Spike and Recovery Experiments for ELISA Validation: A Complete Guide to Principles, Methods, and Troubleshooting
This comprehensive guide details the critical role of spike and recovery experiments in validating Enzyme-Linked Immunosorbent Assay (ELISA) accuracy and reliability for researchers, scientists, and drug development professionals.
Spike and Recovery Experiments for ELISA Validation: A Complete Guide to Principles, Methods, and Troubleshooting
Abstract
This comprehensive guide details the critical role of spike and recovery experiments in validating Enzyme-Linked Immunosorbent Assay (ELISA) accuracy and reliability for researchers, scientists, and drug development professionals. It covers the foundational principles of assessing matrix interference, provides step-by-step methodological protocols for execution and data analysis, outlines systematic troubleshooting for common recovery issues, and explores integrative validation through dilutional linearity and parallelism studies. The article synthesizes established guidelines and current best practices to equip scientists with the knowledge to ensure their immunoassay data is fit-for-purpose in biomedical research and regulatory contexts.
Understanding Spike and Recovery: The Foundation of Reliable ELISA Data
Defining Spike and Recovery in the Context of ELISA Validation
The enzyme-linked immunosorbent assay (ELISA) provides a methodical quantification of specific analytes through antibody-analyte binding affinity and colorimetric development, serving as a fundamental tool in clinical and research laboratories [1]. However, the accuracy of this quantification can be compromised when the complex composition of biological samples interferes with the detection system. Spike and recovery experiments are therefore an essential validation component, determining whether a known amount of analyte can be accurately measured when introduced into a biological sample matrix [2] [3]. This process confirms the assay's accuracy by revealing if sample constituents affect antigen detection by the antibody, which could lead to either underestimation or overestimation of the true concentration [4].
The fundamental question addressed by spike and recovery is whether the percent recovery obtained from the standard diluent is identical to that obtained from the natural sample matrix [1]. When the sample matrix contains components that affect the assay response differently than the standard diluent, the recovered value will differ significantly from the expected concentration, indicating interference [2] [5]. Such interference can manifest from factors such as high or low pH, high protein or salt concentration, or presence of detergents or organic solvents, all known to interfere with ELISA quantification [3]. Conducting this assessment is therefore critical for researchers and drug development professionals to have confidence in their data quality and to qualify their assays in accordance with regulatory guidelines [3].
Core Concepts and Definitions
What is Spike and Recovery?
Spike and recovery involves introducing ("spiking") known amounts of a purified analyte into various sample types and measuring whether the "recovery" measurements are accurate when compared to the same spike in a standard diluent [2] [3]. The process quantitatively evaluates the effect of the sample matrix on the detection of the antigen by the antibody [4]. In a typical experiment, a known quantity of analyte is added to both the biological sample matrix (e.g., serum, plasma, urine) and a standard diluent (the solution used to prepare the standard curve) [2]. The assay is then run to measure the response of the spiked sample matrix compared to the identical spike in the standard diluent [2].
The recovery percentage is calculated using the formula:
% Recovery = (ConcentrationSpiked Sample - ConcentrationEndogenous) / ConcentrationControl Spike × 100% [5]
Where:
- ConcentrationSpiked Sample is the measured concentration of the sample after spiking
- ConcentrationEndogenous is the measured concentration of the endogenous analyte in the sample before spiking
- ConcentrationControl Spike is the measured concentration of the analyte spiked into the standard diluent [5] [4]
Interference: Over-Recovery and Under-Recovery
Interference occurs when components in the product formulation buffer cause inaccuracies in the ability of the assay to detect and quantify impurities, leading to either over-recovery or under-recovery [3].
- Under-recovery is more common and typically manifests as recovery percentages significantly below the acceptable range. This can be caused by matrix components that inhibit antibody binding, degradation of the analyte, adsorption to surfaces, or poor antibody affinity [3] [6].
- Over-recovery, though less common, occurs when recovery percentages exceed the acceptable range. This can result from matrix components that non-specifically enhance the signal or interact with the capture or detection antibody [3].
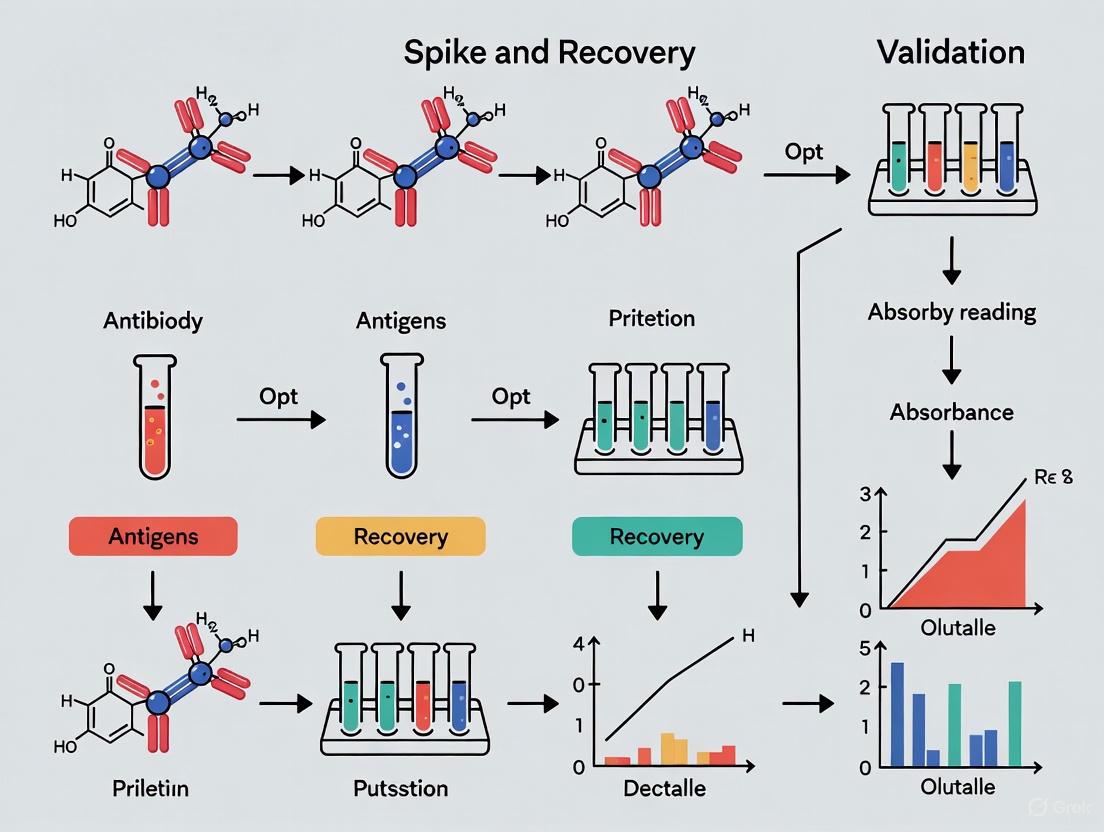
The following diagram illustrates the experimental workflow and potential interference points in a spike and recovery experiment:
Experimental Protocols and Methodologies
Step-by-Step Spike and Recovery Protocol
Performing a robust spike and recovery experiment requires systematic execution with appropriate controls. The following protocol provides a detailed methodology:
Sample Preparation:
Spike Solution Preparation:
- Prepare a concentrated stock solution of the purified analyte (recombinant protein or purified native protein) in the standard diluent [2] [3].
- The spike concentration should be selected to achieve 3-4 concentration levels covering the analytical range of the assay when added to the sample [3].
- Ensure the lowest spiked concentration is at least 2 times the Limit of Quantitation (LOQ) of the assay [3].
Experimental Setup:
Assay Execution:
Calculation and Analysis:
- Calculate the concentration of all samples using the standard curve [4].
- Subtract the endogenous contribution (measured from the control sample with zero standard) from the total measured concentration in the spiked sample [3].
- Calculate the percent recovery using the formula provided in Section 2.1 [5].
Linearity of Dilution Assessment
Linearity of dilution is closely related to spike and recovery and is often assessed simultaneously [2]. This experiment provides information about the precision of results for samples tested at different levels of dilution in a chosen sample diluent [2]. The protocol involves:
Traditional Method:
- Use a low-level sample containing a known spike of analyte or a sample with high endogenous levels of the analyte [2] [1].
- Prepare several serial dilutions (e.g., 1:2, 1:4, 1:8) of the sample in the chosen sample diluent [2] [5].
- Test all dilutions in the assay and calculate the observed concentration for each [2].
Alternative Method:
Interpretation:
- For each dilution, multiply the observed concentration by the dilution factor to obtain the normalized concentration [5].
- Calculate the percent recovery for each dilution: ((ConcentrationDiluted Sample / Dilution Factor) / ConcentrationUndiluted Sample) × 100% [5].
- Assess whether the normalized concentrations remain consistent across dilutions [2].
The relationship between spike and recovery and linearity of dilution assessment, along with their experimental workflows, is illustrated below:
Performance Standards and Acceptance Criteria
Quantitative Acceptance Criteria for Spike and Recovery
Establishing clear acceptance criteria is fundamental for interpreting spike and recovery results. The table below summarizes the performance standards from various sources and contexts:
Table 1: Acceptance Criteria for Spike and Recovery Experiments
| Source/Context | Acceptable Recovery Range | Notes & Applications |
|---|---|---|
| General Bioanalytical Guidelines [6] | 90–110% | Ideal range for most biological samples |
| Regulatory Guidelines (ICH, FDA, EMA) [3] | 75–125% | Applied for HCP ELISA and biopharmaceutical applications |
| Food Allergen Testing (AOAC) [7] | 50–150% | Acceptable for challenging food matrices when consistent |
| Commercial ELISA Kit Validation [8] | 80–120% | Typical range for commercial kit quality control |
| Research ELISA Applications [5] | 80–120% | Commonly cited range for research purposes |
Representative Spike and Recovery Data
The following table presents representative spike and recovery data for recombinant human IL-1 beta in nine human urine samples, demonstrating how results are typically compiled and analyzed:
Table 2: Experimental Spike and Recovery Data for Human IL-1 Beta in Urine Samples [2]
| Sample | No Spike (0 pg/mL) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|---|
| Diluent Control | 0.0 | 17.0 | 44.1 | 81.6 |
| Donor 1 | 0.7 | 14.6 | 39.6 | 69.6 |
| Donor 2 | 0.0 | 17.8 | 41.6 | 74.8 |
| Donor 3 | 0.6 | 15.0 | 37.6 | 68.9 |
| Donor 4 | 0.0 | 15.1 | 36.9 | 67.8 |
| Donor 5 | 0.5 | 12.5 | 33.5 | 63.6 |
| Donor 6 | 0.0 | 14.0 | 33.5 | 68.7 |
| Donor 7 | 0.0 | 14.4 | 38.5 | 69.6 |
| Donor 8 | 7.1 | 16.3 | 41.4 | 69.5 |
| Donor 9 | 0.7 | 12.4 | 37.6 | 68.2 |
| Mean Recovery (± S.D.) | NA | 86.3% ± 9.9% | 85.8% ± 6.7% | 84.6% ± 3.5% |
Linearity of Dilution Performance Standards
For linearity of dilution experiments, the acceptance criteria are similarly strict. The normalized analyte concentrations (accounting for dilution factors) should remain consistent across different dilutions [5]. The percentage recovery for linearity is calculated as: ((ConcentrationDiluted Sample / Dilution Factor) / ConcentrationUndiluted Sample) × 100% [5]. Values between 80–120% generally demonstrate good assay linearity [5] [8].
The table below shows representative linearity of dilution data for human IL-1 beta in different sample matrices:
Table 3: Experimental Linearity of Dilution Data for Human IL-1 Beta [2]
| Sample | Dilution Factor (DF) | Observed (pg/mL) × DF | Expected pg/mL (neat value) | Recovery % |
|---|---|---|---|---|
| ConA-stimulated Cell Culture Supernatant | Neat | 131.5 | 131.5 | 100 |
| 1:2 | 149.9 | 114 | ||
| 1:4 | 162.2 | 123 | ||
| 1:8 | 165.4 | 126 | ||
| High-level Serum Sample | Neat | 128.7 | 128.7 | 100 |
| 1:2 | 142.6 | 111 | ||
| 1:4 | 139.2 | 108 | ||
| 1:8 | 171.5 | 133 | ||
| Low-level Serum Sample Spiked with Recombinant IL-1 Beta | Neat | 39.3 | 39.3 | 100 |
| 1:2 | 47.9 | 122 | ||
| 1:4 | 50.5 | 128 | ||
| 1:8 | 54.6 | 139 |
Troubleshooting and Optimization Strategies
Addressing Poor Spike and Recovery Results
When spike and recovery results fall outside acceptable ranges, several adjustment strategies can be implemented to optimize assay performance:
Alter the Standard Diluent:
- Use a standard diluent whose composition more closely matches the final sample matrix [2].
- For example, when testing culture supernatants, use culture medium as the standard diluent rather than a simple buffer [2].
- Consider adding carrier proteins like BSA (1%) to the standard diluent to mimic the protein content in biological samples [2].
Modify the Sample Matrix:
- If neat biological samples produce poor recovery, test the sample upon dilution in standard diluent or other logical "sample diluent" [2].
- For serum samples that produce poor spike and recovery, a 1:1 dilution in standard diluent may correct the issue, provided the analyte concentration remains detectable [2].
- Adjust the pH of the sample matrix to match the optimized standard diluent [2].
Sample-Specific Interventions:
- For challenging matrices like chocolate (high in tannins and polyphenols), add extra protein (e.g., fish gelatine or milk powder) to the extraction buffer. The excess protein binds to interfering compounds and makes allergens available for extraction [7].
- Add surfactants (e.g., 0.05% Tween-20) to reduce adsorption and stabilize low-concentration targets, particularly in low-protein matrices like CSF [6].
The Scientist's Toolkit: Essential Research Reagents
Successful spike and recovery experiments require specific reagents and materials. The following table details essential research reagent solutions and their functions:
Table 4: Essential Research Reagent Solutions for Spike and Recovery Experiments
| Reagent/Material | Function & Purpose | Application Notes |
|---|---|---|
| Purified Recombinant Protein | Serves as the spike analyte; must be identical to the target protein | Use the same lot for all validation experiments [2] |
| Standard Diluent | Base matrix for preparing standard curves and control spikes | Typically a simple buffer (e.g., PBS) [2] |
| Matrix-Matched Diluent | Standard diluent modified to mimic sample matrix composition | Improves recovery by equalizing matrix effects [6] |
| Carrier Proteins (BSA, Gelatine) | Reduces non-specific binding and surface adsorption | Essential for low-protein samples like CSF or urine [2] [7] |
| Surfactants (Tween-20) | Minimizes hydrophobic interactions and surface adsorption | Typically used at 0.05% concentration [6] |
| Protein Stabilizers | Prevents degradation of spiked analyte during processing | Critical for labile proteins [8] |
Regulatory and Industry Perspectives
Validation in Regulatory Contexts
Spike and recovery experiments hold significant importance in regulatory compliance for pharmaceutical development and clinical diagnostics. Regulatory bodies including the International Council for Harmonisation (ICH), FDA, and European Medicines Agency (EMA) provide guidelines on analytical procedure validation that consider recovery values within 75% to 125% of the spiked concentration as acceptable for host cell protein (HCP) ELISAs and related biopharmaceutical applications [3].
The validation requirements differ based on the application context. For in-house developed methods, a full validation is required, including robustness, precision, trueness, limits of quantification, dilutional linearity, parallelism, recovery, selectivity, and sample stability [9]. For commercial assays, a partial validation is typically sufficient, including all parameters except robustness, which should have been addressed by the manufacturer during method development [9].
Industry Standards Across Applications
Acceptable recovery ranges vary across different industries and applications, reflecting the diverse challenges posed by various sample matrices:
- Clinical Diagnostics: Stringent criteria (typically 85-115%) apply due to the medical decision-making implications [9] [6].
- Biopharmaceutical Development: ICH/FDA guidelines allow 75-125% recovery for HCP ELISA, acknowledging the complexity of drug product matrices [3].
- Food Allergen Testing: The Association of Analytical Communities (AOAC) accepts recoveries between 50-150% for challenging food matrices, provided they are consistent, recognizing the extreme diversity and complexity of food samples [7].
Spike and recovery experiments represent a critical validation component for ELISA methods, providing objective evidence that the assay accurately measures the analyte in specific sample matrices. Through systematic spiking of known analyte amounts into biological samples and comparison with standard diluent controls, researchers can identify and quantify matrix interference effects. The consistent application of standardized protocols, coupled with adherence to industry-specific acceptance criteria (typically 80-120% recovery for most research applications), ensures the generation of reliable, reproducible data. When recovery falls outside acceptable ranges, methodological adjustments—such as matrix-matched standard curves, sample dilution, or addition of carrier proteins—can often optimize performance. As such, spike and recovery validation remains an indispensable practice for researchers, scientists, and drug development professionals seeking to generate quantitatively accurate ELISA data for both basic research and regulatory submissions.
Matrix interference is an inherent challenge in immunoassays like ELISA, where components within a sample matrix (such as proteins, lipids, or salts) disrupt the specific binding between the target analyte and assay antibodies, leading to inaccurate concentration measurements [10]. For researchers and drug development professionals, identifying and quantifying this interference is not optional—it is a critical pillar of assay validation, ensuring that inaccuracies are detected and corrected, thereby safeguarding the reliability of experimental and clinical data [11] [1]. This guide frames the solutions within the essential context of spike and recovery experiments, providing a comparative analysis of methodologies and their performance in delivering accurate results.
Core Experimental Methodologies for Quantification
Three principal experimental protocols are employed to identify and quantify matrix interference, each serving a distinct purpose in assay validation [1].
Spike and Recovery Experiment
This test determines if the sample matrix inhibits or enhances the antibody-analyte binding interaction, providing a direct measure of matrix interference [10] [12].
- Objective: To assess the difference in percent recovery of a known analyte between the standard diluent and the natural sample matrix [1].
- Protocol:
- Spike: Add a known concentration of the purified standard analyte (the "spike") into both the standard diluent and the sample matrix of interest (e.g., plasma, serum) [10] [1].
- Run Assay: Process both the spiked diluent and the spiked matrix through the ELISA.
- Calculate Recovery: Determine the measured concentration from the standard curve and calculate the percent recovery.
- % Recovery = (Measured concentration in spiked matrix / Measured concentration in spiked diluent) × 100 [1].
- Data Interpretation: Ideal recovery is 100%, indicating no matrix interference. Recoveries within 80–120% are generally considered acceptable. Significant deviations outside this range indicate substantial matrix effects that must be addressed [10] [1].
Dilutional Linearity
This experiment assesses whether the matrix effect can be overcome by diluting the sample, and whether the analyte concentration can be reliably measured across different dilutions [1].
- Objective: To verify that a spiked sample, when serially diluted, provides measured concentrations that align with expected values [1].
- Protocol:
- Spike: Introduce a known quantity of standard analyte into the sample matrix at a concentration above the assay's upper detection limit.
- Dilute: Perform a series of dilutions (e.g., 1:2, 1:4, 1:8) using the assay diluent until the predicted concentration falls within the standard curve's range.
- Analyze: Calculate the observed concentration and the percent recovery at each dilution factor [1].
- Data Interpretation: Samples with ideal linearity will show recoveries close to 100% at every dilution. A consistent recovery within the 80–120% range across dilutions confirms that the chosen dilution factor is suitable for accurate measurement [1].
Parallelism
This method validates that the endogenous analyte in a real sample behaves immunologically similarly to the recombinant or purified standard used for the calibration curve [1].
- Objective: To ensure comparable immunoreactivity between the endogenous analyte in a sample and the standard analyte [1].
- Protocol:
- Select Samples: Identify at least three samples with high endogenous concentrations of the analyte.
- Dilute: Perform serial dilutions of these samples using the assay diluent.
- Analyze: Plot the measured concentrations (after applying the dilution factor) against the dilution level [1].
- Data Interpretation: A plot that produces lines parallel to the standard curve indicates that the endogenous and standard analytes are behaving identically. A loss of parallelism suggests differences in immunoreactivity, potentially due to post-translational modifications or other matrix effects [1].
The logical relationship and decision pathway for these experiments can be visualized below.
Comparative Experimental Data and Performance
The following tables summarize quantitative data and performance outcomes from matrix interference experiments, providing a benchmark for researchers.
Table 1: Example Spike and Recovery Data from Various Matrices
This table illustrates how recovery percentages can vary across different sample types, informing the selection of an appropriate minimum dilution [1].
| Sample Matrix | Spike Concentration | % Recovery | Minimum Recommended Dilution |
|---|---|---|---|
| Human Serum (Extracted) | 2 ng/mL | 102% | Neat |
| Human EDTA Plasma (Extracted) | 1 ng/mL | 90% | Neat |
| Mouse Serum (Extracted) | 0.5 ng/mL | 105.8% | 1:2 |
| Porcine Serum (Extracted) | 0.6 ng/mL | 107.8% | 1:2 |
| Human Saliva (Extracted) | 2.5 ng/mL | 98.7% | 1:2 |
| Banana (Extracted) | 1.25 ng/mL | 87.6% | 1:2 |
Table 2: Dilutional Linearity Analysis of a Spiked Sample
This table demonstrates how recovery can improve at certain dilutions, helping to identify the optimal working range [1].
| Dilution | Expected (pg/mL) | Observed (pg/mL) | Recovery (%) |
|---|---|---|---|
| Neat | — | 390.8 | — |
| 1:2 | 195.4 | 194.6 | 100% |
| 1:4 | 97.7 | 105.1 | 108% |
| 1:8 | 48.8 | 67.0 | 137% |
| 1:16 | 24.4 | 27.9 | 114% |
| 1:32 | 12.2 | 12.1 | 99% |
Table 3: Performance of Mitigation Strategies
A comparison of common techniques used to overcome matrix interference after its identification.
| Mitigation Strategy | Principle | Key Advantage | Key Limitation |
|---|---|---|---|
| Sample Dilution [10] [11] | Reduces concentration of interfering components | Simple, cost-effective | Requires analyte to be at a high enough concentration |
| Matrix-Matched Calibration [10] [11] | Uses standards diluted in the analyte-free sample matrix | Corrects for matrix effects on the standard curve | Can be difficult to obtain a true "blank" matrix |
| Buffer Exchange [11] | Physically removes interfering components via chromatography | Effective for salts, lipids, and small molecules | Adds a processing step; risk of analyte loss |
| Sample Neutralization [10] | Adjusts sample pH to the optimal range for the assay | Corrects for pH-specific interference | Does not address other types of interference |
| ELISA Protocol Modification [10] | Alters incubation times, volumes, or steps | Can improve signal-to-noise without extra steps | Requires re-validation of the modified protocol |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successfully navigating matrix interference requires a suite of key reagents and materials. The following table details these essential components and their critical functions in validation and mitigation.
| Item | Function in Identifying/Quantifying Interference |
|---|---|
| Analyte-Free Matrix | Serves as the ideal, but often difficult-to-obtain, negative matrix control and base for spiking experiments [13]. |
| Purified Standard Analyte | The known quantity of protein used for "spiking" in recovery and linearity experiments [1]. |
| Assay Diluent | The buffer used to reconstitute standards and, potentially, to dilute samples. Its composition is critical for minimizing nonspecific binding [10] [11]. |
| Blocking Buffers | Solutions containing proteins (e.g., BSA, skimmed milk) or other agents to cover unsaturated binding sites on the plate, reducing background noise [11] [14]. |
| Positive Control | A sample with a known concentration of analyte, used to verify the assay is functioning correctly [13] [15]. |
| Negative Matrix Control | A sample matrix guaranteed to be free of the analyte, used to determine the signal contribution from the matrix itself [13]. |
The integrated workflow for method selection based on experimental data is outlined below.
The systematic identification and quantification of matrix interference through spike and recovery, dilutional linearity, and parallelism experiments are non-negotiable steps in robust ELISA validation. The data derived from these protocols empower researchers to select evidence-based mitigation strategies, ensuring that the final assay delivers accurate, reliable, and reproducible quantification of biomarkers and therapeutics across diverse biological matrices.
In quantitative Enzyme-Linked Immunosorbent Assays (ELISAs), the accurate measurement of analytes depends heavily on the liquid environment in which the assay is performed. Two critical but distinct liquid environments are the sample matrix and the standard diluent. The sample matrix is the natural biological fluid containing the analyte of interest, such as serum, plasma, or urine. Its complex composition can significantly interfere with assay accuracy. In contrast, the standard diluent is a defined buffer solution used to prepare the standard curve from purified analyte. The fundamental challenge in ELISA validation arises from the differences between these two environments, which can lead to inaccurate quantification. Spike and recovery experiments serve as a crucial methodology to detect, quantify, and correct for these discrepancies, ensuring the reliability of assay results [2] [1].
Defining the Key Components
Sample Matrix
The sample matrix refers to the native biological sample in which the analyte is found.
- Composition: A complex mixture of components such as proteins (e.g., albumin, immunoglobulins), lipids, carbohydrates, salts, and metabolites [16] [17] [10].
- Function: Serves as the medium for the test sample, containing the endogenous analyte.
- Sources: Common matrices include serum, plasma, urine, saliva, and cell culture supernatants [14].
- Challenge: Components within the matrix can interfere with the antibody-antigen binding in the ELISA through various mechanisms, leading to what is known as the "matrix effect" [17] [10]. This can cause either an artificial increase (false positive) or decrease (false negative) in the measured analyte concentration [10].
Standard Diluent
The standard diluent is a specially formulated buffer solution.
- Composition: Typically a simple, defined solution like phosphate-buffered saline (PBS), often containing a carrier protein such as Bovine Serum Albumin (BSA) and other stabilizing agents [18] [16].
- Function: Used to reconstitute and create serial dilutions of the highly purified standard (calibrator) analyte for generating the standard curve [18] [2].
- Objective: To provide an ideal and consistent environment for the antibody-ant interaction, free from interfering substances, thereby establishing a reference for quantification [2].
The table below summarizes the core differences between these two components.
Table 1: Fundamental Comparison Between Sample Matrix and Standard Diluent
| Feature | Sample Matrix | Standard Diluent |
|---|---|---|
| Composition | Complex, variable biological fluid | Simple, defined buffer solution |
| Components | Proteins, lipids, salts, metabolites [17] [10] | Buffer salts, carrier protein (e.g., BSA) [18] |
| Primary Role | Holds the endogenous analyte in its native state | Dilutes the purified standard to create a calibration curve |
| Consistency | Highly variable between individuals and samples | Consistent and reproducible |
| Ideal Use | Measuring unknown analyte concentrations in test samples | Creating the standard curve for quantitative interpolation |
The Interaction Problem: Matrix Effects
A core assumption in ELISA is that the analyte, whether in the standard diluent or the sample matrix, behaves identically. However, the complex composition of the sample matrix can violate this assumption. Matrix effects occur when substances in the sample interfere with the assay, altering the detected signal independently of the actual analyte concentration [17] [10].
These effects can stem from:
- Plasma/serum proteins like albumin, complement proteins, or fibrinogen [10].
- Lipids (e.g., steroids) and carbohydrates [16] [10].
- Variations in pH, salt concentration, or sample viscosity [16] [17].
- Direct interactions where interfering substances bind to the analyte or the antibodies, blocking epitopes [10].
When the standard curve is generated in an idealized diluent but samples are run in a complex matrix, the difference in recovery can lead to systematic over- or under-estimation of the true analyte concentration [2]. The following diagram illustrates the experimental workflow designed to diagnose this specific problem.
Experimental Protocol: Spike and Recovery
The spike and recovery experiment is the definitive method to quantify the impact of the sample matrix on assay accuracy [2] [1] [16].
Materials and Reagents
Table 2: Essential Research Reagent Solutions for Spike and Recovery
| Reagent / Material | Function | Example / Note |
|---|---|---|
| Sample Matrix | The test biological fluid being validated. | Pooled or individual donor serum/plasma [2]. |
| Standard Diluent | The buffer used for the standard curve. | PBS with 1% BSA [18] [16]. |
| Purified Analyte Standard | A known quantity of the target protein for spiking. | Recombinant protein [2] [10]. |
| ELISA Kit/Reagents | Core assay components. | Coated plate, detection antibodies, substrate [14]. |
| Sample Diluent | Buffer used to dilute samples; may differ from standard diluent. | Optimized to reduce matrix interference [18]. |
Step-by-Step Methodology
Spike Preparation:
- Sample Matrix Spike: Add a known, physiologically relevant concentration of the purified analyte standard directly into the undiluted sample matrix [2] [1].
