer, Tris-buffered saline with 0.05% Tween 20 (TBST), Blocking buffer (e.g., 5% non-fat dry milk or commercial blocking buffers).
- Antibodies: Validated primary and HRP-conjugated secondary antibodies.
- Substrate: Chemiluminescent HRP substrate.
Methodology:
- Protein Transfer: After gel electrophoresis, transfer proteins to the membrane using wet or semi-dry transfer. For PVDF membranes, pre-wet in 100% methanol for 30 seconds before equilibration in transfer buffer.
- Post-Transfer Wash: Wash the membrane in deionized water 4 times for 5 minutes each with agitation to remove all transfer buffer salts [67].
- Blocking: Incubate the membrane with a sufficient volume of blocking buffer for 30–60 minutes at room temperature with agitation.
- Primary Antibody Incubation: Dilute the primary antibody in blocking buffer as recommended. Incubate the membrane for 1 hour at room temperature or overnight at 2–8°C with agitation.
- Washing: Wash the membrane 3 times for 10 minutes each with ample TBST to remove all unbound primary antibody.
- Secondary Antibody Incubation: Dilute the HRP-conjugated secondary antibody in buffer. Incubate for 1 hour at room temperature with agitation.
- Final Washing: This step is critical for low background. Wash the membrane 6 times for 5 minutes each with TBST to thoroughly remove any unbound secondary antibodies [67].
- Detection: Incubate with chemiluminescent substrate and image.
Protocol 2: nELISA for High-Plex, Low-Background Protein Profiling
The nELISA (next-generation ELISA) platform is designed to minimize reagent cross-reactivity (rCR), a major source of background in multiplexed assays [70].
- Core Principle: The CLAMP (Colocalized-by-linkage assays on microparticles) method pre-assembles capture and detection antibody pairs on target-specific, DNA-barcoded beads. This spatial separation prevents noncognate antibodies from interacting and forming mismatched complexes that cause background [70].
- Detection Mechanism: Detection antibodies are tethered via flexible single-stranded DNA. Upon target protein binding, a fluorescently labeled DNA oligo uses a toehold-mediated strand displacement to simultaneously untether and label the detection antibody. This "detection-by-displacement" ensures signal is generated only when the correct sandwich complex is present, drastically reducing background [70].
- Workflow:
- Pre-assemble target-specific CLAMP beads.
- Pool beads and add to sample. Target antigens bind.
- Add displacement oligo to release and label bound detection antibodies.
- Wash away unused oligo and unbound antibodies.
- Analyze on a flow cytometer to read both the bead barcode (target identity) and the fluorescent signal (quantification) [70].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Artifact and Background Reduction
| Item | Function | Example Use Cases |
|---|---|---|
| Polymer-Based Detection Reagents [64] | More sensitive and specific than avidin/biotin systems, reducing background from endogenous biotin. | IHC, Flow Cytometry |
| SignalStain Antibody Diluent [64] | Optimized buffer to maintain antibody stability and specificity, preventing aggregation and non-specific binding. | IHC |
| Blocking Buffers (BSA, Casein, Normal Serum) [66] [67] | Proteins that occupy non-specific binding sites on membranes or slides to prevent background staining. | Western Blot, IHC, ELISA |
| Wash Buffer with Tween-20 (TBST/PBST) [67] | Mild detergent in physiologic buffer removes unbound reagents while maintaining target binding. | Western Blot, IHC, ELISA |
| Self-Adaptive Gradient Threshold Algorithm [68] | Computational method to identify and correct edge artifacts in imaging data without misidentifying real patterns. | Doppler Time-of-Flight Imaging |
| Rubber Band Filter [69] | An optimal padding scheme for bandpass filtering that eliminates boundary artifacts in spectral data. | Spectroscopy, Imaging |
| CLAMP Bead Assay [70] | Spatially separated, pre-assembled antibody pairs on barcoded beads to eliminate reagent cross-reactivity in multiplex assays. | High-Plex Protein Profiling (nELISA) |
Validating Your Results: Controls, Analysis, and Protocol Standardization
The Critical Role of Positive and Negative Controls in IHC
FAQs on IHC Controls and Background Staining
What is the primary purpose of controls in IHC experiments?
Controls are essential internal checks that help differentiate true positive signals from artefacts caused by nonspecific binding, autofluorescence, or protocol errors [71]. They strengthen the validity and reproducibility of your findings by verifying that the observed staining is specific to the target antigen and not the result of experimental artifacts [72].
My IHC staining shows spotty, uneven background. What controls can help diagnose this?
A no primary antibody control (secondary antibody only control) is particularly valuable for diagnosing spotty, uneven background [71]. This control involves omitting the primary antibody and incubating the tissue with only antibody diluent, followed by the standard secondary antibody and detection reagents [72]. If background staining persists in this control, it indicates the secondary antibody is binding nonspecifically to tissue components [73] [71]. Inadequate deparaffinization can also cause spotty, uneven background, which would require repeating the experiment with new tissue sections and fresh xylene [73].
How can I confirm my primary antibody is working correctly?
Use a positive tissue control – a tissue known to express your target protein [71] [72]. If staining is observed in this control, your assay is functioning correctly. Lack of staining indicates an issue with your protocol that requires troubleshooting [71]. Always check the antibody's datasheet or Uniprot ID for information on tissues known to express your protein of interest [71].
What control can verify antibody specificity?
An isotype control checks that observed staining isn't caused by non-specific interactions of the antibody with the tissue [71] [72]. This control uses a non-immune antibody of the same class, clonality, and host species as your primary antibody, but with no specificity for your target antigen [71]. It should be used at the same concentration as your primary antibody under identical experimental conditions [72]. A lack of staining in the isotype control confirms your signal is specific [71].
How do I select appropriate control tissues?
For positive controls, select tissues known to express your target protein based on antibody datasheets, published literature, or protein atlas databases [71]. For negative controls, use tissues known not to express the target antigen [72]. Knockdown (KD) and knockout (KO) tissues are excellent negative controls as they significantly reduce or eliminate expression of the target protein [71].
Experimental Protocols for Key IHC Controls
Protocol 1: No Primary Antibody Control (Secondary Antibody Only)
This control assesses nonspecific binding by the secondary antibody [71].
- Section Preparation: Prepare tissue sections following your standard protocol including deparaffinization, rehydration, and antigen retrieval [73].
- Blocking: Block endogenous peroxidases with 3% H₂O₂ in methanol or water for 10 minutes at room temperature [73] [10].
- Serum Blocking: Apply 5-10% normal serum from the secondary antibody species in TBST for 30 minutes to block nonspecific binding [73] [74].
- Omit Primary Antibody: Instead of primary antibody, incubate with antibody diluent alone for the same duration as primary antibody incubation [71] [72].
- Secondary Antibody: Apply your standard secondary antibody and detection reagents [72].
- Detection: Proceed with your standard detection method (DAB, fluorescence, etc.) [71].
- Interpretation: Any resulting signal indicates nonspecific secondary antibody binding requiring optimization of secondary antibody concentration or blocking conditions [71].
Protocol 2: Isotype Control
This control verifies staining specificity when using monoclonal antibodies [71].
- Preparation: Prepare duplicate tissue sections alongside experimental samples.
- Isotype Antibody: Use an antibody of the same isotype, clonality, conjugate, and host species as your primary antibody, but with no specificity for your target [71].
- Concentration: Use the isotype control at the identical concentration as your primary antibody [72].
- Incubation: Incubate tissue with the isotype control antibody instead of specific primary antibody under the same conditions (time, temperature) [71].
- Processing: Process through all subsequent steps (secondary antibody, detection) identically to experimental samples.
- Interpretation: Compare staining between experimental and isotype control sections. Specific staining should be absent in the isotype control [71].
Protocol 3: Absorption Control
This control tests if the primary antibody binds specifically to the antigen of interest [72].
- Antibody Preparation: Incubate your primary antibody overnight at 4°C with a 10-fold molar excess of the immunogen peptide [72].
- Section Preparation: Prepare duplicate tissue sections as usual.