- Standard Diluent Spike: Add the same known concentration of the purified analyte standard into the standard diluent used for the standard curve. This serves as the control [2].
Assay Execution:
Data Calculation:
- Calculate the concentration of the spiked samples based on the standard curve.
Determine the % Recovery using the following formula [16]:
% Recovery = (Spiked Sample Concentration - Unspiked Sample Concentration) / Spiked Standard Diluent Concentration × 100
Data Interpretation and Acceptance Criteria
The recovery percentage indicates the degree of matrix interference.
- ~100% Recovery (Ideal): Components in the sample matrix do not interfere with analyte detection. The sample matrix and standard diluent are effectively equivalent for the assay [1].
- >120% or <80% Recovery (Problematic): Indicates significant matrix effects. A low recovery suggests suppression of the signal (e.g., blocking of antibody binding), while a high recovery suggests signal enhancement [1] [16].
The acceptable recovery range is typically 80-120%, though specific assays may have stricter limits [1] [16] [10]. The following table provides a concrete example from published data.
Table 3: Example Spike-and-Recovery Data for Recombinant Human IL-1 beta in Human Urine [2]
| Sample (n=9) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|
| Diluent Control (Recovered Conc.) | 17.0 pg/mL | 44.1 pg/mL | 81.6 pg/mL |
| Mean Urine Recovery (Recovered Conc.) | 14.7 pg/mL | 37.8 pg/mL | 69.0 pg/mL |
| Mean Recovery % | 86.3% | 85.8% | 84.6% |
| Interpretation | Within acceptable range | Within acceptable range | Within acceptable range |
Resolving Matrix Interference Issues
When spike-and-recovery results fall outside the acceptable range, several strategies can be employed to mitigate matrix effects.
Sample Dilution: Diluting the sample in the standard diluent or a specific sample diluent is the most common and effective approach. This reduces the concentration of interfering substances while ideally keeping the analyte within the detection range of the assay [16] [17] [10]. The optimal Minimum Required Dilution (MRD) must be determined empirically [10].
Matrix-Matched Calibration: The standard curve is prepared in a matrix that closely matches the test sample, such as analyte-free (stripped) serum or a pool of normal serum. This ensures that both standards and samples are exposed to the same matrix environment, normalizing the effects [4] [16] [17].
Alternative Diluents: Using a different, optimized assay diluent specifically formulated for problematic sample types (e.g., plasma or serum) can help. These commercial diluents may contain components that inhibit specific interferents like thrombin or complement activity [18].
Sample Pre-treatment: For specific issues, neutralizing the sample pH, delipidation, or other forms of clean-up can be performed to remove interferents prior to the assay [10].
The distinction between the sample matrix and the standard diluent is a fundamental concept in the rigorous validation of quantitative ELISAs. The sample matrix, with its inherent complexity and variability, is a primary source of interference that can compromise data accuracy. The spike and recovery experiment is an indispensable tool that directly probes the interaction between these two environments, providing a quantitative measure of matrix effects. By systematically employing this validation technique and applying corrective strategies such as sample dilution or matrix matching, researchers can ensure their ELISA results are both accurate and reliable, thereby upholding the integrity of their scientific and diagnostic conclusions.
The enzyme-linked immunosorbent assay (ELISA) provides a methodical quantification of specific analytes through antibody-analyte binding affinity and colorimetric development, serving as a fundamental tool in both research and diagnostic settings [14]. For samples validated by ELISAs, high accuracy and reliability in analyte quantification is the expectation; however, samples that have not been validated may not display similar degrees of reliability [1]. The spike-and-recovery experiment is a critical validation method designed to determine whether analyte detection is affected by differences between the standard curve diluent and the biological sample matrix [2]. In this procedure, a known amount of analyte is added ("spiked") into the natural test sample matrix, and the assay is run to measure the response ("recovery") compared to an identical spike in the standard diluent [2] [19]. When this recovery deviates significantly from 100%, it indicates matrix interference that can lead to either over-estimation or under-estimation of the true analyte concentration, potentially compromising experimental conclusions and diagnostic decisions.
Mechanisms and Consequences of Analytic Over-Estimation
Over-estimation of analytes occurs when the measured concentration exceeds the actual amount present in the sample. This phenomenon typically manifests as "over-recovery" (recovery >125%) and can significantly impact data interpretation [19]. The primary mechanism behind over-estimation involves non-specific interference from matrix components that artificially enhance the assay signal. When the drug substance or other matrix component interacts with the capture or detection antibody, this can result in over-recovery values [19]. Such interactions may include cross-reactivity with structurally similar molecules present in the sample matrix or binding interactions that enhance the enzymatic reaction beyond what would occur with the target analyte alone.
The consequences of analytic over-estimation in research and development can be severe:
- Inaccurate potency assessments in biopharmaceutical development, leading to incorrect dosing determinations
- False positive results in diagnostic applications, potentially causing misdiagnosis
- Inflation of biomarker concentrations in research studies, compromising data validity
- Incorrect conclusions about biological processes or disease states
For drug development professionals, these inaccuracies can have cascading effects throughout the development pipeline, potentially resulting in costly course corrections or failed clinical trials when the true analyte concentrations are discovered at later stages.
Mechanisms and Consequences of Analytic Under-Estimation
Under-estimation represents the more commonly observed direction of error in spike-and-recovery experiments, typically appearing as "under-recovery" (recovery <75%) [19]. This phenomenon occurs when components in the sample matrix inhibit the detection of the target analyte, leading to measured values that are lower than the actual concentration. In the cases where interference is detected, it typically manifests as under-recovery of the spiked analyte [19]. The sample matrix may contain components that affect assay response to the analyte differently than the standard diluent, and a spike-and-recovery experiment is designed to assess this difference in assay response [2].
Multiple mechanisms can contribute to analytic under-estimation:
- Matrix effects from substances such as salts, detergents, lipids, or heterophilic antibodies that interfere with antigen-antibody binding [1]
- Protein degradation from enzymatic activity in the sample matrix that breaks down the target analyte before detection
- Sequestration of the analyte by binding proteins or other matrix components, rendering it unavailable for detection
- High background protein concentrations that hinder antibody binding and increase signal-to-noise ratio, resulting in underestimation of the target concentration [4]
The consequences of under-estimation present significant risks across applications:
- Failure to detect clinically relevant biomarkers in diagnostic settings, leading to false negatives
- Underestimation of impurity levels in biopharmaceuticals, potentially compromising drug safety
- Inaccurate pharmacokinetic data due to underestimated drug concentrations
- Invalid conclusions in research studies regarding biological concentrations and responses
For scientists and drug development professionals, these inaccuracies can be particularly problematic when they occur with precious samples that cannot be easily replaced, emphasizing the critical need for proper validation before running definitive experiments [20].
Experimental Protocols for Assessment
Standard Spike-and-Recovery Protocol
The fundamental spike-and-recovery experiment follows a systematic approach to quantify matrix effects [2] [19]:
- Step 1: Prepare a known concentration of the purified analyte (standard) in the standard diluent used for the ELISA standard curve.
- Step 2: Spike this known amount of analyte into the natural sample matrix at 3-4 concentration levels covering the analytical range of the assay [19]. The lowest spiked concentration should be at least 2 times the Limit of Quantitation (LOQ) of the assay [19].
- Step 3: In parallel, prepare an identical spike of the analyte into the standard diluent as a control.
- Step 4: Run both the spiked sample matrix and spiked standard diluent in the ELISA according to the established protocol.
- Step 5: Calculate the recovery percentage using the formula: Recovery % = (Measured concentration in spiked sample - Endogenous concentration in unspiked sample) / Known spiked concentration × 100.
Table 1: Example Spike-and-Recovery Data for Recombinant Human IL-1 Beta in Human Urine Samples [2]
| Sample | No Spike (0 pg/mL) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|---|
| Diluent Control | 0.0 | 17.0 | 44.1 | 81.6 |
| Donor 1 | 0.7 | 14.6 | 39.6 | 69.6 |
| Donor 2 | 0.0 | 17.8 | 41.6 | 74.8 |
| Donor 3 | 0.6 | 15.0 | 37.6 | 68.9 |
| Donor 9 | 0.7 | 12.4 | 37.6 | 68.2 |
| Mean Recovery | NA | 86.3% | 85.8% | 84.6% |
Linearity of Dilution Assessment
The linearity-of-dilution experiment provides complementary information about the precision of results for samples tested at different levels of dilution in a chosen sample diluent [2]. This protocol determines whether sample matrices spiked with detection analyte above the upper limit of detection can still provide reliable quantification after dilution within standard curve ranges [1].
- Traditional Method: Use a sample containing a known spike of analyte or a sample with high endogenous levels of the analyte, then test several different dilutions of that sample in the chosen sample diluent [2] [1].
- Alternative Method: Prepare several dilutions of a low-level sample and then spike the same known amount of analyte into each one before testing [2].
- Calculation: Assess recovery by comparing observed versus expected values based on non-spiked and/or neat (undiluted) samples [2].
Table 2: Example Linearity-of-Dilution Results for Human IL-1 Beta Samples [2]
| Sample | Dilution Factor | Observed (pg/mL) × DF | Expected (neat value) | Recovery % |
|---|---|---|---|---|
| ConA-stimulated cell culture supernatant | Neat | 131.5 | 131.5 | 100 |
| 1:2 | 149.9 | 114 | ||
| 1:4 | 162.2 | 123 | ||
| 1:8 | 165.4 | 126 | ||
| High-level serum sample | Neat | 128.7 | 128.7 | 100 |
| 1:2 | 142.6 | 111 | ||
| 1:4 | 139.2 | 108 | ||
| Low-level serum sample spiked with recombinant IL-1 beta | Neat | 39.3 | 39.3 | 100 |
| 1:2 | 47.9 | 122 | ||
| 1:4 | 50.5 | 128 |
Troubleshooting and Correction Strategies
Addressing Poor Recovery Results
When spike-and-recovery experiments reveal significant deviations from the expected 100% recovery, several methodological adjustments can be implemented to improve accuracy:
Alter the Standard Diluent: Use a standard diluent whose composition more closely matches the final sample matrix [2]. For example, culture medium could be used as the standard diluent if the samples will be culture supernatants [2]. While this approach may decrease assay range, sensitivity, or signal-to-noise ratio compared to previously optimized conditions, it often represents a necessary compromise for accurate quantification.
Modify the Sample Matrix: If neat biological samples produce poor spike and recovery, dilution in standard diluent or other logical "sample diluent" may improve results [2]. For instance, if an undiluted serum sample produces poor recovery, a sample diluted 1:1 in standard diluent may perform better, provided the analyte concentration remains detectable [2].
Matrix pH Adjustment: Better results for a sample matrix may be obtained by altering its pH to match the optimized standard diluent [2].
Protein Supplementation: Adding BSA or other purified protein as a carrier/stabilizer can improve recovery in some matrices by reducing non-specific binding [2].
Establishing Acceptance Criteria
Regulatory and industry guidelines provide frameworks for interpreting spike-and-recovery results:
- ICH, FDA, and EMA Guidelines: Consider recovery values within 75% to 125% of the spiked concentration to be in the acceptable range [19].
- Alternative Criteria: Some sources suggest a slightly narrower range of 80-120% as acceptable [1] [4] [21].
- Parallelism Assessment: %CV within 20-30% of expectations generally display successful parallelism, although the exact percentage should be decided by end users based on their specific application requirements [1].
Research Reagent Solutions
Table 3: Essential Materials for Spike-and-Recovery Experiments
| Reagent/Material | Function in Experiment | Technical Considerations |
|---|---|---|
| Purified Analyte Standard | Serves as the spike material of known concentration | Should be identical to the native analyte; requires proper storage to prevent degradation [20] |
| Standard Diluent | Matrix for preparing standard curve and control spikes | Optimized for signal-to-noise performance; may need modification to match sample matrix [2] |
| Sample Diluent | Matrix for diluting biological samples | May differ from standard diluent; optimal composition depends on sample type [2] |
| Matrix-Matched Controls | Assess background interference in specific sample types | Should include the same matrix as test samples for accurate recovery assessment [22] |
| Blocking Buffers | Reduce non-specific binding in assay | Composition (BSA, non-fat milk, etc.) may need optimization for different matrices [2] |
| Microplate Reader | Measure absorbance of colorimetric reaction | Capable of reading at appropriate wavelengths (e.g., 450nm); software for curve fitting essential [14] [4] |
Spike-and-recovery experiments represent an essential component of ELISA validation that directly addresses the critical issue of analytical accuracy in complex biological matrices. The consequences of poor recovery—whether leading to over-estimation or under-estimation of analytes—can fundamentally compromise the validity of experimental data and subsequent conclusions. Through systematic implementation of the described protocols and troubleshooting strategies, researchers and drug development professionals can identify matrix effects, implement appropriate corrections, and generate reliable, quantitative data. As ELISA continues to be a cornerstone technology in both research and clinical applications, rigorous attention to recovery validation remains fundamental to scientific rigor and accurate analyte quantification across diverse sample types.
Within the stringent framework of biopharmaceutical development, demonstrating that an analytical method is "fit-for-purpose" is a regulatory imperative. Assay qualification provides objective evidence that a method consistently produces reliable results suitable for its intended use. This guide explores the critical role of spike and recovery experiments, a cornerstone of immunoassay validation, in meeting regulatory standards from agencies like the FDA and EMA. We will examine its fundamental principles, detailed experimental protocols, and its position within the broader validation paradigm, providing researchers and drug development professionals with the knowledge to ensure regulatory compliance and data integrity.
Fit-for-purpose assay qualification is the process of demonstrating that an analytical method, such as an Enzyme-Linked Immunosorbent Assay (ELISA), fulfills predefined requirements for a specific application [9]. Unlike full validation for in vitro diagnostics, a fit-for-purpose approach tailors the stringency and extent of validation experiments to the assay's intended role, whether for process development, product release, or characterization [23] [24]. The overarching goal is to generate objective evidence that the method is precise, accurate, and robust enough to support critical decisions in a regulated environment.
Regulatory agencies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), provide guidelines that shape these qualification efforts [25] [9]. Adherence to these standards is not merely a bureaucratic hurdle; it is fundamental to ensuring the safety and efficacy of biopharmaceuticals. A well-qualified Host Cell Protein (HCP) ELISA, for example, gives analysts and regulators confidence that a purification process consistently reduces process-related impurities to safe levels [23]. The consequences of poor validation are severe, potentially leading to the generation of false positive or false negative results, which can compromise product quality and patient safety [24].
The Centrality of Spike and Recovery Experiments
Principles and Definitions
The spike and recovery experiment is a fundamental procedure used to assess the accuracy of an ELISA [2] [25]. Accuracy refers to the closeness of agreement between the measured value and the true value of the analyte [9]. In this experiment, a known amount of a purified reference analyte is introduced ("spiked") into a sample matrix of interest. The assay is then performed, and the measured concentration of the spiked analyte is compared to its expected concentration [2].
The percentage recovery is calculated as follows: % Recovery = (Measured Concentration / Expected Concentration) × 100
This test is essential because the sample matrix (e.g., serum, drug substance, in-process harvest) can contain components that interfere with the antibody-antigen interaction, leading to an overestimation (over-recovery) or underestimation (under-recovery) of the target impurity [25]. Factors such as high or low pH, high protein or salt concentration, or the presence of detergents or organic solvents are known to cause such interference [25].
Regulatory Acceptance Criteria
Regulatory guidelines provide clear benchmarks for acceptable spike and recovery performance. According to ICH, FDA, and EMA guidelines, recovery values within 75% to 125% of the spiked analyte concentration are generally considered acceptable [25]. This range ensures that the assay delivers accurate quantitation despite the potential complexities of the sample matrix.
Experimental Protocol for Spike and Recovery
A robust spike and recovery experiment must be performed for every unique sample matrix to be tested in the ELISA [25]. The following provides a detailed, step-by-step methodology.
Preliminary Requirement: Dilution Linearity and MRD
Before performing spike and recovery, it is recommended to first conduct dilution linearity studies. This experiment establishes that the condition of antibody excess is met and determines the Minimum Required Dilution (MRD) for the sample, which is the dilution that minimizes matrix interference while keeping the analyte within the assay's quantifiable range [25].
Step-by-Step Procedure
- Sample Preparation: Prepare the neat (undiluted) sample matrix.
- Spike Solution: Prepare a concentrated stock solution of the purified analyte (e.g., recombinant protein or purified HCP) in an appropriate diluent.
- Spiking: Spike the sample matrix at 3-4 concentration levels covering the analytical range of the assay. For instance, to achieve a final spike concentration of 20 ng/mL, add 1 part of a 100 ng/mL standard into 4 parts of the neat sample [25].
- Control Samples: Prepare two critical control samples in parallel:
- Matrix Blank: The sample matrix spiked with a "zero standard" (the diluent used for the spike solution) to determine the endogenous level of the analyte.
- Diluent Control: The standard diluent spiked with the same amount of analyte to represent the 100% recovery baseline.
- Assay Execution: Run the complete ELISA protocol on all spiked samples and controls.
- Data Calculation:
- Subtract the value of the Matrix Blank from the corresponding spiked sample to determine the net measured concentration attributable only to the spike.
- Calculate the % Recovery for each spike level using the Diluent Control as the expected value.
Table 1: Example Spike and Recovery Data for an HCP ELISA in a Final Product Matrix [25]
| Sample Description | Spike Concentration (ng/mL) | Total HCP Measured (ng/mL) | Net Measured Spike (ng/mL) | % Recovery |
|---|---|---|---|---|
| Matrix Blank | 0 | 6.0 | --- | --- |
| Diluent Control | 20 | 20.0 | 20.0 | 100.0 |
| Final Product | 20 | 25.0 | 19.0 | 95.0 |
Troubleshooting Poor Recovery
Poor recovery indicates matrix interference. Two primary adjustments can be made to the method [2]:
- Alter the Standard Diluent: Use a standard diluent whose composition more closely matches the final sample matrix (e.g., using culture medium for culture supernatant samples).
- Alter the Sample Matrix: Dilute the sample further in the standard diluent or adjust its pH. Adding a carrier protein like BSA can also stabilize the analyte and improve recovery.
The following workflow diagrams the logical process of performing and interpreting a spike and recovery experiment.
Integration within the Broader Validation Paradigm
Spike and recovery is a critical component of accuracy, but it is only one part of a comprehensive assay qualification. The following diagram illustrates its relationship with other essential validation parameters.
A fit-for-purpose qualification typically evaluates the following parameters in concert with spike and recovery [23] [24] [9]:
- Precision: The closeness of agreement between a series of measurements. This includes intra-assay precision (repeatability within a single plate) and inter-assay precision (reproducibility across different days, operators, or reagent lots) [24].
- Specificity: The ability of the assay to measure the analyte accurately in the presence of other components, such as the product protein, related isoforms, or formulation excipients. This is often confirmed via cross-reactivity studies or by using a negative control [24].
- Sensitivity: The lowest amount of analyte that can be reliably distinguished from zero, defined as the Lower Limit of Detection (LOD). The Lower Limit of Quantification (LLOQ) and Upper Limit of Quantification (ULOQ) define the assay range [24].
- Linearity and Range: The capacity of the assay to obtain results that are directly proportional to the analyte concentration within the LLOQ and ULOQ [2] [24].
- Robustness: A measure of the assay's capacity to remain unaffected by small, deliberate variations in method parameters (e.g., incubation times, temperatures), indicating its reliability during routine use [9].
Comparison of Analytical Platforms for Biomolecular Detection
While ELISA is the established workhorse for quantitative protein analysis, alternative technologies offer different advantages and limitations. The table below provides a comparative overview, with a focus on data provided for Surface Plasmon Resonance (SPR).
Table 2: Platform Comparison for Biomolecular Detection (ELISA vs. SPR) [26]
| Parameter | ELISA | Surface Plasmon Resonance (SPR) |
|---|---|---|
| Data Obtained | End-point concentration | Real-time affinity (KD) and kinetics (ka, kd) |
| Label Requirement | Requires enzyme-conjugated antibodies | Label-free |
| Experiment Length | Typically > 1 day | Significantly faster; minutes to hours |
| Detection of Low-Affinity Interactions | Poor (washed away in steps) | Effective |
| Throughput | High (96- or 384-well) | Moderate (varies by instrument) |
| Cost & Accessibility | Low cost, widely accessible | High upfront cost, lower operating costs for some systems |
| Best Suited For | High-throughput quantification of analytes in many samples | Detailed characterization of binding mechanisms |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful assay qualification relies on a suite of critical reagents and materials. The following table details key components and their functions.
Table 3: Essential Reagents and Materials for ELISA Qualification
| Item | Function in Qualification |
|---|---|
| Reference Standard | A purified analyte of known concentration and identity used to prepare the standard curve and spiking solutions; essential for defining accuracy [24]. |
| Critical Coating/Capture Antibody | The antibody immobilized on the plate to specifically bind the target analyte; its affinity and specificity are paramount [27]. |
| Detection Antibody | The antibody that binds the captured analyte; often conjugated to an enzyme (e.g., HRP) for signal generation. Must recognize a different epitope than the capture antibody in a sandwich ELISA [27]. |
| Validated Sample Diluent | The buffer used to dilute samples and standards. Its composition is optimized to match the sample matrix and minimize interference, a key factor in spike and recovery [2]. |
| Blocking Buffer | A solution of irrelevant protein (e.g., BSA) used to cover all unsaturated binding sites on the microplate to prevent non-specific binding and high background [27]. |
| Validated Substrate | The reagent converted by the reporter enzyme (e.g., HRP) into a measurable colorimetric, chemiluminescent, or fluorescent signal [27]. |
| Quality Control (QC) Samples | Samples with known, predetermined analyte concentrations used to monitor the precision and accuracy of each assay run [24]. |
Spike and recovery analysis is a non-negotiable element of fit-for-purpose assay qualification, serving as a direct experimental probe into the accuracy of an ELISA within a specific sample matrix. Its proper execution, guided by clearly defined regulatory acceptance criteria, is fundamental to generating data that instills confidence in the safety and efficacy assessments of biopharmaceuticals. While this guide has detailed its central role, it is crucial to remember that spike and recovery is one pillar in a comprehensive validation structure that also includes precision, specificity, and sensitivity. Together, these elements form an objective, evidence-based foundation that supports the entire drug development process, from early research to final product release, ensuring compliance with global regulatory standards and, ultimately, protecting patient health.
Executing a Spike and Recovery Experiment: A Step-by-Step Protocol
Establishing the Minimum Required Dilution (MRD) is a critical pre-experimental step in ELISA validation that ensures accurate quantification of analytes by mitigating matrix interference. This guide objectively compares the performance of different sample preparation strategies and diluents, providing supporting experimental data to help researchers identify optimal dilution factors. Within the broader context of spike and recovery experiments for ELISA validation, proper MRD determination serves as the foundation for reliable assay performance, enabling researchers to generate pharmacologically relevant data that complies with regulatory standards.
The Minimum Required Dilution (MRD) represents the lowest sample dilution that effectively minimizes matrix effects while maintaining the analyte concentration within the assay's quantifiable range [28]. In ELISA validation, determining the MRD is not merely a procedural step but a fundamental prerequisite that directly impacts the accuracy and reliability of all subsequent data, including spike and recovery results. Complex biological matrices such as serum, plasma, and urine contain numerous interfering components—including heterophilic antibodies, complement factors, lipids, and other proteins—that can profoundly affect antibody-binding kinetics and generate inaccurate measurements [24] [29].
Establishing the MRD represents a methodological compromise between sufficiently minimizing matrix interference and maintaining adequate analyte concentration for detection. A dilution that is too low may fail to eliminate matrix effects, while excessive dilution may push analyte concentrations below the assay's limit of quantification [28]. The MRD determination process empirically identifies this optimal balance for each unique sample matrix, ensuring that the condition of antibody excess is maintained across the diverse array of analytes present in samples such as Host Cell Proteins (HCPs) [28]. This is particularly crucial in drug development contexts, where accurate impurity quantification directly impacts product characterization and safety assessment.
Theoretical Framework: The Role of MRD in Assay Validation
Relationship Between MRD and Spike/Recovery Experiments
MRD determination and spike/recovery validation form an interdependent validation sequence in ELISA development. The MRD establishes the dilution framework within which spike/recovery experiments are conducted, creating a foundation for accurate recovery assessment [29] [28]. Without proper MRD establishment, spike/recovery results may be compromised by residual matrix effects, leading to either overestimation ("over-recovery") or underestimation ("under-recovery") of the actual analyte [29].
The conceptual relationship between these validation components follows a sequential logic: MRD determination first identifies the dilution that neutralizes matrix interference, then spike/recovery experiments verify that the chosen dilution yields accurate quantification of known analyte concentrations [2] [29]. This systematic approach ensures that the assay delivers reliable performance across different sample types and matrices, confirming that both the dilution factor and the sample matrix are appropriate for the intended application [28].
Consequences of Inadequate MRD Determination
Failure to establish appropriate MRD can lead to several analytical challenges that compromise data integrity. Poor dilution linearity may manifest when antibody excess is not maintained for one or more analytes in the sample, particularly in assays detecting multiple components such as HCP ELISAs [28]. This can result in a "high-dose hook effect" where high concentrations of specific analytes saturate their cognate antibodies, leading to under-quantification [28]. Additionally, certain "hitchhiker proteins" that interact with the product or become enriched during purification processes can further interfere with assay linearity [28].
Matrix components in product formulation buffers—such as extreme pH, high protein or salt concentrations, detergents, or organic solvents—can also interfere with ELISA quantification, resulting in either over- or under-estimation of the true analyte concentration [29] [28]. These interference effects typically manifest as non-parallelism in dilution curves, indicating differential immunoreactivity between the native protein in the sample and the reference standard protein used for calibration [24]. Such discrepancies may arise from post-translational modifications, protein complexation, or other matrix effects that alter antibody binding affinity [1].
Experimental Protocol for MRD Determination
Sample Preparation and Dilution Scheme
The MRD determination process begins with preparing serial dilutions of the test sample using an appropriate assay diluent. The recommended approach involves creating a doubling dilution series (e.g., neat, 1:2, 1:4, 1:8, etc.) until the predicted analyte concentration falls below the assay's lower limit of quantification [28] [1]. This dilution series should be prepared using the same diluent employed for standard curve generation to maintain consistency, unless preliminary data indicates that an alternative diluent provides superior performance [2].
For each sample type intended for routine testing—including in-process samples and final drug substance—separate MRD determinations should be performed [28]. This matrix-specific approach is necessary because different sample types may contain varying levels of interfering components that affect the assay differently. When working with complex samples containing multiple analytes, such as HCPs, it is advisable to pool multiple lots of samples to create a representative mixture that averages matrix effects across production batches [13]. This pooled sample then serves as the basis for the dilution linearity experiment, ensuring that the established MRD will be applicable across future sample variations.
Experimental Workflow and Data Collection
The following diagram illustrates the complete MRD determination workflow:
After running the ELISA assay, the dilution-corrected concentration for each dilution is calculated by multiplying the measured concentration by the corresponding dilution factor [28]. For example, a 1:4 dilution that yields a measured concentration of 78 ng/mL would have a dilution-corrected value of 312 ng/mL (78 × 4). These corrected values should remain relatively constant across dilutions when matrix effects have been sufficiently minimized and antibody excess conditions are met [28].
Data Interpretation and MRD Selection Criteria
The MRD is identified as the most concentrated (lowest) dilution in the series where the dilution-corrected values stabilize within an acceptable variance range [28]. According to industry standards, acceptable dilution linearity is achieved when corrected analyte concentrations vary no more than ±20% between doubling dilutions, provided the measured concentration (before correction) remains above two times the assay's limit of quantification (LOQ) [28].
The percentage change between successive dilutions is calculated using the formula: [(Corrected Valueₐ - Corrected Valueₐ₋₁) / Corrected Valueₐ₋₁] × 100% [28]. For instance, if a 1:2 dilution yields a corrected value of 233 ng/mL and the subsequent 1:4 dilution gives 312 ng/mL, the percent change would be calculated as [(312 - 233) / 233] × 100% = 34%, which exceeds the acceptable ±20% threshold [28]. In such cases, further dilution would be necessary until the percent change falls within the acceptable range.