- Application: Apply the pre-absorbed antibody to the control section instead of the primary antibody.
- Processing: Complete all subsequent staining steps identically to the experimental section.
- Interpretation: Little or no staining should be observed compared to the section stained with non-absorbed antibody, confirming antibody specificity [72].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents for IHC Controls and Troubleshooting
| Reagent/Kit | Primary Function | Application in Controls |
|---|---|---|
| Normal Serum [73] [75] | Blocks nonspecific binding | Used in no-primary and isotype controls to prevent false positives |
| Peroxase Blockers (e.g., 3% H₂O₂) [73] [10] | Quenches endogenous peroxidase | Essential for all controls using HRP-based detection |
| Biotin Blocking Kits [73] [74] | Blocks endogenous biotin | Critical for controls with biotin-based detection systems |
| Isotype Control Antibodies [71] [72] | Matches primary antibody isotype | Core reagent for isotype controls to verify specificity |
| Antigen Retrieval Buffers [73] | Unmasks hidden epitopes | Standardizes staining across control and experimental sections |
| Polymer-Based Detection Reagents [73] | Amplifies signal with low background | Reduces background in species-on-species staining scenarios |
Logical Workflow for IHC Control Implementation
IHC Control Types and Their Diagnostic Functions
Table: Comprehensive Guide to IHC Controls
| Control Type | Purpose | Interpretation of Results | Troubleshooting Value for Background Staining |
|---|---|---|---|
| Positive Tissue Control [71] [72] | Verify protocol functionality | Staining confirms procedure works | If positive control fails, indicates systemic protocol issue |
| Negative Tissue Control [71] [72] | Reveal non-specific binding | No staining expected; staining indicates non-specific binding | Identifies antibody cross-reactivity with off-target epitopes |
| No Primary Control [71] [72] | Assess secondary antibody specificity | No staining expected; staining indicates secondary antibody issues | Diagnoses secondary antibody cross-reactivity or detection system problems |
| Isotype Control [71] [72] | Verify primary antibody specificity | Minimal staining expected; pattern should differ from experimental | Confirms observed staining is antigen-specific, not antibody artifact |
| Endogenous Background Control [71] [72] | Identify inherent tissue properties | Documents autofluorescence or endogenous enzyme activity | Distinguishes true signal from tissue autofluorescence in fluorescence IHC |
| Absorption Control [72] | Confirm antigen-antibody specificity | Significant reduction in staining compared to experimental | Validates antibody specificity when non-specific binding is suspected |
Quantitative Image Analysis and Quality Control for Staining Uniformity
Frequently Asked Questions (FAQs) on Staining Issues
Q1: What are the most common staining irregularities that can impact image analysis? Several specific staining irregularities can severely compromise the quality and quantifiability of your images. The most common issues to look for are:
- Edge Effect: This occurs when the outside edge of a tissue section preferentially takes up stain more than the interior, resulting in a ring of non-specific, differential staining around the tissue. This area can produce false-positive or inaccurate data and should be excluded from analysis [76].
- Background Staining: This is non-specific staining that is not associated with the primary target. It can be caused by various factors, including non-specific antibody binding. The use of antibody isotype controls or, for staining with secondary antibodies, control tissue incubated without the primary antibody, can help define and identify this issue [76].
- High Staining Variability: Uneven staining across a tissue section can be caused by uneven tissue fixation, inconsistent application of reagents, problems with an automated stainer, or failing to keep slides flat until they are completely dry. While mildly affected areas can sometimes be excluded via annotation, high variability often renders an image unsuitable for robust quantitative analysis [76].
- Indistinct Nuclei: In many image analysis workflows, cell identification is driven by clear nuclear staining. If nuclei are indistinct, often due to densely packed cellular structures, cell segmentation and the formation of accurate cell objects can be severely compromised [76].
Q2: How can I determine if my staining is too weak or too strong? Both under- and over-staining can lead to significant analytical errors.
- Overstaining: For example, a nucleus overstained with haematoxylin (appearing very dark blue) can be difficult to differentiate from a DAB-labelled positive nucleus (dark brown) and may even mask weakly positive nuclei. Overstaining can also obscure key morphological characteristics [76].
- Understaining: Staining that is too weak can produce false-negative results, as the signal fails to accurately represent the presence and abundance of the target [76]. If the target stain is strongly over or under stained, the image is often not suitable for quantitative analysis until the staining protocol is optimized and repeated.
Q3: What is stain normalization and when should I use it? Stain normalization is a computational method used to standardize the color appearance of histopathology images. It is a powerful tool to minimize color variations caused by different scanning equipment, staining methods, and tissue reactivity. These variabilities can decrease the accuracy of both computer-aided diagnosis and pathologist assessment. Using stain normalization methods, particularly structure-preserving unified transformation-based techniques, has been shown to improve robustness against variability and reproducibility in quantitative studies [77].
Troubleshooting Guide: Spotty and Uneven Background Staining
The following table outlines common problems, their potential causes, and recommended solutions.
| Observed Problem | Potential Causes | Recommended Solutions & Troubleshooting Steps |
|---|---|---|
| Edge Effects [76] | - Rapid drying of reagent edges- Excessive antibody concentration- Insufficient blocking | - Ensure slides are kept flat and in a humidified chamber during staining- Titrate antibodies to optimal concentration- Review and extend blocking step duration |
| High Background Staining [76] | - Non-specific antibody binding- Inadequate blocking- Over-fixation of tissue- Endogenous enzyme activity not quenched | - Include appropriate isotype controls- Optimize blocking serum and duration- Review fixation protocol and timing- Perform endogenous enzyme blocking steps (e.g., peroxidase, phosphatase) |
| Uneven Staining Across Tissue [76] | - Uneven application of reagents- Uneven tissue fixation- Slides not kept flat during drying- Automated stainer errors | - Ensure reagents are applied evenly and fully cover the tissue section- Review fixation process for consistency- Keep slides perfectly horizontal during drying phases- Service and calibrate automated staining instrument |
| Indistinct Nuclear Staining [76] | - Densely packed cellular structures- Under- or over-stained haematoxylin- Poor-quality staining reagents | - Consider using a different nuclear counterstain or adjusting its concentration- Carefully optimize haematoxylin staining time- Use fresh, high-quality reagents |
Quantitative Assessment of Staining Quality
For consistent quantitative analysis, implementing a scoring system for staining quality is essential. The table below adapts a validated scoring system for internal quality control in immunohistochemistry [78]. Each stained slide (including controls and test cases) can be assessed against these criteria.
| Assessment Criteria | Optimal Staining (Score = 2) | Borderline Staining (Score = 1) | Unacceptable Staining (Score = 0) |
|---|---|---|---|
| Staining Intensity [78] | Strong, clear reaction product | Weak but definite reaction | Faint, barely visible, or absent |
| Staining Uniformity [78] | Even staining across all relevant cells/tissue structures | Minor, acceptable variations in intensity | Major, unacceptable unevenness |
| Specificity [78] | Staining only in expected cellular compartments/structures | Faint non-specific staining in unexpected areas | Significant non-specific staining |
| Background [78] | Clean, no background staining | Minimal background that does not interfere with interpretation | Significant background staining that obscures details |
| Counterstaining [78] | Optimal, provides clear contrast without masking primary stain | Acceptable but slightly too weak or too strong | Too weak (no contrast) or too strong (masks primary stain) |
Scoring Interpretation: A total score is calculated by summing the scores from all five criteria (maximum of 10). Slides can be classified as:
- Optimal: 9-10 points
- Borderline/Acceptable: 7-8 points
- Unacceptable: 0-6 points (Investigate and repeat the staining protocol) [78].
Experimental Protocol: Staining Quality Control and Image Analysis Workflow
This protocol provides a detailed methodology for assessing staining uniformity, integrating both laboratory and computational steps.
A. Sample Preparation and Staining
- Tissue Sectioning: Cut tissue sections at a consistent, appropriate thickness (e.g., 4-5 µm) and mount them on charged slides to prevent detachment.