Comparative Performance Data
Representative MRD Determination Data
The following table presents experimental data from a typical MRD determination study, illustrating how sample dilution affects corrected analyte concentrations and the subsequent identification of the appropriate MRD:
Table 1: Sample Dilution Linearity Data for MRD Determination [28]
| Sample Dilution | Dilution-Corrected Value (ng/mL) | % Change from Previous Dilution | Meets ±20% Criterion |
|---|---|---|---|
| Neat (undiluted) | 146 | NA | No |
| 1:2 | 233 | 60% | No |
| 1:4 | 312 | 34% | No |
| 1:8 | 361 | 16% | Yes |
| 1:16 | 356 | 1% | Yes |
| 1:32 | 370 | 4% | Yes |
| 1:64 | Not calculated (<2×LOQ) | NA | No |
Based on this data, the MRD would be established at 1:8 dilution, as it represents the most concentrated sample where the dilution-corrected values stabilize within the acceptable variance range (±20%) and remain above the assay's quantifiable limit [28]. The reported HCP concentration for this sample would be calculated as the average of the results at and below the MRD that remain above 2×LOQ (in this case, the average of 312, 361, 356, and 370 = 350 ng/mL) [28].
Comparison of Sample Matrices and Dilution Requirements
Different sample matrices demonstrate varying dilution requirements due to their unique composition and potential interfering components. The following table compares MRD results across different biological matrices:
Table 2: Comparison of MRD Across Sample Matrices [1]
| Sample Matrix | Endogenous Analyte Concentration | Established MRD | Recovery at MRD |
|---|---|---|---|
| Human Serum | Moderate | Neat | 83-124% |
| Mouse Serum | Low | 1:2 | 90-116% |
| Porcine Serum | High | 1:2 | 103-113% |
| Human Saliva | Variable | 1:2 | 83-108% |
| Fruit Extract | Variable | 1:2 | 88-116% |
This comparative data illustrates how matrix complexity and endogenous analyte levels influence the required dilution to achieve optimal recovery. Complex matrices such as serum typically require greater dilution (1:2) compared to simpler buffers, which may be tested neat [1]. The recovery percentages following MRD establishment should ideally fall within 75-125% according to ICH, FDA, and EMA guidelines [29].
Research Reagent Solutions for MRD Studies
Successful MRD determination requires carefully selected reagents and materials designed to maintain assay integrity while identifying optimal dilution factors. The following table outlines essential research reagent solutions for robust MRD studies:
Table 3: Essential Research Reagent Solutions for MRD Determination
| Reagent Solution | Function in MRD Studies | Performance Considerations |
|---|---|---|
| Assay Diluent | Base solution for preparing sample dilutions; should match standard diluent when possible | Composition should approximate sample matrix without interfering components; may contain stabilizing proteins like BSA [2] |
| Coated ELISA Plates | Solid phase for immuno-capture reaction | Should have high protein-binding capacity (>400 ng/cm²) and low well-to-well variation (CV <5%); clear for colorimetric, black/white for fluorescent detection [27] |
| Coating Buffer | Immobilizes capture antibody or antigen | Typically carbonate-bicarbonate buffer (pH 9.4) or PBS (pH 7.4); composition affects binding efficiency and stability [27] |
| Blocking Buffer | Covers unsaturated binding sites to prevent nonspecific binding | Various solutions including BSA, casein, or proprietary commercial formulations; requires optimization for specific sample types [24] [27] |
| Washing Buffer | Removes unbound reagents between steps | Typically PBS or Tris-based with detergent (e.g., Tween-20); critical for reducing background signal [24] |
| Reference Standard | Known concentration of analyte for standard curve generation | Should be identical to natural analyte when possible; serial dilutions must span assay dynamic range [24] [13] |
Troubleshooting and Optimization Strategies
Addressing Poor Dilution Linearity
When samples fail to demonstrate acceptable dilution linearity (±20% variance) even at high dilutions, several optimization strategies may be employed. The first approach involves further dilution of the sample until the corrected values stabilize, provided the measured concentration remains above 2×LOQ [28]. If additional dilution does not resolve the issue, modification of the assay protocol or alteration of the sample diluent may be necessary to improve accuracy for problematic sample types [28].
For persistent linearity issues, consider adjusting the standard diluent to more closely match the final sample matrix composition [2]. For example, if analyzing culture supernatants, using culture medium as the standard diluent may improve parallelism. Alternatively, modifying the sample matrix itself by adjusting pH to match the optimized standard diluent or adding carrier proteins like BSA can correct recovery problems [2]. In cases where the sample contains high background proteins (e.g., serum albumin), the optimal standard diluent may contain added protein while the sample diluent may not require additional protein [2].
Regulatory Considerations and Acceptance Criteria
When establishing MRD for regulated environments, adherence to established guidelines is essential. Regulatory agencies including ICH, FDA, and EMA specify that spike recovery values following proper dilution should fall within 75-125% of the expected concentration [29]. Similarly, dilution linearity is considered acceptable when corrected concentrations vary no more than ±20% between doubling dilutions [28].
For samples demonstrating significant product or matrix interference despite optimization attempts, it may be necessary to implement additional sample processing steps, such as extraction, precipitation, or chromatography, to remove interfering components before ELISA analysis [13]. In such cases, spiked matrix samples become essential for evaluating extraction efficiency by comparing the detected quantity of analyte after extraction to the known input quantity [13].
Establishing the Minimum Required Dilution represents a foundational element in the ELISA validation workflow, creating the necessary conditions for reliable spike/recovery assessment and accurate sample quantification. Through systematic dilution linearity testing and adherence to defined acceptance criteria (±20% variance between doubling dilutions), researchers can identify the optimal balance between minimizing matrix effects and maintaining adequate analyte detectability. The comparative data presented in this guide demonstrates how MRD requirements vary across sample matrices, emphasizing the need for matrix-specific validation approaches. By implementing the detailed protocols, reagent solutions, and troubleshooting strategies outlined herein, researchers can ensure their ELISA methods generate pharmacologically relevant data compliant with regulatory standards, ultimately supporting robust analytical decision-making in drug development and biomedical research.
In enzyme-linked immunosorbent assay (ELISA) development, the spike-and-recovery experiment is a fundamental validation tool used to assess assay accuracy and the influence of sample matrix effects. This method determines whether the biological sample matrix (e.g., serum, plasma, or tissue homogenate) affects the detection of the target analyte compared to the standard diluent used to generate the calibration curve [2] [1]. The core principle involves adding a known quantity of the purified analyte ("spiking") into the natural sample matrix and then measuring the amount recovered by the assay. Discrepancies between the measured value and the expected value indicate that components within the sample matrix are interfering with antigen-antibody binding, potentially leading to inaccurate quantification [2]. Addressing these issues is critical for ensuring that ELISA results are reliable, particularly in regulated environments like drug development [22].
The selection of appropriate spike concentrations is paramount to this process. A well-designed concentration series that covers the analytical range of the assay can diagnose problems and confirm the assay's robustness across the entire range of expected sample values, from the lower limit of quantification (LLOQ) to the upper limit of quantification (ULOQ) [1]. This guide will objectively compare strategies for selecting these concentrations, supported by experimental data and detailed protocols.
Theoretical Framework and Strategic Approaches
The strategic selection of spike concentrations is guided by the intended use of the ELISA. The sample matrix itself can cause interference through various mechanisms, including the presence of binding proteins, proteases, or high levels of lipids or bilirubin that may affect antibody affinity or the function of the reporter enzyme [2] [1]. The goal of spike-and-recovery is to quantify this interference.
Two primary strategic approaches exist for selecting spike concentrations, each serving a distinct purpose in assay validation:
- Covering the Analytical Range: This strategy involves spiking the sample matrix at multiple concentration levels that span the dynamic range of the standard curve. This is the most comprehensive approach as it verifies assay accuracy at low, mid, and high concentrations, ensuring the entire assay range is valid for the sample type [2] [1]. It is the recommended approach for full method validation.
- Bracketing the Minimum Required Performance Level (MRPL): In some applications, particularly in regulatory screening for residues like chloramphenicol in food, the critical requirement is to ensure accurate detection at a specific threshold. Here, spiking concentrations are chosen to bracket this MRPL (e.g., 0.15 to 0.60 ng/g, as demonstrated in a study on crab and shrimp muscle) to confirm the assay's performance at the level of regulatory concern [30].
The following table compares the strategic considerations for these two approaches:
Table 1: Strategic Approaches for Selecting Spike Concentrations
| Strategy | Objective | Typical Spike Levels | Key Application |
|---|---|---|---|
| Covering the Analytical Range [2] [1] | To validate assay accuracy across the entire standard curve, from Lower Limit of Quantification (LLOQ) to Upper Limit of Quantification (ULOQ). | Low, Medium, and High levels (e.g., near LLOQ, mid-point, and near ULOQ of the standard curve). | Full method validation for drug development, biomarker quantification, and research requiring precise measurement across a wide concentration range. |
| Bracketing the MRPL [30] | To confirm that the assay reliably detects the analyte at a specific, critically important concentration. | Concentrations slightly above and below the mandatory performance level (e.g., 0.15 and 0.60 ng/g for a 0.30 ng/g MRPL). | Regulatory screening and monitoring where detection at a defined threshold is legally required. |
The Critical Role of the Standard Diluent
A key principle in spike-and-recovery is the comparison of the analyte's behavior in the sample matrix versus the standard diluent [2]. The ideal recovery is observed when the standard diluent closely mimics the sample matrix. If the standard is diluted in a simple buffer like PBS while the sample is a complex matrix like serum, differences in recovery are likely. To mitigate this, the standard can be diluted in a matrix that more closely matches the sample, such as culture medium for cell supernatant samples or a defined solution of irrelevant protein like BSA for serum samples [2]. However, this may involve a trade-off with the assay's signal-to-noise ratio.
Experimental Protocol for Spike-and-Recovery
The following is a detailed, step-by-step protocol for performing a spike-and-recovery experiment designed to cover the analytical range.
Materials and Reagents
Table 2: Research Reagent Solutions for Spike-and-Recovery Experiments
| Item | Function/Description | Example |
|---|---|---|
| Purified Analyte | The known quantity of protein or antigen used for spiking. Should be identical or highly similar to the endogenous analyte. | Recombinant SARS-CoV-2 Spike protein [31]. |
| Sample Matrix | The biological fluid or extract being validated (e.g., serum, plasma, urine, tissue homogenate). | Pre-pandemic human serum [32], crab and shrimp muscle [30]. |
| Standard Diluent | The buffer used to prepare the standard curve. | Phosphate-buffered saline (PBS) often with a carrier protein like 1% BSA [2]. |
| Assay Buffer | The diluent used to prepare sample and standard serial dilutions. | PBS with 0.05% Tween 20 (PBS-T) [32]. |
| Negative Control Matrix | A confirmed source of the sample matrix that does not contain the target analyte. | Used to establish baseline and confirm the absence of endogenous interference. |
Step-by-Step Methodology
- Preparation of Spike Solutions: Prepare a concentrated stock solution of the purified analyte in a compatible buffer. From this stock, create working solutions for spiking at low, medium, and high concentrations.
- Sample Preparation:
- Spiked Sample Matrix: Aliquot a known volume of the negative control sample matrix. Add a known volume of the spike working solution to achieve the final desired concentrations (e.g., low near the LLOQ, medium at the EC50, and high near the ULOQ).
- Spiked Standard Diluent: Prepare identical spikes in the standard diluent. This serves as the control, representing 100% expected recovery.
- Unspiked Controls: Include wells with sample matrix alone and standard diluent alone to measure any background signal.
- ELISA Execution: Run the complete ELISA protocol on all prepared samples, including the standard curve, following the established workflow. All samples and controls should be run in duplicate or triplicate.
- Data Calculation and Analysis:
The logical flow and key comparisons of this experiment are summarized in the diagram below.
Data Interpretation and Performance Benchmarking
Acceptance Criteria
Ideal recovery is 100%, indicating no matrix interference. However, in practice, recoveries between 80% and 120% are generally considered acceptable for most ELISA applications [1]. The variability between replicate recoveries should also be low, with a coefficient of variation (%CV) typically below 15% [33].
Comparative Performance Data
The following table summarizes recovery data from published studies, illustrating how different matrices and analytes can affect performance.
Table 3: Experimental Spike-and-Recovery Data from Literature
| Sample Matrix | Analyte | Spike Level | Observed Recovery (%) | Reference / Kit |
|---|---|---|---|---|
| Human Urine (n=9) | Recombinant Human IL-1 beta | Low (15 pg/mL) | 86.3% | Novex IL-1 beta ELISA Kit [2] |
| Medium (40 pg/mL) | 85.8% | |||
| High (80 pg/mL) | 84.6% | |||
| Crab & Shrimp Muscle | Chloramphenicol | 0.15 - 0.60 ng/g | 102 - 107% | Ridascreen ELISA Kit [30] |
| Porcine Serum (Extracted) | Not Specified | 3.0 ng/mL | 102.8% | Enzo Life Sciences (Example) [1] |
| 0.6 ng/mL | 107.8% | |||
| 0.12 ng/mL | 112.5% |
Troubleshooting Poor Recovery
- Problem: Low Recovery (<80%): The sample matrix is inhibiting antibody binding or enzyme activity. Solution: Dilute the sample in the standard diluent or a modified buffer. Alternatively, alter the standard diluent to more closely match the sample matrix (e.g., by adding a carrier protein) [2].
- Problem: High Recovery (>120%): The sample matrix may contain substances that cause non-specific binding or amplify the signal. Solution: Improve blocking conditions, increase the number or stringency of washes, or dilute the sample to minimize these effects [33].
Complementary Validation Experiments
Spike-and-recovery is one component of a comprehensive ELISA validation. Two other key experiments are:
- Linearity of Dilution: Assesses whether a sample can be reliably diluted and still provide accurate results. A sample with a high concentration of the endogenous analyte is serially diluted. Good linearity is shown when the calculated concentration, after accounting for the dilution factor, remains constant [2] [1].
- Parallelism: Determines if the antibody has comparable affinity for the endogenous analyte in the sample and the purified standard used for the curve. It is tested by serially diluting a sample with a high endogenous level of the analyte. A loss of parallelism (high %CV between dilutions) suggests a difference in immunoreactivity, potentially due to post-translational modifications in the native protein [1] [22].
Selecting appropriate spike concentrations to cover the analytical range is a critical, non-negotiable step in ELISA validation for rigorous scientific and drug development research. The data generated provides direct evidence of the assay's accuracy and reveals the presence of matrix effects that could compromise data integrity. While commercial kits offer a starting point, performance must be verified for each specific sample matrix. A systematic approach—using multiple spike levels, comparing against the standard diluent, and applying corrective strategies when recovery falls outside acceptable limits—ensures the generation of reliable, high-quality quantitative data. This foundational work supports robust decision-making in both research and clinical applications.
In the development and validation of Enzyme-Linked Immunosorbent Assays (ELISAs), the spike and recovery experiment is a fundamental analytical procedure used to assess assay accuracy and identify matrix effects [2]. This method systematically compares the detection of a known analyte amount between a controlled standard diluent and a biological sample matrix, determining whether components in the sample matrix interfere with analyte detection [2] [1]. The core question this experiment addresses is whether the sample matrix affects the immunoassay's ability to detect the analyte compared to the ideal conditions of the standard diluent [1]. When sample matrix effects are identified, researchers can make adjustments such as altering the standard diluent composition to more closely match the sample matrix or diluting the biological sample in a more compatible diluent to correct for these discrepancies [2].
Core Concepts and Experimental Principles
Purpose and Importance of Matrix Comparison
Spiking a known amount of analyte into both the standard diluent and the natural sample matrix serves a critical purpose: it quantifies the difference in assay response between these two environments [2]. The ideal scenario is identical recovery percentages, indicating that the sample matrix does not interfere with antibody-analyte binding or the detection system. However, biological matrices often contain components such as salts, proteins, lipids, or other macromolecules that can inhibit or enhance the assay signal, leading to inaccurate quantification [1]. Validating the assay through spike and recovery is therefore essential before employing an ELISA for quantitative analysis of unknown samples, as it establishes the reliability of the measurements within a specific matrix [1].
Relationship with Other Validation Parameters
Spike and recovery is closely related to, and often performed alongside, the assessment of linearity of dilution [2]. While spike and recovery tests the effect of the matrix at a specific concentration, linearity of dilution evaluates whether this effect remains consistent across different sample dilutions [2]. Poor performance in either parameter indicates that the natural sample matrix, the sample diluent, and/or the standard diluent affect analyte detectability differently. The causes—often related to interfering components whose influence changes with concentration—are frequently the same for both poor spike recovery and poor linearity [2]. Another related parameter is parallelism, which specifically determines if samples with high endogenous levels of the analyte demonstrate the same immunoreactivity as the standard curve analyte after dilution, revealing differences in antibody binding affinity [1].
Comparative Experimental Protocols
Protocol for Spiking into Standard Diluent
The standard diluent is typically an optimized buffer solution designed to maximize the assay's signal-to-noise ratio.
- Preparation of Spiked Standard Diluent: A known, purified quantity of the recombinant analyte or protein standard is spiked (added) into the standard diluent. This creates a reference sample where the expected concentration is known precisely [2].
- Assay Execution: The spiked standard diluent is run in the ELISA alongside a standard curve, which is also prepared in the same standard diluent [2].
- Calculation of Recovery: The observed concentration of the spike is calculated based on the standard curve. The percent recovery is determined using the formula:
- Recovery % = (Observed Concentration / Expected Concentration) × 100 [1]. A recovery of 100% indicates perfect detection in the ideal matrix.
Protocol for Spiking into Sample Matrix
The sample matrix is the biological fluid (e.g., serum, plasma, urine, cell culture supernatant) in which the endogenous analyte is to be measured.
- Preparation of Spiked Sample Matrix: The same known quantity of analyte is spiked into the natural, neat (undiluted) biological sample matrix. It is critical to account for any endogenous analyte already present in the sample [2].
- Assay Execution: The spiked sample matrix is run in the ELISA, and its observed concentration is determined from the standard curve [2].
- Calculation of Recovery and Correction for Endogenous Level: The recovery calculation must subtract the endogenous signal from the observed value to isolate the signal from the spike alone [2].
- Corrected Observed Concentration = Observed Concentration (Spiked Sample) – Observed Concentration (Unspiked Sample)
- Recovery % = (Corrected Observed Concentration / Expected Concentration) × 100
Workflow Diagram
The following diagram illustrates the parallel workflows for spiking into standard diluent versus sample matrix and how the results are interpreted.
Data Interpretation and Performance Comparison
Acceptance Criteria and Quantitative Comparison
The interpretation of spike and recovery data relies on comparing the recovery percentages from the sample matrix against those from the standard diluent. The following table summarizes typical acceptance criteria and the implications of the results.
- Table 1: Interpretation of Spike and Recovery Results
Recovery Percentage Interpretation Required Action 80% - 120% [1] Acceptable recovery; minimal matrix interference. The sample matrix is valid for the assay procedure as-is [2]. < 80% or > 120% [1] Poor recovery; significant matrix interference. Assay requires optimization (e.g., change diluent, dilute sample, add carrier protein) [2].
The data from a spike and recovery experiment is often summarized in a table for clear comparison. The example below, based on a validation study for a human IL-1 beta ELISA, shows how recovery can be calculated at multiple spike concentrations across different sample matrices.
- Table 2: Example ELISA Spike and Recovery Data for Human IL-1 Beta in Urine Samples [2]
Sample (n) Spike Level Expected (pg/mL) Observed (pg/mL) Recovery % Diluent Control Low (15 pg/mL) 17.0 17.0 100.0% Urine (9) Low (15 pg/mL) 17.0 14.7 86.3% Diluent Control Medium (40 pg/mL) 44.1 44.1 100.0% Urine (9) Medium (40 pg/mL) 44.1 37.8 85.8% Diluent Control High (80 pg/mL) 81.6 81.6 100.0% Urine (9) High (80 pg/mL) 81.6 69.0 84.6%
Troubleshooting Poor Recovery
When recovery falls outside the acceptable range, it indicates that the sample matrix is interfering with the assay. Two primary adjustments can be made to the method [2]:
- Alter the Standard Diluent: The composition of the standard diluent can be modified to more closely match the sample matrix. For example, if analyzing culture supernatants, using culture medium as the standard diluent may improve recovery. This may, however, compromise the assay's signal-to-noise ratio [2].
- Alter the Sample Matrix: The biological sample can be diluted in the standard diluent or an alternative sample diluent. Diluting a serum sample 1:1, for instance, can often reduce interference from background proteins. Additionally, adjusting the sample matrix's pH or adding a carrier protein like BSA can improve recovery [2].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials required for performing robust spike and recovery experiments.
- Table 3: Essential Reagents and Materials for ELISA Spike and Recovery Experiments
Item Function in the Experiment Purified Recombinant Analyte The known quantity of protein used for spiking into the standard diluent and sample matrix. It serves as the reference material [2]. Optimized Standard Diluent A buffer solution (e.g., PBS with 1% BSA) designed to provide an ideal environment for the immunoassay, used to create the standard curve and as a control for spiking [2]. Biological Sample Matrix The test fluid from the study (e.g., serum, urine, cell culture supernatant) whose potential interference is being evaluated [2] [34]. Sample Diluent A buffer used to dilute the biological sample matrix to reduce interference while maintaining analyte detectability [2]. Matched Antibody Pair (for sandwich ELISA) The capture and detection antibodies that are specific to the analyte. Their quality and specificity are paramount for accurate detection [35]. Blocking Buffer A solution (e.g., containing BSA or synthetic blockers) used to cover non-specific binding sites on the microplate to prevent false-positive signals [34]. Microplate Reader A spectrophotometer capable of measuring the absorbance (e.g., at 450 nm for TMB substrate) of all wells in a 96-well plate to quantify the assay output [34].
The direct comparison between spiking into a sample matrix versus a standard diluent is a non-negotiable step in rigorous ELISA validation. This procedure objectively reveals how the complex environment of a biological sample influences analyte quantification, which is invisible when using only the ideal conditions of a standard diluent. By implementing the detailed protocols for both paths, correctly calculating recovery, and applying systematic troubleshooting, researchers can ensure their ELISA data is accurate, reliable, and fit-for-purpose in both research and diagnostic applications.
Spike-and-recovery experiments are fundamental for validating the accuracy of enzyme-linked immunosorbent assays (ELISAs) and other immunoassays in bioanalytical research and drug development. These experiments quantify the percentage recovery of a known analyte amount spiked into a biological sample matrix, identifying potential matrix interferences that compromise data integrity. This guide details the standardized methodologies for calculating percentage recovery, interprets the results against industry-accepted criteria, and provides supporting experimental data. Mastery of these calculations is essential for researchers and scientists to ensure their immunoassays are fit-for-purpose, yielding reliable and reproducible quantitative data.
In immunoassay development, the sample matrix—such as serum, plasma, or cell culture supernatant—often contains components that can interfere with antibody-antigen binding. This interference can lead to an overestimation or underestimation of the target analyte's concentration [2] [36]. A spike-and-recovery experiment is designed to assess this effect by determining whether the assay can accurately detect a known quantity of analyte introduced into the complex sample matrix [22]. The core principle involves adding ("spiking") a known concentration of a purified analyte standard into the natural test sample matrix and into an ideal standard diluent. The assay is then run to measure the concentration of the analyte in both the spiked sample and the spiked diluent. The percentage recovery is calculated to quantify the agreement between the observed value in the sample matrix and the expected value from the standard diluent [2] [5]. This metric is a critical indicator of assay accuracy and the absence of matrix effects.
Experimental Protocol for Spike-and-Recovery
Core Workflow
The following diagram outlines the fundamental workflow for performing a spike-and-recovery experiment.
Detailed Methodology
- Spike Preparation: A known amount of purified recombinant analyte (the "spike") is added to both the natural sample matrix (e.g., undiluted serum) and to the standard diluent used to prepare the standard curve (e.g., phosphate-buffered saline). It is recommended to use 3-4 different spike concentrations covering the analytical range of the assay, ensuring the lowest is at least 2 times the assay's Limit of Quantitation (LOQ) [36].
- Control Samples: A crucial control involves preparing a sample where the "zero standard" (assay diluent) is added to the sample matrix instead of the spike stock. This measures the endogenous level of the analyte already present in the sample, which must be accounted for in the final calculation [36].
- Assay Execution: All spiked samples and controls are run in the ELISA following the standard protocol, ideally in duplicate or triplicate to ensure statistical reliability [4].
- Data Collection: The absorbance values are converted into concentrations using the standard curve. The total measured concentration in the spiked sample matrix and the measured concentration of the spike prepared in the standard diluent are recorded.
Calculating Percentage Recovery
The Fundamental Formula
The percentage recovery is calculated to determine the proportion of the spiked analyte that is accurately measured in the sample matrix. The standard formula is: % Recovery = (ConcentrationSpiked Sample - ConcentrationEndogenous) / ConcentrationControl Spike × 100% [5] [36]
Where:
- ConcentrationSpiked Sample: The total concentration measured in the sample matrix after the spike has been added.
- ConcentrationEndogenous: The concentration of the analyte naturally present in the sample matrix before spiking (measured from the zero-standard control).
- ConcentrationControl Spike: The concentration measured when the analyte is spiked into the standard diluent [2].
This calculation corrects for any background signal and directly tests the effect of the matrix on analyte detection.
Interpretation of Results and Acceptance Criteria
The calculated percentage recovery indicates the degree of interference from the sample matrix. According to ICH, FDA, and EMA guidelines on analytical procedure validation, recovery values within 75% to 125% are generally considered acceptable [36] [1] [37]. Recoveries outside this range indicate significant matrix interference.
- Under-Recovery (<75%): Suggests components in the sample matrix are inhibiting antibody binding or degrading the analyte, leading to an underestimation of the true concentration.
- Over-Recovery (>125%): Suggests non-specific binding or interaction of matrix components with assay reagents, leading to an overestimation of the true concentration [36].
Table 1: Interpretation of Percentage Recovery Results
| Recovery Range | Interpretation | Potential Cause |
|---|---|---|
| 75% - 125% | Acceptable [36] [37] | Minimal matrix interference; assay is accurate for this sample type. |
| < 75% | Under-Recovery | Matrix components inhibit antibody binding or degrade the analyte [36]. |
| > 125% | Over-Recovery | Non-specific binding or matrix components interact with assay reagents [36]. |
Representative Data and Comparison
The following table presents real experimental data from a spike-and-recovery experiment for recombinant human IL-1 beta in human urine samples, illustrating the calculation and its outcomes [2].
Table 2: ELISA Spike-and-Recovery Data for Recombinant Human IL-1 Beta in Human Urine [2]
| Sample | No Spike (0 pg/mL) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|---|
| Diluent Control | 0.0 | 17.0 | 44.1 | 81.6 |
| Donor 1 | 0.7 | 14.6 | 39.6 | 69.6 |
| Donor 2 | 0.0 | 17.8 | 41.6 | 74.8 |
| Donor 3 | 0.6 | 15.0 | 37.6 | 68.9 |
| ... | ... | ... | ... | ... |
| Mean Recovery (% ± S.D.) | NA | 86.3% ± 9.9% | 85.8% ± 6.7% | 84.6% ± 3.5% |
Calculation Example for Low Spike (Donor 1):
- ConcentrationSpiked Sample = 14.6 pg/mL
- ConcentrationEndogenous = 0.7 pg/mL
- ConcentrationControl Spike = 17.0 pg/mL
- % Recovery = (14.6 - 0.7) / 17.0 × 100% = 81.8%
This data, summarized from multiple donors, shows consistent recoveries between 84-87%, which is within the acceptable range, indicating the urine matrix does not cause significant interference for this specific ELISA [2].
The Scientist's Toolkit: Essential Research Reagents
Successful spike-and-recovery experiments require carefully selected reagents and controls. The following table details key materials and their functions.
Table 3: Key Reagent Solutions for Spike-and-Recovery Experiments
| Reagent / Solution | Function in the Experiment |
|---|---|
| Purified Recombinant Analyte | Serves as the "spike"; must be identical to the target protein for accurate quantification [2]. |
| Standard Diluent | The solution used to prepare the standard curve; a chemically defined buffer like PBS [2]. |
| Sample Matrix | The biological sample being validated (e.g., serum, plasma, urine, cell culture supernatant) [2] [38]. |
| Matrix-Matched Standard Diluent | A diluent whose composition more closely matches the sample matrix; used to correct for matrix effects [2] [4]. |
| Zero Standard (Assay Diluent) | Added to the sample matrix to measure the endogenous analyte level; critical for the recovery calculation [36]. |
Troubleshooting Poor Recovery
If the percentage recovery falls outside the acceptable range, several corrective actions can be taken:
- Alter the Sample Matrix: Dilute the neat biological sample in the standard diluent or a logical sample diluent. Dilution can reduce the concentration of interfering components [2] [4]. The Minimum Required Dilution (MRD) should be established through dilution linearity studies [36].