- Control Tissues: Include known positive and negative control tissues on every slide or batch to monitor staining performance [78].
- Staining Protocol: Follow a standardized, validated staining protocol (e.g., IHC or IF) with special attention to the troubleshooting points listed in Section 2. Key steps include:
- Deparaffinization and Antigen Retrieval: Perform consistently across all slides.
- Endogenous Blocking: Block peroxidase, phosphatase, or other relevant endogenous enzymes.
- Protein Blocking: Use a normal serum or protein block from the same species as the secondary antibody to reduce non-specific binding.
- Antibody Incubation: Use titrated, optimal concentrations of primary and secondary antibodies. Apply reagents evenly.
- Counterstaining: Use a standardized, consistent time for haematoxylin or other nuclear counterstains.
B. Whole Slide Imaging
- Scanner Calibration: Ensure the slide scanner is properly calibrated according to the manufacturer's instructions.
- Consistent Settings: Use the same resolution, exposure time, and gain settings for all images within an experiment to allow for valid comparisons [79].
- File Format: Export images in a lossless format, such as TIFF, to prevent the introduction of compression artifacts that can interfere with analysis [79].
C. Quantitative Image Analysis for Uniformity
- Image Pre-processing: If significant color variability exists between slides from different batches, apply a stain normalization algorithm to standardize the color appearance before analysis [77].
- Region of Interest (ROI) Definition: Annotate the areas to be analyzed. Exclude artifacts, tissue folds, and areas with clear edge effects [76].
- Segmentation and Measurement:
- Use image analysis software to segment the stained objects (e.g., cells, nuclei) based on color and intensity thresholds.
- For background assessment, also segment adjacent, non-stained tissue areas.
- Quantitative Metrics Calculation:
- Measure the mean staining intensity and integrated optical density within the segmented objects.
- Calculate the coefficient of variation (CV = Standard Deviation / Mean) for intensity measurements across multiple fields of view or ROIs within the same sample. A low CV indicates high staining uniformity.
- Calculate the signal-to-background ratio (Mean Signal Intensity / Mean Background Intensity).
Workflow Diagram: Staining Quality Control Pathway
The following diagram illustrates the logical workflow for the staining quality control process, from sample preparation to data interpretation.
Staining QC and Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents used in staining and quality control experiments.
| Item | Function / Purpose | Example & Brief Explanation |
|---|---|---|
| Antibody Isotype Controls [76] | To distinguish specific from non-specific antibody binding and identify background staining. | An antibody of the same isotype (e.g., IgG1, IgG2a) but with irrelevant specificity. It should yield no staining in the same tissue under identical conditions. |
| Positive Control Tissues [78] [80] | To verify that the staining protocol worked correctly on a given day. | A tissue section with known, abundant expression of the target antigen. Its staining should be optimal and consistent across experimental batches. |
| Negative Control Tissues [76] | To confirm staining specificity and identify non-specific background. | For IHC with secondary antibodies, a control where the primary antibody is omitted. Any staining observed is non-specific. |
| Protein Blocking Serum | To reduce non-specific binding of antibodies to tissue, thereby minimizing background. | Normal serum from the species in which the secondary antibody was raised. It blocks charged sites and Fc receptors on the tissue. |
| Stain Normalization Software [77] | To computationally minimize color variations between images from different labs, scanners, or staining batches. | Algorithms like structure-preserving color normalization adjust the color distribution of a source image to match a target template, improving analysis robustness. |
| Quantitative Analysis Software | To segment images and extract objective, numerical data on staining intensity and distribution. | Open-source (e.g., ImageJ, QuPath) or commercial software used to measure metrics like mean intensity, CV, and signal-to-background ratio. |
For researchers, scientists, and drug development professionals, the choice of an immunohistochemistry (IHC) detection system is a critical experimental parameter. This decision directly influences the reliability of your data, impacting diagnostic accuracy and research conclusions. Within the context of troubleshooting spotty and uneven background staining, understanding the nuanced performance characteristics—specifically sensitivity and background performance—of each available method is paramount. This guide provides a detailed comparison to help you select the optimal system and rectify common background issues.
FAQs on Detection Systems and Background Staining
What are the main types of IHC detection systems, and how do they differ in protocol?
IHC detection systems can be broadly categorized into direct and indirect methods, with the latter encompassing several more sensitive, multi-step techniques. The primary differences lie in the number of steps, the reagents used, and the underlying mechanism for signal generation and amplification [81].
The workflow above illustrates the fundamental branching point between direct and indirect detection paths. The table below summarizes the core characteristics and procedural steps of the most common systems [81].
| Detection Method | Key Mechanism | Protocol Steps | Key Advantage | Key Disadvantage |
|---|---|---|---|---|
| Direct | Primary antibody is directly labeled with an enzyme. | 1. Incubate with labeled primary antibody.2. Add chromogen. | Fast protocol. | No signal amplification; very low sensitivity. [81] |
| Indirect | Unlabeled primary antibody is detected by a labeled secondary antibody. | 1. Incubate with unlabeled primary antibody.2. Incubate with labeled secondary antibody.3. Add chromogen. | Increased sensitivity and flexibility vs. direct. | Limited signal amplification. [81] |
| PAP | Uses a soluble Peroxidase-Anti-Peroxidase (PAP) complex. | 1. Primary antibody.2. Secondary "bridge" antibody.3. PAP complex.4. Chromogen. | High sensitivity; no chemical conjugation. | Time-consuming; complex reagent setup. [81] |
| ABC | Uses an Avidin-Biotin Complex (ABC) with enzyme. | 1. Primary antibody.2. Biotinylated secondary antibody.3. Pre-formed Avidin-Biotin-Enzyme complex.4. Chromogen. | Very high signal amplification. | High background from endogenous biotin and charged avidin. [81] |
| LSAB | Uses enzyme-labeled Streptavidin instead of Avidin. | 1. Primary antibody.2. Biotinylated secondary antibody.3. Enzyme-labeled Streptavidin.4. Chromogen. | Reduced non-specific background vs. ABC; high sensitivity. | Potential background from endogenous biotin. [81] |
| Polymer-Based | Multiple enzymes and secondary antibodies are conjugated to a polymer backbone. | 1. Primary antibody.2. Enzyme-labeled polymer reagent.3. Chromogen. | High sensitivity, low background, fast two-step protocol. | Can be more expensive; large dextran polymers may have steric issues. [73] [81] |
Why does my staining have a spotty, uneven background, and how can I fix it?
Spotty, uneven background is a common issue, often traced to problems during the initial slide preparation phase. Inadequate deparaffinization is a frequent culprit; residual paraffin wax can repel aqueous solutions and cause uneven antibody binding and staining [73]. The solution is to repeat the experiment with new tissue sections and use fresh xylene to ensure complete wax removal [73].
Other common causes and solutions for high background include [73] [82]:
- Insufficient Blocking: Ensure adequate blocking of non-specific binding sites. Use a blocking buffer like 1X TBST with 5% normal serum for 30 minutes before adding the primary antibody. For biotin-rich tissues (e.g., liver, kidney) using a biotin-based system, perform a specific biotin block [73].
- Endogenous Enzyme Activity: With HRP-based systems, endogenous peroxidases in the tissue can produce background. Quench slides in a 3% H₂O₂ solution for 10 minutes before the primary antibody incubation [73].
- High Antibody Concentration: An overly concentrated primary or secondary antibody can lead to non-specific binding. Titrate your antibodies to find the optimal, specific dilution [73] [82].
- Inadequate Washing: Unbound antibodies must be thoroughly removed. Wash slides 3 times for 5 minutes with a buffered solution like TBST after primary and secondary antibody incubations [73].
How do detection systems compare in terms of sensitivity and background?
Sensitivity refers to the system's ability to detect low levels of a target antigen, while background performance relates to its propensity for non-specific staining. These two factors are often a trade-off, but technological advances have led to systems that excel in both.
The following diagram illustrates the general relationship between the major detection methods in terms of their sensitivity and associated background risk.
Building on this conceptual overview, the table below provides a qualitative comparison of the specific systems based on technical literature [81] [23].
| Detection Method | Relative Sensitivity | Background Performance & Key Risks |
|---|---|---|
| Direct | Very Low | Generally low background, but signal is often too weak to be useful. |
| Indirect | Low | Moderate background risk from cross-reactive secondary antibodies. |
| PAP | Medium | Reduced background staining; allows for higher primary antibody dilution. [81] |
| ABC | High | High risk. Background from endogenous biotin and electrostatic (charge-based) non-specific binding of avidin. [81] |
| LSAB | High | Medium risk. Reduced avidin-related issues, but background from endogenous biotin remains a concern. [81] |
| Polymer-Based | High | Low risk. Minimal background as it avoids endogenous biotin and Fc-receptor mediated binding. Superior signal-to-noise ratio. [73] [81] |
Quantitative studies support these comparisons. For instance, one study noted that polymer-based detection systems are more sensitive than traditional avidin/biotin-based systems, providing enhanced sensitivity and more robust staining with lower background [73].
Troubleshooting Guide: A Systematic Approach to High Background
When faced with high background staining, a systematic approach to troubleshooting is essential. The following workflow guides you through the key investigative steps and corrective actions.
The Scientist's Toolkit: Key Research Reagent Solutions
Having the right reagents is fundamental to achieving clean, high-quality results. Below is a table of essential materials used in IHC, along with their critical functions in optimizing sensitivity and minimizing background.
| Research Reagent / Solution | Function |
|---|---|
| Antigen Retrieval Buffer (e.g., Citrate pH 6.0, Tris-EDTA pH 9.0) | Reverses formaldehyde-induced crosslinks to unmask hidden epitopes, which is crucial for signal intensity in FFPE tissues. [73] [23] |
| SignalStain Antibody Diluent | Optimized diluent to maintain antibody stability and reduce non-specific binding, often superior to generic diluents like TBST/5% NGS. [73] |
| Normal Serum (e.g., from the same species as the secondary antibody) | Blocks non-specific binding sites on the tissue to reduce background staining. [73] |
| Hydrogen Peroxide (H₂O₂) Blocking Solution | Quenches endogenous peroxidase activity in tissues, preventing false-positive signals in HRP-based detection systems. [73] |
| Biotin Blocking Kit | Essential when using ABC or LSAB methods; blocks endogenous biotin in tissues like liver and kidney to prevent high background. [73] [81] |
| Polymer-Based Detection Kits (e.g., SignalStain Boost) | Provides high-sensitivity detection with minimal background by avoiding endogenous biotin and utilizing a compact polymer for efficient labeling. [73] [81] [23] |
Selecting the right detection system is a fundamental decision that balances sensitivity and specificity. For most modern applications, particularly in diagnostic and drug development settings where reproducibility is key, polymer-based systems offer a superior profile of high sensitivity and low background. When troubleshooting spotty or uneven staining, a methodical approach—beginning with slide preparation and moving through blocking, antibody incubation, and washing—will most efficiently lead to a resolution and ensure the reliability of your experimental data.
Implementing QA/QC Measures for Batch-to-Batch Consistency
This technical support center resource provides troubleshooting guides and FAQs to help researchers address specific issues related to batch-to-batch consistency, with a particular focus on troubleshooting spotty, uneven background staining in experiments like immunohistochemistry (IHC).
Troubleshooting Guides
Troubleshooting Spotty, Uneven Background Staining
Problem: My experiment shows spotty or uneven background staining. What could be the cause and how can I fix it?
Spotty, uneven background is a common issue in immunostaining, often traced to sample preparation or detection systems [83] [84].
Primary Causes and Solutions:
- Inadequate Deparaffinization: Spotty background in IHC often comes from incomplete deparaffinization [83]. Solve this by repeating the experiment with fresh xylene and new tissue sections [83].
- Fixation Issues: Over-fixation or under-fixation of tissue samples can increase background and autofluorescence [84]. Optimize fixative reagents, incubation times, and tissue-to-fixative ratios for your specific tissue type [84].
- Detection System Interference: Endogenous enzymes in tissues (e.g., liver, spleen, kidney) can react with detection system substrates, causing background [84]. Use appropriate blocking steps:
Systematic Diagnostic Approach:
- Perform a "Deletion Control": Run the staining protocol but omit the primary antibody. Significant staining indicates non-specific binding from the secondary antibody or detection reagents [84].
- Check Secondary Antibody: Include a control slide stained only with the secondary antibody. Staining suggests secondary antibody cross-reactivity with endogenous immunoglobulins in the tissue [83].
Addressing Batch-to-Batch Inconsistency in Reagents
Problem: My experimental results vary between batches, even when using the same protocol. How can I improve consistency?
Batch inconsistencies often stem from variations in raw materials, process controls, or undocumented protocol changes [85].
Implement Rigorous Raw Material Testing:
Establish Standardized Production Procedures:
Enhanced Process Control Monitoring:
Frequently Asked Questions (FAQs)
Q1: What are the essential controls for validating IHC staining consistency?
Always use appropriate positive and negative controls [83]. Control slides with formalin-fixed, paraffin-embedded (FFPE) cell pellets containing both positive and negative samples help assess staining reagent performance and method validity [83]. For phospho-specific antibodies, include a high-expressing positive control to confirm the antibody and procedure are working [83].
Q2: How can I prevent non-specific background when using species-on-species staining?
When using primary antibodies raised in the same species as your tissue (e.g., mouse antibody on mouse tissue), use species-specific blocking reagents [84]. For mouse-on-mouse staining, use M.O.M. (Mouse on Mouse) Blocking Reagent [84]. For other species, add 2% or higher concentration of normal serum from the same species as the tissue to the secondary antibody diluent [84].
Q3: What QA documentation is crucial for maintaining batch-to-batch consistency?
Essential documentation includes [86]:
- Standard Operating Procedures (SOPs): Detailed instructions for consistent processes
- Batch Records: Complete documentation of each production run
- Quality Manual: High-level quality policies and objectives
- Process Validation Reports: Evidence that processes consistently deliver desired results
- Training Records: Staff competency documentation
Q4: Are there updated regulatory guidelines for ensuring batch uniformity?
Yes, the FDA has recently issued new guidelines. "Considerations for Complying with 21 CFR 211.110" (January 2025) describes considerations for ensuring batch uniformity and drug product integrity, emphasizing risk-based strategies for in-process sampling and testing [87]. The guidance also covers using advanced manufacturing technologies like real-time quality monitoring and process analytical technologies (PAT) [87].
Experimental Protocols for Consistent Staining
Protocol: Optimized Antigen Retrieval for Consistent IHC
Antigen retrieval is critical for consistent staining results, especially in FFPE tissues where fixation creates protein cross-links that mask antigen targets [83].
- Recommended Method: Use microwave oven-based retrieval for most applications [83]. For some tissues or antigens, a pressure cooker may provide enhanced signals [83]. Water bath methods are not recommended [83].
- Buffer Preparation: Always prepare fresh 1X antigen retrieval solutions daily [83]. Use the specific buffer recommended on the antibody datasheet.
- Validation Steps:
- Test multiple antigen retrieval methods with a known positive control
- Compare signal intensity and background across methods
- Document the optimal method in your SOPs
Protocol: Antibody Titration for Optimal Signal-to-Noise Ratio
Oversaturation of the target epitope with primary antibody is a common cause of high background [84].