- Alter the Standard Diluent: Prepare the standard curve in a matrix that more closely matches the sample, such as culture medium for cell supernatants or a serum diluent for serum samples. This ensures that matrix effects are present in both the standards and samples, allowing for more accurate comparison [2] [4].
- Modify the Sample Diluent: Adjust the pH of the sample matrix to match the standard diluent or add a carrier protein like BSA to stabilize the analyte and prevent non-specific binding [2].
Determining percentage recovery is a non-negotiable step in ELISA validation for researchers and drug development professionals. By systematically spiking a known analyte into a sample matrix and applying the correct calculation, scientists can objectively quantify matrix interference and validate the accuracy of their assay data. Adherence to the experimental protocols and acceptance criteria outlined in this guide ensures that bioanalytical results are reliable, reproducible, and suitable for making critical decisions in research and development.
In the rigorous world of bioanalytical method development, the spike-and-recovery experiment is a fundamental procedure for validating Enzyme-Linked Immunosorbent Assays (ELISAs). It quantitatively assesses whether the sample matrix (e.g., serum, plasma, urine) interferes with the accurate detection and quantification of the target analyte. The resulting recovery percentage is a key metric, indicating the assay's accuracy and reliability. For researchers, scientists, and drug development professionals, interpreting this percentage against an acceptable range is critical for determining an assay's fitness-for-purpose. This guide objectively compares the recovery ranges stipulated by various guidelines and commercial kit manufacturers, providing a framework for robust ELISA validation.
Defining Acceptable Recovery Ranges: A Comparative Analysis
The acceptable range for spike recovery is not a single universal value but is context-dependent, influenced by the sample matrix complexity and the specific regulatory or performance standards applied. The following table summarizes the acceptable recovery ranges from various authoritative sources.
Table 1: Comparison of Acceptable Recovery Ranges from Different Sources
| Source / Context | Stated Acceptable Recovery Range | Notes and Application Context |
|---|---|---|
| ICH, FDA, EMA Guidelines [39] | 75% - 125% | Considered acceptable in accordance with regulatory guidelines for analytical procedure validation. |
| Commercial ELISA Kit Manufacturers (Novus Bio, Bio-Techne) [40] [5] | 80% - 120% | A common acceptability criterion for commercial kits to ensure performance across various sample types. |
| Commercial ELISA Kit Manufacturers (Abcam) [41] | ≥ 80% | A minimum threshold for recommending a kit for a specific sample type. |
| Technical Literature (Enzo) [1] | 80% - 120% | Deviations of 20% or less from 100% are generally considered acceptable. |
Experimental Protocol: How to Perform a Spike-and-Recovery Experiment
A properly executed experiment is essential for generating reliable recovery data. The methodology below outlines the standard protocol.
Objective
To determine the accuracy of an ELISA by measuring the recovery of a known amount of analyte spiked into a specific sample matrix, thereby identifying any matrix effects.
Materials and Reagents
Table 2: Research Reagent Solutions for Spike-and-Recovery Experiments
| Reagent / Material | Function / Description |
|---|---|
| Purified Analyte Standard | A known concentration of the recombinant or native protein used for spiking. |
| Biological Sample Matrix | The test sample (e.g., serum, plasma, urine, cell culture supernatant). |
| Standard Diluent | The buffer used to prepare the standard curve, often provided in ELISA kits. |
| Assay Diluent ("Zero Standard") | A control diluent, typically free of the analyte, used to prepare the control spike. |
| ELISA Kit | Includes pre-coated plate, detection antibodies, wash buffer, substrate, and stop solution. |
Step-by-Step Workflow
Figure 1: Spike-and-Recovery Experimental Workflow
- Prepare the Sample Matrix: Use the biological sample of interest (e.g., final drug product, serum). It is often tested at the Minimum Required Dilution (MRD), which is determined from prior dilution linearity studies [39].
- Spike the Sample: Introduce ("spike") a known amount of purified analyte standard into the sample matrix. This is typically done for 3-4 concentration levels covering the assay's analytical range [39]. For example, spike 100 µL of a 100 ng/mL standard into 400 µL of the "neat" sample, resulting in a final spike concentration of 20 ng/mL [39].
- Prepare the Control Spike: In parallel, spike the same known amount of analyte into the standard diluent or assay diluent. This control measures the recovery in an ideal, interference-free matrix and serves as the baseline for comparison [2].
- Run the ELISA Assay: Analyze both the sample spike and the control spike using the standard ELISA protocol. The sample should also be run unspiked to determine its endogenous level of the analyte [2] [39].
- Calculate the Percentage Recovery: Use the following formula to calculate the recovery for the sample matrix [5] [39].
- % Recovery = (ConcentrationSpiked Sample - ConcentrationEndogenous) / ConcentrationControl Spike × 100%
Representative Data and Interpretation
The following table illustrates a sample data set and the recovery calculation.
Table 3: Example Spike-and-Recovery Data Set and Calculation
| Sample Description | Spike Concentration (ng/mL) | Total HCP Measured (ng/mL) | Calculation | % Recovery |
|---|---|---|---|---|
| Neat Sample (Unspiked) | 0 | 6 | N/A | N/A |
| Sample Matrix Spike | 20 | 25 | (25 - 6) / 20 | 95% |
| Control Diluent Spike | 20 | 20 | (20 - 0) / 20 | 100% |
In this example, the recovery of 95% falls well within the acceptable ranges (e.g., 75-125% or 80-120%), indicating minimal matrix interference and that the assay is accurate for this sample type [39].
Troubleshooting Poor Recovery: Practical Solutions for Researchers
Recovery values outside the acceptable range indicate matrix interference. The following table outlines common issues and corrective actions.
Table 4: Troubleshooting Guide for Poor Spike-and-Recovery Results
| Problem | Potential Cause | Corrective Action |
|---|---|---|
| Under-Recovery (<75-80%) | Components in the sample matrix (e.g., proteases, high salt, detergents) inhibit antibody binding or degrade the analyte [2] [39]. | Further dilute the sample to reduce the concentration of interfering substances [2] [1]. Alter the sample diluent (e.g., change pH, add a carrier protein like BSA) to better match the standard diluent [2]. |
| Over-Recovery (>120-125%) | The drug substance or other matrix component non-specifically interacts with the capture or detection antibody, enhancing the signal [39]. | Increase the dilution factor to minimize non-specific interactions. Re-optimize the assay protocol, such as blocking conditions or wash stringency, to reduce background signal [39]. |
| Poor Recovery Across All Samples | The standard diluent composition is significantly different from the final sample matrix [2]. | Alter the standard diluent to more closely match the sample matrix. For example, use culture medium as the standard diluent if samples are culture supernatants [2]. |
Interpreting recovery results within the 75-125% (regulatory) or 80-120% (general R&D) acceptability ranges is a decisive step in qualifying an ELISA. However, spike-and-recovery is not a standalone metric. It is intrinsically related to other validation parameters like dilution linearity and parallelism [2] [1]. A comprehensive validation strategy ensures that an ELISA method is not only accurate but also precise, specific, and robust, generating data that is reliable for both research conclusions and regulatory submissions.
For researchers, scientists, and drug development professionals, the enzyme-linked immunosorbent assay (ELISA) serves as a fundamental tool for quantifying peptides, proteins, and hormones in biological fluids with accuracy, reliability, and sensitivity [14]. The technique detects antigen-antibody interactions using enzyme-labelled conjugates and substrates that generate measurable color changes [14]. However, the reliability of ELISA results depends heavily on proper validation to ensure that sample matrix effects do not interfere with analyte detection. Spike-and-recovery and linearity-of-dilution experiments are critical validation methods that determine whether analyte detection is affected by differences between the standard curve diluent and the biological sample matrix [2]. Effective presentation of the quantitative data generated from these experiments is equally crucial, as it enables scientists to quickly assess assay performance, identify potential issues, and communicate findings clearly to stakeholders [42] [43]. This guide compares effective formats for summarizing ELISA validation results, providing structured methodologies, visualization techniques, and reagent specifications to support rigorous assay validation.
Key ELISA Validation Experiments
Spike-and-Recovery Experiments
Spike-and-recovery experiments determine whether the biological sample matrix affects the detection of the analyte compared to the standard diluent [2]. In this procedure, a known amount of purified analyte is added (spiked) into the natural test sample matrix, and the assay measures the recovery of this spiked analyte compared to an identical spike in the standard diluent [2] [1]. The experiment follows this fundamental principle: if the recovery observed for the spike in the sample matrix is identical to the analyte prepared in standard diluent, the sample matrix is considered valid for the assay procedure [2]. Discrepancies indicate that components in the sample matrix are interfering with detection, necessitating method adjustments [2].
Ideal sample matrices should achieve 100% recovery, though deviations of ±20% are generally considered acceptable [1]. Recoveries outside this range indicate significant differences between the natural sample matrix and the standard diluent, potentially caused by salts, pH, detergents, protein interactions, or other elements that interfere with antibody binding [1]. The following workflow diagram illustrates the key decision points in a spike-and-recovery experiment:
Linearity-of-Dilution Assessment
Linearity-of-dilution experiments evaluate the precision of results for samples tested at different dilution levels in a chosen sample diluent [2]. This assessment provides information about whether a spiked or natural sample's dose response is linear and falls within the desired assay range [2]. Good linearity across a wide dilution range offers flexibility to assay samples with varying analyte concentrations, enabling researchers to dilute high-concentration samples to fit within the standard curve range while comparing them to low-concentration samples assayed without dilution [2].
There are two primary methodological approaches for linearity-of-dilution experiments. The traditional method involves using a low-level sample containing a known spike of analyte and testing several different dilutions of that sample in the chosen sample diluent [2]. The alternative method involves preparing several dilutions of a low-level sample first, then spiking the same known amount of analyte into each one before testing [2]. Assay recovery is assessed by comparing observed versus expected values based on non-spiked and/or neat (undiluted) samples [2].
Parallelism Testing
Parallelism testing determines whether actual samples containing high endogenous analyte concentrations provide the same degree of detection in the standard curve after dilutions [1]. This validation step signifies differences in antibody binding affinity to endogenous analyte versus standard/calibration analyte [1]. The key distinction from dilutional linearity is that parallelism utilizes samples containing high levels of endogenous analyte rather than spiked standard analyte [1].
The parallelism experiment protocol involves: (1) identifying at least three samples with high concentrations of endogenous analyte (without exceeding the upper limit of quantification); (2) performing 1:2 serial dilutions using sample diluent until predicted concentration falls below the lower limit of quantification; (3) analyzing neat and diluted sample optical density while factoring in dilution factors; and (4) determining mean concentrations with dilution factors calculated and computing the percentage coefficient of variation (%CV) [1]. A %CV within 20-30% of expectations generally indicates successful parallelism, though exact acceptable percentages should be determined by end users based on their specific assay requirements [1].
Data Presentation Formats for ELISA Validation
Structured Tables for Quantitative Data
Effective data presentation begins with clearly structured tables that enable direct comparison of experimental results. For ELISA validation studies, specific table formats have proven particularly effective for different types of validation data:
Table 1: Spike-and-Recovery Results Presentation
| Sample (n) | Spike Level | Expected (pg/mL) | Observed (pg/mL) | Recovery (%) |
|---|---|---|---|---|
| Urine (9) | Low (15 pg/mL) | 17.0 | 14.7 | 86.3 |
| Urine (9) | Medium (40 pg/mL) | 44.1 | 37.8 | 85.8 |
| Urine (9) | High (80 pg/mL) | 81.6 | 69.0 | 84.6 |
| Serum (6) | Low (15 pg/mL) | 17.0 | 15.2 | 89.4 |
| Serum (6) | Medium (40 pg/mL) | 44.1 | 39.1 | 88.7 |
| Serum (6) | High (80 pg/mL) | 81.6 | 73.9 | 90.6 |
Source: Adapted from representative ELISA data [2]
This tabular format immediately draws attention to the recovery percentages, allowing quick assessment of whether results fall within the acceptable 80-120% range [2] [1]. Including the number of replicates (n) provides important context about the experimental design, while separate rows for different sample matrices facilitate direct comparison across sample types.
Table 2: Linearity-of-Dilution Results Presentation
| Sample | Dilution Factor (DF) | Observed (pg/mL) × DF | Expected (pg/mL) | Recovery (%) |
|---|---|---|---|---|
| ConA-stimulated Cell Culture Supernatant | Neat | 131.5 | 131.5 | 100 |
| 1:2 | 149.9 | 114 | ||
| 1:4 | 162.2 | 123 | ||
| 1:8 | 165.4 | 126 | ||
| High-level Serum Sample | Neat | 128.7 | 128.7 | 100 |
| 1:2 | 142.6 | 111 | ||
| 1:4 | 139.2 | 108 | ||
| 1:8 | 171.5 | 133 |
Source: Adapted from ELISA linearity-of-dilution results [2]
This layout effectively demonstrates how recovery percentages change with different dilution factors, highlighting potential matrix effects at specific dilutions. The inclusion of the neat sample as a baseline (100% recovery) provides a reference point for evaluating diluted samples.
Table 3: Parallelism Testing Results
| Sample Type | Endogenous Concentration (pg/mL) | Dilution Factor | %CV (Intra-assay) | %CV (Inter-assay) | Parallelism Assessment |
|---|---|---|---|---|---|
| Corticosterone | 171 | 1:2 | 8.0 | 13.1 | Acceptable |
| 403 | 1:4 | 8.4 | 8.2 | Acceptable | |
| 780 | 1:8 | 6.6 | 7.8 | Acceptable | |
| Custom Assay A | 150 | 1:2 | 25.3 | 31.2 | Borderline |
| 350 | 1:4 | 28.7 | 35.9 | Unacceptable |
Source: Adapted from parallelism validation data [1]
This format emphasizes the percentage coefficient of variation (%CV) across dilutions, with clear assessment indicators for quick interpretation. Separating intra-assay and inter-assay %CV provides insights into both precision and reproducibility aspects of parallelism.
Data Visualization Techniques
Beyond tabular data presentation, effective visualization enhances interpretation and communication of ELISA validation results. The following diagram illustrates the decision-making workflow for troubleshooting failed validation experiments:
Color and Design Principles for Scientific Data
When creating data visualizations for ELISA validation results, strategic use of color and design enhances comprehension and accessibility:
- Color Contrast: Ensure a minimum contrast ratio of 4.5:1 for text against background and 3:1 for adjacent data elements like bars or pie wedges [44].
- Accessibility: Avoid using color as the only way to convey meaning; supplement with patterns, shapes, or text labels to accommodate color vision deficiencies [44] [45].
- Color Psychology: Leverage color associations (red for urgency/warning, blue for trust/calmness, green for growth/positive outcomes) to guide interpretation [46].
- Palette Types: Use qualitative palettes for categorical variables, sequential palettes for ordered numeric values, and diverging palettes to show data on a spectrum [46].
- Color Limitation: Restrict visualizations to seven or fewer colors to prevent cognitive overload and improve processing speed [46].
Experimental Protocols
Detailed Spike-and-Recovery Protocol
- Sample Preparation: Prepare the natural test sample matrix and standard diluent. If using biological samples like serum or plasma, process them according to established protocols [14].
- Spiking: Add a known concentration of purified analyte to both the sample matrix and standard diluent. Use at least three different spike concentrations (low, medium, high) to evaluate recovery across the assay range [2].
- Assay Execution: Run the ELISA according to established protocols. Include a standard curve with known concentrations of the analyte prepared in standard diluent [2] [47].
- Calculation: Determine the concentration of the spiked samples using the standard curve. Calculate percentage recovery as: (Observed concentration / Expected concentration) × 100 [2] [1].
- Interpretation: Compare recovery between sample matrix and standard diluent. Recovery of 100% indicates no matrix effects, while recoveries of 80-120% are generally considered acceptable [1].
Linearity-of-Dilution Protocol
- Sample Selection: Identify samples with known high concentrations of the target analyte, either through endogenous presence or spiking [2].
- Dilution Series: Prepare a series of dilutions (e.g., 1:2, 1:4, 1:8, 1:16) in the chosen sample diluent. Use fresh pipette tips for each dilution to ensure accuracy [2] [47].
- Assay Execution: Analyze all dilutions in the same ELISA run alongside a standard curve [2].
- Data Analysis: Multiply the observed concentration by the dilution factor for each sample. Compare these values to the expected concentration (typically the neat sample value) [2].
- Assessment: Calculate recovery percentages for each dilution. Good linearity demonstrates consistent recovery percentages across dilutions, while poor linearity shows significant deviation from expected values [2].
Parallelism Testing Protocol
- Sample Identification: Select at least three samples with high endogenous analyte concentrations that do not exceed the upper limit of quantification [1].
- Dilution Preparation: Perform 1:2 serial dilutions using appropriate sample diluent until the predicted concentration falls below the lower limit of quantification [1].
- Assay Analysis: Run the ELISA on all dilutions alongside a standard curve. Only use sample values that fall within the standard curve range for analysis [1].
- Statistical Analysis: Calculate mean concentrations with dilution factors applied. Determine the percentage coefficient of variation (%CV) across dilutions [1].
- Interpretation: A %CV within 20-30% generally indicates acceptable parallelism, though specific thresholds should be established based on assay requirements [1].
The Scientist's Toolkit: Research Reagent Solutions
Successful ELISA validation requires specific reagents and materials carefully selected for their functions in the assay system. The following table details essential components and their applications:
Table 4: Essential Research Reagents for ELISA Validation
| Reagent/Material | Function | Specification Guidelines |
|---|---|---|
| Purified Protein Standard | Serves as reference for standard curve preparation | Use purified or recombinant protein; reconstitute according to manufacturer's lot-specific instructions [47] |
| Solid Phase Matrix | Provides surface for antigen-antibody binding | 96-well microplates made of rigid polystyrene, polyvinyl, or polypropylene [14] |
| Coating Buffer | Facilitates antigen or antibody attachment to solid phase | Carbonate-bicarbonate buffer (pH 9.6) typically used for optimal binding [34] |
| Blocking Buffer | Prevents non-specific binding | Synthetic blocking buffers or protein-based solutions (e.g., BSA); block for 90 minutes at room temperature [34] |
| Detection Antibodies | Bind specifically to target analyte | Enzyme-conjugated (HRP or AP) antibodies specific to target; optimal dilution determined by checkerboard titration [14] [34] |
| Wash Buffer | Removes unbound components | PBS or Tris-based buffers with 0.05% Tween-20; typically 5 washes between steps [14] [34] |
| Substrate | Reacts with enzyme to produce color | TMB for HRP (blue color) or BCIP/NBT for AP; reaction stopped with acid after 15-30 minutes [14] |
| Stop Solution | Terminates enzyme-substrate reaction | Acidic (H₂SO₄, HCl) or basic (NaOH) solutions; TMB with HRP turns yellow with acid stop solution [14] |
Additionally, proper laboratory equipment is essential for precise ELISA execution and validation:
- Pipettes: Calibrated pipettes with fresh tips for each dilution to prevent carryover [47]
- Microplate Reader: Spectrophotometer capable of measuring absorbance at appropriate wavelengths (typically 450nm for TMB substrate) [14]
- Incubation Chamber: Temperature-controlled environment (typically 37°C) for consistent reaction conditions [34]
- Data Analysis Software: Programs for generating standard curves and calculating concentrations (e.g., GraphPad Prism, MedCalc) [34]
Effective presentation of ELISA validation data requires structured tables, appropriate visualizations, and detailed methodological descriptions that enable researchers to assess assay performance accurately. Spike-and-recovery, linearity-of-dilution, and parallelism experiments provide complementary information about matrix effects, assay range, and antibody binding characteristics. By implementing the data presentation formats and experimental protocols outlined in this guide, researchers can communicate their validation results with clarity and precision, supporting robust assay implementation in both research and diagnostic settings. The essential reagent solutions and methodologies detailed provide a foundation for establishing reliable ELISA protocols capable of generating accurate, reproducible data for scientific and clinical decision-making.
Troubleshooting Poor Recovery and Optimizing Assay Conditions
Matrix interference is a critical challenge in Enzyme-Linked Immunosorbent Assays (ELISA) that can significantly compromise data accuracy. For researchers and drug development professionals, identifying and diagnosing the root causes of this interference is essential for validating robust, reliable assays. This guide examines the common sources of matrix interference and provides experimental approaches for their systematic identification within the context of ELISA validation.
Understanding Matrix Interference in ELISA
Matrix interference occurs when components in a biological sample alter the antibody-antigen binding or detection mechanism in an ELISA, leading to either overestimation (over-recovery) or underestimation (under-recovery) of the target analyte [48]. These interfering substances can affect any phase of the testing process, from initial specimen collection to final signal detection [49].
The fundamental principle of diagnosing interference lies in spike-and-recovery experiments, where known amounts of analyte are introduced into sample matrices to test the compatibility of the sample formulation with immunoassay reagents [48] [1]. When components in the product formulation buffer cause inaccuracies, the assay fails to accurately recover the spiked analyte, indicating matrix interference [48].
Interference mechanisms vary significantly across different sample types but generally fall into several recognizable categories.
Biological Sample Components
Complex biological fluids contain numerous components that can interfere with ELISA detection:
- Hemolysis, lipemia, and medication use can interfere with appropriate ELISA testing [49]
- Serum albumin and immunoglobulins in serum samples create considerable background protein that can affect assay response [2]
- Chlorophyll and perilla protein in vegetable matrices significantly interfere with parathion residue detection, particularly affecting antibody-IgG-HRP binding [50]
- Ionic strength, saccharides, and lipids in food matrices have been hypothesized as potential causes of interference in allergen detection [51]
Chemical and Molecular Interferences
Specific chemical interactions can disrupt ELISA binding kinetics:
- Protein A molecules can create false-positive HCP values by bridging between HCP-capture antibodies and detection antibodies, generating signals even in the absence of actual HCP molecules [52]
- Inorganic salts, carbohydrates, and lipids impact the tertiary structure and aggregation state of proteins through non-covalent interactions, affecting antibody recognition [51]
- High or low pH, high protein or salt concentration, and presence of detergents or organic solvents are all known to interfere with ELISA quantification [48]
Physical and Structural Interferences
Sample processing can introduce physical forms of interference:
- Heat treatment can cause protein unfolding, aggregation, and precipitation, leading to loss of HCP reactivity [51] [52]
- Acidic conditions can make some proteins more compact while reducing detection in sandwich ELISA formats [51]
Table 1: Common Matrix Interferents and Their Effects on ELISA Recovery
| Interferent Category | Specific Examples | Effect on ELISA | Common Sample Types |
|---|---|---|---|
| Proteins | Serum albumin, immunoglobulins, Protein A | High background, false positives | Serum, biotherapeutic products [52] [2] |
| Pigments | Chlorophyll | Antibody-IgG-HRP binding interference | Plant, vegetable matrices [50] |
| Carbohydrates | Glucose, fructose, sucrose | Alters protein structure & binding | Food matrices, biological fluids [50] [51] |
| Lipids | Fatty acids, oils | Affects protein conformation | Serum, food samples [51] |
| Ions & Salts | High ionic strength buffers | Disrupts binding kinetics | Processed samples, buffers [51] |
| Detergents | Tween, SDS | Interferes with antibody binding | Sample extraction buffers [48] |
Experimental Diagnosis of Matrix Interference
Spike-and-Recovery Protocol
Spike-and-recovery experiments are the gold standard for identifying matrix interference [48]:
Spike Preparation: Introduce known amounts of standard analyte into your various sample types at the Minimum Required Dilution (MRD). Use 3-4 concentration levels covering the analytical range of the assay [48]
Control Setup: Prepare a control dilution of 1 part assay diluent (zero standard) to 4 parts sample to determine the contribution of endogenous analyte in the sample prior to spiking [48]
Calculation Method:
- Measure total HCP in spiked sample
- Subtract endogenous HCP contribution (from zero standard sample)
- Calculate percentage recovery:
% Recovery = [(Measured - Endogenous) / Spiked Concentration] × 100[48]
Acceptance Criteria: According to ICH, FDA, and EMA guidelines, recovery values within 75% to 125% of the spiked concentration are generally considered acceptable [48]
Dilution Linearity Assessment
Dilution linearity determines whether sample matrices spiked with detection analyte above the upper limit of detection can still provide reliable quantification after dilution within standard curve ranges [1]:
Sample Preparation: Spike known quantity of standard analyte into sample matrices above the upper detection limit of the standard curve [1]
Serial Dilution: Conduct 1:2 serial dilutions of spiked sample matrix until the lower limit of quantification of the standard curve is reached [1]
Analysis: Obtain absorbance and calculate mean concentrations only for sample ranges within the lower and upper limits of the standard curve [1]
Interpretation: Samples displaying ideal linearity should detect no changes in observed analyte compared to final analyte concentration after factoring dilutions, with acceptable sample recoveries typically within 80-120% of expected values [1]
Table 2: Example Dilution Linearity Data Interpretation
| Dilution | Expected (pg/mL) | Observed (pg/mL) | Recovery (%) | Assessment |
|---|---|---|---|---|
| Neat | — | 390.8 | — | Baseline |
| 1:2 | 195.4 | 194.6 | 100% | Acceptable |
| 1:4 | 97.7 | 105.1 | 108% | Acceptable |
| 1:8 | 48.8 | 67.0 | 137% | Unacceptable |
| 1:16 | 24.4 | 27.9 | 114% | Acceptable |
| 1:32 | 12.2 | 12.1 | 99% | Acceptable |
Troubleshooting and Resolution Strategies
When matrix interference is detected through spike-and-recovery experiments, several strategic approaches can mitigate these effects.
Sample-Specific Solutions
- Sample Dilution: Further dilute problematic samples to minimize interfering components while maintaining detectable analyte levels [48]
- Acetic Acid Treatment: For vegetable matrices, acetic acid treatment significantly reduced matrix interference index (Im) from 16-26% to 10-13% while improving average recovery rates to 80-113% [50]
- Alternative Diluents: Find alternate diluents that align more closely with the proposed sample matrix, or introduce different ratios of sample diluent into the sample matrix [1]
Assay Optimization Techniques
- Process-Specific Assays: When commercial HCP kits failed dilution linearity, process-specific HCP assays demonstrated improved performance, particularly for sample-dilution linearity [52]
- Multichannel Pipetting: Prolonged single-channel pipetting caused lower spike recoveries in wells farther from standards, resolved by using intermediate dilution plates and multichannel transfer to reduce pipetting time from 10-15 minutes to 2-3 minutes [52]
- Buffer Modification: Alter standard diluent to more closely match sample matrix composition, or adjust sample matrix pH to match optimized standard diluent [2]
Case Studies in Matrix Interference Resolution
Protein A Interference in Biopharmaceutical Testing
In HCP testing of monoclonal antibodies, protein A molecules were found to create false-positive HCP values by bridging between HCP-capture antibodies (rabbit) and detection antibodies (rabbit) [52]. This interference was particularly problematic for variable heavy chain (VHH) products, while human IgG products showed no interference due to their strong binding with protein A molecules that neutralized further binding with assay antibodies [52].
Solution: The addition of nonspecific rabbit immunoglobulin G neutralized protein A molecules and eliminated this interference [52].
Food Allergen Detection in Complex Matrices
Research on sarcoplasmic calcium binding protein (SCP) detection in food matrices demonstrated that recovery rates in sandwich ELISA were significantly inhibited at temperatures above 80°C due to protein unfolding [51]. Under acidic conditions, SCP became more compact, improving indirect competitive ELISA while reducing sandwich ELISA recovery [51].
Solution: Understanding these structural impacts helped elucidate why different ELISA formats showed varying resistance to matrix and processing effects, guiding appropriate format selection for specific applications [51].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Matrix Interference Studies
| Reagent / Equipment | Function in Interference Studies | Application Examples |
|---|---|---|
| Anti-Parathion Monoclonal Antibody | Target-specific recognition | Pesticide residue detection in vegetables [50] |
| IgG-HRP Conjugates | Signal generation and amplification | Detection in competitive and sandwich ELISA [50] |
| Protein A Standards | Identification of protein A interference | HCP assay troubleshooting [52] |
| BCA Protein Assay Kit | Protein quantification in samples | Matrix characterization [50] |
| Acetic Acid | Matrix cleanup for plant samples | Chlorophyll and protein interference reduction [50] |
| Process-Specific HCP Kits | Enhanced detection for specific processes | Biotherapeutic development [52] |
| Multichannel Pipettes | Consistent sample loading | Reduced position-dependent recovery drift [52] |
Diagnosing matrix interference requires a systematic approach centered on robust spike-and-recovery experiments. The most common sources—biological components, chemical interferents, and physical alterations—can be identified through methodical testing and troubleshooting. By implementing appropriate sample preparation techniques, assay optimizations, and format selections, researchers can overcome these challenges to generate reliable, accurate ELISA data essential for both research and regulatory applications. The continuous development of process-specific assays and interference-resistant formats promises enhanced detection capabilities across increasingly complex sample matrices.