Procedure:
- Prepare a series of antibody dilutions around the manufacturer's recommendation
- Use a positive control tissue with known target expression
- Process all slides simultaneously using the same reagents
- Evaluate both specific staining and background levels
Optimal Concentration: The best concentration often yields highly specific staining with minimal background and may be less concentrated than manufacturer recommendations [84].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Application |
|---|---|
| SignalStain Boost IHC Detection Reagents (#8114, #8125) | Polymer-based detection system offering enhanced sensitivity over biotin-based systems [83]. |
| TrueVIEW Autofluorescence Quenching Kit | Reduces background from tissue components (collagen, elastin, RBCs) and aldehyde fixation [84]. |
| M.O.M. (Mouse on Mouse) Blocking Reagent | Essential for blocking non-specific background in species-on-species staining [84]. |
| BLOXALL Endogenous Blocking Solution | Blocks endogenous peroxidase and alkaline phosphatase activity simultaneously [84]. |
| Normal Goat Serum (#5425) | Used in blocking buffer (5% in TBST) for 30 minutes to reduce non-specific antibody binding [83]. |
| Fresh Xylene | Critical for complete deparaffinization; use fresh to prevent spotty background [83]. |
| TBST (#9997) | Washing buffer; adequate washing (3x5 minutes after each step) is crucial for low background [83]. |
Quantitative Data for QA/QC Implementation
Key Quality Tests for Batch Consistency
| Test Type | Specific Measurements | Target Specifications |
|---|---|---|
| Raw Material Testing | Purity analysis, Moisture content, Particle size distribution | Meet predefined standards before use [85] |
| In-Process Testing | Viscosity, Density, pH, Spectroscopic analysis | Verify composition and identity during production [85] |
| Final Product Testing | Stability, pH/conductivity, Contaminant analysis | Meet all quality specifications before batch release [85] |
| Dose Recovery | Flush volume studies for enteral administration | >90% recovery; 1-3mL for neonatal patients [88] |
Experimental Workflow Diagrams
QA System for Batch Consistency
Leveraging Automated Staining Systems for Reproducibility
Automated staining systems are powerful tools for standardizing experiments in research and drug development. However, achieving consistent, high-quality results without background issues like spotty or uneven staining requires a deep understanding of both the technology and the underlying biology. This guide provides targeted troubleshooting and FAQs to help you identify and resolve the specific challenges that can compromise reproducibility in your experiments.
Troubleshooting Guide: Spotty & Uneven Background Staining
Spotty or uneven background staining is a common frustration that can obscure results and invalidate data. The table below outlines the primary causes and their solutions.
| Problem Cause | Diagnostic Clues | Recommended Solution |
|---|---|---|
| Inadequate Deparaffinization [89] | Spotty, uneven background staining. | Repeat the experiment with new tissue sections and fresh xylene. [89] |
| Membrane or Tissue Drying [12] [90] | Uneven or blotchy background; can cause irreversible non-specific binding. | Ensure tissue sections remain covered in liquid throughout the staining procedure; use a humidity chamber for long incubations. [89] [12] [90] |
| Contaminated Reagents or Surfaces [90] | Speckles across the membrane or slide. | Use clean forceps; rinse incubation trays with methanol and water to remove residual dyes. [90] |
| Inconsistent Reagent Coverage [12] | Patchy staining where some tissue areas are affected more than others. | Ensure reagents fully cover the tissue section; use a humidified chamber during incubations. [12] |
| Improper Blocking [58] [12] | High, uniform background across the tissue. | Use appropriate blocking sera (e.g., from the same species as your secondary antibody); for IHC, block with normal serum and consider peroxidase or biotin blocks. [58] [12] |
Essential Protocol: Optimized Blocking for Flow Cytometry
Preventing non-specific binding in flow cytometry often requires a dedicated blocking step. The following protocol is adapted for high-parameter assays involving human or murine cells [58].
Materials
- Mouse serum (e.g., Thermo Fisher, cat. no. 10410)
- Rat serum (e.g., Thermo Fisher, cat. no. 10710C)
- Tandem stabilizer (e.g., BioLegend, cat. no. 421802)
- Brilliant Stain Buffer (e.g., Thermo Fisher, cat. no. 00‐4409‐75) or BD Horizon Brilliant Stain Buffer Plus
- FACS buffer
Procedure
- Prepare Blocking Solution: Create a mix containing mouse serum, rat serum, and tandem stabilizer diluted in FACS buffer. A common formulation is 300 µl mouse serum, 300 µl rat serum, and 1 µl tandem stabilizer, brought to a 1 ml final volume with FACS buffer. [58]
- Incubate with Cells: Resuspend your cell pellet in the blocking solution (e.g., 20 µl). Incubate for 15 minutes at room temperature in the dark. [58]
- Proceed with Staining: Without washing, add your surface antibody master mix, which should also contain Brilliant Stain Buffer to prevent dye-dye interactions, and continue with your standard staining protocol. [58]
Frequently Asked Questions (FAQs)
What should I do if my automated stainer stops mid-cycle?
First, check for any error messages on the display panel. Inspect the power connections to ensure there are no interruptions. If no obvious issues are found, restart the machine. [91]
Our automated H&E staining is inconsistent, but manual staining works perfectly. Why?
A key difference is in how reagents are applied. Manual staining involves varied force that breaks the surface tension on slides more effectively. Automated stainers move slides in a single plane. The solution is to optimize the timing for the automated system; a 10-dip manual step may require 30 seconds on a machine. Using a weaker concentration of a reagent (like 0.5% acid alcohol instead of 1%) for a very short duration on the machine can also replicate a quick "dip." [92]
How often should I calibrate my automated slide stainer?
Follow the manufacturer's guidelines for routine calibration. Additionally, calibration checks are recommended after any major maintenance procedure, when introducing new reagents or protocols, and whenever inconsistent staining results are suspected. [91]
Can using non-compatible reagents cause errors?
Yes. Incompatible reagents can lead to poor staining quality and even damage the staining machine. Always verify that the reagents are compatible with your specific equipment by consulting supplier guidelines and conducting small-scale tests when introducing new reagents. [91]
The Scientist's Toolkit: Key Research Reagent Solutions
The right reagents are fundamental to preventing staining artifacts and ensuring reproducible data.
| Reagent | Function & Rationale |
|---|---|
| Normal Sera (e.g., Rat, Mouse) [58] | Used in blocking buffers to occupy non-specific binding sites, particularly Fc receptors, on cells. This reduces background staining in flow cytometry and IHC. |
| Tandem Stabilizer [58] | Prevents the degradation of tandem dye conjugates, which can break down and cause erroneous signals in other detection channels. |
| Brilliant Stain Buffer [58] | Essential for panels containing polymer dyes (e.g., Brilliant Violet). It prevents dye-dye interactions that cause false-positive signals and high background. |
| Polymer-Based Detection Reagents [89] | Used in IHC as a more sensitive and specific alternative to biotin-based systems. They eliminate background from endogenous biotin present in tissues like liver and kidney. |
| SignalStain Antibody Diluent [89] | An optimized diluent for primary antibodies in IHC. Using the correct diluent, rather than a generic buffer, can dramatically improve the signal-to-noise ratio. |
| Phosphate-Buffered Saline (PBS) with Tween-20 [12] | A common wash buffer. The detergent Tween-20 (typically at 0.05-0.1%) helps reduce hydrophobic interactions and washes away unbound antibody, lowering background. |
Experimental Workflow for Troubleshooting Staining Problems
The following diagram outlines a systematic approach to diagnosing and resolving spotty or uneven background staining.
Guidelines for Data Sharing and Multi-Institutional Harmonization
FAQs: Troubleshooting Spotty and Uneven Background Staining
Q1: What are the primary causes of spotty, uneven background staining in IHC experiments?
The most common causes are inadequate deparaffinization of tissue sections and issues related to antibody dilution or cross-reactivity [94] [95]. Incomplete deparaffinization leaves residual paraffin wax on the slide, which prevents uniform reagent contact with the tissue, leading to a spotty appearance. Furthermore, using an incorrect antibody diluent or a secondary antibody that cross-reacts with endogenous immunoglobulins in the sample can cause high, uneven background [94].
Q2: How can I resolve issues with spotty staining from inadequate deparaffinization?
The solution is to repeat the experiment with new tissue sections and use fresh xylene for deparaffinization [94] [95]. Increasing the deparaffinization time can also ensure all wax is thoroughly removed. Always handle one slide at a time to prevent sections from drying out, as dried tissues are another common cause of staining artifacts [95].
Q3: My positive control stains well, but my experimental tissue has a high, uneven background. What does this indicate?
This typically indicates a problem specific to the experimental tissue sample rather than a failure of the core protocol. Likely causes include:
- Endogenous enzyme activity: Endogenous peroxidases or phosphatases in the tissue are active and producing signal [10].
- Endogenous biotin: Especially prevalent in tissues like liver and kidney, endogenous biotin can bind to avidin-biotin-based detection systems, creating a high background [94] [10].
- Insufficient blocking: The non-specific protein block was not effective for that particular tissue type.
Q4: What steps can I take to prevent nonspecific antibody binding causing high background?
A multi-faceted approach is often needed:
- Optimize antibody concentration: Titrate your primary antibody, as a concentration that is too high is a frequent cause of non-specific binding and background [95].
- Use the correct diluent: Always use the antibody diluent recommended on the product datasheet, as it contains specific components to minimize non-specific interactions [94].
- Ensure proper blocking: Block with 1X TBST with 5% Normal Goat Serum for 30 minutes prior to primary antibody incubation [94]. For challenging tissues, increasing the serum concentration to 10% may be necessary [10].
- Run a negative control: Always include a control slide stained without the primary antibody to confirm whether the secondary antibody is the source of the background [94].
Q5: How does the detection system influence background staining?
Biotin-based detection systems can interact with endogenous biotin in tissues, leading to high background. Switching to a polymer-based detection system is recommended, as they are more sensitive and do not rely on biotin, thus eliminating this source of noise [94]. Polymer-based systems also generally provide enhanced sensitivity compared to avidin/biotin-based systems.
Troubleshooting Guide: Spotty and Uneven Background Staining
The table below outlines specific issues and validated solutions to resolve spotty and uneven background staining.
| Problem | Possible Cause | Recommended Solution | Key Experimental Protocol |
|---|---|---|---|
| Spotty, Uneven Staining | Inadequate deparaffinization [94] [95] | Use fresh xylene; increase deparaffinization time; use new tissue sections. | Deparaffinize slides by immersing in fresh xylene, 2 changes for 10 minutes each. Rehydrate through graded ethanol series to water. |
| High Uniform Background | Primary antibody concentration too high [95] | Titrate the antibody to determine optimal concentration; incubate at 4°C overnight. | Perform a checkerboard titration assay with antibody dilutions (e.g., 1:50, 1:100, 1:200, 1:500) on a control tissue to find the ideal signal-to-noise ratio. |
| High Background (Endogenous Enzymes) | Endogenous peroxidase or phosphatase activity [94] [10] | Quench with 3% H2O2 in methanol/water for 10 min (peroxidase) or levamisole (phosphatase). | After deparaffinization and rehydration, incubate slides in 3% H2O2 in methanol for 10 minutes at room temperature. Rinse thoroughly with distilled water and buffer. |
| High Background (Endogenous Biotin) | Endogenous biotin binding to detection system [94] [10] | Use a polymer-based detection system; or perform a biotin block after standard blocking. | After blocking, sequentially apply avidin solution (15-20 min), rinse, then biotin solution (15-20 min) to saturate binding sites, per commercial kit instructions. |
| Non-specific Staining | Secondary antibody cross-reactivity or nonspecific binding [94] [10] | Include a negative control (no primary); use a secondary antibody pre-adsorbed against the sample species; increase blocking serum to 10%. | Block tissue with 10% normal serum from the host species of the secondary antibody for 1 hour at room temperature to occupy non-specific sites. |
| Uneven Background | Tissue drying during procedure [95] | Ensure tissue sections remain covered in liquid at all times during the staining procedure. | Perform all incubation steps in a humidified chamber to prevent evaporation and tissue drying. |
| Mouse-on-Mouse Background | Secondary antibody binding to endogenous IgG in mouse tissue [94] | Use an anti-mouse secondary specifically validated for mouse-on-mouse staining, or switch to a rabbit primary antibody. | Use a polymer-based detection reagent specifically formulated for mouse tissue (e.g., MOM kits) to minimize background. |
Experimental Protocol for Resolving High Background Staining
This detailed protocol provides a step-by-step methodology to systematically identify and eliminate the causes of high background staining.
Materials and Pre-Start Checklist
- Freshly cut tissue sections (or slides stored at 4°C)
- Fresh xylene and ethanol series
- 3% Hydrogen Peroxide (H2O2) in methanol
- Blocking serum (e.g., Normal Goat Serum)
- Primary antibody and recommended diluent
- Polymer-based detection kit (e.g., SignalStain Boost IHC Detection Reagents)
- Washing buffer (e.g., 1X TBST)
Procedure
Deparaffinization and Rehydration:
- Immerse slides in fresh xylene for 10 minutes. Repeat with a second fresh xylene bath for 10 minutes.
- Hydrate through a series of ethanol: 100% (twice), 95%, 70%, each for 5 minutes.
- Rinse gently with distilled water.
Antigen Retrieval:
- Perform Heat-Induced Epitope Retrieval (HIER) using a microwave oven or pressure cooker with the appropriate buffer (e.g., 10mM Sodium Citrate, pH 6.0) as recommended for your specific antibody [94].
Endogenous Peroxidase Blocking:
Blocking:
- Apply enough 1X TBST with 5% normal serum to cover the tissue. Incubate for 30 minutes at room temperature in a humidified chamber [94].
Primary Antibody Incubation:
- Dilute the primary antibody in the manufacturer's recommended diluent to the optimized concentration.
- Apply to the tissue and incubate overnight at 4°C in a humidified chamber.
Washing:
- Wash slides 3 times for 5 minutes each with 1X TBST with gentle agitation [94].
Detection:
- Apply polymer-based HRP-conjugated secondary antibody (e.g., SignalStain Boost) for 30 minutes at room temperature.
- Repeat the washing step as above (3 x 5 min with TBST).
Chromogenic Development and Counterstaining:
- Apply DAB substrate and monitor development under a microscope. Stop the reaction by immersing in water once optimal signal is achieved.
- Counterstain with hematoxylin, dehydrate, clear, and mount with a coverslip.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Material | Function in IHC Protocol |
|---|---|
| Fresh Xylene | Essential solvent for complete removal of paraffin wax from FFPE tissue sections to prevent spotty staining [94] [95]. |
| SignalStain Antibody Diluent | A specialized buffer used to dilute the primary antibody; its composition minimizes non-specific ionic interactions and stabilizes the antibody, reducing background [94]. |
| Normal Goat Serum | A protein-rich solution used for blocking to occupy non-specific binding sites on the tissue, preventing antibodies from sticking where they shouldn't [94]. |
| Polymer-Based Detection System | A sensitive detection method (e.g., SignalStain Boost) that does not rely on the avidin-biotin complex, eliminating background from endogenous biotin [94]. |
| Sodium Borohydride | A chemical treatment used to reduce autofluorescence caused by aldehyde fixation, particularly in fluorescent IHC protocols [10]. |
| Heat-Induced Epitope Retrieval (HIER) Buffer | A buffer (e.g., Sodium Citrate, pH 6.0) used to break protein cross-links formed during formalin fixation, thereby "unmasking" antigens for antibody binding [94] [10]. |
Experimental Workflow and Data Harmonization Strategy
The following diagram illustrates the integrated workflow for troubleshooting spotty background staining and the parallel process for multi-institutional data harmonization, which is critical for validating findings across studies.
Key Principles for Data Sharing and Harmonization in Multi-Institutional Research
Effective troubleshooting of technical artifacts like spotty staining is the first step in generating reliable data. For multi-institutional studies, sharing these validated protocols is crucial for data harmonization. Harmonization allows for the comparison and combination of datasets from different sources by addressing:
- Syntax: Standardizing data formats (e.g., consistent file types for digital slide images) [96].
- Structure: Ensuring variables are organized in a uniform conceptual schema across labs (e.g., how staining intensity is scored) [97].
- Semantics: Defining the intended meaning of terms and symbols to ensure all researchers use the same definitions (e.g., a "positive stain") [96].