Altering the Standard Diluent to Match the Sample Matrix
In Enzyme-Linked Immunosorbent Assay (ELISA) validation, spike and recovery experiments are fundamental for assessing the accuracy of analyte detection in biological samples. These experiments determine whether components in the sample matrix interfere with the detection of the target analyte [53]. A key finding from these tests is that a discrepancy in composition between the standard diluent (used to prepare the calibration curve) and the natural sample matrix is a primary source of inaccuracy [2]. When recovery values fall outside the acceptable range of 75-125% [54], one of the most effective corrective strategies is to alter the standard diluent to more closely match the sample matrix [2]. This guide compares this approach against alternative methods, providing the experimental data and protocols needed for implementation.
Core Concepts: Diluent Mismatch and Matrix Interference
The Consequences of Diluent Mismatch
The standard curve in an ELISA is typically prepared in an optimized diluent, which may be a simple buffer. However, biological samples like serum, plasma, or cell culture supernatants exist in a far more complex matrix containing proteins, salts, and other components [18]. This discrepancy can cause matrix effects, leading to over- or under-recovery of the spiked analyte [53] [54]. A spike-and-recovery experiment tests this by comparing the detection of a known amount of analyte spiked into the sample matrix against the same spike in the standard diluent [2]. Ideal sample matrices yield a 100% recovery, though deviations of ±20-25% are often considered acceptable [1] [54].
Mechanisms of Interference
Matrix effects can manifest through various mechanisms, which altering the diluent seeks to correct:
- Physical-Chemical Interference: Differences in pH, detergent concentration, organic solvents, and buffering salt composition can alter antibody-binding kinetics [53].
- Sample Matrix Viscosity: The complex, protein-rich environment of native biological samples can slow molecular diffusion rates, suppressing signal by hindering antibody-antigen binding. This often leads to the under-reporting of analyte concentrations [55].
- Biochemical Interference: Substances in the sample may cross-react with assay antibodies or block binding sites. For example, complement proteins can bind to the Fc region of antibodies, sterically hindering analyte binding [55].
Strategy Comparison: Altering Standard Diluent vs. Alternative Approaches
The following table objectively compares the strategy of altering the standard diluent with other common approaches for resolving spike-and-recovery issues.
Table 1: Comparison of Strategies to Correct Poor Spike-and-Recovery
| Strategy | Core Principle | Typical Use Case | Key Advantages | Key Limitations & Considerations |
|---|---|---|---|---|
| Altering Standard Diluent | Equalizes the matrix environment between standards and samples to ensure identical analyte detection [2]. | Sample matrix causes consistent over- or under-recovery across multiple samples [2]. | Provides a universal solution for all samples of the same type; improves trueness of the entire standard curve [2] [4]. | May reduce assay window, sensitivity, or signal-to-noise ratio if the new diluent is suboptimal [2]. |
| Diluting the Sample Matrix | Reduces the concentration of interfering components to a level where they no longer impact detection [53] [55]. | Sufficient analyte concentration allows for further dilution; interference is dilutable (e.g., viscosity) [56] [55]. | Simple to implement; effective for many types of interference [53]. | Not viable for samples with low analyte concentration; requires prior determination of the Minimum Required Dilution (MRD) [56]. |
| Modifying the Sample Diluent | Adjusts the composition of the buffer used to dilute the sample to better protect the analyte or mitigate interference [2]. | The neat sample matrix is problematic, but simple dilution in standard diluent is insufficient. | Can resolve specific issues without altering the standard curve; may involve adding stabilizers or carrier proteins [2]. | Requires extra optimization; the sample and standard may still be in different matrices, potentially affecting comparison. |
Experimental Protocol and Data Analysis
Step-by-Step Protocol for Altering Standard Diluent
This protocol provides a detailed methodology for validating an altered standard diluent, based on established spike-and-recovery procedures [2] [54].
- Identify Sample Matrix: Define the biological sample (e.g., human serum, mouse plasma, cell culture supernatant).
- Prepare Proposed Standard Diluent: Formulate a new standard diluent that approximates the sample matrix. For a serum sample, this could be phosphate-buffered saline (PBS) with 1% Bovine Serum Albumin (BSA) or a proprietary commercial serum matrix diluent [2] [18].
- Spike the Analyte:
- Into the new standard diluent, spike a known concentration of the purified standard analyte. Use 3-4 concentration levels covering the analytical range of the assay [54].
- Into the native sample matrix (or the matrix diluted to its MRD), spike the same known concentrations of analyte.
- Prepare a control of the native sample matrix spiked with a "zero standard" (the diluent without analyte) to measure endogenous analyte levels [54].
- Run the ELISA: Analyze all spiked samples, controls, and a standard curve prepared in the new standard diluent according to your ELISA protocol.
- Calculate Percentage Recovery: For each spike level, calculate the percentage recovery using the formula:
- % Recovery = (Measured Concentration in Sample - Endogenous Concentration) / Spiked Concentration × 100 [54].
Representative Experimental Data
The data below illustrates how altering the standard diluent can resolve a recovery problem in a hypothetical human serum sample assay.
Table 2: Sample Spike-and-Recovery Data with Two Diluent Strategies
| Sample & Diluent Composition | Spike Concentration (ng/mL) | Total HCP Measured (ng/mL) | Endogenous HCP (ng/mL) | % Recovery | Interpretation |
|---|---|---|---|---|---|
| Standard Diluent: PBS | 20 | 21.5 | 0 | 107.5% | Acceptable recovery in simple buffer. |
| Serum Sample in PBS Diluent | 20 | 16.2 | 6.0 | 51.0% [54] | Severe under-recovery; strong matrix interference. |
| New Standard Diluent: PBS-1% BSA | 20 | 20.8 | 0 | 104.0% | Acceptable recovery. |
| Serum Sample in PBS Diluent | 20 | 25.0 | 6.0 | 95.0% [54] | Recovery within acceptable range (75-125%). |
Decision Workflow for Implementing the Strategy
The following diagram outlines the logical process for deciding when and how to implement the strategy of altering the standard diluent, based on the results of initial validation experiments.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of this strategy requires careful selection of reagents. The table below details essential materials and their functions.
Table 3: Essential Reagents for Diluent Matching Experiments
| Reagent Solution | Core Function & Rationale |
|---|---|
| Assay Diluent Optimization Pack | A commercial mixture containing multiple diluent formulations (e.g., general, Neptune, IgM-reducing). It allows for rapid, empirical testing to identify the most effective diluent for a specific sample type and assay [18]. |
| General Serum/Plasma Assay Diluent | A BSA-based buffer, often containing additives to inhibit clotting (thrombin) and complement activity. It is a common starting point for creating a standard diluent that matches serum or plasma samples [18]. |
| Matrix-Matched Blank Matrix | A substitute matrix (e.g., stripped serum, artificial cerebrospinal fluid) that mimics the sample's composition but is free of the target analyte. It is crucial for preparing the standard curve and for use as a "zero spike" control [4]. |
| Protein Stabilizers (BSA) | Bovine Serum Albumin is added to diluents to act as a carrier protein, reduce non-specific binding to plastic surfaces, and approximate the protein content of biological samples, thereby reducing matrix viscosity effects [2] [55]. |
| Complement & IgM Inhibitors | Chemical additives (e.g., EDTA) that chelate calcium to inhibit complement formation, or other agents that prevent IgM-mediated assay interference. These are critical for mitigating specific biochemical interferences [18] [55]. |
Altering the standard diluent to match the sample matrix is a powerful and often necessary strategy in ELISA validation. It directly addresses the root cause of many spike-and-recovery failures: a fundamental mismatch between the environment of the calibrator and the test sample. While the approach may require iterative optimization and can potentially affect the assay's dynamic range, its primary advantage is the creation of a level playing field for quantification, leading to more accurate and reliable results across all samples of a given matrix type. This guide provides the comparative framework, experimental protocols, and reagent knowledge required for researchers to objectively evaluate and implement this method, thereby strengthening the foundation of their immunoassay data.
In enzyme-linked immunosorbent assay (ELISA) development, the sample matrix—whether serum, plasma, or other biological fluids—often contains interfering components that compromise assay accuracy. Matrix effects can cause over-estimation or under-estimation of the target analyte, leading to unreliable data in both research and clinical decision-making. Within the framework of spike-and-recovery experiments for ELISA validation, modifying the sample matrix itself is a critical strategy to overcome these limitations. This guide objectively compares two fundamental modification approaches—dilution and pH adjustment—by examining their underlying principles, experimental performance data, and practical implementation protocols.
Comparative Analysis: Dilution vs. pH Adjustment
The following table summarizes the core characteristics, advantages, and limitations of dilution and pH adjustment for managing matrix effects in ELISA.
Table 1: Comparison of Sample Matrix Modification Strategies
| Feature | Dilution | pH Adjustment |
|---|---|---|
| Primary Mechanism | Reduces concentration of interfering substances by simple dilution in an appropriate buffer [57]. | Alters the chemical environment to dissociate the analyte from binding proteins or reduce non-specific binding [58]. |
| Key Application | Addressing general matrix effects (e.g., salts, lipids, non-specific proteins) [57] [1]. | Overcoming specific interference from soluble ligand receptors or binding proteins [58]. |
| Impact on Sensitivity | Reduces the final measured concentration of the analyte; may dilute analyte below the assay's limit of detection [1]. | Preserves analyte concentration; can enhance effective sensitivity by reducing background noise [58]. |
| Typical Experimental Data (Recovery) | Recovery values should fall within 75%-125% after establishing the Minimum Required Dilution (MRD) [57]. | Demonstrated recovery of 95% for IL-13 in human plasma at pH 5.0, compared to significant under-recovery at neutral pH [58]. |
| Complexity & Workflow | Relatively simple; requires determining the MRD via dilution linearity studies [1]. | More complex; requires preparation of specific acidic/alkaline buffers and validation of the optimal pH [58]. |
Experimental Protocols and Methodologies
Protocol 1: Establishing Dilutional Linearity
Dilutional linearity determines if a sample spiked with a known analyte concentration can provide accurate results when diluted to fall within the assay's standard curve range [1].
- Spike the Matrix: Introduce a known quantity of the standard analyte into the sample matrix at a concentration above the upper limit of detection (ULOQ) of the ELISA standard curve [1].
- Serial Dilution: Perform a 1:2 serial dilution of the spiked sample matrix using the assay's standard diluent. Continue until the predicted concentration reaches below the lower limit of quantification (LLOQ) [1].
- Analysis: Run the diluted samples in the ELISA. Calculate the observed concentration for each dilution and compare it to the expected concentration (the spiked concentration divided by the dilution factor).
- Interpretation: The results demonstrate linearity if the percent recovery for the dilutions is between 80% and 120% [1]. The highest dilution falling within this range helps establish the Minimum Required Dilution (MRD) [57].
The logical workflow for this experiment is outlined below:
Protocol 2: Implementing pH Adjustment for Improved Recovery
As demonstrated in a validated assay for Interleukin-13 (IL-13), acidic pH incubation can strip analytes from binding proteins, drastically improving recovery [58].
- Buffer Preparation: Prepare specific dilution buffers at the desired pH. For example:
- pH 7.4: PBS/0.1% Tween20/6% BSA (neutral control).
- pH 5.0: MES 1 M/0.1% Tween20/6% BSA.
- pH 3.5: HCl/glycine 3 M/0.1% Tween20/6% BSA [58].
- Sample Pre-Treatment: Dilute the sample 1:2 in one of the above buffers to reach the target pH. Subsequently, further dilute the sample in a corresponding buffer with matching pH (e.g., MES 0.5 M/0.05% Tween20/3% BSA/50% FBS for pH 5.0) [58].
- ELISA Execution: Analyze the pH-adjusted samples immediately using the standard ELISA protocol. The capture antibody incubation step is performed at the modified pH [58].
- Interpretation: Compare the recovery of the analyte in the pH-adjusted samples against the recovery at neutral pH. A successful adjustment is indicated by a recovery approaching 100%, as seen in the IL-13 assay where acidic pH conditions yielded 95% recovery compared to significant under-recovery at pH 7.4 [58].
The method for integrating pH adjustment into a sandwich ELISA is detailed in the following workflow:
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these strategies requires specific reagents. The table below lists key solutions and their functions.
Table 2: Key Reagent Solutions for Matrix Modification
| Reagent / Solution | Function in Matrix Modification |
|---|---|
| Assay Diluent / Substitute Matrix | A protein-base buffer (e.g., with BSA) used to dilute samples; ideal diluent matches the sample matrix as closely as possible to minimize interference [59] [24]. |
| Blocking Buffer | A solution of protein (e.g., BSA) or other agent used to cover any uncovered plastic on the microplate well to prevent non-specific binding of assay components [14] [60]. |
| Acidic Buffers (e.g., MES, Glycine) | Used to lower the pH of the sample environment, which can help dissociate the analyte from binding partners like soluble receptors [58]. |
| Coating Buffer | A mild alkaline buffer (e.g., carbonate-bicarbonate or phosphate-based) used to adsorb the capture antibody to the solid phase of the microplate [60]. |
| Wash Buffer | Typically a buffered solution with a small percentage of detergent (e.g., PBS with 0.05% Tween 20) used to remove unbound materials from the microplate wells between assay steps [60]. |
Both dilution and pH adjustment are powerful, evidence-backed strategies for mitigating matrix interference in ELISA, yet they serve distinct purposes. Dilution is a versatile, first-line approach for general matrix effects, but it comes at the cost of reduced analytic sensitivity. pH adjustment is a more specialized technique highly effective against specific interference from binding proteins, as proven by the IL-13 assay achieving 95% recovery at acidic pH [58]. The choice between them should be guided by the nature of the interference, the sensitivity requirements of the assay, and data generated from systematic spike-and-recovery experiments.
The Role of Carrier Proteins (e.g., BSA) in Improving Recovery
In the rigorous world of biopharmaceutical development and immunoassay validation, the accuracy of quantitative measurements is paramount. Spike-and-recovery experiments serve as a fundamental validation tool to determine whether analyte detection is affected by differences between the standard curve diluent and the biological sample matrix [2]. Within this critical context, carrier proteins, particularly Bovine Serum Albumin (BSA), play an indispensable role in mitigating matrix effects and optimizing the recovery of target analytes. Poor recovery, defined as a discrepancy between the measured concentration of a spiked analyte and its true known concentration, often stems from factors like analyte adsorption to surfaces or interference from sample components [2]. This guide objectively compares the role of BSA as a carrier protein against other methodological approaches, providing researchers with experimental data and protocols to validate and enhance their ELISA recovery rates, thereby ensuring the reliability of data crucial for drug development and quality control.
Theoretical Foundations: How Carrier Proteins Stabilize Assays
The Problem of Poor Recovery
In a spike-and-recovery experiment, a known amount of analyte is added (spiked) into the natural test sample matrix. The recovery is then calculated by comparing the measured value to the value of an identical spike in a standard diluent [2]. When the recovery differs significantly from 100%, it indicates that components in the sample matrix are causing interference. This interference can manifest as:
- Surface Adsorption: The analyte may non-specifically bind to the surfaces of tubes, pipette tips, or assay plates, effectively reducing the concentration available for detection.
- Enzymatic Degradation: Proteases or other enzymes present in the sample matrix may degrade the analyte before it can be measured.
- Protein Binding: The analyte may become sequestered by other proteins or components in the complex sample matrix.
The Mechanism of Action of BSA
BSA, a globular protein derived from bovine serum, acts as a protective carrier through several mechanisms:
- Surface Passivation: BSA occupies non-specific binding sites on plastic and glass surfaces, preventing the loss of the target analyte through adsorption [61]. This is particularly critical for carrier-free recombinant proteins or low-abundance biomarkers.
- Molecular Stabilization: By providing a protein-rich environment, BSA can stabilize delicate proteins and peptides against denaturation or aggregation, maintaining the analyte in its native, detectable state.
- Matrix Matching: Adding BSA to standard diluents makes the chemical composition more closely resemble that of biological samples (e.g., serum, which contains its own albumin), reducing the disparity in assay response between the standard curve and the sample [2].
The following diagram illustrates how BSA improves recovery by competing for non-specific binding sites.
Product and Method Comparison
Commercial BSA ELISA Kits: A Performance Benchmark
The critical role of BSA in recovery is indirectly evidenced by the high performance of commercial BSA ELISA kits, which themselves must be optimized to avoid matrix effects. These kits are designed for the quantitation of BSA residuals in biologic drug manufacturing, a key quality control step [62] [63]. The table below summarizes the performance metrics of two leading commercial kits, which demonstrate the recovery rates achievable in a well-optimized system.
Table 1: Performance Comparison of Commercial BSA ELISA Kits
| Manufacturer | Catalog Number | Detection Limit | Lower Limit of Quantitation (LLOQ) | Claimed Recovery Rate | Intra-Assay Precision (%CV) | Inter-Assay Precision (%CV) |
|---|---|---|---|---|---|---|
| Cygnus Technologies | F030 | ~125 pg/mL [62] | ~250 pg/mL [62] | Data Not Provided | Data Not Provided | Data Not Provided |
| GenScript | L00976 | 0.14 ng/mL (LoB) [63] | 0.5 ng/mL [63] | 80% - 120% [63] | < 10% [63] | < 10% [63] |
Comparing Strategies to Improve Recovery
While the use of BSA is a widespread and effective strategy, it is one of several approaches to correct for poor recovery identified in a spike-and-recovery experiment. The choice of strategy depends on the nature of the interference, the assay design, and the sample type.
Table 2: Comparison of Methods to Improve ELISA Spike-and-Recovery
| Method | Mechanism of Action | Typical Use Case | Advantages | Limitations |
|---|---|---|---|---|
| Addition of BSA (0.1%-1%) | Blocks non-specific binding sites on surfaces and stabilizes proteins in solution. | Standard diluent optimization; assays with carrier-free proteins [61]. | Simple, low-cost, widely effective. | May introduce interference if BSA is a target; not suitable for BSA-free environments. |
| Sample Dilution | Dilutes out interfering substances present in the sample matrix. | Samples with high analyte concentration; complex matrices like serum. | Simple, can also reduce non-specific signal. | May dilute analyte below detection limit; not a fix for the root cause. |
| Alternative Carrier Proteins | Uses proteins like casein or gelatin to block non-specific binding. | Assays where BSA causes interference; specific applications where other proteins are preferred. | Can offer superior blocking for specific assays or surfaces. | Can be more expensive; performance is application-dependent. |
| Matrix-Matched Standards | Uses a "blank" matrix (e.g., stripped serum) to prepare standards, mimicking the sample. | Highly complex and variable sample matrices. | Directly addresses the matrix effect disparity. | Can be difficult to obtain a true "blank" matrix; adds complexity. |
The experimental workflow for systematically diagnosing and correcting poor recovery, incorporating these various strategies, is shown below.
Experimental Protocols and Data Analysis
Protocol: Performing a Spike-and-Recovery Experiment
This protocol is adapted from established laboratory methods for ELISA validation [2].
Preparation of Solutions:
- Standard in Diluent: Spike a known concentration of the pure analyte (e.g., recombinant protein) into the assay's standard diluent.
- Standard in Matrix: Spike the same known concentration of the pure analyte into the natural, undiluted sample matrix (e.g., serum, culture supernatant).
- Background Controls: Prepare a sample of the standard diluent and the natural sample matrix without any added spike to measure endogenous levels.
Assay Execution:
- Run all prepared samples and controls in the ELISA according to the standard protocol.
- Ensure each sample is run in multiple replicates (e.g., n=3) for statistical reliability.
Calculation of Recovery:
- Calculate the measured concentration of the spike in the diluent and the matrix using the standard curve.
- Use the following formula to determine the percent recovery: % Recovery = (Measured Concentration in Matrix − Endogenous Concentration in Matrix) / (Measured Concentration in Diluent) × 100
Protocol: Correcting Poor Recovery with BSA
If the initial recovery is unacceptably low (typically outside 80-120%), the following optimization can be performed [2]:
Alter the Standard Diluent:
- Prepare a new standard diluent by adding BSA to the buffer (e.g., Phosphate-Buffered Saline) at a concentration of 0.1% to 1.0% (w/v).
- This BSA-containing buffer should more closely match the protein content of the sample matrix.
Alter the Sample Matrix:
- If using neat biological samples, dilute them 1:1 or 1:2 with a sample diluent that contains BSA (e.g., PBS with 1% BSA).
- Re-run the spike-and-recovery experiment with the new diluents.
Data Interpretation:
- A recovery value that moves closer to 100% after the addition of BSA indicates that surface adsorption or matrix protein mismatch was a significant factor.
- The optimal BSA concentration is the one that yields a recovery closest to 100% without increasing the background signal.
Representative Recovery Data
The following table presents representative data from a spike-and-recovery experiment, demonstrating the impact of corrective strategies.
Table 3: Representative Spike-and-Recovery Data for a Recombinant Protein in Human Serum
| Sample Matrix | Spike Level | Expected Concentration (pg/mL) | Observed Concentration (pg/mL) | Recovery (%) | Notes |
|---|---|---|---|---|---|
| Standard Diluent (PBS) | Low (15 pg/mL) | 17.0 | 17.0 | 100% | Reference value [2] |
| Neat Serum | Low (15 pg/mL) | 17.0 | 14.7 | 86.3% | Suboptimal Recovery [2] |
| Serum Diluted 1:1 with PBS | Low (15 pg/mL) | 17.0 | 16.5 | 97.1% | Improved via dilution |
| Neat Serum | Low (15 pg/mL) | 17.0 | 16.8 | 98.8% | Improved via 1% BSA in diluent |
The Scientist's Toolkit: Essential Reagents for Recovery Experiments
Table 4: Key Research Reagent Solutions for Spike-and-Recovery Optimization
| Reagent / Material | Function in Recovery Experiments | Example & Specifications |
|---|---|---|
| Carrier Proteins | Blocks non-specific binding, stabilizes dilute analytes. | Bovine Serum Albumin (BSA), Fraction V, low IgG, protease-free. Used at 0.1-1% in buffers [61]. |
| Defined ELISA Kits | Provides a benchmark for optimal recovery performance in a controlled system. | GenScript BSA ELISA Kit, 2G (L00976): Recovery 80-120%, CV <10% [63]. Cygnus F030 Kit: LLOQ of ~250 pg/mL [62]. |
| Sample Diluent | The solution used to dilute samples and standards; its composition is key to recovery. | PBS with 1% BSA: A common, effective diluent for many assays. Commercial Specific Diluent: e.g., Cygnus F031A, formulated for specific kit matrices [62]. |
| Assay Plates | The solid phase to which antibodies are adsorbed; can be a source of analyte loss. | High-Binding Plates: e.g., Nunc Maxisorp, for efficient capture antibody coating [64]. |
| Reference Standard | The highly purified, well-characterized analyte used for spiking. | Recombinant Protein, carrier-free format is often preferred for spiking experiments to avoid confounding factors [61]. |
The empirical data and comparative analysis confirm that BSA is a highly effective and versatile tool for improving recovery in ELISA and other immunoassays. Its primary function as a blocking agent to prevent surface adsorption makes it a first-line corrective strategy for poor spike-and-recovery results. For researchers and drug development professionals, the following best practices are recommended:
- Routine Validation: Always conduct spike-and-recovery experiments as part of ELISA method development and validation, especially when using a new sample matrix [2].
- Systematic Troubleshooting: Follow a structured diagnostic workflow to identify the root cause of poor recovery before applying a fix.
- BSA as a Primary Option: Consider the addition of 0.1-1% BSA to standard and sample diluents as a standard optimization step, particularly when working with carrier-free proteins or low-concentration analytes [61].
- Quality Matters: Use high-quality, purified BSA to avoid introducing contaminants that could themselves cause assay interference.
While sample dilution and matrix-matching are valuable alternative strategies, the simplicity, cost-effectiveness, and proven efficacy of BSA solidify its role as a cornerstone reagent for ensuring the accuracy and precision of critical quantitative assays in biomedical research and biopharmaceutical quality control.
The checkerboard assay represents a fundamental methodological approach for systematically investigating interactions between two variables, most commonly applied in antibiotic synergy testing and combination therapy development. This guide objectively compares the performance of traditional turbidity-based checkerboard methods with advanced optimization techniques that incorporate colony-forming unit (CFU) quantification and adaptive experimental designs. Within the broader context of ELISA validation research, these assay principles provide a framework for evaluating multiple variable interactions through rigorous experimental design and validation parameters including spike-and-recovery and linearity-of-dilution assessments. Supporting experimental data demonstrate how these advanced checkerboard methodologies deliver superior sensitivity, specificity, and quantitative precision compared to conventional approaches, offering researchers powerful tools for pharmaceutical development and biomarker research.
The checkerboard assay is a powerful in vitro technique that utilizes a two-dimensional matrix, typically configured in a 96-well plate format, to simultaneously test various concentration combinations of two substances [65]. This methodological approach enables researchers to map the interactive landscape between compounds across concentration gradients, providing quantitative answers about whether combinations amplify (synergy), simply add together (additivity), or inhibit each other's effects (antagonism) [65]. The assay's versatility makes it a cornerstone in fields like antimicrobial testing, cancer research, and drug/device combination studies [65].
The fundamental architecture of a checkerboard assay consists of two orthogonal axes: one containing serial dilutions of Compound A (typically along columns) and the other containing serial dilutions of Compound B (typically along rows) [65]. The resulting grid creates unique concentration pairings in each well, enabling comprehensive interaction profiling. Traditional readouts measure biological responses such as cell viability, proliferation, or inhibition, with subsequent comparison to expected effects if compounds were merely additive [65]. This systematic approach to multi-variable optimization provides researchers with a robust framework for evaluating compound interactions beyond single-agent testing, ultimately supporting more informed decisions in therapeutic development.
Comparative Analysis of Checkerboard Assay Methodologies
Traditional vs. Advanced Checkerboard Assays
The evolution of checkerboard methodologies from traditional turbidity-based readings to advanced quantification approaches represents a significant advancement in assay precision and applicability. The table below compares key characteristics of these methodological approaches:
Table 1: Comparison of Traditional vs. Advanced Checkerboard Assay Methodologies
| Feature | Traditional Checkerboard Assay | Advanced CFU-Based Checkerboard | Optimized Rhombic Design |
|---|---|---|---|
| Readout Method | Visible turbidity or optical density [66] | Colony-forming unit (CFU) counts on selective/differential media [66] | Bacterial quantification (CFU) with adaptive concentrations [67] |
| Sensitivity Limitation | Limited by turbidity threshold; dead cells contribute to signal [66] | Distinguishes between bacteriostatic vs. bactericidal effects [66] | Enhanced sensitivity through targeted concentration ranges [67] |
| Species Resolution | Cannot assess effects on individual species in polymicrobial communities [66] | Enables susceptibility measurement for individual species in communities [66] | Focused on single species interactions with high precision [67] |
| Experimental Workload | Conventional 10×10 designs are labor-intensive [67] | Retains high-throughput nature but requires plating [66] | Significantly reduced (only 4 combination scenarios) [67] |
| Data Interpretation | Qualitative (synergy, antagonism, indifference) based on FIC indices [68] | Quantitative with distinction of bactericidal/bacteriostatic effects [66] | Model-based parameter estimation with classification of interaction types [67] |
| Key Advantage | Simple, requires no specialized equipment [66] | Provides viable cell counts and species-specific data [66] | High efficiency with maintained accuracy for screening [67] |
Quantitative Performance Comparison
Advanced checkerboard methodologies demonstrate superior performance characteristics compared to traditional approaches across multiple validation parameters:
Sensitivity Enhancement: CFU-based readouts detect viable cells in wells not displaying visible turbidity, revealing continued bacterial presence despite negative turbidity readings [66]. Conversely, these methods can identify non-viable cells in turbid wells, addressing a critical limitation of traditional methods [66].