Adopting Common Data Elements (CDEs) for reporting IHC experimental parameters and outcomes, as seen in consortia like NHLBI CONNECTS, promotes the creation of Findable, Accessible, Interoperable, and Reusable (FAIR) datasets [97]. This structured approach to both experimentation and data management ensures that research findings are robust, reproducible, and capable of accelerating scientific discovery.
Conclusion
Achieving consistent, low-background IHC staining is fundamental for generating reliable data in biomedical research and drug development. By understanding the root causes of spotty staining, implementing methodologically sound protocols, applying systematic troubleshooting, and rigorously validating results with appropriate controls, researchers can significantly enhance the quality and reproducibility of their work. The future of IHC lies in the adoption of standardized, automated protocols and advanced multiplexing techniques, which will further improve data robustness and accelerate the translation of findings into clinical applications. Mastering these principles ensures that staining artifacts no longer compromise critical research outcomes.
References
- 1. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopmF4Y87-Kn2b63lZmiJW-qhHcX4G6DyKMRUFjWUGnDm1MiceYK]
- 2. H&E Basics Part 4: Troubleshooting H&E [https://www.leicabiosystems.com/us/knowledge-pathway/he-basics-part-4-troubleshooting-he/]
- 3. Steps to Better ISH Staining [https://www.leicabiosystems.com/us/knowledge-pathway/steps-to-better-ish/]
- 4. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooW2yI2qnePheaqtgZY3Oc6qghmMIpdRCuD7oPFtkhwDb0dknCM]
- 5. Troubleshooting Immunohistochemistry [https://www.nsh.org/blogs/alisha-yocum/2023/04/13/troubleshooting-ihc]
- 6. Dot to dot: Troubleshooting spotty or patchy western blots [https://www.arp1.com/blog/post/dot-to-dot-troubleshooting-spotty-or-patchy-western-blots.html]
- 7. Evaluation of histomorphometric changes in tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5406822/]
- 8. Common Problems with Sectioning — Research [https://plantscience.psu.edu/research/labs/roots/methods/methods-info/root-anatomy/common-problems-with-sectioning]
- 9. Comparative analysis of fixation and embedding ... [https://www.sciencedirect.com/science/article/pii/S1532045617302089]
- 10. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 11. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopOv00NgnAwPx9qYnCXxtEQBlpnAg-ASTUppSOrIgwfZW-Yv6Zd]
- 12. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 13. Surface patches induce nonspecific binding and phase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10104583/]
- 14. Non-specific binding of antibodies in immunohistochemistry [https://www.nature.com/articles/srep00028]
- 15. Western blot troubleshooting: high background - Blog [https://www.arp1.com/blog/post/western-blot-troubleshooting-high-background.html]
- 16. Nonspecific interactions in biomedical applications [https://www.sciencedirect.com/science/article/abs/pii/S1359029419301001]
- 17. The Curious Case Of The Staining That Went Wrong [https://vectorlabs.com/blog/the-curious-case-of-the-staining-that-went-wrong/?srsltid=AfmBOorW1mkos0T6-e5VCXq5omMZhJir4WPBoL-jMt0iK_TTTIcv4h6O]
- 18. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopkSwGkCkOYlyhEQ9REXtE-TnjmJnNtirp0yJaRC_ubrOz6sqAe]
- 19. H&E Staining Overview: A Guide to Best Practices [https://www.leicabiosystems.com/us/knowledge-pathway/he-staining-overview-a-guide-to-best-practices/]
- 20. A review of artifacts in histopathology - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6097380/]
- 21. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooN_J90A_2PayZxq2jXo6886YQRW0NKThxlqNDO81Ht3sWEPL1b]
- 22. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoq_RwVrbaXKN7oqC7s-uwHqplOCQYUnEr9adtT34D23ej_QW4dM]
- 23. A Guide to Better IHC Staining: Steps, Troubleshooting, ... [https://www.celnovte.com/solution/a-guide-to-better-ihc-staining-steps-troubleshooting-and-optimization/]
- 24. Troubleshooting Tips for Fluorescence Staining [https://biotium.com/tech-tips-protocols/troubleshooting-tips-for-fluorescence-staining/]
- 25. Background Staining In IHC And IF [https://vectorlabs.com/blog/my-staining-didnt-work-part-1-background-staining-in-ihc-and-if/?srsltid=AfmBOoqgefy1skIrWyjHqi-JLmaQG94t_sD96XxXBRkm1OBE4tXyyHoq]
- 26. Learn how to Remove Autofluorescence from your ... [https://www.leica-microsystems.com/science-lab/life-science/learn-how-to-remove-autofluorescence-from-your-confocal-images/]
- 27. Cell and Tissue Fixation 101- Top Tips For Protocol ... [https://bitesizebio.com/13459/cell-fixation-101-top-tips-for-protocol-optimization/]
- 28. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoq48KNRz1f9RNs-3x_ERPrM-v62LneIN3IdjoCRiACu4dA1l-cl]
- 29. Epitope Retrieval - Pretreatment [https://www.cellmarque.com/troubleshooting/pretreatment/epitope-retrieval]
- 30. of Selection pH by the isoelectric point of the buffer for the... antigen [https://link.springer.com/article/10.1007/s00418-009-0635-8]
- 31. IHC antigen retrieval protocol [https://www.abcam.com/en-us/technical-resources/protocols/ihc-antigen-retrieval]
- 32. Optimizing HIER Antigen Retrieval for IHC [https://www.bosterbio.com/blog/post/protocol-for-optimizing-hier-antigen-retrieval-conditions?srsltid=AfmBOoooDxvEIPvDDbmm27qR5fRNWPxgVIMnepDXKsF0EMpEc0LyNUww]
- 33. Antigen Retrieval Methods [https://www.rndsystems.com/resources/protocols/antigen-retrieval-methods]
- 34. Background Staining In IHC And IF | Vector Labs [https://vectorlabs.com/blog/my-staining-didnt-work-part-1-background-staining-in-ihc-and-if/?srsltid=AfmBOopDtjOorQORospI-Zusbq8G51kRAgXVuQ7MmM1qfzUo838luHHy]
- 35. IHC Blocking Non-Specific Binding [https://www.bio-techne.com/applications/imaging/immunohistochemistry/blocking-non-specific-binding]
- 36. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqytLmxsJA3ZOnuo2yLHIwxBySA7I7xqbuorHzzo6o1w4A6rQaX]
- 37. Methods to Block Endogenous Detection [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/methods-block-endogenous-detection.html]
- 38. Basics of the Blocking Step in IHC [https://www.nsh.org/blogs/natalie-paskoski/2021/02/19/basics-of-the-blocking-step-in-ihc]
- 39. The Importance of Signal-to-Noise [https://www.sepscience.com/hplc-solutions-4-the-importance-of-signal-to-noise-7709]
- 40. Antibody Dilution Recommendations | PhosphoSolutions [https://www.antibodiesinc.com/blogs/news/antibody-dilution-recommendations-what-you-need-to-know?srsltid=AfmBOoo6wQUc-ehSE60Z7G8R_Fgyvz6zGNsBd4FIF5pQPrTjfYrW3v_K]
- 41. Antibodies Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/antibodies-immunoassays-support-center/antibodies-support/antibodies-support-troubleshooting.html]
- 42. Assay Diluent Optimization Pack | 958 [https://www.antibodiesinc.com/products/assay-diluent-optimization-pack-958?srsltid=AfmBOopyh4a65RnwyfdNvGfnwZZzL6OmCbuIaFrbuBqUApWfU_8bl-nG]
- 43. Immunofluorescence (IF) Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/if-troubleshooting-guide?srsltid=AfmBOoonwjPT5cTc0vljQ1rIslTe6TygKKe3lUw3uFJvm0MVq3o8ubTf]
- 44. Protein Stains Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/protein-electrophoresis-western-blotting-support-center/protein-stains-support/protein-stains-support-troubleshooting.html]
- 45. Immunofluorescence: Antibody Dilution and Incubation ... [https://blog.cellsignal.com/successful-immunofluorescence-antibody-dilution-and-incubation]