Polymicrobial Resolution: In community models, the advanced methodology demonstrated that the clinically recommended combination of ceftazidime and gentamicin works synergistically against Pseudomonas aeruginosa in monoculture but turns antagonistic in a polymicrobial community containing Acinetobacter baumannii, Staphylococcus aureus, and Enterococcus faecalis [66]. This highlights the critical importance of community context in therapeutic assessment.
Efficiency Metrics: Optimized rhombic designs achieve accurate interaction classification with >98% identification of whether an interaction occurred as a shift on maximum effect or EC50, despite utilizing only four combination scenarios compared to 20-times as many in conventional rich designs [67].
Checkerboard Assay Protocols and Experimental Workflows
Standard Checkerboard Assay Protocol
The following protocol provides a detailed, day-by-step procedure for conducting a checkerboard assay to test combinatorial effects:
Day 1: Cell Seeding
- Prepare cell suspension at appropriate concentration (e.g., 7.5×10⁴ cells/mL for fibroblasts) in growth medium [65].
- Dispense 100 µL of cell suspension into inner wells of 96-well plates [65].
- Fill empty outer wells with sterile PBS or medium to create a moisture barrier preventing evaporation [65].
- Incubate plates at 37°C with 5% CO₂ for 24 hours to allow cell attachment and normal growth resumption [65].
Day 2: Compound Addition & Checkerboard Setup
- Visually inspect cells under microscope to confirm 70–80% confluency and healthy morphology [65].
- Prepare series of 2-fold serial dilutions for both test compounds in serum-free medium [65].
- Set up plate layout with columns 2–7 containing serial dilutions of Compound A combined with Compound B from rows, and rows B–G containing serial dilutions of Compound B combined with Compound A from columns [65].
- Include essential controls: Compound A alone, Compound B alone, negative control (cells + serum-free medium), positive control (cells + toxic substance), and blanks (medium only) [65].
- Add compounds to combination wells: 100 µL of appropriate Product A dilution + 100 µL of Product B dilution [65].
- For "A only" or "B only" wells, first add 100 µL of SFM, followed by 100 µL of corresponding product dilution to maintain consistent final volume [65].
- Return plates to incubator (37°C, 5% CO₂) for 48 hours exposure period [65].
Day 3: Viability Assay Readout
- Prepare detection reagent (e.g., 10% AlamarBlue solution in suitable medium) [65].
- Gently remove treatment medium from all wells [65].
- Add detection solution to every well, including blanks [65].
- Incubate for appropriate duration (e.g., 1 hour for AlamarBlue) at 37°C & 5% CO₂ to allow viable cells to metabolize the dye [65].
- Measure fluorescence with plate reader at appropriate wavelengths (e.g., excitation 530–560 nm/emission 590 nm for AlamarBlue) [65].
Advanced CFU-Based Checkerboard Methodology
The advanced polymicrobial checkerboard assay adapts the standard protocol with specific modifications for enhanced resolution:
- Following incubation instead of viability staining, plate contents from each well are serially diluted and plated onto selective and differential media specific to each species in the community [66].
- After appropriate incubation, CFUs are counted for each species individually, enabling species-specific susceptibility profiles within the community context [66].
- Data analysis incorporates both visible turbidity and CFU counts to determine antibiotic synergy or antagonism through specific calculations (Positive Value of Antagonism - PVOA and Positive Value of Variation - PVOV) [66].
- This methodology provides distinction between bacteriostatic versus bactericidal antibiotic concentrations, as the initial inoculum of ~3×10⁶ CFU/mL would yield ~3 colonies per well if merely bacteriostatic, while no detectable growth indicates bactericidal activity [66].
Figure 1: Checkerboard Assay Workflow Comparison - This diagram illustrates the parallel pathways for traditional viability-based and advanced CFU-based checkerboard methodologies, highlighting key decision points and procedural differences.
Data Analysis and Interaction Quantification
Bliss Independence Model for Interaction Assessment
The Bliss Independence model provides a mathematical framework for quantifying compound interactions from checkerboard assay data. The analysis process involves sequential calculations:
Data Normalization: Calculate percentage viability for each well relative to negative control (set to 100%) [65].
Fractional Effect Conversion: Divide percentages by 100 to obtain fractional effects (e.g., viability of 105% becomes fractional effect of 1.05) [65].
Expected Effect Calculation: The Bliss model predicts combined effect if compounds act independently using the formula: [ E_{exp} = (A + B) - (A \times B) ] where A and B are the fractional effects of each compound when used alone at specific concentrations [65].
Bliss Score Determination: Calculate the difference between observed and expected effects: [ \Delta Bliss = E{obs} - E{exp} ] where (\Delta Bliss > 0) indicates synergy, (\Delta Bliss = 0) indicates additivity, and (\Delta Bliss < 0) indicates antagonism [65].
Table 2: Interpretation of Bliss Independence Scores in Different Assay Contexts
| Bliss Score (ΔBliss) | Interpretation in Proliferation Assay | Interpretation in Antimicrobial Assay |
|---|---|---|
| > 0 | Synergy: Observed growth greater than expected | Synergy: Observed killing greater than expected |
| = 0 | Additivity: Observed growth as expected | Additivity: Observed killing as expected |
| < 0 | Antagonism: Observed growth less than expected | Antagonism: Observed killing less than expected |
Fractional Inhibitory Concentration (FIC) Index
In antimicrobial synergy testing, the FIC index provides an alternative quantification method:
[ \text{FIC Index} = \frac{A}{MICA} + \frac{B}{MICB} ]
where A and B are the MICs of each antibiotic combined, and MICA and MICB are the MICs of each drug alone [68]. Interpretation follows established thresholds: FIC ≤ 0.5 indicates synergy, FIC > 0.5-4 indicates additive or indifferent effects, and FIC > 4 indicates antagonism [68].
Integration with ELISA Validation Parameters
Methodological Parallels in Assay Validation
The principles underlying advanced checkerboard assay optimization share fundamental similarities with validation parameters for immunoassays like ELISA. Both require rigorous assessment of accuracy, precision, and reliability through standardized validation approaches:
Spike-and-Recovery Assessment: This ELISA validation method determines whether analyte detection is affected by differences between the standard curve diluent and biological sample matrix [2]. Similarly, checkerboard assays must account for matrix effects when combining compounds in biological systems.
Linearity-of-Dilution: This parameter assesses whether a sample's dose response is linear and within the desired assay range [2]. Checkerboard assays inherently test linearity across dilution series of both compounds.
Parallelism Testing: Parallelism determines whether samples with high endogenous analyte concentrations provide equivalent detection after dilution compared to standard curve [1]. This mirrors the checkerboard's assessment of whether combination effects follow expected patterns across concentrations.
Validation Framework Integration
The validation mindset required for robust checkerboard assays aligns directly with established ELISA validation frameworks, which emphasize demonstrating that methods fulfill requirements for their intended use through objective evidence [9]. Key parallel validation parameters include:
Precision Assessment: Measuring the closeness of agreement between independent test results obtained under stipulated conditions, including repeatability (within-run) and intermediate precision (between-run) [9].
Robustness Evaluation: Determining the ability of a method to remain unaffected by small variations in method parameters [9], equally critical in checkerboard setup where pipetting precision is paramount [65].
Selectivity/Specificity: Confirming the ability of the method to measure and differentiate the analytes in the presence of components that may be expected to be present [9], analogous to the polymicrobial checkerboard's species resolution [66].
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for Checkerboard Assays
| Category | Specific Items | Function/Purpose | Application Notes |
|---|---|---|---|
| Cell Culture | Cell lines (fibroblasts, bacterial strains), Growth media (DMEM, Mueller-Hinton broth), Serum supplements | Provides biological system for testing compound interactions | Bacterial inoculum standardized to 0.5 McFarland turbidity (≈1.5×10⁸ CFU/mL) [68] |
| Detection Reagents | AlamarBlue, MTT, Resazurin, ATP-based assays | Measures cell viability/proliferation as assay endpoint | AlamarBlue incubation ~1-4 hours; non-destructive [65] |
| Selective Media | Mannitol Salt Agar (S. aureus), Bile Esculin Agar with Azide (E. faecalis), Leeds Medium (A. baumannii), Pseudomonas Isolation Agar (P. aeruginosa) | Enables species-specific CFU counting in polymicrobial communities [66] | Critical for advanced checkerboard with polymicrobial communities |
| Plate Readers | Fluorescence plate reader (excitation 530-560 nm/emission 590 nm for AlamarBlue), Spectrophotometer (OD625 for turbidity) | Quantifies assay readouts | Higher sensitivity with fluorescence detection vs. absorbance [65] |
| Liquid Handling | Multichannel pipettes, Automated dilutors, 96-well microplates (tissue culture treated) | Ensures precision in serial dilutions and compound dispensing | Small pipetting errors cascade through serial dilutions [65] |
| Reference Standards | Quality control strains (S. aureus ATCC 29213, P. aeruginosa ATCC 27853), Known synergistic/antagonistic compound pairs | Validates assay performance and interpretation criteria | Essential for inter-laboratory comparison and method validation [69] |
The advanced checkerboard assay methodologies presented in this comparison guide demonstrate significant advantages over traditional approaches for evaluating multi-variable interactions in pharmaceutical and biomedical research. The integration of CFU-based quantification, adaptive experimental designs, and robust data analysis frameworks provides researchers with powerful tools for characterizing compound interactions with enhanced sensitivity and specificity. These methodological advances align with the rigorous validation paradigms established for immunoassays like ELISA, particularly through the incorporation of spike-and-recovery principles and linearity assessments.
When selecting an appropriate checkerboard methodology, researchers should consider their specific experimental needs: traditional turbidity-based methods offer simplicity for initial screening, CFU-based approaches provide species resolution in complex communities, and optimized rhombic designs maximize efficiency for high-throughput applications. Regardless of the specific format, the checkerboard assay remains an indispensable tool for moving beyond single-variable optimization toward the combinatorial therapeutic strategies that represent the future of precision medicine.
The accurate measurement of protein biomarkers in complex biological matrices such as serum and urine remains a significant challenge in biomedical research and clinical diagnostics. Spike-and-recovery experiments are fundamental for validating enzyme-linked immunosorbent assay (ELISA) performance, determining whether analyte detection is affected by differences between the standard curve diluent and the biological sample matrix [2]. When a known amount of analyte is spiked into a natural sample matrix and the measured recovery differs significantly from the amount prepared in standard diluent, it indicates that components in the sample matrix are interfering with accurate quantification [2]. These matrix effects can lead to both false positives and false negatives, potentially compromising research conclusions and clinical decisions.
Urine presents particularly challenging matrix effects for immunoassays compared to serum, as demonstrated by a systematic evaluation of ELISA performance for bladder cancer biomarkers. This study found that the vast majority of commercially available ELISA tests showed disappointing performance with coefficients of variation >20% when applied to urine samples. Of eleven tests for seven different biomarkers, only three assays (for Secreted protein acidic and rich in cysteine, Survivin, and Slit homolog 2 protein) passed acceptable accuracy thresholds for clinical application [70]. These findings collectively reflect the difficulties in developing urine-based ELISA assays of sufficient analytical performance, presumably attributed to the urine matrix itself and/or the presence of markers in various isoforms [70].
Table 1: Key Challenges in Complex Matrices
| Challenge | Impact on ELISA Performance | Common Matrices Affected |
|---|---|---|
| Matrix Interference | Altered antibody-antigen binding, leading to inaccurate quantification | Serum, plasma, urine |
| Protein Variants | Detection of only specific isoforms, missing others | Urine (various biomarker isoforms) |
| Variable Composition | Inconsistent recovery between samples | Urine (pH, salts, concentration) |
| Autofluorescence | Background signal elevation | Serum, plasma |
Experimental Protocols for Assessing Recovery
Spike-and-Recovery Methodology
The spike-and-recovery experiment is designed to assess differences in assay response between the standard diluent and sample matrix [2]. The protocol involves spiking a known amount of analyte into both the natural test sample matrix and the standard diluent, then comparing the measured responses based on values calculated from a standard curve [2]. The specific experimental workflow can be visualized as follows:
The recovery percentage is calculated by comparing the observed concentration to the expected concentration, with the acceptable range typically being 80-120% recovery [2] [21]. If the recovery differs significantly from 100%, adjustments must be made to the method to minimize the discrepancy. Two primary approaches can be employed: altering the standard diluent to more closely match the final sample matrix composition, or modifying the sample matrix itself through dilution or the addition of carrier proteins [2].
Linearity of Dilution Assessment
Linearity-of-dilution experiments provide information about the precision of results for samples tested at different dilution levels in a chosen sample diluent [2]. This assessment is particularly important for samples with high analyte concentrations that need to be diluted to fall within the standard curve range. The traditional method involves preparing several dilutions of a sample containing a known concentration of analyte and testing each dilution to assess whether the measured concentrations demonstrate linearity when corrected for the dilution factor [2]. Poor linearity indicates that the natural sample matrix, sample diluent, and/or standard diluent affect analyte detectability differently, potentially caused by dilution of interfering components that inhibit or enhance detection in the assay method [2].
Case Study: ELISA Performance in Urine Matrix
A comprehensive 2016 study systematically evaluated the analytical performance of commercially available ELISA assays in urine for a series of potential biomarkers for bladder cancer [70]. The investigation focused on seven biomarkers previously described in the literature as having differential expression in bladder cancer: Secreted protein acidic and rich in cysteine (SPARC), Survivin, Slit homolog 2 protein (SLIT-2), NRC-Interacting Factor 1 (NIF-1), Histone 2B (H2B), Proteinase-3 (PR3), and Profilin-1 (PFN-1) [70]. The researchers conducted extensive analytical validation according to FDA guidelines, including standard curve analysis, assay reproducibility, linearity, and spiking experiments.
Table 2: ELISA Performance in Urine Matrix Case Study
| Biomarker | Number of Kits Tested | Passed Accuracy Thresholds | Key Performance Issues |
|---|---|---|---|
| SPARC | 1 | Yes | Acceptable recovery and reproducibility |
| Survivin | 2 | Yes (1 of 2) | Acceptable recovery and reproducibility |
| SLIT-2 | 1 | Yes | Acceptable recovery and reproducibility |
| NIF-1 | 2 | No | Poor reproducibility (CV>20%) |
| H2B | 2 | No | Poor reproducibility (CV>20%) |
| PFN-1 | 3 | No | Poor reproducibility (CV>20%) |
| PR3 | 1 | No | Poor reproducibility (CV>20%) |
The results demonstrated that only 3 out of 11 commercially available ELISA tests (27%) passed the accuracy thresholds and were found suitable for application in marker quantification [70]. The majority of assays showed coefficients of variation >20%, reflecting substantial challenges in achieving reliable biomarker quantification in urine matrices. This poor performance was attributed to the complex nature of urine matrix itself and potential presence of biomarkers in various isoforms that may not be equally recognized by the detection antibodies [70].
The experimental parameters assessed in this case study followed rigorous methodology:
- Recovery experiments were performed by spiking a negative urine sample with three different standard concentrations (high, medium, low) in four replicates each [70]
- Reproducibility was assessed using three urine samples containing high, medium, and low concentrations of each marker with at least five technical replicates to calculate coefficients of variation [70]
- Linearity was evaluated by performing serial dilutions (1:2 to 1:32) of urine samples with high marker concentration, with each test performed in at least four replicates [70]
- The limit of quantitation was determined by interpolating the absorbance of the lowest or highest standard on the standard curve [70]
Strategies for Improving Recovery in Complex Matrices
Methodological Adjustments
When spike-and-recovery experiments detect significant discrepancies, several adjustment strategies can improve assay performance. The two primary approaches include altering the standard diluent to more closely match the final sample matrix composition, or modifying the sample matrix itself through dilution in standard diluent or other logical "sample diluent" [2]. For example, if an undiluted serum sample produces poor spike and recovery, a sample diluted 1:1 in standard diluent may yield better results, provided the analyte level remains detectable [2]. Better recovery may also be obtained by adjusting the matrix pH to match the optimized standard diluent or by adding BSA or other purified protein as a carrier/stabilizer [2].
The selection of an appropriate ELISA kit requires careful evaluation of performance characteristics. Key factors to consider include:
- Accuracy and recovery data for the specific sample matrix of interest [21]
- Dilution linearity and parallelism demonstrating ≤20% difference from undiluted samples [21]
- Precision data showing both within-run and between-run coefficients of variation ≤15% [21]
- Specificity and cross-reactivity information ensuring detection only of the target analyte [21]
Alternative Technology Platforms
While ELISA remains the gold standard for biomarker validation, advanced technologies offer potential solutions to matrix effect challenges. Digital ELISA platforms represent a significant advancement, with one evaporation-driven approach demonstrating a >280-fold improvement in limit of detection compared to conventional 96-well ELISA [71]. This platform achieved a limit of detection of 64.23 fM for cardiac troponin I while maintaining >86% recovery in diluted human plasma with minimal non-specific adsorption [71].
Meso Scale Discovery (MSD) technology utilizes electrochemiluminescence detection to provide up to 100 times greater sensitivity than traditional ELISA, enabling detection of lower abundance proteins and offering a broader dynamic range [72]. MSD's U-PLEX multiplexed immunoassay platform allows researchers to design custom biomarker panels and measure multiple analytes simultaneously within a single sample, enhancing efficiency in biomarker research [72]. Liquid chromatography tandem mass spectrometry (LC-MS/MS) also surpasses ELISA in sensitivity and specificity, making it particularly useful for detecting low-abundance species and validating results obtained by immunoassays [72].
Table 3: Technology Comparison for Complex Matrices
| Technology | Sensitivity | Sample Volume | Multiplexing Capacity | Recovery in Complex Matrices |
|---|---|---|---|---|
| Traditional ELISA | Moderate | Moderate | Low | Variable (matrix-dependent) |
| Digital ELISA | Very High | Low | Low | >86% (reported) |
| MSD | High | Low | High | Improved (broader dynamic range) |
| LC-MS/MS | Very High | Moderate | Very High | Excellent (with proper sample prep) |
The following diagram illustrates the strategic decision process for addressing recovery issues:
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful resolution of recovery issues in complex matrices requires access to appropriate reagents and tools. The following table details essential research reagent solutions for ELISA validation in challenging matrices:
Table 4: Essential Research Reagent Solutions
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| Matrix-Matched Standards | Calibrators prepared in matrix similar to samples | Improves accuracy by minimizing matrix effects |
| Species-Specific ELISA Kits | Optimized for specific sample sources | Reduces cross-reactivity issues |
| Sample Dilution Buffers | Dilutes interfering substances | Critical for linearity of dilution |
| Carrier Proteins (BSA) | Stabilizes analytes in dilute solutions | Prevents adsorption to surfaces |
| Plate Coating Antibodies | Captures target analyte | High affinity antibodies improve sensitivity |
| Enzyme-Labeled Conjugates | Detects captured analyte | HRP and AP are most common |
| Chromogenic Substrates | Generates detectable signal | TMB is widely used for HRP |
| Blocking Buffers | Reduces non-specific binding | Critical for clean background |
| Plate Washers | Removes unbound material | Consistent washing is essential for precision |
The case studies and experimental data presented demonstrate that recovery issues in complex matrices like serum and urine represent significant challenges in ELISA-based biomarker research. The systematic evaluation of ELISA performance in urine matrix revealed that only a minority of commercially available tests (3 out of 11) demonstrated sufficient analytical performance for clinical application, with the majority showing coefficients of variation >20% [70]. These findings underscore the critical importance of thorough assay validation using appropriate spike-and-recovery and linearity-of-dilution experiments before applying ELISA methods to complex matrices [2].
Based on the evidence, researchers working with challenging matrices should implement the following best practices:
- Conduct comprehensive spike-and-recovery experiments during assay validation, with acceptance criteria of 80-120% recovery [2] [21]
- Perform linearity-of-dilution assessments to ensure samples can be accurately measured at different dilution factors [2]
- Carefully select ELISA kits with documented performance data in the specific matrix of interest [21]
- Consider alternative technology platforms such as digital ELISA, MSD, or LC-MS/MS when traditional ELISA demonstrates persistent recovery issues [71] [72]
- Systematically troubleshoot recovery problems using method adjustments including sample dilution, standard diluent modification, and carrier protein addition [2]
As the field advances, technologies such as evaporation-driven digital ELISA that lower limits of detection by >280-fold while maintaining >86% recovery in complex matrices represent promising approaches to overcoming current limitations [71]. By implementing rigorous validation methodologies and considering advanced technology platforms when appropriate, researchers can significantly improve the accuracy and reliability of biomarker quantification in challenging biological matrices.
Beyond Spike and Recovery: Integrating Dilutional Linearity and Parallelism for Comprehensive Validation
Linking Spike/Recovery with Dilutional Linearity and Parallelism
Enzyme-Linked Immunosorbent Assay (ELISA) validation is crucial for ensuring accurate and reliable quantification of specific analytes in various sample matrices. Differing antibody-analyte binding characteristics and potential interfering effects inherent to sample matrices exemplify the critical importance of thorough ELISA validation for accurate measurements [1]. Among the most essential validation experiments are spike/recovery, dilutional linearity, and parallelism - each providing distinct yet complementary information about assay performance and matrix effects. This guide compares these three fundamental approaches, providing researchers with methodologies, interpretation guidelines, and comparative analysis to ensure robust ELISA validation.
Understanding the Three Pillars of ELISA Validation
Spike/Recovery Experiments
Spike/recovery experiments determine whether the sample matrix affects analyte detection differently than the standard diluent [2]. This test measures the percent recovery between sample matrices and standard diluent by spiking a known quantity of standard analyte into both solutions [1] [22].
The fundamental question addressed is: "Does the percent recovery obtained from the standard diluent match the percent recovery obtained from the natural sample matrix?" [1] Ideal sample matrices should achieve 100% recovery, though deviations of ≤20% are generally acceptable [1] [2].
Dilutional Linearity Assessment
Dilutional linearity determines whether sample matrices spiked with detection analyte above the upper limit of detection can provide reliable quantification after dilution within standard curve ranges [1]. This confirms assay flexibility at varying dilutions and identifies whether low concentration samples without dilutions exhibit similar concentrations to equivalent samples generated from high concentration spike dilutions [1].
Samples displaying ideal linearity show minimal changes in observed analyte concentration compared to expected values after factoring dilutions, typically within 80-120% of expected values [1].
Parallelism Testing
Parallelism evaluates whether actual samples containing high endogenous analyte concentrations provide equivalent detection in the standard curve after dilution, signifying potential differences in antibody binding affinity between endogenous and standard analytes [1]. This test is particularly important for identifying differences in immunoreactivity that may arise from post-translational modifications or unspecified matrix effects affecting the analyte [1].
Experimental Protocols
Spike/Recovery Methodology
The spike/recovery protocol follows these essential steps [2]:
- Spike Preparation: Add a known amount of purified target protein to both the natural sample matrix and standard diluent
- Assay Execution: Run the ELISA to completion for both spiked solutions
- Concentration Calculation: Determine concentrations against a standard curve
- Recovery Calculation: Compare the observed concentration to the expected concentration
Calculation Formula: % Recovery = (Observed Concentration / Expected Concentration) × 100
Dilutional Linearity Protocol
The standard protocol for dilutional linearity assessment includes [1]:
- Sample Preparation: Spike sample matrices with a known quantity of standard analyte above the upper detection limit
- Serial Dilution: Perform 1:2 serial dilutions of spiked sample matrix until reaching the lower limit of quantification
- Measurement: Obtain absorbance readings and calculate mean concentrations for samples within the standard curve range
- Analysis: Compare observed versus expected concentrations after applying dilution factors
Parallelism Testing Protocol
A standard parallelism experiment involves [1]:
- Sample Identification: Select at least 3 samples with high endogenous analyte concentrations (not exceeding the upper quantification limit)
- Serial Dilution: Perform 1:2 serial dilutions using sample diluent until predicted concentrations fall below the lower limit of quantification
- Analysis: Analyze neat and diluted sample optical densities with dilution factors applied
- Calculation: Determine mean concentrations and calculate percentage coefficient of variation (%CV)
%CV within 20-30% generally indicates successful parallelism, though exact acceptable percentages should be determined by researchers based on their specific requirements [1].
Comparative Experimental Data
Performance Comparison Table
Table 1: Key Characteristics of ELISA Validation Methods
| Parameter | Spike/Recovery | Dilutional Linearity | Parallelism |
|---|---|---|---|
| Primary Purpose | Assess matrix effects on detection [2] | Verify accuracy across dilutions [1] | Compare immunoreactivity between endogenous and standard analyte [1] |
| Sample Requirements | Sample matrix + standard diluent [2] | Sample matrix spiked above ULOQ [1] | Samples with high endogenous analyte [1] |
| Acceptance Criteria | 80-120% recovery [1] | 80-120% of expected values [1] | 20-30% CV [1] |
| Key Output | Percentage recovery [2] | Linearity across dilution series [1] | Coefficient of variation (%CV) [1] |
| Identifies Issues With | Matrix interference [1] | Hook effect, dilution inconsistencies [1] | Antibody affinity differences [1] |
Representative Experimental Data
Table 2: Example Spike/Recovery Data for Human IL-1 Beta in Urine Samples [2]
| Sample | No Spike (0 pg/mL) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|---|
| Diluent Control | 0.0 | 17.0 | 44.1 | 81.6 |
| Donor 1 | 0.7 | 14.6 | 39.6 | 69.6 |
| Donor 2 | 0.0 | 17.8 | 41.6 | 74.8 |
| Donor 3 | 0.6 | 15.0 | 37.6 | 68.9 |
| Mean Recovery | NA | 86.3% ± 9.9% | 85.8% ± 6.7% | 84.6% ± 3.5% |
Table 3: Example Dilutional Linearity Results [1]
| Dilution | Expected (pg/ml) | Observed (pg/ml) | Recovery (%) |
|---|---|---|---|
| Neat | — | 390.8 | — |
| 1:2 | 195.4 | 194.6 | 100% |
| 1:4 | 97.7 | 105.1 | 108% |
| 1:8 | 48.8 | 67.0 | 137% |
| 1:16 | 24.4 | 27.9 | 114% |
| 1:32 | 12.2 | 12.1 | 99% |
Interrelationship Visualization
Troubleshooting Common Issues
Addressing Poor Spike/Recovery Results
When spike/recovery experiments detect significant discrepancies, two primary adjustments can optimize ELISA performance [2]:
- Alter the Standard Diluent: Use a standard diluent whose composition more closely matches the final sample matrix
- Modify the Sample Matrix: Dilute neat biological samples in standard diluent or adjust pH/add carrier proteins like BSA to improve compatibility
Correcting Dilutional Linearity Problems
Poor linearity indicates that the natural sample matrix, sample diluent, and/or standard diluent affect analyte detectability differently [2]. This may be caused by dilution of components in one solution that inhibit or enhance detection compared to other solutions. Optimization typically involves adjusting the sample diluent to better align with the standard diluent's composition [1].
Resolving Parallelism Issues
Higher %CV than acceptable values indicates a loss of parallelism and suggests significant differences in immunoreactivity between endogenous and standard analyte [1]. This may result from post-translational modifications or unspecified matrix effects affecting the analyte, potentially requiring antibody selection or sample processing modifications.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Reagents for ELISA Validation Experiments
| Reagent/Category | Function in Validation | Examples/Specifications |
|---|---|---|
| Coating Antibodies | Immobilize target antigen | Concentration range: 1-15 µg/mL depending on purity [59] |
| Detection Antibodies | Bind captured antigen for detection | Concentration range: 0.5-10 µg/mL depending on purity [59] |
| Blocking Buffers | Prevent non-specific binding | 4% skimmed milk, BSA, or commercial blocking solutions [73] |
| Sample Diluents | Dilute samples while maintaining compatibility | PBS with carrier proteins, matching sample matrix composition [2] |
| Standard Diluents | Dilute standard curve analytes | Optimized for signal-to-noise performance, often with stabilizers [2] |
| Enzyme Conjugates | Enable detection through enzymatic reaction | HRP: 20-200 ng/mL (colorimetric); AP: 100-200 ng/mL (colorimetric) [59] |
| Validation Controls | Monitor assay performance | Positive, negative, and non-specific binding controls [22] |
Integrated Validation Strategy
A comprehensive ELISA validation approach strategically combines these three methodologies to provide complementary data. While each method addresses specific aspects of assay performance, their interrelationship creates a robust validation framework:
- Spike/recovery identifies general matrix effects
- Dilutional linearity confirms accurate quantification across concentrations
- Parallelism validates antibody compatibility with endogenous analyte
This integrated approach ensures reliable analyte quantification across different sample types and concentrations, providing confidence in ELISA results for both research and diagnostic applications [1] [2] [21].
Dilutional linearity is a critical method in ELISA validation that determines whether a sample spiked with a known analyte concentration, or a sample with high endogenous analyte levels, provides reliable quantification across different dilution factors. This assessment confirms the precision of results for samples tested at various dilution levels in a chosen sample diluent, providing essential information about matrix effects and assay compatibility. When an assay demonstrates good linearity over a wide range of dilutions, researchers gain flexibility to assay samples with different analyte concentrations, ensuring that values fall within the standard curve range while maintaining accuracy and reliability. The fundamental principle of dilutional linearity verification lies in demonstrating that the observed concentration of an analyte, when multiplied by its dilution factor, consistently approximates the expected concentration, typically within an acceptable recovery range of 80-120% [1].
In the broader context of ELISA validation, dilutional linearity is intrinsically related to spike-and-recovery experiments, as both address how sample matrices and diluents affect analyte detection. While spike-and-recovery experiments determine whether sample constituents affect antigen detection by comparing recovery rates between sample matrix and standard diluent, dilutional linearity specifically evaluates how these potential matrix effects behave across a dilution series. This relationship is crucial because poor performance in either test typically stems from the same root causes: components in the sample matrix that interfere with antibody-antigen binding, such as salts, pH variations, detergents, or competing protein interactions [2] [1]. Understanding this interconnection allows researchers to design efficient validation protocols that simultaneously address both parameters, optimizing resources while ensuring comprehensive assay validation.
Theoretical Foundation and Relationship to Assay Validation
Key Concepts and Definitions
Dilutional linearity, parallelism, and spike-and-recovery represent three interconnected validation parameters that collectively ensure ELISA reliability. Dilutional linearity specifically determines whether sample matrices spiked with detection analyte above the upper limit of detection can still provide reliable quantification after dilution within standard curve ranges [1]. Samples displaying minimal deviation in concentration after factoring dilutions demonstrate linearity, confirming assay accuracy and flexibility across varying dilution factors. This characteristic is fundamental for researchers working with samples of unknown concentration that may require dilution to fall within the assay's dynamic range.
Parallelism represents a related but distinct validation parameter that determines whether actual samples containing high endogenous analyte concentrations provide equivalent detection in the standard curve after dilutions [1]. This parameter specifically signifies differences in antibody binding affinity between endogenous analyte and standard/calibration analyte. The key methodological distinction lies in the sample source: parallelism utilizes samples containing high levels of endogenous analyte rather than spiked samples, revealing whether the immunological characteristics of the native analyte match those of the recombinant or purified standard used for calibration.
Spike-and-recovery experiments form the third component of this validation triad, determining the effect sample constituents have on detection of the antigen by the antibody [4]. In this assessment, known concentrations of protein are spiked into both the sample matrix and a standard diluent, followed by quantification using the assay and comparison of results [4]. This approach directly tests whether components in the biological sample matrix (such as plasma proteins, proteases, or other interfering substances) affect the antibody-antigen interaction differently than the optimized standard diluent.
Interrelationship of Validation Parameters
These three validation approaches form a complementary framework for assessing different aspects of assay reliability. While each tests distinct characteristics, they share common underlying principles and interpretative frameworks. The same matrix effects that cause poor spike recovery (such as salts, pH imbalances, detergents, or protein interactions) typically also manifest as non-linearity in dilution experiments [2] [1]. Similarly, discrepancies between endogenous and standard analyte detection in parallelism studies often reflect the same matrix interference issues that affect dilutional linearity. This interconnectedness means that experimental designs can efficiently combine these assessments using checkerboard matrices of spike levels, sample types, and dilution factors to simultaneously evaluate multiple validation parameters [2].
The following diagram illustrates the experimental workflow and decision process for integrated ELISA validation incorporating dilutional linearity, parallelism, and spike-and-recovery assessments:
Diagram: ELISA Validation Workflow integrating dilutional linearity, parallelism, and spike-and-recovery assessments.
Experimental Protocols and Methodologies
Dilutional Linearity Experimental Protocol
The dilutional linearity experiment follows a systematic approach to evaluate assay accuracy across a dilution series. The following protocol represents the standard methodology:
Sample Preparation: Spike a known quantity of standard analyte into the sample matrix at a concentration exceeding the upper detection limit of the standard curve. Commonly used matrices include substitute matrices that replicate actual test samples or sample matrices with free or low concentrations of detectable analyte [1].
Dilution Series: Conduct 1:2 serial dilutions of the spiked sample matrix using the chosen sample diluent until the predicted concentration falls below the lower limit of quantification of the standard curve [1]. Ensure proper dilution technique by using fresh pipette tips for each transfer and adequate mixing between dilutions.
Assay Execution: Run the complete ELISA procedure on all diluted samples alongside the standard curve according to manufacturer protocols. Include appropriate controls to account for background signal and matrix effects.
Data Collection: Obtain absorbance values for all samples and calculate mean concentrations only for sample ranges within the lower and upper limits of the standard curve [1]. Exclude any values that fall outside the measurable range of the assay.
Calculation: For each dilution, calculate the observed concentration, multiply by the dilution factor, and compare to the expected concentration (typically the neat or starting concentration). Express the relationship as percentage recovery using the formula: (Observed × Dilution Factor / Expected) × 100% [1].
Parallelism Testing Protocol
Parallelism testing follows a distinct protocol focused on samples with endogenous analyte:
Sample Selection: Identify at least three samples that display high concentrations of endogenous analyte, ensuring they do not exceed the upper limit of quantification in the standard curve [1].
Dilution Series: Perform 1:2 serial dilutions using sample diluent until the predicted concentration falls below the lower limit of quantification of the standard curve [1].
Assay Execution: Analyze both neat and diluted sample optical density values alongside the standard curve, ensuring all measurements fall within the standard curve limits.
Data Analysis: Determine mean concentrations of samples with dilution factors applied and calculate the percentage coefficient of variation (%CV) across the dilution series [1].
Integrated Experimental Design
For comprehensive validation, researchers can implement an integrated approach that simultaneously assesses dilutional linearity, parallelism, and spike-and-recovery using a checkerboard matrix of spike levels, sample types, sample diluents, and dilution factors [2]. This efficient experimental design maximizes information while conserving valuable samples and reagents. The integrated approach involves preparing a master sample set that includes:
- Samples with high endogenous analyte levels for parallelism assessment
- Sample matrices spiked with known analyte concentrations at low, medium, and high levels
- Multiple dilution factors for each sample type (e.g., neat, 1:2, 1:4, 1:8)
- Corresponding standard curve points prepared in both standard diluent and sample matrix
This comprehensive design generates data sufficient for evaluating all three validation parameters while identifying optimal dilution factors for different sample types and establishing the practical working range of the assay for each validated matrix.
Data Analysis and Interpretation
Calculation Methods and Acceptance Criteria
Proper data analysis is essential for accurate interpretation of dilutional linearity experiments. The fundamental calculation involves determining the percentage recovery at each dilution level using the formula:
Recovery % = (Observed Concentration × Dilution Factor / Expected Concentration) × 100% [1]
Samples displaying ideal linearity should demonstrate minimal changes in observed analyte concentration compared to the final analyte concentration after factoring dilutions. While 100% recovery represents perfection, acceptable linearity is typically achieved for sample recoveries within 80-120% of expected values [1]. The highest dilution of an analyte that maintains linearity within this acceptable range is designated the "limit of dilution," establishing the practical working range for the assay with that specific sample matrix.
For parallelism assessments, interpretation focuses on the percentage coefficient of variation (%CV) across the dilution series. The %CV is calculated using the formula:
%CV = (Standard Deviation / Mean) × 100% [74]
Successful parallelism generally displays %CV within 20-30% of expectations, though researchers should establish exact percentage thresholds based on their specific accuracy requirements [1]. Consistent %CV values within this range indicate comparable immunoreactivity between endogenous and standard analytes, validating the use of the standard curve for quantifying native samples.
Representative Data Presentation
The following table presents typical dilutional linearity results for a hypothetical cytokine ELISA in cell culture supernatant, illustrating the calculation method and interpretation:
Table 1: Representative Dilutional Linearity Data for Cytokine ELISA in Cell Culture Supernatant
| Dilution Factor | Expected (pg/mL) | Observed (pg/mL) | Observed × DF | Recovery (%) | Interpretation |
|---|---|---|---|---|---|
| Neat | — | 390.8 | 390.8 | — | Reference value |
| 1:2 | 195.4 | 194.6 | 389.2 | 100% | Acceptable |
| 1:4 | 97.7 | 105.1 | 420.4 | 108% | Acceptable |
| 1:8 | 48.8 | 67.0 | 536.0 | 137% | Unacceptable |
| 1:16 | 24.4 | 27.9 | 446.4 | 114% | Acceptable |
| 1:32 | 12.2 | 12.1 | 387.2 | 99% | Acceptable |
This representative data demonstrates several key interpretation principles. The 1:8 dilution shows unacceptable recovery (137%), potentially due to matrix effects becoming pronounced at intermediate dilution levels, while more extreme dilutions (1:16, 1:32) show improved recovery as interfering components are sufficiently diluted. This pattern supports establishing a minimum recommended dilution of 1:16 for this specific sample type to ensure accurate quantification [1].
For parallelism assessment, the following table illustrates typical data presentation and evaluation criteria:
Table 2: Parallelism Assessment for Three High-Endogenous Analyte Samples
| Sample Type | Dilution Factor | Observed (pg/mL) | Observed × DF | %CV Across Dilutions | Interpretation |
|---|---|---|---|---|---|
| Serum A | Neat | 128.7 | 128.7 | 8.2% | Acceptable |
| 1:2 | 142.6 | 285.2 | |||
| 1:4 | 139.2 | 556.8 | |||
| 1:8 | 171.5 | 1372.0 | |||
| Plasma B | Neat | 95.3 | 95.3 | 15.7% | Acceptable |
| 1:2 | 102.1 | 204.2 | |||
| 1:4 | 98.7 | 394.8 | |||
| 1:8 | 112.4 | 899.2 | |||
| Culture Supernatant C | Neat | 131.5 | 131.5 | 22.4% | Acceptable |
| 1:2 | 149.9 | 299.8 | |||
| 1:4 | 162.2 | 648.8 | |||
| 1:8 | 165.4 | 1323.2 |
This parallelism data demonstrates that all three sample types show %CV values within the generally acceptable 20-30% range, though Culture Supernatant C approaches the upper limit, potentially indicating minor matrix effects or differences in immunoreactivity between endogenous and standard analyte [1].
Troubleshooting and Method Optimization
Addressing Poor Dilutional Linearity
When dilutional linearity falls outside the acceptable 80-120% recovery range, systematic troubleshooting is essential to identify and rectify the underlying causes. The most common contributors to poor linearity include matrix components such as salts, pH imbalances, detergents, protein interactions, or other elements that interfere with antibody binding [1]. The following optimization strategies can address these issues:
Adjust Sample Dilution: The most straightforward approach involves modifying the dilution scheme to ensure samples are analyzed within their optimal dilution range. If specific dilutions show poor recovery (as demonstrated in Table 1), establishing minimum recommended dilutions that skip problematic ranges often resolves linearity issues [1].
Modify Sample Diluent Composition: Altering the sample diluent to more closely match the standard diluent can significantly improve linearity. This may involve adjusting pH, adding carrier proteins like BSA (1% concentration is common), or including stabilizers that protect the analyte-antibody interaction from matrix interference [2].
Optimize Standard Diluent: In cases where sample matrix cannot be sufficiently modified, preparing the standard curve in a diluent that more closely matches the sample matrix can improve comparability. For example, using culture medium as the standard diluent when analyzing culture supernatants aligns the matrix effects between standards and samples [2].
Employ Alternative Dilution Schemes: If 1:2 serial dilutions demonstrate non-linearity at specific points, alternative dilution factors (e.g., 1:5 or 1:10 series) may bypass problematic ranges while still providing sufficient points for accurate quantification.
Correcting Parallelism Issues
When parallelism assessments yield %CV values exceeding the 20-30% acceptable range, this indicates significant differences in immunoreactivity between endogenous and standard analytes. Potential causes include post-translational modifications in native proteins, protein complexes in biological samples that mask antibody epitopes, or unspecified matrix effects affecting analyte detection [1]. Resolution strategies include:
Sample Pre-treatment: Implementing extraction procedures, protein degradation, or other pre-analytical processing steps can reveal masked epitopes and improve detection consistency across dilutions.
Alternative Antibody Pairs: If the ELISA kit employs matched antibody pairs, investigating alternative pairs with different epitope specificities may bypass interference caused by protein modifications or complex formation.
Diluent Optimization: Similar to dilutional linearity issues, adjusting the sample diluent to include mild detergents, salt concentration adjustments, or protein stabilizers can improve parallelism by creating more consistent antibody-antigen interactions across the dilution series.
Platform Validation: When parallelism issues persist despite optimization efforts, validating results with an alternative detection platform (e.g., Western blot, multiplex immunoassay) may be necessary to confirm whether the ELISA itself is inappropriate for the specific sample type due to fundamental immunoreactivity differences.
The Scientist's Toolkit: Essential Research Reagents
Successful dilutional linearity assessment requires specific reagents and materials optimized for ELISA applications. The following table details essential research reagent solutions and their functions in validation experiments:
Table 3: Essential Research Reagents for Dilutional Linearity Assessment
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Reference Standard | Purified analyte for calibration curve and spiking experiments | Use the same lot throughout validation; prepare fresh dilutions for each experiment [75] |
| Sample Diluent | Matrix for diluting samples and standards | Optimize composition to match sample matrix; may include BSA, salts, detergents [2] |
| Matrix-Matched Standard Diluent | Standard diluent modified to mimic sample matrix | Improves comparability when sample matrix affects detection; use culture medium for culture supernatants [2] |
| Low-Analyte Matrix | Native matrix with minimal endogenous analyte | Used as base for spiking experiments in dilutional linearity assessment [1] |
| Coated ELISA Plates | Solid phase with immobilized capture antibody | Ensure consistent lot-to-llot performance; pre-test with quality controls [75] |
| Detection Antibodies | Labeled antibodies for signal generation | Matched pair configurations optimize specificity; conjugate with HRP or other enzymes [4] |
| Wash Buffer | Solution for removing unbound materials | Critical for reducing background; typically PBS with mild detergent (e.g., 0.05% Tween-20) [75] |
| Substrate Solution | Enzyme substrate for colorimetric detection | TMB is most common; protect from light; discard if pre-color development occurs [76] |
| Stop Solution | Acidic solution to terminate enzyme reaction | Stabilizes signal for measurement; compatible with plate reader detection [77] |
Comparative Performance Data
Inter-laboratory Validation Studies
Comprehensive ELISA validation requires assessment across multiple sample matrices and species. The following table compiles spike recovery data across diverse biological matrices, illustrating the variability in assay performance and minimum recommended dilutions:
Table 4: Spike Recovery Performance Across Biological Matrices
| Sample Matrix | Spike Concentration (ng/mL) | % Recovery | Minimum Recommended Dilution | Linearity Assessment |
|---|---|---|---|---|
| Human Serum Extracted | 2 | 102% | Neat | Acceptable |
| 1 | 83% | Neat | Acceptable | |
| 0.5 | 124% | Neat | Marginal | |
| Human EDTA Plasma Extracted | 2 | 101% | Neat | Acceptable |
| 1 | 90% | Neat | Acceptable | |
| 0.5 | 112% | Neat | Acceptable | |
| Mouse Serum Extracted | 1 | 91% | 1:2 | Acceptable |
| 0.5 | 106% | 1:2 | Acceptable | |
| 0.25 | 116% | 1:2 | Acceptable | |
| Porcine Serum Extracted | 3 | 103% | 1:2 | Acceptable |
| 0.6 | 108% | 1:2 | Acceptable | |
| 0.12 | 113% | 1:2 | Acceptable | |
| Human Saliva Extracted | 5 | 83% | 1:2 | Acceptable |
| 2.5 | 99% | 1:2 | Acceptable | |
| 1.25 | 108% | 1:2 | Acceptable | |
| Banana Extracted | 5 | 101% | 1:2 | Acceptable |
| 2.5 | 116% | 1:2 | Marginal | |
| 1.25 | 88% | 1:2 | Acceptable |
This comparative data reveals several important patterns. Human serum and plasma matrices frequently demonstrate acceptable recovery at neat concentrations, suggesting minimal interference in these matrices. In contrast, mouse serum, porcine serum, and saliva matrices require 1:2 dilution to achieve consistent recovery within the 80-120% acceptable range, indicating more pronounced matrix effects in these biological fluids. The plant matrix (banana extract) shows variable performance across spike concentrations but generally achieves acceptability at 1:2 dilution, highlighting the importance of matrix-specific validation [1].
Intra-assay vs. Inter-assay Precision in Validation
Comprehensive ELISA validation further requires assessment of both intra-assay (within-plate) and inter-assay (between-plate) precision, particularly when establishing parallelism and dilutional linearity. The following table presents typical precision data across different analyte concentrations:
Table 5: Intra-assay and Inter-assay Precision in ELISA Validation
| Analyte Concentration | Intra-assay %CV | Inter-assay %CV | Acceptance Met |
|---|---|---|---|
| Low (171 pg/mL) | 8.0% | 13.1% | Yes |
| Medium (403 pg/mL) | 8.4% | 8.2% | Yes |
| High (780 pg/mL) | 6.6% | 7.8% | Yes |
This precision data demonstrates that well-optimized ELISA methods can achieve %CV values well below the generally accepted 20% threshold for duplicates [74], with even inter-assay variability remaining below 15% across different analyte concentrations. Such precision values provide confidence in both dilutional linearity and parallelism assessments, as they indicate minimal technical variability contributing to observed differences across dilution series [1].
Dilutional linearity assessment represents an essential component of comprehensive ELISA validation, providing critical information about matrix effects and assay reliability across sample dilutions. When integrated with parallelism and spike-and-recovery experiments, this approach delivers a robust framework for verifying that ELISA methods generate accurate, reproducible results across diverse biological matrices. The experimental protocols and troubleshooting strategies outlined in this guide provide researchers with practical methodologies for implementing these validation techniques in their own laboratories. As the comparative performance data demonstrates, matrix-specific validation remains essential, with different biological samples often requiring customized dilution schemes or diluent modifications to achieve optimal performance. Through systematic application of these validation principles, researchers can ensure the generation of reliable, reproducible data that meets the rigorous standards required for both basic research and drug development applications.
In the rigorous world of immunoassay validation, particularly with Enzyme-Linked Immunosorbent Assay (ELISA), parallelism serves as a critical experimental approach for evaluating whether the immunoreactivity of an endogenous analyte in a biological sample matches that of a purified standard. This assessment is fundamental for ensuring that quantitation results accurately reflect true analyte concentrations in complex matrices. Spike and recovery experiments, along with linearity-of-dilution assessments, are established methodologies designed specifically to address this challenge by detecting potential matrix effects that could compromise assay accuracy [2]. These experiments are indispensable in pharmaceutical development, clinical diagnostics, and biomedical research, where precise measurement of biomarkers, hormones, and other analytes in biological fluids directly impacts scientific conclusions and therapeutic decisions.
The core principle behind parallelism validation lies in the concern that components within a biological sample matrix—such as proteins, lipids, or salts—may alter antibody binding affinity or otherwise interfere with the detection system, leading to either overestimation or underestimation of the true analyte concentration [78]. When the immunoreactivity of the endogenous analyte differs from that of the standard, the fundamental assumption of the standard curve is broken, potentially invalidating experimental results. Consequently, regulatory bodies like the FDA and EMA emphasize the importance of these validation procedures, with acceptance criteria generally requiring recovery values within 75% to 125% of the spiked concentration to be considered acceptable [78].
Experimental Protocols for Assessing Parallelism
Spike-and-Recovery Experimental Methodology
The spike-and-recovery experiment is designed to determine whether analyte detection is affected by differences between the standard curve diluent and the biological sample matrix. The procedure systematically compares the assay response of a known analyte amount spiked into the natural sample matrix against an identical spike prepared in the standard diluent [2].
Step-by-Step Protocol:
- Sample Preparation: Prepare aliquots of the biological sample matrix (e.g., serum, plasma, urine). For each sample type, include a "neat" (undiluted) aliquot to measure endogenous analyte levels and multiple aliquots for spiking.
- Analyte Spiking: Spike known amounts of the purified standard analyte into the sample matrix aliquots. Typically, 3-4 concentration levels covering the analytical range of the assay are used, ensuring the lowest spike is at least 2 times the assay's Limit of Quantitation (LOQ) [78].
- Control Preparation: In parallel, prepare identical spikes of the standard analyte into the standard diluent used for the standard curve. This serves as the reference for 100% recovery.
- Assay Execution: Run the complete ELISA procedure on all spiked samples, controls, and the neat sample according to the established protocol.
- Data Calculation: Calculate the percentage recovery for each spiked sample using the formula:
- Recovery % = [(Measured concentration in spiked sample - Endogenous concentration in neat sample) / Theoretical spike concentration] × 100
Linearity-of-Dilution Experimental Methodology
The linearity-of-dilution experiment, often performed in conjunction with spike-and-recovery, assesses the precision of results for samples tested at different dilution levels in a chosen sample diluent. It confirms that the dose response remains linear and within the assay's desired range, providing flexibility for samples with varying analyte concentrations [2].
Step-by-Step Protocol:
- Sample Dilution Series: Select a sample with a known level of endogenous analyte or a spiked sample. Prepare a series of dilutions (e.g., neat, 1:2, 1:4, 1:8) in the chosen sample diluent.
- Assay Execution: Analyze all dilutions in the ELISA alongside the standard curve.
- Data Analysis: For each dilution, multiply the observed concentration by its dilution factor to obtain the "calculated neat concentration."
- Recovery Calculation: Compare this calculated value to the actual measured concentration of the neat (undiluted) sample:
- Linearity Recovery % = (Calculated neat concentration / Actual neat concentration) × 100
Table 1: Key Components for Parallelism Experiments
| Component | Function & Description | Examples |
|---|---|---|
| Solid Phase | Matrix to which antibodies or antigens are immobilized [14]. | 96-well microplates (polystyrene, polyvinyl) [14]. |
| Capture & Detection Antibodies | Provide specificity by binding to the target analyte. Pairs are selected to bind different epitopes [79]. | High-quality, validated monoclonal or polyclonal antibodies [79]. |
| Enzyme-Labeled Conjugate | Antibody bound to an enzyme for signal generation [14]. | Horseradish Peroxidase (HRP) or Alkaline Phosphatase (AP) conjugates [14]. |
| Chromogenic Substrate | Reacts with the enzyme to produce a measurable color change [14]. | TMB (tetramethylbenzidine) for HRP; BCIP/NBT for AP [14]. |
| Standard Diluent | Buffer used to prepare the standard curve [2]. | Phosphate-buffered saline (PBS), often with additives like BSA [2]. |
| Sample Diluent | Buffer used to dilute biological samples to the Minimum Required Dilution (MRD) [78]. | PBS, often optimized to match sample matrix and reduce interference [2]. |
Comparative Experimental Data and Performance
Representative Spike-and-Recovery Data
The following table summarizes data from a spike-and-recovery experiment for recombinant human IL-1 beta in human urine samples, illustrating typical results and the calculation of mean recovery percentages [2].
Table 2: ELISA Spike-and-Recovery of Recombinant Human IL-1 beta in Human Urine
| Sample | No Spike (0 pg/mL) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|---|
| Diluent Control | 0.0 | 17.0 | 44.1 | 81.6 |
| Donor 1 | 0.7 | 14.6 | 39.6 | 69.6 |
| Donor 2 | 0.0 | 17.8 | 41.6 | 74.8 |
| Donor 3 | 0.6 | 15.0 | 37.6 | 68.9 |
| ... | ... | ... | ... | ... |
| Mean Recovery % (± S.D.) | NA | 86.3% +/- 9.9% | 85.8% +/- 6.7% | 84.6% +/- 3.5% |
Representative Linearity-of-Dilution Data
The table below demonstrates linearity-of-dilution results for human IL-1 beta in different sample types, showing how recovery percentages are calculated across a dilution series [2].
Table 3: ELISA Linearity-of-Dilution for Human IL-1 Beta
| Sample | Dilution Factor (DF) | Observed (pg/mL) × DF | Expected (pg/mL) | Recovery % |
|---|---|---|---|---|
| ConA-stimulated Cell Culture Supernatant | Neat | 131.5 | 131.5 | 100 |
| 1:2 | 149.9 | 114 | ||
| 1:4 | 162.2 | 123 | ||
| 1:8 | 165.4 | 126 | ||
| High-Level Serum Sample | Neat | 128.7 | 128.7 | 100 |
| 1:2 | 142.6 | 111 | ||
| 1:4 | 139.2 | 108 | ||
| 1:8 | 171.5 | 133 | ||
| Low-Level Serum Sample (Spiked) | Neat | 39.3 | 39.3 | 100 |
| 1:2 | 47.9 | 122 | ||
| 1:4 | 50.5 | 128 | ||
| 1:8 | 54.6 | 139 |
Inter-Assay Variability in Commercial Kits
It is crucial to note that different ELISA kits can yield varying absolute quantitations of the same analyte due to differences in antibody pairs, standard preparation, and buffer composition. A comparative study of four commercial corticosterone ELISA kits on identical rat serum samples found statistically significant differences in reported concentrations, although relative differences within studies remained consistent [80]. This underscores the necessity of full validation, including parallelism, for each specific assay and matrix combination.
Troubleshooting and Optimization Strategies
Addressing Poor Spike-and-Recovery and Linearity
When recovery values fall outside the acceptable range (typically 75-125%), it indicates that the sample matrix is interfering with analyte detection [78]. The following strategies can be employed to resolve these issues:
- Optimize the Sample Diluent and Dilution Factor: The most common corrective action is to dilute the sample in a standard diluent. This dilution reduces the concentration of interfering substances. The optimal Minimum Required Dilution (MRD) should be determined experimentally [78]. For instance, if an undiluted serum sample shows poor recovery, a 1:1 or 1:2 dilution in PBS or a kit-specific diluent may bring recovery within the acceptable range [2].
- Modify the Standard Diluent: If possible, adjust the standard diluent to more closely match the final composition of the sample matrix after dilution. For example, adding a carrier protein like BSA to the standard diluent can mimic the protein background of a serum sample, making the standard and sample behave more similarly during the assay [2].
- Adjust Sample Matrix Properties: In some cases, modifying the pH of the sample diluent to match that of the optimized standard diluent can improve recovery. Additionally, for samples with very low protein content, adding a carrier protein can stabilize the analyte and prevent loss [2].
Research Reagent Solutions for ELISA Validation
Successful parallelism experiments and robust ELISA performance depend on high-quality, specific reagents. The following toolkit is essential for researchers developing or validating immunoassays.
Table 4: Essential Research Reagent Toolkit for ELISA Validation
| Reagent / Material | Critical Function | Selection & Validation Criteria |
|---|---|---|
| Matched Antibody Pairs | Provide the foundation for a sensitive and specific sandwich ELISA. The capture and detection antibodies must bind to non-overlapping epitopes on the target analyte [79]. | Select pairs rigorously validated for specificity and affinity. Reproducibility and batch-to-batch consistency from the supplier are paramount [79]. |
| Purified Recombinant Protein Standard | Serves as the reference material for constructing the standard curve and for spiking in recovery experiments. Its immunoreactivity is the benchmark for comparison [2]. | Must be highly pure and well-characterized. The protein should be identical to the endogenous target to ensure immunological equivalence. |
| Optimized Assay Buffers | Include coating, blocking, sample diluent, and wash buffers. Their composition is critical for minimizing non-specific binding and matrix interference [2] [14]. | Sample diluent must be optimized to match the specific biological matrix (e.g., serum, urine, cell culture supernatant) to achieve valid recovery. |
| Validated Commercial Kits | Provide a complete, optimized system with pre-coated plates, standards, and reagents, offering convenience and standardized protocols [79]. | Choose kits validated for your specific sample matrix. Look for guarantees of batch-to-batch consistency and performance data provided by the manufacturer [80] [79]. |
| High-Affinity Coated Plates | The solid phase to which the capture antibody is immobilized. Plate quality and binding capacity affect assay sensitivity and precision [14]. | Use plates with high protein-binding capacity and low chemical background. 96-well and 384-well formats are standard for high-throughput analysis [14] [79]. |
Designing a Single Experiment to Assess Multiple Validation Parameters
This guide presents a unified experimental design for the simultaneous assessment of spike and recovery, linearity of dilution, and parallelism in ELISA validation. We compare this integrated approach against traditional standalone experiments, providing experimental data that demonstrates how a single, strategically planned assay can deliver comprehensive method validation while conserving resources. Designed for researchers and drug development professionals, this protocol offers a efficient framework for establishing ELISA reliability within a single experimental run.