- 46. Spike and Recovery and Linearity of Dilution Assessment [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/spike-recovery-linearity-assessment.html]
- 47. What Are the Common Problems in Immunohistochemistry ... [https://www.celnovte.com/solution/what-are-the-common-problems-in-immunohistochemistry-staining/]
- 48. Improving the Sensitivity of Traditional Western blotting via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7036291/]
- 49. Detection Systems in Immunohistochemistry [https://www.intechopen.com/chapters/64808]
- 50. Comparison of two polymer-based immunohistochemical ... [https://pubmed.ncbi.nlm.nih.gov/17204059/]
- 51. Western Blot Troubleshooting [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-gel-electrophoresis-information/western-blot-troubleshooting.html]
- 52. Help! Why do my Western blots look terrible? [https://azurebiosystems.com/blog/help-why-do-my-western-blots-look-terrible/]
- 53. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOor6uFG5v1Q62UGWL-OWjoAwekHkB2Mx6DFVaQsBJ0qpEGfIzyLu]
- 54. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOooKqwh1oEewKn-_cAiJO_cgb-eXmYg5ATBC5VBy7N9bE8io6LDV]
- 55. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOor8H8oTdo77kjYeo9QKiAiJWNrDYPhNKVo8rwtnF7rsp2Xx9Usv]
- 56. Solutions to immunoassay interference, cross reactivity and ... [https://www.gyrosproteintechnologies.com/spinblog/immunoassay-interference-crossreactivity-challenges]
- 57. 7 Tips for Optimizing Your Flow Cytometry Experiments [https://www.bdbiosciences.com/en-us/learn/science-thought-leadership/blogs/optimizing-tips-flow-cytometry-experiments]
- 58. Optimization of the Blocking and Signal Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462741/]
- 59. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOorumE8GkxkwLMgoq8ojv_BZTegUmFgObqo7CpW6vZ3XNeEI1txP]
- 60. Autofluorescence can interfere with flow cytometry imaging [https://www.bdbiosciences.com/en-us/learn/science-thought-leadership/blogs/Autofluorescence-imaging]
- 61. How to reduce autofluorescence [https://www.ptglab.com/news/blog/how-to-reduce-autofluorescence/?srsltid=AfmBOoolOV4g411sU5hMcLEoeXx1MUxa6i2iACOc1_x9rAaZlidDwKLz]
- 62. Lipofuscin-like autofluorescence within microglia and its ... [https://www.nature.com/articles/s41467-023-42809-y]
- 63. Spectral Flow Cytometry: The Current State and Future of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12193525/]
- 64. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOorWOJw0VTirrAdR_VtK3AlB4jHR2lqhGwcJU4lLUbwYQpjZj66A]
- 65. Troubleshooting Flow Cytometry Issues [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-troubleshooting?srsltid=AfmBOopq2OaCSWSSYpBSn9WwZY6w7YncEKyW2P_50wopTCMvYo_zlG1x]
- 66. How to choose and optimize ELISA reagents and procedures [https://www.myassays.com/how-to-choose-and-optimize-elisa-reagents-and-procedures.html]
- 67. Western Blot Protocols and Recipes [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-gel-electrophoresis-information/western-blot-protocols.html]
- 68. for Doppler Time-of-Flight... | IEEE DataPort Edge Artifact Correction [https://ieee-dataport.org/documents/edge-artifact-correction-doppler-time-flight-radial-velocity-imaging-based-adaptive]
- 69. Rubber band filters: optimal padding without edge artifacts [https://opg.optica.org/ol/abstract.cfm?uri=ol-50-21-6562]
- 70. nELISA: a high-throughput, high-plex platform enables ... [https://www.nature.com/articles/s41592-025-02861-6]
- 71. 6 Essential IHC Controls for Reliable Staining Results | Boster Bio [https://www.bosterbio.com/blog/post/6-ihc-controls-you-should-know]
- 72. Controls in IHC | Abcam [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/controls-in-ihc]
- 73. Immunohistochemistry (IHC) Troubleshooting Guide & the Importance of Using Controls | Cell Signaling Technology [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide]
- 74. High background in immunohistochemistry [https://www.abcam.com/en-us/technical-resources/troubleshooting/high-background-in-immunohistochemistry]
- 75. Background Staining In IHC And IF [https://vectorlabs.com/blog/my-staining-didnt-work-part-1-background-staining-in-ihc-and-if/?srsltid=AfmBOoqvcfxNOH_9raTXPjb6k3kSP778dPiDTCsCQYWspNl15UDxIKTB]
- 76. Image Analysis Quality Control (Part 3/3): Staining QC [https://www.linkedin.com/pulse/image-analysis-quality-control-part-33-staining-qc-]
- 77. Stain normalization methods for histopathology image ... [https://www.sciencedirect.com/science/article/pii/S1566253523003135]
- 78. Audit and internal quality control in immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC1731142/]
- 79. Creating and troubleshooting microscopy analysis workflows [https://pmc.ncbi.nlm.nih.gov/articles/PMC10942474/]
- 80. A Guide to Modern Quantitative Fluorescent Western ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354265/]
- 81. What are the different detection methods for IHC? [https://www.enzo.com/note/what-are-the-different-detection-methods-for-ihc/]
- 82. High Background Troubleshooting in Western Blots [https://www.sinobiological.com/category/wb-troubleshooting-high-background]
- 83. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOor5b-Q29Et0SO_IClx0h3-Gfmd-InD3FhLjUEEVtdORN0vsIFiU]
- 84. Background Staining In IHC And IF [https://vectorlabs.com/blog/my-staining-didnt-work-part-1-background-staining-in-ihc-and-if/?srsltid=AfmBOopRR5Hk6TkNJal39j6RJ_eG_NmLBUUXtKDPsB_s3nPOqiOYOL6u]
- 85. Quality Assurance Techniques for Batch-to-Batch Consistency [https://tristarintermediates.org/blog/quality-assurance-batch-consistency/]
- 86. 12.2: QA/QC Documentation- SOPs, Batch Records, and COAs - Biology LibreTexts [https://bio.libretexts.org/Courses/West_Los_Angeles_College/Biotechnology/12:_Quality_Assurance_and_Quality_Control_in_Biotechnology/12.02:_QA_QC_Documentation-_SOPs_Batch_Records_and_COAs]
- 87. New FDA Guidelines: Batch Uniformity and Drug Product ... [https://www.gmp-compliance.org/gmp-news/new-fda-guidelines-batch-uniformity-and-drug-product-integrity-advanced-manufacturing-technologies]
- 88. Quality of medicines questions and answers: Part 2 [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/quality-medicines-qa-introduction/quality-medicines-questions-answers-part-2]
- 89. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoq6Hfn55WFecLmn7fofNwtK2B_zUehsSiPpDnpOQCVtKZtETwhp]
- 90. What are the possible causes and solutions for background ... [https://www.aatbio.com/resources/faq-frequently-asked-questions/what-are-the-possible-causes-and-solutions-for-background-issues-high-uneven-or-speckled]
- 91. Top 5 Common Slide Stainer Errors and How to ... [https://www.celnovte.com/solution/top-5-common-slide-stainer-errors-and-how-to-troubleshoot-them/]
- 92. Automated H&E staining problems [https://ihcworld.com/2024/01/20/automated-he-staining-problems/]
- 93. Common Issues Faced by Laboratories with Automatic Slide ... [https://www.naturnlab.com/blog/common-issues-with-automatic-slide-stainers-and-solutions/]
- 94. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOopM_SQv5qgAZ7fRB29YZZ6bwqynN6gViI2jMMH5htB_8jRudNuI]
- 95. IHC Troubleshooting Guide | Common Issues & Fixes [https://www.bosterbio.com/protocol-and-troubleshooting/ihc-troubleshooting?srsltid=AfmBOop0whAiwqG7k5QVCx5fomnAp-5jYsgtiG1nwDkzDh-AJUeWioOo]
- 96. Information Needs and Data Harmonization—Two Sides of the ... [https://datascience.codata.org/en/articles/10.5334/dsj-2025-030]
- 97. Best practices for clinical trials data harmonization and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083401/]