Enzyme-linked immunosorbent assay (ELISA) validation is crucial for producing reliable, reproducible data in research, diagnostic, and drug development settings [35]. Traditional validation involves conducting separate, sequential experiments for key parameters like spike and recovery, linearity of dilution, and parallelism [2] [9]. This fragmented approach consumes significant time, reagents, and sample material. This guide details an alternative: a single, comprehensive experiment that concurrently evaluates all these parameters. The integrated design not only conserves resources but also provides a more holistic view of assay performance under consistent conditions, making it particularly valuable for laboratories validating new methods or transferring established methods to new matrices.
Comparative Analysis: Integrated vs. Traditional Validation
The table below compares the unified experimental approach with traditional standalone validation methods, highlighting key efficiency gains.
Table 1: Comparison of Integrated vs. Traditional Validation Approaches
| Validation Parameter | Traditional Approach | Integrated Unified Approach | Key Advantages of Unified Design |
|---|---|---|---|
| Spike & Recovery | Separate experiment using sample matrix spiked with analyte [2] | Sample matrix spiked with analyte at multiple concentrations | Uses the same spiked dilutions for recovery and linearity assessment |
| Linearity of Dilution | Separate serial dilution of a high-concentration sample [2] | Serial dilution of the same spiked sample matrix | Eliminates need for a separate high-concentration sample |
| Parallelism | Separate serial dilution of a native sample with high endogenous analyte [22] | Serial dilution of a native sample with high endogenous analyte | Uses the same native sample dilutions for parallelism and linearity |
| Data Output | Individual parameter assessments | Combined data set for all parameters | Provides a complete picture of matrix effects and antibody affinity |
| Resource Consumption | High (multiple plates, more reagents) | Low (single plate, minimal reagents) | Saves time, reagents, and sample volume |
Unified Experimental Protocol
Experimental Workflow and Design
The following diagram illustrates the core workflow and logical relationships in the unified experimental design.
Step-by-Step Methodology
Sample Preparation:
- Spiked Matrix Sample: Select the biological matrix of interest (e.g., serum, urine, cell culture supernatant). Spike it with a known, high concentration of the purified recombinant analyte. This creates the primary sample for assessing spike recovery and dilution linearity [2].
- Native Sample: Identify a sample known to contain a high endogenous concentration of the analyte. This sample will be used to assess parallelism [22].
- Standard Curve: Prepare the standard curve by serially diluting the purified analyte in the standard diluent, as per the ELISA protocol [4].
Serial Dilution Scheme:
ELISA Execution:
- Run all samples in a single ELISA plate to ensure consistent conditions. Include the following in duplicate or triplicate:
Data Calculation:
- Calculate the observed concentration for each well using the standard curve generated from the plate reader software, typically via a 4- or 5-parameter logistic (4PL or 5PL) curve fit [4].
Data Analysis and Interpretation
Quantitative Data from a Unified Experiment
The table below summarizes how data from the unified experiment is processed and interpreted for each validation parameter, using hypothetical data for human IL-1 beta.
Table 2: Data Analysis and Acceptance Criteria for Unified Validation
| Parameter | Sample / Dilution | Observed Conc. (pg/mL) | Expected Conc. (pg/mL) | Recovery / Accuracy | Interpretation |
|---|---|---|---|---|---|
| Spike & Recovery | Spiked Matrix (1:2) | 78.5 | 80.0 | 98.1% | Acceptable (85-115%) |
| Spiked Matrix (1:8) | 19.8 | 20.0 | 99.0% | Acceptable (85-115%) | |
| Linearity of Dilution | Spiked Matrix (1:2) | 78.5 | 78.5 | 100% | Linear (CV < 20%) |
| Spiked Matrix (1:4) | 40.1 | 39.3 | 102% | Linear (CV < 20%) | |
| Spiked Matrix (1:8) | 19.8 | 19.6 | 101% | Linear (CV < 20%) | |
| Spiked Matrix (1:16) | 9.5 | 9.8 | 96.9% | Linear (CV < 20%) | |
| Parallelism | Native Sample (1:2) | 149.9 | 131.5 | 114% | Moderate (High CV) |
| Native Sample (1:4) | 162.2 | 131.5 | 123% | Moderate (High CV) | |
| Native Sample (1:8) | 165.4 | 131.5 | 126% | Moderate (High CV) |
Interpretation of Results
The data analysis workflow below outlines the decision-making process for interpreting results from the unified experiment.
- Spike and Recovery: Recovery rates between 85% and 115% are generally considered acceptable, indicating minimal matrix interference [2]. Lower recovery suggests component inhibition, while higher recovery may signal interference.
- Linearity of Dilution: A low coefficient of variation (CV) across dilutions indicates linearity. High CV suggests matrix components affect detectability upon dilution [2].
- Parallelism: A high CV between dilutions of the native sample indicates non-parallelism, suggesting differing antibody affinity for the endogenous versus recombinant analyte [22].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Unified ELISA Validation
| Reagent / Material | Function in Unified Validation | Considerations for Selection |
|---|---|---|
| Matched Antibody Pair | Capture and detection of the target analyte in sandwich ELISA [35]. | Critical for specificity; monoclonal antibodies are preferred for sandwich ELISA to avoid cross-reactivity [35]. |
| Purified Recombinant Analyte | Used for spiking the matrix and generating the standard curve [2]. | Should be highly pure and of known concentration. The same lot should be used for spiking and standards. |
| Biological Matrix | The sample material being validated (e.g., serum, plasma, urine, CSF) [9]. | Matrix choice should reflect the intended use of the validated assay. |
| Sample Diluent | The buffer used for serial dilution of samples [2]. | Optimized to minimize matrix effects; may contain carrier proteins like BSA [2]. |
| Standard Diluent | The buffer used for dilution of the standard curve [2]. | Composition may be adjusted to more closely match the sample matrix for accurate recovery [2]. |
| Microplate Reader | Instrument for measuring absorbance, fluorescence, or luminescence [4]. | Should have software capable of generating 4PL or 5PL standard curves for accurate quantification [4]. |
The unified experimental design for assessing spike and recovery, linearity of dilution, and parallelism in a single ELISA run provides a robust, efficient, and resource-conscious validation pathway. This integrated approach offers a comprehensive view of assay performance, ensuring that analyte detection remains accurate and precise across different sample matrices and concentrations. For researchers in drug development and clinical diagnostics, this method delivers a high level of confidence in ELISA data quality while optimizing the use of valuable time and reagents.
Establishing a Complete Validation Package for Regulatory Compliance
For researchers and drug development professionals, establishing a regulatory-compliant Enzyme-Linked Immunosorbent Assay (ELISA) requires a complete validation package that objectively demonstrates assay reliability. Spike and recovery experiments form a critical component of this package, determining whether analyte detection is affected by differences between the standard curve diluent and biological sample matrices [2]. These experiments, along with parallelism and dilutional linearity assessments, provide essential data on assay accuracy and matrix effects—information that regulatory agencies like the FDA and EMA require for bioanalytical method validation [24] [69]. This guide compares experimental approaches and performance criteria for key validation experiments, providing a framework for selecting optimal strategies based on specific research needs and regulatory contexts.
Core Validation Parameters: Definitions and Regulatory Significance
A complete ELISA validation package must demonstrate consistent performance across multiple parameters that collectively prove assay reliability. The table below summarizes these core parameters, their definitions, and regulatory significance.
Table 1: Core Parameters for ELISA Validation Packages
| Validation Parameter | Definition | Regulatory Significance & Acceptance Criteria |
|---|---|---|
| Precision | Closeness of agreement between independent test results under stipulated conditions [9]. | Intra-assay CV <10%, Inter-assay CV <10% demonstrates repeatability essential for regulatory acceptance [81] [24]. |
| Accuracy (Recovery) | Closeness of agreement between measured value and accepted reference value [9]. | 80-120% recovery indicates minimal matrix interference; critical for demonstrating measurement validity [81] [1]. |
| Specificity | Ability to measure analyte distinctly in the presence of other components [24]. | Demonstrated through cross-reactivity testing with related substances; ensures minimal false positives [81] [24]. |
| Sensitivity (LLOD) | Lowest analyte concentration distinguishable from background [24]. | Determined by mean zero standard O.D. + 2 standard deviations; defines assay working range [81] [24]. |
| Linearity | Assay ability to obtain results directly proportional to analyte concentration in sample [24]. | 70-130% of expected values across dilution series; confirms accurate quantification at different concentrations [81]. |
| Parallelism | Demonstration that natural and recombinant samples are detected similarly [81]. | %CV within 20-30% indicates comparable immunoreactivity between endogenous analyte and standard [1]. |
| Robustness | Capacity to remain unaffected by small variations in method parameters [24] [9]. | Validation of incubation times, temperatures, and reagent variations; ensures reliability under normal lab conditions [9]. |
Experimental Protocols for Key Validation Experiments
Spike and Recovery Experimental Protocol
Purpose: Determine if sample matrix components affect analyte detection accuracy compared to standard diluent [2].
Procedure:
- Spike Preparation: Add a known concentration of purified analyte to both the natural sample matrix and standard diluent [2].
- Assay Execution: Run the ELISA protocol on both spiked samples using identical conditions.
- Recovery Calculation: Compare measured concentrations using the formula: Recovery % = (Measured concentration in sample matrix / Measured concentration in standard diluent) × 100 [2].
Interpretation: Recovery rates of 80-120% are generally acceptable, indicating minimal matrix interference [81] [1]. Consistent deviations outside this range suggest matrix effects requiring protocol adjustments [2].
Table 2: Troubleshooting Poor Spike and Recovery Results
| Problem | Potential Causes | Corrective Actions |
|---|---|---|
| Low Recovery (<80%) | Matrix components binding or degrading analyte [2]. | Alter standard diluent to more closely match sample matrix [2]. |
| High Recovery (>120%) | Interfering substances enhancing signal [2]. | Dilute sample in standard diluent or optimize sample diluent composition [2]. |
| Variable Recovery Across Matrices | Differential matrix effects between sample types [1]. | Incorporate matrix-matched controls for each sample type in final protocol [1]. |
Parallelism Testing Experimental Protocol
Purpose: Verify that endogenous analyte in natural samples behaves similarly to the reference standard across dilutions, confirming comparable immunoreactivity [81] [1].
Procedure:
- Sample Selection: Identify samples with high endogenous analyte concentrations [1].
- Serial Dilution: Perform 1:2 serial dilutions using appropriate sample diluent across the assay's dynamic range [81].
- Analysis: Calculate percent recovery at each dilution level relative to the expected concentration.
- Assessment: Determine if dilution curves parallel the standard curve.
Interpretation: Parallelism demonstrates that the ELISA recognizes the natural protein similarly to the recombinant standard, validating the use of the standard curve for quantifying native samples [81]. A %CV of 20-30% across dilutions typically indicates acceptable parallelism [1].
Dilutional Linearity Experimental Protocol
Purpose: Confirm that samples with analyte concentrations above the assay range can be accurately measured after dilution within the standard curve range [2].
Procedure:
- Sample Preparation: Spike sample matrix with analyte above the upper limit of quantification or use samples with high endogenous levels [2].
- Serial Dilution: Create multiple dilutions (e.g., 1:2, 1:4, 1:8, 1:16) using appropriate diluent [81].
- Calculation: For each dilution, calculate: % Linearity = (Measured concentration / Expected concentration) × 100 [81].
Interpretation: Linearity within 70-130% of expected values across dilutions indicates minimal matrix interference and accurate quantification throughout the assay range [81] [1].
Comparison of Validation Approaches and Performance Data
Method Comparison: Spike/Recovery vs. Parallelism
Table 3: Comparison of Key Validation Methodologies
| Characteristic | Spike/Recovery | Parallelism |
|---|---|---|
| Primary Objective | Assess matrix effects on analyte detection [2] | Confirm comparable immunoreactivity between standard and endogenous analyte [81] |
| Sample Requirements | Sample matrix spiked with known analyte [2] | Samples with high endogenous analyte levels [1] |
| Key Interpretation | Recovery of 80-120% indicates minimal interference [81] | Parallel curves indicate similar antibody binding characteristics [81] |
| Regulatory Focus | Accuracy and matrix effects [9] | Selectivity and assay suitability for natural samples [9] |
| Common Applications | Initial assay validation, matrix compatibility testing [2] | Final assay validation, especially for biomarker assays [1] |
Performance Data Comparison Across Sample Types
Table 4: Representative Spike and Recovery Data Across Matrices
| Sample Matrix | Spike Concentration | % Recovery | Minimum Recommended Dilution |
|---|---|---|---|
| Human Serum Extracted | 2 ng/mL | 102% | Neat [1] |
| Human EDTA Plasma Extracted | 1 ng/mL | 90% | Neat [1] |
| Mouse Serum Extracted | 0.5 ng/mL | 105.8% | 1:2 [1] |
| Human Saliva Extracted | 2.5 ng/mL | 98.7% | 1:2 [1] |
| Rat Serum Extracted | 0.25 ng/mL | 112.4% | Neat [1] |
Experimental Workflow and Signaling Pathways
The following workflow diagrams illustrate the logical relationships and experimental sequences for key validation experiments.
Spike and Recovery Experimental Workflow
Complete ELISA Validation Pathway
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful ELISA validation requires specific reagents and materials designed to maintain assay performance and reproducibility. The following table details essential components for establishing a compliant validation package.
Table 5: Essential Research Reagents for ELISA Validation
| Reagent/Material | Function in Validation | Validation-Specific Considerations |
|---|---|---|
| Reference Standards | Calibrate assay using known analyte concentrations [24]. | Should be traceable to international standards (e.g., NIBSC) [81]. |
| Quality Control Samples | Monitor assay precision and accuracy over time [24]. | Should represent low, medium, and high concentrations within dynamic range. |
| Matrix-Matched Diluents | Minimize matrix effects in spike/recovery experiments [2]. | Composition should mimic natural sample matrix as closely as possible. |
| Cross-Reactivity Panel | Demonstrate assay specificity [81]. | Should include structurally similar compounds and known isoforms. |
| Blocking Buffers | Prevent non-specific binding [24]. | Optimization required for different sample matrices. |
| Coated Microplates | Solid phase for antigen-antibody binding [14]. | Lot-to-lot consistency critical for reproducibility [81]. |
| Enzyme Conjugates | Generate detectable signal proportional to analyte [14]. | Consistent enzyme activity between lots essential. |
| Stable Substrates | Produce measurable colorimetric/chemiluminescent signal [14]. | Must demonstrate consistent performance characteristics. |
Establishing a regulatory-compliant ELISA validation package requires systematic assessment of precision, accuracy, specificity, and matrix effects through carefully designed experiments. Spike and recovery experiments provide critical data on matrix interference, while parallelism testing validates the fundamental assumption that reference standards accurately reflect native analyte behavior. The experimental protocols and performance criteria presented in this guide reflect current industry standards and regulatory expectations [81] [2] [9]. By implementing these methodologies and maintaining rigorous documentation practices, researchers can generate defensible validation data that meets compliance requirements across regulatory jurisdictions—accelerating drug development timelines and ensuring reliable biomarker measurement for critical research applications.
Conclusion
Spike and recovery experiments are a non-negotiable pillar of robust ELISA validation, directly confirming that a sample matrix does not interfere with the accurate quantification of an analyte. When integrated with dilutional linearity and parallelism assessments, they form a powerful framework that guarantees data reliability. Mastering these techniques allows researchers to not only troubleshoot and optimize existing assays but also to preemptively design more resilient methods. For the fields of drug development, clinical research, and biomarker discovery, this rigorous approach to validation is indispensable. It ensures that critical decisions are backed by high-quality, reproducible data, ultimately accelerating scientific discovery and enhancing the safety and efficacy of biopharmaceutical products. Future directions will likely involve greater harmonization of acceptance criteria and the adaptation of these fundamental principles to emerging, multiplexed immunoassay platforms.
References
- 1. Dilutional Linearity, Parallelism, Spike-and-Recovery in ... [https://www.enzo.com/note/dilutional-linearity-parallelism-spike-and-recovery-in-elisa-how-to-qc-your-results/]
- 2. Spike and Recovery and Linearity of Dilution Assessment [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/spike-recovery-linearity-assessment.html]
- 3. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOop1vdTSbvRrDcXKw_DSp3ZadddlmJXpVfzJjPqPbIseUhZ8n2FS]
- 4. Data analysis for ELISA [https://www.abcam.com/en-us/technical-resources/guides/elisa-guide/calculating-elisa-data]
- 5. ELISA Data Analysis Infographic [https://www.bio-techne.com/applications/immunoassays/elisa-infographic]
- 6. Pt. 3: How to Validate Your ELISA Assay for Reproducible, ... [https://blog.avivasysbio.com/pt.-3-how-to-validate-your-elisa-assay-for-reproducible-reliable-results]
- 7. Challenges in Allergen Testing - Spiking and Recoveries [https://www.romerlabs.com/en/library/knowledge/detail/challenges-in-allergen-testing-spiking-and-recoveries]
- 8. ELISA kit validation [https://www.bosterbio.com/elisa-validation-information?srsltid=AfmBOoqdiR6GuOkEHzJSEwV6lV8_QuawJjASTpQ53Xsakvcstm4vuhTA]
- 9. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 10. Matrix Interference in Sandwich ELISA Kits [https://assaybiotechnology.com/site/matrix-interference]
- 11. What is Matrix Interference and How Does It Affect Testing? [https://www.arborassays.com/what-is-matrix-interference/?srsltid=AfmBOoo3PqzIULtPgGm4wt2Sri6WecXWbVCvpFEuyQ8rdmkEKjSEDGTs]
- 12. Developing your own ELISA: Spike & Recovery Experiments [https://www.thermofisher.com/blog/behindthebench/developing-your-own-elisa-spike-recovery-experiments/]
- 13. Which Controls to Use in ELISA Assays? [https://www.enzo.com/note/which-controls-to-use-in-elisa-assays/]
- 14. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 15. ELISA Controls Guide [https://www.assaygenie.com/elisa-controls-guide/?srsltid=AfmBOopzdNZ2WRW-93XLLwWswfetVBmHlRLNBB9pdxNfZojLw9GNSyu7]
- 16. Managing Matrix Interference in Immunoassays: Tips and ... [https://www.bio-connect.nl/news/managing-matrix-interference-in-immunoassays-tips-and-solutions/]
- 17. Beware of Matrix Effects in Your ELISA Assay [https://advansta.com/beware-of-matrix-effects-in-your-elisa-assay/]
- 18. ELISA Diluent: Overview, Types, & Applications [https://www.excedr.com/resources/elisa-diluent]
- 19. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOopAl1L_L89YChE8SsUSOpHefpOCjfRg9hBIOh5LHKakGoX5E2ui]
- 20. ELISA Rescue Protocol: Recovery of sample ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3604139/]
- 21. How to select the right ELISA kit - Biomedica [https://www.bmgrp.com/how-to-select-the-right-elisa/]
- 22. ELISA Guide; Part 3: ELISA Optimization [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/elisa-guide-part-3-elisa-optimization/]
- 23. Assay Qualification & Sample Testing | Cygnus Technologies [https://www.cygnustechnologies.com/assay-qualification-sample-testing]
- 24. Comprehensive Guide to ELISA Assay Validation: Best Practices & Key Insights [https://www.nebiolab.com/elisa-assay-validation-guide/]
- 25. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOopy-H-xVhNz2KxBMshhvMxPhOv73WEPwxMs0p5yAJTxgf0eH2Vg]
- 26. SPR vs ELISA | Comparing techniques for biomolecular ... [https://nicoyalife.com/blog/spr-vs-elisa-comparing-techniques-for-biomolecular-detection/]
- 27. ELISA Assay Technique | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa.html]
- 28. Establishing Dilution Linearity for Your Samples in an ELISA [https://www.cygnustechnologies.com/establishing-dilution-linearity-for-your-samples-in-an-elisa?srsltid=AfmBOop3d53ppujCeg7t2w7OqCF0lEqV9eHqtqPNk-lwZYpovvMrGtcK]
- 29. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOopPCfeZ7Pww_QOuRsQNkbyG030nupQmVFnt7GcF-VILzUr1J4kY]
- 30. Performance Assessment and Comparability of a ... [https://www.sciencedirect.com/science/article/pii/S0362028X22104436]
- 31. Epitope Profiling of SARS-CoV-2 Spike Antigen Provides ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390492/]
- 32. Optimisation and Validation of a conventional ELISA and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1113194/full]
- 33. How to Analyze ELISA Data and Calculate Results [https://www.bosterbio.com/blog/post/how-to-analyze-elisa-data-and-calculate-results-step-by-step-guide-with-troubleshooting-tips?srsltid=AfmBOoouiAf8E8jGGQ_A1f9NopSce3MjnRrACgC4krgDN1bpazL72QJP]
- 34. Development and Validation of ELISA for In Vitro Diagnosis ... [https://www.mdpi.com/2673-8112/5/7/108]
- 35. ELISA: The Complete Guide [https://www.antibodies.com/applications/elisa]
- 36. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOoqQhpKMhOAhGpvO4JXTA6mpzWoUr9de4d6Fa3sw5joick9G25Yv]
- 37. Glossary of terms for ELISA [https://www.abcam.com/en-us/technical-resources/guides/elisa-guide/elisa-terms-glossary]
- 38. Development of a sandwich ELISA for the specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10473979/]
- 39. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOorgZ0COO-eZiMDjSsM9JhSUXRb8wW86y5lk0UEqdhXBgG9u9rOR]
- 40. ELISA Metrics Infographic [https://www.novusbio.com/support/support-by-application/elisa/infographic?srsltid=AfmBOopVUAroYFeyN5xjpcWA4if7901sc1Utyb9wlr0uObop6BksJ5h2]
- 41. What ELISA should I choose? [https://www.abcam.com/en-us/technical-resources/guides/elisa-guide/choose-the-right-elisa-kit]
- 42. 17 Important Data Visualization Techniques - HBS Online [https://online.hbs.edu/blog/post/data-visualization-techniques]
- 43. What Is Data Visualization? Benefits, Types & Best Practices [https://ischool.syracuse.edu/what-is-data-visualization/]
- 44. Data Visualizations, Charts, and Graphs | Digital Accessibility [https://accessibility.huit.harvard.edu/data-viz-charts-graphs]
- 45. Data Visualization Design Guidelines - The CMU Brand [https://www.cmu.edu/brand/brand-guidelines/data-viz.html]
- 46. Your Data Visualization Color Guide: 7 Best Practices | Sigma [https://www.sigmacomputing.com/blog/7-best-practices-for-using-color-in-data-visualizations]
- 47. Guidelines for Preparing ELISA Standards | Boster Bio Blog [https://www.bosterbio.com/blog/post/guidelines-for-preparing-elisa-standards?srsltid=AfmBOoqWSe-AMCafPaAwm8uz5FdKyZ9eVsAOKoSGfDyMLGhEEY8cYB0y]
- 48. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOoqP_NA97VgQ1uZ_4XrvNQaMyypHD9T-7KUXFU9VnRKU6HEszjFt]
- 49. Factors affecting the accuracy and reliability of ELISA results [https://www.mybiosource.com/learn/factors-affecting-the-accuracy-and-reliability-of-elisa-results/]
- 50. Matrix Interference of Vegetable on Enzyme-Linked ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524109/]
- 51. Insights into effects of processing and food matrices on ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625009690]
- 52. Optimized HCP Assay: Reduced Matrix Interference & ... [https://www.bioprocessintl.com/product-characterization/optimized-hcp-assay-with-reduced-matrix-interference-from-protein-a-improved-performance-in-dilution-linearity-and-spike-recovery]
- 53. How to Validate Sample Dilutions and Achieve Linearity in ... [https://www.enzo.com/note/how-to-validate-sample-dilutions-and-achieve-linearity-in-new-sample-types/]
- 54. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOop82CcNK8DGHYBi-FY95xvvPxvfhmQFZOHTeve9KMN7e6H3SzwT]
- 55. Sample Matrix Viscosity, Another Common Contributor to ... [https://www.antibodiesinc.com/pages/sample-matrix-viscosity-another-common-contributor-to-signal-inhibition-in-enzyme-immunoassays?srsltid=AfmBOoruJC20eOVmGJsvmtVb36e_8p46t4pObxyv_vIrB8ulIVsXh3F8]
- 56. Establishing Dilution Linearity for Your Samples in an ELISA [https://www.cygnustechnologies.com/establishing-dilution-linearity-for-your-samples-in-an-elisa?srsltid=AfmBOooYSPB6qbHF_jCDOfH5ZYhqHENLOMSns2Kokr48wFxxtF-WS6j2]
- 57. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOopf9Fu7kRV1kx9DFe0m1xruHRwILHNCfEmkednLcOKvxOPgaftn]
- 58. Development and Validation of an ELISA at Acidic pH for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3810116/]
- 59. ELISA Development and Optimization [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-development-optimization.html]
- 60. Antibody Validation Using the Indirect ELISA Method [https://www.addgene.org/protocols/ab-validation-indirect-elisa/]
- 61. Help & FAQs: Proteins and Enzymes [https://www.rndsystems.com/resources/faqs/proteins-and-enzymes]
- 62. BSA ELISA kit Cygnus Technologies F030 [https://www.cygnustechnologies.com/bsa-elisa-kit.html]
- 63. BSA ELISA Kit, 2G | GenScript [https://www.genscript.com/BSAelisakit.html]
- 64. Development of an ELISA for Evaluation of Swab Recovery Efficiencies of Bovine Serum Albumin | PLOS ONE [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0112876]
- 65. Guide to the Checkerboard Assay - CLYTE Technologies [https://www.clyte.tech/post/the-coolest-assay-to-learn-step-by-step-guide-to-the-checkerboard-assay?srsltid=AfmBOoq-OzWvIGZ7_XIE4t3XiSMIrqX4PG76SFO8m34Seq826ty_zS8d]
- 66. Development of a Polymicrobial Checkerboard Assay as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376321/]
- 67. Optimized Rhombic Experimental Dynamic Checkerboard ... [https://link.springer.com/article/10.1007/s11095-022-03396-7]
- 68. Antimicrobial Synergy Testing/Checkerboard Assay [https://antiviral.creative-diagnostics.com/antimicrobial-synergy-testing-checkerboard-assay.html]
- 69. Validation of Elisa protocol as per FDA Regulation for Drug ... [https://www.mybiosource.com/learn/validation-of-elisa-protocol-as-per-fda-regulation-for-drug-developmen/]
- 70. Analytical Performance of ELISA Assays in Urine [https://pmc.ncbi.nlm.nih.gov/articles/PMC4758723/]
- 71. Evaporation-driven digital ELISA with micro-droplet arrays ... [https://www.sciencedirect.com/science/article/pii/S0956566325009522]
- 72. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 73. Comparative evaluation of in-house ELISA and two ... [https://www.nature.com/articles/s41598-025-97050-y]
- 74. How to Read and Analyze ELISA Data [https://www.rndsystems.com/resources/how-to-analyze-elisa-data]
- 75. How To Perfect Your ELISA Standard Curve | Boster Bio [https://www.bosterbio.com/blog/post/how-to-perfect-your-elisa-standards?srsltid=AfmBOorqykKOB9SKkWnNLyeFVur1B8xyJ3eNtLKmsG1yBpurWbflDeTZ]
- 76. Unusual ELISA colors: What do they mean? [https://www.linkedin.com/posts/elabscience_elisa-labtips-colordetection-activity-7358225252088229888-ll1L]
- 77. ELISA: Data Analysis and Interpretation [https://www.mybiosource.com/learn/elisa-data-analysis-and-interpretation/]
- 78. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOoot9xtevcFMaZyW5fHSx3t3E39U4YQDhtx8Tn7FLzv3PS7N2ynH]
- 79. ELISA testing gets faster and more reproducible [https://www.nature.com/articles/d42473-025-00230-7]
- 80. Comparison of commercial ELISA assays for quantification ... [https://www.nature.com/articles/s41598-017-06006-4]
- 81. ELISA Kit Validation and Quality Testing [https://www.thermofisher.com/us/en/home/life-science/antibodies/immunoassays/elisa-kits/elisa-kit-validation-quality-testing.html]